Abstract
Introduction
The burden of epilepsy is thought to be high but is difficult to measure. Very few studies in Japan have attempted to estimate prevalence and incidence rates of epilepsy in Japan.
Methods
This retrospective cohort study used commercially collected nationwide insurance claims data from a cohort of 10 million persons between 2012 and 2019 among those aged 0 to 74 years. Using the claims data, cases were identified, and incidence and prevalence rates were estimated.
Results
A total of 9,864,278 persons were included. The average age was 34.5 (standard deviation, 18.5) years. A total of 77,312 persons were diagnosed with epilepsy over the 8-year observation period, with a prevalence rate of 6.0 per 1,000 persons with almost no difference by gender. The highest rates were seen among those aged 70–74 years; prevalence rates tended to rise with calendar year (5.4/1,000 in 2012 and 6.0/1,000 in 2019). The incidence rate of epilepsy was 72.1 per 100,000 person-years with slightly higher rates seen among females. Incidence rates were highest at ages less than 12 months (199.8/100,000 person-years), followed by the eldest age group (70–74 years, 179.4/100,000 person-years).
Conclusion
Understanding the magnitude of disease burden is the basis of determining health policies. In this study, the prevalence and incidence of epilepsy in Japan was shown based on the analysis results of a large-scale general population insurance claims data covering all over Japan.
Key words: epilepsy, prevalence, incidence, Japan, claims data
INTRODUCTION
Epilepsy is a neurological disorder affecting an estimated 50 million persons world-wide.1 The disease occurs in all age groups from infants to the elderly. Meta analyses of worldwide rates show large variations due to study design differences and differing case definitions.2 Recent estimates indicate that the prevalence rate is reported to be 4–8 per 1,000 persons,3,4 while the incidence rate is approximately 45–49 per 100,000 population per year in high-income countries. Rates are higher in low- and middle-income countries.2,5 As there have been few epidemiological reports on Japanese national rates of epilepsy, the burden of epilepsy among the population in Japan remains an open research question. Understanding basic epidemiological information, such as prevalence and incidence, is important as a basis for constructing effective disease control measures. “Patient survey” is one of the statistical surveys conducted by the government every 3 years in Japan to estimate the number of patients for all diseases. However, the number of cases based on the patient survey is likely underestimated. Even though patients may be diagnosed with several diseases, the patient survey makes estimates based on only one main disease for each patient. Moreover, the number of patients with chronic diseases may be underestimated, as only those whose interval visit is under 30 days are included (this criterion has been changed to 98 days since 2020). Furthermore, the patient survey cannot provide estimates of incidence. The purpose of this study was to determine the prevalence and incidence of epilepsy in Japan using a large population-based data set.
METHODS
This retrospective cohort study used monthly medical claims data collected in the Japan Medical Data Center (JMDC) database (Japan Medical Data Center, Tokyo, Japan) for 8 years from January 2012 through December 2019. The JMDC system collects information from Japanese health insurance organizations that provide health insurance to employees of large Japanese companies and their dependents.6 Persons employed by small- and medium-sized companies, National Health Insurance subscribers, or welfare recipients were not included. Also, persons certified as having a disability due to epilepsy between ages 64–74 were excluded, as they are eligible for alternative medical benefits. Insured persons could be enrolled for multiple years over the course of the observation period. Persons less than 74 years of age were eligible for the study, as that was the upper limit of persons insured by this insurance association.
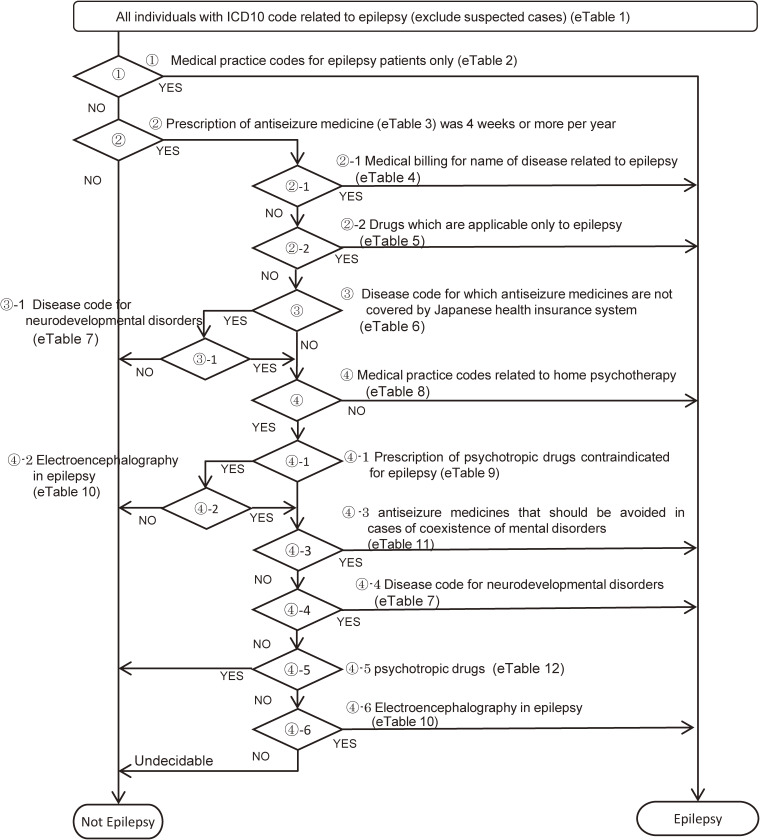
Cases were identified using diagnosis code (International Classification of Diseases, 10th revision [ICD-10]: G40 Epilepsy, G41 Status epilepticus) or a combination of epilepsy-related injury/illness codes and medications. This definition does not include febrile convulsions (ICD10: R56.0). The decision tree was designed to only select those with epilepsy, excluding suspected cases, and included a verification step where results were checked on a month-by-month basis to optimize the algorithm (Figure 1, eTable 1, eTable 2, eTable 3, eTable 4, eTable 5, eTable 6, eTable 7, eTable 8, eTable 9, eTable 10, eTable 11, and eTable 12). This decision tree was developed through discussion with multiple expert physicians for epilepsy belonging to the Ministry of Health, Labour and Welfare research group.
Figure 1. Decision tree for identifying those with epilepsy.
After identifying the unique (non-duplicate) target population and cases, the prevalence of epilepsy by sex and age group was calculated as the ratio of cases to eligible health insurance association members. Prevalence was calculated by year as well as for the 8-year period from January 2012 through December 2019. Prefecture-specific prevalence rates could not be calculated, as prefecture information was not available on the supplied records. The 95% confidence intervals (CIs) were estimated using Wald’s method. The prevalence of epilepsy were compared by calendar year using the Cochran-Armitage test.
The incidence of epilepsy was calculated as the rate of new cases over the 8-year follow-up period (January 2012 through December 2019) divided by the person-years at risk. Prior claims were available back to 2005 (earliest), and persons known to have been diagnosed with epilepsy prior to January 2012 (based on “date of start treatment”) were excluded from the analysis. Cases diagnosed within 1 year of joining JMDC were censored because the possibility that the diagnosis was due to a change in insurance. The 95% CIs were estimated using the Poisson distribution for incidence as follows:
where r and T are the number of new cases detected during the observational period and the total observed person-years, respectively. was the upper 97.5% point of a χ2 distribution with 2r degrees of freedom (df) and the upper 2.5% point of a χ2 distribution with 2r + 2 df.
The incidence rate at ages less than 12 months and the eldest age group (70–74 years) were compared to the other age groups using Z test adjusted using the Bonferroni test. Z-variable is obtained as follows:
where I1 and I2 denoted the incidence rates, r1 and r2 denoted the number of new cases of epilepsy, and T1 and T2 were the observation periods (person-years). The crude P-value was obtained by calculating the upper probability of Z under the normal distribution and adjusted using the Bonferroni method.
This study was conducted after obtaining permission from the Ethical Review Committee for Epidemiological Research at Hiroshima University for ethical review of medical research (epidemiology) involving human subjects (Permission No.: E-2298). The claims data used for the analysis is existing information after anonymization. Individuals cannot be identified and no disadvantage to any subjects is anticipated.
RESULTS
A total of 9,864,278 eligible individuals were identified over the 8-year period from January 2012 through December 2019. Insured subjects could be enrolled for multiple years over the course of the observation period. The number of eligible subjects enrolled in a 1-year period ranged from 1,785,253 persons in 2012 to 7,442,394 persons in 2019 (Table 1).
Table 1. Count of eligible persons included in the study based on the JMDC Claims Database, by year.
| Year | Number of health insurance subscribers |
| 2012 | 1,785,253 |
| 2013 | 2,824,800 |
| 2014 | 2,979,938 |
| 2015 | 4,174,628 |
| 2016 | 5,202,333 |
| 2017 | 6,199,167 |
| 2018 | 7,236,266 |
| 2019 | 7,442,394 |
| Total* | 9,864,278 |
JMDC, the Japan Medical Data Center.
*Excluding duplicates.
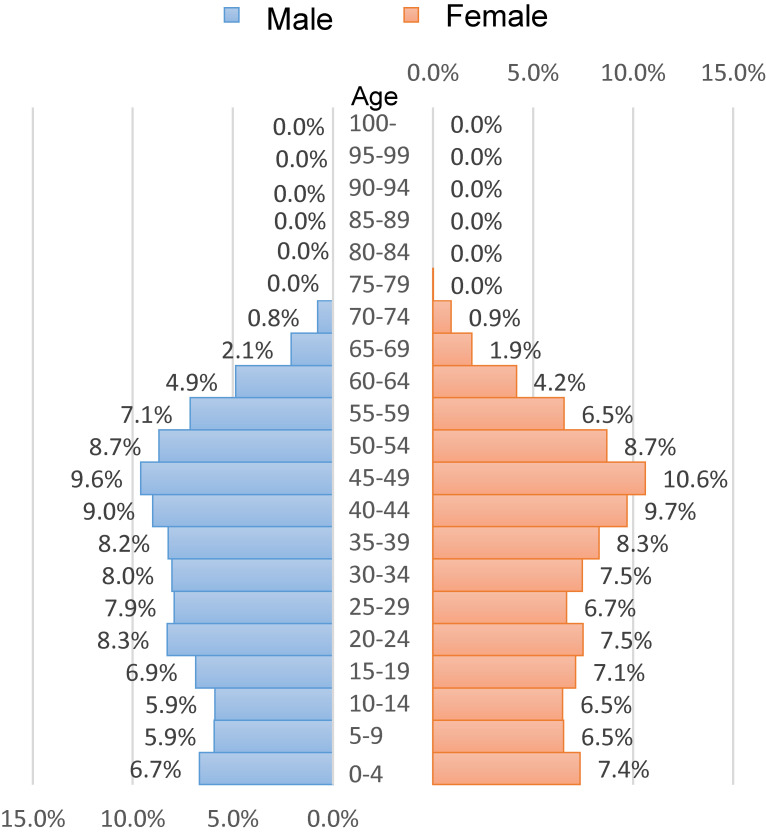
The average age of 7,442,394 persons in 2019 was 34.5 (standard deviation, 18.5) years, and males comprised 53.7% of the sample. The distribution of persons by age and sex is shown in Figure 2. For each sex, 45–49 years old was the most common 5-year age group.
Figure 2. Age distribution by sex of the study population in 2019 (N = 7,442,394).
A total of 77,312 persons were diagnosed with epilepsy over the follow-up period. The prevalence of epilepsy was 6.0 per 1,000 population with almost no difference by gender (6.1 for males and 5.8 for females in 2019). The secular change in epilepsy prevalence from 2012 to 2019 was a slight upward trend (5.4/1,000 population in 2012 rising to 6.0/1,000 in 2019) (trend P < 0.0001). This upward trend was seen in both males (5.4–6.1/1,000) and females (5.4–5.8/1,000) (both trend P < 0.0001) (Table 2).
Table 2. Count persons, prevalent cases, and prevalence rates, by calendar year and sex.
| Year | Total | Male | Female | |||||||||
|
| ||||||||||||
| Persons (n) |
Prevalent Cases (n) |
Prevalence Rate per 1,000 |
Trend P* | Persons (n) |
Prevalent Cases (n) |
Prevalence Rate per 1,000 |
Trend P* | Persons (n) |
Prevalent Cases (n) |
Prevalence Rate per 1,000 |
Trend P* | |
| 2012 | 1,785,253 | 9,705 | 5.4 | P < 0.0001 | 1,001,565 | 5,456 | 5.4 | P < 0.0001 | 783,688 | 4,249 | 5.4 | P < 0.0001 |
| 2013 | 2,824,800 | 15,319 | 5.4 | 1,568,664 | 8,476 | 5.4 | 1,256,136 | 6,843 | 5.4 | |||
| 2014 | 2,979,938 | 16,355 | 5.5 | 1,656,390 | 9,076 | 5.5 | 1,323,548 | 7,279 | 5.5 | |||
| 2015 | 4,174,628 | 23,436 | 5.6 | 2,302,577 | 12,991 | 5.6 | 1,872,051 | 10,445 | 5.6 | |||
| 2016 | 5,202,333 | 29,950 | 5.8 | 2,867,978 | 16,645 | 5.8 | 2,334,355 | 13,305 | 5.7 | |||
| 2017 | 6,199,167 | 36,129 | 5.8 | 3,372,022 | 19,988 | 5.9 | 2,827,145 | 16,141 | 5.7 | |||
| 2018 | 7,236,266 | 42,736 | 5.9 | 3,897,629 | 23,481 | 6 | 3,338,637 | 19,255 | 5.8 | |||
| 2019 | 7,442,394 | 44,568 | 6 | 3,995,265 | 24,474 | 6.1 | 3,447,129 | 20,094 | 5.8 | |||
*Cochran-Armitage test.
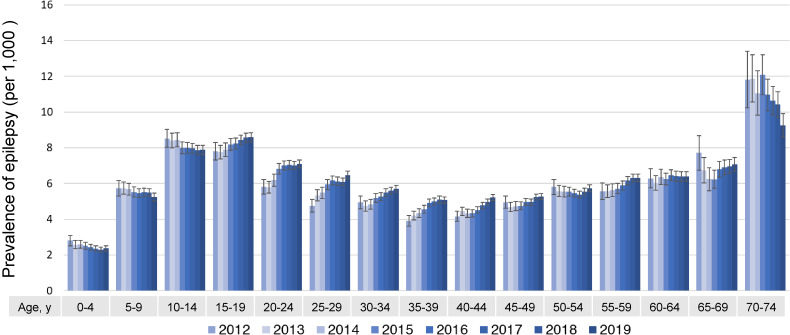
By age group, the prevalence of epilepsy in the 70–74 age group was the highest compared to other age groups (9.2/1,000 in 2019), followed by those in their teens (15–19 years: 8.6/1,000; 10–14 years: 7.9/1,000 in 2019) (Figure 3).
Figure 3. Prevalence of epilepsy by year and age group.
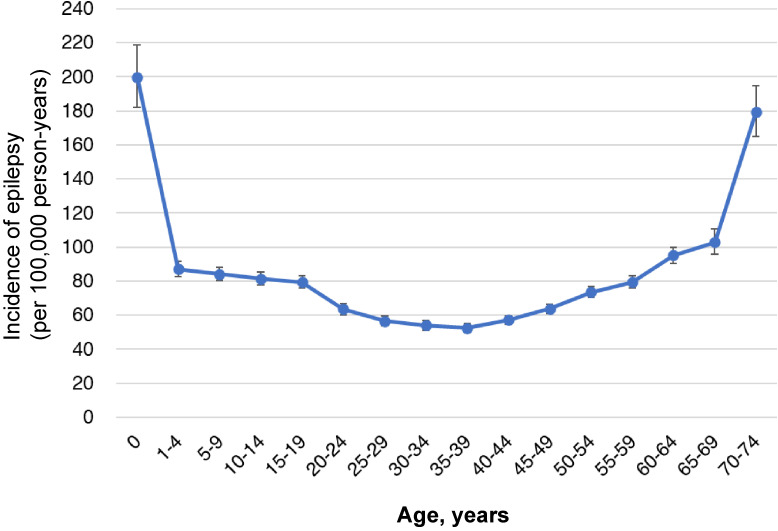
Among the 77,312 subjects diagnosed with epilepsy, 47,387 were diagnosed prior to January 2012. Another 5,925 subjects were diagnosed with epilepsy within 1 year of joining the health insurance association and were censored from the incidence calculation. Therefore, there were 24,000 incident cases among 33,299,234 eligible person-years of follow-up from 2012–2019 resulting in an incidence rate of 72.1 per 100,000 person-years (95% CI, 71.2–73.0/100,000 person-years). The incident rate in females (73.7; 95% CI, 72.3–75.1/100,000 PY) was slightly higher than that observed in males (70.7; 95% CI, 69.5–72.0/100,000 PY) (Table 3). By age group, the incidence rate was highest at ages less than 12 months (199.8; 95% CI, 182.1–218.7/100,000), followed by the eldest age group (70–74 years) at rates of 179.4/100,000 person-years (95% CI, 164.9–194.7/100,000 person-years), which was significantly higher than the other age groups (P < 0.0001). A U-shaped curve was observed (Figure 4). The age-specific complication rates of stroke (ICD-10: I63, I69) and Alzheimer’s disease (ICD-10: G30) in epilepsy patients were shown in Table 4. Among epileptic patients aged 70–74 years, 24.1% had stroke, 15.1% had post-stroke sequelae, and 12.8% had Alzheimer’s disease.
Table 3. Incidence of epilepsy (per 100,000 person-years) observed in the cohort over the period 2012–2019, by sex.
| Persons (n) |
Person-Years | Number of incident cases | Incidence Rate (per 100,000 person-years) |
95% CI | |
| Total | 9,816,891 | 33,299,234 | 24,000 | 72.1 | 71.2–73.0 |
| Male | 5,139,227 | 18,401,137 | 13,018 | 70.7 | 69.5–72.0 |
| Female | 4,677,664 | 14,898,098 | 10,982 | 73.7 | 72.3–75.1 |
Figure 4. Incidence rate of epilepsy by age (with 95% CIs). CI, confidence interval.
Table 4. The age-specific complication rates of stroke (ICD10: I63, I69) and Alzheimer’s disease (ICD10: G30) in epilepsy patients.
| ICD10 | ICD-10 Disease name |
Number of epilepsy patients by age group | |||||||||||||||||
|
| |||||||||||||||||||
| 0–9 years N = 3,881 |
10–19 years N = 3,658 |
20–29 years N = 2,725 |
30–39 years N = 2,890 |
40–49 years N = 4,043 |
50–59 years N = 3,950 |
60–69 years N = 2,284 |
70–74 years N = 569 |
Total N = 24,000 |
|||||||||||
| I63 | Stroke | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 365 | 15.9% | 137 | 24.1% | 502 | 2.1% |
| I69 | Post-stroke sequelae | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 265 | 11.6% | 86 | 15.1% | 351 | 1.5% |
| G30 | Alzheimer’s disease | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 73 | 12.8% | 73 | 1.4% |
ICD-10, International Classification of Diseases, 10th revision.
DISCUSSION
Patients with epilepsy worldwide were estimated to be 45.9 million in 2016 using a simulation model, and the age-standardized prevalence in Japan was 130 to <180 per 100,000 population, which was lower than that of the world.7 Understanding the magnitude of disease burden is the basis of determining health policies. In this study, we estimated the prevalence and incidence of epilepsy in Japan using a large-scale claims-based database consisting of approximately 10 million people (2012–2019) aged between 0 and 74 years covered all over Japan. In this study, the prevalence of epilepsy (2012–2019) was calculated to be 5.4–6.0 per 1,000 population. This result is consistent with reports on epilepsy prevalence in Asia: 6 per 1,000 population.8 The prevalence in Europe is at the same level: 4.5–5.0 in children and 6.0–7.0 in adults per 1,000 population,9 but it is higher in Africa and South America (15 per 1,000 in sub Saharan Africa and 18 per 1,000 in Latin America).8 A population-based study from Japan surveying residents aged 40 and over reported a prevalence of epilepsy of 6.9 per 1,000.10 Another population-based study of children aged younger than 13 years reported that the prevalence of epilepsy, including febrile convulsions, was 8.8 per 1,000, and the prevalence of epilepsy, excluding febrile convulsions, was 5.3 per 1,000.11 However, both were reports of surveys in limited areas. A nationwide statistical survey conducted in 2020 in Japan reported a prevalence of 3.3 per 1,000 population (3.7 for male, 3.0 for female), which was lower than the results of this study.12 The number of patients from the patient survey may have been underestimated, as mentioned above. The prevalence of epilepsy was nearly the same for both sexes, and this result was consistent with previous reports.2,9,10
The prevalence of epilepsy by age group in developed countries is known to be highest in the elderly, because symptomatic epilepsy associated with stroke or Alzheimer’s disease increases with age.9,13,14 This study also showed a high comorbidity of stroke and Alzheimer’s disease among subjects who were 70–74 years old. In the present study, the prevalence of epilepsy in the age group of 70–74 years was the highest compared to other age groups, followed by those in their teens. The influence of benign childhood epilepsy with a short disease duration may be one of the reasons why the prevalence of epilepsy in teenagers is higher than in other age groups.
The incidence of epilepsy in females was slightly higher than that in males. By age group, the incidence of epilepsy was highest at less than 12 months of age, followed by the age group 70–74 years. These age-dependent incidence trends were similar to previously reported studies.15–18
This is the first report to estimate the incidence of epilepsy based on large-scale insurance claims in Japan. These estimates, based on a large representative cohort covering subjects aged 0–74 in all regions of Japan, are important, as they help determine public health needs, such as building a medical system for epilepsy patients through cooperation between general practitioners and specialists, as well as enhancing support systems for families in Japan. The incidence calculated by this study is about 1.5 times higher than the incidence of 45–49/100,000 person-years obtained from previous meta-analysis reports in developed countries.2,5 Since insurance claims are documents for medical billing, they may be artificially inflated, so the possibility of overestimation cannot be ruled out. However, we guarded against this bias by taking the following measures: (1) comparing diagnoses in chronological order, (2) adopting information that includes epilepsy guidance fees, and (3) collecting information on antiseizure medicine drug administration. On the other hand, it is also possible that past reports were underestimated due to selection bias. This study suggests that the incidence of epilepsy may be higher than conventionally recognized, suggesting the need to further evaluation to confirm that support system for epilepsy patients and their families are sufficient.
Limitations
There were several study limitations that may reduce the generalizability of its conclusions. While the cohort included nearly 10 million persons, it was limited to those employed by large companies and their dependents younger than 75 years old, which did not include employees of small- and medium-sized companies, National Health Insurance subscribers, or welfare recipients. This suggests that the representativeness of this population for the Japanese population is limited but should provide important initial results based on Japanese population data. Other exclusions included persons certified as having a disability due to epilepsy between ages 64–74, as they are eligible for alternative medical benefits. As a result, there is a possibility that the number of epilepsy patients in the 64–74 years age group could be slightly underestimated. As for the definition of epilepsy, a validation study was not performed, though the decision tree of this study was developed with multiple expert physicians. In addition, analysis of the type of epilepsy was not possible because detailed classification of epilepsy was often not listed in the medical claims. However, even with those limitations, there have been very few epidemiological studies reporting the burden of epilepsy in a large general population covering all of Japan, meaning that the results of this study should be important for evaluating disease control policies for epilepsy in Japan. To understand the prevalence and incidence of epilepsy among all ages, including those aged 75 years and older, analysis using National Database of Health Insurance Claims and Specific Health Checkups of Japan (NDB) is desired in the future.
ACKNOWLEDGEMENTS
We thank Eric Grant for supporting the development of this manuscript.
Ethics approval and consent to participate: The ethics committee for epidemiological research of Hiroshima University approved this study (approval number, E-2298). All study activities were performed in accordance with the Declaration of Helsinki and relevant guidelines and regulations in Japan.
Availability of data and materials: The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Funding sources: This study was supported in part by a Grant-in-Aid from the Ministry of Health Labor and Welfare of Japan (grant number 19GC1013). The funder had no role in the study design, data collection, analysis, interpretation, or manuscript preparation.
Authors’ contributions: Study concept and design: JT. Acquisition of data: JT. Data management: AK. Data analysis: AK, AS TA and JT. Statistical analysis: AK, AS, TA, and JT. Interpretation of data: AK, AS, HY, KI and JT. Manuscript development: AS and JT. Study supervision: HY, KI and JT. All authors reviewed and approved the final version of the manuscript.
Conflicts of interest: None declared.
SUPPLEMENTARY MATERIAL
The following is the supplementary data related to this article:
eTable 1. List of ICD-10 codes related to epilepsy
eTable 2. List of Japan’s original code of medical billing for medical practice for epilepsy patients
eTable 3. List of antiseizure medicine
eTable 4. List of Japan’s original code of medical billing for name of disease related to epilepsy
eTable 5. List of the codes specified by the Ministry of Health, Labor and Welfare Japan for drugs which are applicable only to epilepsy
eTable 6. List of disease codes for which antiseizure medicine are not covered by Japanese health insurance system
eTable 7. List of disease name codes for neurodevelopmental disorders
eTable 8. List of medical practice codes related to home psychotherapy for outpatients
eTable 9. List of drug codes for psychotropic drugs contraindicated for epilepsy
eTable 10. List of medical practice codes for electroencephalography in epilepsy
eTable 11. List of drug codes of antiseizure medicine that should be avoided in cases of coexistence of mental disorders
eTable 12. List of psychotropic drugs
REFERENCES
- 1.World Health Organization. Epilepsy Fact Sheet. Available at: https://www.who.int/news-room/fact-sheets/detail/epilepsy. Accessed 5 May 2022.
- 2.Fiest KM, Sauro KM, Wiebe S, et al. Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies. Neurology. 2017;88:296–303. 10.1212/WNL.0000000000003509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fisher RS, Acevedo C, Arzimanoglou A, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55:475–482. 10.1111/epi.12550 [DOI] [PubMed] [Google Scholar]
- 4.Fisher RS, van Emde Boas W, Blume W, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46:470–472. 10.1111/j.0013-9580.2005.66104.x [DOI] [PubMed] [Google Scholar]
- 5.Ngugi AK, Kariuki SM, Bottomley C, Kleinschmidt I, Sander JW, Newton CR. Incidence of epilepsy: a systematic review and meta-analysis. Neurology. 2011;77:1005–1012. 10.1212/WNL.0b013e31822cfc90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kimura S, Sato T, Ikeda S, Noda M, Nakayama T. Development of a database of health insurance claims: standardization of disease classifications and anonymous record linkage. J Epidemiol. 2010;20:413–419. 10.2188/jea.JE20090066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Collaborators GE . Global, regional, and national burden of epilepsy, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:357–375. 10.1016/S1474-4422(18)30454-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mac TL, Tran DS, Quet F, Odermatt P, Preux PM, Tan CT. Epidemiology, aetiology, and clinical management of epilepsy in Asia: a systematic review. Lancet Neurol. 2007;6:533–543. 10.1016/S1474-4422(07)70127-8 [DOI] [PubMed] [Google Scholar]
- 9.Forsgren L, Beghi E, Oun A, Sillanpää M. The epidemiology of epilepsy in Europe - a systematic review. Eur J Neurol. 2005;12:245–253. 10.1111/j.1468-1331.2004.00992.x [DOI] [PubMed] [Google Scholar]
- 10.Tanaka A, Hata J, Akamatsu N, et al. Prevalence of adult epilepsy in a general Japanese population: the Hisayama study. Epilepsia Open. 2019;4:182–186. 10.1002/epi4.12295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oka E, Ohtsuka Y, Yoshinaga H, Murakami N, Kobayashi K, Ogino T. Prevalence of childhood epilepsy and distribution of epileptic syndromes: a population-based survey in Okayama, Japan. Epilepsia. 2006;47:626–630. 10.1111/j.1528-1167.2006.00477.x [DOI] [PubMed] [Google Scholar]
- 12.Ministry of Health, Labour and Welfare Japan. Report of the patient survey 2020. https://www.e-stat.go.jp/stat-search/files?page=1&toukei=00450022&tstat=000001031167&tclass1=000001166809&tclass2=000001166811&tclass3=000001166812&tclass4=000001166813.
- 13.Olafsson E, Hauser WA. Prevalence of epilepsy in rural Iceland: a population-based study. Epilepsia. 1999;40:1529–1534. 10.1111/j.1528-1157.1999.tb02036.x [DOI] [PubMed] [Google Scholar]
- 14.Sen A, Jette N, Husain M, Sander JW. Epilepsy in older people. Lancet. 2020;395:735–748. 10.1016/S0140-6736(19)33064-8 [DOI] [PubMed] [Google Scholar]
- 15.Hauser WA, Annegers JF, Kurland LT. Incidence of epilepsy and unprovoked seizures in Rochester, Minnesota: 1935–1984. Epilepsia. 1993;34:453–468. 10.1111/j.1528-1157.1993.tb02586.x [DOI] [PubMed] [Google Scholar]
- 16.Olafsson E, Hauser WA, Ludvigsson P, Gudmundsson G. Incidence of epilepsy in rural Iceland: a population-based study. Epilepsia. 1996;37:951–955. 10.1111/j.1528-1157.1996.tb00532.x [DOI] [PubMed] [Google Scholar]
- 17.Wallace H, Shorvon S, Tallis R. Age-specific incidence and prevalence rates of treated epilepsy in an unselected population of 2,052,922 and age-specific fertility rates of women with epilepsy. Lancet. 1998;352:1970–1973. 10.1016/S0140-6736(98)04512-7 [DOI] [PubMed] [Google Scholar]
- 18.Christensen J, Vestergaard M, Pedersen MG, Pedersen CB, Olsen J, Sidenius P. Incidence and prevalence of epilepsy in Denmark. Epilepsy Res. 2007;76:60–65. 10.1016/j.eplepsyres.2007.06.012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.