Abstract
Purpose
To understand the influence of the coronavirus disease 2019 (COVID-19) pandemic on clinical autonomic education and research in Europe.
Methods
We invited 84 European autonomic centers to complete an online survey, recorded the pre-pandemic-to-pandemic percentage of junior participants in the annual congresses of the European Federation of Autonomic Societies (EFAS) and European Academy of Neurology (EAN) and the pre-pandemic-to-pandemic number of PubMed publications on neurological disorders.
Results
Forty-six centers answered the survey (55%). Twenty-nine centers were involved in clinical autonomic education and experienced pandemic-related didactic interruptions for 9 (5; 9) months. Ninety percent (n = 26/29) of autonomic educational centers reported a negative impact of the COVID-19 pandemic on education quality, and 93% (n = 27/29) established e-learning models. Both the 2020 joint EAN–EFAS virtual congress and the 2021 (virtual) and 2022 (hybrid) EFAS and EAN congresses marked higher percentages of junior participants than in 2019. Forty-one respondents (89%) were autonomic researchers, and 29 of them reported pandemic-related trial interruptions for 5 (2; 9) months. Since the pandemic begin, almost half of the respondents had less time for scientific writing. Likewise, the number of PubMed publications on autonomic topics showed the smallest increase compared with other neurological fields in 2020–2021 and the highest drop in 2022. Autonomic research centers that amended their trial protocols for telemedicine (38%, n = 16/41) maintained higher clinical caseloads during the first pandemic year.
Conclusions
The COVID-19 pandemic had a substantial negative impact on European clinical autonomic education and research. At the same time, it promoted digitalization, favoring more equitable access to autonomic education and improved trial design.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10286-023-00985-3.
Keywords: COVID-19 pandemic, Autonomic nervous system, Clinical autonomic education, Clinical autonomic research, e-Learning, Telemedicine
Introduction
With the rise of herd immunity, four years into the coronavirus disease 2019 (COVID-19) pandemic, diminishing numbers of newly diagnosed COVID-19 cases and deaths are registered worldwide [36]. Notwithstanding, the COVID-19 pandemic brought major changes to our society and healthcare systems, the consequences of which are still being dealt with. Beyond the global drug [19] and medical device shortages [29], supply chain disruptions [6, 35], and increased healthcare workers’ burden [18, 22, 26], the COVID-19 pandemic directly affected clinical neurological practice in multiple ways. In the field of autonomic nervous system disorders, many referral centers were forced throughout Europe to stop their activities due to pandemic containment measures, with major consequences on the quality and continuity of autonomic healthcare provision [4, 12]. On the other hand, both COVID-19 and, to a lesser extent, COVID-19 vaccines were reportedly associated with new diagnoses or significant worsening of previously diagnosed cardiovascular autonomic disorders, increasing the number of individuals requiring specialized autonomic care [12, 13, 30].
Studies among neurology trainees and teachers highlighted how the COVID-19 pandemic negatively influenced not only clinical practice, but also bedside learning and training of neurological skills [9, 15, 32]. Likewise, the pandemic outbreak severely impacted neurological research, with several non-COVID-19-related clinical trials being put on hold, not initiated at all, or undergoing substantial amendments to mitigate the pandemic-related recruitment losses and drop-outs [2, 5, 9].
It is however still unknown how and to what extent the COVID-19 pandemic influenced the educational and research activities in neurology subspecialties with limited availability of referral centers across European countries, such as the autonomic field. To answer this question, the European Federation of Autonomic Societies (EFAS) and the Scientific Panel for Autonomic Nervous System Disorders of the European Academy of Neurology (EAN) launched a joint web-based survey among the European neurological autonomic centers investigating the influence of the COVID-19 pandemic on clinical autonomic education and research.
Methods
Survey participants
A comprehensive description of the survey methodology has been previously published [16]. Briefly, we invited all the directors of neurology-driven and interdisciplinary (i.e., with at least one neurologist in the core team) European autonomic centers to complete a web-based survey between September and November 2021. Up to three reminders were sent to nonrespondents prior to the survey closure.
Questionnaire
The questionnaire covered the following topics (see full text in the Supplementary Material):
Demographic information of the survey respondents and characteristics of the autonomic center, including equipment, staff and pre-pandemic-to-pandemic caseload;
Influence of the COVID-19 pandemic on autonomic educational activities and lessons learned for an improved autonomic educational offer;
Influence of the COVID-19 pandemic on clinical autonomic research, time availability for scientific writing, and lessons learned for an optimized autonomic research practice.
COVID-19 pre-pandemic-to-pandemic proportion of junior participants in international neurological congresses
To understand the effect of in-person versus virtual or hybrid congress formats on the proportion of junior participants attending the annual general neurology (i.e., EAN) and autonomic subspecialty congresses (i.e., EFAS), we asked the EAN head office and the organizers of the 2019–2022 EFAS congresses about the overall number of congress participants and registered junior participants (residents, research fellows, and undergraduate students).
COVID-19 pre-pandemic-to-pandemic publication output in different neurological subspecialties
For comparison purposes, we searched the PubMed database for the 2017–2022 number of publications/year on autonomic versus other main neurological disorders and subspecialties using the search terms reported in the Supplementary Material. The count included all types of manuscripts without language restrictions. The annual percentage change in the number of publications was plotted separately for each neurology subspecialty for visual comparison.
Statistical analysis
Qualitative variables were summarized in frequencies (percentages) and compared using the chi-square or Fisher exact test. Quantitative variables were summarized in median values (25th; 75th percentile) or mean ± standard deviation. The Mann–Whitney U-test was used for comparing non-normally distributed quantitative variables, the t test for normally distributed ones. Associations between variables were tested with the Spearman’s correlation coefficient. All statistical analyses were performed with IBM-SPSS (version 25). Two-sided P values < 0.05 were considered statistically significant.
Firstly, we performed a descriptive analysis of the characteristics of the survey respondents and autonomic centers involved in autonomic education compared with those respondents who were not. We then assessed the influence of the COVID-19 pandemic on the availability and quality of clinical autonomic education. Whenever the number of respondents was more than eight per subgroup, we determined whether the respondent or center characteristics, including their geographical localization [16], were significantly associated with any educational outcome measure.
Secondly, we summarized the characteristics of the centers actively involved in clinical autonomic research versus those that were not. Afterwards, we analyzed how the COVID-19 pandemic influenced the research performance of the respondents, including time availability for paper and grant writing. Whenever an adequate sample size was available (i.e., more than eight respondents per subgroup), we determined whether any specific respondent or center characteristic was significantly associated with the reported changes in research practice.
Open-ended questions on lessons learned from the COVID-19 pandemic for an improved autonomic education and research practice were analyzed with a semiquantitative technique.
Thirdly, we documented the pre-pandemic-to-pandemic percentage of junior participants in the annual EAN and EFAS congresses, and the annual percentage change in the number of PubMed publications on autonomic versus other main neurological disorders.
Data availability statement
The first and the last authors take full responsibility for the integrity of data and agree to share any de-identified data not published herewith upon reasonable request from any qualified investigator.
Results
Survey respondents
Forty-six out of 84 (55%) directors of clinical autonomic centers from 22 European countries answered the survey. Detailed information on the respondents and center characteristics has been previously published [16]. Briefly, the respondents and autonomic centers showed homogeneous characteristics across Europe, but their geographical distribution was skewed towards Northern/Western European countries compared with Southern/Eastern European ones [16].
Twenty-nine (63%) survey respondents were reportedly involved in autonomic educational activities, without differences in terms of demographic characteristics, years of clinical practice, or geographical localization with respect to respondents not involved in autonomic education (Table 1). The percentage of autonomic centers closed during the COVID-19 pandemic and the length of such closures also did not differ between centers that were or were not involved in autonomic education (Table 1). Notwithstanding, centers involved in autonomic education performed a higher number of tilt-table tests (TTT) (p = 0.016) and autonomic outpatient visits (p = 0.034) in the first pandemic year compared with those not involved in educational activities (Table 1).
Table 1.
Characteristics and COVID-19 pre-pandemic-to-pandemic clinical caseloads of the European autonomic centers involved versus non-involved in clinical autonomic education and research
| Variable | Clinical autonomic education | Clinical autonomic research | |||
|---|---|---|---|---|---|
| Involved labs | Non-involved labs | p value | Involved labs | Non-involved labs | |
| (n = 29) | (n = 17) | (n = 41) | (n = 5) | ||
| Head of the laboratory | |||||
| Female (%) | 9 (31%) | 9 (52.9%) | 0.212 | 17 (41.5%) | 1 (20%) |
| Age (years) | |||||
| 30–39 | 5 (17.2%) | 3 (17.6%) | 0.689 | 8 (19.5%) | 0 |
| 40–49 | 15 (51.7%) | 6 (35.3%) | 20 (48.8%) | 1 (20%) | |
| 50–59 | 7 (24.1%) | 7 (41.2%) | 10 (24.4%) | 4 (80%) | |
| 60–69 | 2 (6.9%) | 1 (5.9%) | 3 (7.3%) | 0 | |
| Years into practice | |||||
| Resident | 1 (3.4%) | 1 (5.9%) | 0.235 | 2 (4.9%) | 0 |
| Junior consultant (0–4 years) | 0 | 1 (5.9%) | 1 (2.4%) | 0 | |
| Consultant (5–9 years) | 3 (10.3%) | 1 (5.9%) | 4 (9.8%) | 0 | |
| Senior consultant (10–19 years) | 13 (44.8%) | 3 (17.6%) | 15 (36.6%) | 1 (20%) | |
| > 20 years | 12 (41.4%) | 11 (64.7%) | 19 (46.3%) | 4 (80%) | |
| Geographical localization* | 20 (69%):9 (31%) | 10 (59%):7 (41%) | 0.534 | 25 (61%):16 (39%) | 5 (100%):0 (0%) |
| Cumulative number of staff members | 9 (7–12) | 7 (6–13) | 0.755 | 8 (6–12) | 10 (8–24) |
| No. of TTT/year before COVID-19 | 150 (55; 300) | 50 (42; 175) | 0.06 | 120 (50; 252) | 40 (24; 200) |
| No. of outpatient visits/year before COVID-19 | 220 (150; 400) | 113 (65; 250) | 0.06 | 200 (100; 340) | 100 (;) |
| No. of inpatient visits/year before COVID-19 | 20 (5; 95) | 50 (1; 125) | 0.79 | 25 (5; 118) | 4 (;) |
| No. of TTT in the 1st pandemic year | 66 (30; 161) | 20 (1; 75) | 0.016 | 60 (20; 118) | 15 (5; 145) |
| No. of outpatient visits in the 1st pandemic year | 140 (50; 235) | 45 (15; 90) | 0.034 | 110 (40; 210) | 80 (;) |
| No. of inpatient visits in the 1st pandemic year | 10 (2; 43) | 7 (0; 38) | 0.438 | 10 (1; 46) | 3 (;) |
| Percentage reduction in TTT/year | −50% (−67%; −27%) | −47% (−92%; −20%) | 0.45 | −50% (−75%; −24%) | −29% (−80%; −10%) |
| Percentage reduction in outpatient visits/year | −43% (−61%; −10%) | −50% (−72%; −10%) | 0.563 | −50% (−66%; −18%) | −20% (;) |
| Percentage reduction in inpatient visits/year | −50% (−86%; −14%) | −56% (−98%; −23%) | 0.41 | −53% (−88%; −20%) | −35% (;) |
| No. of inhabitants in the referral area | |||||
| ≤ 500,000 | 6 (20.7%) | 6 (35.3%) | 0.651 | 9 (22%) | 3 (60%) |
| 500,000–1,000,000 | 13 (44.8%) | 7 (41.2%) | 18 (43.9%) | 2 (40%) | |
| 1,000,000–5,000,000 | 9 (31%) | 3 (17.6%) | 12 (29.3%) | 0 | |
| > 5,000,000 | 1 (3.4%) | 1 (5.9%) | 2 (4.9%) | 0 | |
| Closure of TTT labs during the pandemic | 21 (75%) | 10 (58.8%) | 0.326 | 29 (72.5%) | 2 (40%) |
| Length of closure of the TTT labs, in months | 2 (2; 5) | 5 (4; 9) | 0.072 | 5 (2; 9) | 2 (;) |
| Closure of outpatient clinics during the pandemic | 17 (60.7%) | 10 (58.8%) | 1 | 25 (62.5%) | 2(40%) |
| Length of closure of outpatient clinics, in months | 2 (2; 5) | 5 (2; 9) | 0.486 | 5 (2; 9) | 2 (;) |
| Closure of inpatient clinics during the pandemic | 12 (42.9%) | 8 (47.1%) | 1 | 20 (50%) | 0 |
| Length of closure of inpatient clinics, in months | 2 (2; 8) | 5 (2; 9) | 0.348 | 2 (2; 9) | – |
Comparisons between centers involved and non-involved in clinical autonomic research were not performed due to the low number of centers not involved in research (n = 5)
Statistically significant differences are highlighted in bold
No./n , number; TTT, tilt-table tests
*Northern/Western Europe versus Southern/Eastern Europe
Most survey respondents were involved in autonomic research (89%, n = 41), mainly focused on autonomic failure in movement disorders, postural orthostatic tachycardia syndrome and reflex syncope (Table 1) [16]. No subgroup comparison was therefore performed.
Impact of the COVID-19 pandemic on clinical autonomic education in Europe
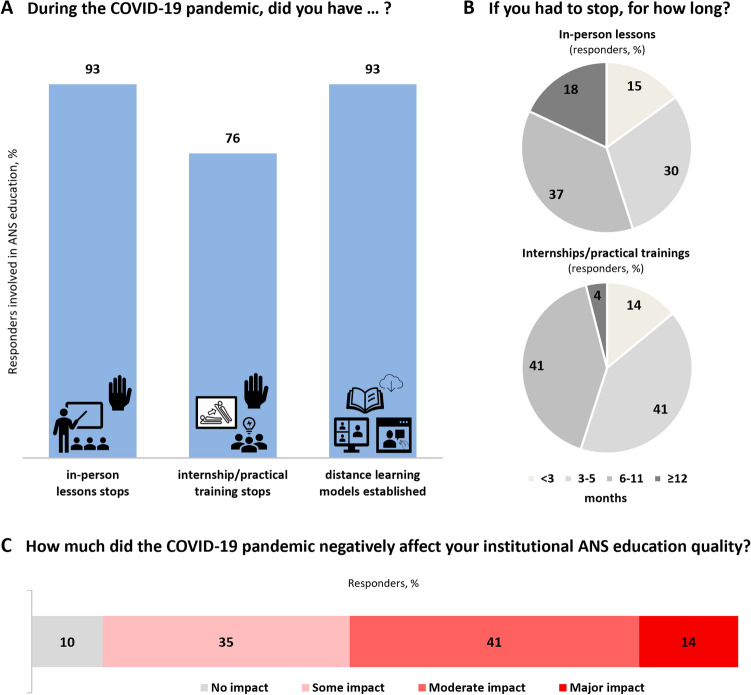
Since the pandemic outbreak, 93% (n = 27/29) of autonomic centers involved in education were forced to stop in-person teaching for a median of 9 (5; 9) months (Fig. 1). Seventy-six percent (n = 22/29) of centers involved in autonomic education also interrupted internship and practical training programs for 5 (5; 9) months (Fig. 1). In response to the COVID-19 pandemic-related educational barriers, most centers (93%, n = 27/29) switched to e-learning formats (Fig. 2). Notwithstanding, 90% of survey respondents involved in clinical autonomic education agreed that the COVID-19 pandemic had a negative effect on the overall quality of their institutional educational offer; 55% (n = 16/29) judged such effect as moderate to severe (Fig. 1C).
Fig. 1.
Type (A) and length (B) of changes in clinical autonomic educational activities from the beginning of the COVID-19 pandemic in the institutions of the European clinical autonomic centers. C The estimated impact of the COVID-19 pandemic on the overall quality of clinical autonomic education in the opinion of the survey respondents. Centers with in-person lesson stops for more than 6 months had a significantly lower number of TTT (74 ± 81 versus 231 ± 223, p = 0.037) and autonomic inpatient admissions during the first pandemic year (15 ± 28 versus 45 ± 38, p = 0.036), as well as longer autonomic function laboratory [5 (4; 9) versus 2 (2; 3) months, p = 0.013] and outpatient clinic [5 (5; 9) versus 2 (2; 2) months, p = 0.004] closures. Centers reporting internship training stops for longer than 6 months had a significantly higher cumulative number of staff members (11 ± 4 versus 7 ± 4, p = 0.038) and bigger reduction in the number of TTT during the first pandemic year (−57 ± 29% versus −30 ± 25%, p = 0.027). Participants who reported a moderate to severe negative effect of the COVID-19 pandemic on clinical autonomic education were more frequently from Southern/Eastern European than Northern/Western European countries (89% versus 40%, p = 0.020), had greater reductions in the number of autonomic outpatient visits during the first pandemic year (−49 ± 25% versus −23 ± 28%) and longer autonomic function laboratory closures [5 (2; 9) versus 2 (2; 3) months, p = 0.049]
Fig. 2.
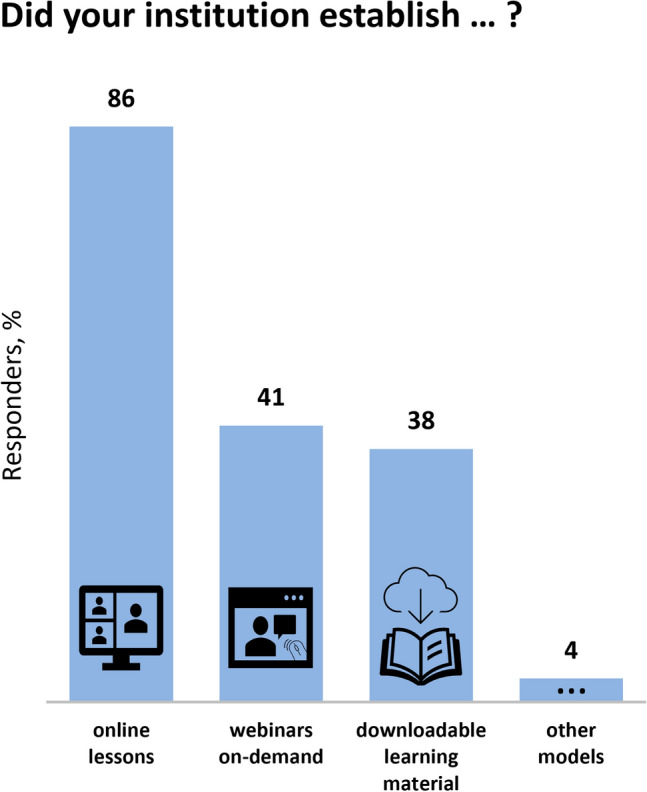
Types of distance learning models established in the institutions of the European clinical autonomic centers involved in autonomic education since the COVID-19 pandemic begin.
Other models of distance learning included interactive case presentations
Lessons learned from the COVID-19 pandemic for an improved clinical autonomic education
Six respondents made suggestions regarding possible strategies to raise the quality of clinical autonomic education in the future. They recommended the integration of online courses and on-demand webinars in medical school curricula and the enrichment of neurology residency programs with rotations in autonomic units, autonomic case-series classes, and in-person or remote autonomic video clinic attendance.
COVID-19 pre-pandemic-to-pandemic proportion of junior participants in the annual EAN and EFAS congresses
Following the world-wide lockdown in March 2020, the EAN rapidly converted the planned annual congress into a fully virtual event with free registration for all attendees. This was an EAN–EFAS joint congress and marked a substantial increase in the number of registered junior participants (Fig. 3) from European, North American, South American, and Asian countries [33]. In 2021, the EAN and EFAS annual congresses were organized in a virtual format, with reduced registration fees for EAN neurology trainees and waved fees for EFAS trainees and EAN/EFAS undergraduate students. Both congresses ultimately achieved higher percentages of registered junior participants than in pre-pandemic years (Fig. 3). Such rising trend was confirmed in 2022, when both the EAN and EFAS opted for a hybrid congress format (Fig. 3).
Fig. 3.
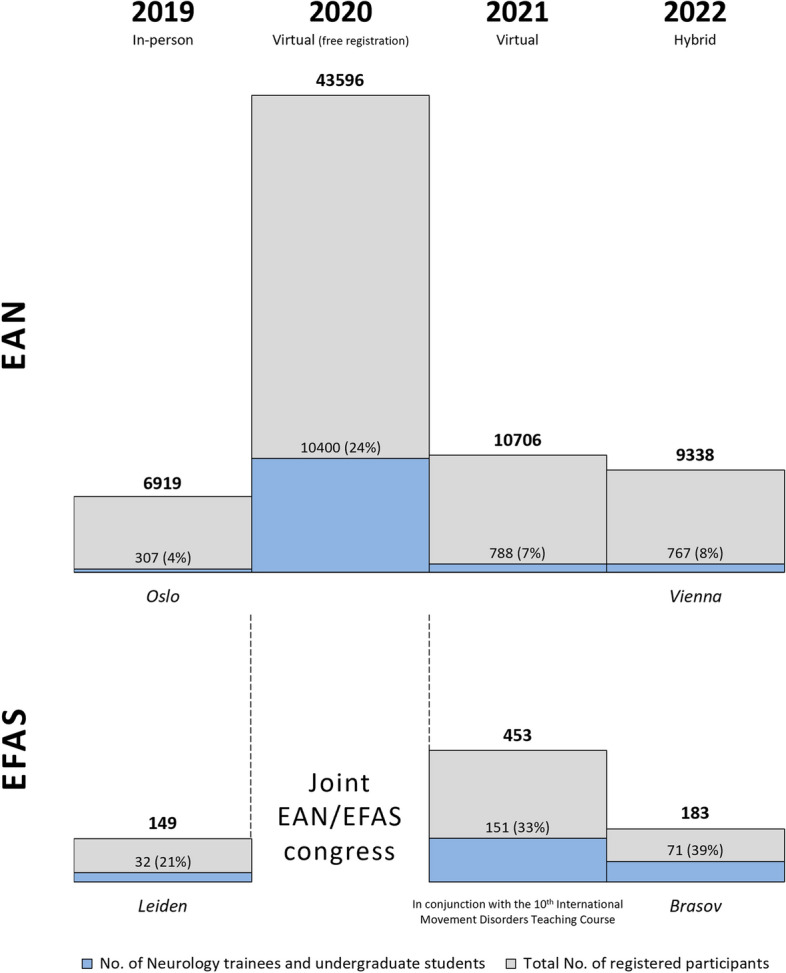
COVID-19 pre-pandemic-to-pandemic number of neurology trainees and undergraduate students participating in the annual congresses of the European Academy of Neurology (EAN) and European Federation of Autonomic Societies (EFAS). The EAN congress program entailed two sessions on autonomic nervous system topics in 2019, five in 2020, three in 2021, and two in 2022
Impact of the COVID-19 pandemic on clinical autonomic research in Europe
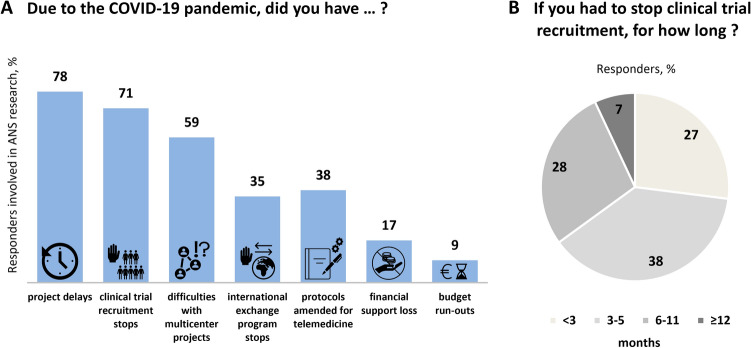
Since the pandemic onset, 78% of European autonomic centers involved in research activities experienced project delays, with clinical trial recruitment stops for 5 (2; 9) months (Fig. 4A, B), difficulties in managing multicenter projects (59% of respondents, n = 23/39), and international scientific exchange programs (35%, n = 14/40). As a result, 17% (n = 7/41) of researchers faced financial losses and 9% (n = 3/33) budgetary runouts. Thirty-eight percent (n = 15/40) of autonomic researchers were able to amend their study protocols, embedding telemedicine-based visits and study outcome measures (Fig. 4).
Fig. 4.
Impact of the COVID-19 pandemic on clinical autonomic research in Europe (A), including cumulative trial recruitment stop duration (B). Centers reporting trial recruitment stops for more than 6 months had a significantly lower number of autonomic outpatient visits during the first pandemic year [48 (25; 123) versus 125 (85; 274), p = 0.045] compared with those whose trial recruitment stops lasted 6 months or less. Survey respondents, who amended their study protocols for telemedicine had a significantly higher number of TTT both in pre-pandemic years [250 (50; 400) versus 100 (47; 195), p = 0.015] and during the first pandemic year (194 ± 219 versus 63 ± 72, p = 0.039), as well as higher numbers of autonomic inpatient admissions during the first pandemic year [28 (9; 96) versus 5 (0; 24), p = 0.022] compared with those who did not implement telemedicine in their research protocols
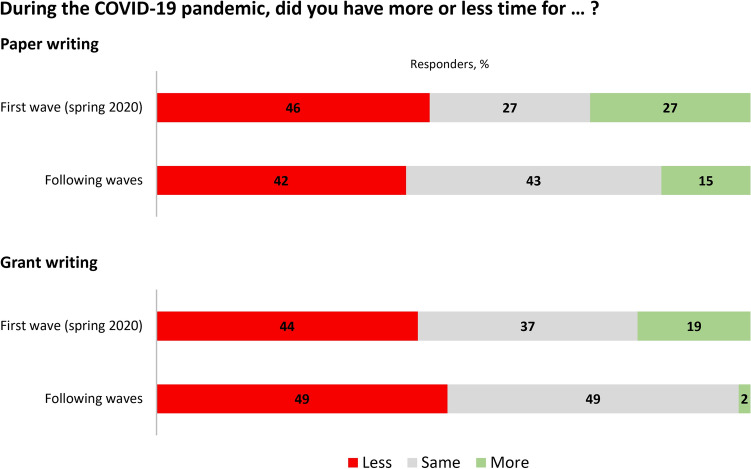
When specifically asked about the availability of time to write scientific papers during the first COVID-19 pandemic wave, 46% (n = 19/41) of autonomic researchers had less time, while 27% (n = 11/41) had more time than before the pandemic (Fig. 5). During the following waves, the percentage of respondents who had less time than usual for paper writing remained similar (42%, n = 17/41), but the percentage of those who reported to have more time for publishing than usual dropped to 15% (n = 6/41, Fig. 5). Such time constraints were reportedly even more impactful on the preparation of research grant proposals (Fig. 5).
Fig. 5.
Impact of the COVID-19 pandemic on time availability for paper and grant writing in the experience of the survey respondents involved in clinical autonomic research. We found no association between any respondent or autonomic center characteristic and the COVID-19 pre-pandemic-to-pandemic change in time availability for paper writing. Likewise, we observed no difference in the respondents or center characteristics between respondents reporting increased or diminished time available for grant writing during the first pandemic wave, but respondents reporting less time for grant writing during the following waves belonged to centers with longer autonomic function laboratory closures (6 ± 4 versus 4 ± 3 months, p = 0.036)
Lessons learnt from the COVID-19 pandemic for improved clinical autonomic research practice
Eleven respondents shared their opinion on novelty elements and needs raised by the COVID-19 pandemic in autonomic research settings; eight considered the introduction of online meetings a cost- and time-effective strategy for lowering the networking barriers among autonomic centers. Two respondents stressed the importance of securing adequate amounts of research time, financial, and infrastructural support for clinical autonomic research. Three respondents finally highlighted how the COVID-19 pandemic facilitated telemedicine implementation in research protocols, overall adding flexibility to clinical trial design.
Pre-pandemic-to-pandemic number of PubMed publications on autonomic versus other neurological disorders
Before the pandemic, the number of PubMed publications on autonomic disorders was the lowest among several other major neurological subspecialties (n = 4675, Fig. 6A) but showed comparable annual percentage increases [+1% versus +3% (3%; 5%), Fig. 6B].
Fig. 6.
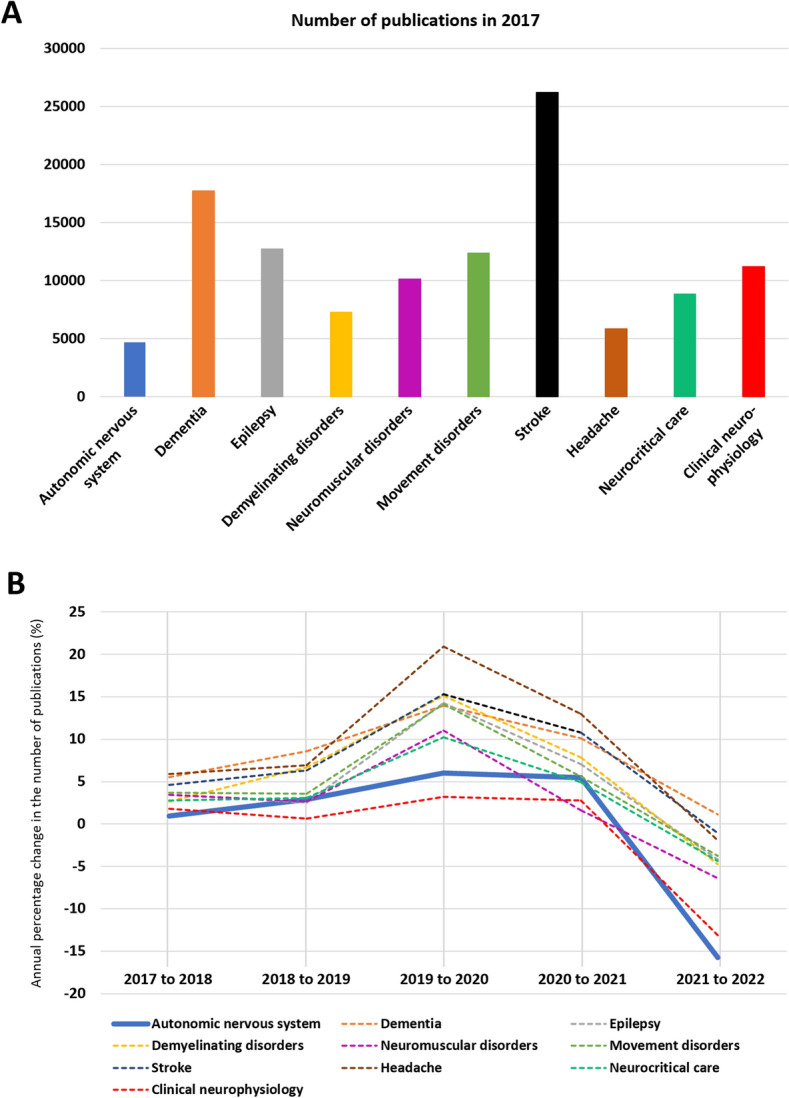
Cumulative number of publications in a pre-COVID-19 pandemic year (2017) on autonomic nervous system versus other frequent neurological disorders and neurology subspecialties (A). B The COVID-19 pre-pandemic-to-pandemic annual percentage change in the number of publications on autonomic topics (blue line) compared with other main neurological disorders and subspecialties (dotted lines)
In 2020, the annual number of publications increased substantially in all neurology subspecialties [+14% (11%; 15%)]. In the autonomic field, however, the annual percentage increase was substantially lower (+6%) compared with other fields, such as headache (+21%), multiple sclerosis (+15%), or stroke (+15%, Fig. 6B). In 2021, the annual percentage increase in the number of publications attenuated in all neurology subspecialties [+7% (4%; 10%)], including autonomic nervous system disorders (+5%). Except for the dementia field, in 2022, the number of publications diminished by 4% (−2%; −6%) in all neurology fields compared with 2021. This reduction was most prominent for autonomic (−16%) and clinical neurophysiology (−13%) research topics.
Discussion
This survey highlighted a previously underestimated, substantial impact of the COVID-19 pandemic on clinical autonomic education in Europe.
We found that centers involved in clinical autonomic education maintained higher clinical caseloads than non-involved centers during the first pandemic year. Educational centers were possibly national referral centers enabled to continue working and/or receive referrals from other peripheral centers, which were closed during the lockdown. Among the centers involved in clinical autonomic education, those with longer teaching interruptions were also those with major pandemic-related reductions in the autonomic outpatient and inpatient metrics. This may indicate increased difficulties in controlling the pandemic spread at a local level, or alternatively reflect stricter lockdown policies in some European countries [7, 17, 37].
Respondents from Southern/Eastern European countries pinpointed a more severe pandemic-related autonomic educational gap than those from Northern/Western European countries. Such a gap likely affected trainees of two to three subsequent academic years, who may have been also exposed to increased risks of anxiety, depression, and burnout [11] and now need to close their knowledge gaps with individual efforts. To this end, the survey respondents indicated e-learning educational formats as a useful tool to break down the geographical barriers to clinical autonomic education. Digital educational formats may, in fact, promote more equitable access to education in neurology and its subspecialties, as highlighted by the increasing number of trainees, especially those from lower-income countries participating in the EAN and EFAS annual congresses since the introduction of less expensive virtual formats. At the same time, in-person participation of younger colleagues in international congresses should be actively encouraged with dedicated travel grants, reduced registrations fees, and invitations to give oral presentations to promote their engagement in professional networks [21, 34].
The survey respondents also highlighted multiple interferences of the COVID-19 pandemic with European autonomic research. Early during the pandemic, lawmakers may have deemed the risk–benefit ratio of research activities unfavorable in the short term. The long-term effects of missed or delayed research progress on healthcare quality are, however, yet to be quantified, especially considering that autonomic disturbances may frequently develop or worsen within the so-called post-COVID-19 condition [12, 25, 30]. To this end, it is concerning that most survey respondents reported diminished time available for scientific writing since the pandemic onset, which further decreased during the following pandemic waves. The fact that many regular duties had to be carried on with additional COVID-19 safety constraints possibly raised the overall individual workload to a critical level. This is mirrored by the number of PubMed publications on autonomic nervous system disorders, which showed the least annual percentage increase with respect to other neurological subspecialties during the first two pandemic years and the most pronounced reduction in 2022. Similar negative trends were observed in other subspecialties relying on elective diagnostic workups, such as clinical neurophysiology.
In analogy to the autonomic educational outcomes, we found that centers interrupting their trial recruitment for longer times also had lower clinical performances during the first pandemic year. These centers might have been hit “harder” in terms of local pandemic spread, or staff members might have suffered severe COVID-19 forms or developed post-COVID-19 disturbances, diminishing their working capability for some time. On the other hand, some institutions might have been better able to implement pandemic-mitigating strategies, as shown by the fact that centers implementing telemedicine in their research activities also performed more autonomic assessments and visits during the first pandemic year.
The pandemic-related healthcare digitalization, thus, promoted resilience not only in clinical autonomic practice [12, 31], but also in research, reshaping clinical trial design in several ways. Several observational studies—and even parts of interventional studies—are now often run in a decentralized way, with comparable recruitment rates and degrees of patient satisfaction [23]. For this purpose, video-based versions of conventional motor rating scales have been developed [14], eventually highlighting a high intra-individual variability in motor performance in home settings, which would have otherwise remained undetected with traditional hospital-based assessments [10, 14]. Telemonitoring tools are being increasingly integrated in clinical studies [1], further shifting the focus towards rater-independent outcome measures [27, 28]. Many organizational study meetings are now also run in a virtual format, reducing organizational costs. This is particularly important in the setting of rare autonomic disorders, where lower operational costs may encourage industry investments.
Research digitalization may also provide other types of benefits to the scientific community. Faster information exchange through online meetings fosters multicenter cooperation. Lowered need for business traveling has the potential of promoting individual productivity, work–life balance, and gender parity, facilitating child and other familial care duties. The decreased number of both business flights and patients’ travels to study centers may ultimately reduce the ecological footprint of research activities.
The present study has some limitations. First, the results are based on the information provided by the survey respondents, while consulting source data was beyond the scope of the present work. The survey respondents were, however, directors of autonomic centers with experienced insights into the European clinical autonomic landscape. The additional objective outcome measures considered in the present study, such as the pre-pandemic-to pandemic number of junior participants attending international congresses and the number of scientific publications on autonomic versus other neurology subspecialty topics, were also aligned with the respondents’ views. Second, our study might have underestimated the impact of the pandemic on clinical autonomic education and research in regions without available autonomic centers or in those identified centers that did not complete the survey despite the reminders sent. In order to reduce inequity in clinical autonomic education and research across Europe, both EFAS and the EAN should work on further promoting the inclusion of currently underserved countries and colleagues in their professional network and future initiatives. Third, the keywords used for the PubMed search on the pre-pandemic-to-pandemic number of publications across neurology subspecialties might have missed publications including autonomic outcome measures among the secondary objectives or studies investigating autonomic disturbances in common neurological conditions, such as movement disorders, stroke, or epilepsy, may have been counted multiple times in the PubMed search. To overcome this potential methodological bias, we based our comparative analysis on the annual percentage change in the number of publications per neurology subspecialty. Fourth, we were unable to quantify the monetary impact of the COVID-19 pandemic on academic research funding. Studies in other medical specialties reported pandemic-related financial losses of 13 to 25% [3, 20], and this might have been the case in autonomic settings as well.
In conclusion, while exerting a negative effect on the quality of clinical autonomic education in Europe, the COVID-19 pandemic promoted its digitalization and therefore fruition outside of autonomic referral centers. Likewise, the pandemic had a negative impact on clinical autonomic research and the scientific output of autonomic researchers. Nevertheless, it facilitated telemedicine implementation in clinical autonomic research, lowered the organizational barriers for networking among autonomic centers, and promoted digital literacy even among elderly individuals [24]. Altogether, digital communication tools provide novel educational and scientific opportunities, which the autonomic community should build upon beyond the COVID-19 pandemic horizon while taking into account legal and security aspects, as well as the needs of vulnerable patients with lower education and/or [23] cognitive disability [8].
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank Ms. Lucia Pavlakova, Ms. Abigail Magno (EAN Scientific Department), Mr. Martin Dunzinger (EAN IT-Coordinator) and Mr. Peter Hofmann (EAN Registration Department) for their excellent administrative support and the following collaborators of the European Network of Neurological Autonomic Laboratories for their thoughtful completion of the survey: Ivan Adamec—Department of Neurology, University Hospital Centre Zagreb, Zagreb, Croatia; Arnaud Aerts—Department of Cardiology, Zuyderland Medical Centre, Heerlen, Netherlands; Leo LR Canta—Department of Neurology, Catharina Ziekenhuis, Eindhoven, Netherlands; Robert Shane Delamont—Department of Neurology and Clinical Neurophysiology, King’s College Hospital, London, UK; Frederik de Lange—Syncope Unit, Amsterdam University Medical Center, Amsterdam, Netherlands; Francesca Del Sorbo—Parkinson and Movement Disorders Unit, ASST Gaetano Pini-CTO, Milano, Italy; Grazia Devigili—Parkinson and Movement Disorder Unit, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, Italy; Rita Di Leo—Department of Neurology, Ospedale San Giovanni e Paolo, Venezia, Italy; Trang Dinh—Department of Cardiology, Maastricht University Medical Center, Maastricht, Netherlands; Jacques-Olivier Fortrat—Explorations Fonctionnelles Vasculaires, Centre Hospitalier Universitaire, Angers, France; Janne Gierthmühlen—Department of Neurology, University Hospital of Schleswig-Holstein, Campus Kiel, Kiel, Germany; Martin Hemels—Department of Cardiology, Rijnstate Hospital and Radboud University Medical Center, Arnhem—Nijmegen, Netherlands; Julia Köhn—Department of Neurology, University of Erlangen-Nuremberg, Erlangen, Germany; Thomas Krøigård—Department of Neurology, Odense University Hospital, Odense, Denmark; Axel Lipp—Department of Neurology, Park-Klinik Weißensee, Berlin, Germany; Andrea Maier—Department of Neurology, Outpatient Service for ANS Disorders, University Clinic RWTH Aachen, Aachen, Germany; Lucio Marinelli—Department of Neuroscience, IRCCS Ospedale Policlinico San Martino, Genova, Italy; Anna Mazzeo—Department of Clinical and Experimental Medicine, Neurology and Neuromuscular Disease Unit, Messina, Italy; Ivan Milenkovic—Department of Neurology, Medical University of Vienna, Vienna, Austria; Maciej Motyl—Department of Neurology, Jagiellonian University Medical College, Krakow, Poland; Maria Grazia Natali Sora—Department of Neurology, Ospedale San Raffaele, Milano, Italy; Judith Navarro-Otano—Department of Neurology, Hospital Clinic, Barcelona, Spain; Kristian Bernhard Nilsen—Department of Neurology, Oslo University Hospital, Oslo University Hospital, Norway; Mario Oliveira—Department of Cardiology, Santa Marta Hospital, Lisbon, Portugal; Petter Moe Omland—Department of Neurology, Section of Clinical Neurophysiology, St. Olaversus University Hospital, Trondheim, Norway; Giuseppe Pelliccioni—Department of Neurology, Istituto Nazionale di Ricovero e Cura per Anziani IRCCS Ancona, Ancona, Italy; Yann Pereon—Reference Centre from Neuromuscular Disorders, Department of Neurology, University Hospital, Nantes, France; Roland Josef Resch—Department of Neurology, Kepler University, Linz, Austria; Camilla Rocchi—Department of Neurology, Policlinico Tor Vergata, University of Rome "Tor Vergata", Rome, Italy; Frederic Roche—Department of Clinical Physiology, CHU And INSERM U 1059 Sainbiose, Saint Étienne, France; Joost Rutten—Department of Internal Medicine, Radboud University Medical Center, Nijmegen, Netherlands; Beatriz Tijero-Merino—Movement Disorders and Autonomic Disorders Unit, Cruces Hospital, Barakaldo, Spain; Marcin Tutaj—Department of Neurology, Jagiellonian University Medical College, Krakow, Poland; A. M. H. G. van der Heijden-Montfroy—Department of Neurology, VieCuri, Venlo, Netherlands; Bas JA van Hoeve—Department of Neurology, ZorgSaam Hospital, Terneuzen, Netherlands; Narender van Orshoven—Department of Neurology, Zuyderland Medical Centre, Heerlen, Netherlands; Ruihao Wang—Department of Neurology, University of Erlangen-Nuremberg, Erlangen, Germany; Werner J Z'Graggen—Department of Neurology, University Hospital Bern, Bern, Switzerland.
Author contributions
Study conception: A.F., J.C., P.C., C.F.P., P.G., R.H., M.J.H., V.I., J.J., A.P.L.T., I.R., J.S., J.M.S., A.T., G.K.W., E.M., T.B., R.T., W.S., M.H. Study design: A.F., D.R.C., R.H., A.P.L.T., J.S., T.B., R.T., W.S., M.H. Study coordination: A.F., M.H. Data collection: A.F., F.L., N.C., G.C.B., G.C., C.F.P., R.G., P.G., V.I., E.C.A.K., A.K., A.P.L.T., A.T., G.K.W., R.T., W.S., M.H. Data analysis: A.F., M.K.S., F.L., N.C., M.H. Writing of the first draft: A.F. Writing—review and editing: M.K.S., F.L., D.R.C., N.C., G.C.B., J.C., G.C., P.C., C.F.P., R.G., P.G., R.H., M.J.H., V.I., J.J., E.C.A.K., A.K., A.P.L.T., I.R., J.S., J.M.S., A.T., G.K.W., E.M., T.B., R.T., W.S., M.H.
Funding
Open access funding provided by University of Innsbruck and Medical University of Innsbruck. Academic study without dedicated external financial support. We received administrative support from the EAN Head Office. Dr. Fanciulli, Dr. Leys, and Dr. Campese received travel grants from the Austrian Exchange Program. Dr. Campese is supported by the US MSA Coalition. Dr. Leys is supported by the US MSA Coalition and the Johannes und Hertha Tuba Stiftung. Financial disclosures for the last 12 months: Alessandra Fanciulli: Dr. Fanciulli reports royalties from Springer Verlag, speaker fees and honoraria from Theravance Biopharma, GE Health Care, Austrian Autonomic Society, Stopp-HSP, Elsevier, and research grants from the FWF-Austrian Science Fund, Medical University of Innsbruck, US MSA Coalition, and Dr Johannes and Hertha Tuba Foundation, outside of the present work. Magdalena Krbot Skorić: Dr Krbot Skoric reports consultation and/or speaker fees from Sanofi Genzyme and Roche, outside of the present work. Fabian Leys: Dr. Leys has nothing to disclose. Diogo Reis Carneiro: Dr. Reis-Carneiro reports speaker fees from Abbvie and Zambon, outside of the present work. Nicole Campese: Dr. Campese has nothing to disclose. Giovanna Calandra-Buonaura: Dr. Calandra-Buonaura reports speaker fees from Zambon and Bial, outside of the present work. Jennifer Camaradou: Ms. Camaradou reports speaker fees from MEDABLE Inc, Reuters Pharma events, Patients as Partners Europe and consultancy fees from Roche Global, GlaxosmithKline GSK, the FutureScience Group and Springer Healthcare (scientific publishing) outside of the scope of current work. Ms. Camaradou is a current assigned lay member of the UK NICE Covid Expert panel, a former Citizen partner at COVID END Evidence synthesis network, and former speaker at Cochrane Convenes. Ms. Camaradou is part of the strategic advisory board for EU project DIGITPREDICT (GA no. 101017915) Edge AI deployed Digital Twins for predicting disease progression and need for early intervention in infectious and cardiovascular disease beyond Covid-19 and part of the community advisory for EU project RBDCOV which is developing an adjuvanted recombinant protein vaccine*, based on a receptor binding domain* (RBD) fusion heterodimer against SARS-CoV-2. Giacomo Chiaro: Dr. Chiaro has nothing to disclose. Pietro Cortelli: Dr. Pietro Cortelli has nothing to disclose. Cristian Falup-Pecurariu: Dr. Falup-Pecurariu reports editor fees from Springer and Elsevier; speaker fees from Abbvie and from the International Parkinson and Movement Disorder Society (MDS), outside of the present work. Roberta Granata: Dr. Granata has nothing to disclose. Pietro Guaraldi: Dr. Guaraldi has been advisory board member of Alnylam and Sobi; received speaker fees and honoraria from Alnylam, Akcea Therapeutics, Chiesi, and Theravance Biopharma. Received congress and travel accommodation expense compensations from Abbvie, AB Pharm, Alnylam, Bial, and Zambon, outside of the present work. Raimund Helbok: Dr. Helbok reports honoraria from companies and societies outside of the present work and research grants from the Austrian Science Fund (FWF) related to COVID-19. Max J. Hilz: Dr. Hilz reports consultancy and speaker fees from Sanofi Genzyme and from Amicus Therapeutics, consultancy fees from Pfizer, and editor honoraria from Elsevier BV, outside of the present work. Valeria Iodice: Dr. Iodice reports speaker fees and honoraria from Theravance Biopharma and Janssen, outside of the present work. Jens Jordan: Dr. Jordan served a consultant for Menarini and Novo-Nordisk, received research support from Novo-Nordisk and Boehringer-Ingelheim, and is Co-Founder of Eternygen GmbH, outside of the present work. Evert C. A. Kaal: Dr. Kaal has nothing to disclose. Anita Kamondi: Dr. Kamondi reports speaker fee from Eisai, outside of the present work. Anne Pavy Le Traon: Dr. Pavy Le Traon reports speaker fees from Alnylan and honoraria from Biohaven, outside of the present work. Isabel Rocha: Dr. Rocha has nothing to disclose. Johann Sellner: Dr. Sellner reports honoraria for lectures, the assembly of teaching material or participation in advisory boards from Alexion, Angelini, BMS, Biogen, Boehringer, Horizon, Janssen, Kedrion, Merck, Novartis, Immunic, Sandoz, and Sanofi, outside of the present work. Jean Michel Senard: Dr. Senard has nothing to disclose. Astrid Terkelsen: Dr. Terkelsen reports consultation and/or speaker fees from Alnylam Pharmaceuticals, Akcea Therapeutics, Pfizer, and Allergan, outside of the present work. Gregor K. Wenning: Dr. Wenning reports consultancy and lecture fees from Inhibicase, Ono, and Theravance and research grants from the FWF-Austrian Science Fund, US MSA Coalition, Parkinson Fonds Austria, Dr. Johannes und Hertha Tuba Foundation, outside of the present work. Thomas Berger: Dr. Berger has participated in meetings sponsored by and received honoraria (lectures, advisory boards, consultations) from pharmaceutical companies marketing treatments for MS: Allergan, Bayer, Biogen, Bionorica, BMS/Celgene, GSK, GWD/Jazz Pharma, Horizon, Janssen-Cilag, MedDay, Merck, Novartis, Octapharma, Roche, Sandoz, Sanofi-Genzyme, and Teva. His institution has received financial support in the past 12 months by unrestricted research grants (Biogen, Bayer, BMS/Celgene, Merck, Novartis, Sanofi Aventis, Teva) and for participation in clinical trials in multiple sclerosis and related disorders sponsored by Alexion, Bayer, Biogen, BMS/Celgene, Merck, Novartis, Octapharma, Roche, Sanofi-Genzyme, Teva, outside of the present work. Elena Moro: Dr. Moro reports honoraria from Medtronic and research grant from Abbott, Ipsen, and France Parkinson, outside the present work. Roland Thijs: Dr. Thijs received research support from Medtronic, the Human Measurement Models Programme co-funded by Health ~ Holland, Top Sector Life Sciences & Health and ZonMw (Brain@Home—agreement 114025101), Michael J Fox Foundation, Epilepsie NL and received speaker or consultancy fees from Theravance Biopharma, Arvelle, Medtronic, Zogenix, Xenon, Angelini, UCB, NewLife Wearables, and Novartis, outside of the present work. Walter Struhal: Dr. Struhal reports royalties from Manz-Rechtsverlag, Springer, Oxford University Press, honorarium from Elsevier, speaker fees from Medconvent, Donau-Universität Krems, Austrian Neurology Society and Manz-Rechtsverlag, outside of the present work. Mario Habek: Dr. Habek participated as a clinical investigator and/or received consultation and/or speaker fees from Biogen, Sanofi Genzyme, Merck, Bayer, Novartis, Pliva/Teva, Roche, Alvogen, Actelion, Alexion Pharmaceuticals, and TG Pharmaceuticals, outside of the present work.
Declarations
Conflict of interest
The authors declare no competing interests. Full financial disclosures of the authors are reported above.
Ethical standards
Survey studies among healthcare professionals do not require an institutional review board approval per Austrian law. All participants gave electronic informed consent before answering the survey and for being listed among the collaborators of the European Network of Neurological Autonomic Laboratories in the resulting publications. The study adhered to the rules of good scientific practice of the Austrian Agency for Research Integrity and to the European General Data Protection Regulation.
Footnotes
The Collaborators of European Network of Neurological Autonomic Laboratories mentioned in “Acknowledgements” section.
Contributor Information
Alessandra Fanciulli, Email: alessandra.fanciulli@i-med.ac.at.
the Collaborators of European Network of Neurological Autonomic Laboratories:
Ivan Adamec, Arnaud Aerts, Leo L. R. Canta, Robert Shane Delamont, Frederik de Lange, Francesca Del Sorbo, Grazia Devigili, Rita Di Leo, Trang Dinh, Jacques-Olivier Fortrat, Janne Gierthmühlen, Martin Hemels, Julia Köhn, Thomas Krøigård, Axel Lipp, Andrea Maier, Lucio Marinelli, Anna Mazzeo, Ivan Milenkovic, Maciej Motyl, Maria Grazia Natali Sora, Judith Navarro-Otano, Kristian Bernhard Nilsen, Mario Oliveira, Petter Moe Omland, Giuseppe Pelliccioni, Yann Pereon, Roland Josef Resch, Camilla Rocchi, Frederic Roche, Joost Rutten, Beatriz Tijero-Merino, Marcin Tutaj, A. M. H. G. van der Heijden-Montfroy, Bas J. A. van Hoeve, Narender van Orshoven, Ruihao Wang, and Werner J. Z’Graggen
References
- 1.Artusi CA, Imbalzano G, Sturchio A, Pilotto A, Montanaro E, Padovani A, Lopiano L, Maetzler W, Espay AJ. Implementation of mobile health technologies in clinical trials of movement disorders: underutilized potential. Neurotherapeutics. 2020;17:1736–1746. doi: 10.1007/s13311-020-00901-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Audisio K, Lia H, Robinson NB, Rahouma M, Soletti G, Jr, Cancelli G, Perezgrovas Olaria R, Chadow D, Tam DY, Vervoort D, Farkouh ME, Bhatt DL, Fremes SE, Gaudino M. Impact of the COVID-19 pandemic on non-COVID-19 clinical trials. J Cardiovasc Dev Dis. 2022;9:19. doi: 10.3390/jcdd9010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blaise D, Berger P, Mokart D, Camerlo J, Fougereau E, Giovannini M, Houvenaeghel G, Turrini O, Chabannon C, Piana G, Brenot-Rossi I, Tallet A, Goncalves A, Charbonnier A, Vey N, Grossi S, Viens P. The management of a comprehensive cancer center during the first six months of the COVID-19 pandemic in the south of France: lessons from the Paoli-Calmettes Institute's Experience. Clin Hematol Int. 2021;3:119–129. doi: 10.2991/chi.k.210919.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bodini B, Moro E, Jaarsma J, Cunningham E, Sellner J, Walsh D, Force EAC-T. Lessons learned from people with neurological diseases at the time of COVID-19: The EFNA-EAN survey. Eur J Neurol. 2022;29:318–323. doi: 10.1111/ene.15087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bratan T, Aichinger H, Brkic N, Rueter J, Apfelbacher C, Boyer L, Loss J. Impact of the COVID-19 pandemic on ongoing health research: an ad hoc survey among investigators in Germany. BMJ Open. 2021;11:e049086. doi: 10.1136/bmjopen-2021-049086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Callaway Kim K, Tadrous M, Kane-Gill SL, Barbash IJ, Rothenberger SD, Suda KJ. Changes in purchases for intensive care medicines during the COVID-19 pandemic: a global time series study. Chest. 2021;160:2123–2134. doi: 10.1016/j.chest.2021.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng T, Chen T, Liu Y, Aldridge RW, Nguyen V, Hayward AC, Michie S. Human mobility variations in response to restriction policies during the COVID-19 pandemic: an analysis from the Virus Watch community cohort in England, UK. Front Public Health. 2022;10:999521. doi: 10.3389/fpubh.2022.999521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cubo E, Arnaiz-Rodriguez A, Arnaiz-Gonzalez A, Diez-Pastor JF, Spindler M, Cardozo A, Garcia-Bustillo A, Mari Z, Bloem BR. Videoconferencing software options for telemedicine: a review for movement disorder neurologists. Front Neurol. 2021;12:745917. doi: 10.3389/fneur.2021.745917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cuffaro L, Carvalho V, Di Liberto G, Klinglehoefer L, Sauerbier A, Garcia-Azorin D, Tabuas-Pereira M, Vashchenko N, Moro E, Bassetti CLA. Neurology training and research in the COVID-19 pandemic: a survey of the Resident and Research Fellow Section of the European Academy of Neurology. Eur J Neurol. 2021;28:3437–3442. doi: 10.1111/ene.14696. [DOI] [PubMed] [Google Scholar]
- 10.Davies EH, Matthews C, Merlet A, Zimmermann M. Time to see the difference: video capture for patient-centered clinical trials. Patient. 2022;15:389. doi: 10.1007/s40271-021-00569-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dedeilia A, Papapanou M, Papadopoulos AN, Karela NR, Androutsou A, Mitsopoulou D, Nikolakea M, Konstantinidis C, Papageorgakopoulou M, Sideris M, Johnson EO, Fitzpatrick S, Cometto G, Campbell J, Sotiropoulos MG. Health worker education during the COVID-19 pandemic: global disruption, responses and lessons for the future-a systematic review and meta-analysis. Hum Resour Health. 2023;21:13. doi: 10.1186/s12960-023-00799-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fanciulli A, Leys F, Krbot Skoric M, Carneiro DR, Calandra-Buonaura G, Camaradou J, Chiaro G, Cortelli P, Falup-Pecurariu C, Granata R, Guaraldi P, Helbok R, Hilz MJ, Iodice V, Jordan J, Kaal ECA, Kamondi A, Pavy Le Traon A, Rocha I, Sellner J, Senard JM, Terkelsen A, Wenning GK, Moro E, Berger T, Thijs RD, Struhal W, Habek M, Collaborators of European Network of Neurological ANSl Impact of the COVID-19 pandemic on clinical autonomic practice in Europe A survey of the European Academy of Neurology (EAN) and the European Federation of Autonomic Societies (EFAS) Eur J Neurol. 2023;30:1712. doi: 10.1111/ene.15787. [DOI] [PubMed] [Google Scholar]
- 13.Frontera JA, Tamborska AA, Doheim MF, Garcia-Azorin D, Gezegen H, Guekht A, Yusof Khan AHK, Santacatterina M, Sejvar J, Thakur KT, Westenberg E, Winkler AS, Beghi E, contributors from the Global C-NRC Neurological events reported after COVID-19 vaccines: an analysis of VAERS. Ann Neurol. 2022;91:756–771. doi: 10.1002/ana.26339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grobe-Einsler M, Taheri Amin A, Faber J, Schaprian T, Jacobi H, Schmitz-Hubsch T, Diallo A, Tezenas du Montcel S, Klockgether T. Development of SARA(home), a new video-based tool for the assessment of ataxia at home. Mov Disord. 2021;36:1242–1246. doi: 10.1002/mds.28478. [DOI] [PubMed] [Google Scholar]
- 15.Guadix SW, Winston GM, Chae JK, Haghdel A, Chen J, Younus I, Radwanski R, Greenfield JP, Pannullo SC. Medical student concerns relating to neurosurgery education during COVID-19. World Neurosurg. 2020;139:e836–e847. doi: 10.1016/j.wneu.2020.05.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Habek M, Leys F, Krbot Skoric M, Reis Carneiro D, Calandra-Buonaura G, Camaradou J, Chiaro G, Cortelli P, Falup-Pecurariu C, Granata R, Guaraldi P, Helbok R, Hilz MJ, Iodice V, Jordan J, Kaal ECA, Kamondi A, Pavy Le Traon A, Rocha I, Sellner J, Senard JM, Terkelsen A, Wenning GK, Berger T, Thijs RD, Struhal W, Fanciulli A, Collaborators of the European Network of Clinical ANSl Clinical autonomic nervous system laboratories in Europe: A joint survey of the European Academy of Neurology and the European Federation of Autonomic Societies: a joint survey of the European Academy of Neurology and the European Federation of Autonomic Societies. Eur J Neurol. 2022;29:3633–3646. doi: 10.1111/ene.15538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hale T, Angrist N, Goldszmidt R, Kira B, Petherick A, Phillips T, Webster S, Cameron-Blake E, Hallas L, Majumdar S, Tatlow H. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker) Nat Hum Behav. 2021;5:529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- 18.N Fountoulakis K, N Karakatsoulis G, Abraham S, Adorjan K, Ahmed HU, Alarcón RD, Arai K, Auwal SS, Bobes J, Bobes-Bascaran T, Bourgin-Duchesnay J, Bredicean CA, Bukelskis L, Burkadze A, Cabrera Abud II, Castilla-Puentes R, Cetkovich M, Colon-Rivera H, Corral R, Cortez-Vergara C, Crepin P, de Berardis D, Zamora Delgado S, de Lucena D, de Sousa A, di Stefano R, Dodd S, Elek LP, Elissa A, Erdelyi-Hamza B, Erzin G, Etchevers MJ, Falkai P, Farcas A, Fedotov I, Filatova V, Fountoulakis NK, Frankova I, Franza F, Frias P, Galako T, Garay CJ, Garcia-Álvarez L, García-Portilla P, Gonda X, Gondek TM, Morera González D, Gould H, Grandinetti P, Grau A, Groudeva V, Hagin M, Harada T, Hasan TM, Azreen Hashim N, Hilbig J, Hossain S, Iakimova R, Ibrahim M, Iftene F, Ignatenko Y, Irarrazaval M, Ismail Z, Ismayilova J, Jacobs A, Jakovljević M, Jakšić N, Javed A, Yilmaz Kafali H, Karia S, Kazakova O, Khalifa D, Khaustova O, Koh S, Kopishinskaia S, Kosenko K, Koupidis SA, Kovacs I, Kulig B, Lalljee A, Liewig J, Majid A, Malashonkova E, Malik K, Iqbal Malik N, Mammadzada G, Mandalia B, Marazziti D, Marčinko D, Martinez S, Matiekus E, Mejia G, Memon RS, Meza Martínez XE, Mickevičiūtė D, Milev R, Mohammed M, Molina-López A, Morozov P, Muhammad NS, Mustač F, Naor MS, Nassieb A, Navickas A, Okasha T, Pandova M, Panfil AL, Panteleeva L, Papava I, Patsali ME, Pavlichenko A, Pejuskovic B, Pinto da Costa M, Popkov M, Popovic D, Raduan NJN, Vargas Ramírez F, Rancans E, Razali S, Rebok F, Rewekant A, Reyes Flores EN, Rivera-Encinas MT, Saiz PA, Sánchez de Carmona M, Saucedo Martínez D, Saw JA, Saygili G, Schneidereit P, Shah B, Shirasaka T, Silagadze K, Sitanggang S, Skugarevsky O, Spikina A, Mahalingappa SS, Stoyanova M, Szczegielniak A, Tamasan SC, Tavormina G, Tavormina MGM, Theodorakis PN, Tohen M, Tsapakis EM, Tukhvatullina D, Ullah I, Vaidya R, Vega-Dienstmaier JM, Vrublevska J, Vukovic O, Vysotska O, Widiasih N, Yashikhina A, Prezerakos PE, Berk M, Levaj S, Smirnova D. (2023) Results of the COVID-19 mental health international for the health professionals (COMET-HP) study: depression, suicidal tendencies and conspiracism. Soc Psychiatry Psychiatr Epidemiol. 9:1387-1410. [DOI] [PMC free article] [PubMed]
- 19.Lau B, Tadrous M, Chu C, Hardcastle L, Beall RF. COVID-19 and the prevalence of drug shortages in Canada: a cross-sectional time-series analysis from April 2017 to April 2022. CMAJ. 2022;194:E801–E806. doi: 10.1503/cmaj.212070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liebensteiner MC, Khosravi I, Hirschmann MT, Heuberer PR, Board of the AGASoA. Joint S, Saffarini M, Thaler M. It is not 'business as usual' for orthopaedic surgeons in May 2020—the Austrian-German-Swiss experience. J Exp Orthop. 2020;7:61. doi: 10.1186/s40634-020-00272-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Macerollo A, Rona-Voros K, Holler N, Chiperi R, Gyorfi O, Papp V, Sauerbier A, Balicza P, Sellner J. Preferences of residents and junior neurologists to attend conferences—an EAYNT survey. J Neurol Sci. 2015;357:297–299. doi: 10.1016/j.jns.2015.06.060. [DOI] [PubMed] [Google Scholar]
- 22.Majid U, Hussain SAS, Zahid A, Haider MH, Arora R. Mental health outcomes in health care providers during the COVID-19 pandemic: an umbrella review. Health Promot Int. 2023;38:2. doi: 10.1093/heapro/daad025. [DOI] [PubMed] [Google Scholar]
- 23.Myers TL, Augustine EF, Baloga E, Daeschler M, Cannon P, Rowbotham H, Chanoff E, Me Research T. Jensen-Roberts S, Soto J, Holloway RG, Marras C, Tanner CM, Dorsey ER, Schneider RB. Recruitment for remote decentralized studies in Parkinson's disease. J Parkinson's Dis. 2022;12:371–380. doi: 10.3233/JPD-212935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Naude B, Rigaud AS, Pino M. Video calls for older adults: a narrative review of experiments involving older adults in elderly care institutions. Front Public Health. 2021;9:751150. doi: 10.3389/fpubh.2021.751150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.NICE (2021) COVID-19 rapid guideline: managing the long-term effects of COVID-19. In: Excellence NIfHaC (ed). NICE, United Kingdom
- 26.Perego G, Cugnata F, Brombin C, Milano F, Mazzetti M, Taranto P, Preti E, Di Pierro R, De Panfilis C, Madeddu F, Di Mattei VE (2023) Analysis of healthcare workers' mental health during the COVID-19 pandemic: evidence from a three-wave longitudinal study. J Health Psychol:13591053231168040 [DOI] [PMC free article] [PubMed]
- 27.Raccagni C, Goebel G, Gassner H, Granata R, Ndayisaba JP, Seebacher B, Schoenherr G, Mitterhuber J, Hendriks P, Kaindlstorfer C, Eschlboeck S, Fanciulli A, Krismer F, Seppi K, Poewe W, Bloem BR, Klucken J, Wenning GK. Physiotherapy improves motor function in patients with the Parkinson variant of multiple system atrophy: A prospective trial. Parkinson Relat Disord. 2019;67:60–65. doi: 10.1016/j.parkreldis.2019.09.026. [DOI] [PubMed] [Google Scholar]
- 28.Raccagni C, Sidoroff V, Goebel G, Granata R, Leys F, Klucken J, Eskofier B, Richer R, Seppi K, Wenning GK, Fanciulli A. The footprint of orthostatic hypotension in Parkinsonian syndromes. Parkinson Relat Disord. 2020;77:107–109. doi: 10.1016/j.parkreldis.2020.06.029. [DOI] [PubMed] [Google Scholar]
- 29.Ranney ML, Griffeth V, Jha AK. Critical supply shortages—the need for ventilators and personal protective equipment during the covid-19 pandemic. N Engl J Med. 2020;382:e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 30.Reis-Carneiro DRI, Habek M, Helbok R, Sellner J, Struhal W, Wenning GK, Fanciulli A. Clinical presentation and management strategies of cardiovascular autonomic dysfunction following a COVID-19 infection—a systematic review. Eur J Neurol. 2023;30:1528. doi: 10.1111/ene.15714. [DOI] [PubMed] [Google Scholar]
- 31.Russo V, Boggian G, Bolognesi MG, Carretta DM, Cencetti S, De Laura D, Hrovatin E, Pastori P, Tomaselli C, Parente E, Rafanelli M, Ungar A, On Behalf Of Covid-Gimsi Study G The impact of COVID-19 outbreak on syncope units activities in Italy: a report from the Italian Multidisciplinary Working Group on Syncope (GIMSI) Int J Environ Res Public Health. 2021;18:9194. doi: 10.3390/ijerph18179194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sandrone S, Albert DV, Dunham SR, Kraker J, Noviawaty I, Palm M, Kushlaf H. Training in neurology: how lessons learned on teaching, well-being and telemedicine during the COVID-19 pandemic can shape the future of neurology education. Neurology. 2021;96:e3007–3010. doi: 10.1212/WNL.0000000000012010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stamelou M, Struhal W, Ten Cate O, Matczak M, Caliskan SA, Soffietti R, Marson A, Zis P, di Lorenzo F, Sander A, Deuschl G, de Visser M, Bassetti CLA. Evaluation of the 2020 European Academy of Neurology virtual congress: transition from a face-to-face to a virtual meeting. Eur J Neurol. 2021;28:2523–2532. doi: 10.1111/ene.14702. [DOI] [PubMed] [Google Scholar]
- 34.Struhal W, Sellner J, Eaynt European teaching course on autonomic nervous system disorders : reaching out to young physicians. Clin Auton Res. 2009;19:130. doi: 10.1007/s10286-009-0523-2. [DOI] [PubMed] [Google Scholar]
- 35.Suda KJ, Kim KC, Hernandez I, Gellad WF, Rothenberger S, Campbell A, Malliart L. Tadrous M (2022) The global impact of COVID-19 on drug purchases: a cross-sectional time series analysis. J Am Pharm Assoc. 2003;62(766–774):e766. doi: 10.1016/j.japh.2021.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.WHO (2023) WHO coronavirus (COVID-19) Dashboard. Available at: https://covid19.who.int/
- 37.Wong KLM, Gimma A, Coletti P, CoMix Europe Working G, Faes C, Beutels P, Hens N, Jaeger VK, Karch A, Johnson H, Edmunds W, Jarvis CI. Social contact patterns during the COVID-19 pandemic in 21 European countries—evidence from a two-year study. BMC Infect Dis. 2023;23:268. doi: 10.1186/s12879-023-08214-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The first and the last authors take full responsibility for the integrity of data and agree to share any de-identified data not published herewith upon reasonable request from any qualified investigator.