Abstract
Objective.
Prevalence rates of cannabis use and PTSD vary, with men reporting greater cannabis use than females, females reporting higher rates of PTSD than males, and race and ethnic minority persons reporting higher rates of both cannabis and PTSD compared to non-Hispanic White individuals. This study extends our understanding of directional associations between cannabis use and PTSD from early to late young adulthood (18 – 26 years old) using two theoretical models: symptom-driven pathway and substance-induced pathway.
Methods.
Participants provided yearly data for 14 years, and the present study utilized data from waves 9 through 14. Those endorsing Criterion A in at least one wave of data collection (n = 1,454) were included in the analytic sample. We used auto regressive latent trajectory with structured residuals [ALT-SR] to understand reciprocal associations for the full sample, as well as by sex and race or ethnicity.
Results.
For the full sample, we noted support for both symptom-driven and substance-induced pathways during early young adulthood (18–20), but only support for a symptom-driven pathway during late young adulthood (21–26). Males showed the same pattern as the full sample; however, for females, only a symptom driven-pathway during late young adulthood was found. For race and ethnic minority participants, we showed full cross-lagged effects during both early and late young adulthood and no associations for non-Hispanic White individuals.
Conclusions.
Results indicate both men and individuals from minoritized racial and ethnic groups are more likely to report heightened PTSD symptomology, maladaptive coping, and worsening symptoms.
Keywords: childhood trauma, stress, pain, violence, substance use treatment, discrimination
Introduction
Besides alcohol, cannabis is the most commonly used substance among young adults ages 18 to 25, with about 34.5% (11.6 million) young adults reporting past year use and 24.1% reporting past month use (SAMHSA, 2022). Males (26.1%) report greater cannabis use than females (22.2%), and some research indicates racial and ethnic minority differences as well. For example, young adults identifying as more than two races (34.0%), as well as Black or African American (26.6%), report greater past month use than non-Hispanic White (25.5%), Hispanic or Latino (20.4%), and Asian (14.5%) individuals (SAMHSA, 2022). However, when looking at past year use (e.g., used at least once in the past year) use was higher among Multiracial people (41.6%) than among White (37.9%), Black (37.0%), Hispanic (30.7%), or Asian people (21.6%). In addition to being characterized by increased cannabis use, young adulthood is a developmental period in which many individuals report exposure to traumatic events. Recent data from the World Mental Health Survey indicate that 70% of nearly 69,000 respondents across 24 countries experienced at least one traumatic event in their life, such as physical violence, accidents, or war-related traumas (Kessler et al., 2017). Posttraumatic stress disorder (PTSD) is a mental health disorder that can result from experiencing one or multiple traumatic events, and although the majority of individuals who experience some type of trauma do not develop PTSD (Atwoli, Stein, Koenen, & McLaughlin, 2015), young adults in the U.S. have an estimated 11% prevalence rate (Kessler et al., 2017; National Comorbidity Survey (NCS), 2007). It is not uncommon for individuals who have experienced past traumatic events to use substances, such as cannabis, to ameliorate symptoms of PTSD (Khantzian, 2003). In fact, PTSD symptoms often co-occur with substance use and substance use disorders, with a recent meta-analysis reporting high rates of cannabis use disorder among individuals with PTSD and vice versa (Hicks, Zaur, Keeley, & Amstadter, 2022).
Variation in prevalence of PTSD: Theory and empirical support
Before we can explore potential reciprocal associations between PTSD symptoms and cannabis use, we must first understand theoretical models of PTSD and how these models may or may not equate across sex and racial and ethnic minority populations. Rates of PTSD are not equal among all people. For example, recent epidemiological studies indicate that females have a higher prevalence rate of PTSD than males (5.2% vs 1.8%). Among adult racial and ethnic minority persons, those identifying as Black or African American (8.7%), have a slightly higher prevalence of PTSD than non-Hispanic White adults (7.4%), Hispanic (7.0%), and Asian (4.0%) individuals (Roberts, Gilman, Breslau, Breslau, & Koenen, 2011). Unlike other psychiatric conditions such as generalized anxiety disorder or major depressive disorder, PTSD requires that one has experienced a prior traumatic event. This is referred to as Criterion A, which specifies the type of event that constitutes a trauma and encompasses experiences such as childhood trauma, exposure to war, sexual assault, kidnapping, natural disasters, or motor accidents (American Psychiatric Association., 2013).
Numerous studies have explored sex and racial and ethnic minority differences for diagnosis of PTSD and two possible explanations have emerged in the literature. The first explanation relates to potential differences in trauma exposure. This explanation posits that females (compared to males) and racial and ethnic minority (compared to non-Hispanic White) individuals may be more likely to experience potentially traumatic events, thus the higher risk of developing PTSD is an artifact of higher risk of traumatization (Roberts et al., 2011; Tolin & Foa, 2008). A second hypothesis posits that females and racial and ethnic minority individuals have a higher likelihood of experiencing more severe or pathogenic events compared to males and non-Hispanic White participants. Evidence supporting these hypotheses is mixed across studies. Some early studies assessing sex differences have noted that females experience greater rates of traumatic events compared to males (Cuffe et al., 1998), whereas others have noted no differences or that males experience higher rates (Chilcoat & Breslau, 1998; Kessler et al., 1995). In a review of the literature on sex differences in PTSD, Tolin and Foa (2008) reported that differences in PTSD rates do exist; however, the nature of these differences is dependent on type of trauma, with females more likely to experience sexual assault and child sexual abuse and males more likely to experience accidents, witness death, or experience war/combat. A similar story emerges in research focused on racial and ethnic minority differences, with early research and reviews noting mixed results for higher rates of trauma exposure based on the type of trauma experienced (Hatch, Bruce, & Dohrenwend, 2007; Kilpatrick & Acierno, 2003). However, a recent study using a large nationally representative sample reported that differences in trauma exposure for racial and ethnic groups varied by event type: White individuals were more likely to report indirect trauma (i.e., witness or hear about trauma), whereas Black and Hispanic individuals reported higher risk of childhood trauma and witnessing parental violence (Roberts et al., 2011). Similarly, recent research utilizing a population-based sample notes that vulnerability to PTSD varies across groups, with Asian individuals being less likely and Black/African American individuals being more likely to develop PTSD following traumatic event exposure than non-Hispanic White individuals (Mclaughlin et al., 2019).
Conceptually, there are two models that can help explain sex and racial and ethnic differences seen in PTSD and aid in understanding why we might expect differences in the association between PTSD and cannabis use across sex and race and ethnicity. According to the socialization theory of PTSD, males and females display different cognitive, emotional, and behavioral responses to traumatic events (Cromer & Smyth, 2009; Tolin & Gender, 2022). Socialization theory posits that variation in cognitive appraisal of traumatic events may be due to biological differences between males and females, as well as the socio-cultural norms that may lead to alterations in response to trauma (Tolin & Gender, 2022). For example, some research has noted that exposure to more severe types of trauma and having a higher risk for other psychiatric problems, such as depression and anxiety, place females at greater odds of developing PTSD than males (Ahern et al., 2015; Hapke, Schumann, Rumpf, John, & Meyer, 2006; Zeidner, 2006). However, some studies have noted no sex differences in PTSD after controlling for trait anxiety, mood problems, and trauma exposure (Breslau, Davis, Andreski, Peterson, & Schultz, 1997; Fullerton et al., 2001; Spindler, Elklit, & Christiansen, 2010). Socialization theory also posits that males and females cope with traumatic events differently. For example, some have noted that females tend to rely on emotion-focused coping styles whereas males tend to rely on disengagement-focused coping styles (Cromer & Smyth, 2009; Gil, Caspi, Ben-Ari, Koren, & Klein, 2005; Tolin & Gender, 2022), both of which have been shown to increase PTSD symptoms and lead to greater probability of using substances (e.g., alcohol or cannabis) to cope with symptoms of PTSD (Littleton, Horsley, John, & Nelson, 2007).
The second model is based on minority stress theory and proposes that individuals in a minority position in society experience unique stigmatizing stressors that may, eventually, lead to greater risk of negative health outcomes (Frost & Meyer, 2023). Although originally conceptualized to explain health outcomes among sexual and gender minority populations, Pascoe and Richman (2009) noted that minority stress theory can also be applied to racial and ethnic minority individuals. In particular, racial and ethnic minority individuals may deal with both acute and chronic stressors, which can include Criterion A traumatic events. It is also important to note that racial and ethnic minority individuals experience both current discrimination-based stressors as well as historical, reoccurring, stressors that may exacerbate psychiatric symptoms (e.g., PTSD) and reliance on substances (e.g., cannabis) to alleviate symptoms and related stressors (Coleman, 2016; Kirmayer, Gone, & Moses, 2014).
PTSD and cannabis use: Developmental and theory driven support
Socialization theory and minority stress theory can aid in our understanding of heterogeneity in PTSD across subpopulations. However, these theories do not address important, developmental, temporal associations between PTSD symptomology and cannabis use. There are two major theories that we focus on in this paper that can address the issue of directionality. The first is a symptom-driven pathway in which PTSD symptomology precedes greater cannabis use (this is sometimes referred to as the self-medication hypothesis). Thus, as one believes that cannabis use can be a method for coping with symptoms of PTSD (e.g., disengagement coping), heavy use can be established, which can potentially lead to negative consequences (Khantzian, 1985). The second is a substance-induced pathway, which posits that greater use of cannabis can potentially increase risk of PTSD symptom escalation (Brady, Back, & Coffey, 2004; Brady, Killeen, Brewerton, & Lucerini, 2000).
Recently, Hicks and colleagues (2022) completed a review of the literature to shed some light on associations between PTSD and cannabis use. Forty-five studies were included in their review, 37 of which focused on assessing a symptom-driven pathway and eight assessing a substance-induced pathway. In general, there was strong support for both symptom-driven and substance-induced pathway across reviewed studies. However, among the 45 studies included in this review only eight were longitudinal, and of these, only two addressed temporally lagged effects of PTSD symptoms and cannabis use. Among the two studies assessing temporality, both used a method known as ecological momentary assessment (Shiffman, Stone, & Hufford, 2008) whereby participants provide data multiple times per day over multiple days. The first study included a small sample of trauma exposed pregnant females (n = 33), with results noting peak daily PTSD symptoms predicting greater cannabis use the next day, thus supporting a symptom-driven pathway (Sanjuan, Pearson, Poremba, Amaro, & Leeman, 2019). The second study was a small sample of sexual and gender minority females (n = 114), with results noting higher daily PTSD symptoms were associated with greater cannabis use on any given day, again supporting a symptom-driven pathway (Dworkin, Kaysen, Bedard-Gilligan, Rhew, & Lee, 2017). These studies provide important information; however, they have several shortcomings. First, both studies had small samples and did not have a comparator group, thus limiting ability to generalize results and understand if associations between PTSD symptoms and cannabis use vary by important demographic variables. Second, these studies were not able to examine how associations unfold over the course of development as they use snapshots of time and do not model data over the course of an entire developmental period. Therefore, these studies provide information on lagged associations on a short time scale (e.g., moments or days) but cannot provide information on these reciprocal associations across longer developmental periods.
The present study
The present study extends our current understanding of directional associations between cannabis use and PTSD from early to late young adulthood (18 – 26 years old) by examining these associations over six years. In an attempt to provide greater specificity on these associations, we initially estimated a model with the full sample of respondents who endorsed a past-year traumatic experience (e.g., Criterion A) to examine whether PTSD was associated with greater cannabis use throughout young adulthood (symptom-driven pathway) or whether cannabis use was associated with greater PTSD symptoms throughout young adulthood (substance-induced pathway). Next, we tested two shared vulnerability models by examining whether sex (males vs. females) and race and ethnicity (non-Hispanic White individuals vs. racial or ethnic minority individuals) accounted for differential associations between PTSD and cannabis during young adulthood (ages 18- to 26). In the present study we use advanced methods that allow for testing bidirectional associations over time, and developmental variation, to assess directionality and explore differences across key subgroups. However, due to lack of consensus in the field, we had no a priori hypotheses with respect to whether or how directionality or group differences (e.g., sex, race and ethnicity) would emerge, thus all aims in the present study are exploratory. Of note, due to low sample sizes, model non-convergence, or unacceptable fit criteria, we were unable to estimate models by all specific race and ethnic minority subgroups, and instead were limited to a comparison between non-Hispanic White individuals and those in all other racial and ethnic groups. However, we do provide estimates for those with Hispanic identity in the supplemental materials as this was the only subgroup to provide acceptable model fit.
Methods
Participants and Procedures
Participants were initially recruited in 2008 from 16 middle schools in Southern California for an evaluation of a voluntary school-based substance use prevention program, CHOICE (D’Amico et al., 2012). We obtained consent/assent and procedures were approved by the institution’s internal review board. Schools were selected to obtain a diverse sample, have similar substance use rates at baseline, and were matched to their nearest neighbor school based on a squared Euclidean distance measure (D’Amico et al., 2012). We recruited from 16 middle schools; 92% of parents returned a consent form; 71% of parents gave permission for their child to participate, and 94% of consented students completed the first survey. Two cohorts of 6th and 7th graders were followed annually across 14 waves through 2022. Participants who did not complete a particular wave of data collection remained eligible to complete subsequent waves. Wave-to-wave retention rates averaged 85% across all 14 waves, and 90% from age 18 forward (waves 8–14), and were not significantly associated with demographics (e.g., age, sex, race and ethnicity) until wave 11. Based on multivariate logistic regression analyses, retention was slightly higher among those who were younger versus older (23.6 vs 23.8 years at wave 13, respectively). Retention from wave 13 to wave 14 was not predicted by wave 13 past-month days of alcohol or cigarette use, similar to all previous waves; however, past-month days of cannabis use was slightly lower for individuals who completed wave 14 compared to those who did not (3.8 vs. 5.6 days at wave 13, respectively). Of the full sample, 90.4% was retained from waves 13 to 14 (n = 2,174; n = 230 not retained) and year-to-year retention rates were excellent for both those who did and did not report cannabis use in wave 13 (87.5% vs. 91.7%, respectively).
For the present study, all prospective analyses used data from wave 9, when participants were between the ages of 18 and 21 (M = 19.4, SD = 0.73), through wave 14, when participants were between 23 and 26 (M = 24.7, SD =0.8). Data analysis began from wave 9 onward because this is when participants were first asked about PTSD symptoms. To be included in the present study, a participant had to endorse Criterion A (experiencing a traumatic event in the past year) in at least one wave of data collection [wave 9: n = 730; wave 10: n = 723; wave 11: n = 700; wave 12: n = 735; wave 13: n = 724; wave 14: n = 638]. Because data were set up in naturally occurring cohorts (e.g., age), an accelerated longitudinal cohort design was used, which creates a planned missing data pattern such that participants only contribute data at the time points in which they are in the study. However, because our metric of time is age (versus follow-up wave), we are able to model development from 18 to 26 years old. Due to missingness on some variables and our inclusion criteria of Criterion A, our final analytic sample size was 1,454.
Measures
Covariates.
All analyses controlled for sex (female = 1; male = 0), race and ethnicity (coded: racial and ethnic minority individuals = 1, non-Hispanic White individuals = 0), parental education which ranged from did not finish high school to college degree. Parental education was recoded as (1 = high school or less education; 0 = college degree or greater), and CHOICE intervention status (coded: 1 = received intervention in middle school in 2008). Further, covariates included past year frequency of binge drinking (4 or more drinks for females and 5 or more drinks for males) and past year frequency of cannabis use at wave 8.
Cannabis use.
Using items similar to those in large-scale national surveys (Johnston, Miech, O’Malley, Bachman, Schulenberg, & Patrick, 2019; SAMHSA, 2018) participants were asked the number of days they had used cannabis in the past year (Ellickson, McCaffrey, Ghosh-Dastidar, & Longshore, 2003). We re-coded the values from 1–6 to values of 0–20 (1=None, 2=1 day, 3=2, 4=6.5, 5=15.5, 6= 20) to represent actual number of days of use so each response corresponds to the number of days participants used cannabis in the past year.
PTSD Symptoms.
PTSD symptoms were assessed over the past year with the 5-item Primary Care PTSD screen for DSM-5 (Prins et al., 2004). Prior to endorsing yes/no to five items representing clusters of PTSD symptoms (i.e., re-experiencing, avoidance, negative cognitions and mood, and arousal), participants were asked if they had ever experienced an event that was “unusually or especially frightening, horrible, or traumatic. For example, a serious accident or fire, physical or sexual assault or abuse, earthquake or flood, war, seeing someone be killed or seriously injured, or having a loved one die through homicide or suicide.” If participants answered “yes” to this item, they then met Criterion A for PTSD, and were asked the five Primary Care PTSD items. Sum scores range from 0 to 5 on the scale.
Analytic Approach
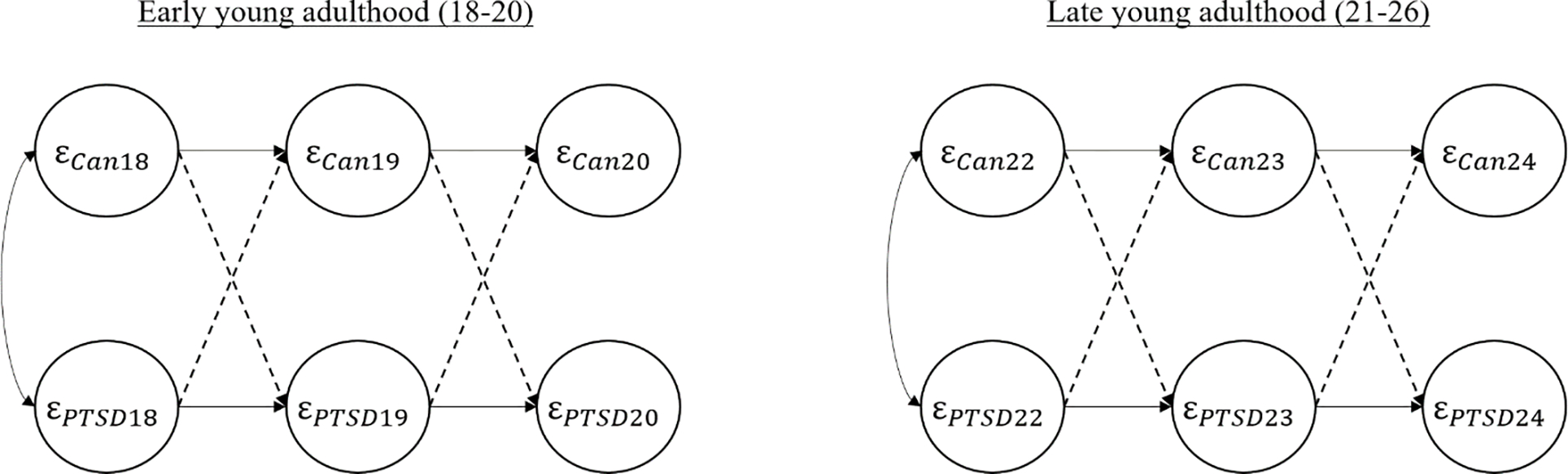
The present study uses advanced modeling techniques, in particular the auto regressive latent trajectory with structured residuals [ALT-SR] (see Figure 1 for conceptual model) to understand how PTSD symptoms and cannabis use are reciprocally associated from 18 to 26 years old (Berry & Willoughby, 2017; Curran, Howard, Bainter, Lane, & McGinley, 2014). Using this model allows us to test associations across three different levels of variance. That is, the ALT-SR separates the variance into three separate ‘bins.’ The first level or bin is the portion of variance that does not change (e.g., the level or intercept), which aids in our understanding of basic differences at age 18. The second bin is the portion of variance that changes over the entire span of the study (e.g., the slope), which aids in our understanding of basic individual differences in changes in cannabis use and symptoms of PTSD. The third bin is the portion of variance that changes wave-to-wave (e.g., the within-person cross lags), which aids in our understanding of within-person fluctuations across the developmental period of young adulthood.
Figure 1.
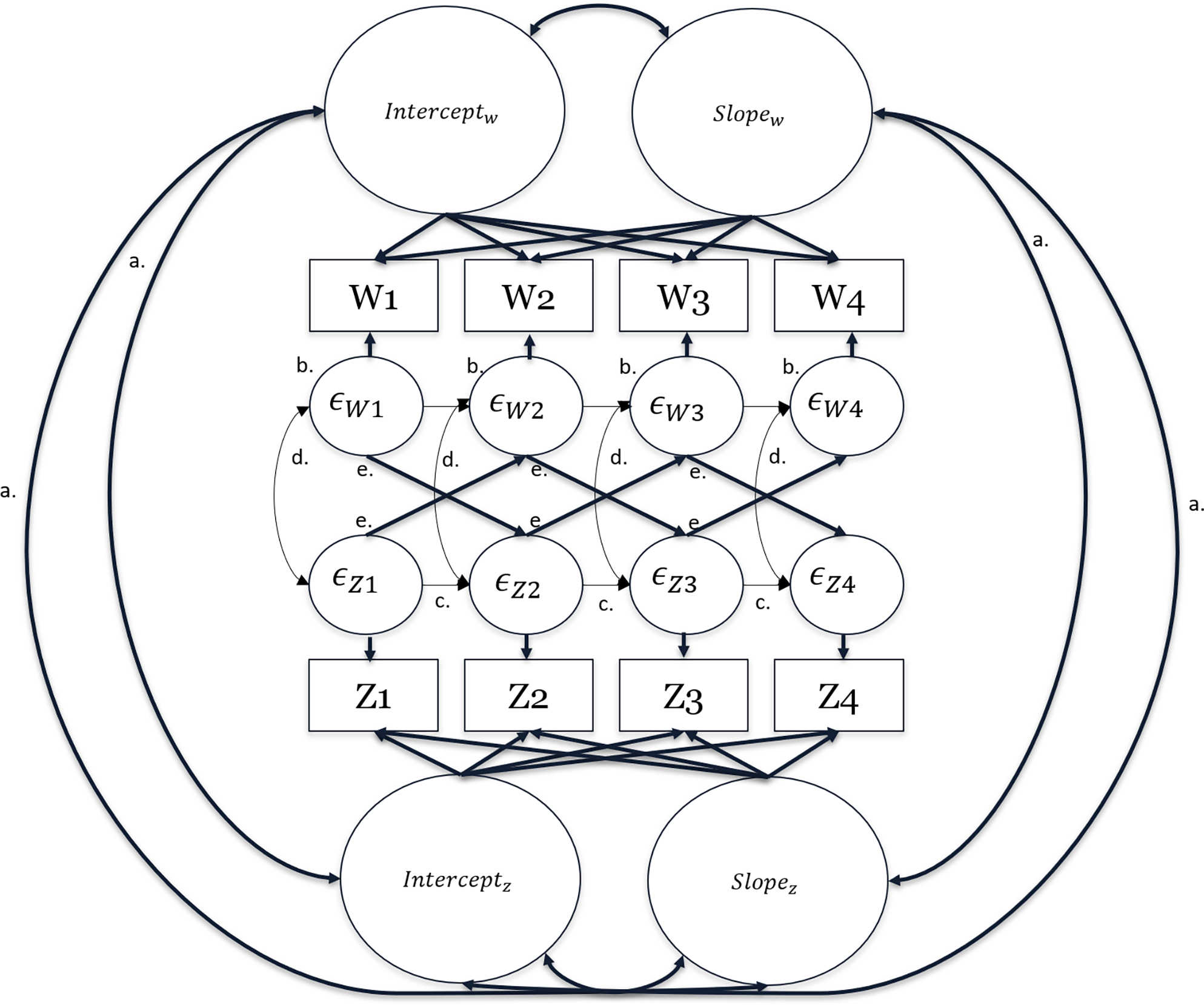
Conceptual ALT-SR model
Note: The model above is only conceptual representing two observed variables (W and Z). The corresponding numbers (e.g. W1, W2; Z1, Z2 etc.) represent measurement of the same construct over time. This model does not represent the complexity of every aspect of ALT-SR models. The correlations between intercepts and slopes (letter ‘a’) represent the between-person effects of each variable in the model. The residuals (e.g., error) of our measured variables are identified as latent residuals (letter ‘b’) with observed means and variances constrained to zero. Here we estimate the residual variance as a newly created latent variable (e.g., or ) and estimate the “residuals of the residuals” to identify newly created within-person latent constructs. These newly created structured residuals (e.g., or ) are then used to estimate the remaining variance that is left over after our intercept and slope correlations are accounted for. We estimate the auto-regressive components of our structured residuals (letter ‘c’), the within-time correlations of our structured residuals (letter ‘d’), and the within-person cross-lagged effects (letter ‘e’).
Using an ALT-SR specification, the between-person effects are captured by correlating our latent intercepts and growth parameters (labeled letter ‘a’ in Figure 1). The remaining variance is “pushed” into the residuals (errors). By creating a latent construct of this remaining error, we can model the within-person cross-lagged portion of the model. Here, the residuals of our observed variables are identified as latent variables (labeled letter ‘b’ in Figure 1) by constraining all observed means and variances to zero (similar to creating a latent growth model). However, diverging from basic latent growth modeling, newly created structured residuals are used (e.g., or ). These newly created structured residuals are used to estimate remaining variance left over after accounting for our correlated change processes (e.g., intercept and slopes) by estimating auto-regressive components (labeled letter ‘c’), within-time correlations (labeled letter ‘d’), and the within-person cross-lagged effects (labeled letter ‘e’).
For the present study we assessed developmental variation in the magnitude of time-specific associations of PTSD symptoms and cannabis use by allowing within-person cross-lagged effects to vary across early young adulthood (ages 18–20) and late young adulthood (ages 21–26). That is, effects from 18–20 years old were constrained to be the same and effects from 21–26 years old were constrained to be the same. We used model constraint tests (negative two log likelihood ratio test) to determine if the constrained model (compared to a freely estimated model) provided fit that was not significantly worse than a freely estimated model. Doing this allows us to use age 21 as a pivot point to understand developmental shifts in effects. We chose this as the pivot point for two reasons: 1) this is a California based sample and cannabis is legal for recreational and medical use, individuals are legally able to purchase cannabis at age 21; and 2) substance use tends to decline around age 22–24, which may influence associations in our model. This model allows us to understand potential developmental variation in the association between PTSD and cannabis use for the whole sample and by sex and race and ethnicity.
We used general fit statistics to determine model fit including Comparative Fit Index (CFI) of 0.95 or greater, Root Mean Square Error of Approximation (RMSEA) of 0.05 or less, and Standardized Root Mean Square Residual (SRMR) of less than 0.08 to indicate good model fit. Data for some analytic variables were missing for 12%–15% of the sample. To address missing data, we used full information maximum likelihood estimator (FIML) in Mplus. Maximum likelihood treats all observed indicators as latent factors and allows each person to contribute whatever data are available instead of removing individuals with missing data. To adjust for non-normality, all standard errors were estimated with robust maximum likelihood. All models controlled for participant self-reported biological sex, race and ethnicity, mother’s education, prior levels of binge drinking and cannabis use, and CHOICE intervention assignment. All analyses were conducted in Mplus version 8.6 (Muthén and Muthén, 1997–2018)
Results
Table 1 provides sample demographics broken out by sex as well as by race and ethnicity. Tables 2 and 3 provide all model results with all parameter estimates (unstandardized) and standard errors. Below, we focus on the within-person lagged portion of the models and report only on the models exploring developmental variation. We have, however, provided a thorough supplement that describes results for the models assessing overall associations, where effects were constrained to be equal over time (e.g., effects were constrained to be the same during the entire developmental period).
Table 1.
Participant demographics and descriptive statistics at wave 9
| Total Sample N = 1,454 |
Men n = 604 |
Females n= 845 |
Racial or ethnic minority n = 1,135 |
Non-Hispanic White n = 319 |
|
|---|---|---|---|---|---|
|
| |||||
| Variable | M(SD) or n(%) | M(SD) or n(%) | M(SD) or n(%) | M(SD) or n(%) | M(SD) or n(%) |
|
| |||||
| Age | 19.4 (0.73) | 19.4 (0.72) | 19.3 (0.74) | 19.3 (0.75) | 19.4 (0.66) |
| Female | 845 (58.1%) | -- | -- | 684 (60.3%) | 161 (50.5%) |
| Race and Ethnicity | |||||
| Non-Hispanic White | 319 (21.9%) | 158 (26.2%) | 161 (19.1%) | -- | -- |
| Non-Hispanic Black | 37 (2.5%) | 12 (2.0%) | 25 (3.0%) | -- | -- |
| Hispanic | 730 (50.2%) | 282 (46.7%) | 443 (52.4%) | -- | -- |
| Asian | 285 (19.6%) | 122 (20.2%) | 163 (19.3%) | -- | -- |
| Multiracial/Other | 83 (5.7%) | 30 (5.0%) | 53 (6.3%) | -- | -- |
| Mother’s Education | |||||
| High school or less | 503 (34.6%) | 188 (31.2%) | 312 (37.0%) | 466 (41.1%) | 37 (11.6%) |
| Days of Cannabis Use | 5.55 (8.01) | 6.42 (8.75) | 4.94 (7.39) | 4.91 (7.63) | 7.83 (8.90) |
| PTSD Symptoms | 2.13 (1.87) | 1.85 (1.88) | 2.30 (1.84) | 2.17 (1.87) | 1.97 (1.88) |
Table 2.
Final model for full sample and by sex assessing associations between PTSD symptoms and cannabis use
| Full sample (n = 1,454) | Males (n = 604) | Females (n = 845) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Effect | Early young adulthood | Late young adulthood | Early young adulthood | Late young adulthood | Early young adulthood | Late young adulthood |
|
| ||||||
| Within-Person Cross-Lags | B [95% CI] | B [95% CI] | B [95% CI] | |||
|
| ||||||
| Can Uset+1 on PTSDt | 0.37 [0.11, 0.63] | 0.19 [−0.11, 0.49] | 0.85 [0.39, 1.29] | 0.56 [−0.02, 1.14] | 0.07 [−0.23, 0.37] | 0.13 [−0.21, 0.46] |
| PTSDt+1 on Can Uset | 0.03 [0.01, 0.05] | 0.04 [0.01, 0.06] | 0.04 [0.01, 0.06] | 0.07 [0.03, 0.10] | 0.01 [−0.03, 0.04] | 0.04 [0.01, 0.07] |
|
| ||||||
| Auto-Regressive | B [95% CI] | B [95% CI] | B [95% CI] | |||
|
| ||||||
| Can Uset+1on Can Uset | 0.37 [0.32, 0.43] | 0.31 [0.23, 0.39] | 0.38 [0.29, 0.46] | 0.26 [0.13, 0.39] | 0.37 [0.30, 0.45] | 0.33 [0.23, 0.43] |
| PTSDt+1on PTSDt | 0.17 [0.07, 0.28] | 0.20 [0.08, 0.33] | 0.27 [0.09, 0.44] | −0.01 [−0.23, .21] | 0.15 [0.01, 0.28] | 0.26 [0.11, 0.40] |
|
| ||||||
| Co-Variances (between-person) | r (se) | r (se) | r (se) | |||
|
| ||||||
| Can Useint with PTSDint | −0.23 (0.18) | −0.43 (0.34) | −0.02 (0.21) | |||
| Can Useint with PTSDslp | 0.33 (0.23) | 0.53 (0.38) | 0.18 (0.33) | |||
| PTSDint with Can Useslp | 0.46 (0.32) | 0.63 (0.56) | 0.32 (0.37) | |||
| Can Useslp with PTSDslp | −0.52 (0.48) | −0.89 (0.78) | −0.36 (0.33) | |||
|
| ||||||
| Mean intercept and slope | B [95% CI] | B [95% CI] | B [95% CI] | |||
|
| ||||||
| Can Useint | 7.54 [6.12, 8.97] | 7.18 [6.22, 8.15] | 5.05 [4.32, 5.77] | |||
| PTSDint | 1.43 [0.95, 1.90] | 1.82 [1.51, 2.13] | 2.39 [2.15, 2.63] | |||
| Can Useslp | 0.13 [−0.16, 0.42] | 0.10 [−0.10, 0.30] | 0.14 [−0.01, 0.28] | |||
| PTSDslp | −0.08 [−0.20, 0.03] | −0.08 [−0.15, −0.003] | −0.10 [−0.16, −0.05] | |||
|
| ||||||
| Variance intercept and slope | B [95% CI] | B [95% CI] | B [95% CI] | |||
|
| ||||||
| Can Useint | 17.39 [10.5, 24.3] | 17.04 [4.16, 29.9] | 17.4 [9.84, 25.0] | |||
| PTSDint | 1.21 [0.59, 1.84] | 1.45 [0.40, 2.51] | 0.99 [0.22, 1.76] | |||
| Can Useslp | 0.26 [−0.04, 0.55] | 0.31 [0.22, 0.84] | 0.24 [−0.09, 0.56] | |||
| PTSDslp | 0.03 [0.002, 0.06] | 0.05 [0.004, 0.10] | 0.02 [−0.02, 0.06] | |||
|
| ||||||
| Residual (Co) Variances | B [95% CI] | B [95% CI] | B [95% CI] | |||
|
| ||||||
| Can UseЄit18–Єeit26 | 27.8 [25.9, 29.8] | 24.6 [22.8, 26.8] | 30.0 [26.5, 33.4] | 27.9 [24.7, 31.2] | 25.6 [23.3, 27.9] | 21.7 [19.7, 23.8] |
| PTSDЄit18–Єit26 | 1.87 [1.65, 2.09] | 1.94 [1.73, 2.15] | 1.56 [1.26, 1.85] | 1.70 [1.35, 2.05] | 2.06 [1.75, 2.36] | 1.99 [1.73, 2.26] |
|
| ||||||
| Fit Statistics | ||||||
|
| ||||||
| AIC | 84703.2 | 33526.9 | 48645.9 | |||
| BIC | 85004.2 | 33751.5 | 48887.6 | |||
| RMSEAd | 0.03 | 0.04 | 0.04 | |||
| SRMRe | 0.09 | 0.16 | 0.13 | |||
| CFIf | 0.95 | 0.94 | 0.94 | |||
Note: Estimates for all control variables on all latent intercept, and linear growth parameters, are not shown for readability. Can Use = Frequency of cannabis use; PTSD = post-traumatic stress disorder. In the table above, subscripts identify time of measurement. For example, a single t indicates paths were constrained to be equal over time. Subscript int indicates latent intercept (mean level) to obtain between-person parameter estimates. Subscripts with an epsilon (Єit) indicate residual variance measured over time.
RMSEA (Root Mean Square Error) indices below .05 are considered to be representative of good model fit
SRMR (Standardized Root Mean Square Residual) indices below .08 are considered to be representative of good model fit
CFI (Comparative Fit Index) scores above .90 are indicative of good model fit.
df = degrees of freedom.
Bold indicates confidence interval does not include 0
Table 3.
Final model for associations between PTSD symptoms and cannabis use by race and ethnic minority status
| Race or ethnic minority (n = 1,135) | Non-Hispanic White (n = 319) | |||
|---|---|---|---|---|
|
| ||||
| Effect | Early young adulthood | Late young adulthood | Early young adulthood | Late young adulthood |
|
| ||||
| Within-Person Cross-Lags | B [95% CI] | B [95% CI] | ||
|
| ||||
| Can Uset+1 on PTSDt | 0.35 [0.05, 0.65] | 0.33 [0.01, 0.66] | 0.40 [−0.20, 0.99] | −0.53 [−1.22, 0.15] |
| PTSDt+1 on Can Uset | 0.03 [0.01, 0.06] | 0.05 [0.02, 0.07] | −0.01 [−0.05, 0.03] | 0.01 [−0.03, 0.06] |
|
| ||||
| Auto-Regressive | B [95% CI] | B [95% CI] | ||
|
| ||||
| Can Uset+1on Can Uset | 0.36 [0.29, 0.43] | 0.33 [0.24, 0.42] | 0.44 [0.31, 0.57] | 0.21 [0.06, 0.36] |
| PTSDt+1on PTSDt | 0.18 [0.06, 0.30] | 0.22 [0.08, 0.36] | 0.16 [−0.09, .41] | 0.11 [−0.13, 0.34] |
|
| ||||
| Co-Variances (between-person) | r (se) | r (se) | ||
|
| ||||
| Can Useint with PTSDint | −0.31 (0.26) | −0.12 (0.23) | ||
| Can Useint with PTSDslp | 0.46 (0.43) | 0.25 (0.25) | ||
| PTSDint with Can Useslp | 0.21 (0.32) | 0.13 (0.28) | ||
| Can Useslp with PTSDslp | −0.07 (0.04) | 0.04 (0.31) | ||
|
| ||||
| Mean intercept and slope | B [95% CI] | B [95% CI] | ||
|
| ||||
| Can Useint | 6.60 [5.08, 8.11] | 11.8 [8.56, 14.9] | ||
| PTSDint | 1.52 [0.98, 2.05] | 0.99 [0.06, 1.92] | ||
| Can Useslp | 0.35 [0.03, 0.66] | −0.60 [−1.20, −0.01] | ||
| PTSDslp | −0.09 [−0.22, 0.45] | −0.05 [−0.27, 0.17] | ||
|
| ||||
| Variance intercept and slope | B [95% CI] | B [95% CI] | ||
|
| ||||
| Can Useint | 12.2 [4.70, 19.7] | 33.9 [13.9, 53.9] | ||
| PTSDint | 1.05 [0.33, 1.78] | 1.79 [0.59, 3.00] | ||
| Can Useslp | 0.06 [−0.27, 0.40] | 0.71 [0.06, 1.37] | ||
| PTSDslp | 0.20 [−0.02, 0.06] | 0.07 [0.01, 0.12] | ||
|
| ||||
| Residual (Co) Variances | B [95% CI] | B [95% CI] | ||
|
| ||||
| Can UseЄit18–Єit26 | 28.6 [26.4, 30.9] | 25.0 [22.9, 27.2] | 25.4 [21.6, 29.2] | 22.3 [18.9, 25.7] |
| PTSDЄit18–Єit26 | 1.92 [1.67, 2.18] | 2.08 [1.81, 2.34] | 1.66 [1.25, 2.06] | 1.47 [1.14, 1.80] |
|
| ||||
| Fit Statistics | ||||
|
| ||||
| AIC | 65822.1 | 18812.3 | ||
| BIC | 66088.9 | 19011.8 | ||
| RMSEAd | 0.03 | 0.05 | ||
| SRMRe | 0.09 | 0.17 | ||
| CFIf | 0.96 | 0.91 | ||
Note: Estimates for all control variables on all latent intercept, and linear growth parameters, are not shown for readability. Can Use = Frequency of cannabis use; PTSD = post-traumatic stress disorder. In the table above, subscripts identify time of measurement. For example, a single t indicates paths were constrained to be equal over time. Subscript int indicates latent intercept (mean level) to obtain between-person parameter estimates. Subscripts with an epsilon (Єit) indicate residual variance measured over time.
RMSEA (Root Mean Square Error) indices below .05 are considered to be representative of good model fit
SRMR (Standardized Root Mean Square Residual) indices below .08 are considered to be representative of good model fit
CFI (Comparative Fit Index) scores above .90 are indicative of good model fit.
df = degrees of freedom.
Bold indicates confidence interval does not include 0
Developmental variation among the full sample
The first model assessed associations between PTSD symptoms and cannabis use among the whole sample and had excellent fit (CFI = 0.95, RMSEA = 0.03, SRMR = 0.09). When comparing the fully free model to one where values were constrained by developmental variation results indicate constraints do not provide a worse fit (Δ −2LL: 16.07; Δ df : 14; p = 0.30). Results indicated full reciprocal associations between PTSD symptoms and cannabis use, supporting both a symptom-driven and substance-induced model during early young adulthood from ages 18–20 (see Figure 2 for visual representation of results). Thus, support for the symptom-driven pathway is indicated because reporting greater PTSD symptoms than one’s typical average was associated with reporting greater cannabis use than one’s typical average the next year (B = 0.37). Support of the substance-induced pathway is indicated because reporting greater cannabis use than one’s typical average was associated with greater PTSD symptoms than one’s own average the next year (B = 0.03). As individuals transitioned into late young adulthood from ages 21–26, results indicate support for a substance-induced model only. That is, during late young adulthood, reporting greater cannabis use than one’s typical average was associated with reporting greater PTSD symptoms than one’s own average (B = 0.04). See Table 2 for results.
Figure 2.
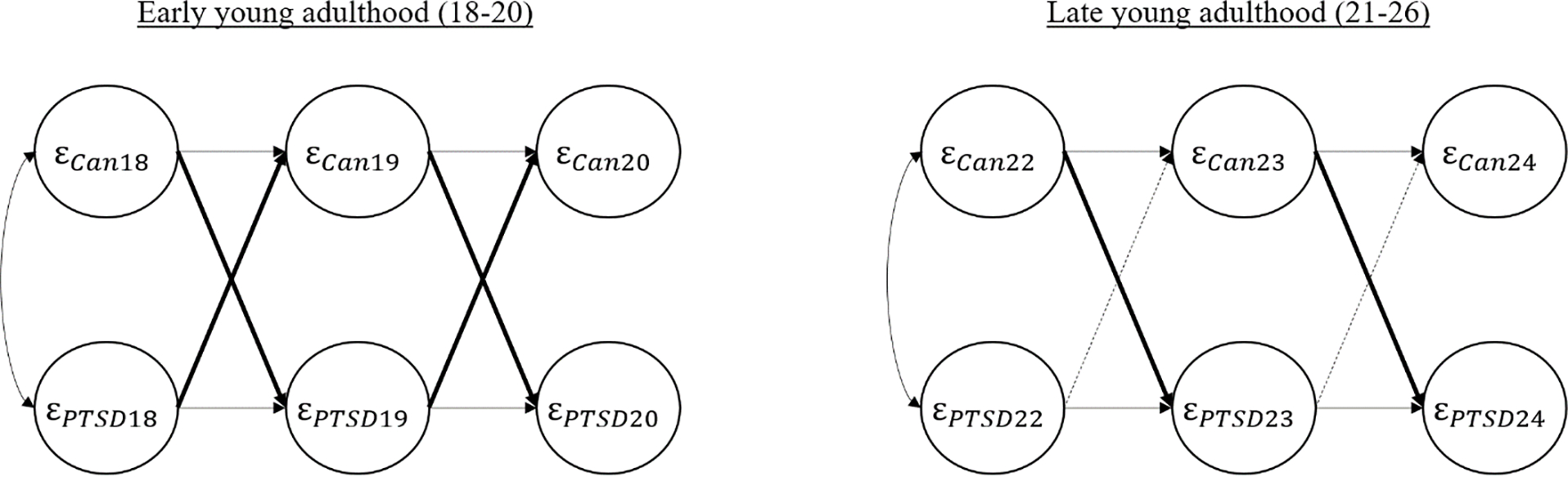
Visual representation of within-person lagged effects between PTSD symptoms and cannabis use from 18 to 26 years old for the whole sample
Note: Bold lines indicate significant lagged effect and dashed lines indicate non-significant lagged effect. Please see Table 2 and in-text description for beta estimates of these lagged effects.
Developmental variation among males and females
Final models for both males and females had excellent fit (males: CFI = 0.94; RMSEA = 0.04; SRMR = 0.16; females: CFI = 0.94; RMSEA = 0.04; SRMR = 0.13). Similar to the full sample, all model constraints did not result in significantly worse model fit. Results for males followed that of the full sample, noted above (see Table 2 for results). Specifically, results indicated a full reciprocal association between PTSD symptoms and cannabis use, supporting both a symptom-driven and substance-induced model during early young adulthood or ages 18–20 (see Figure 3a for visual representation of results). Reporting greater PTSD symptoms than one’s typical average was associated with reporting greater cannabis use than one’s typical average the next year (B = 0.85) and reporting greater cannabis use than one’s typical average was associated with greater PTSD symptoms than one’s own average the next year (B = 0.04). As males transitioned into late young adulthood from ages 21–26, similar to the full sample, there was only support for a substance-induced model whereby reporting greater cannabis use than one’s typical average was associated with reporting greater PTSD symptoms (B = 0.07).
Figure 3a.
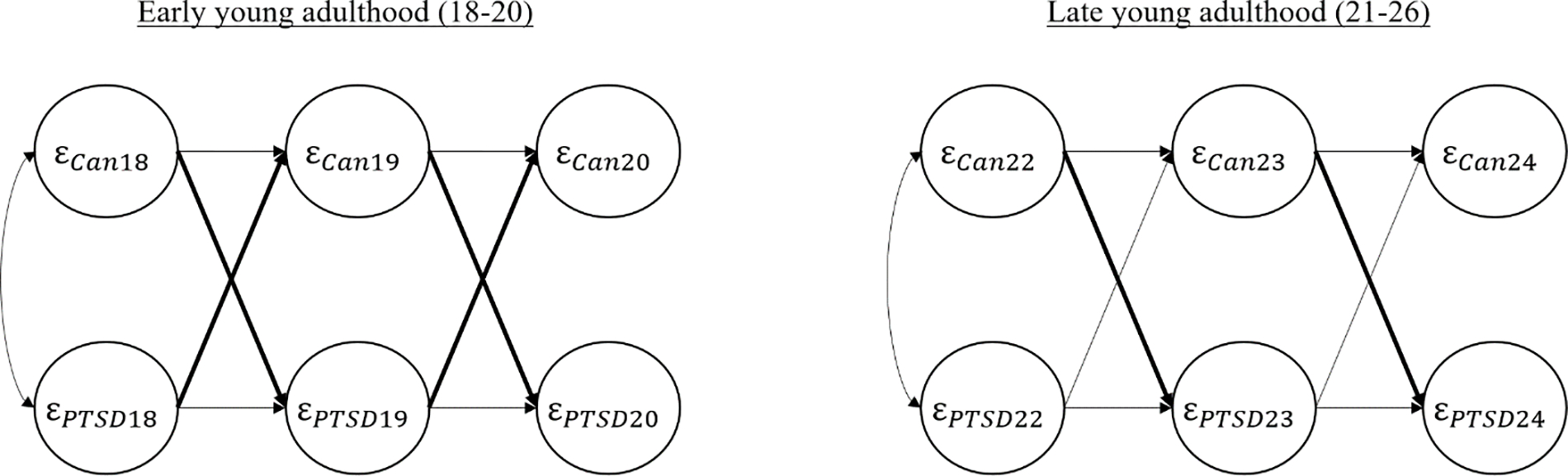
Visual representation of within-person lagged effects between PTSD symptoms and cannabis use from 18 to 26 years old for the men .
In contrast, for females, results revealed no reciprocal associations between cannabis use and PTSD symptoms during early young adulthood from age 18–20 (See Figure 3b for visual representation of results). However, as females transitioned to late young adulthood from ages 21–26, similar to results for the full sample and males, results only supported a substance-induced model in which reporting greater cannabis use than one’s typical average was associated with reporting greater PTSD symptoms (B = 0.04).
Figure 3b.
Visual representation of within-person lagged effects between PTSD symptoms and cannabis use from 18 to 26 years old for the females .
Note: bold lines indicate significant lagged effect – dashed lines indicate non-significant lagged effect. Please see Table 2 and in-text description for beta estimates of these lagged effects.
Developmental variation among racial and ethnic minority and non-minority young adults
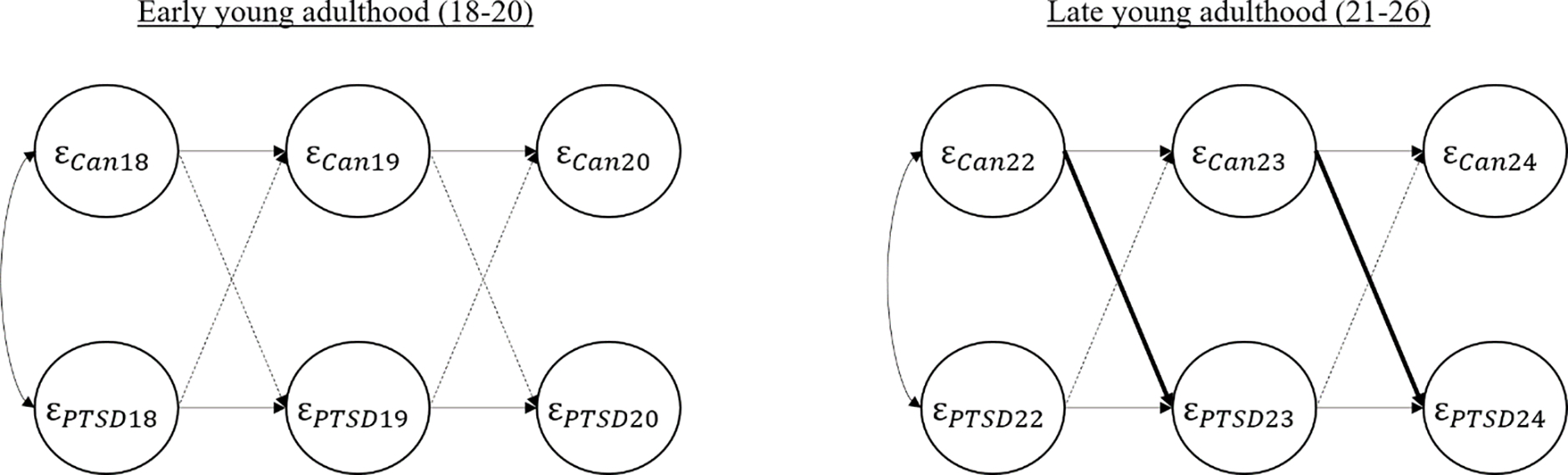
The final model for racial and ethnic minority participants had excellent fit (CFI = 0.96; RMSEA – 0.03; SRMR = 0.09). Similar to results for the full sample, results supported a full cross-lagged association between PTSD symptoms and cannabis use throughout both developmental periods (See Figure 4a for visual representation of results and Table 3). Thus, we found support for both pathways whereby reporting greater PTSD symptoms than one’s typical average was associated with reporting greater cannabis use than one’s own average the next year during both early young adulthood (B = 0.35) and late young adulthood (B = 0.33). In contrast to the full sample, we found support for the substance-induced pathway at both developmental periods whereby reporting greater cannabis use than one’s typical average was associated with greater PTSD symptoms than one’s own average during both early young adulthood (B = 0.03) and late young adulthood (B = 0.05).
Figure 4a.

Visual representation of within-person lagged effects between PTSD symptoms and cannabis use from 18 to 26 years old for racial and ethnic minority.
The final model for non-Hispanic White participants had adequate fit (CFI = 0.91; RMSEA – 0.05; SRMR = 0.17). Results did not support any reciprocal associations during either early and late young adulthood (see Figure 4b for visual representation of results). That is, our results did not show support of either pathway as there were no significant associations between PTSD and cannabis use for non-Hispanic White participants at either developmental period.
Figure 4b.
Visual representation of within-person lagged effects between PTSD symptoms and cannabis use from 18 to 26 years old for non-Hispanic White.
Note: bold lines indicate significant lagged effect – dashed lines indicate non-significant lagged effect. Please see Table 2 and in-text description for beta estimates of these lagged effects.
Post-hoc analyses
Though we were unable to provide lagged associations for each of the subgroups, the model for Hispanic participants did converge and provided good fit (CFI = 0.95; RMSEA = 0.04; SRMR = 0.11). Below we briefly describe results of effects for those identifying as Hispanic (all model results, tables, and figures can be found in supplemental materials). Results indicated no associations during early young adulthood. However, as individuals transitioned into late young adulthood, results indicated full reciprocal associations such that reporting greater cannabis use than one’s typical average was associated with greater symptoms of PTSD the next year (B = 0.05) and reporting greater PTSD symptoms than one’s own average was associated with greater cannabis use the next year.
Discussion
The transition from early to late young adulthood is a time of numerous developmental changes and a time when cannabis use peaks. Research has also shown that PTSD symptoms from recent or prior traumatic events may also begin to emerge during this time period. The goal of the present study was to help characterize the dynamic developmental interplay between cannabis use and PTSD symptomology by testing two directional hypotheses: the symptom-driven pathway, in which PTSD symptoms are a catalyst for future cannabis use, and the substance-induced pathway, in which cannabis use fuels greater PTSD symptomatology. Further, we examined shared vulnerabilities in these directional associations by sex and race and ethnicity given prior work in both the PTSD and cannabis fields showing differential symptom expressions and substance use between males and females and between non-Hispanic White and racial and ethnic minority individuals. Our results both support and refute prior theory and empirical work. Results also provide a more nuanced look at developmental associations between PTSD symptoms and cannabis use between males and females as well as between racial and ethnic minority individuals and non-Hispanic White individuals.
The first aim was to examine temporal associations between PTSD symptoms and cannabis use among all respondents with trauma exposure (i.e., those who met Criterion A). This is an important first step given that in a recent review of the literature focused on cannabis use and PTSD, only eight studies of 45 were longitudinal and none explored developmental effects. Our results supported both symptom-driven and substance-induced pathways during early young adulthood from ages 18–20 (see Figure 2 for visual representation of results); however, only support for a substance-induced pathway was noted for late young adulthood. Our results can be understood from stress-coping models of addiction. For decades, stress-coping models of addiction have posited that some individuals use cannabis (or other substances) to cope with life stress and to reduce negative affect (Wagner, Myers, & McIninch, 1999; Wills & Filer, 1996). Research on the association between stress and cannabis use dates to the mid-1980s when adults who used cannabis were interviewed and described its use as an escape or relief from problems, and that it helped ease frustrations and life stressors (Haas & Hendin, 1987). A review of studies addressing the connection between cannabis use and stress concluded that using cannabis to cope with stressful events may be one of the most common reasons for use among those who report heavy use (Hyman & Sinha, 2009). Thus, it may be that young adults cope with symptoms of PTSD by using cannabis as a way to avoid, forget, or relieve these stressful feelings, emotions, and physical sensations. This is a reasonable hypothesis given that many studies have noted that individuals with a diagnosis of PTSD may use cannabis and cannabis-related compounds due to their anxiolytic and sedative effects (Elms, Shannon, Hughes, & Lewis, 2019; Greer, Grob, & Halberstadt, 2014; Tull, McDermott, & Gratz, 2016). Our results, however, also revealed an interesting and dynamic interplay between PTSD and cannabis use. In particular, during early young adulthood when participants were ages 18–20, we noted a fully cross-lagged, reciprocal association between PTSD and cannabis use. Thus, during this period of development both the symptom-driven pathway and substance-induced pathway were supported whereby reporting heightened symptoms of PTSD was associated with greater cannabis use the following year and, in turn, this greater cannabis use was associated with greater PTSD symptoms the next year. Thus, from ages 18–20, it seems that utilizing cannabis as a way to relieve symptoms of PTSD has the opposite effect. However, when participants reached late young adulthood from ages 21–26, results only supported a substance-induced pathway, with greater cannabis use associated with greater PTSD symptoms the next year. There is growing interest in the use of medical cannabinoids for treatment refractory PTSD; however, research in this area remains mixed. For example, some research supports use of cannabis as a primary or adjunctive treatment for PTSD, demonstrating reductions or amelioration of trauma-related symptoms including intrusive thoughts, anxiety, and sleep (Bedard-Gilligan, Lehinger, Cornell-Maier, Holloway, & Zoellner, 2022); however, recent reviews of the literature and comprehensive reports from the National Academies of Science, Engineering, and Medicine note little evidence in the use of cannabis or synthetic cannabis for PTSD symptoms reduction (Orsolini et al., 2019). Thus, although many believe that cannabis may alleviate, or mask, symptoms of PTSD, our results suggest that individuals may experience worsening symptomatology with greater use as they transition into late adulthood.
Results for the whole sample provide a first step in understanding the dynamic interplay between PTSD symptoms and cannabis use, and we also note important differences by sex and race and ethnicity. First, results indicate some stark differences between males and females. Results for males mirrored that of the whole sample; however, for females, we saw no associations between PTSD symptoms and cannabis use during early young adulthood. Yet, in late young adulthood, heightened cannabis use was associated with increased PTSD symptoms the next year for females, similar to results for males (and the sample as a whole), highlighting that both groups experience worsening symptomatology with greater use as they transition into late adulthood. There are likely multiple explanations for these male and female differences in early young adulthood, and one reason may be differences in coping with traumatic events. In general, there is agreement in the literature that substance use may be used to navigate unwanted and uncomfortable symptoms of PTSD – thus, a cycle ensues whereby one experiences a traumatic event, which cues an individual to use cannabis (or other substance) as a way to self-medicate or avoid overwhelming feelings, which can lead to other downstream negative outcomes (e.g., greater PTSD). Prior work has suggested that individuals who experience trauma, in particular males, are more prone to utilize disengagement coping strategies, such as cannabis use, and engagement in these coping strategies is linked to PTSD (Tripp et al., 2020). Unfortunately, disengagement coping strategies are relatively common among those who have experienced trauma, as actively working through a traumatic experience can be perceived as emotionally unbearable. Our results support this notion such that males, especially in early young adulthood, seemed to be caught in a cycle of experiencing heightened symptoms of PTSD, which leads to greater cannabis use, and subsequently to greater PTSD symptoms. In contrast, females tend to utilize emotion-focused coping strategies more often such as positive reappraisal or prayer, which focus on helping the individual lessen psychological distress and reduce negative affect (Heckhausen & Schulz, 1995). Thus, in line with our results, it may be that, for females, cannabis use is not a viable response to heightened symptoms of PTSD and other emotion-focused constructs such as guilt or shame may play a larger role. In fact, some research with females who have experienced intimate partner violence suggests this may be the case as females who frequently use emotion-focused forms of coping are at heightened risk for PTSD symptoms, regardless of the extent of their violence exposure (Lilly & Graham-Bermann, 2010). Future research may wish to explore these more emotion-focused constructs in relation to PTSD symptoms to unearth important, longitudinal, lagged effects.
Finally, our results indicate important, and somewhat surprising, differences between non-Hispanic White individuals compared to racial and ethnic minority individuals in the dynamic interplay of PTSD with cannabis use. Among non-Hispanic White participants, we did not find lagged associations between PTSD symptoms and cannabis use during either early or late young adulthood. On the other hand, full reciprocal associations between PTSD symptoms and cannabis use were found throughout both early and late young adulthood for racial and ethnic minority participants. In our post-hoc analyses for those identifying as Hispanic, we also noted full reciprocal associations during late young adulthood (but no associations in early young adulthood). From an epidemiological perspective, rates of PTSD in the United States are estimated to be slightly higher for Black (compared to White) adults, and slightly lower for Hispanic (compared to White) adults (Roberts et al., 2011). Further, racial and ethnic variation exists in the frequency of cannabis use among adults (Jeffers et al., 2021; SAMHSA, 2021). Given these differences in basic prevalence rates, there is likely variation in associations between PTSD symptoms and cannabis use when examining specific racial and ethnic subgroups. This is a limitation of the present study as our grouping variable included Asian American, Hispanic, and Black individuals given the small sample sizes of some groups and the complexity of our models. We hope that this study spurs further research into uncovering heterogeneity across racial and ethnic minority groups as the literature in this area is quite limited (D’Amico et al., 2023).
Another potential explanation for racial and ethnic differences lies in: 1) the way in which racial and ethnic minority communities have experienced and endured both current and historical trauma; and 2) the way in which we conceptualize PTSD. Unfortunately, there are certain racial and ethnic groups in the United States who have experienced both current and historical traumatic events, including (but not limited to) resettlement, colonization, slavery, forced assimilation, and genocide (Gone et al., 2019). Though some may consider these events too far in the past to influence behavior, historical trauma has been shown to transfer consciously or unconsciously through learned behavior (e.g., violence), hypervigilance of a caregiver or family member, learned cognitive schemas (e.g., the world is dangerous), and through genetic or epigenetic changes (Yahyavi, Zarghami, & Marwah, 2013). In addition to these historical events, ethnic and racial minorities also experience current, acute, and chronic stressors associated with discrimination and oppression. Studies also highlight that individuals identifying as a racial or ethnic minority experience more discrimination than White individuals with a recent report showing greater prevalence rates of discrimination for Black (31.8%) and Hispanic (27%) respondents compared to White respondents (23.5%), (Lee, Perez, Malik Boykin, & Mendoza-Denton, 2019). The culmination of both historical, acute, and chronic stressors may help, in part, explain why our results noted strong, reciprocal, associations between PTSD and cannabis use among ethnic and racial minority participants and no association among non-Hispanic White participants. Theories such as minority stress theory indicate that the cumulative effects of these stressors can lead to health disparities, with some empirical work showing that discrimination-based stress is associated with both psychological and physiological maladaptive stress responses (Deuster, Kim-Dorner, Remaley, & Poth, 2011). In fact, some have even suggested that these cumulative discrimination-based stressors may serve as a catalyst for psychiatric disorders such as PTSD (Helms, Nicolas, & Green, 2016). Recent research has criticized the current Criterion A language for a PTSD diagnosis because it does not include insidious trauma that is oppression and discrimination focused (Holmes, Facemire, & DaFonseca, 2016). This is a major oversight by the American Psychiatric Association as oppression (in the form of both discrimination experiences as well as imbalance of power) can occur at the intrapersonal level (e.g., internalized oppression), interpersonal level (e.g., experiences verbal or emotional abuse, actual threats of violence), environmental level (e.g. social fragmentation), as well as the local/state level (e.g., structural inequalities/discrimination) (Prilleltensky & Gonick, 1996). Though we are not able to determine this from the present study, our results may be picking up signals of trauma among ethnic and racial minority individuals that are not currently present in the DSM 5 for a diagnosis of PTSD yet may be acting as a catalyst for the use of certain coping strategies (e.g., cannabis use) which seem to fuel worsening symptoms of PTSD. From our results, it appears that individuals from minoritized groups are more likely to experience an ongoing cycle of heightened PTSD symptomology, which contributes to greater cannabis use, which in turn contributes to worsening PTSD symptoms throughout the entire duration of young adulthood, which may be related to current, acute, and chronic stressors associated with discrimination and oppression.
Other explanations for our results may lie in access to care or resources. Prior to the Affordable Care Act, numerous studies noted vast disparities in both insurance coverage as well as access to care between non-Hispanic White individuals compared to racial and ethnic minority individuals (Mahajan et al., 2021). Although recent research does note that coverage expansions coinciding with the Affordable Care Act have been associated with reduced racial and ethnic disparities, these gains have all but stalled since 2018 (Baumgartner, Collins, Radley, & Hayes, 2020). Thus, some of our results may be artifacts that have re-emerged in recent years with Medicaid and insurance expansion coming to a standstill, thus potentially contributing to lack of access or lack of coverage for health care.
Limitations and conclusion
This study should be interpreted in light of several limitations. First, data are self-reported and thus results are potentially biased due to shared variance. Second, PTSD symptoms were measured using a well-established screener for possible PTSD diagnosis, but it is not a diagnostic measure. Third, although we have temporally ordered data, we cannot determine causality. Fourth, although we did address heterogeneity across sex and race and ethnicity, more research is needed to address subgroup differences by race and ethnicity, sexual and gender minority identities, and other shared vulnerabilities. The present study is meant to be an initial step forward in understanding long-term associations between PTSD and cannabis use. Unfortunately, our sample sizes are too small to extract meaningful estimates across all racial and ethnic subgroups, thus our results may conflate effects and should not be used as an “end all” for this area of study. It is vitally important for future research to explore effects using a more robust intersectional approach. Finally, although our study does represent one of the largest samples to test associations between PTSD and cannabis use, our subsample analyses may be underpowered to detect effects.
Overall, the present study supports and extends our understanding of directional associations between PTSD symptomatology and cannabis use. In particular, we show a nuanced set of results supporting a dynamic interplay between PTSD and cannabis use. It is essential for clinicians to recognizing how pathways between cannabis use and PTSD symptoms may interact, especially the distinct differences that emerged between males and females, as well as between non-Hispanic White individuals and racial and ethnic minority individuals. This is especially critical as recent reports of increased cannabis potency are associated with greater likelihood of onset of psychiatric symptomology (Wilson, Freeman, & Mackie, 2019). Research is needed to better understand variation in associations for different racial and ethnic groups, which can help inform prevention and interventions efforts to address disparities. Future research also should continue exploring within-person change and include important mechanisms that may link PTSD and cannabis use during young adulthood such as experiences of discrimination, coping strategies, as well as other psychiatric disorders. Further, future research may also wish to explore lagged effects based on PTSD symptom clusters as this may reveal unique associations across sex and race and ethnicity. Overall, our results highlight that the link between cannabis use and PTSD is complex with important differences emerging depending upon shared vulnerabilities.
Supplementary Material
Public health statement:
This study indicates that longitudinal associations between PTSD and cannabis use vary by demographic characteristics, with male and minoritized racial and ethnic young adults showing a cyclic nature of experiencing heightened symptoms of PTSD leading to greater cannabis use which, in turn, results in worsening PTSD.
Funding:
Work on this article was supported by one grant from National Institute on Drug Abuse (1R21DA051802) to Jordan P. Davis and four grants from the National Institute of Alcohol Abuse and Alcoholism (R01AA016577; R01AA020883; R01AA025848; R01AA028812) to Elizabeth D’Amico.
Footnotes
Declaration of interest: none to declare
References
- Ahern J, Worthen M, Masters J, Lippman SA, Ozer EJ, & Moos R (2015). The Challenges of Afghanistan and Iraq Veterans’ Transition from Military to Civilian Life and Approaches to Reconnection. PLOS ONE, 10(7), e0128599. 10.1371/journal.pone.0128599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders : DSM-5. American Psychiatric Association. [Google Scholar]
- Atwoli L, Stein DJ, Koenen KC, & McLaughlin KA (2015). Epidemiology of posttraumatic stress disorder: prevalence, correlates and consequences. Current Opinion in Psychiatry, 28(4), 307. 10.1097/YCO.0000000000000167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgartner J, Collins S, Radley D, & Hayes S. (2020). How the Affordable Care Act (ACA) Has Narrowed Racial and Ethnic Disparities in Insurance Coverage and Access to Health Care, 2013–18. Health Services Research, 55(S1), 56–57. 10.1111/1475-6773.13406 [DOI] [Google Scholar]
- Bedard-Gilligan M, Lehinger E, Cornell-Maier S, Holloway A, & Zoellner L (2022). Effects of Cannabis on PTSD Recovery: Review of the Literature and Clinical Insights. Current Addiction Reports, 9(3), 203–216. 10.1007/S40429-022-00414-X/METRICS [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry D, & Willoughby M (2017). On the practical interpretabilty of cross-lagged panel models:Rethinking a developmental workhorse. Child Development, 0(0), 1–21. [DOI] [PubMed] [Google Scholar]
- Brady KT, Back SE, & Coffey SF (2004). Substance Abuse and Posttraumatic Stress Disorder. Current Directions in Psychological Science, 13(5), 206–209. 10.1111/j.0963-7214.2004.00309.x [DOI] [Google Scholar]
- Brady KT, Killeen TK, Brewerton T, & Lucerini S (2000). Comorbidity of psychiatric disorders and posttraumatic stress disorder. Journal of Clinical Psychiatry. [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson EL, & Schultz LR (1997). Sex Differences in Posttraumatic Stress Disorder. Archives of General Psychiatry, 54(11), 1044–1048. 10.1001/ARCHPSYC.1997.01830230082012 [DOI] [PubMed] [Google Scholar]
- Chilcoat HD, & Breslau N (1998). Investigations of causal pathways between ptsd and drug use disorders. Addictive Behaviors, 23(6), 827–840. 10.1016/S0306-4603(98)00069-0 [DOI] [PubMed] [Google Scholar]
- Coleman JA (2016). Racial Differences in Posttraumatic Stress Disorder in Military Personnel: Intergenerational Transmission of Trauma as a Theoretical Lens. Http://Dx.Doi.Org/10.1080/10926771.2016.1157842, 25(6), 561–579. 10.1080/10926771.2016.1157842 [DOI] [Google Scholar]
- Cromer LDM, & Smyth JM (2009). Making Meaning of Trauma: Trauma Exposure Doesn’t Tell the Whole Story. Journal of Contemporary Psychotherapy 2009 40:2, 40(2), 65–72. 10.1007/S10879-009-9130-8 [DOI] [Google Scholar]
- Cuffe SP, Addy CL, Garrison CZ, Waller JL, Jackson KL, McKeown RE, & Chilappagari S (1998). Prevalence of PTSD in a Community Sample of Older Adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 37(2), 147–154. 10.1097/00004583-199802000-00006 [DOI] [PubMed] [Google Scholar]
- Curran PJ, Howard AL, Bainter SA, Lane ST, & McGinley JS (2014). The separation of between-person and within-person components of individual change over time: A latent curve model with structured residuals. Journal of Consulting and Clinical Psychology, 82(5), 879–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Dunbar MS, Perez L, Siconolfi D, Davis JP, … Rodriguez A (2023). Unpacking disparities in substance-related outcomes among racial, ethnic, sexual, and gender minoritized groups during adolescence and emerging adulthood. Psychology of Addictive Behaviors : Journal of the Society of Psychologists in Addictive Behaviors, 37(5), 651–656. 10.1037/ADB0000905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JNV, Zhou AJ, Shih RA, & Green HD (2012). Preventing Alcohol Use with a Voluntary After-School Program for Middle School Students: Results from a Cluster Randomized Controlled Trial of CHOICE. Prevention Science, 13(4), 415–425. 10.1007/s11121-011-0269-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deuster PA, Kim-Dorner SJ, Remaley AT, & Poth M (2011). Allostatic load and health status of African Americans and whites. American Journal of Health Behavior, 35(6), 641–653. 10.5993/AJHB.35.6.1 [DOI] [PubMed] [Google Scholar]
- Dworkin ER, Kaysen D, Bedard-Gilligan M, Rhew IC, & Lee CM (2017). Daily-level associations between PTSD and cannabis use among young sexual minority women. Addictive Behaviors, 74, 118–121. 10.1016/J.ADDBEH.2017.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellickson PL, McCaffrey DF, Ghosh-Dastidar B, & Longshore DL (2003). New Inroads in Preventing Adolescent Drug Use: Results From a Large-Scale Trial of Project ALERT in Middle Schools. American Journal of Public Health, 93(11), 1830–1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elms L, Shannon S, Hughes S, & Lewis N (2019). Cannabidiol in the Treatment of Post-Traumatic Stress Disorder: A Case Series. Journal of Alternative and Complementary Medicine, 25(4), 392–397. 10.1089/ACM.2018.0437/ASSET/IMAGES/LARGE/FIGURE1.JPEG [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost DM, & Meyer IH (2023). Minority stress theory: Application, critique, and continued relevance. Current Opinion in Psychology, 51, 101579. 10.1016/J.COPSYC.2023.101579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullerton CS, Ursano RJ, Epstein RS, Crowley B, Vance K, Kao TC, … Baum A (2001). Gender differences in posttraumatic stress disorder after motor vehicle accidents. American Journal of Psychiatry, 158(9), 1486–1491. 10.1176/APPI.AJP.158.9.1486/ASSET/IMAGES/LARGE/J620F1.JPEG [DOI] [PubMed] [Google Scholar]
- Gil S, Caspi Y, Ben-Ari IZ, Koren D, & Klein E (2005). Does memory of a traumatic event increase the risk for posttraumatic stress disorder in patients with traumatic brain injury? A prospective study. American Journal of Psychiatry, 162(5), 963–969. 10.1176/APPI.AJP.162.5.963/ASSET/IMAGES/LARGE/P120F2.JPEG [DOI] [PubMed] [Google Scholar]
- Gone JP, Hartmann WE, Pomerville A, Wendt DC, Klem SH, & Burrage RL (2019). The impact of historical trauma on health outcomes for indigenous populations in the USA and Canada: A systematic review. American Psychologist, 74(1), 20–35. 10.1037/AMP0000338 [DOI] [PubMed] [Google Scholar]
- Greer GR, Grob CS, & Halberstadt AL (2014). PTSD Symptom Reports of Patients Evaluated for the New Mexico Medical Cannabis Program. 10.1080/02791072.2013.873843, 46(1), 73–77. 10.1080/02791072.2013.873843 [DOI] [PubMed] [Google Scholar]
- Haas AP, & Hendin H (1987). The Meaning of Chronic Marijuana Use among Adults: A Psychosocial Perspective. 10.1177/002204268701700402, 17(4), 333–348. 10.1177/002204268701700402 [DOI] [Google Scholar]
- Hapke U, Schumann A, Rumpf HJ, John U, & Meyer C (2006). Post-traumatic stress disorder: The role of trauma, pre-existing psychiatric disorders, and gender. European Archives of Psychiatry and Clinical Neuroscience, 256(5), 299–306. 10.1007/S00406-006-0654-6/METRICS [DOI] [PubMed] [Google Scholar]
- Hatch SL, Bruce AE, & Dohrenwend P (2007). Distribution of Traumatic and Other Stressful Life Events by Race/Ethnicity, Gender, SES and Age: A Review of the Research. American Journal of Community Psychology, 40(3), 313–332. 10.1007/s10464-007-9134-z [DOI] [PubMed] [Google Scholar]
- Heckhausen J, & Schulz R (1995). A Life-Span Theory of Control. Psychological Review, 102(2), 284–304. 10.1037/0033-295X.102.2.284 [DOI] [PubMed] [Google Scholar]
- Helms JE, Nicolas G, & Green CE (2016). Racism and Ethnoviolence as Trauma. 10.1177/1534765610396728, 18(1), 65–74. 10.1177/1534765610396728 [DOI] [Google Scholar]
- Hicks TA, Zaur AJ, Keeley JW, & Amstadter AB (2022). The association between recreational cannabis use and posttraumatic stress disorder: A systematic review and methodological critique of the literature. Drug and Alcohol Dependence, 240, 109623. 10.1016/J.DRUGALCDEP.2022.109623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes SC, Facemire VC, & DaFonseca A . (2016). Expanding criterion a for posttraumatic stress disorder: Considering the deleterious impact of oppression. Traumatology, 22(4), 314–321. Retrieved from https://psycnet.apa.org/record/2016-50438-001 [Google Scholar]
- Hyman SM, & Sinha R (2009). Stress-related factors in cannabis use and misuse: Implications for prevention and treatment. Journal of Substance Abuse Treatment, 36(4), 400–413. 10.1016/J.JSAT.2008.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffers AM, Glantz S, Byers A, & Keyhani S (2021). Sociodemographic Characteristics Associated With and Prevalence and Frequency of Cannabis Use Among Adults in the US. JAMA Network Open, 4(11), e2136571–e2136571. 10.1001/JAMANETWORKOPEN.2021.36571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, … Koenenon KC (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology, 8(5). 10.1080/20008198.2017.1353383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, S, F., … Solomon Z,MMFBWY. (1995). Posttraumatic Stress Disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048. 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Khan S, Okuda M, Hasin DS, Secades-Villa R, Keyes K, Lin K-H, … Blanco C (2013). Gender Differences in Lifetime Alcohol Dependence: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcoholism: Clinical and Experimental Research, n/a-n/a. 10.1111/acer.12158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian E. (2003). The self-medication hypothesis revisited: The dually diagnosed patient. Primary Psychiatry, 10(9), 47–54. Retrieved from https://www.researchgate.net/profile/Edward_Khantzian/publication/279937759_The_Self-Medication_Hypothesis_Revised_The_Dually_Diagnosed_Patient/links/55f2d4ad08ae1d9803921bac/The-Self-Medication-Hypothesis-Revised-The-Dually-Diagnosed-Patient [Google Scholar]
- Khantzian EJ (1985). The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. The American Journal of Psychiatry, 142(11), 1259–1264. 10.1176/ajp.142.11.1259 [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, & Acierno R (2003). Mental health needs of crime victims: Epidemiology and outcomes. Journal of Traumatic Stress, 16(2), 119–132. 10.1023/A:1022891005388 [DOI] [PubMed] [Google Scholar]
- Kirmayer L, Gone J, & Moses J (2014). Rethinking historical trauma. Transcultural Psychiatry, 51(3), 299. 10.1177/1363461514536358 [DOI] [PubMed] [Google Scholar]
- Lee RT, Perez AD, Malik Boykin C, & Mendoza-Denton R (2019). On the prevalence of racial discrimination in the United States. PLOS ONE, 14(1), e0210698. 10.1371/JOURNAL.PONE.0210698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilly MM, & Graham-Bermann SA (2010). Intimate Partner Violence and PTSD: The Moderating Role of Emotion-Focused Coping. Violence and Victims, 25(5), 604–616. 10.1891/0886-6708.25.5.604 [DOI] [PubMed] [Google Scholar]
- Littleton H, Horsley S, John S, & Nelson DV (2007). Trauma coping strategies and psychological distress: A meta-analysis. Journal of Traumatic Stress, 20(6), 977–988. 10.1002/JTS.20276 [DOI] [PubMed] [Google Scholar]
- Mahajan S, Caraballo C, Lu Y, Valero-Elizondo J, Massey D, Annapureddy AR, … Krumholz HM (2021). Trends in Differences in Health Status and Health Care Access and Affordability by Race and Ethnicity in the United States, 1999–2018. JAMA, 326(7), 637–648. 10.1001/JAMA.2021.9907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mclaughlin KA, Alvarez K, Fillbrunn M, Green JG, Jackson JS, Kessler RC, … Alegría M (2019). Racial/ethnic variation in trauma-related psychopathology in the United States: a population-based study. Psychological Medicine, 49(13), 2215–2226. 10.1017/S0033291718003082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén BO, & Muthén LK (n.d.). Mplus User’s Guide: Eigth Edition. Los Angeles, CA. [Google Scholar]
- National Comorbidity Survey (NCS). (2007). Data Table 2: 12-month prevalence DSM-IV/WMH-CIDI disorders by sex and cohort. [Google Scholar]
- Orsolini L, Chiappini S, Volpe U, De Berardis D, Latini R, Papanti GD, & Corkery JM (2019). Use of Medicinal Cannabis and Synthetic Cannabinoids in Post-Traumatic Stress Disorder (PTSD): A Systematic Review. Medicina 2019, Vol. 55, Page 525, 55(9), 525. 10.3390/MEDICINA55090525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe EA, & Richman LS (2009). Perceived Discrimination and Health: A Meta-Analytic Review. Psychological Bulletin, 135(4), 531–554. 10.1037/A0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prilleltensky I, & Gonick L (1996). Polities Change, Oppression Remains: On the Psychology and Politics of Oppression. Political Psychology, 17(1), 127. 10.2307/3791946 [DOI] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Camerond RP, Hugelshofer DS, Shaw-Hegwer J, … Sheikh JI (2004). The primary care PTSD screen (PC–PTSD): development and operating characteristics. Primary Care Psychiatry, 9(1), 9–14. 10.1185/135525703125002360 [DOI] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, & Koenen KC (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine, 41(1), 71–83. 10.1017/S0033291710000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA. (2021). Key substance use and mental health indicators in the United States: Results from the 2021 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD. [Google Scholar]
- SAMHSA. (2022). Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality (SAMHSA/CBHSQ, 2022), National Survey on Drug Use and Health, 2021 Detailed Tables. [Google Scholar]
- Sanjuan PM, Pearson MR, Poremba C, Amaro H, de LA, & Leeman L. (2019). An ecological momentary assessment study examining posttraumatic stress disorder symptoms, prenatal bonding, and substance use among pregnant women. Drug and Alcohol Dependence, 195, 33–39. 10.1016/J.DRUGALCDEP.2018.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological Momentary Assessment. Https://Doi.Org/10.1146/Annurev.Clinpsy.3.022806.091415, 4, 1–32. 10.1146/ANNUREV.CLINPSY.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- Spindler H, Elklit A, & Christiansen D (2010). Risk factors for posttraumatic stress disorder following an industrial disaster in a residential area: A note on the origin of observed gender differences. Gender Medicine, 7(2), 156–165. 10.1016/J.GENM.2010.04.001 [DOI] [PubMed] [Google Scholar]
- Tolin DF, & Foa EB (2008). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Trauma: Theory, Research, Practice, and Policy, S(1), 37–85. 10.1037/1942-9681.S.1.37 [DOI] [PubMed] [Google Scholar]
- Tolin D, & Gender F (2022). PTSD: a cognitive model. In Kimerling R, Ouimette P, & Wolfe J (Eds.), Gender and PTSD (pp. 66–97). New York: The Guilford Press. [Google Scholar]
- Tripp JC, Worley MJ, Straus E, Angkaw AC, Trim RS, & Norman SB (2020). Bidirectional Relationship of Posttraumatic Stress Disorder (PTSD) Symptom Severity and Alcohol Use Over the Course of Integrated Treatment. Psychology of Addictive Behaviors. 10.1037/ADB0000564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, McDermott MJ, & Gratz KL (2016). Marijuana dependence moderates the effect of posttraumatic stress disorder on trauma cue reactivity in substance dependent patients. Drug and Alcohol Dependence, 159, 219–226. 10.1016/J.DRUGALCDEP.2015.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner EF, Myers MG, & McIninch JL (1999). Stress-coping and temptation-coping as predictors of adolescent substance use. Addictive Behaviors, 24(6), 769–779. 10.1016/S0306-4603(99)00058-1 [DOI] [PubMed] [Google Scholar]
- Wills TA, & Filer M (1996). Stress—Coping Model of Adolescent Substance Use. Advances in Clinical Child Psychology, 91–132. 10.1007/978-1-4613-0323-7_3 [DOI] [Google Scholar]
- Wilson J, Freeman TP, & Mackie CJ (2019). Effects of increasing cannabis potency on adolescent health. The Lancet Child & Adolescent Health, 3(2), 121–128. 10.1016/S2352-4642(18)30342-0 [DOI] [PubMed] [Google Scholar]
- Yahyavi ST, Zarghami M, & Marwah U (2013). A review on the evidence of transgenerational transmission of posttraumatic stress disorder vulnerability. Brazilian Journal of Psychiatry, 36(1), 89–94. 10.1590/1516-4446-2012-0995 [DOI] [PubMed] [Google Scholar]
- Zeidner M (2006). Gender group differences in coping with chronic terror: The Israeli scene. Sex Roles, 54(3–4), 297–310. 10.1007/S11199-006-9346-Y/METRICS [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


