A 25-year-old female IT professional with a history of LASIK, 4 years back in both eyes, presented with redness, pain, and defective vision for 10 days in the right eye. There was a history of foreign body fall followed by which she had rubbed and washed her eyes frequently with tap water. She used topical fortified Amikacin 1%, Vigamox 0.5%, and homatropine hydrobromide 2% eye drops for the past 3 days from a general ophthalmologist. On examination, she had a mid-peripheral ring infiltrate (5 × 5 mm) in the flap interface with a central dense infiltrate of 3 × 2 mm, and the fluorescein stain was positive in the corresponding area [Fig. 1a].
Figure 1.
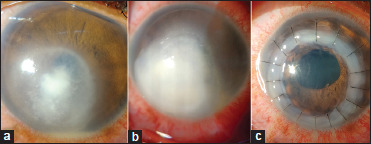
(a) Shows the interface ring infiltrate with central dense infiltrate. (b) Shows rapidly progressing infiltrate after 2 days of presentation. (c) Shows clear graft after therapeutic keratoplasty
What is your next step?
To start empirical topical and oral broad-spectrum antibiotics
Immediately lift the flap–scrap–culture–interface antibiotic and antifungal wash–treat
Based on the clinical findings start antifungal agents
Observation with topical therapy for 48 hrs and then perform corneal scraping
Correct answer:
b) Immediately lift the flap–scrap–culture interface antibiotic and antifungals wash–treat
Findings
Immediately the flap was lifted, scraped, and the stromal bed was washed with moxifloxacin 0.5% and amphotericin B 50 mcg/ml. Though the microbiological diagnosis was inconclusive, the dry texture of the infiltrate alluded us to suspect a fungal infiltrate. Hourly topical 5% natamycin and 1% voriconazole were prescribed, but in 2 days the infiltrate was progressing into the deeper layers of the corneal stroma [Fig. 1b]. A full-thickness therapeutic keratoplasty was done to prevent the intraocular spread of infection. The donor button culture revealed growth of Fusarium sp. in blood agar. Is it the DONOR BUTTON that had Fusarium? At one-month follow-up, the graft was clear without reinfection [Fig. 1c] and antifungals were continued for 4 months. The vision was 6/18 at the final visit.
Clinical diagnosis
Late post-LASIK interface fungal keratitis (LASIK-IFFK)
Discussion
The incidence of microbial keratitis following LASIK is rare (0–1.5%). The most common organisms causing post-LASIK infections are Staphylococcus sp., Streptococcus sp., atypical mycobacteria, and fungus.[1,2,3] The predisposing risk factors are dry eyes, intraoperative epithelial defects, delayed epithelialization, intraoperative contaminations, and the use of topical steroids. Our patient had developed an interface infection with Fusarium sp. following a dust fall, consequent vigorous eye rubbing, and frequent eye washing with tap water. The treatment options for refractory or progressive LASIK-IFFK include flap amputation, AMG, glue, and therapeutic keratoplasty. Often, they are mismanaged as the treatment method is different from corneal ulcers. Since fungus tends to penetrate deeper and involves intraocular structures rapidly, conservative management is not enough. Hence, early meticulous diagnosis and aggressive therapy with close follow-up are necessary.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mittal V, Jain R, Mittal R, Sangwan VS. Post-laser in situ keratomileusis interface fungal keratitis. Cornea. 2014;33:1022–30. doi: 10.1097/ICO.0000000000000227. [DOI] [PubMed] [Google Scholar]
- 2.Soleimani M, Haydar AA. Fungal keratitis after small incision lenticule extraction (SMILE): A case report and review of the literature. J Ophthalmic Inflamm Infect. 2021;11:25. doi: 10.1186/s12348-021-00256-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwartz B. Retaining the past. Surv Ophthalmol. 2004;49:491–508. [Google Scholar]


