Abstract
Background.
Gardening benefits health in older adults, but previous studies have limited generalizability or do not adequately adjust for socio-demographic factors or physical activity (PA).
Objective.
We examined health outcomes, fruit and vegetables (F&V) intake, and 10-year mortality risk among gardeners and exercisers compared to non-exercisers.
Design.
Cross-sectional data of non-institutionalized US adults in the 2019 Behavioral Risk Factor Surveillance System (BRFSS), a landline and cellular phone survey.
Participants/setting.
Adults aged 65+ reporting any PA (n=146,047) were grouped as gardeners, exercisers, or non-exercisers.
Main outcome measures.
Outcomes included cardiovascular disease (CVD) risk factors, mental and physical health, F&V intake, and 10-year mortality risk.
Statistical analyses.
Summary statistics were calculated and adjusted logistic regression models were conducted to calculate odds ratios (aOR) and 95% confidence intervals (CI), accounting for the complex survey design.
Results.
The sample included 10.2% gardeners, 60.0% exercisers, and 30.8% non-exercisers. Gardeners, compared to non-exercisers, had significantly lower odds of reporting all studied health outcomes and higher odds of consuming ≥5 F&V/day (CVD aOR 0.60 [95% CI: 0.53–0.68], stroke aOR 0.55 [95% CI: 0.47–0.64], heart attack aOR 0.63 [95% CI: 0.55–0.73], high cholesterol aOR 0.86 [95% CI: 0.79–0.93], high blood pressure aOR 0.74 [95% CI: 0.68–0.81], diabetes aOR 0.51 [95% CI: 0.46–0.56], BMI ≥25 aOR 0.74 [95% CI: 0.68–0.80], poor mental health status aOR 0.50 [95% CI: 0.43–0.59], poor physical health status aOR 0.35 [95% CI: 0.31–0.39], ≥5 F&V per day aOR 1.56 [95% CI: 1.40–1.57], high 10-year mortality risk aOR 0.39 [95% CI: 0.36–0.42]). Male and female gardeners had significantly lower odds of reporting diabetes even when compared exercisers.
Conclusion.
Among adults aged 65+, gardening is associated with better CVD health status including lower odds of diabetes. Future longitudinal or interventional studies are warranted to determine if promoting gardening activities can be a CVD risk reduction strategy.
Keywords: gardening, chronic disease, dietary intake, physical activity
INTRODUCTION
Cardiovascular disease (CVD) is the leading cause of premature death in the U.S. and unhealthy lifestyle behaviors such as low fruit and vegetable (F&V) intake and physical inactivity are associated with CVD.1–5 Despite the well-known benefits of healthy lifestyle behaviors for the prevention and treatment of CVD, fewer than 13% of Americans meet the minimum daily requirements for F&V intake6 and only 23% of U.S. adults meet both the recommended aerobic physical activity (PA) and muscle strengthening guidelines.7 Given the low number of Americans who meet the dietary and PA recommendations, new and innovative interventions are needed to improve both of these health behaviors.
One possible area for exploration is gardening; an activity that has especially gained popularity during the COVID-19 pandemic.8,9 According to the National Gardening Association, at least 1/3 (35%) of U.S. households participate in gardening10 and it is an activity that can be done in a range of locations (urban and rural) using in-ground, raised bed, or container-based methods. While the majority of U.S. gardening is home-based (92%), there are community gardens located in all 50 states11 including at schools,12 and on medical center campuses.13 The wide range of locations where gardening can be undertaken provides a potential opportunity for the implementation of gardening interventions.
Gardening has drawn the attention of public health advocates given the many investigations demonstrating its health benefits14,15 related to body mass index (BMI),16 diabetes,17 mental health,18 cancer survivorship,19,20 and quality of life.21 Further, there are several plausible reasons that gardening may have positive impacts on health, particularly among older adults. First, gardening is considered a multicomponent PA that encompasses balance, muscle-strengthening, and aerobic exercise obtained through a range of activities and intensities (e.g., watering [metabolic equivalents, METs]=1.5), weeding or cultivating [METs=3.5–4.5], planting crops [METs=4.3], and shoveling/digging [METs=5.0–7.8]).22,23 The Physical Activity Guidelines for Americans recommend that adults engage in a combination of at least 150 minutes (2.5 hours) of moderate intensity aerobic PA (a MET of 3.0 or higher) or 75 minutes of vigorous intensity aerobic PA (a MET of 6.0 or higher) per week in addition to engaging in muscle strengthening activities twice per week.24,25 Some reports have demonstrated that older adult gardeners spend 15–33 hours/week gardening during the active growing season (May-July) and the activities in which they engage average 3.8 METs.23 This is a duration and intensity that would fulfill an individual’s aerobic PA recommendation and potentially their strengthening recommendation depending on the activities in which they engaged.24,25 Second, gardening for fruits and vegetables (F&V) has the additional benefit of providing access to low-cost F&V14,26 and investigations have demonstrated that food gardeners consume more F&V than non-gardeners.27,28 Finally, emerging evidence suggests that exposure to nature in a variety of forms such as gardens, parks or forests, may have anti-inflammatory benefits and improve immune function.29
Given the many potential benefits of gardening, it is reasonable to consider that older adults who garden may have a lower prevalence of chronic diseases, better mental and physical health, and lower mortality risk than non-gardeners. Yet, the majority of studies that have reported on the benefits of gardening have been based on small or non-representative samples that did not account for socio-demographic factors or other PA in the analyses. Therefore, the purpose of this study was to compare health outcomes among gardeners, exercisers, and non-exercisers to better understand the association between gardening and a range of health outcomes in a national sample of older adults (aged 65+). Outcomes examined included CVD and chronic diseases (e.g., CVD, hyperlipidemia, hypertension, BMI, diabetes), stroke, heart attack, mental and physical health status, dietary intake, and 10-year mortality risk.
MATERIALS AND METHODS
The Behavioral Risk Factor Surveillance System (BRFSS) is a cross-sectional landline and cellular phone survey managed by the Centers for Disease Control and Prevention and administered at the state level. It includes a sample of non-institutionalized US adults (aged 18+) in 49 states, the District of Columbia, Guam, and Puerto Rico. Complete details regarding the BRFSS survey and sampling methodology are available elsewhere.30 The questionnaire includes annual core demographic and health-related measures, and biannual rotating core questions (i.e., during odd years). The present analysis included data from the 2019 survey cycle. This study was not considered human subjects research, under federal regulation 45 CFR 46.102(e), because it involved secondary analysis of de-identified, publicly-available data.
Physical Activity (PA) and Groups
Physical activity was assessed using the question: “In the past month, other than your regular job, did you participate in any physical activities such as running, calisthenics, golf, gardening, or walking for exercise? (yes/no)”. Participants were excluded from this analysis if they had a missing response or refused the PA question. Rotating PA questions for odd BRFSS survey years allows participants to choose: “What type of physical activity or exercise did you spend the most time doing during the past month?” Responses for two potential activities (first activity and second activity) were coded from a list of 75 options plus “other”. For this analysis, running and jogging were combined into one category and “other” activities were re-coded as missing. To determine the three groups (gardeners, exercisers, and non-exercisers), participants were grouped using the following criteria: 1) gardeners were those who reported any PA and selected gardening for either their first or second PA, 2) exercisers reported any PA but did not select gardening for either activity, and 3) non-exercisers did not report any PA. Participants were also asked how much time they spent engaged in each PA with the question “And when you took part in this activity, for how many minutes or hours did you usually keep at it?” The number of minutes was then multiplied by the number of times per week the participant indicated they engaged in the activity for a total number of minutes of PA/week. Because gardeners could engage in a second, non-gardening PA, gardening minutes and non-gardening minutes were calculated separately in addition to being summed for a total value. Muscle strengthening was assessed with a single question “During the past month, how many times per week or per month did you do physical activities or exercises to strengthen your muscles?” Based on responses to the above questions, BRFSS includes variables for each of the following coded as met/did not meet recommendations from The Physical Activity Guidelines for Americans including: 1) aerobic PA activity (≥150 minutes of a PA at a MET of 3.0 or higher, ≥75 minutes of vigorous PA at a MET of 6.0 or higher, or some combination), 2) muscle strengthening activities (2 times per week) or 3) met both.24 BRFSS assigns a MET value to each activity based on values outlined in the Compendium of Physical Activities.22 In order to control for the non-gardening PA and intensity in both groups, a non-gardening MET hours value was included in the logistic regression models (see statistical analysis below). Using the individual MET value for each non-gardening activity, MET hours were calculated by first converting minutes of PA/week to hours (minutes of PA per week/60). Then the hours were multiplied by the associated MET value. Non-exercisers were assigned a MET hours value of 0.
F&V Intake and Health Outcomes
Dietary intake of F&V in BRFSS was assessed using 6 items (fruit, fruit juice, green leafy vegetables, potatoes, fried potatoes, and other vegetables) and participants were asked to report how many times per day, week or month they consumed each item in the past 30 days. Responses were standardized to times per day and summed for a fruit and vegetables times per day value. This value was then dichotomized to < 5 times per day v. ≥ 5 times per day based on recent evidence supporting this as a target for potential CVD mortality risk reduction.31,32
Health outcomes were self-reported using the following, individual yes/no questions: “Has a doctor, nurse or other health professional ever told you that you had any of the following? [CVD or Angina, Stroke, Heart Attack, High cholesterol, Hypertension, Diabetes]”. High body mass index (BMI) was calculated with self-reported height and weight (weight in kg/height in meters2) and established using standard cut points (dichotomous: BMI < 25, BMI ≥ 25). Two questions were asked related to mental and physical health status (“Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” and “Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good (range 0–30)?”. Responses to these questions were dichotomized into two groups (0–13 days v ≥14 days) based on previously reported cut-points33 and notated as high or low levels of mental or physical health. We estimated 10-year mortality risk based on a validated index for older adults (aged 65+) which includes a weighted sum of risk factors including age, sex, BMI, medical history, smoking status, and physical functioning (range, 2.5–24.5).34 The index was adapted for BRFSS and scores were dichotomized into high risk (score ≥8) and low risk (0–7) using a previously established method for BRFSS data.35,36
Statistical Analysis
Summary statistics were calculated by group to describe the sample characteristics, health outcomes and the most frequently reported PAs. Differences between the groups for continuous variables were assessed using parametric or equivalent non-parametric t-tests. Differences for categorical variables were evaluated using chi-squared tests. Data presented are the unweighted sample (n) and weighted percentage. Weighting BRFSS data serves as an adjustment for variation in respondents’ probability of selection, non-coverage and non-response to ensure that data are representative of the population on key demographic characteristics (sex, age, race, education, marital status, home and phone ownership, and state/region).30 Bivariate logistic regression was used to calculate adjusted odds ratios (aOR) and 95% confidence intervals (CI) for each of the health outcomes, mental or physical health status, F&V intake, and mortality risk for gardeners and exercisers as compared to non-exercisers [referent group]. Contrast analysis was also performed to calculate OR and 95% CI for gardeners as compared to exercisers. Models were adjusted for the standard participant socio-demographics including: race/ethnicity (non-Hispanic Black, non-Hispanic White, Hispanic, Other), sex (dichotomous: male, female), education level (dichotomous: high school or less, more than high school), and marital status (dichotomous: married or living as married, any other). Non-gardening MET hours/week was included in all models. We also conducted two sensitivity analyses. First, since gardening may be more prevalent among women, we tested for effect modification by sex by including an interaction term for sex and group.10,37 Second, in order to further isolate the impact of gardening, we re-ran all models for gardeners who engaged in <150 minutes of non-gardening PA. Data were analyzed using SAS version 9.3 (SAS Institute Inc., Cary, NC) and were weighted according to BRFSS analytical guidelines.30
RESULTS
The 2019 BRFSS survey included a sample of 152,424 participants aged 65+. After removing those with incomplete physical activity responses (n=6,377), 146,047 (94.7%) remained for analysis. The final sample was 10.2% (n=14,903) gardeners, 60.0% (n=86,190) exercisers, and 30.8% (n=45,007) non-exercisers. Participant socio-demographic and health characteristics by group are presented in Table 1. Among gardeners, 30 participants reported gardening for both their first and second activity and were only counted one time in the gardening group. Gardeners, as compared to exercisers and non-exercisers, were more likely to be women, non-Hispanic white, and married or living as married. Gardeners and exercisers were both more likely than non-exercisers to have more than a high school education (Table 1). Gardening was the second most commonly reported first activity, second only to walking, for both women and men (10.0% and 7.1% respectively). There were differences in the second activity rankings by sex (women: household activities, 9.9%; men: yard work 6.3%). Weighted estimates for the first and second activities by sex are reported in Supplementary Table 2.
Table 1.
Descriptive characteristics of study participants who reported physical activity (yes/no) grouped as gardeners, non-gardening exercisers, or non-exercisers, Behavioral Risk Factor Surveillance System (BRFSS), 2019 (n=146,047)a
| Participants, No. (%)b | |||
|---|---|---|---|
|
| |||
| Characteristic | Gardeners 14,903 (10.2)c | Exercisers 86,190 (60.0) | Non-exercisers 45,007 (30.8) |
| Sex, women | 9,937 (62.2) | 46,868 (51.8) | 28,086 (59.3) |
|
| |||
| Race/ethnicity | |||
| Non-Hispanic Black | 528 (5.8) | 4,887 (8.7) | 3,377 (9.8) |
| Non-Hispanic White | 13,225 (82.5) | 74,406 (78.3) | 36,873 (73.4) |
| Hispanic | 497 (7.2) | 2,926 (7.7) | 2,476 (12.1) |
| Other | 653 (4.5) | 3,918 (5.3) | 2,281 (4.7) |
|
| |||
| Married or living as married | 8,455 (61.1) | 46,506 (59.4) | 19,346 (48.2) |
|
| |||
| Education, High School or Less | 4,277 (35.6) | 24,775 (35.8) | 21,573 (56.0) |
|
| |||
| Chronic Disease | |||
| Hypertension, yes | 8,496 (57.1) | 49,093 (57.8) | 29,834 (66.6) |
| Heart Attack, yes | 1,142 (8.5) | 8,079 (9.5) | 6,171 (13.8) |
| CVDd or Angina, yes | 1,207 (8.0) | 8,383 (10.1) | 5,966 (12.9) |
| Stroke, yes | 867 (5.5) | 5,647 (7.0) | 4,748 (10.6) |
| High cholesterol, yes | 7,268 (50.4) | 41,097 (50.7) | 21,941 (54.0) |
| BMId ≥25, yes | 9,065 (65.5) | 53,764 (65.8) | 30,649 (72.8) |
| Diabetes, yes | 2,379 (16.2) | 16,052 (20.6) | 12,828 (30.8) |
|
| |||
| Mental Health, 14+ days when mental health not good | 861 (6.3) | 4,792 (6.0) | 5,292 (12.6) |
|
| |||
| Physical Health, 14+ days when physical health not good | 1,538 (11.4) | 9,971 (12.4) | 12,315 (29.0) |
|
| |||
| High 10-year mortality risk index (risk score ≥8) | 4,408 (30.4) | 30,469 (35.7) | 25,016 (55.9) |
|
| |||
| Fruit and vegetable consumption, ≥5 times/day | 2,678 (16.6) | 13,989 (15.7) | 4,492 (10.1) |
Data presented are unweighted n and weighted percentage. Weighting serves as an adjustment for variation in respondents’ probability of selection, non-coverage and non-response.
Differences between the groups were evaluated using chi-squared tests. All p-values <0.001.
30 participants reported gardening for both their first and second activity and were only included once.
Abbreviations: CVD=cardiovascular disease, BMI=Body Mass Index
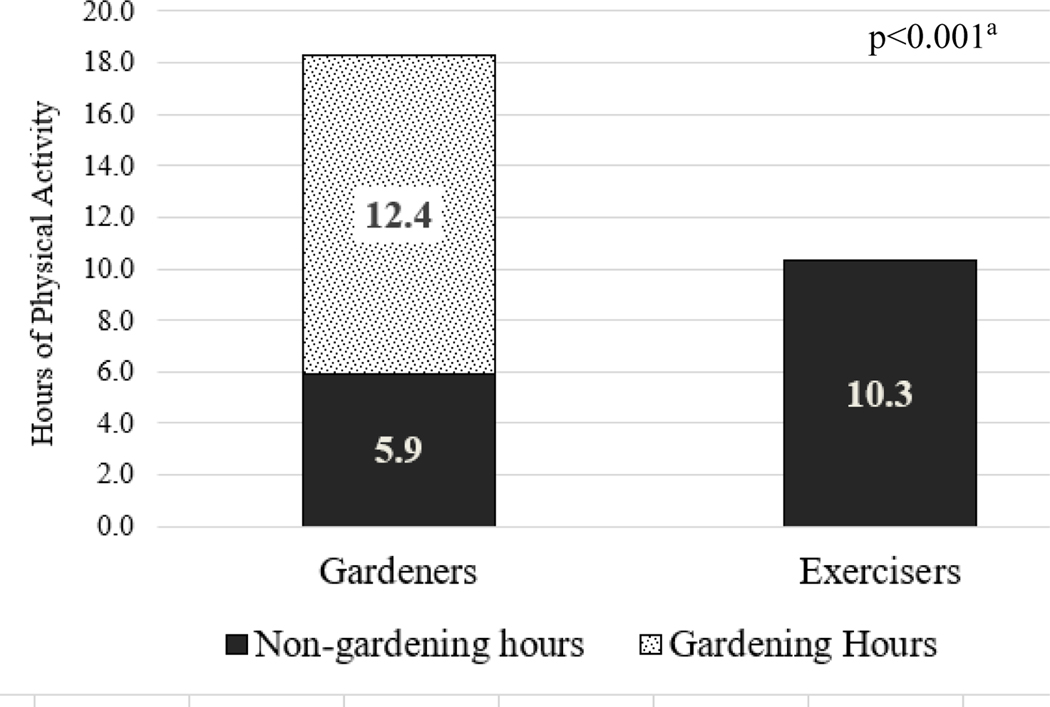
Gardeners reported a significantly greater mean number of hours spent engaged in total PA/week than exercisers (Figure 1). Compared to exercisers, a larger proportion of gardeners met the aerobic PA recommendations (92.7% v. 79.6%, p<0.01). Among gardeners, 75.2% (n=11,208) met the aerobic PA recommendation of 150 minutes/week based on their time spent gardening alone, regardless of the amount of time they spent engaged in non-gardening activities. However, gardeners were less likely to meet strengthening recommendations (28.9% v. 40.6%, p<0.0001) or both aerobic and strengthening recommendations (28.1% v. 35.5%, p<0.0001).
Figure 1.
Hours per week adults aged 65+ spent engaged in gardening or other physical activity by Gardener or Exerciser group
aDifference between the groups for overall hours of exercise was assessed using an independent t-test.
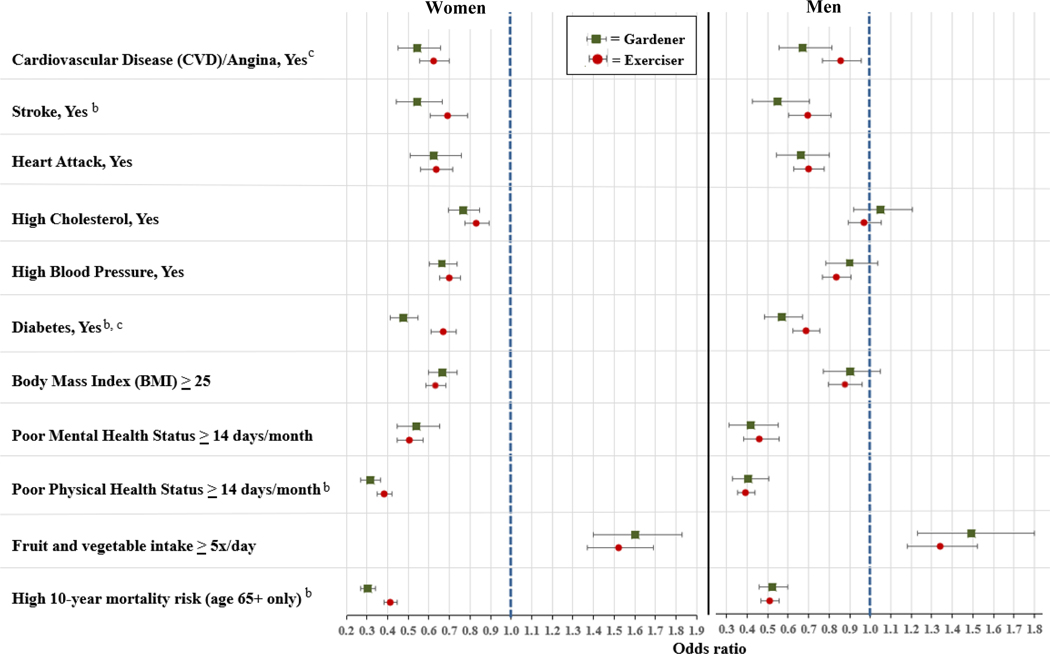
Overall, gardeners, as compared to non-exercisers, had significantly lower odds of reporting all health outcomes and had higher odds of consuming ≥5 F&V/day (CVD aOR 0.60 [95% CI: 0.53–0.68], stroke aOR 0.55 [95% CI: 0.47–0.64], heart attack aOR 0.63 [95% CI: 0.55–0.73], high cholesterol aOR 0.86 [95% CI: 0.79–0.93], high blood pressure aOR 0.74 [95% CI: 0.68–0.81], diabetes aOR 0.51 [95% CI: 0.46–0.56], BMI ≥25 aOR 0.74 [95% CI: 0.68–0.80], poor mental health status aOR 0.50 [95% CI: 0.43–0.59], poor physical health status aOR 0.35 [95% CI: 0.31–0.39], ≥5 F&V per day aOR 1.56 [95% CI: 1.40–1.57], high 10-year mortality risk aOR 0.39 [95% CI: 0.36–0.42]). For the sensitivity analysis to assess gardeners who engaged in <150 minutes of non-gardening exercise, 47.5% (n=7,072/14,903) of the overall sample of gardeners was included. The results revealed no differences in significance for any of the outcomes above with the exception of high cholesterol which was no longer statistically significant for gardeners as compared to non-exercisers (data not shown). For the sensitivity analysis to explore sex-related effect modification, there were significant interactions between sex and group for most health outcomes (pinteraction <0.01) except for diabetes (p=0.06), F&V consumption (p=0.13), heart attack (p=0.11), and physical health status (p=0.17).
Figure 2 presents the aORs and 95% CIs by sex comparing gardeners and exercisers to non-exercisers for outcomes evaluated. Based on results of the contrast analysis where gardeners were compared to exercisers, there were no health-related outcomes where gardeners had significantly higher odds than exercisers. However, female gardeners were significantly less likely than exercisers to report stroke (aOR 0.78 [95% CI: 0.64, 0.96]), diabetes (aOR 0.71 [95% CI: 0.62, 0.82]), poor physical health status (aOR 0.82 [95% CI: 0.70, 0.95]), and high 10-year mortality risk (aOR 0.74 [95% CI: 0.66, 0.83]). Among males, gardeners were significantly less likely than exercisers to report CVD (aOR 0.78 [95% CI: 0.65, 0.94]) and diabetes (aOR 0.83 [95% CI: 0.71, 0.97]). No other significant differences were observed.
Figure 2:
Adjusted odds ratios and 95% Confidence Intervals (95% CI) for self-reported health outcomes, high 10-year mortality risk, and fruit and vegetable intake comparing non-exercisers (referent group) to Exercisers and Gardenersa by sex
aAdjusted for race/ethnicity (non-Hispanic Black, non-Hispanic White, Hispanic, Other), sex (dichotomous: male, female), education level (dichotomous: high school or less, more than high school), and marital status (dichotomous: married or living as married, any other) and non-gardening MET hours. b,cResults of contrast analysis revealed significant differences (p<0.05) between gardeners and exercisers (b=women, c=men).
DISCUSSION
In this large, national sample of US adults aged 65+, compared to non-exercisers, gardeners had better cardiovascular health status and were less likely to report chronic diseases, high 10-year mortality risk, poor mental and physical health status, and they were more likely to consume F&V ≥5 times/day. In addition, both male and female gardeners were significantly less likely to report having diabetes than people who engaged in other exercise. Further, the relationship between gardening and better health status was stronger for women than for men particularly related to CVD, cholesterol, blood pressure, BMI, mental health status, and 10-year mortality risk.
For the most part, these findings are broadly consistent with the larger body of evidence demonstrating a dose relationship between higher amounts of time engaged in PA and better physical health, primary CVD prevention,38 all cause and CVD mortality, incident diabetes, and incident CVD.2,4,25 They are also consistent with observational studies of gardening in smaller samples of older adults.14,15,39 However, this study is the first to compare associations between health outcomes in older adults who garden, those who engage in other physical activities, and those who engage in none. These data suggest the need for further longitudinal or interventional studies to determine whether gardening could be an effective way to reduce CVD-related risk factors and improve the health of older adults.
In this sample, gardening was the second most commonly reported PA in older adults for both men and women. Further, gardeners spent an average of 18 hours/week engaged in PA as compared to exercisers who reported much less time spent (10 hours). Given this long duration of activity, gardeners were more likely than exercisers to meet aerobic activity recommendations (92.7% v. 79.6%) from The Physical Activity Guidelines for Americans. The proportion of gardeners that met both the aerobic and muscle strengthening recommendation (28.9%) was also higher than the national average of 13.3% in this age group.7
These data raise the question as to what motivates gardeners to spend such a large amount of time engaged in this activity. In a large survey of over 6,000 gardeners in the United Kingdom, Chalmin-Pui et al. wanted to understand what motivated gardeners and asked participants to state why they gardened. Of the 19 identified motivations, the most frequently reported was pleasure and enjoyment (from over 50% of participants). “Health benefits” was the third most common reason (among <30% of participants) and was reported with similar frequency as other responses such as “seeing plants/flowers grow,” “expression and self-identity,” and “love the activity.”40 Similarly, other studies have also found that gardeners describe gardening as personally fulfilling, satisfying, calming, and a creative activity which suggests that gardening is a uniquely holistic PA that encompasses aspects of mental, physical, and spiritual wellbeing.14,41,42
From a behavioral theory perspective, Teixeira et al. have suggested that lack of motivation presents a persistent challenge to public health practitioners who are attempting to encourage individuals to meet PA recommendations.43 Based on self-determination theory (SDT), they posit that people are less likely to maintain PA over the long term if they consider it to be something they “have to” do (externally controlled motivation), rather than something they “want to” do (internally controlled motivation). They conclude that intrinsically motivated activities garner feelings of enjoyment, personal accomplishment, and excitement that are able to be sustained over long periods of time.43 The results from the present study, taken together with previous investigations, suggest that while gardening may be considered a physical activity by public health professionals, for gardeners, it is motivated primarily by non-PA-related reasons.40,44,45
Overall, female gardeners were less likely to report being overweight and that both male and female gardeners consumed F&V more frequently than non-exercisers. However, there were no observed differences between gardeners and exercisers in these groups. This could be viewed as in contrast to previous gardening studies that have measured these outcomes.16,27,28 For instance, in a sample of 375 gardeners in Salt Lake City, Utah, Zick et al. found that community gardeners had a significantly lower BMI than their non-gardening siblings, spouses, and neighbors (by a range of 0.60–1.88 kg/m2).16 While the authors did control for age and sex in the analyses, they did not control for other socio-economic characteristics nor did they include any measure of PA. Similar analytical and methodological issues arise when considering dietary intake data. While previous investigators have found a higher F&V intake among gardeners when compared to non-gardeners, none compared gardeners to exercisers or took other PA into account. In addition, each study used brief, self-reported dietary intake measures which introduce measurement error and bias which make it difficult to compare outcomes across studies.27,28
Data from the present study demonstrate that gardening is associated with better outcomes for three critical health problems in older adults: cardiovascular disease risk, diabetes, and mental health.46,47 The findings for diabetes are particularly striking given that the odds of reporting diabetes were lower for gardeners even when compared to those who engage in other exercises. Given that the prevalence of diabetes in older adults is estimated to be near 30%,48 and there is compelling evidence that dietary intake and PA can improve or prevent diabetes, the relationship between gardening and diabetes warrants further exploration.3,5,25,49
In terms of mental health, there are many studies that have used gardening, horticultural therapy, and exposure to nature as an intervention to improve these outcomes.14 In fact, basic exposure to nature such as being present in natural settings, looking at pictures, or inhaling scents from nature has been found to reduce biological markers of inflammation and physiological stress.29 The present study supports previous observations regarding gardening and its association with better mental health.14 However, the BRFSS question included a range of factors including stress, depression, and problems with emotions. Therefore, future studies should assess the association between gardening and specific mental health conditions using formal diagnostic criteria in order to better understand in detail which conditions may be most relevant for gardening.
This study has some limitations. First, the cross-sectional nature of the survey introduces challenges when interpreting the association between gardening and health. For instance, we do not know what kind of gardening the participants engaged in (ornamental, landscape, food), and it is plausible to consider that food gardeners may eat more F&V than other types of gardeners. However, this hypothesis cannot be explored in detail using the current data set.
Second, gardening includes a variety of tasks and this variability presents challenges when comparing gardening to other activities such as walking or running. MET values are a possible proxy for exercise intensity, but due to the large sample size and cross-sectional nature of the data, actual MET values were not directly measured. In the Compendium of Physical Activities, gardening includes a range of activities that each have different METs (e.g., watering =1.5 METs whereas digging/shoveling is 5–7.5 METs).22 However, in the BRFSS dataset, gardening is assigned a single value of 5.0 and this is used to calculate the proportion of adults who meet the PA aerobic guideline. Park et al., conducted direct observations of older adult gardeners engaged in a range of gardening activities in addition to using measured oxygen uptake (VO2) and heart rate values.23 They determined that participants’ gardening physical activity was of moderate intensity and averaged to a MET of 3.8. Therefore, the assumption of a MET of 5.0 in BRFSS may have created some misclassification bias for whether participants met the recommended amount of moderate PA. However, since a MET of 3.8 is still considered moderate intensity PA, the frequency of misclassification is likely to be similar between those classified as meeting and not meeting the recommended amounts of PA.
Third, the health outcomes were all self-reported, and it is possible that those who were more engaged in gardening and exercise were more health conscious, and therefore the observed associations may have been underestimated. Similarly, PA responses were limited to past 30 days so the proportion of adults who garden may be underestimated because gardening is not always possible in all areas of the country (e.g., in February in northern states).
Despite these limitations, a major strength of this analysis is that BRFSS is a large, national sample of US adults and a large group of people who reported being engaged in gardening at the time of the survey was isolated.
Conclusions
Among adults aged 65+, gardening is associated with better CVD health status, lower odds of diabetes, better mental and physical health status, greater fruit and vegetable intake, and lower risk of 10-year mortality. These data suggest that further longitudinal or interventional studies are warranted to explore whether gardening could be employed to improve the health of older adults.
Supplementary Material
Research Snapshot.
Research question:
Among older adults, what is the association between gardening and cardiovascular disease, chronic disease outcomes (e.g., hypertension, hyperlipidemia, diabetes, cardiovascular disease), stroke, heart attack, mental and physical health status, dietary intake, and 10-year mortality risk?
Key findings:
In this national sample of adults aged 65+, gardening was the second most commonly reported physical activity. Gardeners had a better CVD health status than non-exercisers, they were more likely to consume fruits and vegetables ≥5 times/day, and they had lower 10-year mortality risk. These findings suggest the need for further longitudinal or interventional studies to determine whether gardening could be an effective way to reduce CVD-related risk factors and improve the health of older adults.
Funding:
There is no funding to report for this manuscript.
Footnotes
Conflicts to report: The authors have no conflicts to report.
Contributor Information
Susan Veldheer, Penn State College of Medicine, Department of Family and Community Medicine and Department of Public Health Sciences..
Wen-Jan Tuan, Penn State College of Medicine, Department of Family and Community Medicine..
Laila Al-Shaar, Penn State College of Medicine, Department of Public Health Sciences..
Martha Wadsworth, Penn State University, Department of Psychology..
Lawrence Sinoway, Penn State College of Medicine, Department of Medicine..
Kathryn H. Schmitz, Penn State College of Medicine, Department of Public Health Sciences and Department of Physical Medicine and Rehabilitation..
Christopher Sciamanna, Penn State College of Medicine Department of Medicine and Department of Public Health Sciences..
Xiang Gao, Fudan University Department of Nutritional Sciences Department of Nutrition and Food Hygiene and Key Laboratory of Public Health Safety of the Ministry of Education..
References
- 1.Mokdad AH, Ballestros K, Echko M, et al. The State of US Health, 1990–2016: Burden of Diseases, Injuries, and Risk Factors Among US States. JAMA. 2018;319(14):1444–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kyu HH, Bachman VF, Alexander LT, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. Br Med J. 2016;354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lear SA, Hu W, Rangarajan S. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017;390(10113):2626–2626. [DOI] [PubMed] [Google Scholar]
- 4.Sattelmair J, Pertman J, Ding EL, Kohl HW, Haskell W, Lee IM. Dose Response Between Physical Activity and Risk of Coronary Heart Disease A Meta-Analysis. Circulation. 2011;124(7):789–U784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferraro RA, Fischer NM, Xun H, Michos ED. Nutrition and physical activity recommendations from the United States and European cardiovascular guidelines: a comparative review. Curr Opin Cardiol. 2020;35(5):508–516. [DOI] [PubMed] [Google Scholar]
- 6.Lee-Kwan SH, Moore LV, Blanck HM, Harris DM, Galuska D. Disparities in State-Specific Adult Fruit and Vegetable Consumption - United States, 2015. MMWR Morbid Mortal W. 2017;66(45):1241–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Selected Estimates Based on Data from the 2018 National Health Interview Survey. 2018; https://www.cdc.gov/nchs/nhis/releases/released201905.htm#7A. Accessed August 6, 2021.
- 8.Home gardening blooms around the world during coronavirus lockdowns [press release]. Chicago: Reuters; 2020. [Google Scholar]
- 9.Kingsley J, Diekmann L, Egerer MH, Lin BB, Ossola A, Marsh P. Experiences of gardening during the early stages of the COVID-19 pandemic. Health Place. 2022;76:102854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Gardening Association. Garden to Table: A 5-year look at food gardening in America. Williston, VT: Harris Interactive, Inc.; 2014. [Google Scholar]
- 11.American Community Gardening Association. https://www.communitygarden.org/. Accessed May 21, 2020.
- 12.Davis KL, Brann LS. Examining the Benefits and Barriers of Instructional Gardening Programs to Increase Fruit and Vegetable Intake among Preschool-Age Children. J Environ Public Health. 2017;2017:2506864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.George DR, Rovniak LS, Kraschnewski JL, Hanson R, Sciamanna CN. A Growing Opportunity: Community Gardens Affiliated with US Hospitals and Academic Health Centers. Prev Med Rep. 2015;2:35–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soga M, Gaston KJ, Yamaura Y. Gardening is beneficial for health: A meta-analysis. Prev Med Rep. 2017;5:92–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang D, MacMillan T. The benefits of gardening for older adults: a systematic review of the literature. Act Adapt Aging. 2013;37(2):153–181. [Google Scholar]
- 16.Zick CD, Smith KR, Kowaleski-Jones L, Uno C, Merrill BJ. Harvesting more than vegetables: the potential weight control benefits of community gardening. Am J Public Health. 2013;103(6):1110–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weltin AM, Lavin RP. The effect of a community garden on HgA1c in diabetics of Marshallese descent. J Community Health Nurs. 2012;29(1):12–24. [DOI] [PubMed] [Google Scholar]
- 18.Gonzalez MT, Hartig T, Patil GG, Martinsen EW, Kirkevold M. Therapeutic horticulture in clinical depression: a prospective study. Res Theory Nurs Pract. 2009;23(4):312–328. [DOI] [PubMed] [Google Scholar]
- 19.Bail JR, Fruge AD, Cases MG, et al. A home-based mentored vegetable gardening intervention demonstrates feasibility and improvements in physical activity and performance among breast cancer survivors. Cancer. 2018;124(16):3427–3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Demark-Wahnefried W, Cases MG, Cantor AB, et al. Pilot Randomized Controlled Trial of a Home Vegetable Gardening Intervention among Older Cancer Survivors Shows Feasibility, Satisfaction, and Promise in Improving Vegetable and Fruit Consumption, Reassurance of Worth, and the Trajectory of Central Adiposity. J Acad Nutr Diet. 2018;118(4):689–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sommerfeld AJ, Waliczek TM, Zajicek JM. Growing Minds: Evaluating the Effect of Gardening on Quality of Life and Physical Activity Level of Older Adults. Horttechnology. 2010;20(4):705–710. [Google Scholar]
- 22.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: A Second Update of Codes and MET Values. Med Sci Sports Exerc. 2011;43(8):1575–1581. [DOI] [PubMed] [Google Scholar]
- 23.Park SA, Shoemaker C, Haub M. Can older gardeners meet the physical activity recommendation through gardening? Horttechnology. 2008;18(4):639–643. [Google Scholar]
- 24.U. S. Department of Health and Human Services. Physical Activity Guidelines for Americans. 2nd Edition ed2018. [Google Scholar]
- 25.Katzmarzyk PT, Powell KE, Jakicic JM, et al. Sedentary Behavior and Health: Update from the 2018 Physical Activity Guidelines Advisory Committee. Med Sci Sports Exerc. 2019;51(6):1227–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conk SJ, Porter CM. Food Gardeners’ Productivity in Laramie, Wyoming: More Than a Hobby. Am J Public Health. 2016;106(5):854–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Litt JS, Soobader MJ, Turbin MS, Hale JW, Buchenau M, Marshall JA. The influence of social involvement, neighborhood aesthetics, and community garden participation on fruit and vegetable consumption. Am J Public Health. 2011;101(8):1466–1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alaimo K, Packnett E, Miles RA, Kruger DJ. Fruit and vegetable intake among urban community gardeners. J Nutr Educ Behav. 2008;40:94–101. [DOI] [PubMed] [Google Scholar]
- 29.Andersen L, Corazon SSS, Stigsdotter UKK. Nature Exposure and Its Effects on Immune System Functioning: A Systematic Review. Int J Environ Res Public Health. 2021;18(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. The BRFSS Data User Guide. 2013. [Google Scholar]
- 31.Wang DD, Li Y, Bhupathiraju SN, et al. Fruit and Vegetable Intake and Mortality: Results From 2 Prospective Cohort Studies of US Men and Women and a Meta-Analysis of 26 Cohort Studies. Circulation. 2021;143(17):1642–1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sattar N, Forouhi NG. More Evidence for 5-a-Day for Fruit and Vegetables and a Greater Need for Translating Dietary Research Evidence to Practice. Circulation. 2021;143(17):1655–1658. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. Measuring Healthy Days. Atlanta, Georgia: Centers for Disease Control and Prevention; 2000. [Google Scholar]
- 34.Lee SJ, Lindquist K, Segal MR, Covinsky KE. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295(7):801–808. [DOI] [PubMed] [Google Scholar]
- 35.Moss JL, Roy S, Shen C, et al. Geographic Variation in Overscreening for Colorectal, Cervical, and Breast Cancer Among Older Adults. JAMA Netw Open. 2020;3(7):e2011645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cruz M, Covinsky K, Widera EW, Stijacic-Cenzer I, Lee SJ. Predicting 10-year mortality for older adults. JAMA. 2013;309(9):874–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Robinson-Oghogho JN, Thorpe RJ Jr. Garden Access, Race and Vegetable Acquisition among U.S. Adults: Findings from a National Survey. Int J Environ Res Public Health. 2021;18(22). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. J Am Coll Cardiol. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Corley J, Okely JA, Taylor AM, et al. Home garden use during COVID-19: Associations with physical and mental wellbeing in older adults. J Environ Psychol. 2021;73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chalmin-Pui LS, Griffiths A, Roe J, Heaton T, Cameron R. Why garden? - Attitudes and the perceived health benefits of home gardening. Cities. 2021;112. [Google Scholar]
- 41.Clatworthy J, Hinds J,M. Camic P. Gardening as a mental health intervention: a review. Ment Health Rev J. 2013;18(4):214–225. [Google Scholar]
- 42.Howarth M, Brettle A, Hardman M, Maden M. What is the evidence for the impact of gardens and gardening on health and well-being: a scoping review and evidence-based logic model to guide healthcare strategy decision making on the use of gardening approaches as a social prescription. BMJ Open. 2020;10(7):e036923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Teixeira PJ, Carraca EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and self-determination theory: a systematic review. Int J Behavioral Nutr Phys Act. 2012;9:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ramirez-Andreotta MD, Tapper A, Clough D, Carrera JS, Sandhaus S. Understanding the Intrinsic and Extrinsic Motivations Associated with Community Gardening to Improve Environmental Public Health Prevention and Intervention. Int J Environ Res Public Health. 2019;16(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sonti NF, Svendsen ES. Why Garden? Personal and Abiding Motivations for Community Gardening in New York City. Soc Natur Resour. 2018;31(10):1189–1205. [Google Scholar]
- 46.Patnode CD, Redmond N, Iacocca MO, Henninger M. Behavioral Counseling Interventions to Promote a Healthy Diet and Physical Activity for Cardiovascular Disease Prevention in Adults Without Known Cardiovascular Disease Risk Factors: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2022;328(4):375–388. [DOI] [PubMed] [Google Scholar]
- 47.Kastner M, Cardoso R, Lai Y, et al. Effectiveness of interventions for managing multiple high-burden chronic diseases in older adults: a systematic review and meta-analysis. CMAJ. 2018;190(34):E1004–E1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang L, Li X, Wang Z, et al. Trends in Prevalence of Diabetes and Control of Risk Factors in Diabetes Among US Adults, 1999–2018. JAMA. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.