Abstract
Recent decades have seen the remarkable development of China in medical accessibility and quality index, and the application of a number of new advanced cardiovascular technologies benefits more patients. However, according to the Annual Report on Cardiovascular Health and Diseases in China published in this article, which was organized and summarized by National Center for Cardiovascular Diseases, there is still a huge population living with risk factors of cardiovascular diseases (CVD), and the morbidity and mortality of CVD are increasing. It is estimated that there are around 330 million patients suffering from CVD currently, including 245 million of hypertension, 13 million of stroke, 45.3 million of peripheral artery disease, 11.39 million of coronary heart disease (CHD), 8.9 million of heart failure, 5 million of pulmonary heart disease, 4.87 million of atrial fibrillation, 2.5 million of rheumatic heart disease, and 2 million of congenital heart disease. Tobacco use, diet and nutrition factors, physical activity, overweight and obesity, and psychological factors are what affect cardiovascular health, while hypertension, dyslipidemia, diabetes, chronic kidney disease, metabolic syndrome, and air pollution are the risk factors for CVD. In this article, in addition to risk factors for CVD, we also report the epidemiological trends of CVD, including CHD, cerebrovascular disease, arrhythmias, valvular heart disease, congenital heart disease, cardiomyopathy, heart failure, pulmonary vascular disease and venous thromboembolism, and aortic and peripheral artery diseases, as well as the basic research and medical device development in CVD. In a word, China has entered a new stage of transforming from high-speed development focusing on scale growth to high-quality development emphasizing on strategic and key technological development to curb the trend of increasing incidence and mortality of CVD.
Keywords: Epidemiology, Cardiovascular disease, Mortality, Hypertension, Valvular heart disease, Heart failure, Cardiomyopathy
Introduction
In China, there are still a huge population living with risk factors of cardiovascular diseases (CVD), and the morbidity and mortality of CVD are increasing. In order to investigate risk factors influencing cardiovascular health and provide references for health administrators and professionals, each year, China National Center for Cardiovascular Diseases organizes experts in relevant fields to compile the Report on Cardiovascular Health and Diseases in China. In this article, we interpreted key data in the latest published 2022 Report on Cardiovascular Health and Diseases in China.[1]
Factors Affecting Cardiovascular Health
Tobacco use
The 2019 Global Burden of Disease (GBD) study showed that the number of deaths caused by smoking in China increased from 1.5 million in 1990 to 2.4 million in 2019, an increase of 57.9%.[2] China is also the world’s largest consumer of tobacco. According to the 2018 China Adult Tobacco Survey Report, the prevalence of smoking among people aged ≥15 years in China was 26.6%, with over 300 million smokers and approximately 183.5 million smokers suffering from tobacco dependence.[3] The 2021 Global Youth Tobacco Survey (GYTS) showed that the prevalence of experimentation with smoking among secondary school students in China was 16.7%, and the prevalence of smoking was 4.7%, with over a quarter of them being heavy smokers.[4] In 2018, the proportion of second-hand smoke exposure among non-current smokers aged ≥15 years in China was 68.1%. Today, the rate of e-cigarette use is 0.9%, the smoking cessation rate is 20.1%, and the relapse rate is 66.05%.
Diet and nutrition
The dietary and nutritional situation of the Chinese population has generally improved. The 2015–2017 China Nutrition and Health Surveillance data for Chinese residents showed that their average daily caloric intake was 2007.4 kcal per capita, with sufficient availability of the three major classes of nutrients, namely carbohydrates, proteins, and fats.
The total caloric intake of Chinese residents exhibited a decreasing trend, of which protein intake changed little, the proportion of energy supplied by carbohydrates exhibited a significant decreasing trend, and the proportion of energy supplied by fats exhibited an increasing trend, exceeding the upper limit of 20–30% recommended by dietary guidelines since 2012. Between 2015 and 2017, the proportion of energy supplied by fats in rural areas exceeded the recommended upper limit of 30% for the first time, reaching 33.2%.
The intake of major food groups by Chinese residents changed from 1982 to 2015, with a decrease in the intake of grains and vegetables; an increase in the intake of animal-based foods; still-low intakes of fruits, eggs, aquatic products, milk, and soybeans; an increase in the intake of edible oils; and a decrease in the use of salt for home cooking, all of which were well above recommended amounts.
Physical activity
Currently, Chinese residents generally exhibit the characteristics and trends of physical inactivity. In 2017, only 5.12% of primary and secondary school students met the 24-h exercise guideline criteria of ≥60 min/day of moderate-to-vigorous physical activity, ≤2 h/day of screen time, and adequate sleep (9–11 h for 6- to 13-year-olds and 8–10 h for 14- to 17-year-olds). A China Health and Nutrition Survey (CHNS) analysis of 4341 children and adolescents aged 6–17 years revealed that in 2004–2015, the physical inactivity rate of Chinese children and adolescents increased by 5.5%, physical activity decreased by 5.8 metabolic equivalents of task (MET)·h/7 days and the average time spent on sedentary behaviors increased by 1.8 h/7 days.[5]
The China Chronic Disease and Nutrition Surveillance (CCDNS) cross-sectional survey of 298 districts and counties in 31 provinces, autonomous regions, and direct-administered municipalities showed that the rate of regular participation in physical activity among Chinese adults aged ≥18 years was 12.5% in 2015, which is higher than in 2010 (11.9%) but remains at a low level. Except for those aged ≥65 years (10.3%), those aged 25–34 years had the lowest rate of regular physical activity (11.3%). The average duration of sedentary behavior among adults aged ≥18 years in China was 3.2 h/day in 2018, close to that in 2013 (3.3 h/day), and both significantly higher than that in 2010 (2.7 h/day).
Overweight and obesity
Generally, overweight and obesity rates among Chinese residents are trending upward. Based on 2015–2017 China Nutrition and Health Surveillance data, in 2017, the overweight and obesity rates of Chinese children <6 years of age were 6.8% and 3.6%, respectively, and those of children and adolescents aged 6–17 years were 11.1% and 7.9%, respectively. The 2018 China Chronic Disease and Risk Factor Surveillance (CCDRFS) data showed that overweight and obesity rates among Chinese adults aged ≥18 years were 33.3% and 14.1%, respectively.
Overweight and obesity increase the risk of cardiovascular disease (CVD)-related mortality in young and middle-aged adults. Results from the 2003–2008 Guangzhou Biobank Cohort of 19,405 Chinese aged 50 years or older and followed up for an average of 11.5 years showed that after adjusting for potential confounders, there was a 37% increase in CVD-related mortality for every 5 kg/m2 increase in BMI in those with BMI ≥22.5 kg/m2.[6] Data analysis of 48,377 women and 35,989 men aged 40–59 years from two population-based cohort studies (the Shanghai Women’s Health Study and the Shanghai Men’s Health Study) showed that the risk of subsequent CVD-related death in the middle-aged population with a BMI ≥23 kg/m2 was elevated by over 20% for every 5-kg increase in body weight from the onset of adulthood to middle age (men: hazard ratio [HR] = 1.26, 95% confidence interval [CI]: 1.16–1.38; women: HR = 1.23, 95% CI: 1.14–1.33).[7]
Psychological factors
Psychiatric and psychological disorders are increasing annually in China. As of the end of 2017, 5.81 million people with severe psychiatric disorders have been registered nationwide in China. Common psychiatric disorders in patients with CVD include poor emotional state, anxiety and/or depression, panic attacks, and delirium, which are mutually reinforcing and have a causal relationship.
The China Health and Retirement Longitudinal Study (CHARLS) assessed depressive symptoms in 6810 residents without CVD, and found that persistent depressive symptoms were significantly associated with an elevated risk of CVD (relative risk [RR] = 1.77, 95% CI: 1.38–2.26) and mortality (RR = 1.63, 95% CI: 1.01–2.64) compared with study participants without any depressive symptoms. A China Kadoorie Biobank (CKB) analysis of 486,541 Chinese residents aged 30–79 years found that the overall prevalence of major depression was 0.61%. Over a median follow-up period of 7.2 years, patients with major depression had a 32% increased risk of ischemic heart disease (IHD) compared to the general population (HR = 1.32, 95% CI: 1.15–1.53), which was particularly pronounced among urban residents (HR = 1.72, 95% CI: 1.39–2.14).
Risk Factors for Cardiovascular Disease
Hypertension
A nationwide sample from 1958 to 2018 showed an increasing trend in the prevalence of hypertension. The China Hypertension Survey (CHS) found that the crude prevalence of hypertension among Chinese residents aged ≥18 years in 2012–2015 was 27.9%, with a weighted rate of 23.2%. The estimated number of adults with hypertension in China was 245 million. With a crude detection rate of 39.1% and a weighted rate of 41.3%, the number of people with borderline hypertension in China is estimated to be 435 million.[8]
The CHNS study, with a prospective cohort of 12,952 Chinese adults aged >18 years, showed that the age-standardized prevalence of hypertension increased from 40.8/1000 person-years in 1993–1997 to 48.6/1000 person-years in 2011–2015.[9]
The awareness, treatment, and control rates of hypertension were rising among Chinese adults aged ≥18 years, at 51.6%, 45.8%, and 16.8%, respectively in 2015.
Approximately 4% of children in China have persistently elevated blood pressure levels and met the diagnostic criteria for hypertension. The 2012–2015 China Child and Adolescent Cardiovascular Health (CCACH) Survey and a 2018–2019 national survey in six provinces and municipalities showed that despite differences in the prevalence of hypertension at individual time points using different screening criteria in China versus the United States, the overall prevalence of hypertension determined after three consecutive blood pressure measurements on different days were relatively similar (CCACH study: 3.7% vs. 3.3%; national survey of six provinces and municipalities: 8.4% vs. 5.9%).[10]
Dyslipidemia
The prevalence of dyslipidemia among Chinese people aged ≥18 years has increased dramatically, from 18.6% in 2002 to 40.4% in 2012. In the 2012–2015 CHS and the 2014–2019 China Patient-centered Evaluative Assessment of Cardiac Events Million Persons Project (China-PEACE MPP), the prevalence of dyslipidemia in adults aged ≥35 years was 34.7% and 33.8%, respectively. The principal types of dyslipidemia in adults in China are low high-density lipoprotein cholesterol and high triglycerides.
According to the risk stratification definitions of the 10-year atherosclerotic cardiovascular disease (ASCVD) risk assessment process of the 2016 Chinese guidelines for managing dyslipidemia in adults, 10.2% of the China-PEACE MPP study population had a high risk of 10-year ASCVD, with an attainment rate for low-density lipoprotein cholesterol (LDL-C) <2.6 mmol/L of 42.9% and a treatment rate of only 4.5% among those not meeting this standard. Additionally, 3.2% were at very high risk for 10-year ASCVD, with an attainment rate for LDL-C <1.8 mmol/L of 26.6%, a 14.1% treatment rate, and an attainment rate of 44.8% among those meeting the standard for LDL-C treatment.[11]
Diabetes
The prevalence of diabetes in the Chinese population has increased significantly. A 1980 survey of 300,000 individuals found a prevalence of diabetes of 0.67%. Cross-sectional surveys of 75,880 adults aged ≥18 years in 31 provinces, autonomous regions, and direct-administered municipalities in 2015–2017 showed that the prevalence of diabetes based on World Health Organization (WHO) diagnostic criteria was 11.2% (95% CI: 10.5–11.9%).[12] Currently, 129.8 million adults in China are estimated to have diabetes. The detection rate of pre-diabetes was 35.2% (95% CI: 33.5–37.0%).
The Chinese Da Qing Diabetes Prevention Outcome Study of 577 adults with impaired glucose tolerance enrolled from 33 clinics found that at the 30-year follow-up after lifestyle intervention, the intervention group had a delay in the onset of diabetes of 3.96 years, the risks of diabetes, cardiovascular events, composite microvascular events, cardiovascular death, and all-cause death by 39%, 26%, 35%, 33%, and 26%, respectively, and the average life expectancy was increased by 1.44 years compared to the control group.
Chronic kidney disease
From September 2009 to September 2010, the National chronic kidney disease (CKD) prevalence survey of 47,204 adults >18 years of age from 13 provinces, autonomous regions, and direct-administered municipalities showed that the overall prevalence of CKD was 10.8%, accounting for an estimated 120 million patients with CKD in China. The prevalence of abnormal renal function (estimated glomerular filtration rate [eGFR] <60 mL·min–1·1.73 m–2) was 1.7%, and that of albuminuria (urinary albumin/creatinine ratio >30 mg/g) was 9.4%.
Metabolic syndrome
The 2002 and 2010–2012 China Nutrition and Health Surveillance data of Chinese residents included 48,556 and 104,098 survey respondents aged ≥18 years in overall cluster sampling, respectively. According to the diagnostic criteria of the Chinese Diabetes Society of the Chinese Medical Association, the prevalence of metabolic syndrome (MS) increased from 6.6% in 2002 to 15.4% in 2012.
According to the 2010–2012 China Nutrition and Health Surveillance data of Chinese residents, the prevalence of MS among Chinese children and adolescents aged 10–17 years was 2.4% based on the diagnostic criteria established by the Chinese Society of Pediatrics of the Chinese Medical Association. The prevalence of MS was 4.3% based on the Cook criteria.
Air pollution
The 2022 China Ecological Environment Status Bulletin shows that in 2021, 218 of the country’s 339 cities at the prefecture level and above met outdoor air quality standards, with an attainment rate of 64.3%, which was up to 3.5% from 2020. The levels of the six major air pollutants (PM2.5, PM10, SO2, NO2, CO, and O3) were all lower than those in 2020.
During 2000–2016, the number of deaths attributed to PM2.5 pollution in China amounted to 30.8 million. Since 2013, the total number of deaths per year in China due to PM2.5 exposure has gradually decreased.[13]
A study focusing on the economic costs and health benefits of different carbon emission reduction pathways revealed that reducing carbon emissions can prevent approximately 118,000 and 614,000 deaths attributable to PM2.5 in 2030 and 2050, respectively.[14] Studies on the benefits of carbon emission and air quality pollution-prevention policies in China have predicted that the number of PM2.5 and O3-related deaths nationwide will decrease by 235,200 (95% CI: 185,300–292,800) and 53,400 (95% CI: 34,900–67,500) respectively by 2030.
Community Prevention of Cardiovascular Disease
The “Healthy China 2030” initiative calls for “implementing a comprehensive strategy for the prevention and management of chronic diseases and enhancing the construction of demonstration areas for this purpose”. The construction of “demonstration areas” promotes a fundamental shift in CVD prevention and control strategies from high-risk groups to the whole population.
In 2013, Lishan District in Anshan City implemented a demonstration area, and the number of health institutions increased from 73 to 116 (59%) in 2013–2020. CVD risk factors were improved in the Demonstration Area population, with a 15.00% decrease in overweight (36.79% vs. 31.27%), a 40.30% decrease in obesity (16.90% vs. 10.09%), a 35.87% decrease in smoking (30.63% vs. 19.52%), a 50.95% decrease in passive smoking (75.12% vs. 36.85%), a 53.13% decrease in alcohol consumption (32.73% vs. 15.34%). The health behaviors of the population gradually evolved over the 7 years. The use of salt-restriction spoons increased from 3.22% to 15.34%, the use of fat-restriction containers increased from 1.26% to 12.95%, the public demand for knowledge about chronic diseases increased from 48.65% to 65.74%, and the prevalence of hypertension and diabetes mellitus dropped significantly (34.69% vs. 23.51%; 16.76% vs. 8.96%), and the average life expectancy increased by 1.57 years (78.00 vs. 79.57 years).[15]
Cardiovascular Disease
Epidemiological trends of cardiovascular disease
The prevalence of CVD has increased continuously in China. Currently, the projected number of CVD patients is 330 million, of which there are 13 million cases of stroke, 11.39 million cases of coronary heart disease, 8.9 million cases of heart failure, 5 million cases of pulmonary heart disease, 4.87 million cases of atrial fibrillation, 2.5 million cases of rheumatic heart disease, 2 million cases of congenital heart disease, 45.3 million cases of peripheral arterial disease, and 245 million cases of hypertension.
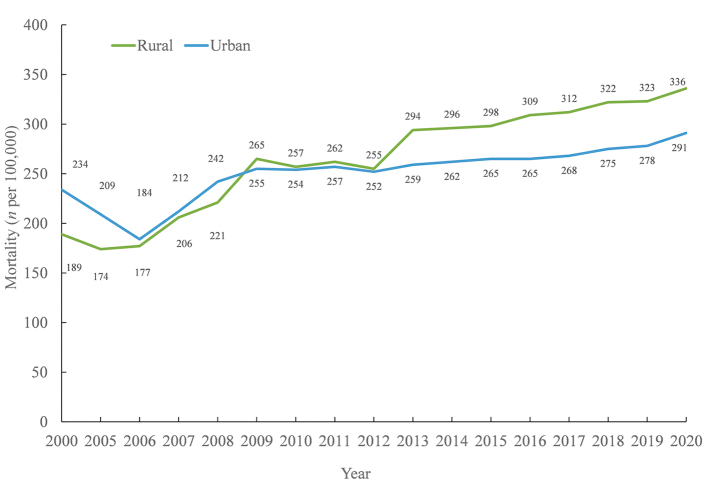
According to the China Health Statistical Yearbook 2021, CVD ranks first in morbidity and mortality rates among urban and rural residents in 2020, surpassing cancer and other diseases. Rural and urban cases of CVD accounted for 48.00% and 45.86% of causes of death, respectively, with two of every five deaths attributed to CVD. Since 2009, rural CVD mortality rates have consistently exceeded urban rates [Figure 1]. In 2020, the rural CVD mortality rate was 336.13/100,000, of which the heart disease mortality rate was 171.36/100,000 and the cerebrovascular disease mortality rate was 164.77/100,000. The urban CVD mortality rate was 291.04/100,000, of which the heart disease mortality rate was 155.86/100,000, and the cerebrovascular disease mortality rate was 135.18/100,000.
Figure 1.
Changes in cardiovascular disease mortality rates among urban and rural residents in China, 2000–2020.
A China National Mortality Surveillance System analysis found that the number of CVD deaths in China increased from 3.09 million in 2005 to 4.58 million in 2020. The age-standardized mortality rate (ASMR) decreased from 286.85/100,000 in 2005 to 245.39/100,000 in 2020. The burden of premature CVD mortality in China decreased by 19.27% in 2020 compared to 2005. IHD, hemorrhagic stroke, and ischemic stroke are the three leading causes of CVD-related death in China.
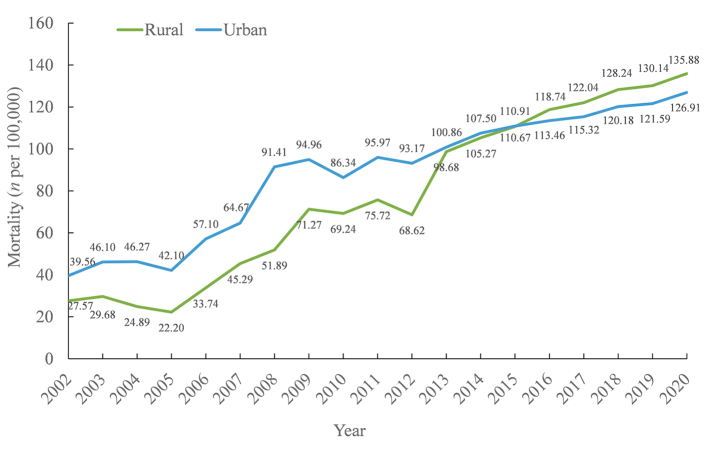
Coronary heart disease
Coronary heart disease mortality exhibited a continuous upward trend from 2012 to 2020, with a marked increase in rural areas, surpassing urban levels by 2016 [Figure 2]. In 2020, coronary heart disease-related mortality was higher in men than in women in both urban and rural areas (129.92/100,000 vs. 123.80/100,000; 140.06/100,000 vs. 131.56/100,000).
Figure 2.
Coronary heart disease mortality in urban and rural areas of China, 2002–2020.
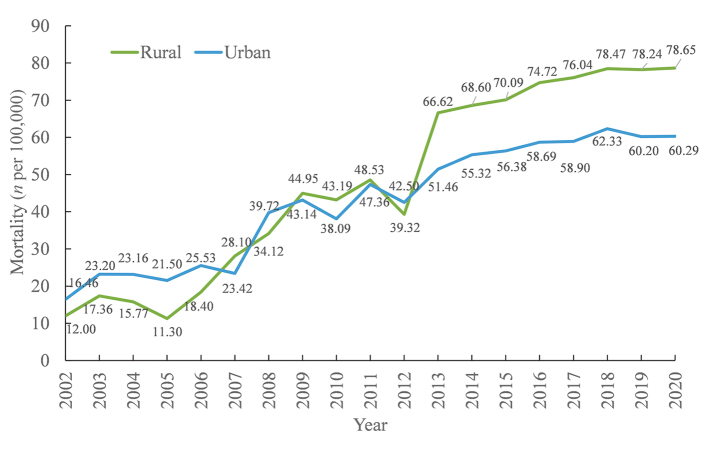
Acute myocardial infarction (AMI) mortality rates generally increased in 2002–2020 [Figure 3].
Figure 3.
Acute myocardial infarction mortality in urban and rural areas of China, 2002–2020.
A study using data from the China Acute Myocardial Infarction (CAMI) study evaluated the benefit of late percutaneous coronary intervention (PCI) of the infarct-related coronary artery in patients with ST-segment elevation myocardial infarction at 12 h after onset. The results showed a significant reduction in the 2-year incidence of major adverse cardiovascular and cerebrovascular events (MACCE), all-cause mortality, myocardial infarction, stroke, and vascular remodeling in patients with PCI interventions compared with medication-based therapy. Subgroup analyses consistently showed PCI to be superior to medication-based therapy. Additionally, at the 2-year follow-up, left ventricular ejection fraction (LVEF) had increased in the PCI group, whereas it did not improve significantly in the medication-based therapy group. Late PCI is common in Chinese clinical practice and is associated with significant improvements in cardiac function and survival compared with medication-based therapy alone.[16]
In 2021, the total number of registered coronary intervention cases in Chinese mainland was 1,164,117 (excluding cases at military hospitals), with a 20.18% increase from 2020. In 2021, the average number of stents/drug-coated balloons was 1.48. The utilization shares of drug-coated balloons in 2019, 2020, and 2021 were 6.4%, 10.9%, and 15.0%, respectively, indicating continuous increase. Surgical mortality was unchanged from 2020 to 2021 at 0.38% and has maintained a low level since 2009.
A study investigated changes in the quality of coronary artery bypass grafting (CABG) in hospitals across China several years after implementing nationally registered quality improvement measures. This cohort study analyzed data from 66,971 patients with CABG alone in 74 tertiary hospitals in China between January 2013 and December 2018. The CABG in-hospital mortality rate was found to have decreased from 0.9% in 2013 to 0.6% in 2018. The interhospital heterogeneity in patient outcomes after CABG has been significantly reduced, and the prevalence of adherence to guideline recommendations on evidence-based surgical processes and secondary prevention progressively increased.[17]
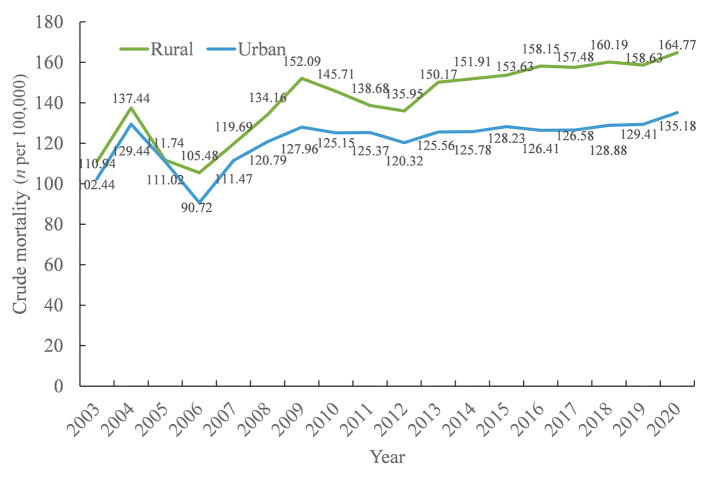
Cerebrovascular disease
There is an overall increasing trend in (crude) cerebrovascular disease mortality from 2003 to 2020 [Figure 4]. According to the China Health Statistics Yearbook 2021, cerebrovascular disease accounted for 21.30% of all urban deaths in 2020, ranking 3rd leading cause of death among urban residents. Among rural residents, cerebrovascular disease deaths accounted for 23.53% of all deaths, ranking 2nd leading cause of death in rural areas. The (crude) cerebrovascular disease mortality rate is higher among Chinese men than among Chinese women in both urban and rural areas (149.87/100,000 vs. 120.02/100,000; 182.00/100,000 vs. 147.00/100,000).
Figure 4.
Cerebrovascular disease mortality rates in urban and rural areas of China, 2003–2020.
GBD 2019 data showed that the age-standardized incidence of stroke in China in 2019 was 200/100,000, with 144/100,000 cases of ischemic stroke, 44/100,000 cases of hemorrhagic stroke, and 11/100,000 cases of subarachnoid hemorrhage. Compared to those in 1990, the age-standardized incidence of stroke decreased by 9.0%, with the incidence of ischemic stroke increasing by 35.0% and the incidences of hemorrhagic stroke and subarachnoid hemorrhage decreasing by 53.0% and 39.0%, respectively.
Based on the GBD 2019 results, the age-standardized prevalence of stroke in China in 2019 was 1468.9/100,000, with 1255.9/100,000 ischemic strokes, 214.6/100,000 hemorrhagic strokes, and 81.4/100,000 subarachnoid hemorrhages. Compared with those in 1990, the age-standardized prevalence of stroke increased by 13.2%, with ischemic stroke increasing by 33.5% and hemorrhagic stroke and subarachnoid hemorrhage decreasing by 31.9% and 21.9%, respectively.
GBD 2019 data showed that the age-standardized disability adjusted life year (DALY) rate for stroke in China in 2019 was 2412.5/100,000, a significant decrease of 41.6% from the rate in 1990. The age-standardized years of life lost (YLL) decreased by 45.7%, but the age-standardized years lived with disability (YLD) rate increased by 15.9%.[18]
Arrhythmias
A stratified, multi-stage study of 114,039 residents in 22 provinces, autonomous regions, and direct-administered municipalities found that, from 2020 to 2021, the prevalence of atrial fibrillation (AF) among Chinese residents aged ≥18 years was 1.6%, with higher prevalence in males (1.7%) than in females (1.4%), in rural areas (1.7%) than in urban areas (1.6%), and in the central region (2.5%) than in the western (1.5%) and eastern regions (1.1%).[19]
According to National Health Commission online registration system statistics and data reported by provincial quality control centers, there were 99,306 cases of pacemaker placement nationwide in 2021, an increase of 15.2% from 2020.
Data from National Arrhythmia Intervention Quality Control Center show that the number of radiofrequency catheter ablation (RFCA) procedures has grown rapidly nationwide from 2009 to 2021, with an annual growth rate of 13.2–17.5%. In 2021, 210,609 patients who underwent catheter ablation were included in the direct reporting system for interventional treatment of arrhythmia in China. Among them, the proportion of RFCA for AF among all RFCA procedures has increased annually, at 31.9%, 33.0%, 32.2%, and 46.4% from 2018 to 2021, respectively.
In 2021, the direct reporting system for interventional treatment of arrhythmia included 6547 patients with ICD placement, a 36% increase from 2020, with 2876 (44%) cases of dual-chamber implantable cardioverter defibrillators (ICDs).
Valvular heart disease
Between 2012 and 2015, a study conducted stratified multi-stage random sampling of 31,499 residents aged ≥35 years who underwent echocardiography examination identified that 1309 had valvular heart disease. This resulted in a weighted prevalence of valvular heart disease of 3.8%, equating to an estimated 25 million cases in China.[20] Rheumatic valvular disease remains the leading cause of valvular heart disease in China, while the prevalence of degenerative valve disease has increased significantly in recent years. Among patients with valvular heart disease in China, 55.1% had rheumatic valvular disease, and 21.3% had degenerative valve disease. The incidence of rheumatic valvular disease tended to decrease with increasing age, whereas the incidence of degenerative valve disease tended to increase, but the prevalence of rheumatic valvular disease remained higher in the elderly population than in the younger population.
Congenital heart disease
According to the China Statistical Yearbook 2021, the mortality rate of congenital heart disease in rural areas of China in 2020 was higher than in urban areas (0.76/100,000 vs. 0.61/100,000), with no significant difference between genders.
In 2021, 728 hospitals nationwide (including Hong Kong, China) performed 71,693 surgeries for congenital heart diseases, accounting for 25.8% of all cardiac and aortic surgical procedures; this percentage has decreased to a minimum in recent years. In 2021, the number of cardiac surgeries for in-patients aged <18 years was 41,985, accounting for 58.6% of all congenital heart diseases, a decrease of 1.5% from 2020. This suggests that corrective surgery for adult congenital heart diseases continues to constitute a high proportion of all surgeries in China and is increasing annually.
According to data from the National Center for Cardiovascular Quality Improvement, 36,528 patients underwent interventions for congenital heart disease in China in 2020. The overall rate of discharge by medical advice was 97.1%, the in-hospital mortality rate was 0.5%, and the discharge-against-medical-advice rate was 0.8%. The 30-day readmission rate (1.1%) did not change significantly between 2018 (1.0%) and 2019 (1.3%).
Cardiomyopathy
A stratified cluster survey of 8080 residents in nine provinces and cities (districts) in China between October 2001 and February 2002 showed that the crude prevalence of hypertrophic cardiomyopathy (HCM) in the population was 0.16%, with a higher prevalence in men (0.22%) than in women (0.10%), and age- and gender-corrected prevalence of 80/100,000 accounting for an estimate of over 1 million cases of HCM in Chinese adults.[21] The prevalence of dilated cardiomyopathy (DCM) was 19/100,000.
A 2022 article published by Nature Publishing Group systematically describes the metabolic profiles and altered characteristics of myocardial tissue and plasma in HCM, thus elucidating its regulatory mechanisms and providing potential intervention targets. This study provides a deeper understanding of the molecular pathological features of HCM, promotes the development of rational therapies, and provides a theoretical foundation for precision therapy.[22]
Heart failure
The CHS analysis of 22,158 residents in 2012–2015 showed a prevalence of 1.3% for heart failure, 1.4% for left ventricular systolic dysfunction (LVEF <50%), and 2.7% for moderate/severe diastolic dysfunction among Chinese adults aged ≥35 years.
According to data from China’s heart transplant registry, 738 heart transplants were performed in 66 heart transplant-qualified medical institutions in China in 2021. Non-ischemic cardiomyopathy accounted for 75.2% of patients who received heart transplants. In 2021, the in-hospital survival rate for heart transplant recipients in China was 91.0%, with multi-organ failure and transplant heart failure responsible for early death in approximately 40% of cases. In 2015–2021, the national 1-year survival rate after heart transplant was 85.4%, and the 3-year survival rate was 79.9%.
Pulmonary vascular disease and venous thromboembolism
The results from the largest national multicenter prospective registry study of pulmonary arterial hypertension (PAH) show that congenital heart disease is the predominant cause of PAH in China. The study included 2031 patients diagnosed with PAH by right heart catheterization at 34 tertiary medical centers in 31 provinces, autonomous regions, and directly administered municipalities between August 2009 and December 2019. The patients had a mean age of 35 ± 12 years, with 76.2% being female and 45.2% having congenital heart disease-associated PAH (PAH-CHD). Other PAH types included idiopathic PAH (IPAH) (38.8%), connective tissue disease-associated PAH (PAH-CTD) (13.1%), and other subtypes (3.0%). The survival rate for PAH patients at 1, 3, 5, and 10 years were 95.6%, 87.6%, 79.2%, and 63.2%, respectively. The outcomes of PAH-CHD patients were better than those of IPAH and PAH-CTD patients.[23]
A registry study in Hong Kong (China) of 2214 newly diagnosed hospitalized patients with venous thromboembolism (VTE) between January 2004 and December 2016 included 1444 (65.2%) patients with deep vein thrombosis (DVT) and 770 (34.8%) patients with pulmonary embolism (PE). Over the 13-year period, the incidence of VTE increased from 28.1 per 100,000 person-years in 2004 to 48.3 per 100,000 person-years in 2016. Active cancer is the principal etiology of VTE, increasing from 34.8% in 2005 to 60.9% in 2014.[24]
A Chinese VTE hospitalization and mortality study included 105,723 patients with VTE in 90 hospitals between 2007 and 2016, of which 41.2% presented with PE, with or without DVT, and 58.8% had DVT alone. The age- and gender-adjusted hospitalization rate increased from 3.2/100,000 in 2007 to 17.5/100,000 in 2016, the in-hospital mortality rate decreased from 4.7% to 2.1%, and the length of hospital stay decreased from 14 days to 11 days. This study showed that the hospitalization rate of VTE in China increased over a decade. However, the in-hospital mortality rate decreased annually, and the length of hospital stay continued to shorten, suggesting the rising incidence of VTE in China, alongside significant improvement in diagnostic awareness and treatment.
Aortic and peripheral arterial diseases
Aortic disease
Health insurance data for over 300 million urban residents from 2015–2016 showed that the annual incidence of acute aortic dissection in Chinese mainland was 2.78 per 100,000 person-years, and the incidence in men was significantly higher than that in women (3.96 per 100,000 person-years vs. 1.59 per 100,000 person-years).
Hospital Quality Monitoring System (HQMS) data show that the number of both endoluminal and open surgery procedures for aortic disease in China has been increasing in recent years, with the number of endoluminal aortic surgery procedures in HQMS-enrolled hospitals increasing from 21,320 in 2017 to 46,651 in 2021 (an increase of 118.8%), the number of Bentall procedures increasing from 3105 to 5901 (an increase of 90.0%), and the number of total arch replacements from 3707 to 9400 (an increase of 153.6%).
During 2017–2021, the in-hospital mortality rate for thoracic endoluminal aortic repair in HQMS-enrolled hospitals decreased from 2.0% to 1.3%, and the in-hospital mortality and discharge-against-medical-advice rates decreased from 4.9% to 4%. The in-hospital mortality rate for abdominal endoluminal aortic repair decreased from 1.7% to 1.3%, and the in-hospital mortality and discharge-against-medical-advice rates were 3.7–3.9%. The in-hospital mortality rate for the Bentall procedure was 1.5–1.9%, and the in-hospital mortality and discharge-against-medical-advice rates decreased from 4.4% to 2.5%. The in-hospital mortality rate for total arch replacement was 5.9–7.4%, and the in-hospital mortality and discharge-against-medical-advice rates were 11.2–14.6%.
Peripheral arterial disease
Lower extremity arterial disease (LEAD). A stratified random sample study in China showed that the prevalence of LEAD among adults aged ≥35 years was 6.6%, and it was hypothesized that there were approximately 45.3 million cases of LEAD in China. The prevalence of asymptomatic LEAD in the Chinese population is approximately 95%. The principal risk factors for LEAD are smoking, hypertension, hypercholesterolemia, and type 2 diabetes mellitus (T2DM).
Carotid atherosclerotic disease (CASD). A 2017–2019 cross-sectional study in the health management centers of two tertiary hospitals in North and South China enrolled a total of 38,642 participants with a median age of 46 years and a prevalence of CASD of 30.0%.[25] According to the Report on Stroke Prevention and Treatment in China, 2020, 6600 cases of carotid endarterectomy were reported in 2019, and carotid stenting was performed in 18,649 cases.[26]
Subclavian artery stenosis (SCAS). An inter-arm systolic blood pressure difference of ≥15 mmHg is a predictor of SCAS >50%. A study of 3133 individuals aged ≥60 years in Shanghai communities found that 1.8% of individuals had an inter-arm systolic blood pressure difference of ≥15 mmHg. A single-center in-patient etiologic composition study showed that atherosclerosis accounted for 95.9% of SCAS patients aged >40 years, and arteritis accounted for 90.5% of patients aged ≤40 years.
Mesenteric artery disease (MAD). Epidemiological data on MAD is lacking, but acute or chronic MAD has been identified as underdiagnosed in clinic, with correspondingly high rates of misdiagnosis and mortality. A meta-analysis of case reports of mesenteric artery embolism and thrombosis in 1994–2006 found a misdiagnosis rate of 61.3% and a mortality rate of 60.6% among 111 confirmed cases. Another meta-analysis of cases of misdiagnosis of bowel ischemia in 1998–2008 found a misdiagnosis rate of 63.4% (312/492 cases).
Renal artery stenosis (RAS). The prevalence of RAS is often underestimated, with a detection rate of 16.3% when coronary angiography and renal angiography are performed concurrently. A single-center study of 2905 consecutive patients with RAS over 18 years found that the principal causes of RAS in the Chinese population were atherosclerosis (82.4%), arteritis (11.9%), and fibromuscular dysplasia (4.3%). The prevalence of atherosclerosis increased from 50% in 1999–2000 to 85% in 2015–2016. Etiologies unrelated to atherosclerosis were more common among patients aged ≤40 years.
Cardiovascular Rehabilitation
Cardiac rehabilitation
A 2016 survey on the current status of cardiac rehabilitation in hospitals across China included 124 tertiary hospitals in seven geographic regions of Chinese mainland. The results showed that only 30 hospitals (24%) provided cardiac rehabilitation services, with an average of 2.2 hospitals providing cardiac rehabilitation for a population of 100 million. Of the 13 hospitals that completed the 36-item survey and conducted cardiac rehabilitation, 3 (23%) conducted in-hospital phase I rehabilitation, 3 (23%) conducted phase II rehabilitation, and 7 (54%) conducted both phase I and phase II rehabilitation.
Stroke rehabilitation
The number of rehabilitation beds in Chinese medical institutions continues to grow. In 2020, there were 246,907 rehabilitation beds in hospitals across China. The top five provinces in number of rehabilitation beds were Jiangsu, Zhejiang, Henan, Shandong, and Guangdong.
Early rehabilitation helps to improve neurological function in patients with acute ischemic stroke or cerebral hemorrhage. Ischemic stroke patients who underwent rehabilitation 24–48 h or 72 h after onset had significantly higher Fugl-Meyer Assessment of Motor Recovery after Stroke scores than those who underwent rehabilitation 72–96 h or 72 h–7 days after onset. A study that included 82 patients with cerebral hemorrhage showed that early intervention and training starting 2–7 days after onset facilitated the improvement of motor function, neurological function, and activities of daily living in patients with cerebral hemorrhage than rehabilitation training 3–4 weeks after onset.
Basic Research in Cardiovascular Diseases and Medical Device Development
Basic research in cardiovascular diseases
Overall, 74 high-level basic research articles with both corresponding and lead authors from Chinese mainland were published between August 2021 and August 2022 and focused on investigating the cardiac anatomy, development, function, and pathogenesis of the cardiovascular system, including AMI, heart failure, ischemia-reperfusion injury, cardiomyopathy, cardiac remodeling, cardiac arrhythmia, aneurysm/dissection, atherosclerosis, and vascular remodeling. Some popular research topics include cardioprotective agents, regeneration, single-cell sequencing technology, and gene therapy.
Development of cardiovascular medical devices and other products
From September 1, 2021, to August 5, 2022, the State Food and Drug Administration approved 59 medical devices through the innovative medical device review channel, of which 26 (44.1%) were cardiovascular products, indicating that innovation in cardiovascular medicine dominates the field of medical device innovation in China.
From September 1, 2021, to August 5, 2022, the State Food and Drug Administration approved 189 registration certificates for three types of cardiovascular medical devices based on risk levels, with 130 being domestic products. Among which, four products were approved through the National innovative medical device review channel. Of these 130 domestic products, 115 are interventional, three are related to imaging, seven are blood flow measurement systems, two are open surgery techniques, one is an artificial intelligence (AI) software, and two are diagnostics.
Economic Burden of Cardiovascular Diseases
In 2020, 24,288,300 patients with cardiovascular and cerebrovascular diseases were discharged from Chinese hospitals, accounting for 14.68% of all discharges over the same period. Of these, 12,899,400 patients had been admitted for cardiovascular diseases (7.80%), and 11,388,900 were admitted for cerebrovascular diseases (6.89%).
The discharged patients with CVD were mostly patients with IHD (7,989,900, of which 2,806,500 were cases of angina pectoris and 1,501,100 were cases of AMI) and cerebral infarction (7,610,200), at 32.90% and 31.33% respectively. In 2020, 4,073,900 patients with diabetes were discharged.
The total hospitalization cost for cardiovascular disease in 2020 was RMB 270.901 billion Yuan. Specifically, the total hospitalization cost for cardiovascular diseases amounted to RMB 165.222 billion Yuan, including RMB 116.959 billion Yuan for IHD (of which RMB 43.135 billion Yuan was for angina pectoris and RMB 34.685 billion Yuan for AMI), RMB 17.082 billion Yuan for cardiac arrhythmia, RMB 14.461 billion Yuan for heart failure, RMB 13.260 billion Yuan for hypertension (RMB 2.496 billion Yuan was for hypertensive heart disease and kidney disease), RMB 1.849 billion Yuan for pulmonary embolism, RMB 1.520 billion Yuan for chronic rheumatic heart disease, and RMB 91 million Yuan for acute rheumatic fever. The total hospitalization cost for cerebrovascular diseases was RMB 105.679 billion Yuan, including RMB 74.770 billion Yuan for cerebral infarction, RMB 30.909 billion Yuan for cerebral hemorrhage; additionally, the cost was RMB 31.641 billion Yuan for diabetes mellitus.
In a word, China has entered a new stage of transforming from high-speed development focusing on scale growth to high-quality development emphasizing on strategic and key technological development to curb the trend of increasing incidence and mortality of CVD.
Acknowledgements
Thanks for all experts participated in compiling the 2022 Report on Cardiovascular Health and Diseases in China. All experts are listed in the Reference[1].
Conflicts of interest
None.
Footnotes
How to cite this article: Wang ZW, Ma LY, Liu MB, Fan J, Hu SS; on behalf of The Writing Committee of the Report on Cardiovascular Health and Diseases in China. Summary of the 2022 report on cardiovascular health and diseases in China. Chin Med J 2023;136:2899–2908. doi: 10.1097/CM9.0000000000002927
References
- 1.National Center for Cardiovascular Diseases . 2022 Report on Cardiovascular Health and Diseases in China (in Chinese). Beijing: Peking Union Medical College Press, 2023. [Google Scholar]
- 2.Reitsma MB Kendrick PJ Ababneh E Abbafati C Abbasi-Kangevari M Abdoli A, et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet 2021;397:2337–2360. doi: 10.1016/S0140-6736(21)01169-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu Z Li YH Cui ZY Li L Nie XQ Yu CD, et al. Prevalence of tobacco dependence and associated factors in China: findings from nationwide China Health Literacy Survey during 2018-19. Lancet Reg Health West Pac 2022;24:100464. doi: 10.1016/j.lanwpc.2022.100464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zeng X, Di X, Liu S, Xie H, Meng Z, Xiao L. Smoking behavior among secondary school students- China, 2021. China CDC Wkly 2022;4:441–447. doi: 10.46234/ccdcw2022.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang X, Leung AW, Jago R, Yu SC, Zhao WH. Physical activity and sedentary behaviors among chinese children: recent trends and correlates. Biomed Environ Sci 2021;34:425–438. doi: 10.3967/bes2021.059. [DOI] [PubMed] [Google Scholar]
- 6.Jiang CQ Xu L Zhang WS Jin YL Zhu F Cheng KK, et al. Adiposity and mortality in older Chinese: an 11-year follow-up of the Guangzhou Biobank Cohort Study. Sci Rep 2020;10:1924. doi: 10.1038/s41598-020-58633-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jia G Shu XO Liu Y Li HL Cai H Gao J, et al. Association of adult weight gain with major health outcomes among middle-aged Chinese persons with low body weight in early adulthood. JAMA Netw Open 2019;2:e1917371. doi: 10.1001/jamanetworkopen.2019.17371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Z Chen Z Zhang L Wang X Hao G Zhang Z, et al. ; China Hypertension Survey Investigators . Status of Hypertension in China: results From the China Hypertension Survey, 2012–2015. Circulation 2018;137:2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 9.Luo Y, Xia F, Yu X, Li P, Huang W, Zhang W. Long-term trends and regional variations of hypertension incidence in China: a prospective cohort study from the China Health and Nutrition Survey, 1991–2015. BMJ Open 2021;11:e042053. doi: 10.1136/bmjopen-2020-042053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu K Li C Gong H Guo Y Hou B Chen L, et al. Prevalence and risk factors for hypertension in adolescents aged 12 to 17 years: a school-based study in China. Hypertension 2021;78:1577–1585. doi: 10.1161/HYPERTENSIONAHA.121.17300. [DOI] [PubMed] [Google Scholar]
- 11.Teng H Gao Y Wu C Zhang H Zheng X Lu J, et al. Prevalence and patient characteristics of familial hypercholesterolemia in a Chinese population aged 35–75 years: results from China PEACE Million Persons Project. Atherosclerosis 2022;350:58–64. doi: 10.1016/j.atherosclerosis.2022.03.027. [DOI] [PubMed] [Google Scholar]
- 12.Li Y Teng D Shi X Qin G Qin Y Quan H, et al. Prevalence of diabetes recorded in China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ 2020;369:m997. doi: 10.1136/bmj.m997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liang F Xiao Q Huang K Yang X Liu F Li J, et al. The 17-y spatiotemporal trend of PM2.5 and its mortality burden in China. Proc Natl Acad Sci U S A 2020;117:25601–25608. doi: 10.1073/pnas.1919641117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tang R Zhao J Liu Y Huang X Zhang Y Zhou D, et al. Air quality and health co-benefits of China’s carbon dioxide emissions peaking before 2030. Nat Commun 2022;13:1008. doi: 10.1038/s41467-022-28672-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang WW, Wang LJ. Evaluation of the effectiveness of the construction of a model area for comprehensive prevention and control of chronic diseases in Lishan District, Anshan City from 2013 to 2020 (in Chinese). Preventive Medicine Tribune, 2022,28:81–83. [Google Scholar]
- 16.Hu M Peng Y Gao X Yang J Xu H Wu Y, et al. Coronary intervention in ST-segment elevation myocardial infarction patients with symptom onset >12 hours: data from China Acute Myocardial Infarction Registry. Angiology 2023;74:171–180. doi: 10.1177/00033197221098885. [DOI] [PubMed] [Google Scholar]
- 17.Li X Gu D Wang X Diao X Chen S Ma H, et al. Trends of coronary artery bypass grafting performance in a cohort of hospitals in China between 2013 and 2018. Circ Cardiovasc Qual Outcomes 2021;14:e007025. doi: 10.1161/CIRCOUTCOMES.120.007025. [DOI] [PubMed] [Google Scholar]
- 18.Ma Q Li R Wang L Yin P Wang Y Yan C, et al. Temporal trend and attributable risk factors of stroke burden in China, 1990-2019: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2021;6:e897–e906. doi: 10.1016/S2468-2667(21)00228-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shi S Tang Y Zhao Q Yan H Yu B Zheng Q, et al. Prevalence and risk of atrial fibrillation in China: a national cross-sectional epidemiological study. Lancet Reg Health West Pac 2022;23:100439. doi: 10.1016/j.lanwpc.2022.100439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang Y Wang Z Chen Z Wang X Zhang L Li S, et al. Current status and etiology of valvular heart disease in China: a population-based survey. BMC Cardiovasc Disord 2021;21:339. doi: 10.1186/s12872-021-02154-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zou Y Song L Wang Z Ma A Liu T Gu H, et al. Prevalence of idiopathic hypertrophic cardiomyopathy in China: a population-based echocardiographic analysis of 8080 adults. Am J Med 2004;116:14–18. doi: 10.1016/j.amjmed.2003.05.009. [DOI] [PubMed] [Google Scholar]
- 22.Wang W Wang J Yao K, et al. Metabolic characterization of hypertrophic cardiomyopathy in human heart. Nat Cardiovasc Res 2022;1:445–461. doi: 10.1038/s44161-0022-00057-1. [DOI] [PubMed] [Google Scholar]
- 23.Quan R Zhang G Yu Z Zhang C Yang Z Tian H, et al. Characteristics, goal-oriented treatments and survival of pulmonary arterial hypertension in China: insights from a national multicentre prospective registry. Respirology 2022;27:517–528. doi: 10.1111/resp.14247. [DOI] [PubMed] [Google Scholar]
- 24.Huang D Chan PH She HL Wong CK Ho CW Cheng YY, et al. Secular trends and etiologies of venous thromboembolism in Chinese from 2004 to 2016. Thromb Res 2018;166:80–85. doi: 10.1016/j.thromres.2018.04.021. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y Li L Li Y Liu M Gan G Zhou Y, et al. The impact of dietary diversity, lifestyle, and blood lipids on carotid atherosclerosis: a cross-sectional study. Nutrients 2022;14:815. doi:10.3390/nu14040815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Writing Group of the Chinese Stroke Prevention and Treatment Report 2020 . Summary of the Chinese Stroke Prevention and Treatment Report 2020 (in Chinese). Chin J Cerebrovasc Disease 2022;19:136–144. [Google Scholar]