Abstract
Background:
When transplanting skin grafts, a compressive dressing is usually used to hold the skin graft in place. Dressing fixation can be achieved with either sutures or staples. The purpose of this study was to compare sutures and staples as a method of fixation for the compressive dressings of the nipple-areola complex (NAC) grafts, during double incision chest contouring surgery in assigned-female-at-birth persons with diagnosis of gender dysphoria. The two methods of fixation were compared according to pain at removal, time consumption, difficulty of removal, costs, and sustainability.
Methods:
Forty patients were randomized to dressing fixation with either sutures or staples. Timing for dressing fixation during surgery and removing the dressing was measured. Pain during removal was measured using vNRS-11. Difficulty of removal was measured with VAS-100. Costs of materials were compared.
Results:
All NAC grafts survived, and no complications such as infection or bleeding occurred. Staples were significantly more painful to remove when compared to sutures [mean vNRS-11 2.98 (SD ± 2.43) versus 1.25 (SD ± 0.92), P < 0.001]. Fixation with staples was faster than fixation with sutures (5.3 versus 94.6 s). No difference in removal time was found. Nurses found staples easier to remove. Sutures were slightly less costly (18 SEK) compared to staples (30 SEK). Finally, sutures produce less material waste.
Conclusion:
Being that all other outcomes are similar or insignificant, the less-pain experienced at removal of sutures makes this the preferable method for fixation of the compressive dressing for NAC grafts during double incision chest contouring surgery.
Takeaways
Question: Is there a difference between sutures and staples with regards to pain, speed, complexity of removal, and cost when used to fixate compressive dressings during double incision mastectomy in trans men?
Findings: A study of 40 trans men undergoing double incision mastectomy was randomized to either sutures or staples for fixating the compressive dressings. Staples are significantly more painful to remove and slightly more expensive, but faster to apply than sutures.
Meaning: We suggest using sutures for fixating compressive dressings in double incision mastectomy.
INTRODUCTION
When transplanting skin grafts in plastic surgery procedures, a compressive dressing is usually used to hold the skin grafts in place. The compressive dressings are fastened to the skin with either sutures or staples. Earlier studies comparing sutures and staples have shown varied results: one meta-analysis in orthopedic wounds concluded higher complications with staples1; however, a later review in orthopedics and two Cochrane reviews showed no significant differences.2–4 Neither of these studies were limited to nonabsorbable sutures. All these reviews compared sutures to staples with regards to wound closure.1–4 Some of the results from these studies, such as speed of fixation, pain of removal, and risk of infection, also apply to the fixation of the compressive dressing during skin graft surgery. It seems there is consensus that the application of staples is faster,1 and staples are more painful to remove.5–9 According to a recent systematic review on the different types of tie-over sutures or dressing materials, the securing method has little effect on survivability of the graft.10
In the present study, we specifically investigate sutures versus staples as methods of fixation for the compressive dressings securing the nipple-areola complex (NAC) grafts during double incision chest contouring surgery, which is the most common surgical technique used for chest contouring in gender-affirming surgery.11 The purpose of this study was to compare sutures and staples as a method of fixation for compressive dressings, specifically for NAC grafts during double incision chest contouring surgery. Which of these two methods (sutures versus staples) is faster to apply and remove? Which is less painful at removal? Which costs less and is more sustainable?
MATERIALS AND METHODS
Ethics
Ethical approval was obtained from the Swedish Ethical Review Authority (# 2019-05624).
Surgical Technique
During double incision chest contouring surgery, the NAC was deepithelialized as a full-thickness skin graft at the beginning of surgery. After being harvested, it was wrapped in damp gauze pads and stayed so until the removal of the breast was completed, and the skin was sutured. Then, the area where the NAC graft is to be transplanted was drawn and deepithelialized, the NAC was further thinned with scissors, and then sutured with 4/0 Monocryl in its new position onto the chest. The final step of the surgery consisted of applying Jelonet gauze (Smith & Nephew plc, Watford, United Kingdom) and a compressive dressing, which could be either sutured or stapled to the skin. Specifically at our institution, Allevyn nonadhesive dressing (Smith & Nephew PLC, London, UK) was used. Figure 1 depicts a schematic representation of the fastening with sutures and staples, respectively.
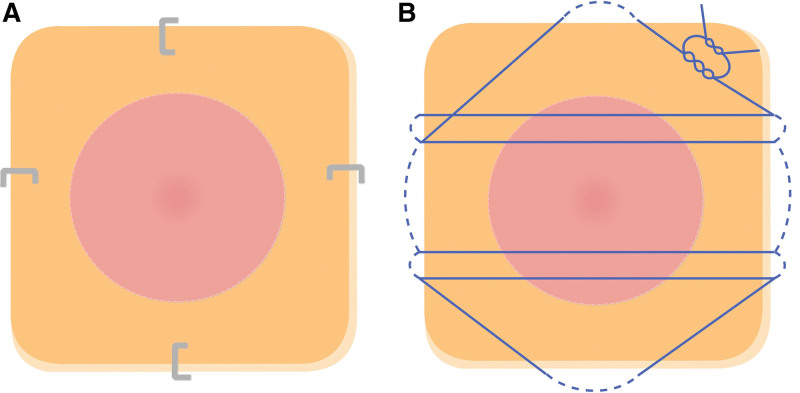
Fig. 1.
Schematic drawing of the method of fixating the compressive dressing. Allevyn nonadhesive dressing was applied on top of the NAC with a layer of Jelonet gauze between the dressing and the NAC. In the schematic drawing, the dressing is depicted in orange, with the pink centered circle representing the underlying NAC. The compressive dressing was fastened to the skin using either sutures or staples. A, Dressing fastened with four surgical staples on each side of the dressing. However, it should be noted that the position of the staples could vary between patients depending on perioperative conditions. B, Compressive dressing fastened with sutures tied over the dressing. The star-shaped pattern of the sutures is an approximate representation of how the sutures were placed.
To accomplish adequate compression to the entire chest, a compressive corset was also applied. Indeed, this also gave further compression to the underlining Allevyn dressing.
Patients’ Group
Forty patients undergoing chest contouring surgery with the double incision technique with NAC grafts were prospectively enrolled in the study. Patients were all assigned female at birth and, regardless one’s gender identity, presented with a diagnosis of gender dysphoria.
Before enrolling specific patients into the study, a sequence list was created, and individuals were randomized using block randomization. The randomization plan was constructed using randomization.com.12 The size of the blocks was set at 20 in two separate blocks. Seed code for reproduction is 2284. Block randomization was used to ascertain equally weighted groups.
One group had the dressings fixed with sutures (4/0 nylon, passed through the skin and over the dressing in a star-like shape); the other group had the dressing fixed with staples (four staples in total, one over each side of the dressing).
Timing for dressing fixation was measured using the stopwatch feature of a smartphone. Starting time began in a coordinated manner between the surgeon and researcher at the application of the first suture or staple, and it stopped as the suture knot was cut, or the last staple was set. The surgical approach was otherwise equal between groups.
Surgeons were not blinded to the fixation method. Patients were blinded to the fixation method until removal. Fixation of the compressing dressing was removed by nurses at day 5 postoperative. Timing for removing the dressing was measured in the same way as timing for fixation.
The nurse removing the dressing estimated the complexity of removal using the visual analog 100 mm scale (VAS-100mm). The end-points were labeled in Swedish as: 0 mm being “inte alls besvärligt” (translated by authors as “not difficult at all”) and 100 mm being “mycket besvärligt” (translated by authors as “very difficult”).
Pain during removal was measured using the verbal numerical rating scale 11 (vNRS-11) with end-points verbally instructed in Swedish, as 0 being “ingen smärta alls” (translated by authors as “no pain at all”) and 10 being “den värsta smärtan du kan tänka dig” (translated by authors as “the worst pain you can imagine”). One nurse removed 70% of the dressings, whereas the remaining dressings were removed independently by seven other nurses, all with several years of experience working at our plastic surgery clinic. Costs of the materials were calculated.
Statistics
All statistical calculations were performed using Microsoft Excel, version 16.71 (Microsoft Corp., Redmond, Wash.). P values were calculated using a two-tailed independent t test. Results were considered statistically significant with a P value less than 0.5.
RESULTS
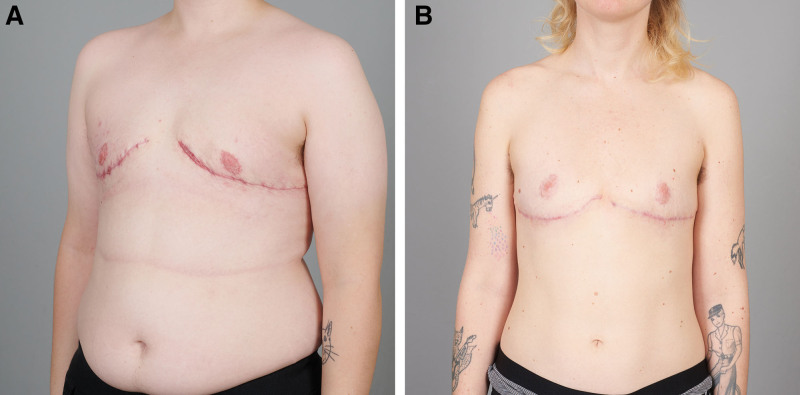
No patients were lost to follow-up. No serious complications were observed at any point during surgery or at follow-up, such as NAC necrosis, infection, or acute reoperation. Surgical results of both sutures and staples are depicted in Figure 2.
Fig. 2.
Postoperative pictures. A, Example of surgical results using staples for fastening the compressive dressing. The image was taken 6 weeks postoperatively. B, Example of surgical results using sutures for fastening the compressive dressing. This image was taken 15 weeks postoperatively. Apart from the fixation material of the compressive dressing, the surgical method was identical for both examples.
Mean time for applying staples to the compressive dressing was 5.3 (SD ± 1.0) seconds, whereas mean time for applying sutures was 94.6 (SD ± 20.2) seconds. This difference was statistically significant (P <0.001).
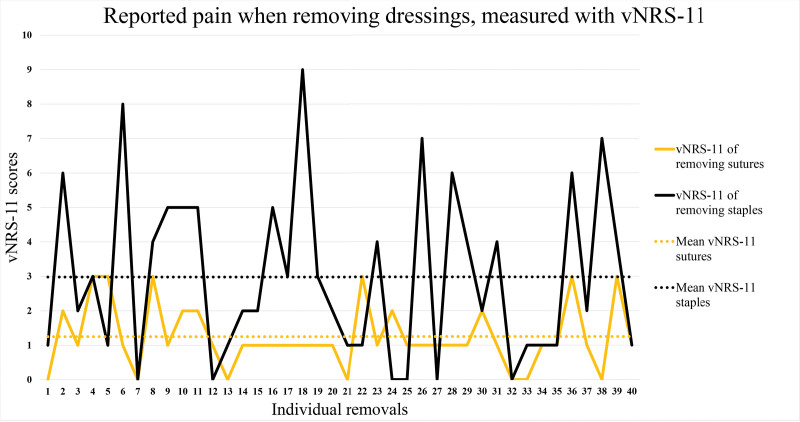
Mean vNRS-11 scores for pain during removal were 1.25 (SD ± 0.92) for sutures, and 2.98 (SD ± 2.43) for staples. This difference was also statistically significant (P < 0.001) (Fig. 3).
Fig. 3.
Pain reported when removing dressings and measured with vNRS-11. This graph illustrates vNRS-11 scores of pain at removal of the compressive dressings. The y axis represents vNRS-11 scores, ranging from 0 to 10. The x axis shows removal of each compressive dressing, with each number representing one breast. The vNRS-11 score for removal of the sutures is marked in yellow, and its mean value (1.25) is marked with a yellow dotted line. The vNRS-11 score for removal of the staples is marked in black, and its mean value (2.98) is marked with a black dotted line.
The removal of sutures of the compressive dressing took a mean 38.8 seconds (SD ± 9.90 s) versus 39.9 seconds (SD ± 22.12 s) for staples. This difference was not statistically significant (P = 0.79).
Nurses found staples more difficult to remove (mean VAS-100 mm: staples 18.3 mm versus sutures 6.0 mm, P < 0.001). Sutures were slightly less costly (18 Swedish crowns) compared to staples (30 SEK). One stapler (Covidien Appose ULC 35W, Minneapolis, Minn.) was sufficient to fixate two dressings whilst sutures required two separate packages to be opened. However, staplers were one time use, and it never occurred that all staples in the stapler’s magazine had to be used; thus, staplers produced more plastic and metallic waste, compared to sutures.
DISCUSSION
According to scientific literature in the field of plastic surgery, compressive dressing for skin grafts can be fixed in a variety of ways.10 More specifically, a recent systematic review shows that the different methods (such as staples and sutures) for fixation of the compressive dressing onto skin grafts have little effect on the graft survival.10 Thus, when choosing the best method for fixation of the compressive dressing, other characteristics have to be considered, such as speed of fixation, pain experienced by patients at removal of the fixation and dressing material, risk of infection, costs, and environmental impact. The focus of the present study is a group of 40 patients undergoing double incision chest contouring surgery with free NAC graft.
Results from this study demonstrates that, in the operating theater, the application of staples is considerably quicker (3 min) to apply compared to sutures; however, this 3-minute difference is not large enough to affect the efficiency of the operating theater use, nor is a 3-minute longer anesthesia duration believed to impact the risk of postoperative complications.
On the other hand, the removal of sutures is less painful compared to staples, scoring 1.73 points lower on the vNRS-11. However, this raises the question if a difference of 1.73 on the vNRS-11 is meaningful for patients. Previous studies have reported the minimum clinically significant change on the vNRS-11 to be between 1 and 1.5,13–16 with a change of 1.74–4.4 equaling a much-improved pain intensity.13,14,16 Therefore, we argue the difference of 1.73 to be clinically significant.
Nurses found sutures easier to remove. Despite being statistically significant, both of these results (VAS 6 mm for sutures, and VAS 18.3 mm for staples) are in the lowest part (first fifth) of the percentile scale. Hence, neither sutures nor staples can be considered difficult to remove. Therefore, it is likely that this difference is not clinically significant. Although this study did not investigate the aesthetical difference in NAC grafts following the fixation of the compressive dressing with sutures versus staples, it indeed shows that there is no difference in partial or total graft loss between the two groups.
Finally, although in our series of patients, there were no reported complications, a larger series of cases might show complications specific to the method of fixation, for example, cases of infection of sutures or staples.
This research compared two methods of fixation (sutures and staples) of the Allevyn compressive dressing for skin grafts. Other methods of compressions, such as gauze bolster, and other methods of fixations, such as plastic occlusive dressings, require future investigation and comparison with the results presented here.
CONCLUSIONS
There is no evidence of complications or evidence of different graft take when comparing sutures versus staples as a method of fixation of the compressive dressing for the NAC in double incision chest contouring surgery. Staples are quicker to apply; however, it has a minimal, thus not significant, impact on the total surgical time.
Being that all the other outcomes are similar or not significant, the less-pain experienced at removal of sutures makes sutures the preferable method for fixation of the compressive dressing for NAC grafts during double incision chest contouring surgery. In addition, sutures are less costly than staples; finally, sutures produced less material waste.
In conclusion, the use of sutures rather than staples is advocated as the fixation method for the NAC graft in double incision chest contouring surgery for assigned-female-at-birth persons presenting gender dysphoria.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
REFERENCES
- 1.Smith TO, Sexton D, Mann C, et al. Sutures versus staples for skin closure in orthopaedic surgery: meta-analysis. BMJ. 2010;340:c1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krishnan RJ, Crawford EJ, Syed I, et al. Is the risk of infection lower with sutures than with staples for skin closure after orthopaedic surgery? A meta-analysis of randomized trials. Clin Orthop Relat Res. 2019;477:922–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mackeen AD, Berghella V, Larsen ML. Techniques and materials for skin closure in caesarean section. Cochrane Database Syst Rev. 2012;11:CD003577. [DOI] [PubMed] [Google Scholar]
- 4.Biancari F, Tiozzo V. Staples versus sutures for closing leg wounds after vein graft harvesting for coronary artery bypass surgery. Cochrane Database Syst Rev. 2010;12:CD008057. [DOI] [PubMed] [Google Scholar]
- 5.Daniilidis K, Stukenborg-Colsman C, Ettinger S, et al. Nylon sutures versus skin staples in foot and ankle surgery: is there a clinical difference? Musculoskelet Surg. 2020;104:163–169. [DOI] [PubMed] [Google Scholar]
- 6.Yuenyongviwat V, Iamthanaporn K, Hongnaparak T, et al. A randomised controlled trial comparing skin closure in total knee arthroplasty in the same knee: nylon sutures versus skin staples. Bone Joint Res. 2016;5:185–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stockley I, Elson RA. Skin closure using staples and nylon sutures: a comparison of results. Ann R Coll Surg Engl. 1987;69:76–78. [PMC free article] [PubMed] [Google Scholar]
- 8.Selvadurai D, Wildin C, Treharne G, et al. Randomised trial of subcuticular suture versus metal clips for wound closure after thyroid and parathyroid surgery. Ann R Coll Surg Engl. 1997;79:303–306. [PMC free article] [PubMed] [Google Scholar]
- 9.Slade Shantz JA, Vernon J, Morshed S, et al. Sutures versus staples for wound closure in orthopaedic surgery: a pilot randomized controlled trial. Patient Saf Surg. 2013;7:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steele L, Brown A, Xie F. Full-thickness skin graft fixation techniques: a review of the literature. J Cutan Aesthet Surg. 2020;13:191–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Selvaggi G. Mastectomy in trans men. In: Cordova A, Innocenti A, Toia F, Tripoli M, editors. Plastic and Cosmetic Surgery of the Male Breast. Cham: Springer International Publishing; 2020. p. 161–70. [Google Scholar]
- 12.Dallal GE. 2020. Available at http://www.randomization.com. Accessed October 1, 2020.
- 13.Kendrick DB, Strout TD. The minimum clinically significant difference in patient-assigned numeric scores for pain. Am J Emerg Med. 2005;23:828–832. [DOI] [PubMed] [Google Scholar]
- 14.Farrar JT, Young JP, Jr, LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–158. [DOI] [PubMed] [Google Scholar]
- 15.Bijur PE, Chang AK, Esses D, et al. Identifying the minimum clinically significant difference in acute pain in the elderly. Ann Emerg Med. 2010;56:517–521.e1. [DOI] [PubMed] [Google Scholar]
- 16.Salaffi F, Stancati A, Silvestri CA, et al. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain. 2004;8:283–291. [DOI] [PubMed] [Google Scholar]