Abstract
Background
The incidence of falling has always been high among the elderly, and it was easy to cause injuries to the elderly and seriously affect their quality of life. There were many studies have been conducted on risk factors affecting the fall of the elderly, but the results widely, retirement institutions as a gathering place for the elderly, there was currently no comprehensive analysis of the factors related to elderly falls in pension institutions. This study aimed to explore the influencing factors of falls among older adults in Chinese nursing homes.
Methods
Chinese and English databases were searched for literature published from database inception to 5 April 2023 on the influencing factors of falls among older adults in Chinese nursing homes. Two reviewers independently screened articles, extracted data, and assessed the quality of the included studies. Meta-analysis was performed using RevMan 5.4 software.
Results
Eleven studies involving 3503 participants were included in the meta-analysis. The pooled estimate of falls among older adults in Chinese nursing homes was 32% [95% confidence interval (95%CI) (24.0%, 39.0%)]. The main influencing factors for falls among older adults in Chinese nursing homes were age (Odds Ratio (OR) = 1.53), gender (OR = 5.50), visual impairment (OR = 2.30), sedative-hypnotics (OR = 2.36), fear of falling (OR = 2.95), hypertension (OR = 3.72), static balance (OR = 2.02), three or more chronic diseases (OR = 5.63), cognitive status (OR = 2.64), walking aid use (OR = 1.98), fall-related chronic diseases (OR = 2.48), self-awareness of abilities (OR = 2.43), and frequent reminders for fall prevention (OR = 0.10).
Conclusion
Falls among older adults in Chinese nursing homes were common, and there were many influencing factors. Timely screening and intervention should be implemented to reduce the adverse consequences of falls on older adults.
Trial registration
Registration number: CRD42023421099.
1 Introduction
The results of China’s seventh national census showed that the population of elderly people aged 60 and above has reached 264 million, accounting for 18.7% of the total population [1]. With the increasing number of only children and the majority of them working outside their hometowns, home-based elderly care can no longer meet the social demands of contemporary society. As a result, more and more elderly people are choosing to live in elderly care institutions [2, 3].
Falling is an unintentional act of falling to the ground or a lower surface, but does not include violence, loss of consciousness, paralysis, or seizures as causes [4]. As the most common injurious behavior, it was a major health problem faced by older people worldwide. It has the highest incidence and mortality rates in accidental injuries among older people, not only causing physical and mental harm but also seriously affecting their quality of life. Falling also imposed heavy economic and care burdens on families and society [5–7].
Research has shown that the incidence of falls among elderly people living in elderly care institutions is higher, with a rate of 30% to 50%, which was three times higher than that of elderly people in the community. The annual incidence rate of falls in people aged 65 and above exceeded 50%, and 4% to 15% of falls result in serious injuries [8, 9]. Some studies conducted meta-analysis on fall-related factors of the elderly suffering from different diseases such as hypertension and stroke, or conducted quantitative and comprehensive analysis on the overall fall rate of the elderly in China. At the same time, due to the influence of research location and social environment, the fall rate and related influencing factors obtained in the existing literature are different, and there is a lack of a comprehensive quantitative analysis. No studies on the influencing factors of falls among older adults in Chinese retirement institution have been found. Therefore, it was necessary to comprehensively understand the influencing factors of falls among elderly people in Chinese elderly care institutions and provide targeted care. The aim of this study is to explore the influencing factors of falls among elderly people in Chinese elderly care institutions through a meta-analysis and provide theoretical basis for the prevention of falls among elderly people in elderly care institutions.
2 Materials and methods
2.1. Registration
The protocol of this review was registered in the International Prospective Register of Systematic Overview (PROSPERO) database (https://www.crd.york.ac.uk/PROSPERO/), registration number: CRD42023421099.
2.2. Ethics
Ethics approval is not required in Meta-analysis.
2.3 Literature search strategy
The literature search strategy included comprehensive searches of several databases, including Chinese Biomedical Literature Database (CBM, http://www.sinomed.ac.cn/index.jsp), China National Knowledge Infrastructure (CNKI, https://www.cnki.net/), VIP Database (http://lib.cqvip.com/) and Wanfang Database (https://new.wanfangdata.com.cn/index.html), Embase, Web of Science, The Cochrane Library, and PubMed, up to 5 April 2023, for cross-sectional studies, cohort studies, and case-control studies related to the influencing factors of falls among elderly residents in Chinese retirement institutions. In addition, relevant references from the included articles were manually searched and added. The English search strategy was determined as follows: (the aged OR elder people OR senior citizens OR old folks OR the elderly OR old people) AND (senior housing OR senior center OR residential aged care facility OR old age homes OR nursing home residents OR old-age care institutions OR the old folk′s homes OR retirement home OR rest home) AND (falls OR falling OR accidental fall OR slip and fall) AND (risk factor OR predictor OR influencing factor OR protective factor OR promotive factor OR correlate).
2.4 Inclusion and exclusion criteria for literature selection
2.4.1 Inclusion criteria for literature selection
(1) Study population: Elderly individuals aged 60 years and above; (2) Study topic: Falls and their influencing factors among elderly residents in Chinese nursing homes; (3) Study design: Cross-sectional studies, case-control studies, or cohort studies; (4) Articles must report the Odds Ratios (ORs) and 95% Confidence Intervals (CIs) of relevant influencing factors; (5) Articles must be published in either Chinese or English and available online.
2.4.2 Exclusion criteria for literature selection
(1) Studies with a quality score of less than 4 points, indicating low-quality research; (2) Studies for which the full text or sufficient data cannot be obtained; (3) Duplicate publications of the same study; (4) Conference abstracts, systematic reviews, animal experiments, case reports, experience summaries, or other types of non-original research articles.
2.5 Article screening and data extraction
All searched literature was imported into the Endnote X9 software, and two researchers independently conducted title and abstract screening, as well as full-text reading to perform the initial and secondary screening of literature and extract relevant information. In case of any discrepancies, they would be resolved through discussion or consultation with a third party. The information extracted will include the author, year of publication, study location, study design, sample size, rate of falling, relevant factors, quality score, and other relevant information.
2.6 Quality assessment
The Newcastle-Ottawa scale (NOS) [10] is used to evaluate case-control and cohort studies. It consists of eight items, with scores ranging from7 to 9 indicating high-quality literature, 5 to 6 indicating moderate-quality literature, and 0 to 4 indicating low-quality literature. The Agency for Healthcare Research and Quality (AHRQ) [11] in the United States uses a similar scale to evaluate cross-sectional studies, with total scores ranging from 8 to 11 indicating high-quality studies, 4 to 7 indicating moderate-quality, and 0 to 3 indicating low-quality. Methodological quality evaluation is independently conducted by two evaluators. In the event of disagreements, they can resolve them through discussion or have a third researcher make the final decision.
2.7 Statistical analysis
Descriptive analysis was used in most sections to report relevant content, and the statistical software package RevMan 5.4 was used to analyze quantitative data extracted from each study. OR values and their 95% CIs were used for statistical combination, and the χ2 test (with a significance level of α = 0.1) combined with I2 value was used to determine the degree of heterogeneity. If P≤0.1 and I2>50%, a random effects model was used for meta-analysis; otherwise, a fixed effects model was used for meta-analysis. Descriptive analysis was used for influencing factors that were not suitable for meta-analysis. Sensitivity analysis was conducted for each influencing factor by transforming different effect models. If the number of studies was ≥10, Egger’s test and Begg’s test were used to evaluate publication bias in the literature.
3 Results
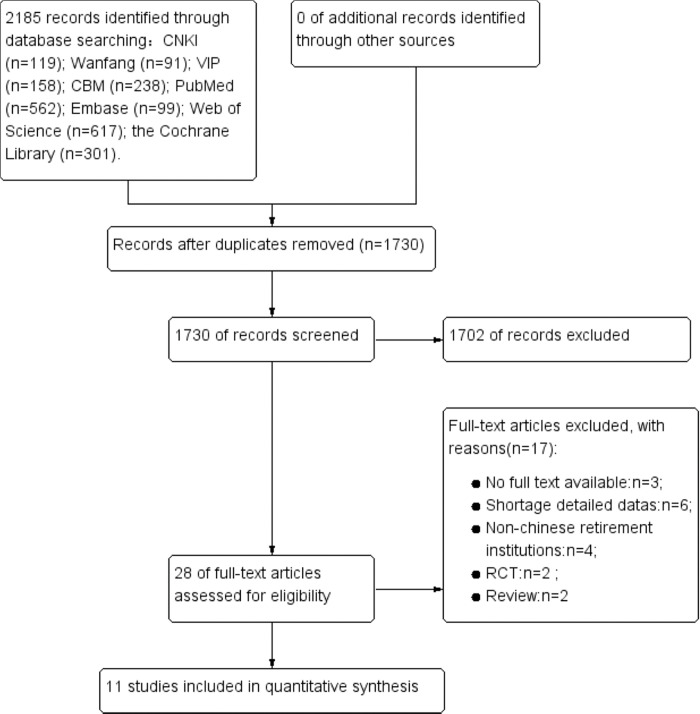
3.1 Literature search results
A total of 2185 literature sources were initially retrieved, including 606 in Chinese and 1579 in English. Literature sources were then screened step by step, and 11 studies [12–22] were ultimately included in the present study. The literature screening process is shown in Fig 1.
Fig 1.
3.2 Characteristics of included literature and results of literature quality assessment
A total of 11 literature sources with a combined sample size of 3503 were included in the analysis, with 1126 cases in the fall group and 2377 cases in the non-fall group. The NOS scores for the case-control and cohort studies were both ≥5 points, and the AHRQ scores for the cross-sectional studies were all ≥4 points, all studies included in the analysis were of medium to high quality, indicating that the literature quality met the requirements. The main information extracted from the literature sources is shown in Table 1.
Table 1. Characteristics of included studies and quality assessment results.
| First authors | Year | Region | Study design | The survey time periods | The time periods for falls | Fall example | Non-fall example | Total sample size | Fall rate (%) | Factors | Quality assessment tool | Quality score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Li Cuizha | 2022 | Kunming City | Cross-sectional study | May to July 2021 | —— | 82 | 141 | 223 | 36.77 | adn | AHRQ | 7 |
| Feng Wenting | 2022 | Xinyang, | Cross-sectional study | April to October 2020 | In the past year | 107 | 324 | 431 | 24.83 | abcfjklmno | AHRQ | 8 |
| Lin Shuang | 2021 | Shenyang, | Cross-sectional study | July to September 2018 | In the past year | 114 | 569 | 683 | 16.70 | cjo | AHRQ | 9 |
| Hu Huiju | 2021 | Tangshan, | Cross-sectional study | August to November 2020 | In the past year | 223 | 267 | 490 | 45.50 | aelp | AHRQ | 8 |
| Cheng Xiao | 2020 | Chenzhou | Cross-sectional study | October to December 2018 | In the past year | 41 | 79 | 120 | 34.16 | cghi | AHRQ | 6 |
| Zhang L | 2019 | Xiamen | Cross-sectional study | June to September 2016 | In the past year | 69 | 149 | 218 | 31.65 | dgikl | AHRQ | 8 |
| Liang Danyan | 2017 | Hohhot | Cross-sectional study | —— | August 2015 to August 2016 | 27 | 63 | 90 | 30.00 | bfmp | AHRQ | 7 |
| Zhao Ming | 2016 | Hangzhou | Cross-sectional study | —— | November 2012 to October 2013 | 48 | 322 | 370 | 12.97 | ae | AHRQ | 6 |
| Zhang Yu | 2016 | Urumqi | Cross-sectional study | June to December 2015 | In the past year | 232 | 264 | 496 | 46.77 | cdgnq | AHRQ | 7 |
| Chen Yang | 2014 | Nanjing City | Cross-sectional study | October 2012 to January 2013 | In the past year | 29 | 45 | 74 | 39.19 | dkq | AHRQ | 5 |
| Liu Yongyi | 2002 | Beijing | 1:1 Case-control study | —— | Within the past 18 months. | 154 | 154 | 308 | —— | dfgh | NOS | 7 |
Note: "——" indicates not applicable; AHRQ = Agency for Healthcare Research and Quality; NOS = Newcastle-Ottawa Scale; a = age; b = gender; c = visual impairment; d = sedative-hypnotic medication; e = reduced activity due to fear of falling; f = hypertension; g = static balance; h = three or more chronic conditions; i = cognitive status; j = mobility aid; k = fall-related chronic conditions; l = activities of daily living; m = indoor lighting; n = regular physical exercise; o = realistic self-perception; p = frequently reminded to prevent falls; q = sleep.
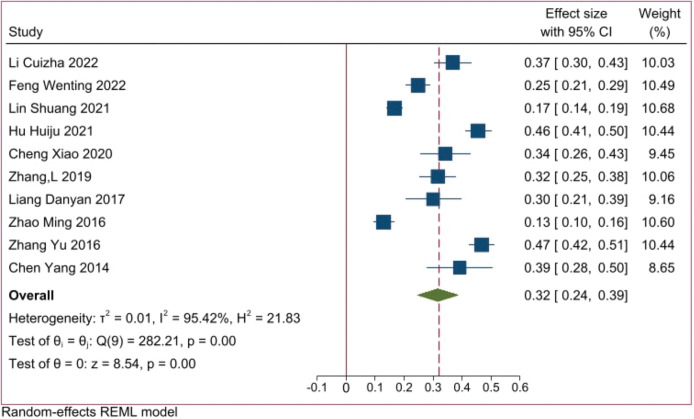
3.3 The fall rate of elderly residents in Chinese retirement institutions
The final inclusion in the literature review consisted of a one-to-one case-control study that did not involve fall rates. Therefore, a quantitative synthesis was conducted specifically for the fall rates mentioned in the remaining ten studies. The analysis results showed that the fall rate of elderly residents in Chinese nursing homes was 32% [95%CI (0.24, 0.39), P < 0.001] (Fig 2).
Fig 2.
3.4 Influencing factors and results
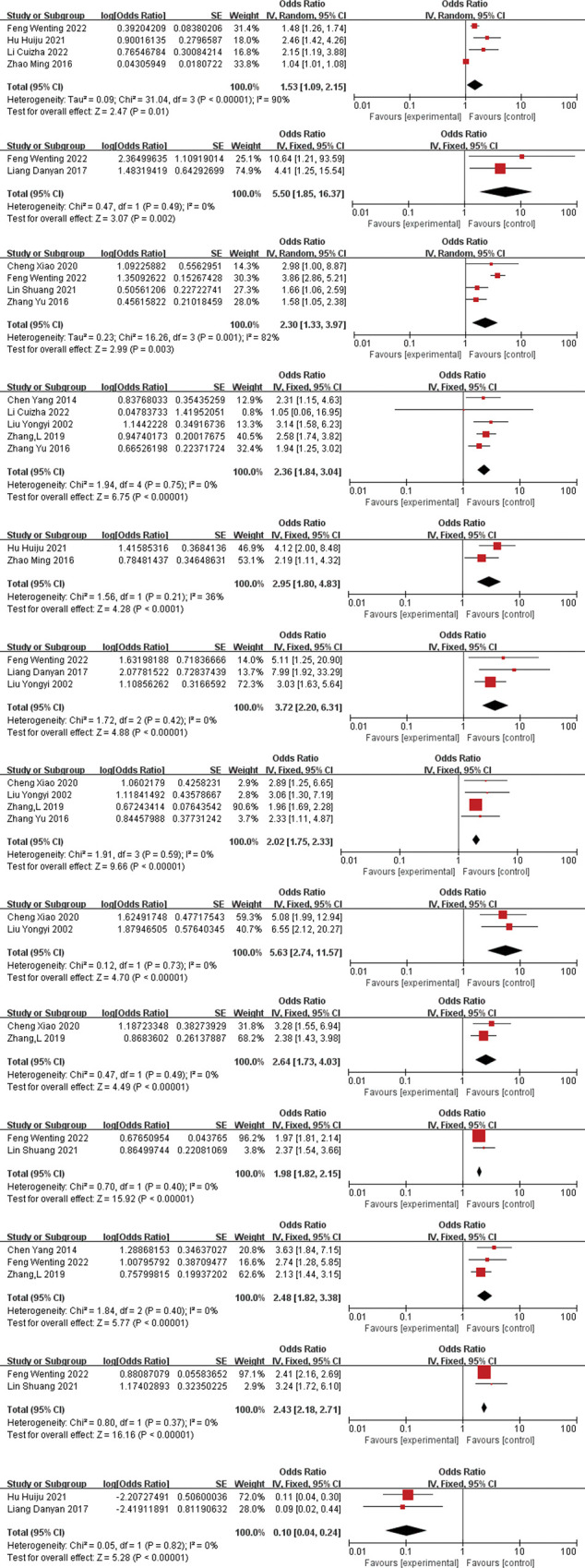
3.4.1 Meta-analysis results
Two or more study reporting the same influencing factors were combined using RevMan5.4 software, and 17 influencing factors related to falls among elderly residents in nursing homes were included in the quantitative analysis. The meta-analysis results showed that age (OR = 1.53, 95%CI = 1.09–2.15), gender(OR = 5.50, 95%CI = 1.85–16,37), visual impairment(OR = 2.30,95%CI = 1.33–3.97), sedatives-hypnotics(OR = 2.36,95%CI = 1.84–3.04, fear of falling(OR = 2.95, 95%CI = 1.80–4.83), hypertension(OR = 3.72, 95%CI = 2.20–6.31), postural balance(OR = 2.02, 95%CI = 1.75–2.33), three or more chronic diseases(OR = 5.63, 95%CI = 2.74–11.57), cognitive status(OR = 2.63, 95%CI = 1.73–4.03), walking aids(OR = 1.98, 95%CI = 1.82–2.15), fall-related chronic diseases(OR = 2.48, 95%CI = 1.82–3.38), self-awareness of abilities(OR = 2.43, 95%CI = 2.18–2.71), being frequently reminded to prevent falls(OR = 0.10, 95%CI = 0.04–0.24), were statistically significant factors related to falls among elderly residents in Chinese nursing homes(P<0.05). However, indoor lighting, regular physical exercise, and sleep were not significantly associated with falls. Please refer to Table 2 for details. And the forest plot for 13 influencing factors refer to Fig 3 (From Fig 3A to 3M).
Table 2. Meta-analysis and sensitivity analysis results of factors influencing falls among elderly residents in Chinese nursing homes.
| Influencing Factors | Number of included studies | Heterogeneity test results | Meta-analysis results | Sensitivity analysis | ||
|---|---|---|---|---|---|---|
| I2(%) | P | effect model | OR (95%CI) | OR (95%CI) | ||
| Age (≥60 years old) | 4 | 90 | <0.00001 | random | 1.53 (1.09, 2.15) * | 1.07 (1.03, 1.10) |
| gender | 2 | 0 | 0.49 | fixed | 5.50 (1.85,16.37) * | 5.50 (1.85,16.37) |
| visual impairment | 4 | 82 | 0.001 | random | 2.30 (1.33, 3.97) * | 2.52 (2.05, 3.11) |
| sedative-hypnotics use | 5 | 0 | 0.75 | fixed | 2.36 (1.84, 3.04) * | 2.36 (1.84, 3.04) |
| reduced activity due to fear of falling | 2 | 36 | 0.21 | fixed | 2.95 (1.80, 4.83) * | 2.97 (1.60, 5.51) |
| hypertension | 3 | 0 | 0.42 | fixed | 3.72 (2.20, 6.31) * | 3.72 (2.20, 6.31) |
| postural balance | 4 | 0 | 0.59 | fixed | 2.02 (1.75, 2.33) * | 2.02 (1.75, 2.33) |
| having three or more chronic diseases | 2 | 0 | 0.73 | fixed | 5.63(2.74, 11.57) * | 5.63(2.74, 11.57) |
| cognitive status | 2 | 0 | 0.49 | fixed | 2.64 (1.73, 4.03) * | 2.64 (1.73, 4.03) |
| walking aids | 2 | 0 | 0.4 | fixed | 1.98 (1.82, 2.15) * | 1.98 (1.82, 2.15) |
| fall-related chronic diseases | 3 | 0 | 0.4 | fixed | 2.48 (1.82, 3.38) * | 2.48 (1.82, 3.38) |
| activities of daily living | 3 | 88 | 0.0003 | random | 1.26 (0.38, 4.16) | 1.64 (1.23, 2.18) |
| indoor lighting | 2 | 95 | <0.0001 | random | 1.25 (0.02, 94.64) | 6.72 (3.70, 12.22) |
| regular physical exercise | 3 | 85 | 0.001 | random | 1.38 (0.44, 4.33) | 1.24 (0.80, 1.92) |
| self-awareness of abilities | 2 | 0 | 0.37 | fixed | 2.43 (2.18, 2.71) * | 2.43 (2.18, 2.71) |
| being frequently reminded to prevent falls | 2 | 0 | 0.82 | fixed | 0.10 (0.04, 0.24) * | 0.10 (0.04, 0.24) |
| sleep | 2 | 86 | 0.009 | random | 0.92 (0.27, 3.06) | 1.36 (0.99, 1.85) |
Note
*P<0.05.
Fig 3.
3.4.2 Descriptive analysis
The studies [12–14, 17, 18, 22] have identified that the use of analgesics, arthritis, osteoporosis, dizziness, poor overall health assessment, no spouse, post-stroke sequelae, sensory loss, wearing slippers, drinking alcohol, and taking four or more medications are factors influencing falls among elderly residents in nursing homes. However, due to the limited number of studies on these influencing factors, only qualitative descriptions can be provided.
3.4.3 Sensitivity and publication bias analysis
According to the sensitivity analysis conducted using the transformation model, the consistency of all influencing factors was found to be stable, indicating that the results are stable and reliable (Table 2). Since the number of studies included for each influencing factor is less than 10, and the significance of publication bias for the literature on fall rates is low, no publication bias analysis was conducted.
4 Discussion
After comprehensive search and strict literature screening, this Meta-analysis included 11 articles consisting of 10 cross-sectional studies and 1 case-control study, all of which clearly stated the inclusion and exclusion criteria of the investigated subjects and the factors influencing falls. The quality of the literature meets the requirements, and the statistical methods used are correct. Therefore, the meta-analysis has high credibility.
4.1 The incidence of falls among elderly residents in Chinese nursing homes is relatively high
A total of 11 Chinese literature on factors influencing falls among elderly residents in nursing homes were included in this study, comprising 3,503 research subjects from 11 provinces, cities, and autonomous regions in China. Meta-analysis results showed that the incidence of falls among elderly residents in Chinese nursing homes was 32% [95% CI (24%, 39%), P < 0.001].
4.2 Analysis of factors influencing falls among elderly residents in Chinese nursing homes
4.2.1 General factors
The results of this study show that age, gender, and poor static balance are risk factors for falls among elderly residents in nursing homes. As the body’s physiological functions decline and organs age with increasing age, reaction time lengthens and various balance abilities deteriorate, leading to a higher incidence of falls and more severe injuries after falls [23]. Females experience a decline in estrogen levels after menopause, which increases the risk of osteoporosis, while female muscle strength and physique are relatively poor compared to males [24]. This is consistent with the results of previous studies conducted by Yao Yuhua et al. [25], which found that older women have a higher risk of falls. An unstable gait can easily lead to a loss of balance and falls, which is consistent with the results of Wang Liancheng’s study [26]. Therefore, as a place where elderly people live together, nursing homes should strengthen the care of high-risk groups for falls and regularly provide rehabilitation training targeted at improving balance ability to prevent falls.
4.2.2 Disease-related factors
As the elderly population ages, the risk of developing multiple chronic diseases gradually increases. Studies have shown that the prevalence of chronic diseases among elderly people in China is 43.6% [27]. The results of this study showed that the risk factors for falls among elderly people in Chinese nursing homes include having a fall-related chronic disease (OR = 2.48) and having three or more chronic diseases (OR = 5.63). However, due to limitations in the available data from the literature included in this study, specific types of chronic diseases were not analized. The study shows that visual impairment (OR = 2.30) is a risk factor for falls, and factors affecting vision include cataracts, glaucoma, retinal vascular disease, age-related macular degeneration, and diabetic retinopathy [28]. Compared to adults with normal vision, adults with visual impairment are 1.7 times more likely to fall and 1.9 times more likely to fall multiple times [29]. Hypertension (OR = 3.72) is also a contributing factor to falls in elderly residents of nursing homes, with over half of middle-aged and elderly people in China suffering from the condition. Hypertension, combined with a decrease in blood pressure regulation ability, the presence of other diseases, and the use of antihypertensive drugs, can lead to non-physiological changes in blood pressure fluctuation amplitude and frequency, making individuals more susceptible to dizziness and increasing the risk of falls [30, 31], which is consistent with the results of a study by Zhang Di [32]. Weiner [33] found that elderly individuals taking psychotropic drugs have a 2.4 times higher risk of falls compared to those who do not take these medications. Multiple guidelines [34, 35] have pointed out that sedatives and hypnotics can increase the risk of falls, which is consistent with the results of this study. Sedatives and hypnotics (OR = 2.36) are a risk factor for falls in elderly residents of nursing homes. Therefore, Medical and nursing staff in elderly care institutions should pay attention to the treatment of various chronic diseases in elderly residents, take medications on time and use medications reasonably, and strengthen the observation of medication side effects. For elderly individuals with visual impairment, early detection and treatment of diseases that cause visual impairment should be carried out, or the use of reading glasses to correct vision should be considered.
4.2.3 Other factors
The results of this study showed that fear of falling, cognitive status, lack of self-awareness of abilities, walking aids, and frequent reminders to prevent falls are risk factors for falls in older adults in long-term care facilities. A study [36] found that older adults who fear falling have a 4.14 times higher risk of falling than those who do not. Fear of falling is an emotional and psychological disorder closely related to falling,which is often manifested as continuous worry about falling in daily life and avoidance of activities within the capacity. Declining cognitive abilities can affect the perception and coping abilities of older adults to the outside world, thereby increasing the risk of falls [37], which is consistent with the findings reported by scholars such as Sun Xiaoya [38]. Older adults with lower activities of daily living and poorer motor function are more likely to fall [39]. In addition, older adults’ lack of self-awareness of abilities includes: overconfidence, lack of protection when engaging in activities such as getting out of bed, reaching for high objects, or hanging clothes, which can lead to falls, or even if they do fall, they are unwilling to seek help from others; inadequate awareness of fall prevention, not realizing the serious consequences that falls may cause [13]. This study showed that walking aids (OR = 1.98) are a contributing factor to falls, which is consistent with the findings of Gell [40]. Improper use of walking aids can increase the risk of falls [41]. Regular reminders from nursing staff to prevent falls have a positive impact on reducing falls in older adults. Therefore, for older adults in long-term care facilities, their activities of daily living should be regularly assessed, and they should be encouraged to engage in appropriate activities to improve their abilities. Regular health education lectures on fall prevention should also be provided to enhance their awareness of fall prevention, while guiding them on the correct use of walking aids.
4.3 Limitations
Although this study included 11 provinces, municipalities, and autonomous regions in China, there is limited literature on the factors influencing falls in older adults in Chinese long-term care facilities. Among all retrieved literature, there were more cross-sectional studies with a local focus, while the number of cohort studies and case-control studies was extremely small, with small sample sizes and inadequate coverage. There were significant differences in sample size among the included studies, with the largest sample size being 683 cases and the smallest being 74 cases, leading to some inconsistencies. Additionally, the study results may have been affected by objective factors such as the source of literature and the focus of the research. Therefore, it is necessary to conduct higher quality case-control and cohort studies on falls in older adults in Chinese long-term care facilities, to provide a basis for fall prevention strategies in this population.
5 Conclusion
This study showed that the incidence of falls among elderly residents in Chinese nursing homes was relatively high. The main contributing factors to falls among elderly residents in Chinese nursing homes included age, gender, visual impairment, sedative-hypnotics use, fear of falling, hypertension, static balance, having three or more chronic diseases, cognitive status, walking aids, fall-related chronic diseases, self-awareness of abilities, and being frequently reminded to prevent falls. Medical and nursing staff in elderly care institutions should pay attention to these factors and conduct timely screening and interventions to reduce the incidence of falls among elderly residents and avoid the negative impact of falls on their quality of life.
Supporting information
(DOCX)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by Medical science and technology Project of Sichuan Provincial Health Commission [grant number:21ZD007] The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Zhenwu Zhai, Wenli Liu. Quality of the Seventh National Census Data and the New "Changes" in China’s Population. Population Research. 2021;45(03): 46–56. [Google Scholar]
- 2.Xiaoyun Mu, Jiang Du, Yanli Ding, et al. Investigation on the Risk Factors of Falls in Elderly People in Nursing Homes in Shenyang City. Nursing Research. 2014;28(21): 2598–2600. doi: 10.3969/j.issn.10096493.2014.21.012 [DOI] [Google Scholar]
- 3.Wen Yan, Xuemei Zhang, Qian Chen. Study on the Effectiveness of Fall Prevention and Its Influencing Factors in Elderly People in Nursing Homes. Chinese Journal of General Practice. 2019; 22(19): 2356–2360. doi: 10.12114/j.issn.1007-9572.2019.00.324 [DOI] [Google Scholar]
- 4.Gibson M J, Andres R O, Kennedy T E, et al. Kellogg International Work Group on the Prevention of Falls by the Elderly. The prevention of falls in later life Danish Medical Bulletin. 1987;34(4): 1–24. [PubMed] [Google Scholar]
- 5.Lian Hao, Sheng Li, Fang Xiang, et al. Time Trend Analysis of the Falling Mortality Rate in China from 2003 to 2018. Modern Preventive Medicine. 2020; 47(23): 4357–4360. [Google Scholar]
- 6.Lintao Li, Shengyong Wang. Disease Burden and Risk Factors of Falls in the Elderly. Chinese Journal of Epidemiology. 2001;04: 28–30. doi: [DOI] [Google Scholar]
- 7.White U E, Black A A, Wood J M, et al. Fear of falling in vision impairment. Optometry and vision science. 2015;92(6): 730–735. doi: 10.1097/OPX.0000000000000596 [DOI] [PubMed] [Google Scholar]
- 8.Dan Jiang, Wei Liu, Dandan Huang, et al. Analysis of Fall Risk and Its Risk Factors in Elderly People in Nursing Homes. Modern Clinical Nursing. 2019;18(05): 1–5. doi: 10.3969/j.issn.1671-8283.2019.05.001 [DOI] [Google Scholar]
- 9.Kolola T. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories. 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European journal of epidemiology. 2010;25(9): 603–605. doi: 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 11.Xiantao Zeng, Hui Liu, Xi Chen, et al. Meta-analysis series four: quality assessment tools for observational studies. Chinese Journal of Evidence-Based Cardiovascular Medicine. 2012; 4(04): 297–299. doi: 10.3969/j.1674-4055.2012.04.004 [DOI] [Google Scholar]
- 12.Cuizha Li, Rui Xu, Shuhua Song. Analysis of the current status and influencing factors of falls in elderly residents of nursing homes. Chinese Journal of Geriatric Care Medicine. 2022; 20(01): 67–71. doi: 10.3969/j.issn.1672-2671.2022.01.021 [DOI] [Google Scholar]
- 13.Wenting Feng, Tiantian Yan, Ruping Liu. Status and influencing factors of falls in elderly residents of nursing homes in Xinyang region. South China Journal of Preventive Medicine. 2022; 48(05): 551–555. [Google Scholar]
- 14.Shuang Lin. Study on the incidence and influencing factors of falls among the elderly in nursing homes in Shenyang City. China Medical University. 2021. [Google Scholar]
- 15.Huiju Hu, Jing Han, Qiqun Tang, et al. Study on the current situation and influencing factors of falls among elderly residents in nursing homes in Tianjin and Tangshan. Modern Preventive Medicine. 2021;48(11): 2018–2021. [Google Scholar]
- 16.Xiao Cheng, Lixia Lei, Xuran Qiu, et al. Status and influencing factors of falls in elderly residents of nursing homes in Chenzhou City. Journal of Xiangnan University (Medical Science). 2020; 22(04): 56–59. doi: 10.16500/j.cnki.1673-498x.2020.04.016 [DOI] [Google Scholar]
- 17.Zhang L, Zeng Y, Weng C, et al. Epidemiological characteristics and factors influencing falls among elderly adults in long-term care facilities in Xiamen, China. Medicine. 2019;98(8). doi: 10.1097/MD.0000000000014375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ming Zhao, Hao Wang, Yong He, et al. Epidemiological characteristics and risk factors of falls in elderly residents of nursing homes. Chinese Journal of Emergency Medicine. 2016;25(5): 654–658. doi: 10.3760/cma.j.issn.1671-0282.2016.05.022 [DOI] [Google Scholar]
- 19.Danyan Liang, Shengyun Duan, Ting Li, et al. Study on influencing factors of falls among elderly residents in nursing homes in Hohhot City. Injury Medicine (Electronic Edition). 2017; 6(01): 30–34. doi: 10.3868/j.issn.2095-1566.2017.01.007 [DOI] [Google Scholar]
- 20.Yu Zhang, Yan Wang, Yali Dai. Study on the incidence and influencing factors of falls among elderly residents in nursing homes in Urumqi City. Journal of Xinjiang Medical University. 2016;39(08): 1032–1034. doi: 10.3969/j.issn.1009-5551.2016.08.023 [DOI] [Google Scholar]
- 21.Yang Chen, Yayuan Ding, Nan Wang, et al. Investigation on the current status of falls among elderly residents in nursing homes in Nanjing City. Journal of Qilu Nursing. 2014;20(04): 52–53. doi: 10.3969/j.issn.1006-7256.2014.04.027 [DOI] [Google Scholar]
- 22.Yongyi Liu. A case-control study on the risk factors of falls among elderly residents in nursing homes. Chinese Journal of Comprehensive Medicine. 2002; 3(6): 559–560. [Google Scholar]
- 23.Ambrose A F, Paul G, Hausdorff J M. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1): 51–61. doi: 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 24.Zhou DD, Xu NT, Gao N, et al. Analysis of influencing factors for falls among elderly people in central urban area of Shanghai using structural equation model. Chinese Journal of Environmental & Occupational Medicine. 2019;36(08): 703–709. doi: 10.13213/j.cnki.jeom.2019.19223 [DOI] [Google Scholar]
- 25.Yao YH, Zhou DD, Ling LM, et al. Investigation of falls among elderly people in Hongkou district of Shanghai. Injury Medicine (Electronic Edition). 2019;8(02): 40–45. doi: 10.3868/j.issn.2095-1566.2019.02.009 [DOI] [Google Scholar]
- 26.Wang LC, Zhang LQ, Zhang Y, et al. Application of balance and gait analysis in the evaluation of fall risk in the elderly. Chinese Journal of Rehabilitation Medicine. 2012;27(03): 251–253. doi: 10.3969/j.issn.1001-1242.2012.03.014 [DOI] [Google Scholar]
- 27.Zhang R, Lu Y, Zhang SS, et al. Analysis of comorbidity patterns and disease correlations among elderly people with chronic diseases in China. Chinese Journal of Public Health. 2019;35(08): 1003–1005. doi: 10.11847/zgggws1120351 [DOI] [Google Scholar]
- 28.Shi YH, Chen LX. Research progress on factors of visual impairment and safety management strategies for elderly people. Journal of General Nursing. 2023;21(10): 1353–1356. doi: 10.12104/j.issn.1674-4748.2023.10.014 [DOI] [Google Scholar]
- 29.Keel S, Xie J, Foreman J, et al. The prevalence of diabetic retinopathy in Australian adults with self-reported diabetes: the National Eye Health Survey. Ophthalmology. 2017;124(7): 977–984. doi: 10.1016/j.ophtha.2017.02.004 [DOI] [PubMed] [Google Scholar]
- 30.Liming Tan, Lu Chen, Mingyan Long, et al. Spatial distribution and influencing factors analysis of hypertension among middle-aged and elderly people. Chinese Journal of Preventive Medicine. 2019;31(03): 236–241. doi: 10.19485/j.cnki.issn2096-5087.2019.03.005 [DOI] [Google Scholar]
- 31.Jing Li, Jing Tan, Weiwei Zhu, et al. Clinical diagnosis and treatment consensus of abnormal blood pressure fluctuations in elderly people in China. Chinese Journal of Hypertension. 2017;25(02): 132–140. doi: 10.3969/j.issn.1007-5410.2017.01.001 [DOI] [Google Scholar]
- 32.Di Zhang, Yao He, Jing Zeng, et al. Meta-analysis of risk factors for falls-related diseases among elderly people in China. Chinese Journal of Health Care and Medicine. 2017;19(04): 329–333. doi: 10.3969/.issn.1674-3245.2017.04.016 [DOI] [Google Scholar]
- 33.Weiner D K, Hanlon J T, Studenski S A. Effects of central nervous system polypharmacy on falls liability in community-dwelling elderly. Gerontology. 1998;44(4): 217–221. doi: 10.1159/000022013 [DOI] [PubMed] [Google Scholar]
- 34.Barker W. Assessment and prevention of falls in older people. Nursing older people. 2014. 26(6). doi: 10.7748/nop.26.6.18.e586 [DOI] [PubMed] [Google Scholar]
- 35.Panel On Prevention Of Falls In Older Persons A G S A. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. Journal of the American Geriatrics Society. 2011;59(1): 148–157. doi: 10.1111/j.1532-5415.2010.03234.x [DOI] [PubMed] [Google Scholar]
- 36.Hewston P, Deshpande N. Fear of falling and balance confidence in older adults with type 2 diabetes mellitus: a scoping review. Canadian journal of diabetes. 2018;42(6): 664–670. doi: 10.1016/j.jcjd.2018.02.009 [DOI] [PubMed] [Google Scholar]
- 37.Cao WZ, Huang YY, Xi SX. Meta-analysis of risk factors for falls in elderly Chinese people. Nursing Research. 2018;32(20): 3222–3228. doi: 10.12102/j.issn.1009-6493.2018.20.016 [DOI] [Google Scholar]
- 38.Sun XY, He ZQ, Wang LQ, et al. Association between mild cognitive impairment and risk of falls in community-dwelling population aged 55 years and above. Chinese Journal of Disease Control and Prevention. 2020;24(02): 200–203. doi: 10.16462/j.cnki.zhjbkz.2020.02.015 [DOI] [Google Scholar]
- 39.Pandey M K, Karelia D, Amin S G. Gambogic acid and its role in chronic diseases. Anti-inflammatory Nutraceuticals and Chronic Diseases. 2016:375–395. doi: 10.1007/978-3-319-41334-1_15 [DOI] [PubMed] [Google Scholar]
- 40.Gell N M, Wallace R B, Lacroix A Z, et al. Mobility device use in older adults and incidence of falls and worry about falling: Findings from the 2011–2012 national health and aging trends study. Journal of the American Geriatrics Society. 2015;63(5): 853–859. doi: 10.1111/jgs.13393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang CH, Huang Y, Zang XL, et al. Application of intervention mapping in improving self-management abilities for fall prevention in elderly patients. International Journal of Nursing. 2016; 35(11): 1452–1455. doi: 10.3760/cma.j.issn.1673-4351.2016.11.004 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.