Abstract
Selective mutism (SM) is a relatively rare, but highly interfering, child anxiety disorder characterized by a consistent failure to speak in certain situations, despite demonstrating fluent speech in other contexts. Exposure-based cognitive behavioral therapy and Parent-Child Interaction Therapy adapted for SM can be effective, but the broad availability and accessibility of such specialty care options remains limited. Stay-at-home guidelines to mitigate the spread of COVID-19 further limited the accessibility of office-based specialty care for SM. Building on separate lines of research supporting intensive treatments and telehealth service delivery models, this paper is the first to describe the development, preliminary feasibility, acceptability, and efficacy of a Remote Intensive Group Behavioral Treatment (IGBT) for families of young children with SM (N=9). Treatment leveraged videoconferencing technology to deliver caregiver training sessions, lead-in sessions, 5 consecutive daily IGBT sessions, and an individualized caregiver coaching session. Remote IGBT was found to be both feasible and acceptable. All families (100%) completed diagnostic assessments and caregiver-report questionnaires at four major study timepoints (i.e., intake, pre-treatment, post-treatment, 4-month follow-up) and participated in all treatment components. Caregivers reported high treatment satisfaction at post-treatment and 4-month follow-up and low levels of burden associated with treatment participation at post-treatment. Approximately half of participating children were classified as treatment responders by independent evaluators at post-treatment and 4-month follow-up. Although these pilot results should be interpreted with caution, the present work underscores the potential utility of using videoconferencing to remotely deliver IGBT to families in their natural environments.
Keywords: child anxiety, selective mutism, intensive treatment, telehealth, COVID-19
Selective mutism (SM) is an anxiety disorder characterized by a child’s consistent failure to speak in certain situations, despite demonstrating fluent speech in other contexts (American Psychiatric Association, 2013). Notably, although SM symptoms can be highly debilitating and impair educational, occupational, and/or social development, research on the disorder is still relatively limited. This may be due, in part, to the relatively rare nature of SM, with prevalence rates ranging from 0.71 to 2%, though higher rates have been reported among immigrant and/or bilingual children (Bergman et al., 2002; Elizur & Perednik, 2003; Kumpulainen et al., 1998; Toppelberg et al., 2005). Nonetheless, general consensus that SM is an anxiety or fear-related disorder (American Psychiatric Association, 2013) is supported by both caregiver- and youth self-reports (Schwenk et al., 2019; Vogel et al., 2019). Additionally, youth with SM are frequently diagnosed with co-occurring anxiety disorders, including especially high rates of co-occurring social anxiety disorder, and often have parents with a history of social anxiety disorder themselves (Bögels et al., 2010; Chavira et al., 2007; Driessen et al., 2020). As such, well-established treatments for anxiety, including exposure-based cognitive-behavioral therapy (CBT; Comer et al., 2019; Higa-McMillan, 2016), seem to be particularly well-suited for addressing SM symptoms. Furthermore, SM is most often identified in early childhood (Viana et al., 2009) and consensus across the early child anxiety treatment literature highlights the critical importance of incorporating behavioral parenting interventions into the treatment of young children with anxiety (Comer et al., 2019). Indeed, several relatively recent clinical trials evaluating the efficacy of exposure-based CBT and/or Parent-Child Interaction Therapy (PCIT) adapted for SM have demonstrated efficacy in reducing SM symptoms (Bergman et al., 2013; Catchpole et al., 2019; Cornacchio et al., 2019; Oerbeck et al., 2014; Zakszeski & DuPaul, 2017).
Unfortunately, the broad availability and accessibility of supported treatments for SM remains limited, as is typically the case for low base rate mental health disorders (Comer & Barlow, 2014). Professional workforce shortages, as well as the clustering of specialty care providers and services within metropolitan areas and academic hubs, present particularly pronounced barriers for families of youth with SM (Health Resources and Services Administration, 2013; Merwin et al., 2006; Morse et al., 2012; Reschovsky & Staiti, 2003; Turner et al., 2020). Geographical disparities in treatment availability, as well as the field’s predominant reliance on traditional treatment formats/models—e.g., weekly, individual, clinic-based service delivery—further compound problems with the availability of care (Comer & Barlow, 2014; Kazdin & Blase, 2011; Ollendick et al., 2018). Thus, expanding access to treatment through alternative and/or innovative formats is critical, particularly for youth with low base rate problems and conditions requiring specialty providers (Comer & Barlow, 2014).
To this end, specialty programs have increasingly offered intensive treatment options, designed to provide a full course of treatment via massed sessions over a condensed period of time (Öst & Ollendick, 2017). Intensive treatments can improve the accessibility and availability of care by offering new options to families who lack evidence-based specialty care in their regions, face logistical barriers to participating in traditional, weekly treatment sessions, or whose preference and/or needs suggests a treatment course that includes a high loading dose. Intensive treatments demonstrate efficacy across a range of youth psychopathologies, including SM (Angelosante et al., 2009; Cornacchio et al., 2019; Elkins et al., 2016; Flancbaum et al., 2011; Gallo et al., 2013; Ollendick & Davis, 2013; Öst & Ollendick, 2017; Santucci & Ehrenreich-May, 2013; Storch et al., 2007). Additionally, by simulating naturalistic settings (e.g., classroom environments, recreational activities), intensive treatments can improve upon the ecological validity of care, promote child and caregiver skill acquisition that is more generalizable to daily life, and in turn may more readily promote the maintenance of treatment gains. Nonetheless, the great distance families must travel and the additional costs associated with intensive treatment participation (e.g., travel, lodging) may preclude many families from participating (Ollendick et al., 2018). Innovations that can expand the reach and scope of intensive treatments by delivering services in alternative, nontraditional formats are needed, particularly to facilitate equitable access to services for marginalized populations often underrepresented in intensive treatment studies (Ollendick et al., 2018).
A parallel line of research increasingly suggests that telehealth formats can transcend the traditional barriers that interfere with established treatments reaching families in need through the use of remote technologies (e.g., videoconferencing; Comer & Barlow, 2014; Comer et al., 2015; Doss et al., 2017; Grist et al., 2019). Telehealth formats allow mental health specialists to deliver real-time behavioral interventions to families directly in the very settings in which youth demonstrate the greatest impairment (e.g., homes, schools, communities) and clinical trials examining videoconferencing-based treatments delivering care to naturalistic settings have demonstrated success with regard to feasibility, client satisfaction, efficacy, and maintenance (Carpenter et al., 2018; Comer et al., 2014; Comer et al., 2021; Comer, Furr, Kerns et al., 2017; Comer, Furr, Miguel et al., 2017; Hilty et al., 2013; Nelson et al., 2003). In fact, findings suggest that leveraging videoconferencing to treat families directly in natural settings may enhance EBT potency for some (see also Comer & Timmons, 2019).
Nonetheless, despite the promise of remotely delivered treatments, prior to the COVID-19 pandemic, telehealth approaches were rarely used in mainstream clinical practice (American Well, 2019). However, mass calls for social/physical distancing measures and national stay-at-home mandates following the onset of the pandemic necessitated a rapid transition to engaging with educational, occupational, social, and healthcare-related activities remotely (U.S. Department of Health & Human Services, 2020; Centers for Medicare & Medicaid Services, 2020). Fortunately, many youth programs were able to successfully transition to delivering services remotely (Barney et al., 2020; Nicholas et al., 2021; Sharma et al., 2020), patients and providers reported feeling substantially more comfortable with and accepting of telehealth services than they were previously, and psychologists intend to continue delivering telehealth services following the pandemic (Pierce et al., 2021; Sammons et al., 2020).
The need to both maintain and enhance access to treatment for anxious youth—especially those with SM and social anxiety—has been particularly pressing given the extent to which social distancing measures can reinforce patterns of anxious avoidance in the absence of continued exposure to feared stimuli (Khan et al., 2021). For this population, utilizing remote treatment formats that deliver services directly to these children within their home environments and with the support of caregivers—which are arguably the most familiar environments and people with which they interact—may present unique advantages to reach more families and enhance treatment success. Given existing evidence supporting the efficacy of telehealth formats of family-based CBT and PCIT for early childhood populations (Comer, Furr, Kerns et al., 2017; Comer, Furr, Miguel et al., 2017; Comer et al., 2021), clinicians have been encouraged to use internet-delivered PCIT (iPCIT) to address a broad range of child mental health difficulties during the COVID-19 pandemic (Gurwitch et al., 2020).
Moreover, delivering treatment in group-based formats aligns well with both the overall goals of increasing social communication behaviors and social interaction opportunities among youth with SM and social anxiety. Group-based treatment programs offer within-treatment opportunities for youth to not only interact on a 1:1 basis with a greater number of peers, but to also practice engaging in social interactions in groups of varying sizes that mimic common situations children face in school and community settings (e.g., working collaboratively within a small group for a class assignment, playing a competitive/team-based game, giving a presentation to a larger audience). Moreover, group formats partially help overcome challenges presented by professional workforce shortages, geographical disparities in the availability of specialty care, and the higher costs associated with individual care. Additionally, many group-based treatment programs are led by licensed professionals and supported by trainees, allowing the ratio of clinicians to participating families to remain high, while reducing the burden on individual licensed/specialty care providers.
Taken together, a remotely-delivered intensive group behavioral treatment program for families of children with SM may facilitate treatment engagement and progress by (a) eliminating barriers to in-person treatment participation; (b) delivering treatment within natural environments (i.e., the home); (c) involving familiar individuals (i.e., caregivers) in treatment and promoting caregivers’ implementation of treatment-related strategies; (d) enabling children to engage in more gradual exposure to novel contexts and people via audio and webcam features as opposed to more flooded exposures inherent in face-to-face, in-person treatment; and (e) offering a greater number and variety of opportunities to engage in social communication behaviors in individual and group situations. A telehealth service delivery model of intensive group behavioral treatment may also help promote the maintenance of gains and support the generalization of skills to natural settings following treatment participation. This paper describes a remote intensive group behavioral treatment (i.e., Remote IGBT) for SM delivered via telehealth and presents the initial feasibility, acceptability, and efficacy of this program for families of children with SM (N=9).
Method
Participants
Prior to the onset of the COVID-19 pandemic, participants (N=20 children and their primary caregivers) were recruited and scheduled to participate in research on an in-person IGBT in the summer, followed by telehealth booster treatment sessions in the fall. Families were eligible to participate if: (a) their child was between the ages of 4–10 years; (b) their child met DSM-5 criteria for a diagnosis of SM; (c) their child spoke English fluently and the caregiver(s) spoke English or Spanish fluently; and (d) they had access to a computing device, smartphone, or equivalent device. Families were excluded if: (a) their child was identified as having any psychiatric condition significantly more impairing than SM that required urgent alternate care; and/or (b) their child was nonverbal with all caregivers.
Approximately three months prior to the start of the treatment program, it became clear that the pandemic may interfere with the ability to hold an in-person IGBT. Research team members corresponded with enrolled families via telephone and email to share information and solicit feedback regarding potential revisions to the study design due to COVID-19-related restrictions. Approximately two months prior to the start of the treatment program, families were provided with concrete information regarding the revised program and study procedures (described below). Nine families (45%) expressed interest in participation and provided informed consent (and assent, if applicable) for the revised treatment and study procedures. Of the 11 families who chose not to enroll their children in the Remote IGBT, all but one family stated their preference for in-person services and/or interest in being placed on a waitlist for the following year in hopes that pandemic-related circumstances would allow for the program to be held in-person again. Table 1 presents detailed sociodemographic and diagnostic information across the initial and revised study samples for comparative purposes.
Table 1.
Sociodemographic and diagnostic information for the initial and revised study samples.
| Initial Study Sample (N=20) | Non-retained Families (n=11) | Retained Families (n=9) | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| M | SD | M | SD | M | SD | |
| Child age | 5.96 | 1.39 | 5.89 | 1.38 | 6.05 | 1.49 |
| Average # of child diagnoses | 2.25 | 0.97 | 1.91 | 1.04 | 2.67 | 0.71 |
| CGAS Score | 48.95 | 5.80 | 50.73 | 5.87 | 46.78 | 5.21 |
| Distance (miles) | 333.76 | 441.68 | 349.47 | 492.95 | 314.61 | 398.53 |
|
| ||||||
| N | % | n | % | n | % | |
|
| ||||||
| Child SM Diagnosis | 20 | 100 | 11 | 100 | 9 | 100 |
| Child SocAD Diagnosis | 14 | 70 | 6 | 54.5 | 8 | 88.9 |
| Child Sex | ||||||
| Male | 8 | 40 | 4 | 36.4 | 4 | 44.4 |
| Female | 12 | 60 | 7 | 63.6 | 5 | 55.6 |
| Child Race | ||||||
| White | 11 | 55 | 6 | 54.5 | 5 | 55.6 |
| Black or African American | 3 | 15 | 1 | 9.1 | 2 | 22.2 |
| Asian | 4 | 20 | 3 | 27.3 | 1 | 11.1 |
| Biracial | 2 | 10 | 1 | 9.1 | 1 | 11.1 |
| Child Ethnicity | ||||||
| Hispanic/Latinx | 6 | 30 | 3 | 27.3 | 3 | 33.3 |
| Non-Hispanic/Latinx | 14 | 70 | 8 | 72.7 | 6 | 66.7 |
| Primary Caregiver Relationship | ||||||
| Biological mother | 17 | 85 | 9 | 81.8 | 8 | 88.9 |
| Biological father | 2 | 10 | 1 | 9.1 | 1 | 9.1 |
| Other | 1 | 5 | 1 | 9.1 | 0 | 0 |
| Primary Caregiver Education | ||||||
| Less than a Bachelor degree | 2 | 10 | 2 | 18.2 | 0 | 0 |
| Bachelor degree or higher | 18 | 90 | 9 | 81.8 | 9 | 100 |
| Income-to-Needs Ratio | ||||||
| Extreme poverty | 2 | 10 | 1 | 9.1 | 1 | 11.1 |
| Low-income | 4 | 20 | 1 | 9.1 | 3 | 33.3 |
| Adequate | 2 | 10 | 1 | 9.1 | 1 | 11.1 |
| Affluent | 12 | 60 | 8 | 72.7 | 4 | 55.6 |
Note: CGAS = Children’s Global Assessment Scale; SM = selective mutism; SocAD = social anxiety disorder.
The nine families retained in the study reported diverse sociodemographic characteristics. Children were primarily from racial/ethnic minority (67%) and varied socioeconomic backgrounds, with all primary caregivers having received Bachelor’s (77.8%) or graduate (22.2%) degrees of education and a fair proportion (44.4%) reporting an income-to-needs ratio in the low-income or extreme poverty ranges (United States Census Bureau, 2020; U.S. Department of Health & Human Services, 2020). The majority of families (67%) lived “out of town,” defined by a distance of > 45 miles—to estimate ≥ 1 hour drive—between the family’s residence and the clinic. Henceforth, “all families” refers to these nine families retained in the study.
Procedures
All procedures were approved by the Florida International University Institutional Review Board (IRB) and conducted remotely via telephone, a HIPAA-compliant videoconferencing platform (i.e., Zoom for Healthcare), and/or a secure, online data collection platform (i.e., REDCap).
Study recruitment and enrollment
Families were primarily recruited from the general clinic flow of families contacting the Florida International University clinic seeking services for their child’s anxiety and difficulty speaking in social situations. This recruitment strategy was supplemented by the distribution of recruitment flyers and email messages through mental health organization listservs. Families expressing interest in participation were contacted by staff to provide information about study procedures. Families expressing continued interest in study participation completed a brief phone screen to confirm preliminary eligibility. Prior to participating in study procedures, caregivers provided informed consent via REDCap. Children ages ≥ 7 years also provided assent via REDCap.
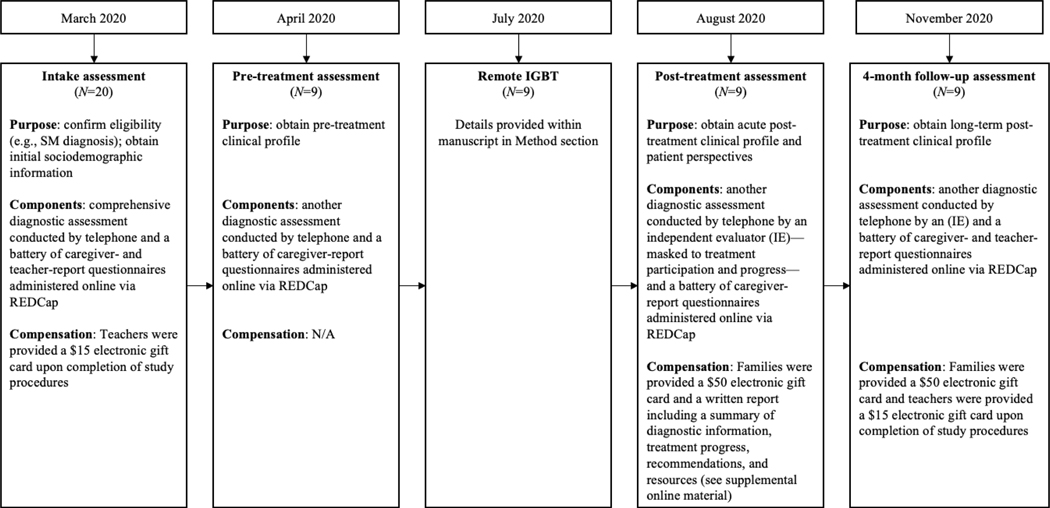
Assessment
Families participated in an intake assessment, a pre-treatment assessment, the Remote IGBT program, a post-treatment assessment, and a 4-month follow-up assessment. Figure 1 presents the general study timeline and corresponding details.
Figure 1.
Study timeline and details.
Note: teacher-report data are not presented within this paper due to concerns regarding the generalizability and interpretability of teacher-report questionnaires, as well as differences in virtual schooling experiences and school closures among our sample due to COVID-19
Remote IGBT program
Program description.
IGBT for SM includes an adaptation of PCIT for SM, which is informed by exposure-based CBT principles (e.g., shaping, fading, positive reinforcement, contingency management) and uses two specific treatment skill sets to increase child verbal and nonverbal participation in a variety of social situations (i.e., Child-Directed Interaction [CDI] and Verbal-Directed Interaction [VDI]; Furr et al., 2020). For more detailed information, the reader is referred to Lorenzo and colleagues (2020), who provide a full description of the content and procedures of in-person IGBT and to Cornacchio and colleagues (2019), who present results from a waitlist-controlled examination of the in-person IGBT for SM. Although efforts were made to replicate as much of the in-person IGBT as possible, numerous adaptations were necessary to accommodate the delivery of the Remote IGBT. First, unlike the in-person IGBT, all aspects of the Remote IGBT were conducted via telehealth through a HIPAA-compliant videoconferencing platform (i.e., Zoom for Healthcare), in accordance with consensus guidelines for telepsychotherapy (Joint Task Force for the Development of Telepsychology Guidelines for Psychologists, 2013; Myers et al., 2017). Secondly, program materials typically made available to families when they presented for treatment in-person needed to be shared with families to facilitate access from their home environments. Third, due to anticipated difficulty with “Zoom fatigue,” scheduling conflicts, time constraints, and increased reliance on caregiver participation during at least some treatment-related activities (e.g., lead-in sessions), the order and duration of child and caregiver components of the IGBT were modified. Specifically, instead of delivering caregiver training in the afternoons during the week of the Remote IGBT, this content was delivered to caregivers prior to participation in any treatment-related activities. Moreover, the duration of each child Remote IGBT daily session was reduced by approximately 50% (i.e., from 6 hours to 2.5–3 hours per day). Specific details about these and other adaptations, corresponding to (a) program materials; (b) caregiver training; (c) contingency management; (d) lead-in sessions; and (e) consecutive daily Remote IGBT sessions are described below.
Program materials.
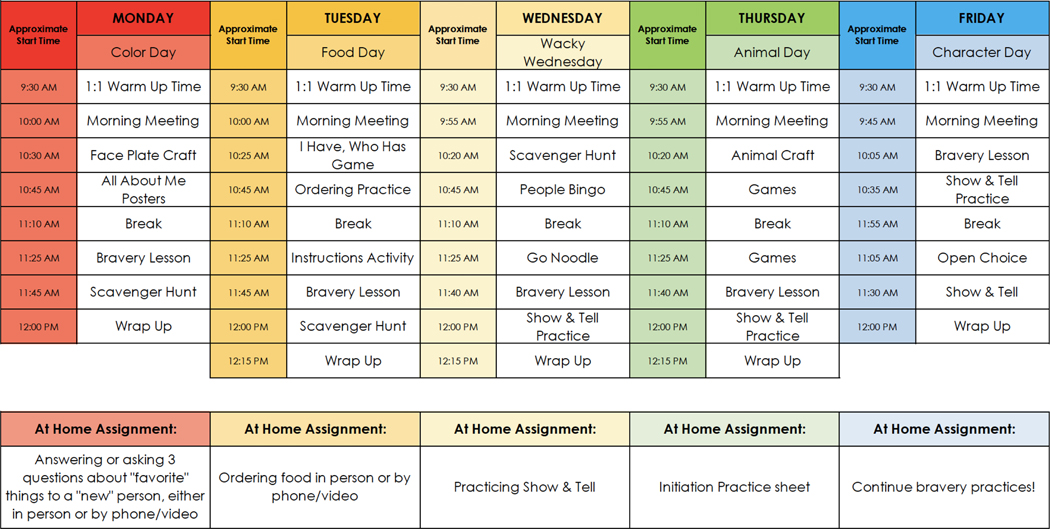
To reduce financial and/or resource barriers and facilitate participation in shared activities, in addition to using screensharing features within Zoom (e.g., drawing on a Whiteboard, playing online games), families were mailed a package of materials prior to the treatment program. This package included: (a) the schedule for consecutive daily Remote IGBT sessions (see Figure 2); (b) contingency management supplies (e.g., “Bravery Chart,” dry erase markers, small toys; described in further detail below); and (c) materials for various program activities (e.g., arts and crafts supplies, scavenger hunt clues, handouts). Materials and shipping costs averaged $30.79 per family and was paid for by the research team.
Figure 2.
Example schedule for the consecutive daily Remote IGBT sessions.
Caregiver training.
Providing caregivers with training opportunities through didactics and direct coaching experiences is a core component of the IGBT program, as transferring control to caregivers is considered a key driver of sustained progress in the context of family-based treatment of anxious youth (Silverman & Kurtines, 1996). As such, all primary caregivers participated in a 5-hour synchronous training series—offered across three 1–2 hour long sessions—prior to engaging in lead-in sessions. To facilitate caregiver attendance, two rounds of sessions were offered during the evening hours approximately one month prior to the Remote IGBT (i.e., week 1: Monday through Wednesday; week 2: Tuesday through Thursday). Although primary caregivers were required to attend sessions consecutively (i.e., attending session 1 prior to session 2), they were provided with flexibility across weeks (e.g., attendance at session 1 during week 1 and attendance at sessions 2 and 3 during week 2). Secondary caregivers were welcome, but not required to attend. The number of caregivers participating in each session varied, with caregivers from between three to eight families attending each session. Collectively, these sessions included introductions, psychoeducation regarding the nature and course of anxiety and SM, an overview of Remote IGBT procedures and activities, didactics related to treatment-related strategies, interactive role-plays, and open-ended discussion pertaining to generalizing treatment gains to community settings, with an emphasis on the school environment. As previously mentioned, this content was consistent with the 5-hours of didactics provided during the afternoons of the in-person IGBT, but was delivered prior to the Remote IGBT in order to prepare caregivers to engage in lead-in sessions (and daily Remote IGBT sessions, if needed).
Contingency management.
Consistent with the in-person IGBT (Cornacchio et al., 2019; Lorenzo et al., 2020), contingency management systems were utilized to reinforce children’s verbal and nonverbal participation throughout all treatment-related activities. To this end, each family was provided with a personalized, laminated “Bravery Chart,” designed to correspond to the child’s interests (e.g., using favorite colors/characters), which included a blank table of cells. Bravery Charts are used to monitor, reinforce, and reward child speech by placing a check mark in one of the cells each time the child spoke and providing the child with a “point” each time the entire chart was filled. Whereas “points” in the in-person IGBT are typically tracked by providing children with plastic tokens in the clinic setting, an online platform—ClassDojo—was used in the Remote IGBT. ClassDojo is a free and secure application often used in educational settings for behavioral management and home-school communication purposes. It has been shown to outperform paper/pencil methods for tracking child behavior and is particularly well-suited for virtual classroom environments, as it allows both individual (i.e., privately linked to the child/family’s account) and collective (i.e., representative of the full classroom) “points” to be viewed by both providers and families from their respective devices (see Krach et al., 2017 and Robacker et al., 2016). During the Remote IGBT, all clinical team members used “teacher” profiles, allowing them to view and provide individual and collective points. During individual and small group activities, each child’s assigned counselor monitored and provided points within ClassDojo on an individual basis, whereas just one counselor per classroom was assigned to monitor and provide points to all participating children during larger group activities (e.g., Morning Meetings, Bravery Lessons). At the end of each Remote IGBT session, children were able to exchange points for tangible rewards determined collaboratively between lead clinicians and families (e.g., from the set of small toys provided by the research team or other rewards provided by the family).
Lead-in sessions.
Families participated in individual lead-in sessions beginning one week prior to the first day of the Remote IGBT, with the exception of one family who participated in their first lead-in session approximately two weeks prior due to scheduling conflicts. Consistent with the in-person IGBT, lead-in sessions focused on familiarizing families with treatment-related strategies and fading in and promoting child speech with staff members using shaping procedures. During the in-person IGBT, clinicians utilize bug-in-the-ear technologies to coach caregivers in their use of treatment skills through a one-way mirror (see Furr et al., 2020), while fading in and promoting child speech with staff members. Ultimately, caregivers are faded out of the session (e.g., becoming gradually less involved in activities, exiting the room). However, instead of coaching caregivers through a one-way mirror, Remote IGBT lead-in sessions were set up similar to other behavioral parenting intervention sessions delivered via telehealth, whereby webcam devices are positioned to allow clinical team members to observe parent-child interactions remotely and headsets are used to communicate with caregivers discretely through bug-in-the-ear technologies (e.g., Bluetooth earpieces, headphones; see Comer et al., 2015; Gurwitch et al., 2020; Hong et al., 2019). This approach was useful for Remote IGBT lead-in sessions, as the clinical team members’ presence in session could be particularly subtle, and introduced even more gradually over time (e.g., turning on audio without video, turning on video without a clinical team member on screen).
During in-person lead-in sessions, children are required to speak directly to at least two staff members without caregivers present, as this level of independence is considered a prerequisite to prepare the child for successful engagement in the in-person IGBT during which caregivers are not present (Cornacchio et al., 2019; Lorenzo et al., 2020). However, given children would be participating in the Remote IGBT from their home environments and caregivers were expected to be readily available as needed (e.g., to resolve technological difficulties, to assist with verbal and nonverbal participation), the Remote IGBT lead-in criteria was adjusted to require the child to speak audibly in response to at least one staff member, with or without caregivers present. If and when time allowed, Remote IGBT lead-in sessions additionally targeted children’s nonverbal and verbal participation in the absence of caregivers, with peers (e.g., group-based lead-in sessions), and in the context of Remote IGBT activities. Therefore, similar to the in-person IGBT, even after children had met the criteria for participation, they often participated in at least one additional lead-in session. For contingency management purposes, caregivers were coached through use of the child’s Bravery Chart during initial lead-in sessions and ClassDojo was used during later lead-in sessions, particularly when involving peers.
Consecutive daily IGBT sessions.
Consistent with the in-person IGBT, the child treatment component of the Remote IGBT took place on 5 consecutive days and consisted of mostly group-based activities typical of an average school week (e.g., daily morning meetings, arts and crafts, recreational activities, group lessons; see Figure 2). Throughout each day, consistent with CBT principles, exposures to various school-like situations are conducted with children (e.g., asking for help, speaking to peers), with exposures becoming increasingly challenging throughout the week. Children were assigned to “classrooms” with like-age peers and a ≥ 1:1 counselor-child ratio (i.e., five families assigned to the “younger classroom” and four families assigned to the “older classroom”). Each Remote IGBT daily session was scheduled from 9:30AM to 12 or 12:30PM (i.e., 2.5–3 hours per day for a total of 12.5–15 hours), depending on the child’s age and developmental level. All families within each classroom logged in to the same session link at the start of the treatment day. The break out room feature of Zoom was used to separate children and counselors into various “rooms” during the initial warm-up period, as well as for small group activities and/or in the event a child was experiencing particular difficulty (e.g., expressing distress, communicating nonverbally). Break out rooms were also used to provide daily feedback on child progress and “at home assignment” reminders to caregivers during brief, individual “check-out” meetings at the end of each daily session. Such “at home assignments” included practice engaging in exposures focused on speaking to unfamiliar individuals, ordering food from a local restaurant, practicing show and tell presentations, and initating various conversational exchanges with others either in person or by phone/video (see Figure 2). Additionally, caregivers were provided access to daily progress notes uploaded to a secure cloud platform (i.e., OneDrive).
Individual caregiver coaching session.
Each family was also scheduled to participate in one hour-long in vivo caregiver coaching session during the afternoon of the second, third, or fourth day of the Remote IGBT program. Families were provided the option to engage in the individual caregiver coaching session from their homes and/or in the community (e.g., in-person or virtual playdates, school playgrounds, restaurants, retail locations). The content, location, and target(s) of this coaching session were tailored to the convenience and priorities of each family (e.g., exposures with people from various age ranges, levels of familiarity, across activities simulating various contexts), in addition to considering their comfort level interacting with others in person and/or in public settings given unique considerations during the COVID-19 pandemic. Similar to the in vivo coaching occurring during lead-in sessions, caregivers utilized devices to facilitate observation via webcam and headsets for communication purposes. All coaching sessions included collaborative planning with caregivers regarding the specific exposure(s) for the child to engage in, supporting caregivers in introducing the exposure practice(s) and associated reward to the child, as well as in vivo coaching of treatment-related skills to facilitate the child’s verbalizations with others throughout the session.
Clinical team and training
Consistent with the in-person IGBT, the clinical team included supervisors/directors, masters-level lead clinicians, and multiple undergraduate, post-baccalaureate, or masters-level counselors (e.g., psychology or professional counseling degrees; Cornacchio et al., 2019; Lorenzo et al., 2020). The Remote IGBT directors/supervisors included one licensed clinical psychologist who supervised all Remote IGBT activities, as well as one masters-level clinician per classroom who provided supervision and consultation to the lead clinicians. The Remote IGBT director, supervisors, and lead clinicians all had previous experience leading activities during in-person IGBTs and led caregiver and counselor training sessions (described below). Lead clinicians were assigned as the primary point of contact for one to two families and multiple counselors for one of the Remote IGBT classrooms (i.e., three lead clinicians within the younger classroom; two lead clinicians within the older classroom). Lead clinicians were responsible for conducting lead-in sessions, leading classroom activities during daily sessions, engaging in brief daily caregiver check out meetings, providing individual feedback to counselors, and conducting caregiver coaching sessions for each of their assigned families. Remote IGBT counselors (i.e., five per classroom) were paired with an individual family for lead-in sessions and with a different child during each of the consecutive daily sessions. Counselors were responsible for engaging children individually during initial warm-up periods and small group activities and informed daily feedback and progress notes. In the event a child was experiencing difficulty during Remote IGBT sessions, lead clinicians worked collaboratively with counselors to problem-solve situations and promote child success (e.g., determining whether to utilize a break out room or to engage caregivers).
All clinical team members participated in at least 12-hours of training prior to assisting with the Remote IGBT. Counselors first completed an asynchronous online training course related to SM treatment-related skills (Selective Mutism University, 2021) and subsequently attended a 10-hour synchronous training series—offered across three consecutive daily 3–4 hour long sessions. Counselor training included introductions, an overview of Remote IGBT procedures and activities, didactics related to the remote delivery service model and treatment-related strategies, interactive role-plays, and an individual behavioral observation of each lead clinician and counselor to confirm proficiency in treatment-related skills (consistent with fidelity checks described in Cornacchio et al., 2019). Counselors also attended a 2-hour intensive group behavioral “booster” treatment session for existing SM patients. This 2-hour session involved several activities included in the Remote IGBT program schedule and provided counselors with the opportunity to practice using treatment-related skills through the videoconferencing platform.
Measures
Diagnostic profile
Child diagnostic profiles were obtained via the Anxiety Diagnostic Interview Schedule – Parent Version (ADIS-IV-P; Silverman & Albano, 1996) administered by independent evaluators (IEs). The ADIS-IV-P is a well-supported semi-structured diagnostic interview assessing child mental health disorders via caregiver-report. Disorders were assigned a clinical severity rating (CSR) along a 9-point scale ranging from 0 (no symptoms) to 8 (extremely severe symptoms), with CSRs ≥ 4 indicating that diagnostic criteria in accordance with the DSM-5 were met. The ADIS-IV-P was administered in its entirety at intake. Modules receiving a CSR of > 0 at intake were re-administered at all subsequent assessment timepoints. All IEs met research reliability criteria (i.e., matching diagnostic profiles with more senior evaluators on three out of five consecutive assessments) prior to independently conducting assessments for this study. IEs reviewed and collaboratively developed diagnoses and ratings for each participant at each timepoint with a masked study supervisor. Clinic reliability checks on ADIS assessments yielded high interrater reliability (κ > .80). Consistent with other SM research (e.g., Cornacchio et al., 2019), child interviews were not conducted given that youth in this early childhood age range may be unable to provide reliable and/or valid self-report of symptoms and warnings about the potential consequences of initiating a clinical interview with a child with SM who is unlikely to speak to an unfamiliar adult (see Furr et al., 2020).
Treatment response
Child response to treatment was measured via the Clinical Global Impressions – Improvement scale (CGI-I; Guy & Bonato, 1970). The CGI-I is a widely used clinician-rated scale assessing treatment-related change from 1 (very much improved) to 7 (very much worse), with 4 indicating “no change.” For the present study, treatment response was dichotomized such that children receiving CGI-I scores of 1 (very much improved) or 2 (much improved) were considered “treatment responders” and those receiving CGI-I scores of 3 (minimally improved) or higher were considered “treatment nonresponders.” The CGI-I was rated by IEs following administration of the ADIS-IV-P at post-treatment and 4-month follow-up and reflect improvement relative to pre-treatment SM and social anxiety symptomatology.
Global Functioning
Overall child functioning was measured via the Children’s Global Assessment Scale (CGAS; Shaffer et al., 1983). The CGAS is a commonly used clinician-rated measure of global functioning in youth ranging from 0–100, with higher scores representing greater overall functioning and less overall impairment. The CGAS was rated by IEs following the diagnostic assessment at all timepoints.
SM symptoms
The Selective Mutism Questionnaire (SMQ; Bergman et al., 2008) is a 17-item caregiver-report questionnaire assessing child speech across various contexts. Items are rated on a 4-point Likert scale ranging from 0 (never) to 3 (always) and correspond to three subscales (i.e., Home, School, Public/Social). Subscale scores reflect an average of item responses and therefore also range from 0 to 3, with higher scores indicating more frequent speech within each domain. The SMQ has demonstrated good psychometric properties and has been shown to be sensitive to treatment-related change (Bergman et al., 2013; Bergman et al., 2008). The Frankfurt Scale of Selective Mutism (FSSM; Gensthaler et al., 2020) is a caregiver-report questionnaire assessing SM in youth, comprised of diagnostic and severity scales corresponding to age-specific measures (e.g., for ages 3–7 years up to kindergarten; for ages 6–11 in 1st grade or above). The diagnostic scale was used in the present study. This scale includes 10 items rated 0 (no) or 1 (yes) for both age ranges, with higher scores corresponding to more SM behaviors. The FSSM has demonstrated good psychometric properties and diagnostic accuracy (Gensthaler et al., 2020). The SMQ and FSSM diagnostic scale were administered at all assessment timepoints, with the exception of the SMQ – School subscale at post-treatment, as children were not attending school in the summer months.
Anxiety symptoms
Overall anxiety symptoms were measured via the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2000; Achenbach & Rescorla, 2001). The CBCL is a widely used caregiver-report questionnaire consisting of 99- and 120-items (for ages 1.5–5 and 6–18 years, respectively), assessing a broad range of behavioral and emotional problems in youth. Items are rated on a 3-point Likert scale ranging from 0 (not true) to 2 (very true or often true). Subscale scores are normed by age and gender and yield T Scores corresponding to a variety of domains. For the present study, the CBCL Anxiety Problems subscale T Scores were used to measure overall anxiety symptoms at all assessment timepoints.
Previous videoconferencing experience
Previous videoconferencing experience was measured using a single item from the Technological Ease and Computer-based Habits Inventory (TECHI; Comer & Bry, 2021). Caregivers were asked to rate the degree to which they agreed with the following statement: “I regularly use Skype or another videoconferencing service.” The item was rated on a 6-point Likert scale, ranging from 0 (“strongly disagree”) to 5 (“strongly agree”). This item was administered during the pre-treatment assessment.
Treatment participation
Caregiver and child participation in treatment was measured via standardized session progress notes. Progress notes included information about the family’s attendance, participation, and individualized targets. Progress notes were completed by clinical team members following each program session (i.e., caregiver training, lead-ins, Remote IGBT, caregiver coaching).
Perspectives on treatment experiences
Caregiver satisfaction with treatment was measured via the Client Satisfaction Questionnaire-8 (Larsen et al., 1979). The CSQ-8 is a patient/caregiver-report questionnaire containing 8-items, each rated on a 4-point Likert scale. Scores range from 8 to 32, with higher scores indicating greater treatment satisfaction. The CSQ-8 has demonstrated good psychometric properties and has been used to measure caregiver satisfaction with child treatment in other early child SM treatment research (e.g., Cornacchio et al., 2019). The CSQ-8 was administered to caregivers at post-treatment and 4-month follow-up.
The overall burden associated with participating in the Remote IGBT was assessed using the Burden of Treatment Participation (BTP) Scale, a caregiver-report measure developed for the present study. The BTP includes 10 items rated on a 5-point Likert scale ranging from 0 (strongly disagree) to 4 (strongly agree). Scores range from 0 to 40, with higher scores indicating greater burden (i.e., scores from 0–13 reflect “low” burden; scores from 14–27 reflect “medium” burden; scores from 28–40 reflect “high” burden). Example items include, “The time(s) when this treatment program was offered were not ideal for my family,” and “Participating in this treatment program required too much time from my family”. The BTP was administered at post-treatment.
Caregiver strategy use
Caregivers were also prompted to report the frequency with which they used treatment-related strategies following program completion. Specifically, caregivers were asked: (1) “On average per week, how often did you spend 5 minutes of Child-Directed Interaction (CDI) ‘special time’ with your child since your last study assessment?” (i.e., “CDI time”) and (2) “On average per week, how often did you lead your child through ‘bravery practices’ using verbal-directed interaction skills, exposure, and shaping strategies?” (i.e., “exposure practices”). Items were rated on a 5-point Likert-scale that ranged from 0 (never) to 4 (daily). Caregiver strategy use was measured at post-treatment and 4-month follow-up.
Teacher-report questionnaires
As noted in Figure 1, teacher-report questionnaires were administered as part of the intake and 4-month follow-up assessments. However, these data are not presented within this paper due to concerns regarding the generalizability and interpretability of teacher-report questionnaires, as well as differences in virtual schooling experiences and school closures among our sample due to COVID-19. Specifically, social/physical distancing measures and national stay-at-home guidelines led to many school closures that overlapped with intake assessments (i.e., in March 2020) and youth participating in the study were engaged in a range of fully virtual, hybrid, and/or in-person schooling experiences at the time of the 4-month follow-up (i.e., in November 2020).
Results
Feasibility and Acceptability
Completion rates
All families (100%) completed all study assessments at all timepoints. The vast majority of teachers completed study questionnaires at intake (88.9%) and 4-month follow-up (77.8%; one family requested the research team not send questionnaires to their child’s teacher).
Primary caregivers for all families (100%) attended the full 5-hour caregiver training series. All children (100%) successfully met lead-in criteria to participate in the Remote IGBT within 2 sessions, with the majority (77.8%) meeting criteria within 1 lead-in session. On average, families participated in a total of 2 lead-in sessions (M=2.22 sessions; SD=.44 sessions), to increase peer interaction after meeting criteria to participate in the Remote IGBT. Lead-in sessions lasted no longer than 2.5 hours per session (M=1.72 hours; SD=.41 hours). All children (100%) logged in to Remote IGBT sessions within 6 minutes of the start time and attended the full IGBT session each day of the program. Some of the caregivers of children in the younger classroom (i.e., caregivers of 2 or 3 children per day) were involved in at least 50% of daily sessions to assist with sustained attention and/or engagement, whereas none of the caregivers of children in the older classroom required such assistance from caregivers. All families (100%) participated in one caregiver coaching session during the Remote IGBT week (M=1.17 hours; SD=.47 hours). Although families were provided the option to engage in the individual caregiver coaching session from a community/public setting, all families (100%) opted to participate from their homes and those involved in exposures (e.g., extended family members, peers from school, unfamiliar adults) joined sessions remotely. Nonetheless, caregiver coaching sessions specifically focused on guiding caregivers through leading their children through exposures targeting speech and social interactions with others through asking and responding to questions, engaging in scavenger hunts, presenting a show and tell performance, simulated practice ordering from a restaurant, and advocating for oneself (e.g., correcting someone if/when they misunderstand the child).
Perspectives on treatment experiences
Participating families were relatively familiar with videoconferencing prior to engaging in Remote IGBT components. At pre-treatment, caregivers reported regular use of videoconferencing services, with the majority (77.8%) reporting they agree or strongly agree with the statement, “I regularly use Skype or another videoconferencing service.”
Caregivers reported high levels of treatment satisfaction on the CSQ-8 at post-treatment (M=29.00; SD=2.83) and 4-month follow-up (M=29.78; SD=2.17). Overall, caregivers reported low levels of burden associated with participation on the BTP at post-treatment (Range=0–23; M=9.56; SD=9.22).
Treatment Outcomes
IE ratings
At post-treatment, 55.6% of children (n=5) were classified as at least minimally improved by IEs on the CGI-I, with 44.4% (n=4) classified as “treatment responders.” By the 4-month follow-up, 66.7% (n=6) of children were classified as at least minimally improved by IEs on the CGI-I, with 44.4% (n=4) still classified as “treatment responders.” Paired-samples t-tests used to examine IE ratings of child global functioning on the CGAS across time showed that scores significantly increased from pre-treatment (M=49.11; SD=4.04) to post-treatment (M=54.22; SD=3.87), t(8)=3.707, p<.05, as well as from pre-treatment to 4-month follow-up (M=59.11; SD=11.98), t(8)=3.08, p<.05, indicating treated children displayed significant improvements in overall functioning.
Caregiver-report
Caregiver ratings of child SM and overall anxiety symptoms remained relatively stable across assessment timepoints. At pre-treatment, SMQ subscale scores were comparable to norms reflecting other clinical SM samples and substantially lower (reflecting less frequent speech) than non-SM samples (Bergman et al., 2008). Across time, caregiver ratings demonstrated modest increases on the SMQ subscale scores (indicating more frequent speech), decreases on the FSSM diagnostic scale (indicating fewer SM behaviors), and decreases in CBCL Anxiety Problems T Scores at post-treatment and 4-month follow-up relative to pre-treatment. Paired-samples t-tests used to examine caregiver ratings of child SM and overall anxiety symptoms across time showed that mean differences in scores did not reach significance. Following program completion, caregivers reported engaging in CDI time and exposure practices with their children on an average of 1–4 days per week at post-treatment and 4-month follow-up. These data are presented in Table 2.
Table 2.
Caregiver-report across study assessments.
| Pre-treatment | Post-treatment | 4-month follow-up | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| M | SD | M | SD | M | SD | ||
| SMQ | School | 0.52 | 0.52 | N/A | N/A | 1.21 | 0.91 |
| Home | 2.03 | 0.63 | 2.3 | 0.37 | 2.32 | 0.64 | |
| Public | 0.53 | 0.38 | 0.93 | 0.64 | 1.01 | 0.8 | |
| FSSM | Diagnostic Scale | 8.22 | 1.48 | 7.11 | 2.67 | 7.11 | 3.55 |
| CBCL | Anxiety Problems | 58.22 | 9.19 | 55.56 | 8.96 | 55.22 | 7.87 |
| Caregiver Strategy Use | CDI Time | N/A | N/A | 2.11 | 1.45 | 2.11 | 1.69 |
| Exposure Practices | N/A | N/A | 2.56 | 1.51 | 2.11 | 1.54 | |
Note: SMQ = Selective Mutism Questionnaire; FSSM = Frankfurt Scale of Selective Mutism; CBCL = Child Behavior Checklist; CDI = Child-Directed Interaction.
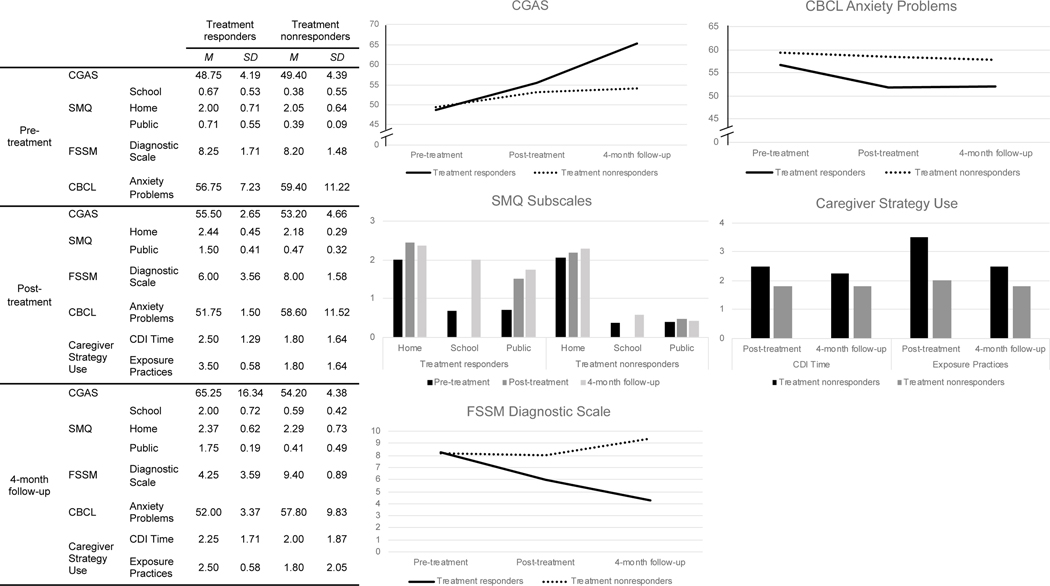
Descriptive comparisons between 4-month follow-up treatment responders and nonresponders
Although the present sample size precludes the opportunity to conduct appropriately powered moderation analyses, youth ultimately classified as treatment nonresponders at the 4-month follow-up appear to have displayed somewhat higher rates of pre-treatment SM impairment and overall anxiety symptoms than treatment responders. However, there were no notable demographic differences found between groups. Comparing longitudinal trajectories among families classified as treatment responders versus treatment nonresponders at 4-month follow-up showed several expected patterns of scores. As shown in Figure 3, relative to treatment nonresponders, treatment responders displayed greater pre- to post-treatment increases in public speech on the SMQ, decreases in diagnostic scale scores on the FSSM, and decreases in anxiety problems on the CBCL. Moreover, in addition to maintaining relative improvements in public speech and anxiety problems, treatment responders also displayed greater improvements in global functioning on the CGAS, increases in school-based speech on the SMQ, and further decreases in diagnostic scale scores on the FSSM than treatment nonresponders at the 4-month follow-up. Notably, caregivers of children classified as treatment responders also reported higher average weekly engagement in CDI time and exposure practices with their children at both post-treatment and 4-month follow up, as compared to caregivers of children classified as treatment nonresponders. Overall, those classified as treatment nonresponders appeared to display very little change across subscales of the SMQ, in global functioning on the CGAS, and in anxiety problems on the CBCL. These children demonstrated increases in diagnostic scale scores on the FSSM from pre-treatment to 4-month follow-up.
Figure 3.
Comparisons between 4-month follow-up treatment responders and nonresponders.
Note: CGAS = Children’s Global Assessment Scale; FSSM = Frankfurt Scale of Selective Mutism; CBCL = Child Behavior Checklist; SMQ = Selective Mutism Questionnaire.
Discussion
Longstanding problems with the broad availability and accessibility of specialty care for SM were further compounded by barriers to in-person service utilization presented by the COVID-19 pandemic. Although pandemic-related stay-at-home guidelines and social distancing mandates served as the initial catalyst for developing and evaluating this particular Remote IGBT, many concerns about the accessibility of in-person intensive treatment options were present prior to the pandemic (e.g., disparities in access to intensive treatment options, associated travel and lodging costs). Although providing treatment in intensive doses may overcome some barriers to care, this treatment format demands a great deal of time and resources from families and the vast majority who travel from out-of-state to access such services come from predominantly White, highly-educated, dual-caregiver homes (Ollendick et al., 2018). Though gaps in Internet accessibility persist for many families living in rural areas and/or from lower-income brackets, access to and use of technology has increased substantially throughout the past several decades, particularly among these underserved groups (Pew Research Center, 2019a; Pew Research Center, 2019b). Accordingly, remotely delivered treatment formats may improve accessibility to specialty care for many underserved families, though more work is needed to better understand how technology can promote mental health service equity. Aligned with calls to adapt services to reach families in need during the COVID-19 pandemic, this paper is the first to describe the preliminary feasibility, acceptability, and efficacy of a Remote IGBT program delivered through telehealth to families of children with SM.
With regard to the program’s feasibility and acceptability, results show that a diverse set of families were interested in participating in the Remote IGBT. Participating families were from a range of ethnic, racial, and socioeconomic backgrounds, with nearly half of participating families identified as having children from racial/ethnic minority and low income-to-needs ratios. There were no differences across families with regard to program completion. All families who consented to participate in the Remote IGBT completed all treatment components and assessments. Moreover, caregivers reported high levels of treatment satisfaction and low levels of burden associated with Remote IGBT participation, highlighting the program’s overall acceptability. These findings may provide preliminary evidence that a Remote IGBT is able to reach more underserved children than traditional in-person intensive treatment options.
Additionally, despite reducing the hours of treatment delivered each day by nearly 50% relative to the in-person IGBT, family outcomes from the Remote IGBT are promising, and do not suggest a dropoff in efficacy relative to the in-person IGBT. Immediately following the Remote IGBT, almost half of participating children were classified as treatment responders, with a larger proportion of children classified as at least “minimally improved,” at both post-treatment and 4-month follow-up. These acute outcomes are roughly comparable to the 50% treatment response observed at post-treatment for in-person IGBT (Cornacchio et al., 2019). Consistent with IE ratings of treatment response, caregiver-report at the post-treatment and 4-month follow-up assessments showed greater decreases in SM and anxiety symptoms and related impairments for children classified as treatment responders at the 4-month follow-up relative to those classified as treatment nonresponders. These findings further demonstrate that the Remote IGBT may lead to both acute and long-term improvements for some, but not all youth.
Adapting in-person IGBT to a remote format brought with it creative modifications and unique features that may have enhanced a number of existing treatment components and facilitated post-treatment gains. For example, engaging families in initial lead-in sessions from their homes—using webcams and bug-in-the-ear coaching strategies—facilitated discrete communication with caregivers and especially gradual exposures relative to typical in-person procedures, where families are greeted by clinical team members upon arrival at the clinic and prompted to interact in a novel environment. Additionally, caregivers of children participating in the Remote IGBT were more likely to be exposed to daily treatment-related strategies and activities due to either (a) directly engaging in session content with their child, or (b) indirect exposure due to co-location while their child participated in treatment from the home environment. Thus, although the dose of child treatment was reduced in the Remote IGBT relative to the in-person IGBT, it is possible, if not likely, that caregivers received an increased dose of treatment due to heightened reliance on caregiver involvement in and/or indirect exposure to treatment-related activities and strategy use throughout the Remote IGBT. Providing caregivers with the opportunity to practice using treatment strategies within ecologically valid contexts (i.e., their own homes, with extended family members and/or individuals from one’s own local community) may have promoted the generalization and continuation of strategy use and/or increased caregivers’ self-efficacy in using treatment skills following the Remote IGBT. This, in turn, may have led to continued clinical gains, as caregiver self-efficacy in using treatment strategies is positively associated with child clinical outcomes (Albanese et al., 2019). Indeed, among families whose children were classified as treatment responders at the 4-month follow-up assessment, caregivers reported continuing to use treatment-related strategies on a more regular basis than families whose children were classified as treatment nonresponders. Future research should directly measure the extent to which caregivers are engaged in intensive treatments for youth with SM (e.g., observation, direct coaching), how regularly caregivers continue to utilize strategies following program completion, and how such varied levels of engagement relate to both caregivers’ self-efficacy and child outcomes.
Of note, given the pilot nature of this intervention program, there were several aspects of the Remote IGBT that serve as “lessons learned” and can inform the adaptation and implementation of future programs. First, reinforcement is a crucial element of motivating youth to participate in exposure-based CBT, but it is rare for one type of reinforcement to be equally motivating across all children in a given program. For example, whereas some children feel rewarded for their verbalizations when they receive stickers on their Bravery Chart, others may prefer discrete verbal praise (e.g., a counselor whispering, “nice job answering”) or more tangible strategies (e.g., providing a plastic token for each verbalization). Although a remote contingency management system was implemented to promote motivation and engagement throughout the program, clinical team members were limited in their ability to individualize reinforcement strategies to ensure they were optimally impactful. Furthermore, it is worth considering how the “dose” of treatment may have been affected by the reduced capacity to provide individualized attention to children during group activities. Specifically, opportunities to engage in more subtle scaffolding (e.g., a counselor whispering a question to a child during a larger group activity to promote participation) and reinforcement (e.g., praising appropriate behavior and verbalization) were constrained within the remote context, as the platform typically only emitted sound from one speaker at a time. Thus, multiple people speaking at the same time introduced challenges to the flow of conversation, which limited some of the common strategies used by counselors to provide individualized, intermittent attention to children during group activities during the in-person IGBT.
To address these potential limitations, future clinical applications of Remote IGBT for SM may consider including more variable contingency management systems (e.g., check charts, coins, stickers) that provide families and clinicians with greater flexibility to personalize approaches and/or make alternative strategies available should a given system lose its potency. Moreover, future program schedules may do well to strategically organize activities such that children alternate between group activities and periodic opportunities to receive more individualized attention from counselors. Such organization may not only provide youth with opportunities to engage in a variety of exposures, but also function as a structured method of providing frequent and consistent individualized reinforcement for approach-oriented behaviors.
Although the current study demonstrated a number of positive outcomes for participating children and families and helpful considerations for future practice, several limitations warrant discussion. First, this pilot study included a relatively small sample of nine families who were all willing to participate in videoconferencing-based treatment services, whereas 11 families chose not to enroll their children in the Remote IGBT. At that time (May 2020), almost all of the families who chose not to participate in the Remote IGBT expressed a preference for in-person services. Although research indicates that, by six months into the pandemic, the perceived acceptability of telehealth services dramatically improved across patients and providers (Pierce et al., 2021; Sammons et al., 2020), the present study did not collect follow-up data from the non-participating families about how they felt about their decision and/or whether they would be more or less willing to participate in a Remote IGBT in the future. Moreover, although the majority of youth in the present sample were from racial and/or ethnic minority backgrounds, the small sample size hinders the ability to generalize findings to the broader SM community, and the absence of a control group precludes the ability to isolate treatment effects or examine mechanistic or moderating factors that may have influenced treatment outcomes. The results of the present study should also be interpreted through the lens of the COVID-19 pandemic. It is possible that families may have been more or less likely to participate in and/or find the Remote IGBT acceptable under different circumstances. Additionally, the COVID-19 pandemic limited many opportunities for families to engage in typical activities (e.g., attending school in-person, engaging in recreational activities, visiting with family members, scheduling playdates), which made it particularly challenging to draw conclusions about how observable improvements in child speech demonstrated during the Remote IGBT could generalize to “every day life.” Given variability in child interactions with teachers and experiences with remote schooling, data collected from teacher-report questionnaires were not included in the present study. However, given many youth with SM present with the greatest difficulty speaking within the school setting, teacher-report is often critical to measuring child outcomes following SM treatment. Taken together, unique circumstances tied to the COVID-19 pandemic may render caregiver-report of SM symptoms unreliable due to limited opportunities to observe their child in social situations, though caregiver bias could have gone in either direction (i.e., overreporting progress due to limited exposure to distressing situations and/or underreporting progress given limited opportunities to observe the child demonstrating treatment gains in naturalistic settings).
Overall, these pilot findings indicate that a remote service delivery model of intensive treatment is feasible, acceptable, and possibly efficacious for families of children with SM, showing that IGBT holds promise for families of children with SM, even if they are unable to participate in treatment in person. Favorable caregiver feedback and positive child outcomes underscore the need for future work examining the efficacy of the Remote IGBT in larger samples and using randomized-controlled trial designs to directly compare outcomes from the Remote IGBT to the in-person IGBT and supported weekly services. Although the present findings are encouraging, research examining which children benefit most from which different modalities of supported SM treatments, and the extent to which additional treatment (e.g., number of hours per day and/or consecutive days of treatment) leads to further improvements, will be particularly useful for clinical decision-making and the tailoring of treatments to individual families. Additionally, future work should seek to develop a more comprehensive understanding of the extent innovative service delivery models that have the potential to reach traditionally underserved, marginalized communities actually do so—e.g., examining whether using telehealth leads to reaching more families from the same sociodemographic backgrounds as those who typically receive in-person services or other families for whom supported treatments typically fail to reach. Such research is critical to promote more equitable access to mental health services. That said, the present work offers a key step forward in efforts to expand the portfolio of treatment options for children with SM by harnessing novel treatment formats that may be able to overcome traditional barriers and reach more youth in need.
Funding details:
This work was supported by the National Institutes of Health under Grants F31MH122101 (PI: Hong); T32DA043449 (PI: Pelham); and F31HD104336 (PI: Heflin).
Footnotes
Disclosure statement: Dr. Comer receives royalties from Macmillan Learning unrelated to the present work. No other authors have financial interests to declare.
References
- Achenbach TM, & Rescorla LA (2000). Manual for the ASEBA preschool forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Albanese AM, Russo GR, & Geller PA (2019). The role of parental self‐efficacy in parent and child well‐being: A systematic review of associated outcomes. Child: Care, Health and Development, 45(3), 333–363. doi: 10.1111/cch.12661 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American Psychiatric Association. [Google Scholar]
- American Well. (2019). Telehealth index: 2019 consumer survey. https://static.americanwell.com/app/uploads/2019/07/American-Well-Telehealth-Index-2019-Consumer-Survey-eBook2.pdf
- Angelosante AG, Pincus DB, Whitton SW, Cheron D, & Pian J. (2009). Implementation of an intensive treatment protocol for adolescents with panic disorder and agoraphobia. Cognitive and Behavioral Practice, 16(3), 345–357. doi: 10.1016/j.cbpra.2009.03.002 [DOI] [Google Scholar]
- Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. (2020). The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: Challenges and opportunities for innovation. Journal of Adolescent Health, 67(2), 164–171. doi: 10.1016/j.jadohealth.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman RL, Keller ML, Piacentini J, & Bergman AJ (2008). The development and psychometric properties of the selective mutism questionnaire. Journal of Clinical Child & Adolescent Psychology, 37(2), 456–464. doi: 10.1080/15374410801955805 PMID: 18470781 [DOI] [PubMed] [Google Scholar]
- Bergman RL, Piacentini J, & McCracken JT (2002). Prevalence and description of selective mutism in a school-based sample. Journal of the American Academy of Child and Adolescent Psychiatry, 41(8), 938–946. doi: 10.1097/00004583-200208000-00012 [DOI] [PubMed] [Google Scholar]
- Bergman RL, Gonzales A, Piacentini J, & Keller ML (2013). Integrated behavior therapy for selective mutism: A randomized controlled pilot study. Behaviour Research and Therapy, 51(10), 680–689. doi: 10.1016/j.brat.2013.07.003 [DOI] [PubMed] [Google Scholar]
- Bögels SM, Alden L, Beidel DC, Clark LA, Pine DS, Stein MB, & Voncken. (2010). Social anxiety disorder: Questions and answers for the DSM-V. Depression and Anxiety, 27(2), 168–189. doi: 10.1002/da.20670 [DOI] [PubMed] [Google Scholar]
- Carpenter AL, Pincus DB, Furr JM, & Comer JS (2018). Working from home: An initial pilot examination of videoconferencing-based cognitive behavioral therapy for anxious youth delivered to the home setting. Behavior Therapy, 49(6), 917–930. doi: 10.1016/j.beth.2018.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catchpole R, Young A, Baer S, & Salih T. (2019). Examining a novel, parent child interaction therapy-informed, behavioral treatment of selective mutism. Journal of Anxiety Disorders, 66, 102112. doi: 10.1016/j.janxdis.2019.102112 [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. (2020, March 17). Medicare telemedicine health care provider fact sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- Chavira DA, Shipon-Blum E, Hitchcock C, Cohan S, & Stein MB (2007). Selective mutism and social anxiety disorder: All in the family? Journal of the American Academy of Child & Adolescent Psychiatry, 46(11), 1464–1472. doi: 10.1097/chi.0b013e318149366a [DOI] [PubMed] [Google Scholar]
- Comer JS, & Barlow DH (2014). The occasional case against broad dissemination and implementation: Retaining a role for specialty care in the delivery of psychological treatments. American Psychologist, 69(1), 1–18. doi: 10.1037/a0033582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Cooper-Vince CM, Kerns CE, Chan PT, Edson AL, Khanna M, Franklin ME, Garcia AM, & Freeman JB (2014). Internet-delivered, family-based treatment for early-onset OCD: A preliminary case series. Journal of Clinical Child & Adolescent Psychology, 43(1), 74–87. doi: 10.1080/15374416.2013.855127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Cooper-Vince C, Madigan RJ, Chow C, Chan P, Idrobo F, Chase RM, McNeil CB, & Eyberg SM (2015). Rationale and considerations for the Internet-based delivery of Parent Child Interaction Therapy. Cognitive and Behavioral Practice, 22(3), 302–316. doi: 10.1016/j.cbpra.2014.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, del Busto C, Silva K, Hong N, Poznanski B, Sanchez AL, Cornacchio D, Herrera A, Coxe S, Miguel E, Georgiadis C, Conroy K, & Puliafico AC (2021). Therapist-led, internet-delivered treatment for early child social anxiety: A waitlist-controlled evaluation of the iCALM Telehealth Program. Behavior Therapy. Online ahead of print. doi: 10.1016/j.beth.2021.01.004 [DOI] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Kerns CE, Miguel E, Coxe S, Elkins RM, Carpenter AL, Cornacchio D, Cooper-Vince CE, DeSerisy M, Chou T, Sanchez AL, Khanna M, Franklin ME, Garcia AM, & Freeman JB (2017). Internet-delivered, family-based treatment for early-onset OCD: A pilot randomized trial. Journal of Consulting and Clinical Psychology, 85(2), 178–186. doi: 10.1037/ccp0000155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Miguel EM, Cooper-Vince CE, Carpenter AL, Elkins RM, Kerns CE, Cornacchio D, Chou T, Coxe S, DeSerisy M, Sanchez AL, Golik A, Martin J, Myers KM, & Chase R. (2017). Remotely delivering real-time parent training to the home: An initial randomized trial of Internet-delivered parent-child interaction therapy (I-PCIT). Journal of Consulting and Clinical Psychology, 85(9), 909–917. doi: 10.1037/ccp0000230 [DOI] [PubMed] [Google Scholar]
- Comer JS, Hong N, Poznanski P, Silva K, & Wilson M. (2019). Evidence base update on the treatment of early childhood anxiety and related problems. Journal of Clinical Child and Adolescent Psychology, 48(1), 1–15. doi: 10.1080/15374416.2018.1534208 [DOI] [PubMed] [Google Scholar]
- Comer JS, & Timmons AC (2019). The other side of the coin: Computer-mediated interactions may afford opportunities for enhanced empathy in clinical practice. Clinical Psychology: Science and Practice, 26(4), e12308. doi: 10.1111/cpsp.12308 [DOI] [Google Scholar]
- Cornacchio D, Furr JM, Sanchez AL, Hong N, Feinberg LK, Tenenbaum R, del Busto C, Bry LJ, Poznanski P, Miguel E, Ollendick TH, Kurtz SMS, & Comer JS (2019). Intensive group behavioral treatment (IGBT) for children with selective mutism: A preliminary randomized clinical trial. Journal of Consulting and Clinical Psychology, 87(8), 720–733. doi: 10.1037/ccp0000422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doss BD, Feinberg LK, Rothman K, Roddy MK, & Comer JS (2017). Using technology to enhance and expand interventions for couples and families: Conceptual and methodological considerations. Journal of Family Psychology, 31(8), 983–993. doi: 10.1037/fam0000349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driessen J, Blom JD, Muris P, Blashfield RK, & Molendijk ML (2020). Anxiety in children with selective mutism: A meta-analysis. Child Psychiatry & Human Development, 51(2), 330–341. doi: 10.1007/s10578-019-00933-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elizur Y, & Perednik R. (2003). Prevalence and description of selective mutism in immigrant and native families: A controlled study. Journal of the American Academy of Child and Adolescent Psychiatry, 42(12), 1451–1459. doi: 10.1097/00004583-200312000-00012 [DOI] [PubMed] [Google Scholar]
- Elkins RM, Gallo KP, Pincus DB, & Comer JS (2016). Moderators of intensive CBT for adolescent panic disorder: The fear and avoidance. Child and Adolescent Mental Health, 21(1), 30–36. doi: 10.1111/camh.12122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flancbaum M, Rockmore L, & Franklin ME (2011). Intensive behavior therapy for tics: Implications for clinical practice and overcoming barriers to treatment. Journal of Developmental and Physical Disabilities, 23(1), 61–69. doi: 10.1007/s10882-010-9222-0 [DOI] [Google Scholar]
- Furr JM, Sanchez AL, Hong N, & Comer JS (2019). Exposure therapy for childhood selective mutism: Principles, practices, and procedures. In McGuire J, Peris T, & Storch E. (Eds.), A clinicians’ guide to exposure therapy with children and adolescents. New York, NY: Elsevier. [Google Scholar]
- Gallo KP, Chan PT, Buzzella BA, Whitton SW, & Pincus DP (2013). The impact of an eight-day intensive treatment for adolescent panic disorder and agoraphobia on comorbid diagnoses. Behavior Therapy, 43(1), 153–159. doi: 10.1016/j.beth.2011.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gensthaler A, Dieter J, Raisig S, Hartmann B, Ligges M, Kaess M, Freitag CM, & Schwenck C. (2020). Evaluation of a novel parent-rated scale for selective mutism. Assessment, 27(5), 1007–1015. doi: 10.1177/1073191118787328 [DOI] [PubMed] [Google Scholar]
- Grist R, Croker A, Denne M, & Stallard P. (2019). Technology delivered interventions for depression and anxiety in children and adolescents: A systematic review and meta-analysis. Clinical Child and Family Psychology Review, 22(2), 147–171. doi: 10.1007/s10567-018-0271-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurwitch RH, Salem H, Nelson MM, & Comer JS (2020). Leveraging parent-child interaction therapy and telehealth capacities to address the unique needs of young children during the COVID-19 public health crisis. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S82–S84. doi: 10.1037/tra0000863 [DOI] [PubMed] [Google Scholar]
- Guy W, & Bonato RR (1970). Clinical global impressions. Chevy Chase, MD: United States Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health. [Google Scholar]
- Health Resources & Services Administration. (2013). Report to Congress on the Nation’s Substance Abuse and Mental Health Workforce Issues. Retrieved from https://store.samhsa.gov/shin/content/PEP13-RTC-BHWORK/PEP13-RTC-BHWORK.pdf
- Higa-McMillan CK, Francis SE, Rith-Najarian L, & Chorpita BF (2016). Evidence base update: 50 years of research on treatment for child and adolescent anxiety. Journal of Clinical Child and Adolescent Psychology, 45(2), 91–113. doi: 10.1080/15374416.2015.1046177 [DOI] [PubMed] [Google Scholar]
- Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, & Yellowlees PM (2013). The effectiveness of telemental health: A 2013 review. Telemedicine and e-Health, 19(6), 444–454. doi: 10.1089/tmj.2013.0075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong N, Feinberg L, Comer JS, & Bagner D. (2019). Internet-delivered Parent-Child Interaction Therapy for children with Autism Spectrum Disorder: rationale, considerations, and lessons learned. In McNeil CB, Quetsch LB, & Anderson CM (Eds.) Handbook of Parent-Child Interaction Therapy for Children on the Autism Spectrum (pp. 545–557). New York: Springer. doi: 10.1007/978-3-030-03213-5_30 [DOI] [Google Scholar]
- Joint Task Force for the Development of Telepsychology Guidelines for Psychologists. (2013). Guidelines for the practice of telepsychology. American Psychologist, 68 (9), 791–800 DOI: 10.1037/a0035001 [DOI] [PubMed] [Google Scholar]
- Kazdin AE, & Blase SL (2011). Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspectives on Psychological Science, 6(1), 21–37. doi: 10.1177/1745691610393527 [DOI] [PubMed] [Google Scholar]
- Khan AN, Bilek E, Tomlinson RC, & Becker-Haimes EM (2021). Treating social anxiety in an era of social distancing: Adapting exposure therapy for youth during COVID-19. Cognitive and Behavioral Practice, online ahead of print. doi: 10.1016/j.cbpra.2020.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krach SK, McCreery MP, & Rimel H. (2017). Examining teachers’ behavioral management charts: A comparison of Class Dojo and paper-pencil methods. Contemporary School Psychology, 21, 267–275. doi: 10.1007/s40688-016-0111-0 [DOI] [Google Scholar]
- Kumpulainen K, Räsänen E, Raaska H, & Somppi V. (1998). Selective mutism among second-graders in elementary school. European Child and Adolescent Psychiatry, 7(1), 24–29. doi: 10.1007/s007870050041 [DOI] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, & Nguyen TD (1979). Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning, 2(3), 197–207. doi: 10.1016/0149-7189(79)90094-6 [DOI] [PubMed] [Google Scholar]
- Lorenzo NE, Cornacchio D, Chou T, Kurtz SMS, Furr JM, & Comer JS (2020). Expanding treatment options for children with selective mutism: Rationale, principles, and procedures for an intensive group behavioral treatment. Cognitive and Behavioral Practice, online ahead of print. doi: 10.1016/j.cbpra.2020.06.002 [DOI] [Google Scholar]
- Merwin E, Snyder A, & Katz E. (2006). Differential access to quality rural healthcare: Professional and policy challenges. Family & Community Health, 29(3), 186–194. [DOI] [PubMed] [Google Scholar]
- Morse G, Salyers MP, Rollins AL, Monroe-DeVita M, & Pfahler C. (2012). Burnout in mental health services: a review of the problem and its remediation. Administration and Policy in Mental Health and Mental Health Services Research, 39, 341–352. doi: 10.1007/s10488-011-0352-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers KM, Nelson EL, Hilty DM, Rabinowitz T, Barwell SS, Bernard J, Boyce G, Bufka L, Cain S, Chui L, Comer JS, Cradock C, Varrell JR, Goldstein F, Johnston B, Krupinski EA, Lo K, Luxton D, McSwain D, McWilliams J, North S, Ostrowski J, Pignatiello A, Roth D, Turvey C, & Wright S. (2017). American Telemedicine Association Practice Guidelines for Telemental Health with Children and Adolescents. Telemedicine and e-Health, 23(10), 779–804. doi: 10.1089/tmj.2017.0177 [DOI] [PubMed] [Google Scholar]
- Nelson EL, Barnard M, & Cain S. (2003). Treating childhood depression over videoconferencing. Telemedicine and e-Health, 9(1), 49–55. doi: 10.1089/153056203763317648 [DOI] [PubMed] [Google Scholar]
- Nicholas J, Bell IH, Thompson A, Valentine L, Simsir P, Sheppard H, & Adams S. (2021). Implementation lessons from the transition to telehealth during COVID-19: A survey of clinicians and young people from youth mental health services. Psychiatry Research, 299. Online ahead of print. doi: 10.1016/j.psychres.2021.113848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oerbeck B, Stein MB, Wentzal-Larsen T, Langsrud O, & Kristensen H. (2014). A randomized controlled trial of a home and school-based intervention for selective mutism: Defocused communication and behavioral techniques. Child and Adolescent Mental Health, 19(3), 192–198. doi: 10.1111/camh.12045 [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Ryan SM, Capriola-Hall NN, Austin KE, & Fraire M. (2018). Have phobias, will travel: Addressing one barrier to the delivery of an evidence-based treatment. Behavior Therapy, 49, 594–603. doi: 10.1016/j.beth.2017.11.003 [DOI] [PubMed] [Google Scholar]
- Ollendick TH, & Davis TE III. (2013). One-session treatment for specific phobias: A review of Öst’s single-session exposure with children and adolescents. Cognitive Behaviour Therapy, 42(4), 275–283. doi: 10.1080/16506073.2013.773062 [DOI] [PubMed] [Google Scholar]
- Öst LG, & Ollendick TH (2017). Brief, intensive, and concentrated cognitive behavioral treatment for anxiety disorders in children: A systematic review and meta-analysis. Behaviour Research and Therapy, 97, 134–145. doi: 10.1016/j.brat.2017.07.00 [DOI] [PubMed] [Google Scholar]
- Pew Research Center. (2019a, May 7). Digital divide persists even as lower-income Americans make gains in tech adoption. https://www.pewresearch.org/fact-tank/2019/05/07/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption/
- Pew Research Center. (2019b, May 31). Digital gap between rural and nonrural America persists. https://www.pewresearch.org/fact-tank/2019/05/31/digital-gap-between-rural-and-nonrural-america-persists/
- Pierce BS, Perrin PB, Tyler CM, McKee GB, & Watson JD (2021). The COVID-19 telepsychology revolution: A national study of pandemic-based changes in U.S. mental health care delivery. American Psychologist, 76(1), 14–25. doi: 10.1037/amp0000722 [DOI] [PubMed] [Google Scholar]
- Reschovsky JD, & Staiti AB (2003). Access and quality: Does rural America lag behind? Health Affairs, 24(4), 1128–1139. doi: 10.1377/hlthaff.24.4.1128 [DOI] [PubMed] [Google Scholar]
- Robacker CM, Rivera CJ, & Warren SH (2016). A token economy made easy through ClassDojo. Intervention in School and Clinic, 52(1), 39–43. doi: 10.1177/1053451216630279 [DOI] [Google Scholar]
- Sammons MT, VandenBos GR, Martin JN, & Elchert DM (2020). Psychological practice at six months of COVID-19. A follow-up to the first national survey of psychologists during the pandemic. Journal of Health Service Psychology. Online ahead of print. doi: 10.1007/s42843-020-00024-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santucci LC, & Ehrenreich-May J. (2013). A randomized controlled trial of the child anxiety multi-day program (CAMP) for separation anxiety disorder. Child Psychiatry & Human Development, 44(3), 439–451. doi: 10.1007/s10578-012-0338-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwenk C, Gensthaler A, & Vogel F. (2019). Anxiety levels in children with selective mutism and social anxiety disorder. Current Psychology. doi: 10.1007/s12144-019-00546-w [DOI] [Google Scholar]
- Shaffer D, Gould M, Brasic J, Ambrosini P, Fisher P, Bird H, & Aluwahlia S. (1983). A Children’s Global Assessment Scale (CGAS). Archives of General Psychiatry, 40(11), 1228–1231. doi: 10.1001/archpsyc.1983.01790100074010 [DOI] [PubMed] [Google Scholar]
- Sharma A, Sasser T, Gonzalez ES, Vander Stoep A, & Myers K. (2020). Implementation of home-based telemental health in a large child psychiatry department during the COVID-19 crisis. Journal of Child and Adolescent Psychopharmocology, 30(7), 404–413. doi: 10.1089/cap.2020.0062 [DOI] [PubMed] [Google Scholar]
- Selective Mutism University. (2021). Selective mutism skills training. https://selectivemutismuniversity.thinkific.com/courses/sm-101
- Silverman WK, & Albano AM (1996). The Anxiety Disorders Interview Schedule for Children for DSM-IV: Child and Parent Versions. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Silverman WK, & Kurtines WM (1996). Building blocks. In Silverman and Kurtines, Anxiety and phobic disorders: A pragmatic approach (pp. 55–62). New York: Plenum Press. [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ, Mann G, Duke D, Munson M, Adkins J, Grabill KM, Murphy TK, & Goodman WK (2007). Family-based cognitive-behavioral therapy for pediatric obsessive-compulsive disorder: Comparison of intensive and weekly approaches. Journal of the American Academy of Child and Adolescent Psychiatry, 46(4), 469–478. doi: 10.1097/chi.0b013e31803062e7 [DOI] [PubMed] [Google Scholar]
- Toppelberg CO, Tabors P, Coggins A, Lum K, & Burger C. (2005). Differential diagnosis of selective mutism in bilingual children. Journal of the American Academy of Child and Adolescent Psychiatry, 44(6), 592–595. doi: 10.1097/01.chi.0000157549.87078.f8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner A, Ricketts T, & Leslie LK (2020). Comparison of number and geographic distribution of pediatric subspecialists and patient proximity to specialized care in the US between 2003 and 2019. JAMA Pediatrics, 174(9), 852–860. doi: 10.1001/jamapediatrics.2020.1124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Status Census Bureau. (2020, August 26). How the Census Bureau measures poverty. https://www.census.gov/topics/income-poverty/poverty/guidance/poverty-measures.html
- U.S. Department of Health & Human Services. (2020, January 21). 2020 poverty guidelines. https://aspe.hhs.gov/2020-poverty-guidelines
- U.S. Department of Health & Human Services. (2020). Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html
- Viana AG, Beidel DC, & Rabian B. (2009). Selective mutism: A review and integration of the last 15 years. Clinical Psychology Review, 29(1), 57–67. doi: 10.1016/j.cpr.2008.09.009 [DOI] [PubMed] [Google Scholar]
- Vogel F, Gensthaler A, Stahl J, & Schwenk C. (2019). Fears and fear-related cognitions in children with selective mutism. European Child & Adolescent Psychiatry, 28, 1169–1181. doi: 10.1007/s00787-019-01281-0 [DOI] [PubMed] [Google Scholar]
- Zakszeski BN, & DuPaul GJ (2017). Reinforce, shape, expose, and fade: A review of treatments for selective mutism (2002–2015). School Mental Health, 9, 1–15. doi: 10.1007/s12310-016-9198-8 [DOI] [Google Scholar]