Abstract
Degenerative spine disease is increasing in prevalence as the global population ages, indicating a need for targeted therapies and continued innovations. While autograft and allograft have historically demonstrated robust results in spine fusion surgery, they have significant limitations and associated complications such as infection, donor site morbidity and pain, and neurovascular injury. Synthetic grafts may provide similar success while mitigating negative outcomes. A narrative literature review was performed to review available synthetic materials that aim to optimize spinal fusion. The authors specifically address the evolution of synthetics and comment on future trends. Novel synthetic materials currently in use include ceramics, synthetic polymers and peptides, bioactive glasses, and peptide amphiphiles, and the authors focus on their success in both human and animal models, physical properties, advantages, and disadvantages. Advantages include properties of osteoinduction, osteoconduction, and osteogenesis, whereas disadvantages encompass a lack of these properties or growth factor-induced complications. Typically, the use of synthetic materials results in fewer complications and lower costs. While the development and tuning of synthetic materials are ongoing, there are many beneficial alternatives to autografts and allografts with promising fusion results.
Keywords: synthetic, spine fusion, bioactive glass, synthetic peptide, synthetic polymer, peptideamphiphile, ceramic, implant, autograft, allograft
Introduction
As the global population ages, degenerative spine disease is becoming more prevalent, signifying the need for targeted therapies. Spine fusion, using bone grafts, is an essential treatment for various spinal conditions, including deformity, fractures, dislocations, spondylolisthesis, and intervertebral disc disease. As the demand for spinal fusion continues to increase in the aging population, innovative materials and products are being rapidly developed.1
The use of bone grafts in spinal fusion aims to maximize osteoinduction, osteoconduction, and osteogenesis in the native tissue. Osteoconductive grafts act as physical scaffolds to create a surface supportive of bone and capillary growth. Osteoinduction involves the chemical stimulation of osteoprogenitor cell differentiation, which stimulates this new bone growth (osteogenesis).2 Bone grafts that demonstrate all 3 properties have historically exhibited successful spinal fusion.
Commonly used bone grafts include autologous grafts (autografts) and allografts. An autograft is harvested from the host, often from a separate incision along the iliac crest or locally within the same incision, after decompression of the lamina and spinous processes. It is considered the “gold standard” and creates an osteoconductive, osteoinductive, and osteogenic environment. While iliac crest bone grafting (ICBG) is conducive to fusion, it has been linked to complications such as pain, neurovascular injury, infection, pelvic avulsion fracture, and hematoma.3 Local bone grafting can avoid these adverse events; however, the availability of bone volume can be an issue. To avoid these complications, sterilized cadaver bones (allografts) have been increasingly implemented. However, allograft only demonstrates osteoconductive properties. Despite this, in some anatomic areas, they have produced similar radiographic and clinical outcomes to autografts with fewer complication rates.4,5 Although minor, there is some risk of disease transmission, such as hepatitis B or C and HIV, with the use of allograft.4 To combat these potential risks and complications, there has been significant interest in synthetic products to augment or ultimately replace autografts.
Benefits of synthetic materials include cost, abundant supply, and tailored properties to maximize bone growth.6 Earlier versions of synthetic grafts, such as bone cement, had no bioactivity and served as a mechanical support and binder.7 As synthetic options have been developed further, grafts and extenders have been synthesized that demonstrate greater bioactivity. These include ceramics, synthetic polymers and peptides, bioactive glasses, and peptide amphiphiles (PAs).6
Ceramics
Ceramics are widely used as synthetic graft extenders, often in combination with other bioactive materials. They are generally considered to be osteoconductive but not osteoinductive, thereby requiring additional substances and factors to promote bone growth. Ceramics exist in porous and compact forms, easily moldable into different shapes and sizes. Porous forms support cell adhesion, proliferation, and nutrient infiltration.8 Ceramics are advantageous in their biocompatibility and biodegradability properties compared to other materials. Since they are inert, they typically do not elicit an immune response. An important limitation of ceramics is their low mechanical strength and fragility.9 For example, the greater the porosity of the ceramic, the weaker the mechanical strength. There are numerous types of ceramics that vary in their porosity, composition, and structure. The most frequently used ceramics include calcium sulfates, calcium phosphates, hydroxyapatites (HAs), and silicon nitrides.6
Calcium sulfate ceramics support osteoconduction but are limited by their reduced strength and susceptibility to breakage, particularly with moisture exposure.6 Due to this limit in strength, they are typically used in the setting of smaller defects, not larger procedures such as spinal fusions. Lastly, the rate of degradation of calcium sulfates is quicker than the rate of bone growth, resorbing about 6 weeks postimplantation, which may leave growing bone without a supportive scaffold. Due to this limitation, there are few products that contain this material for the application of spinal fusion.6,9
In contrast, calcium phosphate has both osteoconductive and osteointegrative abilities with greater strength under compression. However, it is still relatively weak, especially under tension and shear stress. Beta-tricalcium phosphate is a porous phosphate similar to cancellous bone in terms of compressive and tensile strength. It has a relatively slow rate of degradation of 6–18 months; however, bone growth and integration may still be incomplete, resulting in unstable bone. The cement formulations of calcium phosphate have an even longer degradation rate of about 2 years.6,8,9
HAs are synthetic mimetics of the naturally occurring HA present in bone minerals. After sintering, or heating, synthetic HAs have greater compression resistance compared to other ceramics. However, these materials are primarily used as extenders or require supplementation with other materials for effective fusion. HAs are unique in that they are considered nonabsorbable, with only about 1%–2% resorbed per year after implantation.6,8 Among the HA ceramics, there is a large variation in solubility, granulometric distribution, crystallinity, and pore shape and size. However, in recent animal studies, these differences have not demonstrated a significant difference in terms of cellular response and bone growth.8
Silicon nitride (Si3N4) is a form of structural ceramic with greater osteoconductivity and osteointegration. Its high mechanical and flexural strengths give it superior resistance to both thermal and heat shock, corrosion, abrasion, and fracture. While it has historically been used for industrial purposes, silicon nitride’s biocompatibility and bioinert properties make it increasingly useful for biomedical purposes. Its orthopedic applications include spinal fusion cages and parts of hip and knee prosthetics. This wide range of utility is largely due to its modifiable chemical and mechanical properties. It can be engineered to mimic the dense, porous structure of cancellous bone for implantation (Figure 1).10 The silicon-amine predominant form creates a hydrophilic surface and homeostatic pH that allows for improved protein adsorption and greater bone affinity. This property also contributes to its bacterial-resistant properties, preventing adhesion and colonization. In 2018, of 35,000 spinal fusions using silicon nitride implants, the adverse event rate was 0.07% (Figure 2).10 Conversely, the major limitations of silicon nitride ceramics are production costs and intensive processing methods.10–12
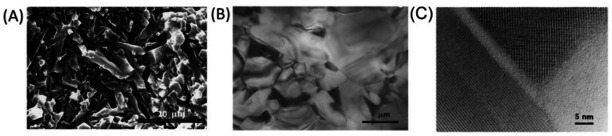
Figure 1.
Scanning electron microscope (SEM) image of silicon nitride ceramic implant.10 (A) SEM image of silicon nitride implant. (B) Transmission electron microscope (TEM) micrograph, low magnification. (C) TEM micrograph, high-resolution showing amorphous phase of the grain pockets. This image is reprinted with permission from Liu and Nemat-Nasser.13 Copyright 1998 Elsevier Publishing Group.
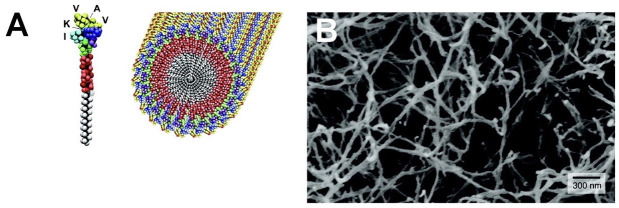
Figure 2.
Thirty-year follow-up after interbody fusion using silicon nitride ceramic spacers.10 (A) Computed tomographic (CT) image showing silicon nitride implant with load bearing nonporous rim (arrow) and porous core conducive to early osseointegration (asterisk). (B) Sagittal CT image showing fusion mass and osteointegration. The coronal CT image shows fusion mass adjacent to the spacer and osseointegration at the bone-ceramic conjunction. (C) Left: Implant anterior translation with posterior revision. Insert: L5 to S1 demonstrating fusion, despite anterior movement of implant. Right: Lack of reaction in surrounding tissue reinforces biocompatibility of silicon nitride implant. This image is reprinted with permission from Mobbs et al.14 Copyright 2018 Elsevier Publishing Group.
Since ceramics are not osteoinductive, they are typically combined with other bioactive materials, including bone marrow aspirate, ICBGs, and/or local autografts. Several commercial ceramic grafts have been developed to be used as bone graft extenders in conjunction with these biomaterials, such as Mastergraft (Medtronic, Mineapolis, MN), BoneSave (Stryker), and others. Nickoli and Hsu demonstrated in a systematic review that the average fusion rate using ceramic grafts in combination with bioactive materials for lumbar spinal fusions was 86.4%.9 It ranged from 72.6% as the lowest fusion rate to 96.2% as the highest fusion rate when combining ceramic with bone marrow aspirate or iliac crest autograft with demineralized bone matrix (DBM), respectively. However, it did not demonstrate a significant difference in fusion based on the different types of ceramic themselves.6,9
Recently,manufacturers of third-generation bioactive ceramics have introduced the possibility of using ceramics as standalone bone graft substitutes. Both AttraX (NuVasive, San Diego, CA) and MagnetOs (Kuros Biosciences, Schlieren, Switzerland) are examples of biphasic calcium phosphate ceramics with improved bioactivity. Following successful trials in animal models, AttraX has undergone several clinical trials. A recent randomized clinical trial used 100 patients as self-control by receiving AttraX putty and autografts on contralateral sides while undergoing posterolateral fusion (PLF).15 AttraX demonstrated a fusion rate of 55% compared to autograft with a 52% fusion rate,15 illustrating the potential for AttraX to function as a standalone graft. In the preclinical setting, MagnetOs has exhibited similar promise. A 2018 study tested MagnetOs vs autograft fusion capacity in an ovine PLF model. The fusion rates for autograft, MagnetOs granules with autograft, and MagnetOs putty with autograft were 75%, 92%, and 83%, respectively.16 More recently, a 2022 study evaluated MagnetOs against autologous bone grafts in rabbit L4 to L5 PLFs. MagnetOs, in combination with autologous bone graft, demonstrated a fusion rate of 62.5% whereas autologous bone graft alone demonstrated a fusion rate of 75%.17 With continued development, both of these ceramic grafts show great potential as a fully synthetic option for successful fusions.6
Synthetic Polymers
Similar to ceramics, synthetic polymers are commonly used as osteoconductive scaffolds in bone grafts or as bone graft extenders. These polymers are long-chain molecules of repeating units, often with a carbon backbone, manufactured through various techniques, including 3D printing, electrospinning, and solvent casting.6 When placed in aqueous environments, these chains will degrade. This property has contributed to its utility in various medical applications when combined with bioactive materials. They may also be engineered to place greater emphasis on different physical properties such as crystallinity, molecular weight, and transition temperature. For example, engineering a polymer that has a high crystallinity or higher molecular weight will make a more robust and durable implant with a lower degradation rate. Higher crystallinity also makes a polymer more stable at certain temperatures. This can allow a spinal fusion cage to remain stable at body temperature long enough for fusion and lasting stability to occur. Lastly, the transition temperature can be modified to adjust viscosity and avoid the spinal cage morphing and flowing.18,19 This variation in chemical composition makes some polymers more advantageous than others for spinal fusion.
The most common polymers are those derived from poly-a-hydroxy acids. These include poly(l-lactic) acid, poly(lactic-co-glycolic acid), polylactide (PLA), polyglycolide (PGA), poly(e-caprolactone), and polymethylmethacrylate (PMMA). Since lactic and glycolic acids are involved in naturally occurring biochemical pathways, PLA and PGA will degrade to natural compounds. However, PGA is very unstable with rapid loss of strength, making it less desirable, particularly as a material for spinal cages. PGA is also incompatible with nerve tissue and dura mater, with reports of fusion to the dura.18 Poly (lactic acid) and PLA are often used in spinal cages as they are more resistant to degradation. While PLA and its related polymers have been shown to be biocompatible, there has been some evidence that PLA may be associated with reductions in cell proliferation, possibly due to acidic degradation products. There have also been reports of irritation, osteolysis, or sinus tract formation at the site of implantation from a sterile immune response.6,18
These polymers are used in combination with ceramics, with autografts, and as a conduit for growth factor delivery. Studies assessing the use of PMMA in spinal fusion procedures have yielded inconsistent results. Some have found no difference in fusion outcomes in patients using PMMA polymers compared to those using ICBG.6 Others have found significantly lower fusion rates with PMMA compared to ICBG, despite no significant differences in clinical outcomes like functional ability.6 Additionally, polymer-ceramic composites are becoming more commonly used, particularly with HA ceramics. This combination increases the transition temperature without altering the crystallinity or melting temperature.20 Ultimately, this allows for a more stable, effective implant.
Synthetic Peptides
While osteoconductive synthetics promote sufficient spinal fusion in conjunction with biomaterials, synthetic peptides are being developed to act as standalone bone grafts. They are synthetically produced amino acid polypeptides that are bound to an anorganic bone mineral (ABM). This compound is then embedded within a hydrogel for implantation. The peptide, in combination with the bone matrix, is considered to be osteoconductive. The main synthetic peptides in use medically include P-15, P-15L, and B2A.21,22
The P-15 bone graft substitute is a bone matrix biomimetic composed of mineral, a synthetic residue, and an amino acid sequence synonymous with the type 1 collagen-binding domain. By only incorporating the cell-binding domain analogous to type 1 collagen, it eliminates the immune response-inducing segment. This product promotes extracellular matrix formation, cell migration, and proliferation, ultimately leading to new bone growth (Figure 3).23 The commercially available P/15-ABM, known as i-FACTOR peptide-enhanced bone graft (Cerapedics, Inc., Westminster, CO), has demonstrated similar fusion results as an autograft when used for anterior cervical discectomy and fusion.22 Furthermore, it has demonstrated greater fusion rates in patients undergoing posterior lumbar interbody fusion when used as a graft extender compared to allograft alone.21,22
Figure 3.
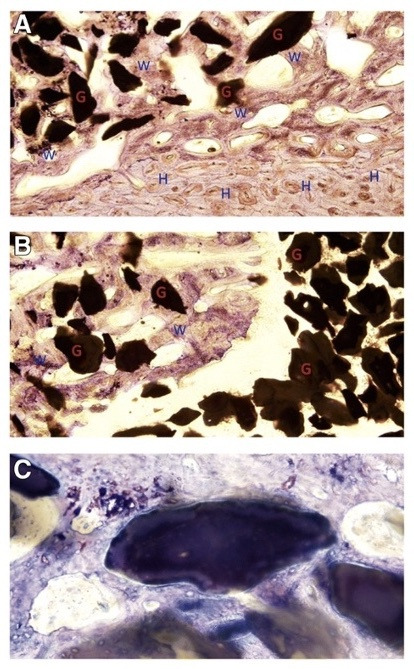
Osteointegration of new bone with anorganic bone mineral (ABM)-P15 as seen on histology with toluidine blue 0.1% staining.23 (A) Proximal transition zone between transverse process and graft, ABM granules (G) with surrounding haversian canals (H) and woven bone (W). (B) Distal transition zone between nonfused graft material and fibrous tissue (lower-left). (C) Osteointegration demonstrated with HA granules within woven bone. This image was reprinted with permission from Axelsen et al.23 Copyright 2019 Springer Nature.
Due to the promising effects of the P-15 bone graft substitute, P-15L was created as a new iteration of the i-FACTOR product. It incorporates P-15 and ABM into a bovine collagen carrier as opposed to a hydrogel or pre-existing putty. A recent study evaluated P-15L fusion success compared to that of ICBG lumbar interbody fusions in ovine models. At 3-month follow-up, the P-15L graft demonstrated superior fusion and morphology than the ICBG. However, at 6 months, the 2 grafts reached similar levels of fusion and stiffness, indicating P-15L is a sufficient bone graft substitute.21,22
Aligned with the success of these synthetic peptides, B2A2-K-NS, commonly known as B2A, is another promising osteoinductive and osteoconductive synthetic peptide currently being evaluated using animal models. B2A amplifies the BMP-2 response, which is an integral bone growth-promoting factor, and increases osteoblast activity by interacting with BMP receptors.24,25 Therefore, it relies on naturally occurring BMP-2 and produces no effect where BMP-2 is not present in the body.26 In animal models, this peptide has in fact proven more effective in spinal interbody fusion than autograft.24,25 Because of these results, a recent phase 1 clinical trial of 24 participants undergoing transforaminal lumbar interbody fusion evaluated the efficacy of B2A-coated ceramic granules (Prefix) when compared with ICBG. The resulting fusion rates were 100% for the B2A 750 µg/cm3 granules group (n = 7), 77.8% for the ICBG control group (n = 9), and 50% in the B2A 150 µg/cm3 granules group (n = 8). Because of the sample size, these differences were not found to be significant but deserve further study as an alternative to ICBG.26
Bioactive Glass
Bioactive glasses are inorganic metallic oxides with osteoconductive properties that allow for greater bone growth and healing. Generally, bioactive glasses are dense and nonporous, with greater durability and strength than materials such as ceramics. Because bioactive glasses are inorganic, they do not require cadaver or patient bone donation to be engineered, making them widely available. They are also relatively cost-effective to use in clinical settings for both patients and providers. Bioactive glasses are able to induce an antimicrobial and osteoblast-stimulating environment by degrading upon contact with body fluids and releasing calcium and phosphorus. These ions then form a layer of HA, which allows for protein adsorption, provides a stable scaffold, and improves integration into the surrounding bone. However, due to biodegradability, the dissolution rate greatly impacts stability and adequate fusion. Additionally, when used with other substrates, like titanium implants, the thermal expansion coefficient often varies significantly from that of the metal prosthetic. In this case, bioactive glass may lift away from the prosthetic surface prior to adequate fusion.6,11,27,28
Bioactive glasses are defined by their composition. They are composed primarily of silicon dioxide. Other components include sodium oxide (Na2O), calcium oxide (CaO), and silicon dioxide (SiO2). The relative concentrations of these secondary components contribute to the biodegradability of the glass. Some of the most common bioactive glasses and their chemical compositions are listed in the Table. Regardless of the variations in these other materials, most bioactive glasses typically have high concentrations of sodium and calcium oxides for biocompatibility purposes.6,11,27,28
Table.
Common bioactive glasses and their composition.6
| Bioactive Glass Name | Composition |
| S53P4 | 53% SiO2, 23% Na2O, 20% CaO, and 4% P2O5 |
| AW-GC (apatite- and wollastonite- glass ceramic composite) | 34.2% SiO2, 44.9% CaO, 16.3% P2O5, 4.6% MgO, and 0.5% CaF2 |
| 45S5 | 45% SiO2, 24.5% Na2O, 24.5% CaO, and 6% P2O5 |
| Chitra-HABg | 80% HA and 20% bioactive glass |
| BGS-7 | 35.82% SiO2, 41.79% CaO, 13.93% P2O5, 5.97% MgO, 1.99% CaF2, and 0.5% B2O3 |
Bioactive glasses have been used in various clinical applications, including spinal fusions.27,29 A recent meta-analysis and systematic review analyzed the use of bioactive glasses for spinal fusion across 12 preclinical studies (267 animals) and 12 clinical studies (396 patients). The studies encompassed cervical, thoracic, and lumbar fusion procedures for an array of causes.27 Analysis demonstrated that, across all these trials, fusion was seen in 84% of the human cases in bioactive glass test groups. In combination with autograft, bioactive glass was shown to be equally effective for fusion success (89.6%) compared to autograft alone (91.6%). However, the same meta-analysis discovered that when bioactive glass and autograft are used independently, bioactive glass alone is less successful (33.6% fusion) than autograft alone (98.8% fusion).6,11,27
New variations in chemical makeup have allowed for the expansion of bioactive glass functions and roles. Silver ions have demonstrated greater antimicrobial effects against bacteria, notably Pseudomonas and Staphylococcus species. The addition of strontium has been introduced for osteoporosis by inhibiting osteoclast activity in areas of weakened bone.6,11,27
Peptide Amphiphiles
As bioactive glasses strive to create an ideal environment with greater strength and healing, PAs provide a unique alternative to bone grafts. PAs are a class of molecules made up of hydrophilic and hydrophobic amino acids that often self-assemble into structures, tubular fibers, or hydrogels19 (Figure 4).30 This occurs due to the interaction between molecular and external factors such as pH, temperature, and exposure to salts.30 In 2001, PA molecules were developed with the ability to self-assemble and create an environment conducive to HA mineralization. Notably, this mineralization was analogous to the alignment seen between collagen fibrils and HA in bone.31 This created the opportunity to incorporate materials that would further enhance mineralization.32
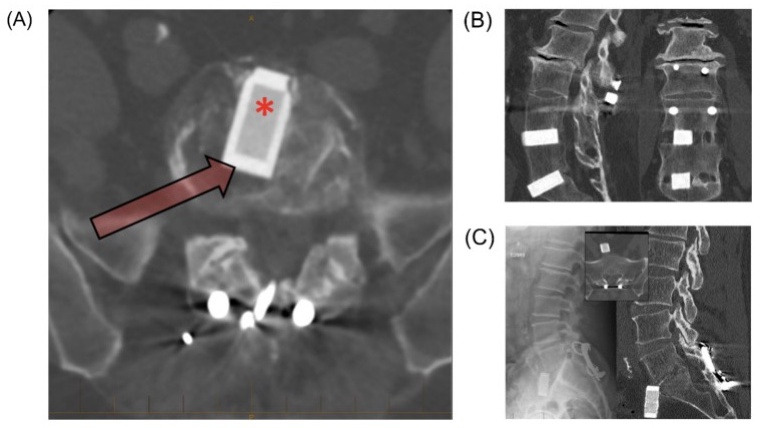
Figure 4.
Peptide amphiphile nanostructure.33 (A) Graphic rendering of peptide amphiphile with representative self-assembling nanofibers. (B) Scanning electron micrograph of peptide amphiphile nanofiber in aqueous solution. This image was reprinted with permission from Silva et al.33 Copyright 2004 The American Association for the Advancement of Science.
Bone morphogenetic protein-2 (BMP-2) is an important osteogenic bioactive factor that aids in bone defect repair and is often combined with various scaffolds to create an osteoinductive environment. Although BMP-2 enhances scaffold performance, it has an extensive side-effect profile, including complications such as ectopic bone formation, inflammation, hematoma, and increased cancer risk.30
One of the first PAs developed was heparin-binding PA, which can bind many different growth factors, such as vascular endothelial growth factor (VEGF) and fibroblast growth factor 2 (FGF-2). When heparan sulfate (HS) was combined with heparin-binding PA and BMP-2, fusion and bone bridging were achieved. Together, the PA and heparan sulfate provide an osteogenic environment, but individually, they were unable to achieve fusion. However, heparan sulfate carries some unwanted effects due to its anticoagulative properties.34
With the promise of PAs and growth factors working in combination, a BMP-2-binding PA (BMP-2bPA) was created. This more specific binding moiety works to confine growth factors to a desired location. This new model proved useful in its bioactive properties due to better stability and a longer half-life with the therapeutic dose of BMP-2 reduced by 10-fold.35 Alkaline phosphatase (ALP) activity is an important indicator of osteogenesis.36 Compared to BMP-2 alone, there was a significant increase in alkaline phosphatase activity and therefore osteogenesis with BMP2b-PA. Additionally, they discovered a 42% fusion rate when the BMP-2bPA was used without exogenous BMP-2, indicating the ability to recruit endogenous BMP-2. This PA provides a unique opportunity for the use of less BMP-2 for an equally robust result.35
While BMP-2 is a crucial growth factor, the success of osteogenesis introduced the possibility of incorporating other growth factors into PAs that target angiogenesis, such as VEGF and FGF.34,37 To achieve this, an HS mimetic PA known as glycopeptide PA (GPA) was created. By honing specific binding motifs, the creation of this mimetic eliminated the less desired effects of HS, such as anticoagulation.34 Due to the ability of the GPA molecules to rearrange, this new PA binds 5 important bone and vascular growth factors, including BMP-2, BMP-4, FGF-1, FGF-2, and VEGF.34 In a rat spinal fusion model, GPA has resulted in excellent fusion rates while maintaining a BMP-2 dose 100 times lower than that of the collagen sponge control.34 Since BMP has been associated with significant side effects, this dosage reduction may mitigate those risks while still providing a robust bone growth response.38 The use of PAs is still being pioneered to evaluate the best mechanism to enhance bone growth while creating an affordable product.
Future Directions and Conclusions
It is evident that synthetic graft substitutes and extenders have been and will continue to be integral to the evolution of future graft materials. Along with further development of the discussed synthetic materials, there are novel materials and technologies that are beginning to emerge as promising alternatives, particularly 3D-printed grafts, bone matrices30 and hydrogels.
Additive manufacturing, or 3D printing, has the ability to create custom scaffolds out of a variety of synthetic materials. These include ceramics, polymers, and other composites. The major benefit of 3D-printed models is their ability to control physical properties like porosity.39 There are several types of 3D printing, but the one most commonly used for biomedical purposes is a form of fused deposition modeling known as extrusion-based 3D printing. This method makes it possible to infuse growth factors, pharmaceuticals, cells, and proteins into the structure itself.40 In addition, it frequently uses DBMs and HA ceramics as the foundation. DBMs are allografts that have undergone an acid extraction process, facilitating the formation of an osteoconductive surface (Figure 5).41 3D printing has enabled engineers to form an HA-DBM scaffold with reduced fragility despite the presence of macropores. In a rat model assessing PLF, this composite HA-DBM scaffold demonstrated a fusion rate of 92% compared to 3D-HA-only scaffolds with a fusion rate of 58% and 3D-DBM-only scaffolds with a fusion rate of 42%. Apart from successful fusion, the HA-DBM 3D-printed scaffold did not elicit an immune or inflammatory response, and cytokine levels remained low postoperatively.6,30
Figure 5.
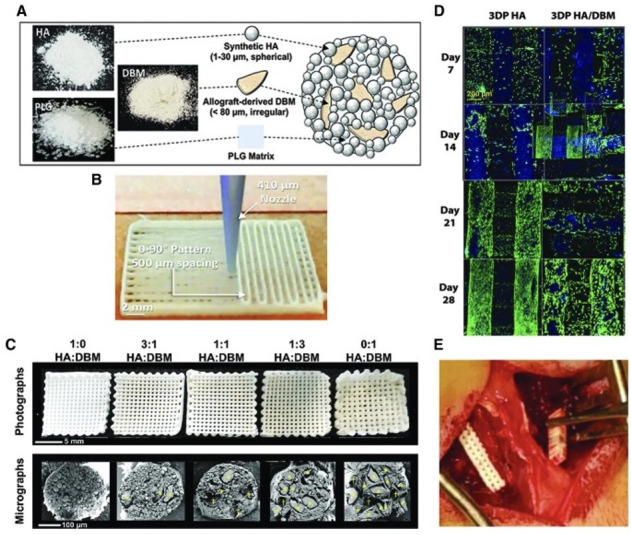
3D HA DBM implant.41 (A and B) Scaffold production and design. (C) Unimplanted scaffolds. Upper: scaffold structure demonstrating macropores. Lower: scanning electron microscope cross-section of struts. (D) Laser-scanning confocal z-projections of 3D-stacks from live-dead stained scaffold seeded with primary rat bone marrow stromal cells. Blue is autofluorescence from the scaffold materials. (E) Intraoperative implantation of a scaffold. This image is exempt from permissions due to same original author. Copyright 2020 Mary Ann Liebert, Inc.
While 3D-printing technology has been utilized to construct synthetic implant structures, it has also been used to create composite materials. The benefit of this innovation is the ability to produce composites with osteogenic and osteoconductive properties to enhance bone regeneration.6,42 Using nanocomposites as additives in products, such as 3D-titanium cages, allows for optimized structural stability and osteoblast activation. Hyperelastic Bone (Dimension Inx, Chicago, IL) is a nanocomposite product composed of HA and polymer binders. It aims to maximize implant elasticity and bone regeneration. In preliminary rat studies, it has demonstrated a 92% fusion rate.6
Apart from 3D printing, other substances have been developed to mimic the organ as a whole. This requires recreating not only the biological functions but also the microenvironment.30 This novel model, known as the bone organoid, has been posited as a future avenue for spinal fusion due to its promising results in bone regeneration.2 It is combined with Matrigel, a natural extracellular matrix (ECM) isolated from mouse tumors, as the supporting biomaterial.43 However, Matrigel has some drawbacks, including its inability to control its effect on gene expression and the variability of its composition.44 In recent years, hydrogels, biomaterials with adjustable functional properties and a 3D structure, have been utilized to replace Matrigel.45 These synthetic hydrogels form from amphiphilic peptide self-assembly into an ECM-like structure.
One hydrogel, polyethylene glycol (PEG), is easily modifiable to target specific tissue types and functionalization. In combination with HA, PEG hydrogel provides an analogous environment to bone marrow that is conducive to the proliferation and differentiation of human bone marrow-derived stromal cells, superior to the response elicited by Matrigel.46 Additionally, PEG can be employed as a “smart” hydrogel with growth factor or cell loading.47 In combination with osteogenic cells, hydrogels provide an ideal model with osteoinductive, osteoconductive, and osteogenic properties.48 They are an important avenue for future work.
3D printing and hydrogels are fast-growing areas of interest due to their highly customizable nature. The ability to create variations in physical properties as well as chemical makeup makes it an increasingly effective way to create superior therapies for degenerative spinal diseases as well as traumatic injuries. Even with the current initial successes of these products, further exploration and development will pave the way for even greater therapies and future formulations.
References
- 1. Sivasubramaniam V, Patel HC, Ozdemir BA, Papadopoulos MC. Trends in hospital admissions and surgical procedures for degenerative lumbar spine disease in England: a 15-year time-series study. BMJ Open. 2015;5(12):e009011. 10.1136/bmjopen-2015-009011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Katsuura Y, Shafi K, Jacques C, Virk S, Iyer S, Cunningham M. New strategies in enhancing spinal fusion. HSS J. 2020;16(2):177–182. 10.1007/s11420-020-09749-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ebraheim NA, Elgafy H, Xu R. Bone-graft harvesting from iliac and fibular donor sites: techniques and complications. J Am Acad Orthop Surg. 2001;9(3):210–218. 10.5435/00124635-200105000-00007 [DOI] [PubMed] [Google Scholar]
- 4. Khan SN, Cammisa FPJ, Sandhu HS, Diwan AD, Girardi FP, Lane JM. The biology of bone grafting. J Am Acad Orthop Surg. 2005;13(1):77–86. 10.5435/00124635-200501000-00010 [DOI] [PubMed] [Google Scholar]
- 5. Miller LE, Block JE. Safety and effectiveness of bone allografts in anterior cervical discectomy and fusion surgery. Spine (Phila Pa 1976). 2011;36(24):2045–2050. 10.1097/BRS.0b013e3181ff37eb [DOI] [PubMed] [Google Scholar]
- 6. Plantz MA, Gerlach EB, Hsu WK. Synthetic bone graft materials in spine fusion: current evidence and future trends. Int J Spine Surg. 2021;15(s1):104–112. 10.14444/8058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cyriac M, Kyhos J, Iweala U, et al. Anterior lumbar interbody fusion with cement augmentation without posterior fixation to treat Isthmic spondylolisthesis in an osteopenic patient-a surgical technique. Int J Spine Surg. 2018;12(3):322–327. 10.14444/5037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ortega B, Gardner C, Roberts S, Chung A, Wang JC, Buser Z. Ceramic biologics for bony fusion-a journey from first to third generations. Curr Rev Musculoskelet Med. 2020;13(4):530–536. 10.1007/s12178-020-09651-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nickoli MS, Hsu WK. Ceramic-based bone grafts as a bone grafts extender for lumbar spine arthrodesis: a systematic review. Global Spine J. 2014;4(3):211–216. 10.1055/s-0034-1378141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Du X, Lee SS, Blugan G, Ferguson SJ. Silicon nitride as a biomedical material: an overview. Int J Mol Sci. 2022;23(12):6551. 10.3390/ijms23126551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fiani B, Jarrah R, Shields J, Sekhon M. Enhanced biomaterials: systematic review of alternatives to supplement spine fusion including silicon nitride, bioactive glass, amino peptide bone graft, and tantalum. Neurosurg Focus. 2021;50(6):2021.3.FOCUS201044. 10.3171/2021.3.FOCUS201044 [DOI] [PubMed] [Google Scholar]
- 12. Calvert GC, VanBuren Huffmon G, Rambo WM, Smith MW, McEntire BJ, Bal BS. Clinical outcomes for lumbar fusion using silicon nitride versus other biomaterials. J Spine Surg. 2020;6(1):33–48. 10.21037/jss.2019.12.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liu M, Nemat-Nasser S. The microstructure and boundary phases of in-situ reinforced silicon nitride. Materials Science and Engineering: A. 1998;254(1–2):242–252. 10.1016/S0921-5093(98)00679-0 [DOI] [Google Scholar]
- 14. Mobbs RJ, Rao PJ, Phan K, et al. Anterior lumbar interbody fusion using reaction bonded silicon nitride implants: long-term case series of the first synthetic anterior lumbar interbody fusion spacer implanted in humans. World Neurosurg. 2018;120:256–264. 10.1016/j.wneu.2018.08.237 [DOI] [PubMed] [Google Scholar]
- 15. Lehr AM, Oner FC, Delawi D, et al. Efficacy of a standalone microporous ceramic versus autograft ininstrumented posterolateral spinal fusion: a multicenter, randomized, intrapatient controlled, noninferiority trial. Spine (Phila Pa 1976). 2020;45(14):944–951. 10.1097/BRS.0000000000003440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. van Dijk LA, Duan R, Luo X, et al. Biphasic calcium phosphate with submicron surface topography in an ovine model of instrumented posterolateral spinal fusion. JOR Spine. 2018;1(4):e1039. 10.1002/jsp2.1039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Belluomo R, Arriola-Alvarez I, Kucko NW, et al. Physico-chemical characteristics and posterolateral fusion performance of biphasic calcium phosphate with submicron needle-shaped surface topography combined with a novel polymer binder. Materials (Basel). 2022;15(4):1346. 10.3390/ma15041346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wuisman P, Smit TH. Bioresorbable polymers: heading for a new generation of spinal cages. Eur Spine J. 2006;15(2):133–148. 10.1007/s00586-005-1003-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ellis-Behnke RG, Schneider GE. Peptide amphiphiles and porous biodegradable scaffolds for tissue regeneration in the brain and spinal cord. Hurst SJ, Biomedical nanotechnology: methods and protocols. Humana Press; 2011:259–281. 10.1007/978-1-61779-052-2 [DOI] [PubMed] [Google Scholar]
- 20. Alizadeh-Osgouei M, Li Y, Wen C. A comprehensive review of biodegradable synthetic polymer-ceramic composites and their manufacture for biomedical applications. Bioact Mater. 2019;4(1):22–36. 10.1016/j.bioactmat.2018.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gomar F, Orozco R, Villar JL, Arrizabalaga F. P-15 small peptide bone graft substitute in the treatment of non-unions and delayed union. A pilot clinical trial. Int Orthop. 2007;31(1):93–99. 10.1007/s00264-006-0087-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Loenen ACY, Connor J, Johnson S, et al. Peptide enhanced bone graft substitute presents improved short-term increase in bone volume and construct stiffness compared to iliac crest autologous bone in an ovine lumbar interbody fusion model. Global Spine J. 2022;12(7):1330–1337. 10.1177/2192568220979839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Axelsen MG, Overgaard S, Jespersen SM, Ding M. Comparison of synthetic bone graft ABM/P-15 and allograft on uninstrumented posterior lumbar spine fusion in sheep. J Orthop Surg Res. 2019;14(1):2:2. 10.1186/s13018-018-1042-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cunningham BW, Atkinson BL, Hu N, et al. Ceramic granules enhanced with B2A peptide for lumbar interbody spine fusion: an experimental study using an instrumented model in sheep: laboratory investigation. J Neurosurg Spine. 2009;10(4):300–307. 10.3171/2009.1.SPINE08565 [DOI] [PubMed] [Google Scholar]
- 25. Smucker JD, Bobst JA, Petersen EB, Nepola JV, Fredericks DC. B2A peptide on ceramic granules enhance posterolateral spinal fusion in rabbits compared with autograft. Spine (Phila Pa 1976). 2008;33(12):1324–1329. 10.1097/BRS.0b013e3181732a74 [DOI] [PubMed] [Google Scholar]
- 26. Sardar Z, Alexander D, Oxner W, et al. Twelve-month results of a multicenter, blinded, pilot study of a novel peptide (B2A) in promoting lumbar spine fusion. J Neurosurg Spine. 2015;22(4):358–366. 10.3171/2013.11.SPINE121106 [DOI] [PubMed] [Google Scholar]
- 27. Cottrill E, Pennington Z, Lankipalle N, et al. The effect of bioactive glasses on spinal fusion: a cross-disciplinary systematic review and meta-analysis of the Preclinical and clinical data. J Clin Neurosci. 2020;78:34–46. 10.1016/j.jocn.2020.04.035 [DOI] [PubMed] [Google Scholar]
- 28. Baino F, Hamzehlou S, Kargozar S. Bioactive glasses: where are we and where are we going? J Funct Biomater. 2018;9(1):25. 10.3390/jfb9010025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ilharreborde B, Morel E, Fitoussi F, et al. Bioactive glass as a bone substitute for spinal fusion in adolescent idiopathic scoliosis: a comparative study with iliac crest autograft. J Pediatr Orthop. 2008;28(3):347–351. 10.1097/BPO.0b013e318168d1d4 [DOI] [PubMed] [Google Scholar]
- 30. Phan EN, Hsu WK. Novel approaches guiding the future of spinal biologics for bone regeneration. Curr Rev Musculoskelet Med. 2022;15(3):205–212. 10.1007/s12178-022-09757-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Greene AC, Hsu WK. Technologies to enhance spinal fusion: bench to bedside. HSS J. 2020;16(2):108–112. 10.1007/s11420-019-09733-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mata A, Geng Y, Henrikson KJ, et al. Bone regeneration mediated by biomimetic mineralization of a nanofiber matrix. Biomaterials. 2010;31(23):6004–6012. 10.1016/j.biomaterials.2010.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Silva GA, Czeisler C, Niece KL, et al. Selective differentiation of neural progenitor cells by high-EPITOPE density nanofibers. Science. 2004;303(5662):1352–1355. 10.1126/science.1093783 [DOI] [PubMed] [Google Scholar]
- 34. Lee SS, Fyrner T, Chen F, et al. Sulfated glycopeptide nanostructures for multipotent protein activation. Nat Nanotechnol. 2017;12(8):821–829. 10.1038/nnano.2017.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lee SS, Hsu EL, Mendoza M, et al. Gel scaffolds of BMP-2-binding peptide amphiphile nanofibers for spinal arthrodesis. Adv Healthc Mater. 2015;4(1):131–141. 10.1002/adhm.201400129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sharma U, Pal D, Prasad R. Alkaline phosphatase: an overview. Indian J Clin Biochem. 2014;29(3):269–278. 10.1007/s12291-013-0408-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hu K, Olsen BR. The roles of vascular endothelial growth factor in bone repair and regeneration. Bone. 2016;91:30–38. 10.1016/j.bone.2016.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. James AW, LaChaud G, Shen J, et al. A review of the clinical side effects of bone morphogenetic protein-2. Tissue Eng Part B Rev. 2016;22(4):284–297. 10.1089/ten.TEB.2015.0357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Turnbull G, Clarke J, Picard F, et al. 3D bioactive composite scaffolds for bone tissue engineering. Bioact Mater. 2018;3(3):278–314. 10.1016/j.bioactmat.2017.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ouyang L. Pushing the rheological and mechanical boundaries of extrusion-based 3d bioprinting. Trends Biotechnol. 2022;40(7):891–902. 10.1016/j.tibtech.2022.01.001 [DOI] [PubMed] [Google Scholar]
- 41. Driscoll JA, Lubbe R, Jakus AE, et al. 3d-printed ceramic-demineralized bone matrix hyperelastic bone composite scaffolds for spinal fusion. Tissue Eng Part A. 2020;26(3–4):157–166. 10.1089/ten.TEA.2019.0166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Van Eps JL, Fernandez-Moure JS, Cabrera FJ, et al. Improved posterolateral lumbar spinal fusion using a biomimetic, nanocomposite scaffold augmented by autologous platelet-rich plasma. Front Bioeng Biotechnol. 2021;9:622099. 10.3389/fbioe.2021.622099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Klotz BJ, Oosterhoff LA, Utomo L, et al. A versatile biosynthetic hydrogel platform for engineering of tissue analogues. Adv Healthc Mater. 2019;8(19):e1900979. 10.1002/adhm.201900979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Benton G, Arnaoutova I, George J, Kleinman HK, Koblinski J. Matrigel: from discovery and ECM mimicry to assays and models for cancer research. Adv Drug Deliv Rev. 2014;79–80:3–18. 10.1016/j.addr.2014.06.005 [DOI] [PubMed] [Google Scholar]
- 45. Xue X, Hu Y, Wang S, Chen X, Jiang Y, Su J. Fabrication of physical and chemical crosslinked hydrogels for bone tissue engineering. Bioact Mater. 2022;12:327–339. 10.1016/j.bioactmat.2021.10.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wu S, Wu X, Wang X, Su J. Hydrogels for bone organoid construction: from a materiobiological perspective. Journal of Materials Science & Technology. 2023;136:21–31. 10.1016/j.jmst.2022.07.008 [DOI] [Google Scholar]
- 47. Xue X, Zhang H, Liu H, et al. Rational design of multifunctional cus nanoparticle-PEG composite soft hydrogel-coated 3d hard polycaprolactone scaffolds for efficient bone regeneration. Adv Funct Materials. 2022;32(33):2202470. https://onlinelibrary.wiley.com/toc/16163028/32/33. 10.1002/adfm.202202470 [DOI] [Google Scholar]
- 48. Vo TN, Shah SR, Lu S, et al. Injectable dual-Gelling cell-laden composite hydrogels for bone tissue engineering. Biomaterials. 2016;83:1–11. 10.1016/j.biomaterials.2015.12.026 [DOI] [PMC free article] [PubMed] [Google Scholar]