Abstract
Background
Dermatological conditions, especially when severe, can lead to sleep disturbances that affect a patient’s quality of life. However, limited research exists on the efficacy of treatments for improving sleep parameters in skin conditions.
Objective
The objective was to perform a systematic review of the literature on dermatological conditions and the treatments available for improving sleep parameters.
Methods
A literature review was performed using the PubMed, Ovid MEDLINE, Embase, Cochrane, and ClinicalTrials.gov databases from 1945 to 2021. After filtering based on our exclusion criteria, studies were graded using the SORT (Strength of Recommendation Taxonomy) algorithm, and only those receiving a grade of “2” or better were included.
Results
In total, 25 treatment studies (n=11,025) assessing sleep parameters related to dermatological conditions were found. Dupilumab appeared to be the best-supported and most effective treatment for improving sleep in atopic dermatitis (AD) but had frequent adverse effects. Topical treatments for AD were mostly ineffective, but procedural treatments showed some promise. Treatments for other conditions appeared efficacious.
Conclusions
The evaluation of sleep parameter changes in dermatological treatments is predominantly restricted to AD. Systemic interventions such as dupilumab and procedural interventions were the most efficacious. Sleep changes in other dermatoses were limited by a paucity of available studies. The inclusion of a sleep assessment component to a broader range of dermatological treatment studies is warranted.
Keywords: sleep, dermatology, atopic dermatitis, chronic idiopathic urticaria, quality of life, literature review, parameter, teledermatology, dermatologist, skin, epidermis, review, polysomnography, polysomnographic, sleep medicine
Introduction
The importance of sleep and the consequences of sleep deprivation on the patient’s quality of life have been thoroughly defined, with decreased health-related quality of life survey measures and daytime impairment [1,2]. Dermatological conditions can affect patients’ lives in numerous ways, with sleep disturbance as one of the most debilitating effects. Sleep may cause aberrations of skin functions, specifically with thermoregulation and fluid balance maintenance. Disruptions in these regulatory mechanisms may contribute to nocturnal pruritus [3,4].
The impact of these conditions on sleep, whether in terms of quality or duration, however, remains understudied. The efficacy of different dermatological treatments for improving sleep parameters is not always clear to clinicians. In this review, we performed a literature search regarding the effects of different treatments on sleep disturbances across dermatological conditions. After filtering studies according to our exclusion criteria, those relating to atopic dermatitis, pruritus and xerosis, prurigo nodularis, and chronic idiopathic urticaria were found.
Methods
We conducted a literature search using the keywords “sleep disturbance,” “dermatology,” and “management” from the PubMed, Ovid MEDLINE, Embase, Cochrane, and ClinicalTrials.gov databases. We included studies from 1945 to September 2021 in our initial review, yielding 1863 results. After discarding duplicates, 973 unique studies were analyzed by 2 independent reviewers (VG and IM) for relevant information pertaining to treatments for sleep management in dermatological conditions, yielding 25 studies for further analysis (Figure 1 and Multimedia Appendix 1 [5]).
Figure 1.
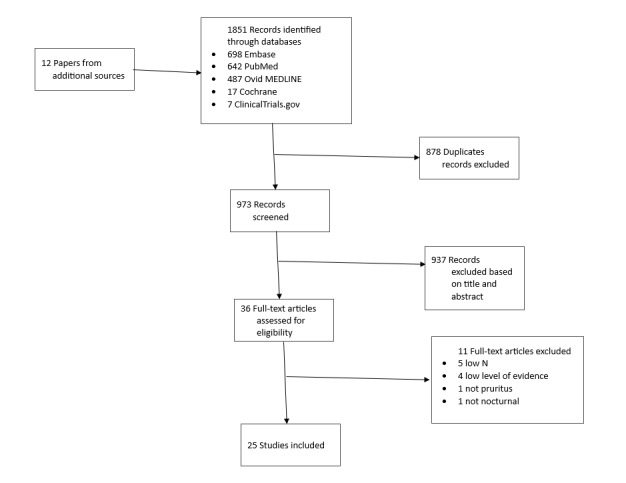
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart.
All disputes were settled by a third independent reviewer (VK). Inclusion criteria included peer-reviewed original articles involving various treatment modalities for sleep management in the form of randomized controlled trials (RCTs) and cohort studies. Only studies that focused solely on dermatological conditions were included. The SORT (Strength of Recommendation Taxonomy) algorithm was used to quantify the level of evidence [6]. Studies that received a level of evidence score worse than a “2” were excluded.
Results
Characteristics of Included Studies
The 26 studies included in this review encompass a total of 11,022 patients. Of these, 21 studies were included for AD, encompassing 4111 patients (n=164, ~4% pediatric patients). A total of 2 studies were included for pruritus and xerosis, including 5965 patients. Only 1 study was included for prurigo nodularis, psoriasis vulgaris, and chronic idiopathic pruritus, analyzing 27 patients, 394 patients, and 525 patients, respectively. Collectively, the studies spanned a period from 1979 to 2021.
Treatment for Atopic Dermatitis
Overview
A wide array of studies has evaluated the efficacy of treatments for AD and concomitant sleep disturbances. These can broadly be arranged into 3 groups, according to whether the treatment modality was systemic, topical, or procedural. Each of the study details, with respective treatment adverse effects, is further delineated in Tables 1 and 2. Sources of funding for each study are provided in Table 3.
Table 1.
Treatments for sleep management in skin disease.
| Study | Disease | Intervention | Level of evidence | Study design | Sample size, N | Dosage | Sleep scale | Outcomes |
| Fargnoli et al [7] (2019) | ADa | Dupilumab | 2 | Retrospective cohort | 109 |
|
|
|
| Cork et al [8] (2019) | AD | Dupilumab | 1 | Pooled data from RCTsd | 1379 |
|
|
|
| Tsianakas et al [9] (2017) | AD | Dupilumab | 1 | RCT | 64 |
|
|
|
| Tofte et al [10] (2018) | AD | Dupilumab | 1 | Pooled data from RCTs | 233 |
|
|
|
| Paller [11] (ongoing clinical trial) | AD | Dupilumab | 2 | Open label | 40 (pediatric) |
|
|
|
| Chang et al [12] (2016) | AD | Melatonin | 1 | RCT | 73 (pediatric) |
|
|
|
| Harper et al [13] (2000) | AD | Cyclosporine | 2 | Prospective, parallel, open label | 40 (pediatric) |
|
|
|
| Silverberg et al [14] (2021) | AD | Abrocitinib | 1 | Pooled data from RCTs | 942 |
|
|
|
| Lio et al [15] (2021) | AD | Baricitinib | 1 | Prospective analysis from RCT data | 440 |
|
|
|
| Kawana et al [16] (2010) | AD | Tandospirone citrate | 1 | RCT | 37 |
|
|
|
| Munday et al [17] (2002) | AD | Chlorpheniramine | 1 | RCT | 151 |
|
|
|
| Ebata et al [18] (1997) | AD | Nitrazepam | 2 | RCT crossover | 10 |
|
|
|
| Savin et al [19] (1979) | AD | Trimeprazine and trimipramine | 2 | RCT | 12 |
|
|
|
| Parikh-Das et al [20] (2017) | AD | Colloidal oatmeal cream | 1 | RCT | 23 (pediatric) |
|
|
|
| Ständer et al [21] (2016) | AD | Sertaconazole 2% cream | 1 | RCT | 70 |
|
|
|
| Kubota et al [22] (2009) | AD | Corticosteroids and tacrolimus (both topical) | 2 | Open label, uncontrolled | 28 (pediatric) |
|
|
|
| Doss et al [23] (2009) | AD | Tacrolimus 0.03% ointment | 1 | RCT | 240 |
|
|
|
| Leo et al [24] (2004) | AD | Pimecrolimus cream 1% | 2 | RCT | 19 |
|
|
|
| Jaworek et al [25] (2020) | AD | UV-B/cyclosporine | 2 | Open label, uncontrolled | 42 |
|
|
|
| Pustišek et al [26] (2016) | AD | Short-term structured educational program | 1 | RCT | 134 |
|
|
|
| Bae et al [27] (2012) | AD | PMRx | 2 | RCT | 25 |
|
|
|
| Deleuran et al [28] (2020) | Pruritus and xerosis | ADE-G1z emollient | 2 | Open label | 5910 |
|
|
|
| Rossi et al [29] (2016) | Pruritus and xerosis | Polidocanol (2%) and prucidine-4 (0.5%) lotion | 2 | Open label | 55 |
|
|
|
| Chiricozzi et al [30] (2020) | Prurigo nodularis | Dupilumab | 2 | Retrospective cohort | 27 |
|
|
|
| Kontochristopoulos et al [31] (2016) | Psoriasis vulgaris | Calcipotriol-betamethasone dipropionate gel | 2 | Prospective open-label study | 394 |
|
|
|
| Zuberbier et al [32] (2009) | Chronic idiopathic pruritus | Bilastine or levocetirizine | 1 | RCT | 525 |
|
|
|
aAD: atopic dermatitis.
bQ2W: once every 2 weeks.
cNRS: numerical rating scale.
dRCT: randomized controlled trial.
eQW: once weekly.
fSCORAD: Scoring Atopic Dermatitis.
gPOEM: Patient-Oriented Eczema Measure.
hVAS: visual analog scale.
iPROMIS: Patient Reported Outcome Measurement Information System.
jQD: once a day.
kUsing a linear mixed-effects model after controlling for age and sex.
lSASSAD: 6 area, six sign atopic dermatitis.
mNTIS: Night Time Itch Scale.
nADSS: Atopic Dermatitis Sleep Scale.
oBSA: body surface area.
pTC: tandospirone citrate.
qQDpm: once a day in the evening.
rBID: twice a day.
sTST: total scratching time.
tEEG: electroencephalogram.
uQDam: once a day in the morning.
vAIS: Athens Insomnia Scale.
wPO: patient oriented.
xPMR: progressive muscle relaxation.
yLOS: loss of sleep.
zADE-G1: Aquaphilus dolomiae extract.
Table 2.
Adverse effects of treatment.
| Disease and therapy | Recommended dosage or treatment schedule | Adverse effects | References | ||||
| ADa | |||||||
|
|
Dupilumab |
|
Exacerbation of AD symptoms, nasopharyngitis, headache, conjunctivitis, and fatigue | [7-11] | |||
|
|
Melatonin |
|
None | [12] | |||
|
|
Cyclosporine |
|
Rhinitis, infected eczema, bronchospasm, upper respiratory tract infection, and headache | [13] | |||
|
|
Tandospirone citrate |
|
Not mentioned | [16] | |||
|
|
Abrocitinib |
|
Not mentioned | [14] | |||
|
|
Baricitinib |
|
Not mentioned | [15] | |||
|
|
Chlorpheniramine |
|
Mentioned but not described | [17] | |||
|
|
Nitrazepam |
|
Not mentioned | [18] | |||
|
|
Trimeprazine |
|
Not mentioned | [19] | |||
|
|
Trimipramine |
|
Not mentioned | [19] | |||
|
|
Sertaconazole 2% cream |
|
Exacerbation of AD | [33] | |||
|
|
Tacrolimus 0.03% or corticosteroids |
|
Folliculitis | [21] | |||
|
|
Tacrolimus 0.03% |
|
Burning sensation, pruritus, bronchitis, rhinitis | [22] | |||
|
|
Pimecrolimus 1% |
|
Not mentioned | [24] | |||
|
|
Colloidal oatmeal cream |
|
Not mentioned | [20] | |||
|
|
UV-B |
|
None | [25] | |||
|
|
PMRh therapy |
|
Not mentioned | [27] | |||
|
|
Structured education program |
|
Not mentioned | [26] | |||
| Pruritus and xerosis | |||||||
|
|
ADE-GIi emollient |
|
Skin irritation, itch, and burning sensation | [28] | |||
|
|
Polidocanol (2%) and prucidine-4 (0.5%) lotion |
|
Not mentioned | [29] | |||
| Chronic idiopathic urticarial | |||||||
|
|
Bilastine |
|
Headache and somnolence | [32] | |||
|
|
Levocetirizine |
|
Headache and somnolence | [32] | |||
| Prurigo nodularis | |||||||
|
|
Dupilumab |
|
Conjunctivitis | [30] | |||
aAD: atopic dermatitis.
bQ2W: once every 2 weeks.
cQD: once a day.
dQDpm: once a day in the evening.
eBID: twice a day.
fQDam: once a day in the morning.
gPRN: as needed.
hPMR: progressive muscle relaxation.
iADE-GI: Aquaphilus dolomiae extract.
Table 3.
Funding sources.
| Study | Disease | Funding sources |
| Fargnoli et al [7] (2019) | ADa | None |
| Cork et al [8] (2019) | AD | Sanofi/Regeneron |
| Tsianakas et al [9] (2017) | AD | Sanofi/Regeneron |
| Tofte et al [10] (2018) | AD | Sanofi/Regeneron |
| Paller [11] (ongoing clinical trial) | AD | Not mentioned |
| Chang et al [12] (2016) | AD | National Taiwan University Hospital and the Yonghe Cardinal Tien Hospital |
| Harper et al [13] (2000) | AD | Novartis Pharmaceuticals |
| Silverberg et al [14] (2021) | AD | Pfizer |
| Lio et al [15] (2021) | AD | Eli Lilly and Company |
| Kawana et al [16] (2010) | AD | Not mentioned |
| Munday et al [17] (2002) | AD | Not mentioned |
| Ebata et al [18] (1997) | AD | Not mentioned |
| Savin et al [19] (1979) | AD | May and Baker Ltd |
| Parikh-Das et al [20] (2017) | AD | Johnson & Johnson |
| Ständer et al [21] (2016) | AD | Not mentioned |
| Kubota et al [22] (2009) | AD | None |
| Doss et al [23] (2009) | AD | Astellas Pharma Europe Limited |
| Leo et al [24] (2004) | AD | Not mentioned |
| Jaworek et al [25] (2020) | AD | Not mentioned |
| Pustišek et al [26] (2016) | AD | None |
| Bae et al [27] (2012) | AD | Korea Health 21 R&D Project |
| Deleuran et al [28] (2020) | Pruritus and xerosis | Pierre Fabre Dermo-Cosmetique |
| Rossi et al [29] (2016) | Pruritus and xerosis | Not mentioned |
| Chiricozzi et al [30] (2020) | Prurigo nodularis | None |
| Kontochristopoulos et al [31] (2016) | Psoriasis vulgaris | Leo Greece |
| Zuberbier et al [32] (2009) | Chronic idiopathic pruritus | Not mentioned |
aAD: atopic dermatitis.
Systemic
Dupilumab, a monoclonal antibody that exerts its effect by blocking interleukin (IL)-4 and IL-13 signaling, is a frequently studied treatment of AD. Using pooled data from 2 RCTs comprising a total of 1379 patients, 1 study using dupilumab found improvements in 2 sleep measures, Scoring Atopic Dermatitis (SCORAD) and Patient-Oriented Eczema Measure (POEM), in 2 treatment groups compared with a control. SCORAD and POEM are clinical tools used to define the eczema severity and monitor its progression [34]. The 2 cohorts either received a once weekly or once every 2 weeks injection of 300 mg dupilumab. Mean decreases in SCORAD were 3.4 (SE 0.14) and 3.3 (SE 0.14) for the weekly and biweekly treatments, respectively. Both significantly outperformed the placebo group (P<.001). In the POEM measure, more patients reported an absence of sleep disturbance in the weekly (n=199, 43.5%) and biweekly (n=234, 51.2%) groups compared with the placebo group (n=81, 17.6%; P<.001) [8].
Another study found significant improvement in visual analog scale (VAS) sleep loss scores for patients with AD undergoing dupilumab treatment. In the 2 pooled RCTs, 300 mg injections were given subcutaneously either weekly or every other week. At week 12, the mean decrease in VAS sleep loss scores for weekly injections was 75% (SD 5.13%) and for biweekly was 52% (SD 10.79%) when compared to the 19.7% (SD 6.17%) and 3.8% (SD 11.55%) reductions for each respective placebo group (P=.001) [10]. Similarly, another study that investigated 300 mg dupilumab implemented SCORAD VAS scores to assess sleep loss. A mean percentage decrease of 66% (SD 17.78%) was observed in the dupilumab group when compared to the placebo group [9]. In a retrospective cohort study, 109 patients received an initial injection of 600 mg dupilumab followed by another 300 mg every other week. A reduction in the Sleep numerical rating scale was seen in the treatment group at 4 weeks (7 to 3) and at 16 weeks (3 to 2; P<.001) [7].
A single ongoing, phase 4 clinical trial using dupilumab for patients with pediatric AD was also found. An estimated 40 participants will be recruited, and a once-weekly subcutaneous injection, based on body weight, will be administered for a total of 12 weeks. Primary sleep outcome measurements include the PROMIS (Patient Reported Outcome Measurement Information System) parent-proxy score, the PROMIS patient score, and a polysomnography-based wake after sleep onset [11].
Melatonin supplementation, given its suppressive effects of autotaxin, has also been attempted as a treatment for sleep disturbance in children with AD [35]. In a double-blinded RCT of 73 children and adolescents, 3 mg of melatonin daily was compared to a placebo. Sleep measures included SCORAD, actigraphy, and subjective assessment. Compared with placebo, melatonin reduced the SCORAD measure by 9.1 (P<.001) and reduced sleep-onset latency by 21.4 minutes (P=.02) [12].
Cyclosporine therapy, given it reduces epidural nerve density, is another potential treatment option for childhood AD [36]. One prospective randomized, parallel study compared short course versus continuous treatment schedules. A total of 40 pediatric patients either underwent multiple 12-week courses or a continued 1-year course of 5 mg/kg/day cyclosporine. Improvement in sleep disturbance was observed in all treatment groups, although no values or P values were given. A tolerability of 80% was observed at week 12 and at the end of the study [13].
Tandospirone citrate, a 5-HT1A receptor agonist, has been used to reduce stress-related symptoms of AD. One RCT of 37 patients assessed the efficacy of tandospirone citrate at a dosage of 10 mg 3 times daily for 4 weeks. Both SCORAD and an insomnia VAS were used to measure changes in sleep. A significant decrease was observed in SCORAD for the treatment group after 4 weeks (P<.001), which was not observed with the control group. However, no significant difference was observed between the groups in either SCORAD or the insomnia VAS [16].
Abrocitinib, a JAK1 inhibitor, was assessed in 1 study using pooled data from 3 RCTs, with a total of 942 patients [37]. Patients received 200 mg, 100 mg, or placebo once daily for 12 weeks, with sleep outcomes measured using the Night Time Itch Scale (NTIS). The percentage of patients reporting a change in NTIS score of >4 was 57% (n=207), 42.7% (n=158), and 12.7% (n=27) for 200 mg, 100 mg, and placebo, respectively. Moreover, the percentage of patients who reported a response in NTIS score after 12 weeks, when compared to placebo, was 44.6% for 200 mg (n=162; P<.001) and 29.8% for 100 mg (n=110; P<.001) [14].
Baricitinib, another JAK inhibitor, was studied in post hoc analysis of data from a phase 3, multicenter, double-blinded RCT of 440 patients, which compared once-daily dosages of 1 mg and 2 mg baricitinib to placebo after 16 weeks. In patients with a baseline body surface area involvement of 10% to 50%, a decrease of at least 1.5 points in the number of nighttime awakenings caused by itch was observed for 2 mg (P=.001) but not 1 mg (P=.15) groups versus placebo. For patients with a baseline Atopic Dermatitis Sleep Scale score ≥1.5, a decrease of at least 1.5 points in the number of nighttime awakenings caused by itch was observed for both 1 mg (P=.04) and 2 mg (P<.001) versus placebo. Adverse effects were not mentioned [15].
Chlorpheniramine, an antihistamine, was assessed in 1 RCT of 151 patients with AD, with no significant difference being observed in AD symptoms when compared to placebo. Dosages included 2.5 mL versus 5 mL, given once at night. There was also no difference in the severity of daytime drowsiness and the number of episodes of sleeplessness [17].
Ebata et al [18] investigated nitrazepam, a benzodiazepine believed to reduce itch by sedation, and found no significant effects on nocturnal scratching behavior. Ten patients either took 5 mg nitrazepam once nightly for 2 consecutive days or 10 mg for 1 night, followed by a 4-day washout period. A decrease in frequency in nocturnal scratching bouts was observed at the 10 mg dosage; however, this coincided with an increase in mean scratching duration. Hence, no significant difference was observed in TST% when compared to placebo [18].
Trimeprazine, an antihistamine and sedative, and trimipramine, a tricyclic antidepressant, were tested against a placebo in 1 double-blinded randomized trial of 12 patients with severe AD. Patients underwent a 3-day treatment course of either 20 mg trimeprazine tartrate, 50 mg trimipramine maleate, or placebo once at night. Electroencephalogram recordings were used to measure wakefulness and stages of sleep. No significant differences were found in total time asleep, sleep latency, or wakefulness once asleep [19].
Topical
Sertaconazole, an antifungal that inhibits ergosterol synthesis, was studied in 1 double-blind RCT with 70 subjects [33]. Topical 2% sertaconazole cream was applied twice daily for 4 weeks. The SCORAD measure was used to assess changes in sleep. No significant differences were observed between sertaconazole and the vehicle control [21].
Given AD has been hypothesized to arise from immune dysregulation, studies have also examined tacrolimus, a calcineurin inhibitor that inhibits T-cell proliferation [38]. In 1 study, 28 patients were treated with sequential application of topical tacrolimus and corticosteroids in a 4-phase treatment process. In phase 1, patients applied 0.03% tacrolimus ointment every morning and a corticosteroid ointment every night for 2 weeks. In phase 2, the same concentration of tacrolimus ointment was applied twice daily for 2 weeks, with the addition of the corticosteroid ointment on weekends. Phase 3 eliminated the corticosteroid treatment while continuing tacrolimus twice daily for 2 weeks. The fourth and final phase involved the application of an emollient once daily, with tacrolimus application as needed for a total of 6 weeks. A 4-point sleep disturbance scale was used to assess changes in sleep disturbance. A decrease was observed from a baseline of 1.0 to 0.03 and 0.04 at 6 and 12 weeks, respectively (P<.001) [22].
Topical tacrolimus has also been compared to topical fluticasone, a corticosteroid agent and T-cell proliferation inhibitor [39]. Tacrolimus or fluticasone was applied twice daily until the clearance of lesions. If lesions persisted by week 3, the application was continued once daily for an additional 3 weeks. Sleep quality, measured with VAS, improved in both groups but with no significant difference [23].
Another immunomodulatory agent, which inhibits calcineurin, pimecrolimus, has also been tested for AD treatment [40]. In 1 RCT of 19 pediatric patients experiencing AD, pimecrolimus cream was not shown to be effective in improving sleep parameters, specifically sleep duration and wakefulness. Moreover, no difference was observed in sleep parameters between the treatment and control groups [24].
Colloidal oatmeal, an anti-inflammatory and antihistaminergic agent via avenanthramide, is another potential treatment option for AD [41]. In 1 study, 23 infants and toddlers with AD received colloidal oatmeal lotion for 14 days. Sleep quality was assessed “clinically and instrumentally,” with improvement noted in continuous sleep duration and number of wakings. The degree and timing of these improvements were not specified [20].
Procedural
UV phototherapy is a common treatment for dermatoses by stimulating prostaglandins and cytokine synthesis [42]. One study compared the efficacy of UV-B and cyclosporine on sleep disturbance secondary to AD, by implementing the Athens Insomnia Scale. UV-B dosage began at 0.22-0.26 J/cm2 and was increased every second session until erythema appeared. Doses were given 3 times a week, with a maximum dose of 0.56 J/cm2. The baseline cyclosporine dosage was 3.5 mg/kg/d, divided in 2 doses, and increased after 2 weeks, with a maximum dose of 5 mg/kg/d. Patients either received UV-B or cyclosporine for a period of 12 weeks. Itch reduction was achieved in both treatment groups, with more significant itch reduction in the UV-B cohort (P<.001). Moreover, UV-B treatment resulted in a reduction from 13.5 to 4 in mean Athens Insomnia Scale scores (P<.001). Cyclosporine, likewise, led to a mean reduction of 13.9 (SD 1.8) to 5.9 (SD 0.9; P<.001) [25].
Progressive muscle relaxation (PMR) therapy is a form of psychological therapy primarily used for stress management [43]. In 1 RCT, 25 patients were randomly assigned to either receive 1 month of PMR therapy in addition to conventional treatment or only undergo 1 month of conventional treatment. A significant decrease in sleep loss horizontal VAS scores was observed in the PMR group but not the control group (P=.007) [27].
Structured parental intervention, which consisted of a 2-hour physician lecture, was evaluated for improving sleep in 1 study of 134 children with AD. Sleep parameters were measured using SCORAD, patient-oriented (PO) SCORAD index, and sleeplessness and evaluated at the second visit (2 mo after initial evaluation). By the second visit, the mean SCORAD scores for the intervention group were 23.08 (SD 15.188) versus 36.44 (SD 16.760) for the control group (P=.001), and PO SCORAD index scores were 24.92 (SD 16.572) and 38.31 (SD 16.253), respectively (P=.001). Likewise, sleep disturbance means were 2.94 (SD 2.981) for the intervention group and 4.69 (SD 2.943) for the control group (P=.001) [26].
Treatment for Pruritus and Xerosis
Aquaphilus dolomiae extract, a biomanufactured derivative from Aquaphilus dolomiae, has been shown in vitro to counteract the mitogenic effects on CD-4+ T-cells, which may result in immunosuppressive effects [44-46]. One open-label study of 5910 patients evaluated the effects of an emollient containing Aquaphilus dolomiae extract on pruritus and xerosis severity and sleep disturbance. The application was done twice daily for 7 days. A VAS derived from the SCORAD index was used to measure changes in sleep, with 0 representing “no sleep disturbance” and 10 representing “very severe sleep disturbance.” After the treatment period, a decrease from 3.3 to 1.3 in sleep score was observed (P<.001) [28].
Polidocanol is a local anesthetic agent shown to have an antipruritic effect on nonhistamine-induced itch [47]. Prucidine-4 is an antipruritic formulation reported to act as a TRPV1 antagonist [48]. One open-label study with 55 patients with xerosis compared compounded polidocanol (2%) to prucidine-4 (0.5%) lotion. Both were applied at least twice daily for 28 days, and each led to a decrease in insomnia scores from 2 to 0 after 28 days (P<.001) [29].
Treatment for Chronic Idiopathic Urticaria
Bilastine and levocetirizine, both H1-receptor antagonists, were compared in 1 RCT on sleep parameters of 525 patients diagnosed with chronic idiopathic urticaria. Patients either received 20 mg bilastine or 5 mg levocetirizine once daily for 28 days. Assessment of sleep was measured using a 5-point sleep disturbance scale. Overall, by 14 and 28 days, a greater percentage of patients treated with bilastine (n=89, 54.6%; n=106, 62.7%) and levocetirizine (n=103, 66.9%; n=115, 72.3%) reported having no sleep disturbance, respectively, when compared to placebo (n=55, 33.4%; n=76, 42.7%; P<.001) [32].
Treatment for Prurigo Nodularis
One retrospective study of dupilumab was performed with 27 patients with prurigo nodularis. An initial loading dose of 600 mg was given via subcutaneous injection, followed by 300 mg injections every other week. Mean sleeplessness numerical rating scale scores decreased from a baseline of 8.2 (SD 2.0) to 1.7 (SD not given), after 16 weeks of treatment (P<.001) [30].
Treatment for Psoriasis Vulgaris
One open-label study evaluated the effect of calcipotriol-betamethasone dipropionate gel in 394 Greek patients with psoriasis vulgaris. The gel was applied once daily for 4 weeks, with various quality-of-life assessments performed before and after the treatment period. Sleep disturbance was measured using a subjective survey, ranging from 1 (no itching) to 10 (worst state). By the end of the treatment period, a significant decrease in mean score from baseline was observed (P<.001) [31].
Discussion
Summary
In this review, a variety of studies assessed treatment efficacy in influencing sleep parameters for dermatological conditions, predominantly AD. Given the inclusion of sleeplessness in SCORAD, a robust clinical tool to assess atopic dermatitis, this result is not surprising. Therefore, the inclusion of a sleep measure into clinical tools assessing other kinds of dermatological conditions may be beneficial.
In terms of atopic dermatitis, 3 broad classes of treatment were found: systemic, topical, and procedural. Among systemic treatments, dupilumab was the most studied. It was shown to be efficacious in improving sleep parameters. All published dupilumab studies for AD found significant improvements in sleep disturbance, sleep quality, and sleep loss. This may be secondary to the notable effect of dupilumab to rapidly reduce pruritis in patients with AD [49]. The adverse effects (AEs) of dupilumab, however, should be taken into consideration (Table 2). While usually mild, AEs were frequently observed in dupilumab treatment studies. Other systemic treatments including melatonin, abrocitinib, and cyclosporine showed promising results in improving sleep parameters, but further studies will be needed to establish their efficacy. While not always discussed in these studies, the potential AEs of these other treatments also warrant further consideration. For example, abrocitinib and baricitinib have been associated with increased risk for infections and malignancy [50,51]. Clinicians should keep such AEs in mind, particularly the immunosuppressive effects of abroctinib, barictinib, and to a lesser extent dupilumab, when attempting a new treatment plan.
The current gap in research on nonimmunosuppressive treatment options for sleep disturbances also deserves mention. Of note, there was a lack of studies for many medications commonly prescribed by dermatologists to assist with sleep, such as sedating antihistamines, tricyclic antidepressants, mirtazapine, gabapentin, and naltrexone. Further research into the sleep-related effects of these drugs is warranted.
Contrary to systemic treatments, topical treatments for AD were mostly ineffective in influencing sleep. One study using a steroid-tacrolimus combination treatment did find a significant improvement in a 4-point sleep disturbance measure in pediatric patients. However, given a relatively small sample size and lack of blinding, more evidence is needed to verify this effect. Similarly, procedural treatments for AD such as UV-B, PMR, and structured educational programs appeared highly efficacious in improving sleep, but replication is needed before definite conclusions can be drawn. The relative absence of AEs in these interventions, however, makes them promising directions for future research.
For dermatoses other than AD, only a limited number of treatment studies were found that included any kind of sleep measure. For the studies that were found, however, significant benefits to sleep measures were observed. Given the importance of sleep for patients’ quality of life, broader inclusion of sleep measures in treatment studies, whether as part of a standardized clinical assessment tool or as a standalone assessment, merits further consideration.
Several limitations of this review exist. First, there was a lack of homogeneity in the studies found, which precluded the performing of a meta-analysis. The time range of our studies also only encompasses studies up to 2021, meaning newer research may not have been included. Additionally, the nature of funding for some of the treatment studies could have introduced a source of bias, especially for recently introduced medications such as dupilumab (Table 3). Lastly, while the methodology of this review fulfilled most requirements of AMSTAR 2 (A Measurement Tool to Assess systematic Reviews), it did not include a risk of bias assessment [52].
Conclusions
Assessment of sleep changes remains an understudied aspect of dermatological treatment studies. A majority of the studies that did measure changes in sleep were related to AD; however, studies related to pruritus and xerosis, prurigo nodularis, psoriasis vulgaris, and chronic idiopathic pruritus were also found. Dupilumab was most effective at improving sleep measures for AD, but its side effect profile must be taken into consideration. For other dermatoses, given the small number of studies found, further research is needed to establish their efficacy. A broader inclusion of sleep change measures in dermatological treatment studies is warranted.
Abbreviations
- AD
atopic dermatitis
- AE
adverse effect
- AMSTAR
A Measurement Tool to Assess systematic Reviews
- IL
interleukin
- NTIS
Night Time Itch Scale
- PMR
progressive muscle relaxation
- PO
patient-oriented
- POEM
Patient-Oriented Eczema Measure
- PROMIS
Patient Reported Outcome Measurement Information System
- RCT
randomized controlled trial
- SCORAD
Scoring Atopic Dermatitis
- SORT
Strength of Recommendation Taxonomy
- VAS
visual analog scale
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist.
Footnotes
Conflicts of Interest: TES served as an editorial board member-at-large for JMIR Dermatology. They did not participate in the editorial oversight or review process for this paper. PL reports research grants/funding from AbbVie, AOBiome, National Eczema Association; is on the speaker's bureau for AbbVie, Arcutis, Eli Lilly, Galderma, Hyphens Pharma, Incyte, La Roche-Posay/L’Oreal, MyOR Diagnostics, ParentMD, Pfizer, Pierre-Fabre Dermatologie, Regeneron/Sanofi Genzyme, Verrica; reports consulting/advisory boards for Alphyn, AbbVie, Almirall, Amyris, Arcutis, ASLAN, Boston Skin Science, Bristol-Myers Squibb, Burt's Bees, Castle Biosciences, Codex Labs, Concerto Biosci, Dermavant, Eli Lilly, Galderma, Janssen, Johnson & Johnson, Kimberly-Clark, LEO Pharma, Lipidor, L’Oreal, Merck, Micreos, MyOR Diagnostics, Regeneron/Sanofi Genzyme, Skinfix, Theraplex, UCB, Unilever, Verrica Yobee Care; stock options with Codex, Concerto Biosciences and Yobee Care. In addition, PL has a patent pending for a Theraplex product with royalties paid and is a Board member and Scientific Advisory Committee Member of the National Eczema Association.
References
- 1.Lee M, Choh AC, Demerath EW, Knutson KL, Duren DL, Sherwood RJ, Sun SS, Chumlea WMC, Towne B, Siervogel RM, Czerwinski SA. Sleep disturbance in relation to health-related quality of life in adults: the Fels Longitudinal Study. J Nutr Health Aging. 2009;13(6):576–583. doi: 10.1007/s12603-009-0110-1. https://europepmc.org/abstract/MED/19536428 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hansen DA, Layton ME, Riedy SM, Van Dongen HP. Psychomotor vigilance impairment during total sleep deprivation is exacerbated in sleep-onset insomnia. Nat Sci Sleep. 2019;11:401–410. doi: 10.2147/NSS.S224641. https://europepmc.org/abstract/MED/31849552 .224641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Podder I, Mondal H, Kroumpouzos G. Nocturnal pruritus and sleep disturbance associated with dermatologic disorders in adult patients. Int J Womens Dermatol. 2021;7(4):403–410. doi: 10.1016/j.ijwd.2021.02.010. https://linkinghub.elsevier.com/retrieve/pii/S2352-6475(21)00039-3 .S2352-6475(21)00039-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lavery MJ, Stull C, Kinney MO, Yosipovitch G. Nocturnal pruritus: the battle for a peaceful night's sleep. Int J Mol Sci. 2016;17(3):425. doi: 10.3390/ijms17030425. https://www.mdpi.com/resolver?pii=ijms17030425 .ijms17030425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372(6001):n71. doi: 10.1136/bmj.n71. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=33782057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ebell MH, Siwek J, Weiss BD, Woolf SH, Susman J, Ewigman B, Bowman M. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69(3):548–556. https://www.aafp.org/link_out?pmid=14971837 . [PubMed] [Google Scholar]
- 7.Fargnoli MC, Esposito M, Ferrucci S, Girolomoni G, Offidani A, Patrizi A, Peris K, Costanzo A, Malara G, Pellacani G, Romanelli M, Amerio P, Cristaudo A, Flori ML, Motolese A, Betto P, Patruno C, Pigatto P, Sirna R, Stinco G, Zalaudek I, Bianchi L, Boccaletti V, Cannavò SP, Cusano F, Lembo S, Mozzillo R, Gallo R, Potenza C, Rongioletti F, Tiberio R, Grieco T, Micali G, Persechino S, Pettinato M, Pucci S, Savi E, Stingeni L, Romano A, Argenziano G. Real-life experience on effectiveness and safety of dupilumab in adult patients with moderate-to-severe atopic dermatitis. J Dermatolog Treat. 2021;32(5):507–513. doi: 10.1080/09546634.2019.1682503. https://www.tandfonline.com/doi/abs/10.1080/09546634.2019.1682503 . [DOI] [PubMed] [Google Scholar]
- 8.Cork MJ, Eckert L, Simpson EL, Armstrong A, Barbarot S, Puig L, Girolomoni G, de Bruin-Weller M, Wollenberg A, Kataoka Y, Remitz A, Beissert S, Mastey V, Ardeleanu M, Chen Z, Gadkari A, Chao J. Dupilumab improves patient-reported symptoms of atopic dermatitis, symptoms of anxiety and depression, and health-related quality of life in moderate-to-severe atopic dermatitis: analysis of pooled data from the randomized trials SOLO 1 and SOLO 2. J Dermatolog Treat. 2020;31(6):606–614. doi: 10.1080/09546634.2019.1612836. https://eprints.whiterose.ac.uk/150175/ [DOI] [PubMed] [Google Scholar]
- 9.Tsianakas A, Luger TA, Radin A. Dupilumab treatment improves quality of life in adult patients with moderate-to-severe atopic dermatitis: results from a randomized, placebo-controlled clinical trial. Br J Dermatol. 2018;178(2):406–414. doi: 10.1111/bjd.15905. https://academic.oup.com/bjd/article-abstract/178/2/406/6732168?redirectedFrom=fulltext&login=false . [DOI] [PubMed] [Google Scholar]
- 10.Tofte SJ, Papp K, Sadick N, Bohnert K, Simpson E, Thaçi D, Bieber T, Blauvelt A, Sofen H, Gooderham M, Chen Z, Gadkari A, Eckert L, Graham NMH, Pirozzi G, Ardeleanu M. Efficacy and safety of dupilumab for the treatment of moderate-to-severe atopic dermatitis in adults: a pooled analysis of two phase 2 clinical trials. J Am Assoc Nurse Pract. 2018;30(9):529–541. doi: 10.1097/JXX.0000000000000088. https://journals.lww.com/jaanp/fulltext/2018/09000/efficacy_and_safety_of_dupilumab_for_the_treatment.10.aspx .01741002-201809000-00010 [DOI] [PubMed] [Google Scholar]
- 11.Paller A. Using dupilumab to improve circadian function, sleep and pruritus in children with moderate/severe atopic dermatitis. ClinicalTrails. 2021. [2023-10-26]. https://clinicaltrials.gov/ct2/show/NCT05042258 .
- 12.Chang YS, Lin MH, Lee JH, Lee PL, Dai YS, Chu KH, Sun C, Lin YT, Wang LC, Yu HH, Yang YH, Chen CA, Wan KS, Chiang BL. Melatonin supplementation for children with atopic dermatitis and sleep disturbance: a randomized clinical trial. JAMA Pediatr. 2016;170(1):35–42. doi: 10.1001/jamapediatrics.2015.3092. https://jamanetwork.com/journals/jamapediatrics/fullarticle/2470860 .2470860 [DOI] [PubMed] [Google Scholar]
- 13.Harper JI, Ahmed I, Barclay G, Lacour M, Hoeger P, Cork MJ, Finlay AY, Wilson NJ, Graham-Brown RA, Sowden JM, Beard AL, Sumner MJ, Berth-Jones J. Cyclosporin for severe childhood atopic dermatitis: short course versus continuous therapy. Br J Dermatol. 2000;142(1):52–58. doi: 10.1046/j.1365-2133.2000.03241.x. https://academic.oup.com/bjd/article-abstract/142/1/52/6690113?redirectedFrom=fulltext&login=false .bjd3241 [DOI] [PubMed] [Google Scholar]
- 14.Silverberg JI, Thyssen JP, Simpson EL, Yosipovitch G, Ständer S, Valdez H, Rojo R, Biswas P, Myers DE, Feeney C, DiBonaventura M. Impact of oral abrocitinib monotherapy on patient-reported symptoms and quality of life in adolescents and adults with moderate-to-severe atopic dermatitis: a pooled analysis of patient-reported outcomes. Am J Clin Dermatol. 2021;22(4):541–554. doi: 10.1007/s40257-021-00604-9. https://europepmc.org/abstract/MED/33954933 .10.1007/s40257-021-00604-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lio PA, Simpson EL, Han G, Soung J, Ball S, Sun L, Casillas M, DeLozier AM, Ding Y, Eichenfield LF. Improvement in sleep and itch and enhanced quality of life in adult patients with moderate-to-severe atopic dermatitis: results from a phase 3 trial of baricitinib therapy. J Dermatolog Treat. 2022;33(4):2057–2062. doi: 10.1080/09546634.2021.1914308. https://www.tandfonline.com/doi/full/10.1080/09546634.2021.1914308 . [DOI] [PubMed] [Google Scholar]
- 16.Kawana S, Kato Y, Omi T. Efficacy of a 5-HT1a receptor agonist in atopic dermatitis. Clin Exp Dermatol. 2010;35(8):835–840. doi: 10.1111/j.1365-2230.2009.03771.x. https://academic.oup.com/ced/article-abstract/35/8/835/6622476?redirectedFrom=fulltext&login=false .CED3771 [DOI] [PubMed] [Google Scholar]
- 17.Munday J, Bloomfield R, Goldman M, Robey H, Kitowska GJ, Gwiezdziski Z, Wankiewicz A, Marks R, Protas-Drozd F, Mikaszewska M. Chlorpheniramine is no more effective than placebo in relieving the symptoms of childhood atopic dermatitis with a nocturnal itching and scratching component. Dermatology. 2002;205(1):40–45. doi: 10.1159/000063138.drm05040 [DOI] [PubMed] [Google Scholar]
- 18.Ebata T, Izumi H, Aizawa H, Kamide R, Niimura M. Effects of nitrazepam on nocturnal scratching in adults with atopic dermatitis: a double-blind placebo-controlled crossover study. Br J Dermatol. 1998;138(4):631–634. doi: 10.1046/j.1365-2133.1998.02174.x. https://academic.oup.com/bjd/article-abstract/138/4/631/6682927?redirectedFrom=fulltext&login=false . [DOI] [PubMed] [Google Scholar]
- 19.Savin JA, Paterson WD, Adam K, Oswald I. Effects of trimeprazine and trimipramine on nocturnal scratching in patients with atopic eczema. Arch Dermatol. 1979;115(3):313–315. [PubMed] [Google Scholar]
- 20.Parikh-Das A, Ganopolsky I, Nunez C, Moreira L. A clinical trial to evaluate the efficacy of a OTC colloidal oatmeal skin protectant cream in the management of mild to moderate atopic dermatitis in infants and toddlers. J Am Acad Dermatol. 2017;76(6):AB10. doi: 10.1016/j.jaad.2017.04.060. doi: 10.1016/j.jaad.2017.04.060. [DOI] [Google Scholar]
- 21.Ständer S, Metz M, Ramos FMH, Maurer M, Schoepke N, Tsianakas A, Zeidler C, Luger TA. Anti-pruritic effect of sertaconazole 2% cream in atopic dermatitis subjects: a prospective, randomized, double-blind, vehicle-controlled, multi-centre clinical trial of efficacy, safety and local tolerability. Acta Derm Venereol. 2016;96(6):792–796. doi: 10.2340/00015555-2268. doi: 10.2340/00015555-2268. [DOI] [PubMed] [Google Scholar]
- 22.Kubota Y, Yoneda K, Nakai K, Katsuura J, Moriue T, Matsuoka Y, Miyamoto I, Ohya Y. Effect of sequential applications of topical tacrolimus and topical corticosteroids in the treatment of pediatric atopic dermatitis: an open-label pilot study. J Am Acad Dermatol. 2009;60(2):212–217. doi: 10.1016/j.jaad.2008.09.034. https://www.jaad.org/article/S0190-9622(08)01215-2/fulltext .S0190-9622(08)01215-2 [DOI] [PubMed] [Google Scholar]
- 23.Doss N, Kamoun MR, Dubertret L, Cambazard F, Remitz A, Lahfa M, de Prost Y. Efficacy of tacrolimus 0.03% ointment as second-line treatment for children with moderate-to-severe atopic dermatitis: evidence from a randomized, double-blind non-inferiority trial vs. fluticasone 0.005% ointment. Pediatr Allergy Immunol. 2010;21(2 Pt 1):321–329. doi: 10.1111/j.1399-3038.2009.00895.x. https://onlinelibrary.wiley.com/doi/10.1111/j.1399-3038.2009.00895.x .PAI895 [DOI] [PubMed] [Google Scholar]
- 24.Leo HL, Bender BG, Leung SB, Tran ZV, Leung DYM. Effect of pimecrolimus cream 1% on skin condition and sleep disturbance in children with atopic dermatitis. J Allergy Clin Immunol. 2004;114(3):691–693. doi: 10.1016/j.jaci.2004.05.037. https://www.jacionline.org/article/S0091-6749(04)01511-8/fulltext .S0091-6749(04)01511-8 [DOI] [PubMed] [Google Scholar]
- 25.Jaworek A, Szafraniec K, Jaworek M, Matusiak L, Wojas-Pelc A, Szepietowski JC. Itch relief in atopic dermatitis: comparison of narrowband ultraviolet b radiation and cyclosporine treatment. Acta Derm Venereol. 2020;100(17):adv00291. doi: 10.2340/00015555-3652. doi: 10.2340/00015555-3652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pustišek N, Šitum M, Živković MV, Hadžavdić SL, Vurnek M, Niseteo T. The significance of structured parental educational intervention on childhood atopic dermatitis: a randomized controlled trial. J Eur Acad Dermatol Venereol. 2016;30(5):806–812. doi: 10.1111/jdv.13519. https://onlinelibrary.wiley.com/doi/10.1111/jdv.13519 . [DOI] [PubMed] [Google Scholar]
- 27.Bae BG, Oh SH, Park CO, Noh S, Noh JY, Kim KR, Lee KH. Progressive muscle relaxation therapy for atopic dermatitis: objective assessment of efficacy. Acta Derm Venereol. 2012;92(1):57–61. doi: 10.2340/00015555-1189. doi: 10.2340/00015555-1189. [DOI] [PubMed] [Google Scholar]
- 28.Deleuran M, Georgescu V, Jean-Decoster C. An emollient containing aquaphilus dolomiae extract is effective in the management of xerosis and pruritus: an international, real-world study. Dermatol Ther (Heidelb) 2020;10(5):1013–1029. doi: 10.1007/s13555-020-00415-6. https://europepmc.org/abstract/MED/32666271 .10.1007/s13555-020-00415-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rossi A, Nocera T, Lapalud P. Clinical and instrumental efficacy and tolerability of a moisturizing body lotion containing polidocanol and prucidine-4 on reducing pruritus and xerosis. J Am Acad Dermatol. 2016;74(5):AB48. doi: 10.1016/j.jaad.2016.02.191. https://www.jaad.org/article/S0190-9622(16)00321-2/fulltext . [DOI] [Google Scholar]
- 30.Chiricozzi A, Maurelli M, Gori N, Argenziano G, De Simone C, Calabrese G, Girolomoni G, Peris K. Dupilumab improves clinical manifestations, symptoms, and quality of life in adult patients with chronic nodular prurigo. J Am Acad Dermatol. 2020;83(1):39–45. doi: 10.1016/j.jaad.2020.03.049. https://linkinghub.elsevier.com/retrieve/pii/S0190962220304692 .S0190-9622(20)30469-2 [DOI] [PubMed] [Google Scholar]
- 31.Kontochristopoulos G, Kouris A, Chantzaras A, Petridis A, Yfantopoulos J. Improvement of health-related quality of life and adherence to treatment with calcipotriol-betamethasone dipropionate gel in patients with psoriasis vulgaris. An Bras Dermatol. 2016;91(2):160–166. doi: 10.1590/abd1806-4841.20164476. https://europepmc.org/abstract/MED/27192514 .S0365-05962016000200160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zuberbier T, Aberer W, Asero R, Abdul Latiff AH, Baker D, Ballmer-Weber B, Bernstein JA, Bindslev-Jensen C, Brzoza Z, Buense Bedrikow R, Canonica GW, Church MK, Craig T, Danilycheva IV, Dressler C, Ensina LF, Giménez-Arnau A, Godse K, Gonçalo M, Grattan C, Hebert J, Hide M, Kaplan A, Kapp A, Katelaris CH, Kocatürk E, Kulthanan K, Larenas-Linnemann D, Leslie TA, Magerl M, Mathelier-Fusade P, Meshkova RY, Metz M, Nast A, Nettis E, Oude-Elberink H, Rosumeck S, Saini SS, Sánchez-Borges M, Schmid-Grendelmeier P, Staubach P, Sussman G, Toubi E, Vena GA, Vestergaard C, Wedi B, Werner RN, Zhao Z, Maurer M. The EAACI/GA²LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy. 2018;73(7):1393–1414. doi: 10.1111/all.13397. https://onlinelibrary.wiley.com/doi/10.1111/all.13397 . [DOI] [PubMed] [Google Scholar]
- 33.Croxtall JD, Plosker GL. Sertaconazole: a review of its use in the management of superficial mycoses in dermatology and gynaecology. Drugs. 2009;69(3):339–359. doi: 10.2165/00003495-200969030-00009. https://link.springer.com/article/10.2165/00003495-200969030-00009 .9 [DOI] [PubMed] [Google Scholar]
- 34.Schram ME, Spuls PI, Leeflang MMG, Lindeboom R, Bos JD, Schmitt J. EASI, (objective) SCORAD and POEM for atopic eczema: responsiveness and minimal clinically important difference. Allergy. 2012;67(1):99–106. doi: 10.1111/j.1398-9995.2011.02719.x. https://onlinelibrary.wiley.com/doi/10.1111/j.1398-9995.2011.02719.x . [DOI] [PubMed] [Google Scholar]
- 35.Krause L, Shuster S. Mechanism of action of antipruritic drugs. Br Med J (Clin Res Ed) 1983;287(6400):1199–2000. doi: 10.1136/bmj.287.6400.1199. https://europepmc.org/abstract/MED/6138120 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ko KC, Tominaga M, Kamata Y, Umehara Y, Matsuda H, Takahashi N, Kina K, Ogawa M, Ogawa H, Takamori K. Possible antipruritic mechanism of cyclosporine A in atopic dermatitis. Acta Derm Venereol. 2016;96(5):624–629. doi: 10.2340/00015555-2318. doi: 10.2340/00015555-2318. [DOI] [PubMed] [Google Scholar]
- 37.Deeks ED, Duggan S. Abrocitinib: first approval. Drugs. 2021;81(18):2149–2157. doi: 10.1007/s40265-021-01638-3. https://europepmc.org/abstract/MED/34807428 .10.1007/s40265-021-01638-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thomson A, Bonham CA, Zeevi A. Mode of action of tacrolimus (FK506): molecular and cellular mechanisms. Ther Drug Monit. 1995;17(6):584–591. doi: 10.1097/00007691-199512000-00007. https://journals.lww.com/drug-monitoring/abstract/1995/12000/mode_of_action_of_tacrolimus__fk506___molecular.7.aspx . [DOI] [PubMed] [Google Scholar]
- 39.Johnson M. Development of fluticasone propionate and comparison with other inhaled corticosteroids. J Allergy Clin Immunol. 1998;101(4 Pt 2):S434–S439. doi: 10.1016/s0091-6749(98)70155-1. https://www.jacionline.org/article/S0091-6749(98)70155-1/fulltext .A86611 [DOI] [PubMed] [Google Scholar]
- 40.Gupta A, Chow M. Pimecrolimus: a review. J Eur Acad Dermatol Venereol. 2003;17(5):493–503. doi: 10.1046/j.1468-3083.2003.00692.x. https://onlinelibrary.wiley.com/doi/10.1046/j.1468-3083.2003.00692.x .692 [DOI] [PubMed] [Google Scholar]
- 41.Cerio R, Dohil M, Jeanine D, Magina S, Mahé E, Stratigos AJ. Mechanism of action and clinical benefits of colloidal oatmeal for dermatologic practice. J Drugs Dermatol. 2010;9(9):1116–1120. https://pubmed.ncbi.nlm.nih.gov/20865844/ [PubMed] [Google Scholar]
- 42.Šitum M, Bulat V, Majcen K, Džapo A, Ježovita J. Benefits of controlled ultraviolet radiation in the treatment of dermatological diseases. Coll Antropol. 2014;38(4):1249. [PubMed] [Google Scholar]
- 43.McCallie MS, Blum CM, Hood CJ. Progressive muscle relaxation. J Hum Behav Soc Environ. 2006;13(3):51–66. doi: 10.1300/J137v13n03_04. doi: 10.1300/J137v13n03_04. [DOI] [Google Scholar]
- 44.Martin H, Laborel-Préneron E, Fraysse F, Nguyen T, Schmitt AM, Redoulès D, Davrinche C. Aquaphilus dolomiae extract counteracts the effects of cutaneous S. aureus secretome isolated from atopic children on CD4+ T cell activation. Pharm Biol. 2016;54(11):2782–2785. doi: 10.3109/13880209.2016.1173069. https://pubmed.ncbi.nlm.nih.gov/27180655/ [DOI] [PubMed] [Google Scholar]
- 45.Barco D, Giménez-Arnau A. Xerosis: a dysfunction of the epidermal barrier. Article in Spanish. Actas Dermosifiliogr. 2008;99(9):671–682. https://www.elsevier.es/en/linksolver/pdf/pii/13127791 .13127791 [PubMed] [Google Scholar]
- 46.Moniaga CS, Tominaga M, Takamori K. Mechanisms and management of itch in dry skin. Acta Derm Venereol. 2020;100(2):adv00024. doi: 10.2340/00015555-3344. doi: 10.2340/00015555-3344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hawro T, Fluhr JW, Mengeaud V, Redoulès D, Church MK, Maurer M, Metz M. Polidocanol inhibits cowhage - but not histamine-induced itch in humans. Exp Dermatol. 2014;23(12):922–923. doi: 10.1111/exd.12555. https://onlinelibrary.wiley.com/doi/10.1111/exd.12555 . [DOI] [PubMed] [Google Scholar]
- 48.Sulzberger M, Worthmann AC, Holtzmann U, Buck B, Jung KA, Schoelermann AM, Rippke F, Stäb F, Wenck H, Neufang G, Grönniger E. Effective treatment for sensitive skin: 4-t-butylcyclohexanol and licochalcone A. J Eur Acad Dermatol Venereol. 2016;30(Suppl 1):9–17. doi: 10.1111/jdv.13529. https://onlinelibrary.wiley.com/doi/10.1111/jdv.13529 . [DOI] [PubMed] [Google Scholar]
- 49.Mastorino L, Viola R, Panzone M, Avallone G, Gallo G, Ortoncelli M, Cavaliere G, Quaglino P, Ribero S. Dupilumab induces a rapid decrease of pruritus in adolescents: a pilot real-life study. Dermatol Ther. 2021;34(6):e15115. doi: 10.1111/dth.15115. https://europepmc.org/abstract/MED/34455663 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Assadiasl S, Fatahi Y, Mosharmovahed B, Mohebbi B, Nicknam MH. Baricitinib: from rheumatoid arthritis to COVID-19. J Clin Pharmacol. 2021;61(10):1274–1285. doi: 10.1002/jcph.1874. https://europepmc.org/abstract/MED/33870531 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klein B, Treudler R, Simon JC. JAK-inhibitors in dermatology - small molecules, big impact? Overview of the mechanism of action, previous study results and potential adverse effects. J Dtsch Dermatol Ges. 2022;20(1):19–24. doi: 10.1111/ddg.14668. https://onlinelibrary.wiley.com/doi/10.1111/ddg.14668 . [DOI] [PubMed] [Google Scholar]
- 52.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=28935701 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist.