Abstract
This scoping review aimed to identify the breadth of healthcare-based food assistance programmes in the United States and organize them into a typology of programmes to provide implementation guidance to aspiring food assistance programmers in healthcare settings. We searched PubMed, Cochrane, and CINAHL databases for peer-reviewed articles published between 1 January 2010 and 31 December 2021, and mined reference lists. We used content analysis to extract programmatic details from each intervention and to qualitatively analyse intervention components to develop a typology for healthcare institutions in the United States. Eligible articles included descriptions of patient populations served and programmatic details. Articles were not required to include formal evaluations for inclusion in this scoping review. Our search resulted in 8706 abstracts, which yielded forty-three articles from thirty-five interventions. We identified three distinct programme types: direct food provision, referral, and voucher programmes. Programme type was influenced by programme goals, logistical considerations, such as staffing, food storage or refrigeration space, and existence of willing partner CBOs. Food provision programmes (n 13) were frequently permanent and leveraged partnerships with community-based organisations (CBOs) that provide food. Referral programmes (n 8) connected patients to CBOs for federal or local food assistance enrollment. Voucher programmes (n 14) prioritised provision of fruits and vegetables (n 10) and relied on a variety of clinic staff to refer patients to months-long programmes. Healthcare-based implementers can use this typology to design and maintain programmes that align with the needs of their sites and patient populations.
Key words: Food assistance, Food insecurity, Healthcare-based intervention, Population health
Introduction
Food insecurity impacts approximately one in eight Americans.(1) People who experience food insecurity lack reliable, consistent access to a sufficient quantity of food to live a healthful life.(2) Households that experience low income are more likely to experience food insecurity and hunger than those with average incomes.(3) While food insecurity is a social issue that can be addressed in multiple settings, evidence points to the connection between food insecurity and negative health outcomes and increased healthcare costs.(4–9) Healthcare institutions in recent years have begun to screen for food insecurity and provide resources to address the issue, and food insecurity screening is also often part of mandatory social determinants of health screens in certain institutions and U.S. states.(10) Food insecurity alleviation programmes at healthcare institutions have the potential to provide food and food-related support services directly to their patients. Provision of food not only impacts dietary intake and alleviates food insecurity, but also can free up food dollars to be spent on other necessities, such as housing, transportation, utilities, or medications.(11) Food insecurity programmes implemented at healthcare institutions have previously found positive impacts on food security,(12) diet quality,(13–17) cardiometabolic biomarkers,(15) hospital admission and readmission rates,(18) and healthcare costs.(19) They can also connect patients to resources that can alleviate food insecurity(20,21) and improve management of chronic conditions and health outcomes.(22) Healthcare-based food insecurity programmes are likely to be more successful if they are consistent and sustainable.(23)
There is a growing literature base regarding healthcare-based food insecurity programmes.(24,25) Nonprofit and advocacy organisations, such as Feeding America, the Food Research & Action Center, and Children's HealthWatch, have established guidelines on creating and executing these programmes.(26) However, there is a lack of specific, detailed, and actionable implementation guidance for healthcare institutions of differing sizes and types to design, operate, and maintain an array of food insecurity alleviation programmes. Healthcare providers have also expressed that education and assistance with logistics would facilitate implementation of food insecurity alleviation programmes.(27)
As a result of United States Department of Agriculture (USDA) funding, there is a small, but growing, evidence base of evaluations of produce prescription programmes,(28) a type of food insecurity intervention located at healthcare institutions in which a provider writes a ‘prescription’ for fruits and vegetables.(29) However, produce prescription programmes may not be the right intervention for every healthcare institution and its patient population.
To support decision-makers and implementers, we aimed to create a typology of intervention components that can be used to create and execute impactful food insecurity programmes at healthcare institutions. We conducted a scoping review of food insecurity interventions based at healthcare institutions and used content analysis(30) to create a typology of programmes. This typology may assist programme implementers consider programmatic intended impact, institutional logistical constraints, and planning for sustainability in an effort to effectively achieve their goals.
Methods
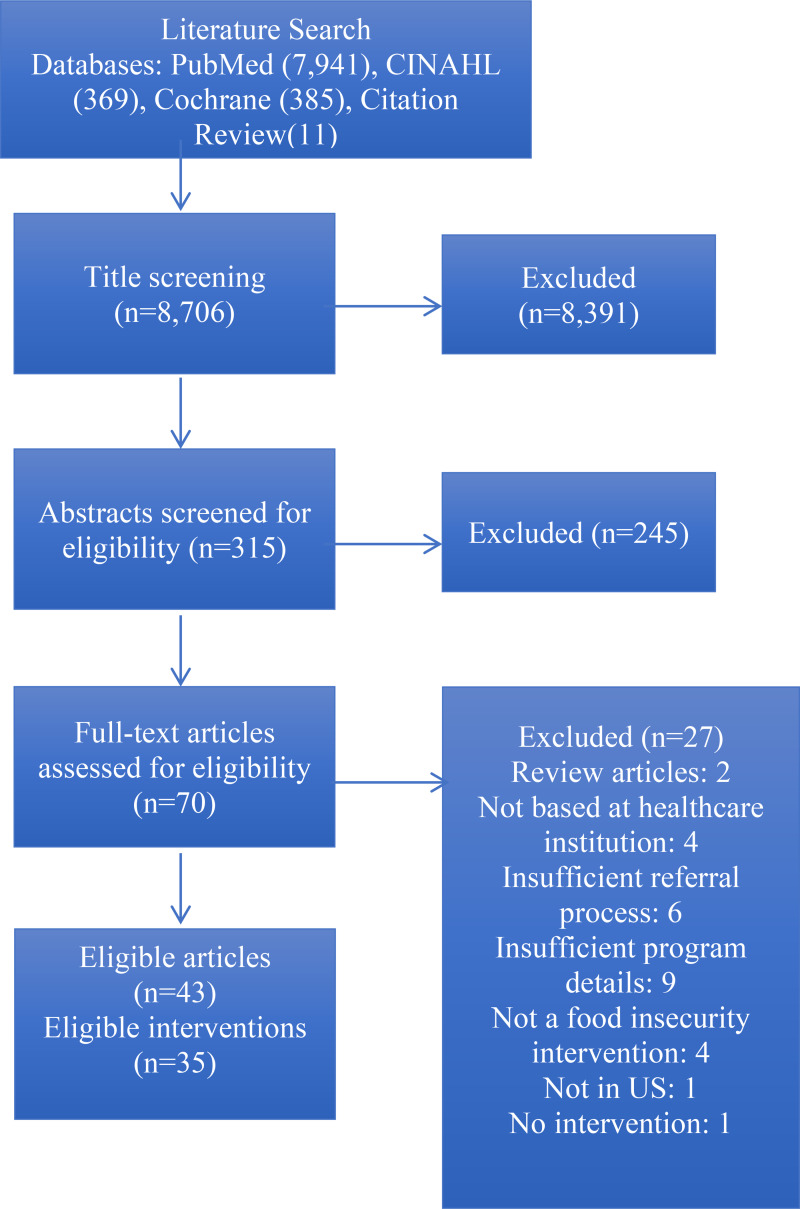
We searched PubMed, CINAHL, and Cochrane databases for papers published between 1 January2010 and 31 December2021, with the following terms: food assistance, initiative, program, health, medical, medical center, academic, community health, federally qualified, and food. We also mined reference lists of relevant research articles. We included peer-reviewed papers of interventions based at healthcare institutions in the United States that provided food assistance for their patient population. Papers were eligible for inclusion if they reported implementation and intervention details and patient population descriptions. We included papers that did not evaluate outcomes as long as details regarding programme design and implementation were included. We excluded interventions that screened for food insecurity without providing assistance obtaining food, and those that used a passive referral process, such as handing out a list of available resources, as these interventions have been found to have minimal success connecting patients to resources.(31) Our search strategy is summarised in Fig. 1.
Fig. 1.
This PRISMA flow diagram depicts our systematic search process that we followed in order to identify articles for inclusion in this work.
After identifying the manuscripts eligible for inclusion in the review, we created a data charting form with intervention component categories previously identified in the literature. Intervention components included the location of the program, type of healthcare institution in which the programme was located, an overview of the program, duration of patients’ participation in the program, and patient eligibility for the programme. Two reviewers, R.R. and E.M., independently read through each complete manuscript and completed the chart by extracting relevant programmatic information and performing a content analysis.(30) Reviewers met regularly throughout the data extraction process to compare completed charts, discuss discrepancies, and create consensus. Any discrepancies were moderated by J.G.
We then analysed programme components and created the typology. We iteratively compared and contrasted different programme components to identify patterns and groupings that often were often observed together or seemed to influence other programme elements. We also compared any overlapping components or patterns found in multiple categories to further explore these classification definitions, identifying distinguishing characteristics. We continued this process through five iterations until each category had a distinct set of characteristics, resulting in a draft typology. Finally, we validated the draft typology against the research articles to ensure accuracy, with each article fitting distinctly into each category.
Results
Among 8706 identified articles, forty-three met inclusion criteria. Several articles reported on the same intervention; ultimately, thirty-five distinct interventions were represented in the forty-three articles identified for inclusion. They are summarised in Table 1.
Table 1.
Description of Healthcare-based food assistance programmes
| First author, year | Location in U.S. | Type of healthcare institution | Programme overview | Programme participation duration | Patient eligibility |
|---|---|---|---|---|---|
| Adams, 2021(32) & Dunn, 2021(33) | Revere, MA | Community Healthcare system | Free produce market | Ongoing | No eligibility requirements |
| Aiyer, 2019(34) | North Pasadena, TX | Federally qualified health center | Fruit and vegetable prescription program | 6 months | 18+, Food insecure based on two-question clinic screener, residing in one of three target zip codes |
| Beck, 2014(35) | Cincinnati, OH | Urban academic pediatric primary care clinic adjacent to Cincinnati Children's Medical Center | Screening, Provision of Infant Formula, Referral | Ongoing | Families with children <12 months with food insecurity (answered yes to at least one of two screening questions), or failure to thrive. Clinical provider given latitude to deem eligible. |
| Berkowitz, 2021(36) & Xie, 2021(37) | North Carolina | Nine primary care clinics (primarily Federally qualified health centers) | SNAP subsidy for fruits and vegetables | 6 months | 18+, current SNAP beneficiaries and identified by staff at primary care clinic as ‘likely to benefit from programme b/c of health status’ |
| Blitstein, 2020(38) | ‘Large Midwest City’ | Federally qualified health centers | Screening, referral, nutrition education, enrollment assistance | Ongoing | Diagnosis of diabetes [All participants received intervention regardless of food insecurity status] |
| Bryce, 2017(39) | Detroit, MI | Federally qualified health center | Fruit and vegetable prescription program | 13 weeks | FQHC patients with diabetes mellitus, hypertension, obesity, hyperlipidaemia, pregnant or with children, and have limited access to fruits and vegetables |
| Cavanagh, 2017(40) | Upstate NY | Community clinic | Fruit and vegetable prescription program | 13 weeks, can receive additional 13 weeks if all coupons used | Low income persons with at risk or with obesity, hypertension, or diabetes |
| Cohen, 2017(41) & 2019(42) | Ypsilanti, MI | Ypsilanti Health Center primary care clinic | Waiting room intervention encouraging Double Up Food Bucks use | One-time | 18+, currently SNAP enrolled, self-identified as a primary food shopper for household |
| Cook, 2021(43) & Newman, 2021(23) | Atlanta, Athens, Augusta, GA | Primary care clinics | Produce Prescription programme with nutrition education | 6 months | SNAP-eligible and/or screen positive for food insecurity on USDA 2-item screener and diagnosed for one or more condition: overweight/obesity, diabetes mellitus, pre-diabetes, hypertension, or hyperlipidaemia |
| Esquivel, 2020(44) | Rural community near Honolulu, HI | Federally qualified health center pediatric clinic | Fruit and vegetable prescription program, on-site farmer's market (pre-existing) | 3 months | Children aged 2–17 with ‘poor nutrition’ based on growth assessment or BMI% < 5 % or >85 %. |
| Ferrer, 2019(15) | San Antonio, TX | Primary care practice | Nutrition education and free box of food | 6 months | A1c > 9 %, screen positive for food insecurity on Hunger Vital Sign |
| Gany, 2020(12) | NYC, NY | Outpatient Cancer Clinics | Co-located medically-tailored food pantries at clinics | Throughout treatment/Ongoing | Screen positive for food insecurity on USDA household food insecurity survey |
| Ghouse, 2020(45) | Michigan | Primary care clinic | Nutrition education and free bag of food | 6 weeks | Pre-diabetic (A1c 5⋅7–6⋅4 %), screen positive for food insecurity using USDA 5-item, able to converse in English |
| Greenthal, 2019(46) | Northeastern US | Academic urban safety-net hospital | Medically-tailored food pantry | Ongoing | Patients who screen positive for food insecurity in hospital's outpatient clinics |
| Hager, 2020(47) | Minneapolis, MN | Safety-net Medical Center hospital, outpatient clinics, and community primary care clinics | EMR Hunger Vital Sign screening and auto-faxed referral to food bank partner, food bank calls patient to provide assistance with obtaining food assistance in the community | One-time | Screen positive for food insecurity on Hunger Vital Sign |
| Izumi, 2020(48) | Multnomah County, OR | Federally qualified health center safety-net clinic | Subsidised Community-Supported Agriculture | 23 weeks | English and Spanish-speaking who receive services at the FQHC. |
| Jones, 2020(49) | Navajo Nation, NM | 19 HC facilities in Navajo Nation (range from small clinics to hospitals) | Fruit and vegetable prescription program | 6 months | Families with pregnant woman or children </=6 years. Some sites used Indian Health Services Food Insecurity Screening Questionnaire to specifically enroll food insecure families. |
| Knowles, 2018(50) | Philadelphia, PA | Academic medical center pediatric primary care outpatient clinics | Screening, Referral, Benefits eligibility screening and application assistance | One-time | Pediatric patients of center clinics who screen positive for food insecurity |
| Kulie, 2021(51) | Washington, DC | Urban academic Emergency Department | Screening, Referral | One-time | 18+, non-life threatening emergency severity index score, insured by DC Medicaid and approved for ED discharge, English-speaking |
| Milliron, 2017(52) | North Carolina | Urban outpatient clinic (free or reduced price services) | Community garden | Ongoing | None |
| Mirsky, 2021(53) | Revere, MA | Community-based academic medical center | On-site plant-based food pantry | 12 weeks* original plan that was altered due to COVID-19 in March 2020 | Food insecure with diagnosis of obesity, hypertension, or diabetes mellitus. Pilot pts were English-speaking only. |
| Morales, 2016(54) | Chelsea, MA | Community health center | Screening, enrollment assistance and pantry info | One-time | Pregnant women 18+ receiving care at the health center |
| Paolantonio, 2020(55) | NYC, NY | Four cancer clinics | Food voucher program | 6 months | 18+, able to answer survey questions in English or Spanish, living independently, score low or very low for food insecurity on the USDA Household Food Security Screener, be within 2 weeks of starting radiation or 1 month of starting chemo. Those receiving or applying for SNAP were ineligible. |
| Sastre, 2021(18) | Greenville, NC | Academic medical center inpatient | Hospital-based Medical Food Pantry | One-time | Screen positive for food insecurity on Hunger Vital Sign |
| Saxe-Custack, 2018(56) & 2019(57) | Flint, MI | University-affiliated residency training pediatric clinic | Fruit and vegetable prescription program | Ongoing | All pediatric patients of practice [all receive Rx regardless of need] |
| Schlosser, 2019a(58); Schlosser, 2019b(59); & Joshi, 2019(60) | Cuyahoga County, OH | Three safety-net clinics | Produce Prescription Program | 3 months | Patient of clinic positive for food insecurity on 2-item screen and diagnosis of hypertension |
| Slagel, 2021(61) | Athens, GA | ‘Clinics’ | Produce Prescription programme with nutrition education | 6 months | 18+, SNAP-eligible or otherwise underserved, with a dx of at least one condition: overweight/obesity, diabetes mellitus, pre-diabetes, hypertension, or hyperlipidaemia |
| Smith, 2017(62) | San Diego, CA | Student-run free clinic associated with medical school | Food Insecurity Screening and Referral with federal programme sign-up assistance, food provided only for patients with DM | One-time; *Patients with diabetes received food bag monthly for unknown amount of time | 18+ and patient of student-run free clinics |
| Stenmark, 2018(63) | Colorado | Two pediatric clinics | Screening, Referral, Assistance signing up for fed asst programmes | One-time | Patient of clinic, screen positive for food insecurity on Hunger Vital Sign |
| Stotz, 2019(64) | Georgia | Safety-net clinic | Nutrition education, 12-week receipt of one bag of locally-grown produce | 12 weeks | Adults eligible for SNAP-Ed living in households below 185 % federal poverty level (as evidenced by enrollment in safety-net clinic) and diagnosis of diabetes mellitus, hypertension, &/or hyperlipidaemia |
| Veldheer, 2021(65) | Reading, PA | Primary care clinic in community-based hospital | Fruit and vegetable prescription program | 7 months | A1c >= 7 %, adults >18 years, BMI >= 25 |
| Walker, 2021(66) | ‘Large metropolitan region in Ohio’ | Two community-based family medicine practices within an academic medical center | Screening, Referral, Vouchers | 90 days | 18+, patients of primary care clinics, screen positive for food insecurity, and meet clinical criteria, including diagnosis of diabetes mellitus, obesity, hypertension, HgbA1c > 9 %, or pregnant w/ gestational diabetes |
| Weinstein, 2014(67) | Bronx, NY | Primary care or diabetes clinics at urban public hospital | Nutrition education and food voucher | One-time | >18 years and established patient on clinics, with diagnosis of type 2 diabetes mellitus, BMI > 25, A1c > 7 % |
| Wetherill, 2018(68) | Oklahoma | Two academic medical center-affiliated free clinics | Nutrition education and free box of food | 6 months | Any patient of affiliated clinics |
| Wynn, 2021(63) | Cook County, IL | Large urban academic medical center – three inpatient units for pilot | Screening for SDOH, paper referral, bag of non-perishable food | One-time | Inpatient on participating floors, screen positive for food insecurity on Hunger Vital Sign |
Results of content analysis
In our content analysis, we identified eight core characteristics of healthcare-based food insecurity programmes: screening for food insecurity, defining eligibility criteria, direct provision of food, provision of vouchers, provision of referrals, offering patient education, healthcare team involved in staffing, and programme length. These characteristics were consistent with the literature, used to assess the forty-three articles in our review, and informed the creation of the typology.
Screening for food insecurity
Eighteen(12,15,18,19,23,34,35,38,43,45,47,50,53,55,58,59,60,62,63,66,69) of the thirty-five programmes discussed screening for food insecurity. Of these, six programmes(23,38,43,45,55,62,70) used the USDA Household Food Security Survey, with number of items ranging from two to eighteen. Thirteen programmes(15,18,34,35–37,47,49,50,53,58–60,63,66,69) screened for food insecurity using the Hunger Vital Sign.,(71–73) two programmes(41,42,51) used unique screeners, and one used a ‘standardised assessment form’.(54) programmes that did not screen for food insecurity were either open to anyone regardless of food insecurity status,(32,33,52) open to patients of clinics that serve primarily low-income populations, or used medical records to identify patients with ‘poor nutrition’.(44) One programme used the clinical expertise of an on-site nutritionist to identify eligible patients.(40)
Defining eligibility criteria
Sixteen(15,23,36–40,43,44,45,53,55,58,59,60,61,64–67) of the thirty-five programmes included a cardiometabolic diagnosis (e.g. overweight, obesity, pre-diabetes, diabetes mellitus, hypertension, or hyperlipidaemia) as part of their eligibility criteria. One programme(54) was created explicitly for pregnant women, four(35,44,50,57) for children, and one(49) for families with either pregnant women or children under age seven. Fourteen(12,15,18,34,35,45–47,50,53,55,58–60,63,69) programmes required patients to screen positive for food insecurity in order to be enrolled. One programme(23,43) required patients to be eligible for the Supplemental Nutrition Assistance Programme (SNAP) or to screen positive for food insecurity.
Direct provision of food
Fourteen programmes(15,18,32,33,35,45,46,48,52,53,55,62–64,68) provided food directly to patients. Of these, eight(12,15,18,45,46,48,53,68) provided both produce and non-perishable foods, three(32,33,52,64) provided only produce, one [40] provided only non-perishable foods, and one(35) provided baby formula. Refrigerated storage capacity was noted as a barrier to providing produce directly to patients.(12,53) programmes circumvented this issue by partnering with community-based organisations (CBOs) to provide same-day delivery and distribution of produce,(12,32,33,48,64) while others obtained dedicated refrigeration space.(46,53) One programme(52) utilised an on-site community garden. Two programmes (12,46) that provided food directly to patients offered a choice of food, while ten programmes(15,18,32,33,45,48,52,53,63,64,68) provided participants with a pre-packed bag. Three programmes (12,18,46) provided medically-tailored foods, that is, foods that met the nutritional requirements of the patient based on their medical status, as designated by their physician or registered dietitian. These three medically-tailored programmes operated as on-site food pantries.
Provision of vouchers
Fourteen programmes (23,34,36,37,39,40–44,49,55–62,65–67) provided vouchers or other cash incentives that allowed participants to increase their purchasing power for food. By virtue of providing cash assistance to purchase foods, all fourteen programmes provided the participant with some form of choice in the foods they received. None of these programmes provided medically-tailored foods.
The amount of money provided to participants in voucher programmes ranged from a minimum of $6 for the entire programme in 2011 dollars(67) to a maximum of $230 per month for six months in 2021 dollars.(55) Four programmes (23,43,49,61) provided $1 (between 2015 and 2018) per household member per day.
Ten programmes(23,39,40–44,56–61,65,67) allowed the vouchers to be utilised only for fresh fruits and vegetables, and three programmes(34,36,37,49) allowed voucher use for both fresh and non-perishable healthful (e.g. fruits, vegetables, or whole grains, etc.) foods. One programme allowed participants to use the voucher for any food purchases, though they were reminded to choose healthful foods.(55) Ten programmes(23,39,41–44,49,56,57–61,65,67) partnered with farmer's markets to accept the vouchers, two(39,44) of which were markets located on-site at the healthcare center where the programme was implemented. One programme(34) provided vouchers for a food pantry, and one programme(40) provided a voucher to be used at a mobile produce truck that parked at the health center where the intervention was implemented once weekly. Three programmes(36,37,49,55) allowed participants to utilize the programme at participating partner supermarkets, and one(49) at convenience stores. Three(39,49,55) used debit cards and one programme(36,37) loaded additional funds onto EBT cards. Others used printed vouchers or tokens.
Nine programmes(23,34,39,43,44,49,56–58,60,61,65) were fruit and vegetable prescription (FVRx) programmes, in which clinicians wrote ‘prescriptions’ that patients could take to farmer's markets to purchase a certain number of fruits and vegetables.
Provision of referrals
Thirteen programmes(12,18,35,38,45,50,51,54,62,63,66,69,71) provided referrals to local or national food programmes, such as local food pantries, SNAP, or the Special Supplemental Nutrition programme for Women, Infants, and Children, commonly referred to as WIC. Of these, twelve(18,35,38,45,50,51,54,62,63,66,69,71) of these programmes referred to local CBOs, such as food pantries, and eight(12,35,38,50,54,62,69,71) assisted with enrollment in SNAP and WIC. Seven programmes(12,35,38,50,54,62,69,71) provided both. Six programmes(18,38,51,54,62,66) utilised on-site benefits specialists to assist with referrals, while five(35,50,63,69,71) used electronic referrals to alternative CBOs (e.g. food bank,(66) NowPow,(63) Benefits Data Trust,(50) medical–legal partnership,(35) or Hunger Free Colorado(69)), who then followed up with the patient.
Offering patient education
Nineteen programmes (15,18,23,34,35,38,39,43,45,46,48,49,52,53,58–61,64,65,67,68) provided education to patients, which included nationally-available courses such as Cooking Matters(45,74) and ‘Eat Right When Money's Tight’,(38) as well as education produced by the intervention healthcare institution. Of the 19, sixteen programmes (15,18,23,34,35,38,43,45,49,52,53,58–61,64,65,67,68) provided nutrition education, while eight(23,39,43,45,46,48,49,61,64) provided cooking demonstrations or education. Five programmes(23,43,45,49,61,64) provided both. Seven of the nineteen programmes(15,23,35,38,43,58,59,60,64,68) provided education on cooking on a budget or food resource management. Six programmes(34,35,38,58,59,64,68) used passive nutrition education, such as with printed materials or online videos, while nine(15,23,39,43,45,46,52,53,61,65) provided in-person education or cooking demonstrations. Two programmes(48,49) provided both printed materials and in-person cooking demonstrations. Four programmes(39,48,52,53) provided education informally, such as during other healthcare visits,(52) in passing and without billing,(53) or during a farmer's market.(39,48)
Health care team members involved in staffing
Staffing of interventions was varied. Screening and/or referral into interventions was completed by clinic staff in eight programmes,(12,34,36,37,48,49,65,68,69) by a physician in three programmes,(44,47,67) by a programme manager in one program,(53) by a nutritionist in one,(40) and by research study staff in four programmes.(41,42,50,51,55) Seven other programmes listed ‘providers’ as tasked with screening and/or referring patients into the program, but did not specify which type of provider.(23,38,39,43,46,52,54,58,60)
Programming was staffed by an array of volunteers and professionals. While some programmes had only one type of staff member running programming, other programmes used a variety of staff to execute different functions of the program, in addition to their primary responsibilities. Community volunteers were utilised by three programmes,(32,33,34,52) while staff volunteers were used by one.(63) CBOs delivered programming in seven interventions.(15,35,50,51,62,66,69) A range of medical staff was used in programme delivery, such as for education: four programmes used providers,(34,35,49,57,67) one used Registered Nurses,(18) one used Nurse Practitioners,(61) five used Registered Dietitian Nutritionists,(18,40,61,65,68) and three used Community Health Workers.(15,48,65) One programme utilised a nutrition educator and licensed chef to deliver education.(45) Research staff delivered programming in one intervention.(62)
Programme length
Eight programmes(12,32,33,35,46,52,53,56,57,62) were permanent. These programmes included on-site food pantries(46,53,55) and gardens,(52) two monthly on-site food distributions,(32,33,62) on-site distribution of baby formula,(35) and a produce prescription programme.(56,57) Eleven programmes(18,38,41,42,47,50,51,54,62,63,67,69) included programming that each patient received only once, even if they attended the healthcare institution repeatedly. All of these programmes, except one,(67) included food insecurity screening and referral to federal or local food assistance programmes. Two of these programmes also provided participants with one bag of non-perishable foods from a hospital-based food pantry,(18,63) and one included ongoing monthly on-site food distributions to participants with diabetes.(62) Eighteen(15,23,34–37,39,40,43,44,48,49,55,58–61,64–66,68) programmes were time-limited, ranging from three to nine months. Fourteen(23,34–37,39,40,43,44,49,55,58–61,65,66) of these programmes utilised cash assistance to increase participants’ purchasing power of food, while four(15,48,64,68) provided food directly to patients.
Results of typology development
We identified three types of food assistance programmes located at healthcare institutions: those that provide food directly to patients, those that refer patients to resources that provide food, and those that provide vouchers or cash assistance in order to purchase food. These are summarised in Table 2.
Table 2.
Typology of healthcare-based food assistance programmes
| Provides food directly | Refers to resources that provide food assistance | Provides vouchers to purchase food | |
|---|---|---|---|
| Recipients | Patients who are both food insecure and have a diagnosis of chronic disease (e.g. diabetes mellitus, cardiovascular disease, or cancer, etc.). Sometimes participants with food insecurity and no additional eligibility requirements. | All patients who screen positive for food insecurity | Patients who are both food insecure and have a diagnosis of cardiometabolic disease (e.g. diabetes mellitus or cardiovascular disease, etc.) or health status associated with nutritional risk (e.g. pregnancy, obesity, or underweight, etc.) |
| Length of Intervention | Ongoing, allows for repeat use by participants. | One-time intervention to connect people to resources | Time-bound, providing resources for an average of 3–6 months |
| Type of Food | Both produce and non-perishable foods | No type of food prioritised (referral to programming, regardless of food provided) | Priority to provide produce (fruits and vegetables) |
| Choice of Food | Limited choice, if any. Typically offer standard bags of food that do not provide patient with choices | No tangible food provided | Moderate choices offered. Allow participants to choose foods within certain parameters (e.g. fruits and vegetables) |
| Education | Typically provides nutrition education, sometimes with cooking demonstrations included | No education provided | Often provides nutrition education, sometimes includes cooking demonstrations |
| Partnerships | Partnerships with CBOs to obtain food to be distributed. | No formal partnerships required. Some programmes set up direct lines to local CBOs (e.g. food pantries, food banks, Feeding America franchise). | Partnerships with food purveyors (e.g. farmers, grocery stores) to accept vouchers. |
| Reach | Varied. Can be limited in size or available to a large proportion of patients (in the case of on-site gardens, pantries) | Significant. Available to a large proportion of patients. Successful reach may be dependent on capacity of referred CBOs. | Limited in size |
| Staffing | Referral and enrollment process facilitated by varying clinic staff members. Two programmes were entirely open access. | No permanent staff focused on this programming. Often filled though research staff roles | Often require a physician to refer patient into programme |
Programmes that provide food directly
programmes that provide food directly to patients provide both produce and non-perishable foods and tend not to offer patients a choice of food, instead, providing a standardised pre-packed bag or box. These programmes frequently include nutrition education, and sometimes cooking demonstrations, and tend to be permanent and on-site. Examples include food pantries, community gardens, and on-site food delivery and distribution in partnership with a local food bank. Often, institutions and programmes partner with CBOs for obtaining the food to be provided.
Patients can be referred to these programmes by their healthcare providers (e.g. physicians or dietitians) and utilize the programme at any time at any time in their care, as they are static programmes. These programmes vary in size: some provide assistance to a limited number of patients, while others provide food to any patient who would benefit. Often these programmes are only developed for and provided to patients with certain diagnoses, most often nutrition-related cardiometabolic diagnoses, such as diabetes, obesity, and cardiovascular disease. However, it is not uncommon that these programmes also provide foods for all patients with food insecurity, regardless of cardiometabolic diagnosis.
Programmes that refer patients to resources that provide food assistance
Programmes that refer to resources that provide food assistance are typically available for all patients that screen positive for food insecurity, either on the Hunger Vital Sign(71,72,73) or another screening tool.(75) These programmes can be time-limited or permanent at the healthcare institution, but each participant's interaction with the programme happens only once, when they are referred to resources.
Referrals can be to local CBOs such as food pantries, regional resources such as a Feeding America site, or enrollment assistance with federal food assistance programmes such as SNAP and WIC. Enrollment assistance happens both on-site or via referral to a CBO to assist.
Referral programmes are more limited in scope than other food assistance programmes. Because the programme consists of a referral to an outside entity, the healthcare institution has no control over the type of food provided; patients instead receive food assistance from the CBO or federal programme. Nutrition education is rarely provided by the healthcare institution in tandem with the referral programme. Reach for these programmes is significant; many patients are able to be referred. The referral programmes we identified used research staff to complete the patient identification and referral process. Use of temporary research staff, rather than permanent healthcare staff, highlights the uncertainty of programme funding and sustainability.
Programmes that provide vouchers to purchase food
Programmes that provide vouchers to purchase food are time-bound, providing patients with vouchers for an average of three to six months. They are typically available for patients with both food insecurity and a health status associated with nutritional risk (e.g. pregnancy obesity, underweight) or cardiometabolic disease. Produce prescription programmes, which are a type of voucher program, are frequently funded by the USDA National Institute of Food and Agriculture Gus Schumacher Nutrition Incentive programme (GusNIP), which requires that they reach low-income populations with diet-related health conditions.(29)
Voucher programmes prioritize the procurement of fruits and vegetables over non-perishable foods and provide a choice of foods within this limitation (i.e. patients can choose which fruits or vegetables they would like to purchase with their voucher). Nutrition education and cooking demonstrations are frequently paired with these programmes. Partnerships with food purveyors, such as farmers, farmer's markets, supermarkets, and convenience stores, are necessary for providing a venue in which the vouchers are accepted.(29,76) These programmes are often limited in reach, helping fewer patients than other types of programmes, likely due to the cost of providing financial assistance. These programmes often require a physician to refer the patient to the program; they are rarely open to all patients; only those with a prescription can participate.
Discussion
We used results of our scoping review to create a typology that identified three distinct types of healthcare-based food insecurity interventions: those that provide food directly to patients, those that refer patients to resources that provide food assistance, and those that provide vouchers to purchase food. Our findings from the typology indicate that logistical considerations and constraints impact feasibility of healthcare-based food insecurity interventions. Important logistics to consider include staffing, refrigeration and storage space, existence of willing CBOs and partners, and programme goals.
Staffing of food insecurity alleviation programmes varied by the type of programme: programmes that provide vouchers or financial assistance to patients often require a physician to refer qualifying patients to the programme, while programmes that provide food directly to patients utilize a variety of clinic staff members, such as registered dietitians and community health workers. Referral programmes rarely used permanent staff, and often filled these positions with members of the research team.
Implementation science literature indicates that staffing of healthcare-based programming heavily influences implementation and sustainability.(77) Analysing staff capacity prior to programme development and implementation and aligning programme choice with existing capacity should help to ensure that adequate human resources are in place. Physicians have previously reported that limited training and time during patient visits are barriers to implementing voucher programmes.(28) If adequate training and time is unavailable, implementers may wish to consider a programme that does not require physician involvement, such as a referral programme. Importantly, having a dedicated, paid, staff member, rather than a volunteer programme champion, to run any type of food insecurity alleviation programme improves provider experiences and overall programming.(28)
Refrigeration and storage space for food provision also heavily impacts the type of programming a healthcare institution can implement. For example, many of the programmes we included in the review lacked refrigeration space for storing fresh produce; some programmes chose to ameliorate this issue by providing only non-perishable foods, while others partnered with CBOs to deliver fresh produce to be distributed to patients on the same day. Securing space agreements and identifying community partners early in programme development not only help to increase likelihood of programme success but also dictate what type of programme may best fit the needs of the healthcare institution and patient population.(53)
Community partnerships were influential in almost all the programmes we identified. Programmes that provided food directly to patients often partnered with local food banks to source the food; referral programmes partnered with CBOs to assist with registering patients for SNAP and WIC, or to local food pantries for additional food resources; and programmes that provided vouchers to patients often partnered with food purveyors such as farmers markets or supermarkets. Identifying and working with community partners early in development and implementation of food assistance programmes will dictate what programming can be provided effectively.(29,53,69).
In addition to logistical constraints, healthcare institutions should consider their goals for the program, including how many and what type of patients they aim to reach and the length of time of the intervention they foresee. As evidenced in the typology, programmes that wish to serve a greater number of food insecure patients may wish to implement a referral program, which allows for higher throughput than a voucher or food provision programme.(69,71) Alternatively, institutions that wish to provide programming for patients with the dual burden of food insecurity and cardiometabolic disease may choose to implement a more rigorous, but less wide-reaching initiative, such as a fruit and vegetable prescription programme.(29) It is, however, important to consider the length of the intervention; provision of food for a months-long period is a worthy goal but may lack durability of any health or food security outcomes observed.(23)
A limitation of this typology is that we do not include information on programme sustainability. Healthcare institutions that aim to create food insecurity alleviation programmes should consider not only their implementation, but their plan for sustainability. Research indicates that sustainability of healthcare-based programmes is heavily influenced by organisational support, staff turnover, and funding.(23,77) Being explicit about programme components and clearly defining scope of work and processes can increase sustainability and achievement of strategic outcomes.(78) Referral programmes may be best able to reach the largest number of patients, but follow-through to ensure that patients are connected to and receive resources is a challenge.(24)
A second limitation to this typology is that we did not assess programme outcomes, but rather the implementation and programming. Importantly, a 2019 review of healthcare-based food insecurity interventions found that the majority of studies were low quality and most analysed only process outcomes.(24) Evaluation of programme impacts and outcomes, such as improvements in health or decreased healthcare utilisation, can lead to increased funding, and thus sustainability, of these programmes.(28) Formal evaluations are often not done, however, because many of these programmes are small in scope and created by clinical staff members to help patients, rather than researchers aiming to evaluate a programme.(79) Additionally, it is difficult to assess the body of literature as a whole because of the heterogeneity of programme components(24,79) and goals: some to improve food security and some to improve overall health and healthcare spending. Future research should aim to identify which programme components and outcomes are most important for improving food insecurity among patient populations.
Lastly, this scoping review and typology included only interventions from the peer-reviewed literature; there are certainly other healthcare-based food insecurity programmes in the United States that have not published peer-reviewed literature of their findings.(22,25,80) There is likely significant institutional knowledge at other sites, and the field would benefit from tapping into both the positive and negative experiences of existing programmes. Communities of practice, focused forums, and other forms of information sharing may be the best way to identify learnings and innovations, and ultimately share effective practices.
Supporting information
Rudel et al. supplementary material
Acknowledgments
The authors would like to thank Eilisha Manandhar, MPH, for her assistance with the scoping review.
This work was supported by the Boston University School of Public Health Maternal and Child Health Center of Excellence Doctoral Fellowship in Maternal Child Health Epidemiology (R.R.). The funder had no role in the design, analysis, or writing of this article.
All authors contributed to this manuscript. R.R. assisted with conceptualisation the study design, conducted data collection and analysis, and authored the manuscript. E.B. assisted with conceptualisation of the study design and provided substantial feedback and edits with the manuscript. K.S. assisted with conceptualisation of the study design and provided substantial feedback and edits with the manuscript. M.-L.D. assisted with conceptualisation of the study design, provided guidance regarding data analyses and creation of the typology, and provided substantial feedback and edits to the manuscript. J.G. assisted with conceptualisation of the study design, provided guidance regarding data analyses and creation of the typology, and provided substantial feedback and edits to the manuscript.
This work was supported by the Boston University School of Public Health Maternal and Child Health Center of Excellence Doctoral Fellowship in Maternal Child Health Epidemiology (R.R.). The funder had no role in the design, analysis or writing of this article.
The authors have no conflicts of interest to declare.
This research did not involve human participants.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/jns.2023.111
References
- 1.Feeding America (2021) The Impact of the Coronavirus on Food Insecurity in 2020 & 2021. Accessed November 2021. https://www.feedingamerica.org/sites/default/files/2021-03/National%20Projections%20Brief_3.9.2021_0.pdf.
- 2.United States Department of Agriculture (2021) Definitions of Food Security. Accessed March 2022. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/definitions-of-food-security/.
- 3.Coleman-Jensen A, Rabbitt MP, Gregory CA & Singh A. Household Food Security in the United States in 2021, ERR-309. U.S. Department of Agriculture, Economic Research Service; 2022. [Google Scholar]
- 4.Seligman HK, Davis TC, Schillinger D & Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Healthcare Poor Underserved. 2010;21(4):1227–1233, 10.1353/hpu.2010.0921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Allen NL, Becerra BJ & Becerra MB. Associations between food insecurity and the severity of psychological distress among African-Americans. Ethnic Health. 2018;23(5):511–520, 10.1080/13557858.2017.1280139. [DOI] [PubMed] [Google Scholar]
- 6.Becerra MB, Allen NL & Becerra BJ. Food insecurity and low self-efficacy are associated with increased healthcare utilization among adults with type II diabetes mellitus. J Diabetes Complicat. 2016;30(8):1488–1493, 10.1016/j.jdiacomp.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 7.Garcia SP. Incremental health care costs associated with food insecurity and chronic conditions among older adults. Prev Chronic Dis. 2018;15:180058, 10.5888/pcd15.180058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gundersen C & Ziliak JP. Food insecurity and health outcomes. Health Affairs. 2015;34(11):1830–1839, 10.1377/hlthaff.2015.0645. [DOI] [PubMed] [Google Scholar]
- 9.Palakshappa D, Garg A, Peltz A, Wong CA, Cholera R & Berkowitz SA. Food insecurity was associated with greater family health care expenditures in the US, 2016–17. Health Affairs. 2023;42(1):44–52, 10.1377/hlthaff.2022.00414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sandhu S, Sharma A, Cholera R & Bettger JP. Integrated health and social care in the United States: a decade of policy progress. Int J Integr Care. 2021;21(4):9, 10.5334/ijic.5687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berkowitz SA, Shahid NN, Terranova J, et al. ‘I was able to eat what I am supposed to eat’– patient reflections on a medically-tailored meal intervention: a qualitative analysis. BMC Endocr Disord. 2020;20(1):10, 10.1186/s12902-020-0491-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gany FM, Pan S, Ramirez J & Paolantonio L. Development of a medically tailored hospital-based food pantry system. J Healthcare Poor Underserved. 2020;31(2):595–602, 10.1353/hpu.2020.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu FX, Alexander GC, Crawford SY, Pickard AS, Hedeker D & Walton SM. The impact of medicare part D on out-of-pocket costs for prescription drugs, medication utilization, health resource utilization, and preference-based health utility. Health Serv Res. 2011;46(4):1104–1123, 10.1111/j.1475-6773.2011.01273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berkowitz SA, O'Neill J, Sayer E, et al. Health center–based community-supported agriculture: an RCT. Am J Prev Med. 2019;57(6, Supplement 1):S55–S64, 10.1016/j.amepre.2019.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferrer RL, Neira LM, De Leon Garcia GL, Cuellar K & Rodriguez J. Primary care and food bank collaboration to address food insecurity: a pilot randomized trial. Nutr Metab Insights. 2019;12:1178638819866434, 10.1177/1178638819866434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freedman DA, Choi SK, Hurley T, Anadu E & Hébert JR. A farmers’ market at a federally qualified health center improves fruit and vegetable intake among low-income diabetics. Prev Med. 2013;56(5):288–292, 10.1016/j.ypmed.2013.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leone LA, Tripicchio GL, Haynes-Maslow L, et al. Cluster randomized controlled trial of a mobile market intervention to increase fruit and vegetable intake among adults in lower-income communities in North Carolina. Int J Behav Nutr Phys Activ. 2018;15(1):2, 10.1186/s12966-017-0637-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sastre L, Wynn D, Roupe M & Jacobs M. Link between redemption of a medical food pantry voucher and reduced hospital readmissions. Prev Med Rep. 2021;23:101400, 10.1016/j.pmedr.2021.101400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berkowitz SA, Terranova J, Randall L, Cranston K, Waters DB & Hsu J. Association between receipt of a medically tailored meal program and health care use. JAMA Intern Med. 2019;179(6):786–793, 10.1001/jamainternmed.2019.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ratcliffe C, McKernan SM & Zhang S. How much does the supplemental nutrition assistance program reduce food insecurity? Am J Agric Econ. 2011;93(4):1082–1098, 10.1093/ajae/aar026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carlson S & Keith-Jennings B. SNAP Is Linked with Improved Nutritional Outcomes and Lower Healthcare Costs. Washington, DC: Center on Budget and Policy Priorities; 2018. Published January 17, 2018. Accessed January 21, 2022. https://www.cbpp.org/research/food-assistance/snap-is-linked-with-improved-nutritional-outcomes-and-lower-health-care [Google Scholar]
- 22.Feinberg AT, Hess A, Passaretti M, Coolbaugh S & Lee TH. Prescribing Food as A Specialty Drug. NEJM Catalyst; 2018. [Google Scholar]
- 23.Newman T & Lee JS. Strategies and challenges: qualitative lessons learned from Georgia produce prescription programs. Health Promotion Practice. 2021;23(4), 10.1177/15248399211028558. [DOI] [PubMed] [Google Scholar]
- 24.De Marchis EH, Torres JM, Benesch T, et al. Interventions addressing food insecurity in health care settings: a systematic review. Ann Fam Med. 2019;17(5):436–447, 10.1370/afm.2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DAISA Enterprises WW (2021) Produce Prescription Programs US Field Scan Report: 2010–2020. Accessed December 2022. https://www.daisaenterprises.com/uploads/4/4/0/5/44054359/produce_prescription_programs_us_field_scan_report__june_2021_final.pdf.
- 26.Children's HealthWatch, Feeding America, and the Food Research & Action Center (2018) Addressing Food Insecurity in Healthcare Settings: Key Actions & Tools for Success. Accessed March 2022. https://frac.org/wp-content/uploads/addressing-food-insecurity-in-health-care-settings-key-actions-and-tools.pdf.
- 27.Coward KB, Cafer A, Rosenthal M, Allen D & Paltanwale Q. An exploration of key barriers to healthcare providers’ use of food prescription (FRx) interventions in the rural South. Public Health Nutr. 2021;24(5):1095–1103, 10.1017/S1368980020005376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stotz SA, Budd Nugent N, Ridberg R, et al. Produce prescription projects: Challenges, solutions, and emerging best practices – perspectives from Healthcare providers. Prev Med Rep. 2022;29:101951, 10.1016/j.pmedr.2022.101951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.United States Department of Agriculture (2020). Gus Schumacher Nutrition Incentive Program. Washington, DC: National Institute of Food and Agriculture; 2020. Accessed December 2022. http://www.nifa.usda.gov/grants/programs/hunger-food-security-programs/gus-schumacher-nutrition-incentive-program. [Google Scholar]
- 30.Hsieh HF & Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288, 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 31.Marpadga S, Fernandez A, Leung J, Tang A, Seligman H & Murphy EJ. Challenges and successes with food resource referrals for food-insecure patients with diabetes. Perm J. 2019;23:18–097, 10.7812/TPP/18-097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adams E. Providing food assistance during the COVID-19 pandemic: a case study of a free produce market at a health care center. J Healthcare Poor Underserv. 2021;32(4):1–10, 10.1353/hpu.2021.0198. [DOI] [PubMed] [Google Scholar]
- 33.Dunn CG, Vercammen KA, Bleich SN, et al. Participant perceptions of a free fresh produce market at a health center. J Nutr Educ Behav. 2021;53(7):573–582, 10.1016/j.jneb.2021.03.012. [DOI] [PubMed] [Google Scholar]
- 34.Aiyer JN, Raber M, Bello RS, et al. A pilot food prescription program promotes produce intake and decreases food insecurity. Transl Behav Med. 2019;9(5):922–930, 10.1093/tbm/ibz112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beck AF, Henize AW, Kahn RS, Reiber KL, Young JJ & Klein MD. Forging a pediatric primary care–community partnership to support food-insecure families. Pediatrics. 2014;134(2):e564–e571, 10.1542/peds.2013-3845. [DOI] [PubMed] [Google Scholar]
- 36.Berkowitz SA, Curran N, Hoeffler S, Henderson R, Price A & Ng SW. Association of a fruit and vegetable subsidy program with food purchases by individuals with low income in the US. JAMA Netw Open. 2021;4(8):e2120377, 10.1001/jamanetworkopen.2021.20377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xie J, Price A, Curran N & Østbye T. The impact of a produce prescription programme on healthy food purchasing and diabetes-related health outcomes. Public Health Nutr. 2021;24(12):3945–3955, 10.1017/S1368980021001828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blitstein JL, Lazar D, Gregory K, et al. Foods for health: an integrated social medical approach to food insecurity among patients with diabetes. Am J Health Promot. 2021;35(3):369–376, 10.1177/0890117120964144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bryce R, Guajardo C, Ilarraza D, et al. Participation in a farmers’ market fruit and vegetable prescription program at a federally qualified health center improves hemoglobin A1C in low income uncontrolled diabetics. Prev Med Rep. 2017;7:176–179, 10.1016/j.pmedr.2017.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cavanagh M, Jurkowski J, Bozlak C, Hastings J & Klein A. Veggie Rx: an outcome evaluation of a healthy food incentive programme. Public Health Nutr. 2017;20(14):2636–2641, 10.1017/S1368980016002081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cohen AJ, Richardson CR, Heisler M, et al. Increasing Use of a healthy food incentive: a waiting room intervention among low-income patients. Am J Prev Med. 2017;52(2):154–162, 10.1016/j.amepre.2016.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cohen AJ, Oatmen KE, Heisler M, et al. Facilitators and barriers to supplemental nutrition assistance program incentive use: findings from a clinic intervention for low-income patients. Am J Prev Med. 2019;56(4):571–579, 10.1016/j.amepre.2018.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cook M, Ward R, Newman T, et al. Food security and clinical outcomes of the 2017 Georgia fruit and vegetable prescription program. J Nutr Educ Behav. 2021;53(9):770–778, 10.1016/j.jneb.2021.06.010. [DOI] [PubMed] [Google Scholar]
- 44.Esquivel MK, Higa A, Hitchens M, Shelton C & Okihiro M. Keiki produce prescription (KPRx) program feasibility study to reduce food insecurity and obesity risk. Hawaii J Health Soc Welf. 2020;79(5 Suppl 1):44–49. [PMC free article] [PubMed] [Google Scholar]
- 45.Ghouse A, Gunther W & Sebastian M. Evaluation of a COVID-influenced curriculum to address food insecurity in a detroit family medicine residency clinic. Spartan Med Res J. 2020;5(2):17649, 10.51894/001c.17649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Greenthal E, Jia J, Poblacion A & James T. Patient experiences and provider perspectives on a hospital-based food pantry: a mixed methods evaluation study. Public Health Nutr. 2019;22(17):3261–3269, 10.1017/S1368980019002040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hager K, De Kesel Lofthus A, Balan B & Cutts D. Electronic medical record-based referrals to community nutritional assistance for food-insecure patients. Annals of Family Medicine. 2020;18(3):278–278, doi: 10.1370/afm.2530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Izumi BT, Martin A, Garvin T, et al. CSA partnerships for health: outcome evaluation results from a subsidized community-supported agriculture program to connect safety-net clinic patients with farms to improve dietary behaviors, food security, and overall health. Trans Behav Med. 2020;10(6):1277–1286, 10.1093/tbm/ibaa041. [DOI] [PubMed] [Google Scholar]
- 49.Jones LJ, VanWassenhove-Paetzold J, Thomas K, et al. Impact of a fruit and vegetable prescription program on health outcomes and behaviors in young navajo children. Curr Dev Nutr. 2020;4(8):nzaa109, 10.1093/cdn/nzaa109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Knowles M, Khan S, Palakshappa D, et al. Successes, challenges, and considerations for integrating referral into food insecurity screening in pediatric settings. J Healthcare Poor Underserv. 2018;29(1):181–191, 10.1353/hpu.2018.0012. [DOI] [PubMed] [Google Scholar]
- 51.Kulie P, Steinmetz E, Johnson S & McCarthy ML. A health-related social needs referral program for medicaid beneficiaries treated in an emergency department. Am J Emerg Med. 2021;47:119–124, 10.1016/j.ajem.2021.03.069. [DOI] [PubMed] [Google Scholar]
- 52.Milliron BJ, Vitolins MZ, Gamble E, Jones R, Chenault MC & Tooze JA. Process evaluation of a community garden at an urban outpatient clinic. J Community Health. 2017;42(4):639–648, 10.1007/s10900-016-0299-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mirsky JB, Zack RM, Berkowitz SA & Fiechtner L. Massachusetts general hospital revere food pantry: addressing hunger and health at an academic medical center community clinic. Healthcare. 2021;9(4):100589, 10.1016/j.hjdsi.2021.100589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morales ME, Epstein MH, Marable DE, Oo SA & Berkowitz SA. Food insecurity and cardiovascular health in pregnant women: results from the food for families program, chelsea, Massachusetts, 2013–2015. Prev Chronic Dis. 2016;13:E152, 10.5888/pcd13.160212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Paolantonio L, Kim SY, Ramirez J, et al. Food purchasing behavior of food insecure cancer patients receiving supplemental food vouchers. Support Care Cancer. 2020;28(8):3739–3746, 10.1007/s00520-019-05183-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Saxe-Custack A, Lofton HC, Hanna-Attisha M, et al. Caregiver perceptions of a fruit and vegetable prescription programme for low-income paediatric patients. Public Health Nutr. 2018;21(13):2497–2506, 10.1017/S1368980018000964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saxe-Custack A, LaChance J, Hanna-Attisha M & Ceja T. Fruit and vegetable prescriptions for pediatric patients living in flint, Michigan: a cross-sectional study of food security and dietary patterns at baseline. Nutrients. 2019;11(6):1423, 10.3390/nu11061423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schlosser AV, Joshi K, Smith S, Thornton A, Bolen SD & Trapl ES. “The coupons and stuff just made it possible”: economic constraints and patient experiences of a produce prescription program. Transl Behav Med. 2019;9(5):875–883, 10.1093/tbm/ibz086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schlosser AV, Smith S, Joshi K, Thornton A, Trapl ES & Bolen S. “You guys really care about me…”: a qualitative exploration of a produce prescription program in safety Net clinics. J Gen Intern Med. 2019;34(11):2567–2574, 10.1007/s11606-019-05326-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Joshi K, Smith S, Bolen SD, Osborne A, Benko M & Trapl ES. Implementing a produce prescription program for hypertensive patients in safety net clinics. Health Prom Prac. 2019;20(1):94–104, 10.1177/1524839917754090. [DOI] [PubMed] [Google Scholar]
- 61.Slagel N, Newman T, Sanville L, et al. A pilot fruit and vegetable prescription (FVRx) program improves local fruit and vegetable consumption, nutrition knowledge, and food purchasing practices. Health Prom Pract. 2021;24(1), 10.1177/15248399211018169. [DOI] [PubMed] [Google Scholar]
- 62.Smith S, Malinak D, Chang J, et al. Implementation of a food insecurity screening and referral program in student-run free clinics in San diego, California. Prev Med Rep. 2017;5:134–139, 10.1016/j.pmedr.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wynn N, Staffileno BA, Grenier JM & Phillips J. Implementing a food is medicine program to address food insecurity in an academic medical center. J Nurs Care Qual. 2021;36(3):262–268, 10.1097/NCQ.0000000000000496. [DOI] [PubMed] [Google Scholar]
- 64.Stotz SA, Thompson JJ, Bhargava V, Scarrow A, Capitano K & Lee JS. A supplemental produce and eLearning nutrition education program for Georgians who use safety-net clinics for their health care. J Nutr Educ Behav. 2019;51(9):1099–1106, 10.1016/j.jneb.2019.06.018. [DOI] [PubMed] [Google Scholar]
- 65.Veldheer S, Scartozzi C, Bordner CR, et al. Impact of a prescription produce program on diabetes and cardiovascular risk outcomes. J Nutr Educ Behav. 2021;53(12):1008–1017, 10.1016/j.jneb.2021.07.005. [DOI] [PubMed] [Google Scholar]
- 66.Walker D, DePuccio M, Hefner J, et al. Utilization patterns of a clinic-based food referral program: findings from the Mid-Ohio farmacy. Health Serv Res. 2021;56:81–81, 10.1111/1475-6773.13836. [DOI] [PubMed] [Google Scholar]
- 67.Weinstein E, Galindo RJ, Fried M, Rucker L & Davis NJ. Impact of a focused nutrition educational intervention coupled with improved access to fresh produce on purchasing behavior and consumption of fruits and vegetables in overweight patients with diabetes mellitus. Diabetes Educ. 2014;40(1):100–106, 10.1177/0145721713508823. [DOI] [PubMed] [Google Scholar]
- 68.Wetherill MS, Chancellor McIntosh H, Beachy C & Shadid O. Design and implementation of a clinic-based food pharmacy for food insecure, uninsured patients to support chronic disease self-management. J Nutr Educ Behav. 2018;50(9):947–949, 10.1016/j.jneb.2018.05.014. [DOI] [PubMed] [Google Scholar]
- 69.Stenmark SH, Steiner JF, Marpadga S, DeBor M, Underhill K & Seligman H. Lessons learned from implementation of the food insecurity screening and referral program at Kaiser Permanente Colorado. Perm J. 2018;22:18–093, 10.7812/TPP/18-093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gany F. Development of a Medically Tailored Hospital-based Food Pantry System. Published 2020. Accessed October 14, 2021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8073793/ [DOI] [PMC free article] [PubMed]
- 71.Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26–e32, 10.1542/peds.2009-3146. [DOI] [PubMed] [Google Scholar]
- 72.Gundersen C, Engelhard EE, Crumbaugh AS & Seligman HK. Brief assessment of food insecurity accurately identifies high-risk US adults. Public Health Nutr. 2017;20(8):1367–1371, 10.1017/s1368980017000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cutts D & Cook J. Screening for food insecurity: short-term alleviation and long-term prevention. Am J Public Health. 2017;107(11):1699–1700, 10.2105/AJPH.2017.304082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cooking Matters. Accessed January 17, 2023. https://cookingmatters.org/
- 75.USDA ERS - Survey Tools. Accessed January 31, 2022. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/survey-tools/#household
- 76.Caceres G. Farmers Markets: Local Partners in the Nutrition Incentive Field. Washington, DC: National Institute of Food and Agriculture; 2021. Accessed January 13, 2023. http://www.nifa.usda.gov/about-nifa/blogs/farmers-markets-local-partners-nutrition-incentive-field [Google Scholar]
- 77.Shelton RC, Cooper BR & Stirman SW. The sustainability of evidence-based interventions and practices in public health and health care. Ann Rev Public Health. 2018;39(1):55–76, 10.1146/annurev-publhealth-040617-014731. [DOI] [PubMed] [Google Scholar]
- 78.Fiori K, Patel M, Sanderson D, et al. From policy statement to practice: Integrating social needs screening and referral assistance with community health workers in an urban academic health center. J Prim Care Community Health. 2019;10:2150132719899207, 10.1177/2150132719899207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Veldheer S, Scartozzi C, Knehans A, et al. A systematic scoping review of How healthcare organizations are facilitating access to fruits and vegetables in their patient populations. J Nutr. 2020;150(11):2859–2873, 10.1093/jn/nxaa209. [DOI] [PubMed] [Google Scholar]
- 80.Feinberg AT, Slotkin JR, Hess A & Erskine AR. How Geisinger Treats Diabetes by Giving Away Free, Healthy Food. Harvard Business Review; 2017. Brighton, Massachusetts. Published online October 25, 2017. Accessed February 24, 2020. https://hbr.org/2017/10/how-geisinger-treats-diabetes-by-giving-away-free-healthy-food [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Rudel et al. supplementary material