Abstract
BACKGROUND:
Unplanned extubations (UEs) in injured patients are potentially fatal, but etiology and patient characteristics are not well described. We have been prospectively characterizing the etiology of UEs after we identified a high rate of UEs and implemented an educational program to address it. This period of monitoring included the years of the COVID-19 pandemic that produced high rates of workforce turnover in many hospitals, dramatically affecting nursing and respiratory therapy services. We hypothesized that frequency of UEs would depend on the etiology and that the workforce changes produced by the COVID-19 pandemic would increase UEs.
METHODS:
This study was a prospective tracking and retrospective review of trauma registry and performance improvement data from 2012–2021.
RESULTS:
UE subjects were younger, were more frequently male, were diagnosed more frequently with pneumonia (38% vs 27%), and had longer hospital (19 d vs 15 d) and ICU length of stay (LOS) (12 d vs 10 d) (all P < .05). Most UEs were due to patient factors (self-extubation) that decreased after education, while UEs from other etiologies (mechanical, provider) were stable. Subjects with UEs from mechanical or provider etiologies had longer ICU LOS, higher mortality, and were less likely to be discharged home. The COVID-19 pandemic was associated with more total patient admissions and more days of ventilator use, but the rate of UEs was not changed.
CONCLUSIONS:
UEs were decreased by education with ongoing tracking, and UEs from patient factors were associated with better outcome than other etiologies. Workforce changes produced by the COVID-19 pandemic did not change the rate of UEs.
Keywords: trauma, respiratory failure, airway, unplanned extubation
Introduction
The establishment of a patent airway is the first priority in the care of injured patients. Because trauma patients suffer brain injuries that can inhibit respiratory drive, have tracheobronchial and pulmonary injuries, or can have an altered sensorium from intoxication at the time of injury, a compromised airway during the initial evaluation of injured patients is a common problem. Endotracheal intubation is performed at multiple steps in the continuum of care of injured patients including in the prehospital setting, at referring institutions, and by providers at definitive care trauma centers and can be a lifesaving intervention. Since trauma patients frequently require transport between facilities and to multiple locations in the hospital during their evaluation (eg, radiology, operating room), establishing and maintaining a secure airway is essential for safe patient management.
Unanticipated loss of an airway prior to the patient being ready for purposeful removal of the endotracheal tube (ETT) can occur for a variety of reasons and is defined as an unplanned extubation (UE). The frequency of UEs varies from 0.6–11.0% of intubated patients depending on the population studied.1–3 The impact of a UE on patient outcome is controversial. Some studies demonstrate a higher mortality in subjects who experience a UE compared to those who do not.4 Other studies have shown that mortality is independent of the UE event itself and is primarily associated with the need for re-intubation.5–7 The frequency of re-intubation ranges from 30–80%, and prior work suggests that the need for re-intubation is primarily responsible for the increased complications and costs of care associated with UEs.5–8 Some authors have recommended that rate of UEs should be tracked as a hospital quality metric.9 Risk factors for UEs have been identified, and the consequences of UEs have been studied. However, most studies have been performed in critically ill medical subjects or in mixed medical/surgical ICUs.1–7 For injured patients who have mechanical impediments to reinsertion of an ETT such as airway injury, airway swelling, and face/neck trauma, loss of an ETT can be catastrophic. Compared to intubated medical ICU patients, trauma patients, therefore, have risk factors that can make UEs more hazardous. The problem of UEs in the trauma patient population, however, has not been extensively studied, and the etiologies for UEs have not been well characterized.
In 2012, our Trauma Performance Improvement (PI) and Patient Safety Program identified an unexpectedly high frequency of UEs in our injured patients. The Trauma PI Program began to prospectively track these events and analyze the reason for the UEs. We implemented an educational program for physicians, nurses, and respiratory therapists (RTs) and have tracked UEs as a routine quality measure. We hypothesized that outcome associated with a UE would vary based on the reason or etiology and that the multidisciplinary education program would reduce the frequency of UEs. This period included the beginning of the COVID-19 pandemic, which dramatically affected management of respiratory failure.10,11 At many United States hospitals, the COVID-19 pandemic also produced widespread changes in institutional capacity, patient population, hospital practice, and health care system function that included substantial workforce turnover.12,13 At our institution, we also witnessed an apparent rise in UE cases being analyzed. A secondary hypothesis was that the hospital and workforce changes associated with the COVID-19 pandemic were associated with an increase in UEs.
QUICK LOOK.
Current knowledge
Unplanned extubations (UEs) can have significant consequences particularly in trauma patients who have impediments to re-intubation. The etiology of UEs is infrequently reported or characterized.
What this paper contributes to our knowledge
Over a 10-y period, UEs in injured patients in a level 1 trauma center decreased associated with education and continuous monitoring, primarily due to decreased patient self-extubations. UEs due to mechanical or provider issues were unchanged. Workforce issues from the COVID-19 pandemic did not alter the frequency of UEs.
Methods
All patients meeting National Trauma Data Standard International Classification of Diseases (ICD)-9 or ICD-10 codes for injury from January 1, 2012–December 31, 2021, who were admitted to University of Louisville Hospital were prospectively entered into the trauma registry of our American College of Surgeons–verified level 1 trauma center. Our trauma center serves the population of metropolitan Louisville, Central/South Central/Western Kentucky, and Southern Indiana, comprising a population of approximately 2–2.5 million people in both urban and rural communities. Approximately 30% of patients are transferred from another facility. To determine incidence of UEs, intubated subjects with ICU days ≥ 1 and ventilator days ≥ 1 were selected from the trauma registry. Intubated patients who died in the emergency department or had no ICU days were excluded. Subjects were counted as having a day of mechanical ventilation if they spent any part of the ICU day on mechanical ventilation or were intubated and on partial support such as CPAP. Use of flow-by oxygen without additional ventilator support was restricted to subjects with a tracheostomy in place, was not used to transition to extubation in trauma subjects with an ETT, and was not counted as a day of mechanical ventilation. Patients who were intubated for operations and extubated in the operating room/post-anesthesia care unit (PACU) were not included.
Subjects were primarily admitted to one of two 10-bed trauma/surgery ICUs with overflow preferentially directed to the 10-bed neuro-trauma ICU. Burn subjects were admitted to a dedicated burn ICU that increased from 5 to 16 beds in the last 3.5 y of the study. All trauma patients were cared for by surgery residents and critical care fellows specifically assigned to the ICU under the supervision of a trauma/critical care attending physician. The patients-to-nurse ratio was a maximum of 2:1 in all ICUs. During the study period, care for intubated patients included a ventilator bundle involving a daily sedation vacation where appropriate, oral care, ETT maintenance, and head-of-bed positioning. Pain management for ventilated subjects was initially provided by continuous infusion (fentanyl, morphine) and transitioned to intermittent and/or oral medications during recovery. Sedation was titrated to the Richmond Agitation-Sedation Scale14 and utilized continuous infusions initially (propofol, midazolam) that were transitioned to intermittent dosing as the subjects progressed toward weaning. The determination of suitability for weaning and extubation from mechanical ventilation was at the discretion of the physicians in conjunction with RTs and nursing staff with weaning mechanics (breathing frequency, tidal volume, minute ventilation, negative inspiratory force) and rapid shallow breathing index measured to assist decision-making. RTs could adjust ventilator settings independently, but an RT-driven wean-and-extubate protocol was not utilized during the study period. Early tracheostomy was performed in subjects with head injuries judged to have stable intracranial pressure or when clinically indicated, and there were no instances of UEs involving tracheostomies.
All subjects admitted to the ICU were prospectively followed by trauma PI nurses who identified cases of UEs. We defined UE as the unexpected removal of a previously placed nasal or oral ETT prior to intentional extubation. Technical issues such as dysfunctional ETT cuffs, tubes inadvertently dislodged by medical personnel during turning or transport, as well as intentional removal by subjects themselves prior to an order to extubate were recorded as UEs. Supraglottic airways inserted by prehospital personnel were routinely replaced in the emergency department with an oral ETT, and these exchanges were not considered UEs. ETTs changed intentionally, such as exchange of a small ETT for a larger ETT for pulmonary hygiene, were not considered UEs. Inadvertent removal of a tracheostomy after the subject had been liberated from mechanical ventilation and was breathing spontaneously was not considered a UE. Subjects who experienced UE were identified, and the circumstances of the event were evaluated. Subject characteristics, details of the event, location of the UE (ICU, emergency department, radiology), nursing details (ie, nursing experience, agency or part-time nurses, restraint use), and need for and timing of re-intubation were collected in addition to subject demographics and injury-related data. All cases of UEs were reviewed by the trauma medical director and classified as being due to patient-related factors (self-extubation), mechanical factors (eg, damaged tube or cuff), or provider factors (eg, dislodged while turning or during transport).
In late 2013, we implemented an education program to decrease our incidence of UEs. The UE events, characteristics, and etiologies were tabulated, presented, and discussed at our multidisciplinary trauma PI meetings that included physician and nursing leadership. The data were reviewed and presented at hospital-wide multidisciplinary critical care meetings that included representatives of all critical care services in addition to nursing ICU leadership and respiratory therapy leadership. Targeted educational presentations, including case presentations with review of data, review of best practices, and assessment of potential problem areas with trauma patients were provided to ICU nurses at unit-specific staff meetings and nursing education programs. Cases of UEs were reviewed with providers to assess the circumstances leading to the UE and individual education provided as needed. For continual reinforcement, the number of UEs were tabulated and presented as a routine performance indicator to physician and nursing leadership on a quarterly basis.
Data are presented as the mean ± SD of the mean. Categorical variables were analyzed by chi-square test, and numerical variables were analyzed by analysis of variance (ANOVA) and Scheffé's post hoc test. For comparisons involving multiple groups, the P values represent omnibus tests across all categories. Binary logistic regression was performed for the outcome of UEs with the described clinical variables entered into the model. We visualized the change in number of days between UEs over time based on an assumed geometric distribution using a rare-event G chart. The upper control limit was based on alpha = 0.005. All analyses were performed using SPSS (IBM, Armonk, New York). A value of P < .05 was considered statistically significant. This study was reviewed and approved by the University of Louisville Institutional Review Board.
Results
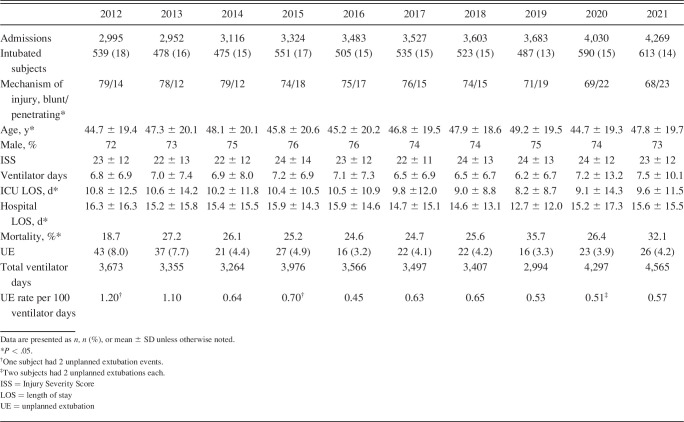
Over the study period, the number of patients admitted to our trauma center increased; but the proportion of subjects who were intubated and admitted to the ICU (n = 5296, 15.1%), comprising the population at risk for UE, remained stable (Table 1). Age and percentage of penetrating injuries in intubated subjects increased over time, but the magnitude of injury measured by Injury Severity Score (ISS) was unchanged. ICU and hospital length of stay (LOS) decreased over time while days of mechanical ventilation were stable (Table 1). Our rate of UEs was initially high (Table 1) but significantly decreased following implementation of our education program in 2013, reaching a low of 3.2% of intubated subjects or 0.45 UE per 100 ventilator days in 2016 (Table 1). Despite the increase in intubated subjects and number of UEs during the COVID-19 pandemic (2020, 2021), the rate of UEs expressed as percent of intubated subjects or UEs per 100 ventilator days remained low (Table 1).
Table 1.
Demographics for Intubated Subjects
Characteristics of subjects with or without UE are presented in Table 2. Subjects who experienced UE were younger and were more commonly male (Table 2). There was no difference in emergency department blood pressure between intubated subjects who did or did not have a UE. ISS and emergency department pulse were statistically significantly different, but the differences were small and clinically insignificant (Table 2). Subjects who had a UE had a longer mean hospital LOS, longer ICU LOS, more days of mechanical ventilation, and were more frequently diagnosed with pneumonia. Unexpectedly, subjects who had a UE were more commonly discharged home or to a rehabilitation facility and had a lower mortality rate compared to intubated subjects who did not experience UE (Table 2). UEs were not clustered in a particular ICU, and no trends in nurse, nurse experience, or restraint use were identified. Analysis of clinical variables using logistic regression demonstrated that younger age, male sex, higher emergency department pulse, lower ISS, and year of admission were significantly associated with risk for UE (Table 3), while mechanism of injury, presence of hypotension, emergency department systolic blood pressure, and emergency department Glasgow coma score were not. The time period was categorized into pre-education (pre, 2012–2013), post-education (post, 2014–2019), and COVID-19 periods (2020–2021) (Table 4). There were 63 trauma patients who tested positive for SARS-CoV-2 in 2020 and 78 who tested positive in 2021, with 41 of these subjects intubated and included in the study (41/1,203, 3.6%). Age and ISS were similar over these periods, but the number of subjects with penetrating injuries increased (Table 4). The percentage of intubated subjects with UE decreased in the post-education period and remained low during the COVID-19 period (Table 4). If the logistic regression was repeated with time categorized as the periods described above, ISS, emergency department pulse, age, and male sex remained significant, and the later time periods were associated with decreased UEs (odds ratio 0.700 [95% CI 0.570–0.859], P < .001).
Table 2.
Characteristics of Subjects With Unplanned Extubation

Table 3.
Logistic Regression Factors Associated With Unplanned Extubation

Table 4.
Unplanned Extubations by Period of Time

A UE statistical process control chart was constructed plotting the days between UE events for each individual UE event consecutively across the respective time periods (Fig. 1A), with the rules for identifying special cause variation listed in Table 5. The statistical process control chart supported the association between implementation of the educational program and decreased UE events. In the pre period, there were more special cause variation cases below the mean demonstrating fewer days between UE events. In the later time periods, there were more total cases above the mean, more special cause variation cases above the mean, and more cases above the upper control limit (filled symbols). These findings are consistent with increased days between UE events in the post-intervention and COVID time periods compared to the pre-intervention period (Fig. 1B) (P < .001 by ANOVA).
Fig. 1.
Days between unplanned extubation (UE) events. A: Days between UE events per UE cases plotted consecutively. Solid line represents the mean for the entire group, and dashed line represents the 3-σ upper control limit. Arrows designate the division between the pre, post, and COVID time periods. B: A plot demonstrating mean days between UE events is shown for pre, post, and COVID periods.
Table 5.
Rules Applied for Identifying Special Cause Variation With Statistical Process Control Chart

The reason for the UE was stratified into mechanical factors, provider factors, and patient factors. One case of UE could not be classified and was not included further. Most cases of UEs were associated with patient-related factors and were described as patient self-extubations during ventilator weaning, periods of decreased sedation, loosening of physical restraints (ie, for neurologic examinations in subjects with brain injuries), pauses in supervision, or a combination of these events (Table 6). There were no differences in age, sex, or mechanism of injury associated with the etiology of UE (Table 6). The ISS and emergency department vital signs were similar between groups. Subjects whose UE was due to mechanical issues more frequently required re-intubation, had a higher rate of pneumonia, and had longer ICU LOS and total hospital LOS than UEs from other causes (Table 6). Mortality though was highest with UEs due to provider factors. UEs due to patient-related factors were associated with the lowest rate of re-intubation, less pneumonia, lowest mortality, and higher proportion of discharge home (Table 6), suggesting a better overall functional status for these subjects despite similar injury burden measured by ISS. Subjects whose UE was due to patient factors tended to have a lower frequency of head injury and a lower head Abbreviated Injury Scale (AIS) score (Table 6), but these differences did not reach statistical significance. There was no difference between groups in the percentage of subjects with chest, abdominal, or extremity injuries or in the AIS scores for these body regions (data not shown).
Table 6.
Category of Unplanned Extubation

When the etiology for the UEs was plotted over time, UEs from mechanical and provider factors were relatively stable. UEs related to patient factors decreased over time from 80% of all UEs in 2012 and 2013 to 54% of UEs in 2021 (Fig. 2), but the difference between groups did not reach statistical significance. The statistical process control charts were repeated for each etiology of UEs, plotting days between each provider-related UE, for example, consecutively with the same rules applied (Table 5). Provider-related and mechanical UEs did not demonstrate any remarkable positive or negative trend while the chart for patient-related UEs was similar to that for the entire cohort displayed in Figure 1 (data not shown).
Fig. 2.
Number of unplanned extubation events per year categorized by patient-related factors, mechanical factors, and provider-related factors.
Discussion
Loss of an established airway can be lethal in injured patients. Loss of an ETT can also cause hypoxia that contributes to secondary traumatic brain injury.15 Intubated trauma patients, therefore, have risk for morbidity and mortality after UE that differs from other intubated patients.1–7 Our analysis of UEs over a 10-y period demonstrates several findings. Our rate of UEs was initially high (8% of subjects) and decreased over the study period. These rates are comparable to those published in other studies.1–3 When compared to subjects who did not experience a UE, those who had UE were younger, more commonly were diagnosed with pneumonia, required longer periods of mechanical ventilation, and had a longer ICU and hospital LOS, findings consistent with the UE negatively impacting care. However, the mortality rate for subjects with UE was lower, and they were more commonly discharged home or to rehabilitation facilities compared to intubated subjects without UE. The latter findings suggest a better functional status for UE subjects. A better functional subject profile was primarily associated with the etiology of the UE. UEs associated with patient-related factors, usually subject self-extubations, were associated with the lowest incidence of pneumonia, re-intubation, and death; had a lower LOS; and had higher frequency of discharge home. These are all findings supporting a better subject functional status in this subset despite the lack of significant difference in ISS, percentage of subjects with a head injury, or head AIS scores compared to other etiologies (Table 6). A good functional status would be required for the subject to intentionally remove the ETT, the most common scenario in this group. Purposeful subject participation is not required for UE from the other etiologies. This hypothesis is consistent with our finding that mortality was highest for subjects with UE due to mechanical or provider factors compared to patient factors (Table 6). We attempted to estimate functional status by measuring ISS, frequency of head injury, and head AIS, all of which estimate magnitude of injury or traumatic brain injury (Table 6), but the differences between groups were not significant. This finding may be due to the low number of subjects in the mechanical- and provider-related groups. It is also likely that ISS and head AIS are imprecise estimates of a patient's functional status after injury. There was no difference in emergency department Glasgow coma score between subjects who did or did not experience UE (Table 2), but this may be a limitation of how Glasgow coma score is recorded. The emergency department Glasgow coma score reported is the initial Glasgow coma score measured on arrival to the emergency department, can be influenced by prehospital medications or subject intoxication, and does not necessarily reflect the best Glasgow coma score obtainable once medications wear off. The effect of sedating medications or intoxicants may, therefore, confound the use of initial Glasgow coma score to reflect brain injury in our analysis. The highest Glasgow coma score within the first 24–48 h of care or at the time of UE would likely be a better measure of neurologic function after injury but was not routinely collected by our trauma registry during the study period.
As demonstrated in Figure 2, the frequency of mechanical and provider factors as an etiology for UE remained relatively stable over time, whereas the frequency of patient-related UEs decreased following implementation of our education/monitoring program. The enhanced education was directed to providers (physicians, RTs, and nurses) to improve awareness of UE, emphasize best practices, and share recommendations for avoiding UEs. Whereas we classified UEs as due to patient-related factors, these patient self-extubations are undoubtedly influenced by several factors including provider actions and institutional practices. Specific factors under provider or institutional control can impact the frequency of UE including method of ETT fixation,16 method of and medication used for sedation,5,17–20 use of ICU quality compliance toolkits,21 and use of physical restraints.20,22 However, none of these factors have consistently been shown to impact UE in a uniform manner. Restraints, for example, have been associated with both increased22 and decreased20 frequency of UEs. Restraints have also been linked to the development of posttraumatic stress disorder,23 confirming that striking the appropriate balance between patient safety and comfort remains challenging in the complex ICU environment. Others have shown that UEs that occur during deliberate attempts at weaning mechanical ventilation are associated with better outcomes,24 likely related to the more favorable clinical status that allows clinicians to intentionally decrease ventilator support. This association is similar to our findings, but we did not specifically measure whether UEs occurred during deliberate attempts at weaning in this analysis. Multiple factors can be involved in cases of UEs, and a multifaceted, multidisciplinary approach raising awareness and providing education to physicians, nurses, and RTs is important to decrease UEs. Our analysis demonstrates that classifying UEs by etiology and not simply grouping all UEs together is useful to determine what changes should be implemented and where they should be targeted to decrease UE frequency.
One could argue that if patients who experienced UE had a better functional status then they could have or should have been intentionally extubated sooner, thus avoiding the UE completely. That is likely a possibility for some patients since some UEs occur during sedation holidays or periods of intentional ventilator weaning. How to identify those patients who are going to “successfully” extubate themselves prior to the UE event or to identify the patient who will not require re-intubation is challenging, and there were no distinguishing factors among the different etiologies of UE, at least in the variables we were able to assess (Table 6). As shown in Table 6, a third of UEs in the subset of patient-related UEs failed and required re-intubation. Therefore, not every patient who can physically remove their own ETT should have it removed. The rate of re-intubation after intentional extubation is approximately 20%,25,26 so even in cases of planned extubation, determining which patients will remain extubated is imperfect. Methods to identify those patients who could have been extubated earlier and avoided the UE will require more detailed analysis.
There are limitations to this analysis. This study was longitudinal, but whether the PI education program was primarily responsible for the decrease in UEs cannot be conclusively determined. Unmeasured factors could have contributed to these findings. Since the analysis of UEs is presented at our multidisciplinary quality improvement meetings on a quarterly basis as one of our routine quality indicators, it is possible that the Hawthorne effect could contribute to these results. Our educational program was directed to physicians, nurses, and RTs, so we cannot determine whether the enhanced awareness of UEs led to changes in behavior or practice for a subset of providers or all providers. We did not measure nursing turnover, record the sedation regimen used, quantify pain medications administered, quantify delirium, assess tube fixation methods, or measure restraint use, all factors that can influence rate of UE.16–22 We also did not quantify timing or frequency of tracheostomy in this analysis. The earlier a tracheostomy is performed the less opportunity exists for an unplanned ETT removal, and some subjects at high risk underwent early tracheostomy. Our trauma/surgical critical care faculty has been stable over the study period with no apparent change in tracheostomy practice, so the likelihood of changes in tracheostomy practice accounting for these findings is low. Our classification system of etiology of UEs is based primarily on nursing and physician documentation and PI records. We acknowledge that documentation for these events can be suboptimal and only partially reflect the actual clinical factors involved. Our analysis included subjects admitted to the ICU, and we excluded patients who died in the emergency department, operating room, and PACU and were never admitted to the ICU. In addition, subjects that experienced UE in the emergency department or PACU may not be captured in this analysis. Any patient who experienced a UE in the emergency department or PACU, did not require re-intubation, was admitted to the floor, and had no ventilator days would not be captured in this analysis unless identified through our PI review process. Patients meeting these criteria though would have a good functional status, minimal injuries, and would likely be similar to subjects in the patient-related category.
Conclusions
UEs with mechanical- and provider- related factors were associated with a higher rate of re-intubation, pneumonia, and death, but their frequency did not change over time. UEs related to patient factors (self-extubations) were less frequently associated with pneumonia or re-intubation, were associated with better patient outcome, and were modifiable by a multidisciplinary PI education program. The hospital staffing challenges produced by the COVID-19 pandemic did not alter the rate of UEs in this analysis.
Footnotes
The authors have disclosed no conflicts of interest.
See the Related Editorial on Page 151
REFERENCES
- 1. Tindol GA, DiBenedetto RJ, Kosciuk L. Unplanned extubations. Chest 1994;105(6):1804–1807. [DOI] [PubMed] [Google Scholar]
- 2. Epstein SK, Nevins ML, Chung J. Effect of unplanned extubations on outcome of mechanical ventilation. Am J Respir Crit Care Med 2000;161(6):1912–1916. [DOI] [PubMed] [Google Scholar]
- 3. Kapadia FN, Tekawade PC, Nath SS, Pachpute SS, Saverkar SS, Bhise RA, et al. A prolonged observational study of tracheal tube displacements: benchmarking an incidence < 0.5–1% in a medical-surgical intensive care unit. Ind J Crit Care Med 2014;18(5):273–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lee JH, Lee HC, Jeon YT, Hwang JW, Lee H, Oh HW, Park HP. Clinical outcomes after unplanned extubation in a surgical intensive care unit population. World J Surg 2014;38(1):203–210. [DOI] [PubMed] [Google Scholar]
- 5. De Groot RI, Dekkers OM, Herold IHF, de Jonge E, Arbous MS. Risk factors and outcomes after unplanned extubations on the ICU: a case control study. Crit Care 2011;15(1):R19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chuang ML, Lee CY, Chen YF, Huang SF, Lin IF. Revisiting unplanned endotracheal extubation and disease severity in intensive care units. PLoS ONE 2015;10(10):e0139864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fontenot AM, Malizia RA, Chopko MS, Flynn WJ, Lukan JK, Wiles CE, Guo WA. Revisiting endotracheal self-extubation in the surgical and trauma intensive care unit: are they all fine? J Crit Care 2015;30(6):1222–1226. [DOI] [PubMed] [Google Scholar]
- 8. Christie JM, Dethlefsen M, Cane RD. Unplanned endotracheal extubation in the intensive care unit. J Clin Anesth 1996;8(4):289–293. [DOI] [PubMed] [Google Scholar]
- 9. Penuelas O, Frutos-Vivar F, Esteban A. Unplanned extubation in the ICU: a marker of quality assurance of mechanical ventilation. Crit Care 2011;15(2):128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cronin JN, Camporota L, Formenti F. Mechanical ventilation in COVID-19: a physiological perspective. Exp Physiol 2022;107(7):683–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Arabi VM, Aldekhyl S, Al Qahtani S, Al-Dorzi HM, Abdukahil SA, Al Harbi MK, et al. ; Saudi Critical Care Trials Group. Effect of helmet noninvasive ventilation vs usual respiratory support on mortality among patients with acute hypoxemic respiratory failure due to COVID-19: the HELMET-COVID randomized clinical trial. JAMA 2022;328(11):1063–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wilensky GR. The COVID-19 pandemic and the US health care workforce. JAMA Health Forum 2022;3(1):e220001. [DOI] [PubMed] [Google Scholar]
- 13. Al-Amin M, Nazmul Islam M, Li K, Shiels N, Buresh J. Is there an association between hospital staffing levels and in-patient–COVID-19 mortality rates? PLoS ONE 2022;17(10):e0275500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 2002;166(10):1338–1344. [DOI] [PubMed] [Google Scholar]
- 15. Okonkwo DO, Shutter LA, Moore CA, Temkin NR, Puccio AM, Madden CJ, et al. Brain oxygen optimization in severe traumatic brain injury phase 2: a phase 2 randomized trial. Crit Care Med 2017;45(11):1907–1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Buckley JC, Brown AP, Shin JS, Rogers KM, Hoftman NN. A comparison of the Haider Tube-Guard endotracheal tube holder versus adhesive tape to determine if this novel device can reduce endotracheal tube movement and prevent unplanned extubation. Anesth Analg 2016;122(5):1439–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tanios M, Epstein S, Grzeskowiak M, Nguyen M, Park H, Leo J. Influence of sedation strategies on unplanned extubation in a mixed intensive care unit. Am J Crit Care 2014;23(4):306–314; quiz 315. [DOI] [PubMed] [Google Scholar]
- 18. Girard TD, Kress JP, Fuchs BD, Thomason JWW, Schweickert WD, Pun BT, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomized controlled trial. Lancet 2008;371(9607):126–134. [DOI] [PubMed] [Google Scholar]
- 19. Tan JA, Ho KM. Use of dexmedetomidine as a sedative and analgesic agent in critically ill adult patients: a meta-analysis. Intensive Care Med 2010;36(6):926–939. [DOI] [PubMed] [Google Scholar]
- 20. Frezza EE, Carleton GL, Valenziano CP. A quality-improvement and risk-management initiative for surgical ICU patients: a study of the effects of physical restraints and sedation on the incidence of self-extubation. Am J Med Qual 2000;15(5):221–225. [DOI] [PubMed] [Google Scholar]
- 21. DuBose JJ, Inaba K, Shiflett A, Trankiem C, Teixeira PGR, Salim A, et al. Measurable outcomes of quality improvement in the trauma intensive care unit: the impact of a daily quality rounding checklist. J Trauma 2008;64(1):22–29. [DOI] [PubMed] [Google Scholar]
- 22. Chang LY, Wang KWK, Chao YF. Influence of physical restraint on unplanned extubation of adult intensive care patients: a case-control study. Am J Crit Care 2008;17(5):408–415; quiz 416. [PubMed] [Google Scholar]
- 23. Jones C, Backman C, Capuzzo M, Flaatten H, Rylander C, Griffiths RD. Precipitants of posttraumatic stress disorder following intensive care: a hypothesis-generating study of diversity in care. Intensive Care Med 2007;33(6):978–985. [DOI] [PubMed] [Google Scholar]
- 24. Razek T, Gracias V, Sullivan D, Braxton C, Gandhi R, Gupta R, et al. Assessing the need for re-intubation: a prospective evaluation of unplanned endotracheal extubation. J Trauma Acute Care Surg 2000;48(3):466–469. [DOI] [PubMed] [Google Scholar]
- 25. Miu T, Joffe AM, Yanez ND, Khandelwal N, Dagal AHC, Deem S, Treggiari MM. Predictors of re-intubation in critically ill patients. Respir Care 2014;59(2):178–185. [DOI] [PubMed] [Google Scholar]
- 26. Bobbs M, Trust MD, Teixeira P, Coopwood B, Aydelotte J, Tabas I, et al. Decreasing failed extubations with the implementation of an extubation checklist. Am J Surg 2019;217(6):1072–1075. [DOI] [PubMed] [Google Scholar]