Abstract
Objective:
At first hospitalization, a long duration of untreated psychosis (DUP) predicts illness severity and worse treatment outcomes. The mechanism of this association, however, remains unclear. It has been hypothesized that lengthy untreated psychosis is toxic, or reflects a more severe form of schizophrenia. Alternatively, the association may be an artifact of lead-time bias. These hypotheses are tested in a longitudinal study of schizophrenia with 2,137 observations spanning from childhood to 20 years after first admission.
Methods:
Data are from the Suffolk County Mental Health Project. The cohort included 287 individuals with schizophrenia or schizoaffective disorder. DUP was defined as days from first psychotic symptom to first psychiatric hospitalization. Psychosocial function was assessed using the Premorbid Adjustment Scale (PAS) and Global Assessment of Functioning (GAF) scale. Psychosocial function trajectories were estimated using multilevel spline regression models adjusted for gender, occupational status, race, and antipsychotic medication.
Results:
Both long and short DUP patients experienced similar declines in psychosocial function, but declines occurred at different times relative to first admission. Long DUP patients experienced most of these declines prior to first admission, while short DUP patients experienced declines after first admission. When psychosocial function was analyzed relative to psychosis onset, DUP did not predict illness course.
Conclusions:
The association between DUP and psychosocial function may be an artifact of early detection, creating the illusion that early intervention is associated with improved outcomes. In other words, DUP may be better understood as an indicator of illness stage than a predictor of course.
Introduction
Duration of untreated psychosis (DUP)—the amount of time that elapses between psychosis onset and treatment initiation—predicts illness course in schizophrenia. DUP predicts likelihood and extent of remission (1), time to remission, response to coordinated specialty care (2), response to antipsychotics (3), as well as symptom severity and psychosocial function (4). In other domains of illness course there is a lack of convergent findings (5), notably in the lack of an association between DUP and cognitive functioning (6). However, while some studies have not detected an effect of DUP (7), meta-analyses show DUP explains 2–13% of variance in outcome, depending on the sample and duration of the follow-up period (4,8). DUP is one of the more potent predictors of course in schizophrenia, with an effect larger than that of premorbid adjustment (4,9) and age of onset (10). Gender may play a larger role (11), but unlike most other predictors, DUP is modifiable. One aim of early intervention programs has been to identify psychosis in its early stages and minimize DUP (2,12,13).
Why long DUP is associated with a poor illness course remains unclear. It has been hypothesized that untreated psychotic symptoms are toxic, meaning a long DUP results in irreversible neurological or psychosocial damage (14–16). According to the neurological variant of this hypothesis, commonly referred to as “neurotoxicity”, individuals have similar premorbid functioning, but a long DUP results in more neuronal damage, a greater functional decline, and chronic impairment. While long DUP appears to be associated with structural and functional abnormalities (17–19), the overall evidence remains inconclusive (20,21). Regardless of associations with brain structure or function, untreated psychosis could result in psychosocial toxicity (16), in which untreated psychosis prevents the individual from navigating developmental hurdles, resulting in chronic impairment. Figure 1A depicts the hypothesis that long DUP is either biologically or psychosocially toxic, or both.
Figure 1.
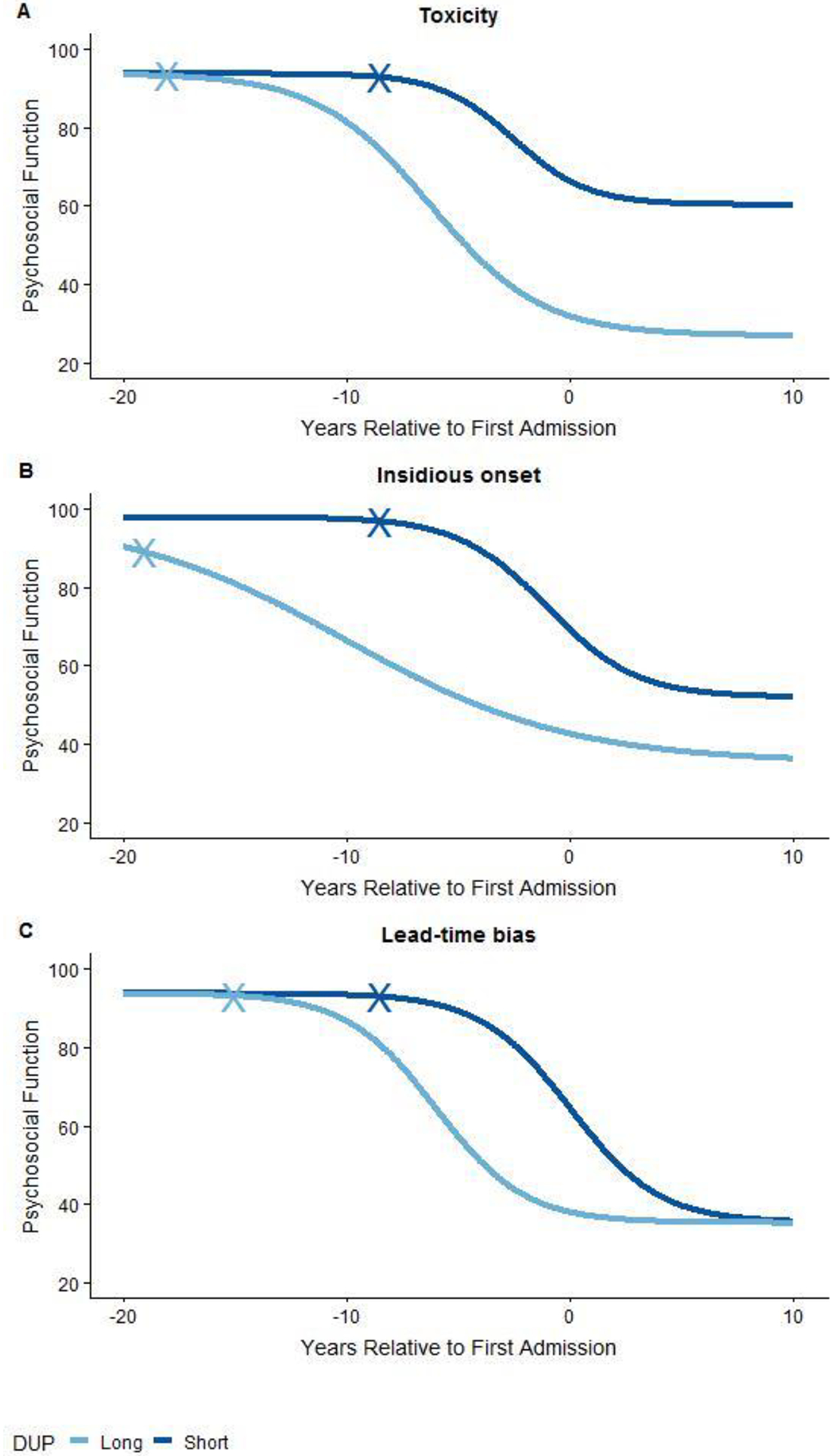
Note. Three hypotheses for the link between DUP and psychosocial function over the course of schizophrenia: (A) toxicity, (B) insidious, persistent form of illness, (C) lead-time bias. DUP = duration of untreated psychosis. X-marks indicate the point of psychosis onset.
Alternatively, some evidence suggests that long DUP reflects a more severe form of schizophrenia, typified by an early and insidious onset (22,23), poor premorbid functioning (24), and treatment resistance (3). Figure 1B illustrates this hypothesis. A patient with long DUP is more impaired throughout the illness course. This hypothesis is consistent with longitudinal research showing that a long DUP is associated with lower odds of recovery after the first psychotic episode, and more commonly precedes non-affective, as opposed to affective, psychosis (5,25).
A third explanation is that DUP reflects differences in illness stage—that is, DUP does not predict a worse illness trajectory, but does indicate that an individual is farther along in their illness trajectory. Compared to someone with short DUP, a long DUP patient may already be in an advanced stage of illness by first admission (26), and therefore functioning more poorly. If so, comparing short and long DUP individuals would introduce lead-time bias, a known artifact of epidemiological studies in which early detection appears to improve outcomes because it shifts the observation window forward. Figure 1C depicts this alternative. Patients with long and short DUP are on the same trajectory, only shifted relative to entry in the study. According to this hypothesis, if time is measured relative to psychosis onset rather than entry into the study, outcomes will be unrelated to DUP.
These models generate testable predictions. If the toxicity hypothesis holds, DUP should be associated with long-term but not premorbid deficits in psychosocial function. If long DUP indicates a more insidious, persistent form of illness, DUP should be associated with differences in both premorbid and long-term psychosocial function. If lead-time bias explains the observed effect, DUP should be associated with psychosocial function only in the period surrounding first admission, and defining illness course relative to psychosis onset should wipe out the association with DUP. A rigorous test of these predictions requires access to several kinds of data: 1) premorbid psychosocial function; 2) date of psychosis onset; 3) date of first treatment; and 4) long-term psychosocial function post-onset. The present study is the first to test these alternative explanations.
Methods
Sample and Procedure
Data were drawn from the Suffolk County Mental Health Project, a longitudinal study of first-admission psychosis (27,28). Between 1989 and 1995, individuals with first-admission psychosis were recruited from the 12 inpatient facilities in Suffolk County, New York (response rate 72%). The Stony Brook University Committee on Research Involving Human Subjects and the hospital review boards approved the protocol annually. Written consent was obtained from all study participants, or from their parents for those who were minors. Eligibility criteria included residence in Suffolk County, age between 15 and 60, ability to speak English, IQ > 70, first admission within the past 6 months, current psychosis, no apparent medical etiology for psychotic symptoms, and capacity to provide informed consent. In-person follow-up interviews were conducted at 6 months, 24 months, 48 months, 10 years, and 20 years after baseline.
At baseline, 628 participants met inclusion criteria. To select those with a reliable schizophrenia diagnosis, the cohort was defined by the last available study diagnosis. Of the 628 participants ascertained at first hospitalization, 287 had a schizophrenia spectrum diagnosis (schizophrenia, schizoaffective, or schizophreniform disorder) at their last available consensus review (29). Their demographic characteristics are reported in Table 1. Detailed statistics on the distribution of DUP are reported in Table S1.
Table 1.
Demographic Characteristics
| N | % | |
|---|---|---|
| Gender | ||
| Male | 185 | 64.5 |
| Female | 102 | 35.5 |
| Race/Ethnicity | ||
| Caucasian | 199 | 69.3 |
| African-American | 54 | 18.8 |
| Hispanic | 23 | 8.0 |
| Asian | 10 | 3.5 |
| Native American | 1 | 0.4 |
| Occupational Status | ||
| Skilled labor or above | 186 | 64.8 |
| Semi-skilled and lower | 101 | 35.2 |
| Antipsychotic Medication | ||
| First admission | 248 | 86.4 |
| 6 months | 248 | 86.7 |
| 24 months | 203 | 74.9 |
| 48 months | 214 | 75.9 |
| 10 years | 185 | 84.9 |
| 20 years | 125 | 82.8 |
| Age at Baseline | ||
| 15–20 | 36 | 12.5 |
| 21–30 | 131 | 45.7 |
| 31–40 | 81 | 28.2 |
| 41–50 | 31 | 10.8 |
| 51–60 | 8 | 2.8 |
| Illness Severity (GAF) at Baseline | ||
| 21–40 | 70 | 24.4 |
| 41–60 | 126 | 43.9 |
| 61–80 | 90 | 31.4 |
| >80 | 1 | 0.3 |
| Duration of Untreated Psychosis (days) | ||
| <30 days | 7 | 2.4 |
| 30–180 days | 53 | 18.5 |
| 180–365 days | 94 | 32.8 |
| >365 days | 133 | 46.3 |
Note. GAF = Global Assessment of Function.
Measures
Diagnosis.
Research diagnoses were made by the consensus of study psychiatrists at baseline, 6 months, 24 months, 10 years, and 20 years using all available information (the diagnostic process is reported in Bromet, 29) including medical records, significant other interviews, and the Structured Clinical Interview for DSM-III at first admission and DSM-IV thereafter (30,31).
Psychosocial functioning.
Premorbid psychosocial function was assessed using an interview based on the Premorbid Adjustment Scale (PAS; 32,33) administered to participants and significant others at baseline and month six. Master’s level social workers with experience treating patients with chronic mental illness made initial PAS ratings based on school records, the participant’s PAS responses, and parents’ PAS responses if available. Ratings were confirmed by RK. The PAS consists of five items (Sociability and withdrawal, Peer relationships, Scholastic performance, Adaptation to School, Social-sexual) rated on 7-point scale (0 to 6 with 0 representing good functioning). Rating periods were childhood (up to age 11), early adolescence (ages 12–15), and late adolescence (ages 16–18).
After first hospitalization, study psychiatrists made consensus psychosocial functioning ratings using the Global Assessment of Function (GAF) scale. GAF ratings combined symptom and functional impairment using all available information. The ratings reflected best level of functioning over any one-month period in the past year. Between the PAS (3 time points) and GAF (6 time points), 2,137 ratings of psychosocial functioning were available over the 9 time points.
In order to express psychosocial function on the same metric throughout, we transformed PAS scores to the GAF metric. First, PAS scores were reverse transformed so that higher numbers reflected better function, and rescaled to a 0–1 metric. Next, composite scores were calculated as the mean of the five PAS items. Seventy-seven individuals had their first admission in late adolescence, and thus had late-adolescent PAS and baseline GAF ratings for the same time period. This group did not differ from the larger sample in terms of functioning at childhood, early adolescent, or baseline hospitalization (Table S2). PAS scores were rescaled to the GAF metric by adding the difference in means (21.5) then multiplying by the ratio of their standard deviations (62.3). Due to illness onset, the number of premorbid ratings decreased from 265 in childhood, to 259 in early adolescence, to 233 in late adolescence.
Duration of Untreated Psychosis.
DUP was defined as the interval between the onset of the first psychotic symptom and the first psychiatric hospital admission. The date of onset was determined based on symptom timelines obtained during the first admission and 6-month follow-up diagnostic interviews (SCID), in which interviewers assessed first date of onset for all threshold hallucinations, delusions, and catatonic symptoms. This information was supplemented by informant interviews that covered pre-baseline psychotic symptoms, school records, and medical records. At the 24-month follow up, psychiatrists used all available information to determine the date of onset of the first clear psychotic symptom. The distribution of DUP was highly skewed, with range from zero days to 24 years, mean 726 (standard deviation 94.89) days, and median 346 (inter-quartile range 200, 945) days. This range is comparable with two meta-analyses on DUP (4,8), which reported mean DUPs of 721 days and 427 days.
Many definitions of DUP have been used in the literature (16). Since some studies of neurotoxicity define the end of the DUP interval as the first treatment with antipsychotic medication, we also calculated DUP according to this operationalization. The median of this score (310 days, inter-quartile range 150, 671) was somewhat shorter than that reported by Kane and colleagues in treatment programs across 21 states in the U.S. (median 518 days, 2). The two DUP scores were strongly correlated (r = 0.77) and produced the same pattern of results in subsequent analyses. Table S3 reports the results of analyses defining DUP relative to first treatment with antipsychotic medication.
Covariates.
Occupational status was quantified as the occupation of the primary breadwinner of the participants’ family, rated on Hollingshead’s rating of occupational status, a scale from 1 (“large business owner/major professional/executive”) to 8 (“not working”) (based on 34). Slightly more than half of participants were of an occupational status of 5 “skilled laborer” or greater (see Table 1). Prescription of antipsychotic medication was based on participants’ self-report, corroborated by medical records when available. This is a dichotomous variable that is 1 for participants who were prescribed antipsychotic medication for greater than 25% of the interval, and 0 for all others. The proportion of participants on antipsychotic medication at each time point is reported in Table 1.
Missing Data
DUP was known for all 287 individuals with a schizophrenia spectrum diagnosis. Psychosocial function ratings were available for at least 70% of participants at each time point. Forty-three participants died over the study’s course, accounting for 14% of missing data points. Participants whose psychosocial function ratings were missing at any time point did not differ from those for whom ratings were known in terms of gender or occupational status. Minority participants were more likely to be missing data in childhood (χ2(N=287,4)=17.86, P=0.001) and early adolescence (χ2(N=287, 4)=13.67, P=0.008). However, missingness was not associated with race at any other time point. Participants whose psychosocial function ratings were known were more likely to be receiving antipsychotic medication at 6 months (Fisher’s exact test P=0.02), 24 months (P<0.001) and 48 months (P<0.001). Analyses used full information maximum likelihood estimation, which includes partial cases. Table S4 reports the number of psychosocial function ratings available at each follow up, as well as their distributions.
Analyses
For cross-sectional analyses of the association between DUP and psychosocial function, DUP was dichotomized by a median split. All other analyses quantified DUP as a continuous variable.
Due to the non-normal distribution of DUP, associations between DUP and change in psychosocial function before and after first admission were tested using Kendall rank-order correlations.
Associations between DUP and illness course were first visualized using a LOESS, a scatterplot smoother. Next, associations were tested using multilevel spline regression models. Multilevel spline models include random effects estimates each person’s intercept and slope, thus modeling individual trajectories. However, these results focus on fixed effects of the multilevel models, which reflect the sample average. Spline models allow for non-linear trajectories by estimating a point or points along the independent variable—time—at which the average trajectory changes. For a review of this method, see Howe and colleagues (35). All multilevel spline models were estimated using the glmmix function in SAS.
Multilevel spline models were built in the following order. First, we modeled mean psychosocial function. Second, we added time as a predictor, measured relative to either psychosis onset or first admission. Third, we added DUP, to quantify stable differences in psychosocial function explained by DUP. Fourth, we estimated an interaction between DUP and time, to test whether DUP predicted differing trajectories of psychosocial function. For each model, we estimated the point at which psychosocial trajectories changed by placing the inflection point at every consecutive 1-year interval and comparing model fit via the Bayesian Information Criterion (reported in Table S5). Optimal models were selected by comparing fit via the Bayesian Information Criterion (BIC, reported in Table S6).
Finally, all analyses were repeated adjusting for gender, occupational status, race, and prescription of an antipsychotic medication. These covariates were added as predictors of both intercepts and slopes.
Results
DUP was associated with psychosocial function at first admission (Cohen’s d = 0.75, P<0.001), six months after first admission (d = 0.34, P=0.01), and 24 months after first admission (d = 0.38, P=0.004). GAF was assessed relative to the best month in the past year. As a result, ratings at first admission and six-month after may have reflected premorbid function for those with short DUP. Note, however, that group differences at 24 months do not show such overlap and remain significant. Associations outside this window were not significant; that is, DUP was not associated with differences in either premorbid or long-term psychosocial function. Bivariate correlations indicated that a longer DUP was associated with greater declines in psychosocial function between childhood and first admission (τ = −0.26, P<0.001). However, in the follow-up period, the opposite pattern emerged. Shorter DUP was associated with larger post-onset declines in psychosocial function (τ = 0.24, P=0.001). Figure 2 depicts the distribution of pre- and post-admission changes in psychosocial function broken down by tertiles of DUP.
Figure 2.
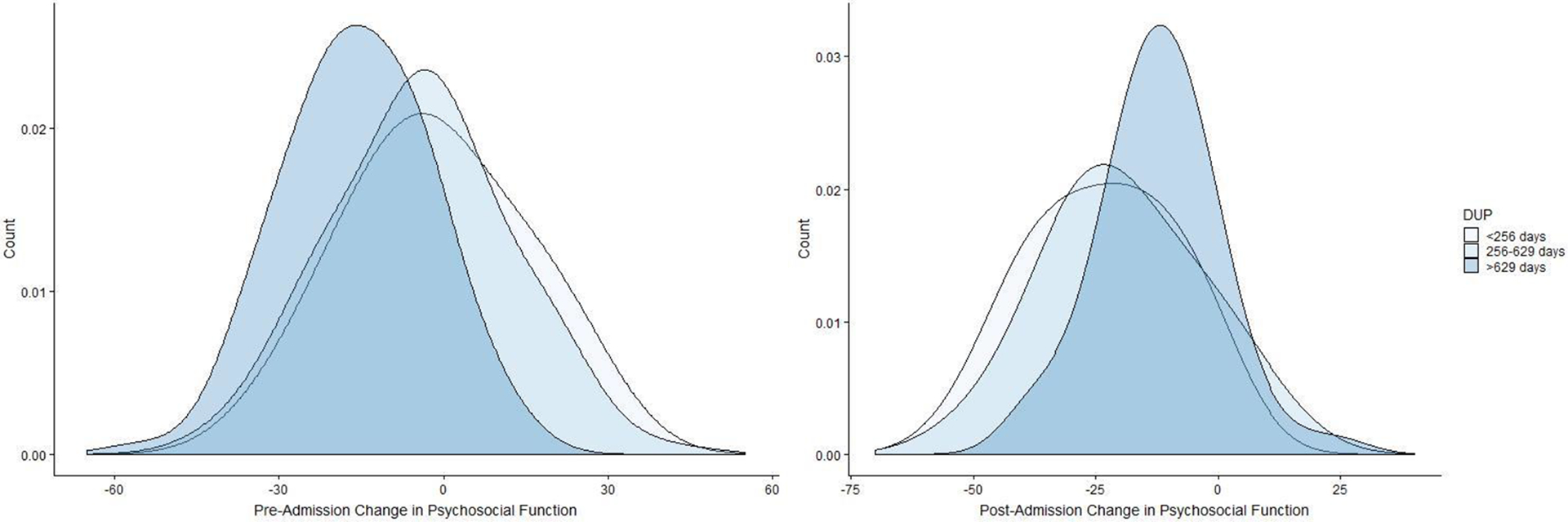
Note. Density plots of pre- and post-admission change in psychosocial function by tertiles of DUP. Those with longer DUP experience greater losses of psychosocial function before first admission than those with short DUP. However, those with short DUPs experience greater psychosocial function after first admission than those with long DUP.
Figure 3 depicts psychosocial function relative to first psychotic symptom. Table 2 reports fixed effects estimates of the multilevel spline models based on these two conceptualizations. When psychosocial function was analyzed relative to first admission, DUP was associated with illness course across the lifespan (B = −0.04, 95% confidence interval [CI] −0.06 to −0.03, P<0.001). When psychosocial function was analyzed relative to onset of the first psychotic symptom, DUP was no longer a significant predictor (B = 0.00, 95% CI −0.01 to 0.02, P=0.79). We also estimated the interaction between included DUP and time and found this worsened fit, indicating DUP did not predict the rate of functional decline (Table S6). Supplemental Figure 1 depicts the model-implied illness course for individuals with a long versus short DUP, plotted relative to psychosis onset. The model-implied trajectories are very similar, and the difference between the two lines is not statistically significant.
Figure 3.
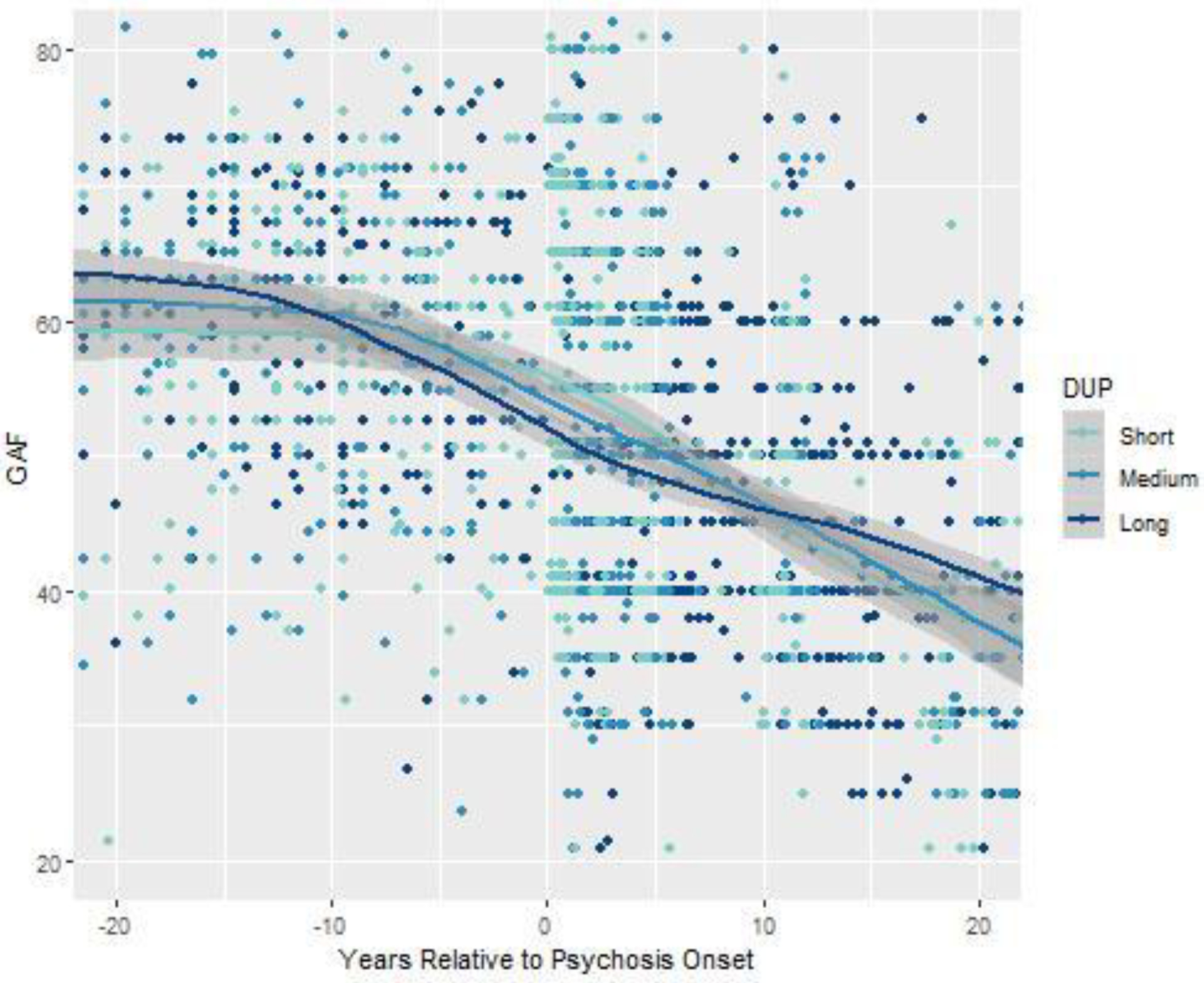
Note. Loess plots of psychosocial function (Global Assessment of Function, GAF) relative to first psychotic symptom. For illustrative purposes, DUP is trichotomized by tertiles, with short DUP less than 256 days, medium DUP 256 to 629 days, and long DUP greater than 629 days.
Table 2.
Course of Illness and DUP in Schizophrenia-Spectrum Disorders (N = 287)
| Years to first admission | Years to onset of psychosis | |||||
|---|---|---|---|---|---|---|
| B | SE | P | B | SE | P | |
| Intercept | 59.17 | 0.60 | <0.001 | 59.24 | 0.54 | <0.001 |
| Slope 1a | −0.18 | 0.05 | 0.00 | −0.11 | 0.05 | 0.04 |
| Slope 2a | −0.85 | 0.03 | <0.001 | −0.81 | 0.03 | <0.001 |
| DUP | −0.04 | 0.01 | <0.001 | 0.00 | 0.01 | 0.79 |
Note. Time is expressed in year increments. Coefficients for DUP were transformed to reflect the difference in illness severity attributable to 30 days untreated psychosis. DUP = duration of untreated psychosis.
Slope 1 reflects annual change in psychosocial function from childhood to the inflection point. Slope 2 reflects annual change in psychosocial function over the remainder of the course of illness.
In post-hoc analyses, we also tested the effects of gender, race, and occupational status as predictors of illness trajectories. These models had worse fit to the data than models with simple mean effects of these covariates, and were not significant predictors of illness course.
Discussion
In this study, we tested three different hypotheses regarding the link between DUP and illness course. The toxicity hypothesis suggests that untreated psychosis causes irreversible neuronal or psychosocial damage (14,36), leading to long-term differences in illness course. Alternatively, a long DUP has been hypothesized to reflect, rather than cause, a more insidious, persistent psychotic disorder (22,37,38). Here we describe a third hypothesis, which is that the effect of DUP is an artifact of lead-time bias. Long DUP patients are ahead of short-DUP patients in illness progression at any given study time-point, causing spurious differences between groups even though they are on the same trajectory.
In a sample of 287 individuals recruited during their first admission for psychosis and ultimately diagnosed with schizophrenia or schizoaffective disorder, and for whom symptom severity and psychosocial function were characterized at 2,137 points from childhood to 20 years post-admission, both long and short DUP groups experienced declines. Long DUP patients experienced most of these declines prior to first admission. Short DUP patients were not spared, but rather, experienced declines after first admission. In this way, lead-time bias creates the illusion of a treatment effect attributable to early intervention. Indeed, DUP no longer predicted trajectories when individuals were compared in terms of time relative to psychosis onset.
These findings suggest a potential for biased inferences in studies of first episode psychosis. Studies that assess outcomes for a short period after first admission may identify protective effects of early diagnosis or treatment that actually reflect differences in illness stage, rather than changes to illness course. However, these results should not be interpreted as evidence that early intervention is ineffective, or that schizophrenia results in an inevitable decline. Rather, our results point to a need to control for lead-time bias in order to assess the effect of early interventions. For instance, in this cohort the association between DUP and psychosocial function at first-admission (d = 0.75) was greater than estimates of antipsychotic efficacy, which are large (39). Such confounds significantly reduce statistical power to detect real treatment effects.
Comprehensive pharmacological and psychosocial treatment has shown to be effective in remediating symptoms and improving quality of life in schizophrenia (2,40). However, without sustained intervention, a majority of patients relapse (41,42). This epidemiological cohort has received intermittent and inconsistent care that relied primarily on antipsychotic medications, as was typical of the era, which may explain the lack of change in trajectory after first admission (43–45). While early intervention alone may not halt the disease process, comprehensive and sustained care improves the quality of life for those with schizophrenia.
Limitations
In the present analyses, both date of onset and premorbid function were estimated based on information collected between first admission and six months later. Depending on the length of DUP and age at first admission, this could require collecting information about events that occurred years ago. We minimized error due to retrospective assessment by supplementing self-report interviews with significant other interviews and historical data from both school and medical records (46). The analysis is also limited by the use of different measures of premorbid and post-admission psychosocial function, which required converting one metric to another (47). To our knowledge, however, no single measure could capture psychosocial function early in development as well as symptoms and functioning in adulthood.
Long periods of time passed between some of the follow-up interviews, however, data were available for time points critical to distinguishing the hypothesized trajectories. In addition, the long-term nature of the study allowed for reappraisal of diagnoses based on longitudinal data. This increases diagnostic validity, reducing the risk of excluding patients with schizophrenia whose initial presentation was that of another psychotic disorder with a better prognosis. There are other outcomes that may be associated with DUP, such as symptom severity or need for treatment, which were not addressed here due to the lack of pre-admission data. In addition, we note that psychosocial function is an indirect measure of neurotoxicity, unlike direct evidence from neuroimaging. Future research should investigate trajectories of these outcomes.
As a first-admission study, this sample does not include people with schizophrenia who were never hospitalized. However, the range of DUP values is broadly in line with other first-episode studies (4), and is shorter than that of a large and diverse sample drawn from clinical settings across the United States (2), suggesting our sample is not biased towards advanced cases. In addition, the wide age range of the sample and range of observed DUP values increases statistical power to detect an effect, relative to analyses of intervention studies aimed at minimizing DUP. Like any single study, these findings require replication.
The interpretation of this and other studies of DUP is qualified by the many ways in which DUP can be defined. We compared multiple definitions of DUP, none of which changed the results. However, there are alternative definitions—the interval start could be defined as the first psychiatric symptom of any kind (16), and the endpoint as the date of first effective treatment (48) or first contact with a mental healthcare provider (49)—which depend on data not available in this cohort.
Conclusions
An inverse association between DUP and illness course is often found in schizophrenia research. However, the association appears to be explained by lead-time bias, in which a short DUP is associated with better outcomes because DUP is confounded with illness stage. That is, those with a short DUP are in an earlier stage, and therefore appear to have better outcomes than those with a long DUP, who are in a later stage. When lead-time is accounted for by analyzing course relative to psychosis onset, DUP no longer predicts outcomes in this cohort. These findings argue against the toxicity of untreated psychosis, as well as the hypothesis that a long DUP signals a more insidious, severe psychotic disorder. To avoid confounding due to lead-time bias, studies of first episode schizophrenia should estimate course of illness and treatment response relative to time since psychosis onset. Treatments more potent than those available to this cohort may be able to alter illness trajectory and make early intervention beneficial.
Supplementary Material
Acknowledgements:
This research was supported by National Institutes of Health (MH44801 to EB and MH094398 to RK). The authors gratefully acknowledge the support of the participants and mental health community of Suffolk County for contributing their time and energy to this project. Special thanks to Janet Lavelle and Jonathan Sandler, as well as the interviewers for their careful assessments, and the psychiatrists who derived the consensus diagnoses.
Disclosures:
Dr. Kane has been a consultant for Alkermes, Amgen, Bristol-Myers Squibb, Eli Lilly, EnVivo Pharmaceuticals (Forum), Forest, Genentech, H. Lundbeck, Intra-Cellular Therapies, Janssen Pharmaceutica, Johnson and Johnson, Merck, Neurocrine, Newron, Novartis, Otsuka, Pierre Fabre, Reviva, Roche, Sunovion, and Teva; he has received honoraria for lectures from Bristol-Myers Squibb, Genentech, Janssen, Lundbeck, and Otsuka; and he is a shareholder in LB Pharmaceuticals and Vanguard Research Group.
References
- 1.Loebel AD, Lieberman JA, Alvir JM, Mayerhoff DI, Geisler SH, Szymanski SR. Duration of psychosis and outcome in first-episode schizophrenia. Am J Psychiatry. 1992. Sep;149(9):1183–8. [DOI] [PubMed] [Google Scholar]
- 2.Kane JM, Robinson DG, Schooler NR, Mueser KT, Penn DL, Rosenheck RA, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE early treatment program. Am J Psychiatry. 2015;173(4):362–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karson C, Duffy RA, Eramo A, Nylander A-G, Offord SJ. Long-term outcomes of antipsychotic treatment in patients with first-episode schizophrenia: a systematic review Neuropsychiatr Dis Treat. 2016. Jan 6;12:57–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: A systematic review. Arch Gen Psychiatry. 2005. Sep 1;62(9):975–83. [DOI] [PubMed] [Google Scholar]
- 5.Craig TJ, Bromet EJ, Fennig S, Tanenberg-Karant M, Lavelle J, Galambos N. Is there an association between duration of untreated psychosis and 24-month clinical outcome in a first-admission series? Am J Psychiatry. 2000;157(1):60–66. [DOI] [PubMed] [Google Scholar]
- 6.Rund BR, Barder HE, Evensen J, Haahr U, Hegelstad W ten V, Joa I, et al. Neurocognition and Duration of Psychosis: A 10-year Follow-up of First-Episode Patients. Schizophr Bull. 2016. Jan 1;42(1):87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ho B-C, Andreasen NC. Long delays in seeking treatment for schizophrenia. The Lancet. 2001. Mar 24;357(9260):898–900. [DOI] [PubMed] [Google Scholar]
- 8.Penttilä M, Jääskeläinen E, Hirvonen N, Isohanni M, Miettunen J. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2014;205(2):88–94. [DOI] [PubMed] [Google Scholar]
- 9.Bottlender R, Sato T, Jäger M, Groll C, Strau\s s A, Möller H-J. The impact of duration of untreated psychosis and premorbid functioning on outcome of first inpatient treatment in schizophrenic and schizoaffective patients. Eur Arch Psychiatry Clin Neurosci. 2002;252(5):226–231. [DOI] [PubMed] [Google Scholar]
- 10.Wieselgren I-M, Lindström L A prospective 1–5 year outcome study in first-admitted and readmitted schizophrenic patients; relationship to heredity, premorbid adjustment, duration of disease and education level at index admission and neuroleptic treatment. Acta Psychiatr Scand. 1996;93(1):9–19. [DOI] [PubMed] [Google Scholar]
- 11.Harrison G, Croudace T, Mason P, Glazebrook C, Medley I. Predicting the long-term outcome of schizophrenia. Psychol Med. 1996. Jul;26(4):697–705. [DOI] [PubMed] [Google Scholar]
- 12.Hegelstad W, Larsen TK, Auestad B, Evensen J, Haahr U, Joa I, et al. Long-term follow-up of the TIPS early detection in psychosis study: effects on 10-year outcome. Am J Psychiatry. 2012;169(4):374–380. [DOI] [PubMed] [Google Scholar]
- 13.McGorry P Early intervention in psychosis. J Nerv Ment Dis. 2015;203(5):310–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wyatt RJ. Neuroleptics and the natural course of schizophrenia. Schizophr Bull. 1991;17(2):325–351. [DOI] [PubMed] [Google Scholar]
- 15.McGorry PD, Warner R. Consensus on early intervention in schizophrenia. 2002; [DOI] [PubMed]
- 16.Compton MT, Carter T, Bergner E, Franz L, Stewart T, Trotman H, et al. Defining, operationalizing and measuring the duration of untreated psychosis: advances, limitations and future directions. Early Interv Psychiatry. 2007;1(3):236–250. [Google Scholar]
- 17.Lappin JM, Morgan K, Morgan C, Hutchison G, Chitnis X, Suckling J, et al. Gray matter abnormalities associated with duration of untreated psychosis. Schizophr Res. 2006. Apr 1;83(2):145–53. [DOI] [PubMed] [Google Scholar]
- 18.Sarpal DK, Robinson DG, Fales C, Lencz T, Argyelan M, Karlsgodt KH, et al. Relationship between duration of untreated psychosis and intrinsic corticostriatal connectivity in patients with early phase schizophrenia. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2017. Oct;42(11):2214–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goff DC, Zeng B, Ardekani BA, Diminich ED, Tang Y, Fan X, et al. Association of hippocampal atrophy with duration of untreated psychosis and molecular biomarkers during initial antipsychotic treatment of first-episode psychosis. JAMA Psychiatry. 2018;75(4):370–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson KK, Rodrigues M, Mann K, Voineskos A, Mulsant BH, George TP, et al. Minimal evidence that untreated psychosis damages brain structures: a systematic review. Schizophr Res. 2015. Mar;162(1–3):222–33. [DOI] [PubMed] [Google Scholar]
- 21.Rund BR. Does active psychosis cause neurobiological pathology? A critical review of the neurotoxicity hypothesis. Psychol Med. 2014. Jun;44(8):1577–90. [DOI] [PubMed] [Google Scholar]
- 22.Haas GL, Sweeney JA. Premorbid and onset features of first-episode schizophrenia. Schizophr Bull. 1992;18(3):373–386. [DOI] [PubMed] [Google Scholar]
- 23.Morgan C, Abdul-Al R, Lappin JM, Jones P, Fearon P, Leese M, et al. Clinical and social determinants of duration of untreated psychosis in the AESOP first-episode psychosis study. Br J Psychiatry J Ment Sci. 2006. Nov;189:446–52. [DOI] [PubMed] [Google Scholar]
- 24.Verdoux H, Liraud F, Bergey C, Assens F, Abalan F, van Os J. Is the association between duration of untreated psychosis and outcome confounded? A two year follow-up study of first-admitted patients. Schizophr Res. 2001. Apr 30;49(3):231–41. [DOI] [PubMed] [Google Scholar]
- 25.Alvarez-Jimenez M, Gleeson JF, Henry LP, Harrigan SM, Harris MG, Amminger GP, et al. Prediction of a single psychotic episode: A 7.5-year, prospective study in first-episode psychosis. Schizophr Res. 2011. Feb 1;125(2):236–46. [DOI] [PubMed] [Google Scholar]
- 26.McGorry P, Keshavan M, Goldstone S, Amminger P, Allott K, Berk M, et al. Biomarkers and clinical staging in psychiatry. World Psychiatry. 2014. Oct 1;13(3):211–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bromet EJ, Schwartz JE, Fennig S, Geller L, Jandorf L, Kovasznay B, et al. The epidemiology of psychosis: the Suffolk County Mental Health Project. Schizophr Bull. 1992;18(2):243–255. [DOI] [PubMed] [Google Scholar]
- 28.Kotov R, Fochtmann L, Li K, Tanenberg-Karant M, Constantino EA, Rubinstein J, et al. Declining clinical course of psychotic disorders over the two decades following first hospitalization: evidence from the Suffolk County Mental Health Project. Am J Psychiatry. 2017;174(11):1064–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bromet EJ, Kotov R, Fochtmann LJ, Carlson GA, Tanenberg-Karant M, Ruggero C, et al. Diagnostic shifts during the decade following first admission for psychosis. Am J Psychiatry. 2011;168(11):1186–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.First MB, Spitzer RL, Gibbon M, Williams JB, others. Structured clinical interview for DSM-IV. N Y N Y State Psychiatr Inst. 1995; [DOI] [PubMed] [Google Scholar]
- 31.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992. Aug;49(8):624–9. [DOI] [PubMed] [Google Scholar]
- 32.Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull. 1982;8(3):470. [DOI] [PubMed] [Google Scholar]
- 33.Rabinowitz J, Levine SZ, Brill N, Bromet EJ. The premorbid adjustment scale structured interview (PAS-SI): preliminary findings. Schizophr Res. 2007;90(1–3):255–257. [DOI] [PubMed] [Google Scholar]
- 34.de Belmont Hollingshead A Four factor index of social status. Department of Sociology, Yale University; 1975. [Google Scholar]
- 35.Howe LD, Tilling K, Matijasevich A, Petherick ES, Santos AC, Fairley L, et al. Linear spline multilevel models for summarising childhood growth trajectories: a guide to their application using examples from five birth cohorts. Stat Methods Med Res. 2016;25(5):1854–1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goff DC, Zeng B, Ardekani BA, Diminich ED, Tang Y, Fan X, et al. Association of hippocampal atrophy with duration of untreated psychosis and molecular biomarkers during initial antipsychotic treatment of first-episode psychosis. JAMA Psychiatry [Internet]. 2018. Feb 21 [cited 2018 Feb 23]; Available from: https://jamanetwork-com.proxy.lib.uiowa.edu/journals/jamapsychiatry/fullarticle/2672208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McGlashan TH. Duration of untreated psychosis in first-episode schizophrenia: marker or determinant of course? Biol Psychiatry. 1999. Oct 1;46(7):899–907. [DOI] [PubMed] [Google Scholar]
- 38.Owens DC, Johnstone EC, Miller P, Macmillan JF, Crow TJ. Duration of untreated illness and outcome in schizophrenia: test of predictions in relation to relapse risk. Br J Psychiatry. 2010;196(4):296–301. [DOI] [PubMed] [Google Scholar]
- 39.Leucht S, Pitschel-Walz G, Abraham D, Kissling W. Efficacy and extrapyramidal side-effects of the new antipsychotics olanzapine, quetiapine, risperidone, and sertindole compared to conventional antipsychotics and placebo. A meta-analysis of randomized controlled trials. Schizophr Res. 1999. Jan 4;35(1):51–68. [DOI] [PubMed] [Google Scholar]
- 40.Robinson D, Woerner MG, Alvir JMJ, Geisler S, Koreen A, Sheitman B, et al. Predictors of treatment response from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry. 1999;156(4):544–549. [DOI] [PubMed] [Google Scholar]
- 41.Robinson D, Woerner MG, Alvir JMJ, Bilder R, Goldman R, Geisler S, et al. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry. 1999;56(3):241–247. [DOI] [PubMed] [Google Scholar]
- 42.De Hert M, Sermon J, Geerts P, Vansteelandt K, Peuskens J, Detraux J. The Use of Continuous Treatment Versus Placebo or Intermittent Treatment Strategies in Stabilized Patients with Schizophrenia: A Systematic Review and Meta-Analysis of Randomized Controlled Trials with First- and Second-Generation Antipsychotics. CNS Drugs. 2015. Aug;29(8):637–58. [DOI] [PubMed] [Google Scholar]
- 43.Craig TJ, Fennig S, Tanenberg-Karant M, Bromet EJ. Rapid versus delayed readmission in first-admission psychosis: quality indicators for managed care? Ann Clin Psychiatry. 2000;12(4):233–238. [DOI] [PubMed] [Google Scholar]
- 44.Mojtabai R, Herman D, Susser ES, Sohler N, Craig TJ, Lavelle J, et al. Service use and outcomes of first-admission patients with psychotic disorders in the Suffolk County Mental Health Project. Am J Psychiatry. 2005;162(7):1291–1298. [DOI] [PubMed] [Google Scholar]
- 45.Mojtabai R, Fochtmann L, Chang S-W, Kotov R, Craig TJ, Bromet E. Unmet need for mental health care in schizophrenia: an overview of literature and new data from a first-admission study. Schizophr Bull. 2009;35(4):679–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fennig S, Fennig S, Bromet E. Who provides the best retrospective information while assessing adult’s premorbid functioning? A methodological study in a first-admission sample with psychosis. Isr J Psychiatry Relat Sci. 1999;36(2):79–87. [PubMed] [Google Scholar]
- 47.Velthorst E, Fett A-KJ, Reichenberg A, Perlman G, van Os J, Bromet EJ, et al. The 20-year longitudinal trajectories of social functioning in individuals with psychotic disorders. Am J Psychiatry. 2016;174(11):1075–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Polari A, Lavoie S, Sarrasin P, Pellanda V, Cotton S, Conus P. Duration of untreated psychosis: a proposition regarding treatment definition. Early Interv Psychiatry. 2011;5(4):301–8. [DOI] [PubMed] [Google Scholar]
- 49.Johnstone EC, Crow TJ, Johnson AL, MacMillan JF. The Northwick Park study of first episodes of schizophrenia: I. Presentation of the illness and problems relating to admission. Br J Psychiatry. 1986;148(2):115–120. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


