Abstract
Objectives
This study aimed to identify the incidence of sudden cardiac death (SCD0 in adult patients under the age of 49 years, including adolescents with an out-of-hospital cardiac arrest that presented to the emergency department of a tertiary care hospital.
Methods
This retrospective cross-sectional study was conducted at the Royal Hospital, Muscat, Oman, between January 2015 and December 2019. All patients with out-of-hospital cardiac arrest were enrolled. The incidence of SCD was evaluated. Information about the patient’s demographic data, the site of cardiac arrest, the mode of arrival, the duration of pre-arrest symptoms and if cardiopulmonary resuscitation was performed was gathered. Survival data at 3-year follow-up was obtained.
Results
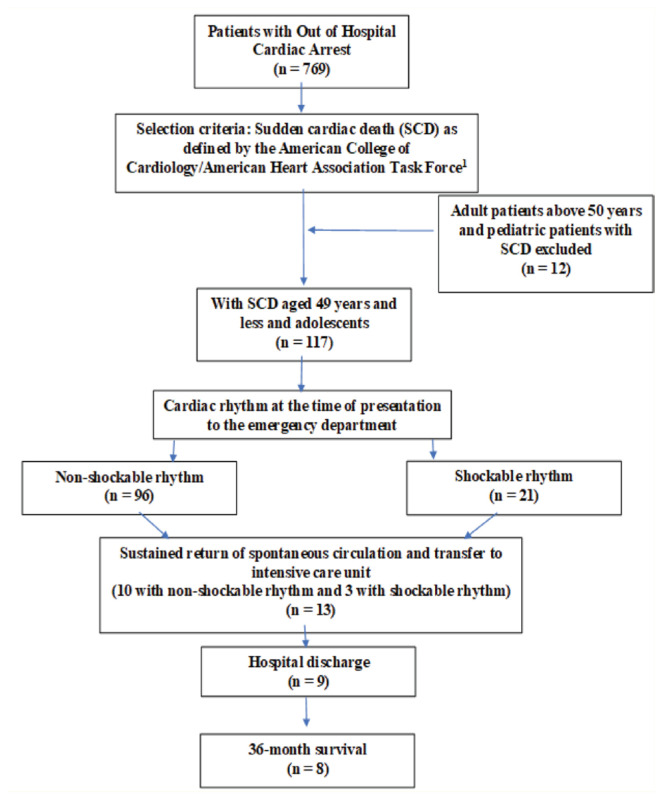
A total of 117 out of 769 (15%) patients met the criteria for SCD. Male gender was predominant, with a median age of 33 years. In about 79.5% of the patients, cardiac arrest was witnessed. Only 43 patients (36.8%) received cardiopulmonary resuscitation at the arrest site; 21 patients (17.9%) had a shockable rhythm and 96 patients (82.1%) had a non-shockable rhythm. Spontaneous circulation was returned in 15 patients (12.8%). Nine patients (7.7%) were discharged from the hospital and 8 (6.8%) survived at least 36 months.
Conclusion
The study findings indicate the prevalence of SCD among patients who experienced a cardiac arrest outside the hospital. Unfortunately, only a small number of patients were able to survive in the long term. By implementing preemptive screening for individuals and their families, it may be possible to prevent SCD and improve outcomes for those affected.
Keywords: Death, Sudden, Cardiac, Epidemiology, Etiology, Risk Factors, Incidence, Cardiopulmonary Resuscitation, Retrospective Studies, Oman
Advances in Knowledge
- The prevalence of sudden cardiac death among patients presenting to a tertiary care hospital in Oman with outside hospital cardiac arrest was determined.
Application to Patient Care
- There is a need to have a national registry and management protocol for patients with sudden cardiac death including family screening to prevent these catastrophic events.
Sudden cardiac death (scd) is a tragic event with serious implications for the patient’s family and the community. The American College of Cardiology/American Heart Association Task Force describes SCD as ‘sudden and unexpected death within an hour of the onset of symptoms, or occurring in patients found dead within 24 h of being asymptomatic and presumably due to a cardiac arrhythmia or hemodynamic catastrophe’.1 It accounts for approximately 25% of all cardiovascular deaths worldwide.2 The reported incidence of SCD in Europe varied between 36 to 128 per 100,000 deaths per year, and in the USA, the incidence reported was between 41 to 89 per 10,000 deaths per year.3,4 The incidence of SCD varies among different ethnic groups and regions. Concerning race, it was found that individuals of African-American descent appear to have higher rates of SCD and poorer outcomes than those of Caucasian or Hispanic descent. Furthermore, the incidence of SCD in individuals of Asian descent is lower than in other ethnic groups.5 The variation in the incidence rate of SCD may be due to differences in the reporting and surveillance methods.
The incidence of SCD in Oman is largely unknown. In Oman, there may be a significant incidence of SCD of unknown aetiology as an autopsy is not done for social and religious reasons. The primary objective of this study was to identify the incidence of SCD in patients with out-of-hospital cardiac arrest (OHCA) that presented to the emergency department of a tertiary care hospital in Muscat, Oman.
Methods
This retrospective cross-sectional study was conducted between January 2015 to December 2019 at the Royal Hospital, Muscat, Oman, after obtaining the institutional ethical committee approval (SRC#89/2019). The hospital electronic system (Al Shifa) provided clinical data for all enrolled patients presenting with OHCA in the emergency department. Those who met the SCD criteria described above were identified.1 Patients above 50, paediatric age group (<13 years of age), patients with witnessed pre-arrest symptoms that lasted above 60 mins and patients with unwitnessed pre-arrest symptoms that lasted more than 24 hours were excluded. The demographic data, including the age and gender of each patient, were recorded. The cardiac arrest site was identified in each patient who sustained an SCD. The month on the Gregorian calendar in which each cardiac arrest that met the criteria of SCD took place was recorded to evaluate any association of SCD with the seasons on the calendar. The time of the shift at which each patient diagnosed with SCD presented to the emergency department was obtained. The patients’ arrival mode to the emergency department and the duration of pre-arrest symptoms when available were noted. Information on whether emergency medical services performed cardiopulmonary resuscitation at the arrest site was obtained. The heart rhythm at the time of admission to the emergency department, the number of patients that had a return of spontaneous circulation, and the disposition of successfully resuscitated patients were obtained from the records. The number of patients discharged home and survival at ≥36 months was also recorded.
The data were analysed using Statistical Package for Social Science (SPSS) Version 23.0 (IBM Corp., Armonk, New York, USA). Bivariate and Chi-squared analyses were performed.
Results
A total of 769 patients suffered an OHCA during the study period. Of these, 117 (15%) patients met the criteria for SCD. The median age was 33 years. There were more male patients, 102 (87.2%) [Figure 1]. Most cardiac arrests occurred at home (43.6%) [Table 1]. The incidence of SCD in each year did not show any predilection to any specific time month [Table 2]. Over one-third of patients (n = 44, 37%) presented to the emergency department during the morning shift, 35% during the evening shift and 27.4% (32) during the night shift. In 93 patients (79.5%), cardiac arrest was witnessed. Family and friends brought 51 patients (46%), 47 patients (40%) arrived by ambulance services, and 19 (16.2%) by other means. A total of 37 patients (31.6%) with SCD had prearrest symptoms of less than 60 mins. There were no prearrest symptoms in 28 patients (23.9%) and the incidence of prearrest symptoms could not be ascertained in 52 patients (44.4%). At the scene of cardiac arrest, 43 out of the 117 patients (37%) received cardiopulmonary resuscitation (CPR), but only 38 out of 117 (32%) were revived by emergency medical services (EMS); 96 patients (82.1%) presented with an unshockable heart rhythm [Table 2]. In the 21 patients (17.9%) with shockable rhythm in the emergency department, spontaneous circulation could be returned in 15 patients (12.8%). Despite an initial return of spontaneous circulation, 2 patients failed to sustain the circulation (one each with un-shockable and shockable rhythms). Thirteen patients (11%; 10 who had non-shockable rhythm and 3 with shockable rhythm) who were shifted to the intensive care unit for further management. Only 3 out of the 13 patients who experienced a return of spontaneous circulation underwent cardiac catheterization. Overall, there was no risk factor in 19 out of the 117 patients (16.2%), while in 54 patients (46.2%), no risk factor could be identified. Of those, two required stenting due to atherosclerosis. Of the 13 initial survivors, only 9 patients (7.7%) survived hospital discharge. There were 3 patients with neurological deficits, two of whom had minor injuries and one of whom had a severe hypoxic-ischaemic injury. Long-term survival, defined as survival ≥36 months, was possible in 8 patients (6.8%) discharged home.
Figure 1.
Patient flow chart.
Table 1.
Frequency percentage distribution of demographic variables among the patients with sudden cardiac death (N = 117)
| Demographic variables | n (%) |
|---|---|
| Age group | |
| Adults ≤49 years old including adolescents | 117 (100) |
| Nationality | |
| Omani | 67 (57.3) |
| Non-Omani | 50 (42.7) |
| Sex | |
| Male | 102 (87.2) |
| Female | 15 (12.8) |
| Geographic Region | |
| Muscat | 95 (81.2) |
| South Batinah | 6 (5.1) |
| North Batinah | 6 (5.1) |
| South Sharqiyah | 4 (3.4) |
| North Sharqiyah | 3 (2.6) |
| Al Dakhiliyah | 3 (2.6) |
| Site of cardiac arrest | |
| Home | 51 (43.6) |
| Emergency department | 12 (10.3) |
| Health center, private clinic, polyclinic | 14 (12.0) |
| Others | 40 (34.2) |
Table 2.
Sudden cardiac death distribution based on Gregorian calendar, gender and the type of rhythm at presentation (shockable vs. non-shockable) between January 2015 and December 2019 (N = 117)
| Variable | n (%) | ||
|---|---|---|---|
| Patients with SCD (n = 117) | Male (n = 102) | Female (n = 15) | |
| Month | |||
| January | 4 (3.4) | 3 (75) | 1 (25) |
| February | 6 (5.1) | 5 (83.3) | 1 (16.7) |
| March | 12 (10.3) | 11 (91.7) | 1 (8.3) |
| April | 6 (5.1) | 6 (100) | 0 |
| May | 12 (10.3) | 11 (91.7) | 1(8.3) |
| June | 15 (12.8) | 13 (86.7) | 2 (13.3) |
| July | 12 (10.3) | 11 (91.7) | 1(8.3) |
| August | 2 (1.7) | 2 (100) | 0 |
| September | 12 (10.3) | 10 (8.3) | 2 (16.7) |
| October | 14 (12.0) | 13 (92.9) | 1 (7.1) |
| November | 11 (9.4) | 8 (72.7) | 3 (27.3) |
| December | 11 (9.4) | 9 (81.8) | 2 (18.2) |
| Year | |||
| 2015 | 18 (15.4) | 17 (94.4) | 1 (5.6) |
| 2016 | 21 (17.9) | 16 (76.2) | 5 (28.8) |
| 2017 | 30 (25.6) | 27 (90) | 3 (10) |
| 2018 | 22 (18.8) | 21 (95.5) | 1 (4.5) |
| 2019 | 26 (22.2) | 21 (80.8) | 5 (19.2) |
| Type of rhythm at presentation | |||
| Patients with non-shockable rhythm | 96 (82.1) | ||
| Male = 82, Female = 14 | |||
| Patients with a shockable rhythm received cardioversion. | 21 (17.9) | ||
| Male = 20, Female = 1 | |||
| Sustained return of spontaneous circulation established | 13 (11) | ||
| 10 with non-shockable rhythm and 3 with shockable rhythm | |||
| Disposition from the emergency department | Intensive care unit = 13 (11.1) | ||
| Mortality in emergency department = 104 (88.9) | |||
| Hospital discharge | 9 (7.7) | ||
| Long-term survival (at ≥36 months) | 8 (6.8) | ||
Discussion
The current single-centre study provided information about the incidence of SCD in out-of-hospital cardiac arrest patients admitted to an emergency department in a tertiary care hospital. About 15% of patients (n = 117) out of 769 patients with outside hospital cardiac arrest could be categorised as patients with SCD during a 4-year period. The patients were from a nearby geographic area to the tertiary care hospital where the study was conducted. In many patients with SCD, the aetiology was unknown and it was impossible to identify the cause as an autopsy was not performed. The proportion of patients with aborted SCD who survived long-term was very small (6.8%). This study suggests that preemptive routine screening of young individuals, specifically patients and close relatives of patients where the possibility of SCD is suspected, may go a long way in preventing and managing individuals at risk. This process may significantly impact society, as the loss of a young person can have catastrophic consequences for their family and community.
A retrospective study conducted in Oman reported that between the years 2012 to 2016, 216 patients presented to the emergency department with out-of-hospital cardiac arrest. History of chest pain was reported in 22% of those patients, and the rest presented after a collapse; 63 patients underwent coronary angiography and coronary artery stenting was performed in 28 patients. In the remaining 35 patients, the cause of cardiac arrest could not be ascertained.6 Bowker et al. suggested that acute coronary thrombosis accounts for 59–86% of SCD cases.7 In this study, of the 117 patients with SCD, the cardiovascular system was identified as the risk factor in 15 patients (12.8%). Three of the 13 patients with return of spontaneous circulation underwent cardiac catheterisation; two of them had evidence of atherosclerosis.
Premature atherosclerotic coronary artery disease is becoming a major health burden worldwide. A recent study of 1,130 male patients who succumbed to acute coronary deaths suggested that the term be applied to all males who suffer from acute myocardial infarction below the age of 49 years.8 In Oman, the incidence of premature coronary artery disease is not well documented. Al-Waili et al reported that 22% of patients with familial hyperlipidemia have premature coronary artery disease. It was highlighted that there was a significant gap in the diagnosis of familial hyperlipidemia. The estimated prevalence of familial hyperlipidemia in Oman is around 28,000 patients.9 This implies that there might be a significant failure to recognize this disease, which is a major contributor of premature coronary artery disease and SCD.
Non-atherosclerotic coronary artery disease accounts for approximately 3% of all SCDs.10 This disease spectrum includes, congenital anomalies involving the origin or the course of the major epicardial coronary arteries, coronary artery dissections, coronary artery vasculitis, coronary spasm, myocardial bridging of mainly the left anterior descending coronary artery and fibromuscular dysplasia. The risk of SCD appears to be the greatest in patients with anomalous aortic origin of a coronary artery. Case reports were published regarding these entities from Oman.11,12 There is a familial clustering of cardiac diseases in approximately 20% of patients with these anomalies a genetic testing may prove informative.13
Cardiomyopathies are a diverse group of disorders characterised by structural and functional heart muscle abnormalities that may result in SCD.14,15 There are various familial and genetic types of cardiomyopathies, including hypertrophic cardiomyopathy, arrhyth-mogenic right ventricular cardiomyopathy, dilated cardiomyopathy, etc. A previous study from Oman reported the incidence of cardiomyopathy to be around 43.2 per 100,000 population.16 Due to the high prevalence of consanguineous marriages in Oman, which ranges from 20–30%, one may expect the genetic component of this disease to be higher than that reported globally.17 Hence, the likelihood of diagnosing these inherited cardiomyopathies leading to SCD may be significant and desirable.
Cardiac ion channelopathies are important causes of SCD, accounting for 5–10% of total cardiac deaths.18,19 To the best of the authors’ knowledge, the prevalence of channelopathies in the Gulf countries is unknown. However, several publications from Oman regarding channelopathies highlighted the prevalence and management strategies available in the country.20,21 These reports suggest that cardiovascular etiologies may contribute to many of the SCD cases. The authors hope that the current study may provide an impetus for focused studies investigating the causes and inheritance pattern of cardiovascular etiologies especially premature atherosclerotic coronary artery disease, cardiomyopathies and channelopathies, which ultimately will influence the management, family screening, including genetic counseling.
In this study, 37% of the patients received an initial cardiopulmonary resuscitation immediately after the cardiac arrest in the current study. This was comparable to the percentage of patients who received cardiopulmonary resuscitation after an OHCA, as reported by the Resuscitation Outcomes Consortium in the American Heart Association report.22 The current study reported a shockable rhythm in 21 out of 117 patients (17.9%) compared to >30% reported by the Resuscitation Outcomes Consortium.22 The Resuscitation Outcomes Consortium, in the report from the American Heart Association, also mentioned that more than 30% of patients survived if the first rhythm was shockable.22 In the current study, only 3 out of 21 patients (14.2%) who presented with an initial shockable rhythm had sustained return of spontaneous circulation. The Resuscitation Outcomes Consortium reported that survival to hospital discharge was about 10% compared to 7.8% in the current study.22 All these data suggest that there is scope for further improvement in managing patients with SCD in Oman.
The limitations of this retrospective cross-sectional study were: (1) There was a lack of accurate documentation in the electronic records. This may be due to the absence of a dedicated entry sheet for SCD or OHCA. The data collection for our study was done retrospectively using the hospital’s electronic documentation system. Unfortunately, no clear guidelines were in place for documenting SCD, resulting in various relevant data not being recorded. Only 117 out of a total of 679 patients with OHCA were identified as meeting our SCD criteria, and it is possible that many patients who may have met SCD criteria were missed; (2) the exact cause of SCD could not be ascertained as an autopsy was not performed; and (3) another limitation of the study was the possibility that patients reported as living in Muscat may not actually be from the Muscat region but from another region or country. This consideration is particularly important when studying the genetics of SCD. The demographic information was gathered from hospital electronic records, which is based on the information provided in the subjects’ civil identification cards. This can introduce bias, which should be considered in future prospective studies.
Conclusion
This study showed that SCD is underreported due to inadequate documentation. Residence of the patients was the most frequent site where the SCD occurred, and on-site cardiopulmonary resuscitation was possible in a few patients, highlighting the importance of educating the general public on the nuisances of basic life support. The battle against SCD is not easy. To establish the aetiology of SCD, molecular autopsy, genetic analysis, and post-mortem imaging may be needed. There is an urgent need to create a national registry of SCD to help identify the incidence accurately and obtain knowledge of this critical issue in the country. The registry may aid in creating policies to address the issue of SCD. It may help arrive at a systematic protocol for managing all cases of SCD along with a comprehensive algorithm for a timely and cost-effective screening of family members. All these measures may aid in managing and possibly preventing SCD in young individuals.
Footnotes
AUTHORS’ CONTRIBUTION: MMM and HNAK did the manuscript writing. ASAH and MJAD were involved in the data collection. SKJ analysed the data. HMAL was responsible for the project idea and data interpretation. All authors approved the final version of the manuscript.
CONFLICT OF INTEREST: The authors declare no conflicts of interest.
FUNDING: No funding was received for this study.
References
- 1.Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2018;72:e91–220. doi: 10.1016/j.jacc.2017.10.054. [DOI] [PubMed] [Google Scholar]
- 2.Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. 2015 ESC Guidelines for the Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. Rev Esp Cardiol (Engl Ed) 2016;69:176. doi: 10.1016/j.rec.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 3.Priori SG, Aliot E, Blomstrom-Lundqvist C, Bossaert L, Breithardt G, Brugada P, et al. European Society of Cardiology. Update of the guidelines on sudden cardiac death of the European Society of Cardiology. Eur Heart J. 2003;24:13–15. doi: 10.1016/s0195-0668x(02)00809-6. [DOI] [PubMed] [Google Scholar]
- 4.Deo R, Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation. 2012;125:620–37. doi: 10.1161/CIRCULATIONAHA.111.023838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hayashi M, Shimizu W, Albert CM. The spectrum of epidemiology underlying sudden cardiac death. Circ Res. 2015;116:1887–906. doi: 10.1161/CIRCRESAHA.116.304521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nadar SK, Mujtaba M, Al-Hadi H, Sadiq M, Al-Riyami A, Ali M, et al. Epidemiology, Outcomes and Coronary Angiography Findings of Patients Following Out-of-Hospital Cardiac Arrest: A single-centre experience from Oman. Sultan Qaboos Univ Med J. 2018;18:e155–60. doi: 10.18295/squmj.2018.18.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bowker TJ, Wood DA, Davies MJ, Sheppard MN, Cary NR, Burton JD, Chambers DR, et al. Sudden, unexpected cardiac or unexplained death in England: a national survey. QJM. 2003;96:269–79. doi: 10.1093/qjmed/hcg038. [DOI] [PubMed] [Google Scholar]
- 8.Abderrahman HA, Al-Abdallat IM, Idhair AK. Age threshold for proper definition of premature coronary artery disease in males. J Forensic Leg Med. 2018;58:45–9. doi: 10.1016/j.jflm.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 9.Al-Waili K, Al-Rasadi K, Zadjali F, Al-Hashmi K, Al-Mukhaini S, Al-Kindi M, et al. Clinical and Genetic Characteristics of Familial Hypercholesterolemia at Sultan Qaboos University Hospital in Oman. Oman Med J. 2020;35:e141. doi: 10.5001/omj.2020.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hill SF, Sheppard MN. Non-atherosclerotic coronary artery disease associated with sudden cardiac death. Heart. 2010;96:1119–25. doi: 10.1136/hrt.2009.185157. [DOI] [PubMed] [Google Scholar]
- 11.Al Kindi HN, Yacoub MH. Transection and Relocation of Anomalous Left Coronary Artery After Aborted Sudden Cardiac Death. Ann Thorac Surg. 2019;108:e25–8. doi: 10.1016/j.athoracsur.2018.11.037. [DOI] [PubMed] [Google Scholar]
- 12.Maddali MM, Al-Abri IA, Waje ND, Arora NR, Chase D, Kandachar PS, Valliattu J. Near-Death Episode in a Young Adult. J Cardiothorac Vasc Anesth. 2017;31:1401–6. doi: 10.1053/j.jvca.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Agrawal H, Mery CM, Sexson Tejtel SK, Fraser CD, McKenzie ED, Qureshi AM, et al. Familial clustering of cardiac conditions in patients with anomalous aortic origin of a coronary artery and myocardial bridges. Cardiol Young. 2018;28:1099–105. doi: 10.1017/S1047951118000835. [DOI] [PubMed] [Google Scholar]
- 14.Behr ER, Dalageorgou C, Christiansen M, Syrris P, Hughes S, Tome Esteban MT, et al. Sudden arrhythmic death syndrome: familial evaluation identifies inheritable heart disease in the majority of families. Eur Heart J. 2008;29:1670–80. doi: 10.1093/eurheartj/ehn219. [DOI] [PubMed] [Google Scholar]
- 15.Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, et al. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29:270–6. doi: 10.1093/eurheartj/ehm342. [DOI] [PubMed] [Google Scholar]
- 16.Agarwal AK, Venugopalan P, Meharali AK, de Debono D. Idiopathic dilated cardiomyopathy in an Omani population of the Arabian Peninsula: prevalence, clinical profile and natural history. Int J Cardiol. 2000;75:147–58. doi: 10.1016/s0167-5273(00)00315-6. [DOI] [PubMed] [Google Scholar]
- 17.Rajab A, Al Rashdi I, Al Salmi Q. Genetic services and testing in the Sultanate of Oman. Sultanate of Oman steps into modern genetics. J Community Genet. 2013;4:391–7. doi: 10.1007/s12687-013-0153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chugh SS, Kelly KL, Titus JL. Sudden cardiac death with apparently normal heart. Circulation. 2000;102:649–54. doi: 10.1161/01.cir.102.6.649. [DOI] [PubMed] [Google Scholar]
- 19.Drory Y, Turetz Y, Hiss Y, Lev B, Fisman EZ, Pines A, Kramer MR. Sudden unexpected death in persons less than 40 years of age. Am J Cardiol. 1991;68:1388–92. doi: 10.1016/0002-9149(91)90251-f. [DOI] [PubMed] [Google Scholar]
- 20.Maddali MM, Thomas E, Al Abri IA, Patel MH, Al Maskari SN, Al Yamani MI. Dilated Cardiomyopathy Phenotype-Associated Left Ventricular Noncompaction and Congenital Long QT Syndrome Type-2 in Infants With KCNH2 Gene Mutation: Anesthetic Considerations. J Cardiothorac Vasc Anesth. 2022;36:3662–7. doi: 10.1053/j.jvca.2022.05.016. [DOI] [PubMed] [Google Scholar]
- 21.Maddali MM, Kandachar PS, Al-Abri IA, Al-Yamani MI. Diagnostic lacunae and implications of an automated implantable cardioverter defibrillator implantation in a child with type 3 Long QT (LQT3) syndrome. Ann Card Anaesth. 2022;25:210–13. doi: 10.4103/aca.aca_13_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation. 2022;145:e153–639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]