Abstract
Introduction:
Singapore instituted lockdown measures from 7 February 2020 to 1 June 2020 in response to the coronavirus disease 2019 (COVID-19) pandemic.
Methods:
A retrospective analysis of cases from the national trauma registry was carried out comparing the lockdown period (from 7 February 2020 to 1 June 2020) to the pre-lockdown period (from 7 February 2019 to 1 June 2019). Data extracted included the volume of Tier 1 (injury severity score [ISS] >15) and Tier 2 (ISS 9–15) cases and epidemiology. Subgroup analysis was performed for Tier 1 patient outcomes.
Results:
Trauma volume decreased by 19.5%, with a 32% drop in Tier 1 cases. Road traffic and workplace accidents decreased by 50% (P < 0.01), while interpersonal violence showed an increase of 37.5% (P = 0.34). There was an 18.1% decrease in usage of trauma workflows (P = 0.01), with an increase in time to intervention for Tier 1 patients from 88 to 124 min (P = 0.22). Discharge to community facilities decreased from 31.4% to 17.1% (P < 0.05). There was no increase in inpatient mortality, length of stay in critical care or length of stay overall.
Conclusion:
There was an overall decrease in major trauma cases during the lockdown period, particularly road traffic accidents and worksite injuries, and a relative increase in interpersonal violence. Redeployment of manpower and hospital resources may have contributed to decreased usage of trauma workflows and community facilities. In the event of further lockdowns, it is necessary to plan for trauma coverage and maintain the use of workflows to facilitate early intervention.
Keywords: COVID-19, trauma surgery, trauma volume, trauma workload
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (coronavirus disease 2019 [COVID-19]) was first identified in December 2019 in Wuhan, China.[1] The first case of COVID-19 was reported in Singapore on 23 January 2020,[2] and subsequent increase in community transmission led the Singapore Ministry of Health to declare a progressive lockdown and closure of non-essential services from 7 February 2020 to reduce public movements and interactions.[3,4] The lockdown was lifted on 2 June 2020 with gradual reopening of schools and other public areas.[5]
Khoo Teck Puat Hospital (KTPH) is an acute restructured hospital and a top regional trauma centre that receives the second highest volume of Tier 1 or injury severity score (ISS) >15 trauma patients nationwide. The majority of trauma patients present after blunt trauma from road traffic accidents or falls from height. The hospital’s trauma activation protocols consist of a first-line trauma activation that is initiated on presentation for patients who have suspected multisystem polytrauma or high-speed injury, and a second-line trauma activation protocol initiated for patients who are haemodynamically unstable and mandate immediate attention by consultant specialists for intervention.[6]
There is limited information available on the impact of widespread community lockdown on the volume of trauma cases seen in public hospitals, as well as the patterns and trends of injury that may be seen during a lockdown. There is also no previous literature on the clinical outcomes of major trauma patients undergoing treatment during a pandemic. This study aimed to describe the impact of community lockdown on the volume and injury patterns of major trauma cases in a single regional hospital in Singapore.
METHODS
Data was extracted from the Singapore national trauma registry, which is maintained and prospectively collected by the Department of General Surgery, KTPH. The periods under study were from 7 February 2020 to 1 June 2020 (lockdown group) versus the month-matched historical cohort from 7 February 2019 to 1 June 2019 (pre-lockdown group). All Tier 1 (ISS >15) and Tier 2 (ISS 9–15) trauma patients who presented to KTPH during this period were included. There were no missing records.
The data extracted included the volume of trauma cases, epidemiological data, mechanism of injury, and outcomes such as activation of first- or second-line trauma protocols, time taken to intervention, length of hospital stay, length of critical care stay, mortality and discharge facility. The study was approved by the institutional research board (reference no. 2020/00567). Analysis of these outcomes was performed with Pearson’s chi-square test and Student’s t-test where appropriate. A P value < 0.05 was considered as statistically significant.
RESULTS
Table 1 shows a comparison of demographics and injury pattern of Tier 1 and Tier 2 trauma patients between the pre-lockdown and lockdown groups. There were 349 patients in the pre-lockdown group and 281 in the lockdown group, with a 19.5% decrease in the overall caseload. There was a more pronounced drop of 32% in Tier 1 trauma cases from 122 to 83 cases. There was a 12.8% decrease in Tier 2 trauma cases from 227 to 183 cases. The month-to-month comparisons are shown in Figures 1 and 2. There were no large gender differences between the pre-lockdown and lockdown groups.
Table 1.
Epidemiology of Tier 1 and Tier 2 trauma patients.
| Variable | n | Change (%) | P | ||
|---|---|---|---|---|---|
|
| |||||
| Total | Pre-lockdown | Lockdown | |||
| Overall | 630 | 349 | 281 | –19.5 | – |
|
| |||||
| Severity | |||||
|
| |||||
| Tier 2 (ISS 9–15) | 425 | 227 | 198 | –12.8 | 0.17 |
|
| |||||
| Tier 1 (ISS >15) | 205 | 122 | 83 | –32.0 | |
|
| |||||
| Gender | |||||
|
| |||||
| Male | 351 | 202 | 149 | –26.2 | 0.25 |
|
| |||||
| Female | 279 | 147 | 132 | –10.2 | |
|
| |||||
| Age range (yr) | |||||
|
| |||||
| 16–64 | 248 | 147 | 101 | –31.3 | 0.13 |
|
| |||||
| ≥ 65 | 382 | 202 | 180 | –10.9 | |
|
| |||||
| Injury mechanism | |||||
|
| |||||
| Fall | 450 | 233 | 217 | –6.9 | <0.01* |
|
| |||||
| Same level fall ≤0.5 m | 416 | 214 | 202 | –5.6 | <0.01* |
|
| |||||
| Fall from height >0.5 m | 34 | 19 | 15 | –21.1 | 0.95 |
|
| |||||
| Vehicular accident | 138 | 92 | 46 | –50.0 | <0.01* |
|
| |||||
| Pedal cyclist/PMD | 29 | 20 | 9 | –55.0 | 0.19 |
|
| |||||
| Motor car driver/passenger | 12 | 10 | 2 | –80.0 | 0.08 |
|
| |||||
| Motorcycle rider/pillion | 79 | 50 | 29 | –42.0 | 0.16 |
|
| |||||
| Pedestrian | 18 | 12 | 6 | –50.0 | 0.46 |
|
| |||||
| Interpersonal violence | 19 | 8 | 11 | +37.5 | 0.34 |
|
| |||||
| Tools/Objects/Machinery | 12 | 8 | 4 | –50.0 | 0.56 |
|
| |||||
| Othersa | 11 | 8 | 3 | –62.5 | 0.36 |
|
| |||||
| Place of injury | |||||
|
| |||||
| Home/Residential institutions | 342 | 177 | 165 | –6.8 | 0.054 |
|
| |||||
| Road | 139 | 86 | 53 | –38.4 | 0.10 |
|
| |||||
| Public places | 116 | 65 | 51 | –21.5 | 0.96 |
|
| |||||
| Workplace | 29 | 17 | 12 | –29.4 | 0.87 |
|
| |||||
| Unknown | 4 | 4 | 0 | –100.0 | 0.13 |
aOther mechanisms of injury include sports injury, asphyxiation by hanging and charcoal burning. *Statistically significant. ISS: injury severity score, PMD: personal mobility device
Figure 1.
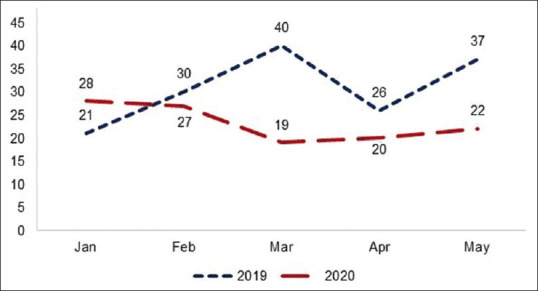
Graph shows the number of Tier 1 cases in 2019 and 2020.
Figure 2.
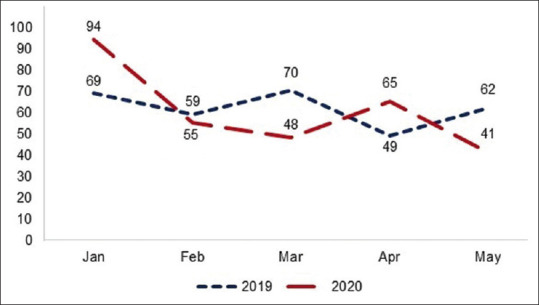
Graph shows the number of Tier 2 cases in 2019 and 2020.
The proportion of patients presenting with road traffic accidents and workplace accidents showed the largest decrease (50% decrease, P<0.01) during the lockdown period across all types of vehicles. The only mechanism of injury that showed an increase was interpersonal violence, which saw a non-significant increase by 37.5% (P = 0.34) from eight cases pre-lockdown to 11 cases during lockdown. Trauma that occurred on the road, public places and the workplace decreased by 38.4%, 21.5% and 29.4%, respectively. There was minimal change in the number of trauma cases that occurred in the household.
Subgroup analysis of patient outcomes for Tier 1 trauma cases is presented in Table 2. Audit of usage of trauma workflows showed that there was a significantly reduced use of first-line trauma activation protocol, from 43.4% pre-lockdown to 25.3% during lockdown, and a non-significant reduction in use of second-line trauma activation protocol, from 9.0% pre-lockdown to 2.4% during lockdown. There was a corresponding increase in time taken to intervention from a pre-lockdown average of 88 min to 124 min during lockdown; however, this was not statistically significant (P = 0.22).
Table 2.
Outcomes of Tier 1 cases.
| Outcome | n (%)/mean±SD | P | |
|---|---|---|---|
|
| |||
| Pre-lockdown (n=122) | Lockdown (n=83) | ||
| First-line trauma activation | 53 (43.4) | 21 (25.3) | 0.01* |
|
| |||
| Second-line trauma activation | 11 (9.0) | 2 (2.4) | 0.08 |
|
| |||
| Time to intervention (min) | 88±45 (n=10) | 124±62 (n=5) | 0.22 |
|
| |||
| Length of hospital staya (day) | 17.2±29.2 | 11.1±14.4 | 0.06 |
|
| |||
| Length of stay in HD/ICU (day) | 5.7±7.4 (n=58) | 3.5±3.3 (n=24) | 0.07 |
|
| |||
| Mortality | 14 (11.5) | 6 (7.2) | 0.44 |
|
| |||
| Discharge dispositiona | n=121 | n=82 | |
|
| |||
| Home | 56 (46.3) | 50 (61.0) | 0.04* |
|
| |||
| Other acute hospital | 3 (2.5) | 2 (2.4) | 1.00 |
|
| |||
| Community hospital/nursing home | 38 (31.4) | 14 (17.1) | 0.03* |
|
| |||
| Cost of hospitalisationa (SGD) | 18,620±31,671 | 7,831±12,013 | 0.01* |
aTwo patients pending discharge from hospital at the point of data extraction. *Statistically significant. HD: high-dependency unit, ICU: intensive care unit, SD: standard deviation, SGD: Singapore dollar
There was no significant difference in mortality between pre-lockdown and during lockdown (11.5% vs. 7.2%, P = 0.44). The number of days that patients spent in critical care pre-lockdown and during lockdown (5.7 vs. 3.5 days) was also not statistically significant. There was no significant difference in length of stay for patients in pre-lockdown and lockdown periods; however, at the point of data extraction (30 days post-lockdown), there were two patients who remained in the general ward pending discharge, one from either period under assessment. This factor might also have had implications on the total cost of hospitalisation.
Breakdown of discharge facility disposition for those patients who had been discharged from hospital showed that there was a significantly larger proportion of patients who were discharged to their own homes (46.3% pre-lockdown vs. 61.0% during lockdown, P < 0.05) and a significantly lower proportion of patients who were discharged to step-down community facilities or nursing homes (31.4% pre-lockdown vs. 17.1% during lockdown, P < 0.05).
DISCUSSION
The substantial decrease in overall major trauma admissions in Singapore was congruent with the epidemiological statistics of other countries that had gone through a similar lockdown phase due to the COVID-19 pandemic. Christey et al.[7] reported an overall drop of 43% for all injury-related admissions in a Level I trauma centre in New Zealand, while Forrester et al.[8] reported a 4.8-fold drop in trauma activations in two Level I trauma centres in Santa Clara County, California, USA. Yang and Fu[9] reported a 39.2% reduction in major trauma patients presenting to Level I trauma centres in Hangzhou, China. The downtrend in rates of traffic-related and workplace trauma can be attributed to the direct effects of the nationwide lockdown decreasing traffic flow[10] and the closure of work sites. While the decrease in traffic volume seems promising, there were concerns raised by the UK Metropolitan Police that reduced volume of traffic might lead to a paradoxical increase in number of speeding vehicles.[11] This was aligned with the local context. Figures from the Singapore Traffic Police showed that in May 2020, the average road trips had fallen from 201 million to 80.4 million per month after the introduction of lockdown measures, while the percentage of speeding violations had risen from 75 to 187 violations per million trips.[12]
The rise in interpersonal violence has also been reported in other articles such as the aptly named Trauma Does Not Quarantine by Hatchimonji et al.[13] While it is not within the scope of this paper to elucidate the cause of the increase, other countries have also seen records of increased partner violence[14] as well as increasing trends of self-harm[15,16] during the period of enforced social isolation, corresponding to an overall increase in anxiety and depression in the general public.[17]
The decrease in use of first- and second-line trauma activation protocols was audited by an interdepartmental trauma committee, and some of the common factors involved included an increased workload presenting to the emergency department (ED), particularly those with acute respiratory infections (ARI).[18] This was particularly prominent in the early pandemic period, when COVID-19 testing was not widely available to primary care practitioners. There was also widespread redeployment of physicians from other departments to ED, often at short notice and with an abbreviated introduction, if any, to trauma protocols and workflows. The overall increase in workload and the need to segregate staff in case of COVID-19 exposure may have contributed to less supervision of junior staff in both ED and surgical teams. The additional psychological burden of working on the frontline of a pandemic with ARI patients may also have taken a toll on even veteran staff, in the form of anxiety, depression and other adverse psychological responses culminating in physician burnout and reducing individual efficiency.[19]
The effect of decreased workflow use was most significant in Tier 1 polytrauma patients, who can be at risk of (a) undertriaging of the mechanism of injury and failure to activate trauma protocols, (b) missing significant injuries, especially in obtunded patients, and (c) delay in review by overstretched medical staff and delay in intervention within the ‘golden hour’ before clinical deterioration. The immediate effects of this can be seen in the increase in time to intervention, which was almost doubled in this study, although the effect was not statistically significant due to small patient numbers.
The downstream outcomes of length of stay, duration of stay in critical care units, mortality and cost of hospitalisation in the lockdown period showed no significant change compared to the pre-lockdown period, although the utilisation of community hospitals as facilities for step-down rehabilitation decreased. This can be attributed to community hospital facilities within the institute being converted to wards for COVID-19 patients, as well as limitation in transfer to external rehabilitation facilities due to nationwide restrictions in cross-institute transfer of patients. Possible measure that may have contributed to maintaining an equivalent length of inpatient stay was the presence of a discharge team actively linking up patients with community-based outpatient rehabilitation programmes, although the outcomes of rehabilitation after those alternative programmes have not yet been studied.
At the time of this study, the future of the COVID-19 pandemic was fluid, with some countries reinstituting lockdowns due to the much-dreaded second wave previously forecasted.[20] It may not be possible for Singapore, a population-dense and globally connected country, to avoid this phenomenon altogether, despite aggressive contact tracing, stringent home quarantine for travellers and other public health measures. Forward planning in the event of further lockdown should utilise data from previous trends to project the needs of the future. The capacity to maintain high-standard care despite resource scarcity in a pandemic is essential for acute surgical conditions and even more so for trauma, where timely intervention is counted in minutes rather than hours.
The guidelines for trauma care during the pandemic have been consolidated in the European Society of Trauma and Emergency Surgery recommendations.[21] Drawing from this paper, the key tenets particularly pertinent to the issues raised above are as follows: (a) care should be taken to maintain the quality of interventions and limit delay of interventions while considering COVID-19 guidelines, and (b) the shift of staff due to necessary redeployment should not have a negative impact on the ability to provide timely care for trauma and emergency surgery patients.
The ability to continue to provide quality care and appropriate intervention hangs on the presence and utilisation of robust institutional workflows. This can be reinforced by departments planning early for a second lockdown by earmarking a number of staff to be redeployed, with early debriefing and dissemination of preparatory materials. This can be performed via intranet electronic resources and virtual meetings rather than physical gatherings. On a larger scale, the utilisation of primary healthcare providers to attend to ARI and COVID-19 testing may also offload a surge in cases presenting to ED.
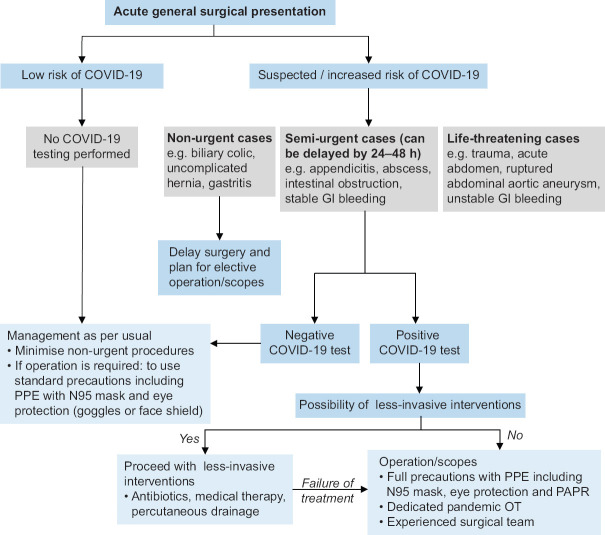
The same vehicles for information can be used within the general surgery department to familiarise staff with trauma processes and reinforce usage of workflows, as well as raise awareness of possible pitfalls and lapses that may occur during the initial redeployment of staff. This would form a ‘safety net’ to reduce the chance of adverse outcomes. The use of COVID-19 guidelines should also be disseminated widely. Figure 3 provides guidance for the management of acute surgical conditions and trauma in patients with suspected COVID-19 within the local context, which takes into account community prevalence of COVID-19 infection, availability of resources and national guidelines for COVID-19 screening. It clearly defines that intervention should be based on the acuity of clinical need, so that provision of high-quality trauma care may be maintained while ensuring judicious use of resources.
Figure 3.
Chart shows the workflow for patients presenting with acute general surgical conditions and trauma during COVID-19 at Khoo Teck Puat Hospital. GI: gastrointestinal, OT: operating theatre, PAPR: powered air-purifying respirator, PPE: personal protective equipment
Public health measures that might contribute to further primary prevention of trauma in the community include further reinforcement of speed limits during and after pandemic lockdowns to stem a surge in high-velocity accidents. Addressing the mental health of the general public and increasing outreach to vulnerable groups are issues that have been raised in other countries, such as having telehealth visits focusing on domestic violence by primary care providers in Australia,[22] as well as development of remote assessment and care pathways for patients at risk of self-harm.[23]
In conclusion, the COVID-19 lockdown period showed a decrease in major trauma admissions and a change in injury trends. There should be adequate pandemic preparedness planning locally in the event of a second wave of lockdowns, which should highlight that there is still a substantial need for the provision of full trauma services within hospitals, unless resource limitations make it unavoidable. The need to reinforce and maintain workflows for major trauma patients is key to maintaining high standards of treatment. There should be increased awareness of mental health within the community of healthcare workers, as well as outreach to the general public during these troubling times to maintain a positive narrative.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ministry of Health, Singapore. Confirmed imported case of novel coronavirus infection in Singapore; multi-ministry taskforce ramps up precautionary measures. [[Last accessed 2021 Sep 28]]. Available from: https://www.moh.gov.sg/news-highlights/details/confirmed-imported-case-of-novelcoronavirus-infection-in-singapore-multi-ministry-taskforce-ramps-upprecautionary-measures .
- 3.Ministry of Health, Singapore. Risk assessment raised to DORSCON Orange. [[Last accessed on 2021 Sep 28]]. Available from: https://www.moh.gov.sg/news-highlights/details/risk-assessment-raised-to-dorscon-orange .
- 4.Ministry of Health, Singapore. Circuit Breaker to minimise further spread of COVID-19. [[Last accessed on 2021 Sep 28]]. Available from: https://www.moh.gov.sg/news-highlights/details/circuit-breaker-to-minimise-further-spread-ofcovid-19 .
- 5.Ministry of Health, Singapore. Roadmap ahead to phase two. [[Last accessed on 2021 Sep 28]]. Available from: https://www.moh.gov.sg/news-highlights/details/roadmap-aheadto-phase-two .
- 6.Kang ML, Goo JTT, Lee DJK. CHOP Protocol:Streamlining access to definitive intervention for major trauma victims. Singapore Med J. 2021;62:620–2. doi: 10.11622/smedj.2020113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christey G, Amey J, Campbell A, Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;133:81–8. [PubMed] [Google Scholar]
- 8.Forrester JD, Liou R, Knowlton LM, Jou RM, Spain DA. Impact of shelter-in-place order for COVID-19 on trauma activations:Santa Clara County, California, March 2020. Trauma Surg Acute Care Open. 2020;5:e000505. doi: 10.1136/tsaco-2020-000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang F, Lu X. The effect of COVID-19 on trauma system in one city of China. Scand J Trauma Resusc Emerg Med. 2020;28:57. doi: 10.1186/s13049-020-00752-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thornton J. Covid-19:A&E visits in England fall by 25% in week after lockdown. BMJ. 2020;369:m1401. doi: 10.1136/bmj.m1401. [DOI] [PubMed] [Google Scholar]
- 11.Park C, Sugand K, Nathwani D, Bhattacharya R, Sarraf KM. Impact of the COVID-19 pandemic on orthopedic trauma workload in a London level 1 trauma center:The “golden month”. Acta Orthop. 2020;91:556–61. doi: 10.1080/17453674.2020.1783621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tan C. Roads become more free-flowing and safer but speeding cases surge. The Straits Times. 2020. [[Last accessed on 2021 Sep 28]]. May 13. Available from: https://www.straitstimes.com/singapore/transport/roads-become-morefree-flowing-and-safer-but-speeding-cases-surge .
- 13.Hatchimonji JS, Swendiman RA, Seamon MJ, Nance ML. Trauma does not quarantine:Violence during the COVID-19 pandemic. Ann Surg. 2020;272:e53–4. doi: 10.1097/SLA.0000000000003996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kofman YB, Garfin DR. Home is not always a haven:The domestic violence crisis amid the COVID-19 pandemic. Psychol Trauma. 2020;12((Suppl 1)):S199–201. doi: 10.1037/tra0000866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iob E, Steptoe A, Fancourt D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br J Psychiatry. 2020;217:543–6. doi: 10.1192/bjp.2020.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Henry N, Parthiban S, Farroha A. The effect of COVID-19 lockdown on the incidence of deliberate self-harm injuries presenting to the emergency room. Int J Psychiatry Med. 2021;56:266–77. doi: 10.1177/0091217420982100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tng XJJ, Chew QH, Sim K. Psychological sequelae within different populations during the COVID-19 pandemic: A rapid review of extant evidence. Singapore Med J. 2022;63:229–35. doi: 10.11622/smedj.2020111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-May 30. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chew QH, Chia FL, Ng WK, Lee WCI, Tan PLL, Wong CS, et al. Perceived stress, stigma, traumatic stress levels and coping responses amongst residents in training across multiple specialties during COVID-19 pandemic-A longitudinal study. Int J Environ Res Public Health. 2020;17:6572. doi: 10.3390/ijerph17186572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cacciapaglia G, Cot C, Sannino F. Second wave COVID-19 pandemics in Europe: A temporal playbook. Sci Rep. 2020;10:15514. doi: 10.1038/s41598-020-72611-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coimbra R, Edwards S, Kurihara H, Bass GA, Balogh ZJ, Tilsed J, et al. European Society of Trauma and Emergency Surgery (ESTES) recommendations for trauma and emergency surgery preparation during times of COVID-19 infection. Eur J Trauma Emerg Surg. 2020;46:505–10. doi: 10.1007/s00068-020-01364-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neil J. Domestic violence and COVID-19:Our hidden epidemic. Aust J Gen Pract. 2020;49 doi: 10.31128/AJGP-COVID-25. doi:10.31128/AJGP-COVID-25. [DOI] [PubMed] [Google Scholar]
- 23.Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–71. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]