Abstract
Background
Transitions of care represent a vulnerable time when patients are at increased risk of medication errors. Medication-related problems constitute one of the main contributors to hospital readmissions. Discharge interventions carried out by pharmacists have been shown to reduce hospital readmissions. Although clinical pharmacists in British Columbia are involved in discharges, their degree of involvement and the interventions they prioritize in practice have not been fully elucidated.
Objectives
To characterize the current involvement of BC hospital pharmacists at the time of discharge, to identify which discharge interventions they believe should be prioritized, and who they feel should be responsible for these interventions, as well as to identify strategies to optimize the discharge process.
Methods
A survey of BC hospital pharmacists was conducted in January and February 2022. The survey included questions about pharmacists’ current involvement at the time of discharge, interventions required for a successful discharge, solutions for optimizing the patient discharge process, and participants’ baseline characteristics.
Results
The survey response rate was 20% (101/500). Pharmacists reported performing all interventions for less than 60% of their patients. Interventions such as medication reconciliation on discharge, medication education, and ensuring adherence were considered very important for a successful discharge and were considered to be best performed by pharmacists. Solutions for optimizing the discharge process included improved staffing, weekend coverage, timely notification of discharge, and prescribing by pharmacists.
Conclusions
Despite the belief that most interventions listed in the survey are necessary for successful discharge, various barriers prevented pharmacists from providing them to all patients. Increased resources and expanded scope of practice for pharmacists could reduce hospital readmissions and enable broader implementation of discharge interventions.
Keywords: hospital discharge, survey, hospital pharmacists, optimization of care, hospital readmission
RÉSUMÉ
Contexte
Les transitions de soins sont une période vulnérable pendant laquelle les patients courent un risque accru d’erreurs médicamenteuses. Les problèmes liés aux médicaments constituent l’un des principaux contributeurs aux réadmissions à l’hôpital. Il a été démontré que les interventions au moment du congé effectuées par les pharmaciens réduisent les réadmissions à l’hôpital. Même si les pharmaciens cliniciens de la Colombie-Britannique participent aux congés, leur degré de participation et les interventions qu’ils privilégient dans la pratique n’ont pas été entièrement élucidés.
Objectifs
Caractériser l’implication actuelle des pharmaciens des hôpitaux de la Colombie-Britannique au moment du congé; recenser les interventions à ce moment qui, selon eux, devraient être prioritaires et quel praticien, selon eux encore, devrait être responsable de ces interventions; enfin, déterminer des stratégies pour optimiser le processus de congé de l’hôpital.
Méthodes
Une enquête auprès des pharmaciens hospitaliers de la Colombie-Britannique a été menée en janvier et février 2022. L’enquête comprenait des questions sur l’implication actuelle des pharmaciens au moment du congé du patient, les interventions requises pour sa réussite, les solutions pour optimiser son processus ainsi que les caractéristiques de base des participants.
Résultats
Le taux de réponse à l’enquête était de 20 % (101/500). Les pharmaciens ont déclaré avoir effectué toutes les interventions auprès de moins de 60 % de leurs patients. Les interventions telles que le bilan comparatif des médicaments à la sortie, l’éducation sur les médicaments et l’assurance de l’observance étaient considérées comme très importantes pour la réussite du congé et les pharmaciens étaient considérés comme étant les mieux placés pour effectuer ces interventions. Les solutions suggérées pour optimiser le processus comprenaient un meilleur personnel, une couverture le week-end, une notification en temps opportun du congé et des prescriptions par les pharmaciens.
Conclusions
Même si l’on croit que la plupart des interventions énumérées dans l’enquête sont nécessaires pour la réussite du congé hospitalier, divers obstacles ont empêché les pharmaciens de les proposer à tous les patients. Des ressources accrues et un champ d’exercice élargi pour les pharmaciens pourraient réduire les réadmissions à l’hôpital et permettre une mise en oeuvre élargie des interventions au moment du congé.
Mots-clés: congé hospitalier, enquête, pharmaciens hospitaliers, optimisation des soins, réadmission à l’hôpital
INTRODUCTION
Transitions from hospital to the community may leave patients vulnerable and at increased risk of medication errors, which can in turn lead to patient harm and burden the health care system with increasing rates of readmissions.1 According to the Canadian Institute for Health Information, 8.5% of patients are readmitted to the hospital within a month of discharge, costing the health care system approximately $1.8 billion annually.2 British Columbia’s performance in this regard is worse than the national average, with 9% of patients being readmitted to hospital within 30 days of discharge. 2 Among all readmissions, 3% to 64% are medication-related, and although medication-related readmissions are not entirely avoidable, 69% of them are preventable.3
Medication-related problems such as medication errors, adverse drug events, inappropriate medication prescribing, and medication nonadherence contribute to readmissions. 4 One risk factor for medication-related problems is polypharmacy, which has a high prevalence, particularly among patients with cancer and dementia, and increases the risk of readmission.5,6 Furthermore, in at least half of the patients with medication-related problems, these problems occur during admission, at discharge, or within 1 month of discharge.7 These findings underline the importance of preventing medication-related problems among high-risk patients at transition points such as admission or discharge.
Several discharge interventions have been shown to reduce medication-related problems and the resulting readmissions. Medication reconciliation, postdischarge follow-up, patient education, coordination of care among team members, and motivational interviewing have been shown to reduce adverse drug events and medication errors, as well as improving medication adherence.7–9 Among these interventions, medication reconciliation has also been shown to be useful in identifying and reducing medication errors or discrepancies.5,10–12
Pharmacists play a valuable role in performing discharge interventions, which include optimizing medication use, reducing medication discrepancies, identifying medication errors, preventing adverse drug events, and improving medication adherence.1,11,13 These interventions, particularly for patients at high risk of readmission, can generate cost savings for the health care system. In studies involving older adults, pharmacist-led interventions such as medication reconciliation, medication counselling, communication with primary care physicians, and postdischarge follow-up by telephone reduced all-cause hospital visits or readmissions, which led to a lower health care cost per patient.14,15 Furthermore, studies have shown that collaboration between pharmacists and physicians reduces readmission rates, while collaboration between community and hospital pharmacists ensures continuity of care, addresses noncompliance, and ensures patient education after discharge.13,16
As the foregoing summary has highlighted, the literature to date provides extensive information on discharge interventions and the pharmacist’s role; however, very few studies have attempted to characterize current practice in British Columbia to show whether these interventions are practical and sustainable in a hospital setting. To address this gap, our research team conducted a focus group study to capture BC hospital pharmacists’ perspectives on the discharge process.17 Overall, the 20 pharmacists who participated in that previous study believed that discharge optimization requires a team-based approach, with pharmacists playing a central role in the process.17 Although clinical pharmacists are best suited to complete medication reconciliation, review discharge prescriptions, and communicate the medication plan with community providers, barriers such as inadequate resources and excessive workload prevent them from optimizing the discharge process for all patients.17 The barriers and potential solutions identified in that earlier study formed the basis for some of the questions in the survey study reported here, in which we explored these themes along with the overall role that pharmacists play in the discharge process. The objective of this study was to characterize the current involvement of pharmacists at discharge, to identify which discharge interventions should be prioritized and which health care team members should provide them, and to identify strategies to optimize the discharge process.
METHODS
Study Design and Participants
The study used a descriptive cross-sectional web-based survey to gain insights into BC hospital pharmacists’ current involvement at discharge and their perspectives on optimizing the discharge process. The participants were hospital pharmacists across British Columbia who were providing clinical services to patients consistent with the clinical pharmacist role, as defined by the American College of Clinical Pharmacy (ACCP), and who were involved in the discharge process. The ACCP defines the clinical pharmacist role as the provision of medication therapy evaluations and recommendations, as well as advice regarding the safe, appropriate, and cost-effective use of medications, to patients and health care professionals.18 Study participants were employed within one of the province’s health authorities. Hospital pharmacists with only dispensary responsibilities and those holding exclusively leadership roles, such as coordinators, managers, and directors, were excluded.
Survey Development and Dissemination
A comprehensive literature search was first conducted to identify the various discharge interventions that have been shown to be beneficial. Based on that information and the results of our focus group study,17 we developed a survey to obtain a more in-depth understanding of pharmacists’ current involvement at discharge and their perspectives on optimizing the discharge process. The survey was divided into the following sections: baseline characteristics, characterization of the current involvement of pharmacists at discharge and the barriers to performing discharge interventions, pharmacists’ perspectives on the requirements for a successful discharge, and potential solutions for optimizing discharges. A variety of survey question formats were used, including but not limited to ranking, Likert-type scale, multiple choice, and open text (for the survey content, please see Supplement 1, available at https://www.cjhp-online.ca/index.php/cjhp/article/view/3433/).
Before dissemination of the survey, it was piloted for content and clarity by 5 clinical pharmacists. Once their feedback was incorporated, the final survey, consisting of 23 questions, was distributed to hospital pharmacists across British Columbia. Administrative or leadership staff within each health authority were asked to disseminate to their respective staff members a letter of invitation to participate, which included a link to the survey. The survey was available through the University of British Columbia’s version of the web-based Qualtrics platform (version: January–February 2022), which complies with the BC Freedom of Information and Protection of Privacy Act, keeping survey data secure and storing data in Canada. All participants provided informed consent before initiating the survey, which was available for completion over a 6-week period, with reminder emails sent at the 3- and 5-week marks. Interested participants could enter a draw for 2 gift cards, as an incentive to take part in the study.
Harmonized approval was obtained from the University of British Columbia Behavioural Research Ethics Board, and operational approval was obtained from each health authority.
Data Analysis
The web-based Qualtrics questionnaire platform was used to collect and aggregate the responses. Descriptive statistics were used to summarize and report the data.
RESULTS
A total of 136 participants consented to participate in the study, of whom 35 were excluded, either because they did not meet the inclusion criteria (n = 14, 10.3%) or because they completed less than 30% of the survey (n = 21, 15.4%). According to the National Association of Pharmacy Regulatory Authorities19 and the Health Employers Association of BC,20 there are approximately 1000 hospital pharmacists in British Columbia, of whom 50% are clinical pharmacists. Based on this estimate of 500 clinical pharmacists practising in British Columbia, the survey response rate was 20%.
Participants’ demographic characteristics are summarized in Table 1. More than half of the respondents had an accredited Canadian Pharmacy Residency Year 1 (ACPR1) designation, and the majority had been practising for 10 years or less. Among the participants, 72% practised in a tertiary setting. Almost two-thirds of the participants were practising in 1 of the following 3 health authorities: Vancouver Coastal Health, Vancouver Island Health, and Fraser Health. On average, each pharmacist was responsible for 31 patients (standard deviation 13, range 4–80).
TABLE 1.
Demographic Characteristics of Participants
| Characteristic | No. (%) of Participants |
|---|---|
| Highest level of training | n = 87 |
| Accredited Canadian Pharmacy Residency Year 1 (ACPR1) | 50 (57) |
| Doctor of Pharmacy (PharmD) | 20 (23) |
| Other | 17 (20) |
|
| |
| Practice experience | n = 88 |
| < 5 years | 38 (43) |
| 5–10 years | 18 (20) |
| > 10 years | 32 (36) |
|
| |
| Practice setting | n = 88 |
| Tertiary hospital | 63 (72) |
| Community hospital | 21 (24) |
| Other | 4 (5) |
|
| |
| Health authority | n = 87 |
| Vancouver Coastal Health | 21 (24) |
| Vancouver Island Health | 17 (20) |
| Fraser Health | 14 (16) |
| Interior Health | 12 (14) |
| Northern Health | 9 (10) |
| Providence Health Care | 8 (9) |
| Provincial Health Services Authority | 6 (7) |
|
| |
| Average pharmacist-to-patient ratio | n = 77 |
| 1:31 | |
Current Involvement of Pharmacists at Discharge
Almost 60% of participants (59/100) reported spending between 75% and 100% of their time on clinical activities, and the majority of participants (67/101) reported that less than 25% of their clinical time was spent on discharge-related activities. This translates to pharmacists spending an average of 26 minutes per day on discharge-related activities, as reported by respondents. Given the limited time spent performing discharge-related activities, it is not surprising that overall only 51% of patients received this type of care (as reported in the survey).
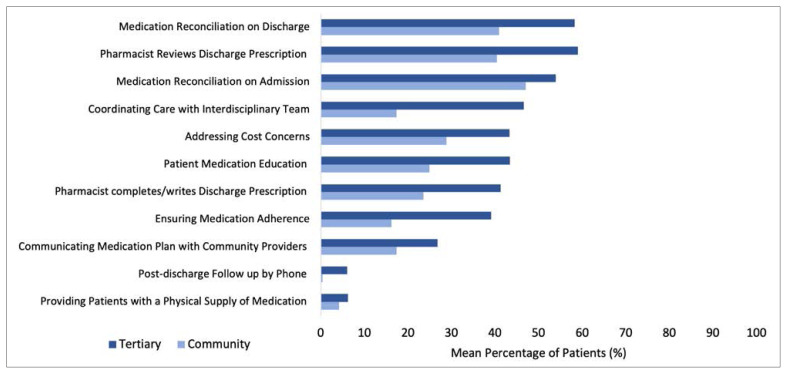
To further characterize the current involvement of pharmacists at discharge, Figure 1 shows the mean percentage of patients for whom participants reported providing each intervention. Overall, all interventions were provided for less than 60% of patients at tertiary sites and less than 50% of patients at community sites. The 3 most frequently performed interventions were medication reconciliation on admission, medication reconciliation on discharge, and review of the discharge prescription. The 3 least frequently performed interventions were communicating the medication plan to community providers, postdischarge follow-up by phone, and providing patients with a supply of medication.
FIGURE 1.
Involvement of clinical pharmacists at discharge, represented as mean percentage of patients receiving each discharge intervention (n = 84 respondents).
Barriers reported as preventing pharmacists from providing these interventions included lack of resources or staffing, competing clinical duties, and time constraints. As such, respondents indicated that they prioritized patients who had a high number of medication changes, those receiving therapy with high-risk medications (i.e., medications with a narrow therapeutic index and/or requiring frequent monitoring), and those admitted because of an adverse drug reaction.
Requirements for Successful Discharge
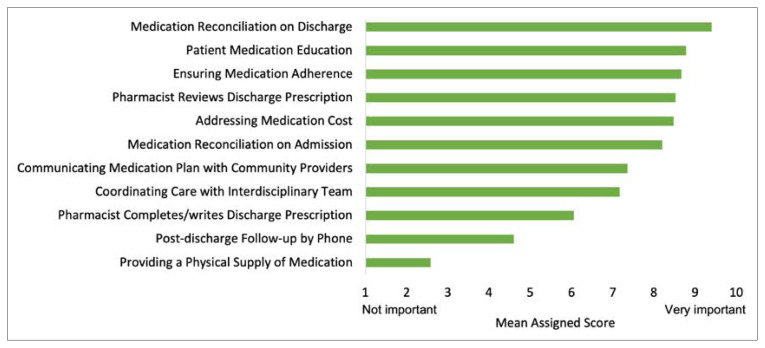
Figure 2 shows the perspectives of pharmacists on the relative importance of each intervention for a successful discharge, in an ideal setting with unlimited resources and without barriers. Among the 11 interventions listed, 8 received a mean score of at least 7 out of 10, indicating that they were rated as important or very important for a successful discharge.
FIGURE 2.
Importance of each intervention for a successful discharge, represented as mean score on a scale of 1 to 10 (n = 90 respondents).
In terms of the health care team member best suited for providing these interventions, respondents believed that the pharmacist should be primarily responsible for medication reconciliation on discharge, patient medication education, and ensuring medication adherence. Most of the other interventions were believed to be best shared between the pharmacist and the physician, whereas addressing medication cost concerns was thought to be best shared between the pharmacist and the social worker.
Solutions for Optimizing the Discharge Process
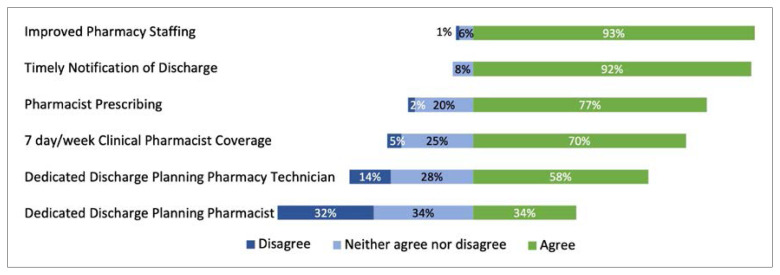
The survey proposed several solutions, based on data gathered from the focus group study, and asked participants to indicate their level of agreement with each one (Figure 3). The majority (at least 70%) of respondents agreed with implementation of improved pharmacy staffing, timely notification of discharge, pharmacist prescribing, and clinical pharmacist coverage every day of the week. Most respondents did not agree with having a dedicated discharge planning pharmacist. Almost all respondents agreed that a pharmacist-generated discharge summary should be shared with the community team (i.e., community or primary care pharmacist, family physician, specialist, nurse) (data not shown).
FIGURE 3.
Clinical pharmacists’ perspectives on solutions for optimizing the discharge process (n = 88 respondents).
DISCUSSION
The findings of this survey illustrate that for BC hospital pharmacists, a large proportion (> 75%) of time is spent on clinical activities, with less than a quarter of that time spent on discharge-related activities. Less than 60% of patients at tertiary sites and less than 50% of patients at community sites receive each intervention. These findings highlight the fact that time constraints and a lack of resources, the latter of which is more pronounced at community sites, can be 2 of the main barriers to pharmacists performing the necessary interventions required for a successful discharge. Whether having additional time would result in pharmacists providing these interventions to more patients is not clear. What is clear, however, is that not receiving these interventions can have a significant impact on the care of patients at community sites in particular, given that these typically rural sites offer limited access to specialized care.
The pharmacists who participated in this study reported that among their most commonly performed interventions were medication reconciliation on admission and on discharge. This does not come as a surprise, given that medication reconciliation has been shown to reduce readmissions due to adverse drug events.1,5,12 However, the high prevalence of medication reconciliation in practice is also influenced by the fact that it is a required organizational practice for hospitals, as specified by Accreditation Canada.21 Among other frequently performed interventions, pharmacist review of the discharge prescription has been shown to improve patient care and is highly valued by care providers.22–24 It can potentially facilitate a smoother transition to community for the patients and can alleviate some of the burden currently placed on nurses and physicians by enabling more rapid discharge.
The interventions least commonly performed by pharmacists were provision of a supply of medication and postdischarge follow-up by phone. In fact, 20% to 40% of respondents indicated that these 2 interventions were not performed by any health care team member at their respective sites. Provision by the hospital of a supply of medications at discharge has been shown to improve patient adherence, reduce the likelihood of all-cause revisits to the emergency department within 30 days, and free up hospital beds occupied by patients waiting for their medications to become available through a community pharmacy.25,26 In British Columbia, however, take-home medications are supplied by hospitals only in cases of emergency or a planned leave of absence (when a patient leaves the hospital setting for a predetermined period, after which they are expected to return), which explains why this intervention was not commonly performed.27
Postdischarge follow-up was reportedly provided to less than 10% of patients. Several studies indicate that this intervention reduces medication errors and readmissions related to adverse drug events and improves patients’ adherence to medication therapy.1,9,11 One reason why this intervention was not being performed might be that clinical pharmacists did not consider outpatient follow-up as part of their responsibility. Other reasons might include time constraints and competing clinical duties.
In the absence of barriers, respondents indicated that they considered 8 of the 11 specified interventions as important or very important for a successful discharge. Interestingly, 3 of the interventions (patient medication education, ensuring medication adherence, and addressing medication cost concerns) considered to be very important for a successful discharge (score of 8 or more out of 10) were reportedly provided by pharmacists for less than 50% of patients. When these interventions are not provided, medication adherence is the aspect of patient care that is most compromised.7–9,11 Although the respondents were aware of the important role that patient adherence plays in optimizing the discharge process, current practice does not address this aspect of medication therapy for all patients. Overall, this signifies the gap between current practice and what pharmacists believe is required for optimal discharge.
Respondents indicated that pharmacists should be the health care team member responsible for medication education, medication reconciliation on discharge, and ensuring medication adherence. In support of these findings, a recent study demonstrated that medication reconciliation performed by clinical pharmacists resulted in interventions that not only were well received by those ordering the medications but also lowered 7-day readmission rates.28 Additionally, pharmacist-performed medication reconciliation and medication education have been associated with improved patient satisfaction scores.29
Nonetheless, for almost all interventions deemed essential for successful discharge, respondents indicated that the responsibility should be mostly shared between physicians and pharmacists. This finding is not surprising, given previous studies showing that hospital pharmacists may not feel directly responsible for patient outcomes.30 This perception could be due to not having the authority to prescribe independently and the belief that the medical hierarchy promotes physicians as the most responsible provider. 30 Consequently, patients may not be receiving these interventions at all, if physicians have other competing responsibilities and are too busy to provide them.
In terms of solutions to address the identified barriers, respondents agreed that improved staffing could allow pharmacists more time and resources to perform interventions. Achieving this improvement may be challenging, given that funding is limited and training new staff adds to the responsibilities of current practising pharmacists. A more practical solution might be to identify which patients should be prioritized to receive these interventions. The results of this survey indicate that high-priority patients would be those with numerous medication changes, those receiving high-risk medications, and those whose admission was due to an adverse drug reaction. Furthermore, the current literature indicates that certain patient populations, such as older adults and those with cancer or dementia, are at increased risk of medication-related problems and thus may benefit the most from these interventions.5,6,10 Timely notification of discharge (i.e., 24 hours in advance) is another solution that allows pharmacists to plan ahead and adjust their workflow to perform certain interventions for as many patients as possible. Lastly, an expanded scope of practice enables pharmacists to take the lead in writing discharge prescriptions. Although most respondents did not agree with having a dedicated discharge pharmacist, other studies have shown that such a role can help prevent medication errors, provide patient education, address cost concerns, and improve patient adherence.31 The common theme, however, is that the solution lies in improved staffing. Whether that occurs through having more ward-based clinical pharmacists or a dedicated discharge pharmacist is something that could be further explored and individualized to each site, according to their staffing needs and overall workflow.
This survey study had several limitations. With approximately 100 responses collected, our survey did not meet our targeted response rate of 40% (n = 200). Furthermore, because the survey was relatively long (requiring 15–20 minutes to complete), 13 entries were left incomplete. With regard to the reported results, pharmacist involvement at discharge was self-reported on the basis of participants’ perceived estimates, which can differ from the actual care received by patients. For example, these self-reported results differ from those of a survey done in 2020/21, where 59% (16/27) of BC hospitals reported that medication reconciliation was performed by pharmacy staff in less than 50% of areas/situations, and only 4% (1/27) of respondents reported medication reconciliation by pharmacy staff in 100% of areas/situations.32 In addition, some questions in our survey, such as those asking about barriers to pharmacists performing discharge interventions and possible solutions, offered participants an a priori list, an approach that can introduce bias. Lastly, approximately 70% of participants were practising at a tertiary site, so the overall results are less representative of the community setting, where resources are typically much more limited and proposed solutions can be challenging to implement.
CONCLUSION
Several interventions have been shown to reduce medication-related problems and the resulting readmissions. Pharmacists responding to this survey believed that these interventions are required for successful discharge and that pharmacists are the health care professionals most suited to provide them. Currently in British Columbia, however, barriers such as lack of resources, time constraints, and competing clinical duties are preventing pharmacists from providing interventions to all patients. To further expand on the findings of this study, future work to understand the perspectives of other stakeholders—including patients, other health care professionals, and pharmacists practising in non–tertiary care settings—would be beneficial in determining how discharges can be optimized.
Supplementary Information
Funding Statement
This study was supported by unrestricted research funds of the primary investigator (K.D.).
Footnotes
Competing interests: None declared.
Funding: This study was supported by unrestricted research funds of the primary investigator (K.D.).
References
- 1. Mekonnen A, McLachlan A, Brien J. Effectiveness of pharmacist-led medication reconciliation programs on clinical outcomes at hospital transitions: a systematic review and meta-analysis. BMJ Open. 2016;6(2):e010003. doi: 10.1136/bmjopen-2015-010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.All-cause readmission to acute care and return to the emergency department. Canadian Institute for Health Information; 2012. [cited 2021 Aug 12]. Available from: https://publications.gc.ca/collections/collection_2013/icis-cihi/H118-93-2012-eng.pdf. [Google Scholar]
- 3. El Morabet N, Uitvlugt E, van den Bemt B, van den Bemt P, Janssen M, Karapinar-Çarkit F. Prevalence and preventability of drug-related hospital readmissions: a systematic review. J Am Geriatr Soc. 2018;66(3):602–8. doi: 10.1111/jgs.15244. [DOI] [PubMed] [Google Scholar]
- 4. Rodrigues C, Harrington A, Murdock N, Holmes J, Borzadek E, Calabro K, et al. Effect of pharmacy-supported transition-of-care interventions on 30-day readmissions: a systematic review and meta-analysis. Ann Pharmacother. 2017;51(10):866–89. doi: 10.1177/1060028017712725. [DOI] [PubMed] [Google Scholar]
- 5. Herledan C, Baudouin A, Larbre V, Gahbiche A, Dufay E, Alquier I, et al. Clinical and economic impact of medication reconciliation in cancer patients: a systematic review. Support Care Cancer. 2020;28(8):3557–69. doi: 10.1007/s00520-020-05400-5. [DOI] [PubMed] [Google Scholar]
- 6. Sawan M, Wennekers D, Sakiris M, Gnjidic D. Interventions at hospital discharge to guide caregivers in medication management for people living with dementia: a systematic review. J Gen Intern Med. 2021;36(5):1371–9. doi: 10.1007/s11606-020-06442-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Daliri S, Boujarfi S, el Mokaddam A, Scholte op Reimer W, ter Riet G, den Haan C, et al. Medication-related interventions delivered both in hospital and following discharge: a systematic review and meta-analysis. BMJ Qual Saf. 2020;30(2):146–56. doi: 10.1136/bmjqs-2020-010927. [DOI] [PubMed] [Google Scholar]
- 8. Burke RE, Guo R, Prochazka AV, Misky GJ. Identifying keys to success in reducing readmissions using the ideal transitions in care framework. BMC Health Serv Res. 2014;14:423. doi: 10.1186/1472-6963-14-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. El Hajj MS, Jaam MJ, Awaisu A. Effect of pharmacist care on medication adherence and cardiovascular outcomes among patients postacute coronary syndrome: a systematic review. Res Soc Admin Pharm. 2018;14(6):507–20. doi: 10.1016/j.sapharm.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 10. Van den Bemt PMLA, van der Schrieck-de Loos EM, van der Linden C, Theeuwes AMLJ, Pol AG. Dutch CBO Study Group. Effect of medication reconciliation on unintentional medication discrepancies in acute hospital admissions of elderly adults: a multicenter study. J Am Geriatr Soc. 2013;61(8):1262–8. doi: 10.1111/jgs.12380. [DOI] [PubMed] [Google Scholar]
- 11. De Oliveira GS, Jr, Castro-Alves LJ, Kendall MC, McCarthy R. Effectiveness of pharmacist intervention to reduce medication errors and health-care resources utilization after transitions of care: a meta-analysis of randomized controlled trials. J Patient Saf. 2021;17(5):375–80. doi: 10.1097/PTS.0000000000000283. [DOI] [PubMed] [Google Scholar]
- 12. Mekonnen A, McLachlan A, Brien J. Pharmacy-led medication reconciliation programs at hospital transitions: a systematic review and meta-analysis. J Clin Pharm Ther. 2016;41(2):128–44. doi: 10.1111/jcpt.12364. [DOI] [PubMed] [Google Scholar]
- 13. Foot H, Scott I, Sturman N, Whitty J, Rixon K, Connelly L, et al. Impact of pharmacist and physician collaborations in primary care on reducing readmission to hospital: a systematic review and metaanalysis. Res Soc Admin Pharm. 2022;18(6):2922–43. doi: 10.1016/j.sapharm.2021.07.015. [DOI] [PubMed] [Google Scholar]
- 14. Gillespie U, Alassaad A, Henrohn D, Garmo H, Hammarlund-Udenaes M, Toss H, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older. Arch Intern Med. 2009;169(9):894–900. doi: 10.1001/archinternmed.2009.71. [DOI] [PubMed] [Google Scholar]
- 15. Tomlinson J, Cheong VL, Fylan B, Silcock J, Smith H, Karban K, et al. Successful care transitions for older people: a systematic review and meta-analysis of the effects of interventions that support medication continuity. Age Aging. 2020;49(4):558–69. doi: 10.1093/ageing/afaa002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ensing HT, Koster ES, Dubero DJ, van Dooren AA, Bouvy ML. Collaboration between hospital and community pharmacists to address drug-related problems: the HomeCoMe-program. Res Soc Admin Pharm. 2019;15(3):267–78. doi: 10.1016/j.sapharm.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 17. Ladhar S, Dahri K, Inglis C, Sambrielaz A, Raza H, Legal M. Insights into British Columbian hospital pharmacists perspectives on the discharge process. Innov Pharm. 2023;13(4) doi: 10.24926/iip.v13i4.5093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. American College of Clinical Pharmacy. Standards of practice for clinical pharmacists. Pharmacotherapy. 2014;34(8):794–7. doi: 10.1002/phar.1438. [cited 2021 Aug 12] Available from: https://www.accp.com/docs/positions/guidelines/standardsofpractice.pdf. [DOI] [PubMed] [Google Scholar]
- 19.National statistics. National Association of Pharmacy Regulatory Agencies; 2022. [cited 2022 Oct 16]. Available from: https://www.napra.ca/national-statistics. [Google Scholar]
- 20.Pharmacists [statistical database] Health Employers Association of BC; 2022. [cited 2022 Oct 16]. Available from: https://www.heabc.bc.ca/Page4349.aspx#.Y0t8Ci8r1fR. [Google Scholar]
- 21.Accreditation Canada; Canadian Institute for Health Information; Canadian Patient Safety Institute; Institute for Safe Medication Practices Canada. Medication reconciliation in Canada: raising the bar Progress to date and the course ahead. Accreditation Canada; 2012. [cited 2022 Oct 16]. Available from: https://www.ismp-canada.org/download/MedRec/20121101MedRecCanadaENG.pdf. [Google Scholar]
- 22. Lineberry E, Rozycki E, Jordan T, Mellett J, North A. Implementation of pharmacist targeted discharge prescription review in an emergency department. Am J Emerg Med. 2021;48:288–94. doi: 10.1016/j.ajem.2021.04.054. [DOI] [PubMed] [Google Scholar]
- 23. Cesarz J, Steffenhagen A, Svenson J, Hamedani A. Emergency department discharge prescription interventions by emergency medicine pharmacists. Ann Emerg Med. 2013;61(2):209–214e1. doi: 10.1016/j.annemergmed.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Elbeddini A, Yang L, Aly A. A case-control study: the impact of unintentional discrepancies and pharmacist discharge prescription review on 30–day hospital readmission. J Prim Care Community Health. 2020;11:215013272093201. doi: 10.1177/2150132720932012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bullock S, Morecroft C, Mullen R, Ewing A. Hospital patient discharge process: an evaluation. Eur J Hosp Pharm. 2016;24(5):278–82. doi: 10.1136/ejhpharm-2016-000928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hatoun J, Bair-Merritt M, Cabral H, Moses J. Increasing medication possession at discharge for patients with asthma: the Meds-in-Hand Project. Pediatrics. 2016;137(3):e20150461. doi: 10.1542/peds.2015-0461. [DOI] [PubMed] [Google Scholar]
- 27.Schedule F part 2: hospital pharmacy standards of practice. College of Pharmacists of BC; 2022. Health Professions Act – bylaws. [cited 2022 Oct 16]. Available from: https://library.bcpharmacists.org/6_Resources/6-1_Provincial_Legislation/5079-HPA_Bylaws_Hospital.pdf. [Google Scholar]
- 28. Gallagher D, Greenland M, Lindquist D, Sadolf L, Scully C, Knutsen K, et al. Inpatient pharmacists using a readmission risk model in supporting discharge medication reconciliation to reduce unplanned hospital readmissions: a quality improvement intervention. BMJ Open Qual. 2022;11(1):e001560. doi: 10.1136/bmjoq-2021-001560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. March K, Peters M, Finch C, Roberts L, McLean K, Covert A, et al. Pharmacist transition-of-care services improve patient satisfaction and decrease hospital readmissions. J Pharm Pract. 2020;35(1):86–93. doi: 10.1177/0897190020958264. [DOI] [PubMed] [Google Scholar]
- 30. Frankel G, Austin Z. Responsibility and confidence. Can Pharm J (Ott) 2013;146(3):155–61. doi: 10.1177/1715163513487309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Balling L, Erstad B, Weibel K. Impact of a transition-of-care pharmacist during hospital discharge. J Am Pharm Assoc. 2015;55(4):443–8. doi: 10.1331/JAPhA.2015.14087. [DOI] [PubMed] [Google Scholar]
- 32.Hospital Pharmacy in Canada Survey Board. Hospital pharmacy in Canada survey report 2020/21. Canadian Society of Hospital Pharmacists; 2022. [cited 2023 June 10]. Available from: https://www.cshp.ca/docs/pdfs/HPCS-2020-21-Report-ENG.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.