Abstract
Background
Persistent anterior knee pain post total knee arthroplasty (TKA) is a significant cause of patient dissatisfaction. Selective patellar resurfacing is commonly practiced for primary total knee replacement (TKR) but there is a paucity in literature regarding its decision making.
Study Objective
This study aims to develop a decision-making algorithm for selective patellar resurfacing using Hospital for Special Surgery Patello-femoral Assessment score (HSS PFA score), weight-bearing patellofemoral X-ray, and intraoperative cartilage wear assessment based on the Outerbridge classification.
Materials and Methods
This prospective study enrolled 65 patients, assessing preoperative factors including HSS PFA score and Baldini view radiography. Intraoperative cartilage wear was categorized using the Outerbridge classification. Preoperative findings were correlated with intraoperative outcomes through statistical analysis, leading to the development of a predictive algorithm. The efficiency of algorithm was assessed at 3-year follow-up using HSS PFA score.
Results
A significant negative correlation (r = − 0.272, p = 0.029) was observed between HSS PFA score and cartilage wear. However, no significant relationships were established between HSS PFA score and Baldini view observations, including radiological tilt (p = 0.517) and displacement (p = 0.277). Intraoperative cartilage wear versus patellar tilt (p = 0.65) and displacement (p = 0.837) also yielded non-significant results. Three-year follow-up examinations revealed no complications and significant HSS PFA score improvements in all patients.
Conclusion
The requirement for patellar resurfacing can be predicted using a combination of preoperative parameter such as HSS PFA score and the intra-operative cartilage wear. We put forward an algorithm based on above findings to aid in the decision making.
Keywords: Selective patellar resurfacing, HSS patella femoral score, Baldini view
Introduction
Persisting anterior knee pain after total knee arthroplasty (TKA) remains a notable source of patient dissatisfaction. Ambiguity prevails regarding the optimal strategy for addressing osteoarthritis of the patellofemoral joint [1]. The existing body of evidence remains insufficient to unequivocally endorse the routine application of patellar resurfacing or its deliberate omission.
Widely used scoring systems like the Knee Society Scoring (KSS) System, Oxford Knee Score (OKS), and Knee Injury and Osteoarthritis Outcome Score (KOOS) fail to consider subjective symptoms or objective data specifically related to the patellofemoral joint [2]. Bindelglass et al. [3] noted a lack of association between patellar pain, malalignment and patient reported outcome scores. Shih et al. [4] found that the KSS scores remained unaffected by patellofemoral radiographic irregularities. Persistent anterior knee pain following TKA and disparities in reported outcomes following TKA could arise not solely from patient-related aspects and surgical methodologies, but also from the lack of suitable assessment scores for the patellofemoral joint.
The patellar tracking observed in an X-ray taken without weight-bearing may differ from real-life activities that load the patellofemoral joint and trigger symptoms [5]. The conventional non weight bearing X-ray of patellofemoral joint taken at a 45° knee flexion angle tends to exaggerate patellar misalignment (tilt and shift) [6]. A weight bearing Baldini x-ray view could enhance the likelihood of establishing correlations between clinical and radiographic evaluations in TKA [6].
We hypothesized that an exclusive patellofemoral scoring system, such as the Hospital for Special Surgery Patella-femoral Assessment score (HSS PFA Score), could enhance the precision of clinical outcome assessments for TKA. By correlating preoperative HSS PFA scores and findings from the Baldini x-ray view with intraoperative observations, we aimed to create an algorithm that could predict the necessity of patellar resurfacing in TKA and assess the efficiency of the algorithm using HSS PFA score at 3-year follow-up.
Materials and Methods
This study was a prospective study designed with the primary aim of developing a predictive tool to facilitate the decision-making process concerning selective patellar resurfacing in total knee arthroplasty (TKA). This tool was meticulously crafted through an examination of both preoperative and intraoperative factors to enhance the precision of treatment selection. Institutional ethical committee clearance was obtained for the study and informed consent was obtained from all participants.
Participants
Participants in this study were selected from individuals who had undergone total knee arthroplasty (TKA) at our facility during the period from August 2018 to March 2020.
Inclusion Criteria
Patients aged 18 years or older undergoing unilateral primary total knee arthroplasty (TKA).
Documented diagnosis of Kellgren Lawrence Grade IV osteoarthritis as the primary indication for TKA.
Patients who have given informed consent to participate in the study.
Exclusion Criteria
Revision arthroplasty.
Inflammatory joint diseases.
Inability to comply with study requirements or follow-up visits.
Data Collection
Preoperative Assessment
Prior to the surgical intervention, patients underwent a comprehensive clinical assessment encompassing an evaluation of their medical history and a thorough physical examination.
Utilization of the HSS PFA score (Table 1), an exclusive tool tailored to the patellofemoral compartment, facilitated the evaluation of preoperative patellofemoral function. This scoring mechanism was composed of a series of subjective and objective variables concentrated on the anterior compartment of the knee.
Table 1.
HSS patella scoring system [6] developed by Baldini et al.
| Type of score | Variable | Score | Points | Maximum | Minimum |
|---|---|---|---|---|---|
| Subjective | Anterior knee pain | VAS score 0–10: 50—(5 × VAS score) | 50 | 0 | |
| How do you rate the pain on the front of your knee while rising from the low chair? | |||||
| Functional limitations | No functional limitations | 15 | 15 | 0 | |
| Limitation in one function | 10 | ||||
| Limitation in two functions | 5 | ||||
| Limitation in three functions | 0 | ||||
| Do you feel that anterior part of your knee is limiting you while: 1. Climbing stairs; 2. Descending stairs; 3. Sitting for prolonged time (30 min at 90°) | |||||
| Objective | Tenderness (Palpation of medial and/or lateral patellar retinaculum-facet) | Absent | 10 | 10 | 0 |
| Present | 0 | ||||
| Crepitus (during active ROM) | None | 15 | 15 | 0 | |
| Mild (for a limited ROM) | 10 | ||||
| Moderate (throughout entire ROM) | 5 | ||||
| Severe (catching/clunk) | 0 | ||||
| Quadriceps strength | Normal (5/5) | 10 | 10 | 0 | |
| Reduced (3–4/5) | 5 | ||||
| Deficient (1–2/5) | 0 | ||||
| Total | 100 | 0 | |||
The scoring system ranged from 0 (worst case scenario) to 100 (best case scenario) points, and included ratings for subjective and objective clinical aspects of the knee.
Radiographic Evaluation
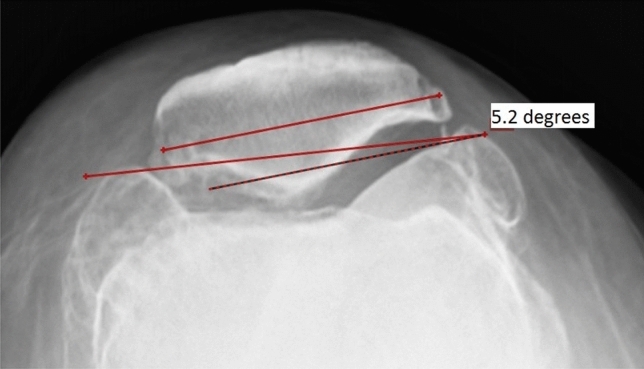
Radiographic assessment was performed using modified Merchant axial views (Axial weight-bearing view of patella/Baldini view) [6]. Baldini view was taken by positioning the standing patient in a semi squatted position with the knees in 45° flexion. The relationship between the X-ray source, the joint angle, and the cassette position was kept unchanged from the original Merchants view. The standing position and consequent muscle involvement were the only differences (Fig. 1). Measurements for patellar alignment (tilt and shift) were performed according to the method described by Gomes et al., using weight bearing axial-view radiographs (Figs. 2, 3) [7]. Preoperative patellar tilt and displacement were calculated.
Fig. 1.
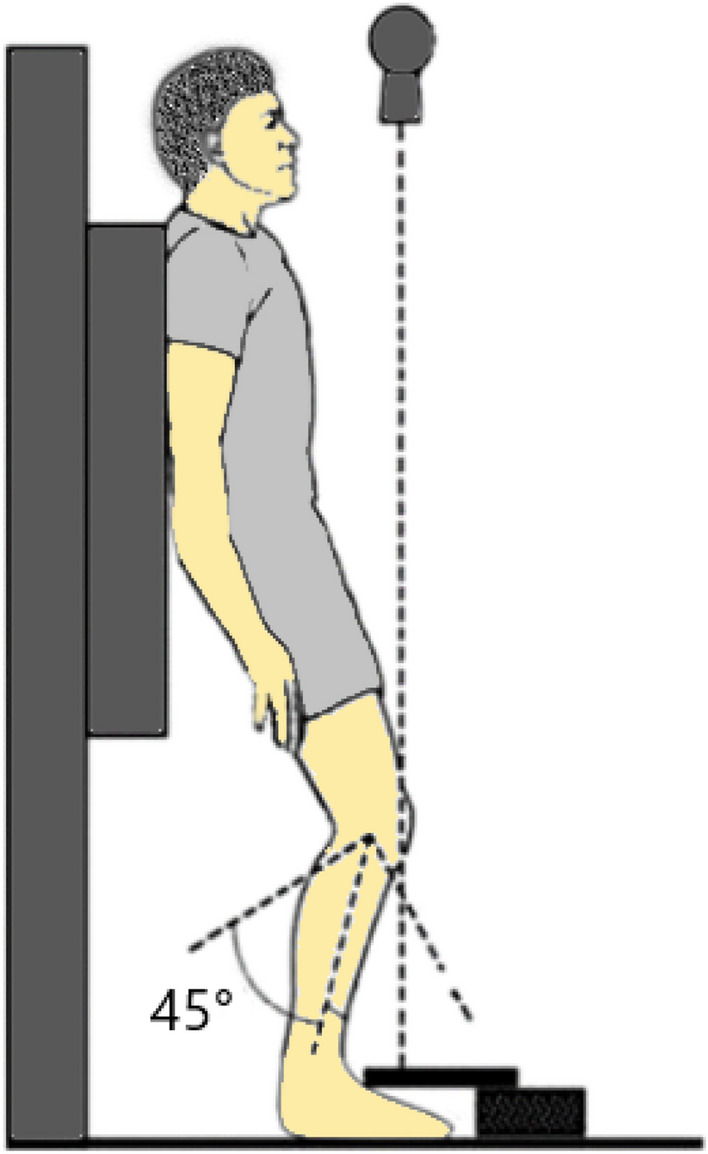
A demonstration of patient positioning for the weight bearing axial view radiograph
Fig. 2.

Patella displacement assessment in a weight bearing modified Merchant view using Radiant dicom viewer
Fig. 3.
Patella displacement assessment in a weight bearing modified merchant view using Radiant dicom viewer
Surgical Technique and Intra-operative Assessment
All patients underwent TKA by medial parapatellar arthrotomy under tourniquet and spinal epidural anaesthesia. All cases were operated using Genesis II Posterior Stabilized Knee System, which included an all-polyethylene patellar component available in sizes ranging from 29 to 35 mm, manufactured by Smith and Nephew. The patella was everted and held with a clamp parallel to the ground. In all the enrolled participants, the patella thickness was quantified using a vernier caliper during TKA. For comprehensive understanding and meticulous analysis, patella was divided into four distinct quadrants Superomedial, Inferomedial, Superolateral, and Inferolateral (Fig. 4).
Fig. 4.

The patella is divided into four quadrants (Superomedial, Inferomedial, Superolateral and inferolateral) to assess pattern of wear
In each quadrant, intraoperative assessment of the degree and pattern of cartilage wear on the patella was done and classified as per the established Outerbridge classification system [8] (Table 2).
Table 2.
Outerbridge classification system
| Grade | Pathology |
|---|---|
| I | Softening and swelling of articular cartilage |
| II | Fragmentation and fissuring of articular cartilage affecting an area of less than 0.5 inches |
| III | Fragmentation and fissuring of articular cartilage affecting an area greater than 0.5 inches |
| IV | Cartilage erosion to bone |
The decision making regarding the need of patellar resurfacing was made based on pre-operative clinical examination, radiological evaluation, HSS PFA score, cartilage wear and thickness noted intra-operatively. Patellae of size more than 21 mm with vernier caliper requiring resurfacing were resurfaced when required with an all-polyethylene, oval-shaped, three-pegged component when required.
The thickness of resurfacing patellar component 9mm was subtracted from the patella thickness and the guide was set at this level. The patella was carefully cut with a jig, removing it down to the subchondral bone of the lateral facet, avoiding any injury to the extensor mechanism. The cut surface was checked in four quadrants and refined free hand with saw till the thickness was equal and symmetrical in all zones. The patellar button was placed on the medial border of the cut surface and the uncovered bone of the lateral facet was sawed off. All synovium in the supra and infra patellar region was excised to prevent patellar crepitus or clunk. Femoral component rotation was adjusted perpendicular to Whiteside line and parallel to the trans-epicondylar axis in all knees. The trial button remained in place on the patella throughout the procedure, up to the point of cementing the patella component (Fig. 5). Patella tracking was checked with the components in place using the no thumb rule.
Fig. 5.
Clinical photos showing Patella resurfacing technique. a Patella cut using guide, b cut revised using free hand technique with saw to get desired thickness in all quadrants, c three peg holes and multiple drill holes inserted, d trial patella component in situ, e pressurisation during cementation f cemented patellar component in situ
It should be noted that for the smallest patellar component, a minimum of 9mm needed to be removed during the procedure. However, for patellae measuring less than 21mm in size, the risk of fracture during a 9mm cut was a concern. Therefore, in such cases, irrespective of the grade of cartilage wear, we chose to perform Patelloplasty as a standalone procedure to avoid potential fracture complications. During Patelloplasty, all osteophytes were excised and rasping of the borders were done. A lateral facectomy was done when significant deformation was there in patella (Fig. 6).
Fig. 6.

Technique of Patelloplasty
Correlation Analysis
A systematic investigation establishing correlations between the preoperative assessments (HSS PFA score and radiographic measurements derived from the Baldini view which include patellar tilt and displacement.) and intraoperative observations encompassing grade/pattern of cartilage wear was done. Correlation analysis was also done between HSS PFA score and need for Patella resurfacing/Patelloplasty was also done.
Algorithm Development
Drawing from the notable correlations elucidated through the correlation analysis, an algorithm was methodically formulated to predict the appropriateness of employing selective patellar resurfacing during TKA procedures.
This algorithm was adeptly tailored to incorporate preoperative parameters as well as intra-operative parameters. The culmination of these methodological steps aimed to make an algorithm with the potential to refine the decision-making process surrounding selective patellar resurfacing in TKA.
Efficiency of the Algorithm
All the enrolled participants were assessed using the HSS PFA score at 3 years. The enrolled patients were classified into two groups. Group A included the group of patients with patella less than 21 where we did Patelloplasty as the standalone procedure. Group B included the group of patients with patients size more than or equal to 21, where we were able to do selective patella resurfacing.
Results
During the designated study period, a total of 65 patients afflicted with degenerative osteoarthritis (OA) were meticulously evaluated and subsequently enrolled following the acquisition of informed consent. Among the participants, 48 (73.84%) patients were women and 17 (26.15%) patients were men, with an age range of 41 to 77 years at the time of the surgical intervention. All enrolled patients were radiographically diagnosed with grade IV OA prior to surgery. The distribution of operated knees revealed that 34 patients (52.3%) were on the left side, while 31 patients (47.7%) were on the right side.
Preoperative assessment of the patellofemoral score exhibited that 34 patients (52.3%) had scores ≤ 40, 21 patients (32.3%) fell within the range of 45 to 60, and 10 patients (15.3%) scored ≥ 65. The measured range of patellar tilt spanned from 0 to 7.7° with an average of 3.2°, while patellar displacement ranged from 0 to 5 mm, having an average displacement of 2.4 mm. Radiographically measured patellar thickness exhibited close concordance with intraoperative measurements, averaging at 22.32 mm.
Upon intraoperative evaluation, patellar cartilage wear was categorized utilizing the Outerbridge classification: Grade I in 3 cases (4.6%), Grade II in 32 cases (49.2%), Grade III in 4 cases (6.2%), and Grade IV in 26 cases (40%). The Superomedial (SM) and Inferomedial (IM) quadrants were commonly affected, accounting for 61 and 64 cases, respectively. Among the cases, 29 (45%) underwent patellar resurfacing, while 36 (55%) underwent Patelloplasty.
The Pearson correlation between the patellofemoral score and cartilage wear (r = − 0.272) was statistically significant (p = 0.029), indicating a negative correlation between the two. Hence, lower scores corresponded to higher grades of cartilage wear.
No significant correlations were observed between the patellofemoral score and Baldini view findings, including patella tilt (p = 0.517) and displacement (p = 0.277). Furthermore, the assessment of correlation between intraoperative cartilage wear and patellar tilt (p = 0.65) as well as patellar displacement (p = 0.837) did not yield statistically significant results.
In cases where the patellofemoral score (PFS) was ≤ 40, patellar resurfacing was performed in 19 cases (55.9%), while 7 cases (33.3%) underwent resurfacing when PFS ranged from 45 to 60. Notably, no cases underwent patellar resurfacing when the PFS was above 65.
The analysis revealed a positive association between the need for patellar resurfacing and the grade of cartilage wear, with a higher grade of wear correlating with an increased need for resurfacing. Specifically, 57.7% of the cases that underwent resurfacing exhibited Grade IV wear.
A receiver operating characteristic curve (ROC curve) was plotted for HSS patella score and patella resurfacing. The Area under curve (AUC) was 67.6% (Fig. 7).
Fig. 7.

ROC curve to predict selective patellar resurfacing based on HSS patella score
The predictability of patellar resurfacing when analysed based on preoperative patellofemoral score alone with cut off score of 50, the sensitivity was 61.5% and specificity was 84.6%.
Functional Outcome Assessment at 3 years Follow Up
The same cohort of 65 patients underwent a follow-up examination three years after their surgeries. It is noteworthy that no complications were reported in either group during this period. The patients were divided into two categories for analysis: Group 1 comprised individuals with a patellar thickness below 21mm, who had undergone a standalone Patelloplasty procedure. In contrast, Group 2 included patients with a patellar thickness of 21mm or more, in whom selective patella resurfacing was performed. The assessment using the HSS PFA score revealed that the average HSS PFA score for Group 1 was 60.5 with a standard deviation of 16.2, while for Group 2, it was 82.8 with a standard deviation of 19.8. Subsequent paired t-tests demonstrated significant differences in PFS scores before and after surgery for both of these groups. (Group A (< 21 cm); p < 0.001 and Group B(≥ 21): p < 0.001) (Table 3; Fig. 8).
Table 3.
Pre-operative and post-operative HSS PFA scores for both patellar thickness groups
| Patellar thickness | N | Pre-operative HSS PFA | Post-operative HSS PFA | Paired difference | Paired t test | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | t | p | ||
| Group A (< 21 cm) | 19 | 35.0 | 15.9 | 60.5 | 16.2 | 17.5 | 15.4 | 4.97 | < 0.001 |
| Group B (≥ 21 cm) | 46 | 48.9 | 18.6 | 82.8 | 7.4 | 33.9 | 19.8 | 11.6 | < 0.001 |
Fig. 8.
Box plot showing the HSS PFA score of both group of patients
Upon analysing the change in HSS PFA score in both the groups, the mean change in group A with patella size less than 21 cm was 30.8 with a standard deviation of 14.1 and the mean change in group B with patella thickness more than or equal to 21 was 33.9 with a standard deviation of 19.8 which was statistically significant using correlation statistics (p < 0.002) (Table 4).
Table 4.
Change in HSS PFA scores for both patellar thickness groups
| Patellar thickness | N | Change in HSS PFA score | t | p | |
|---|---|---|---|---|---|
| Mean | SD | ||||
| Group A (< 21 cm) | 19 | 30.8 | 14.1 | 3.129 | 0.002 |
| Group B (≥ 21 cm) | 46 | 33.9 | 19.8 | ||
Discussion
This study presents an innovative approach to decision-making for selective patellar resurfacing in TKA. By utilizing the HSS PFA score, weight-bearing radiographic views, and intraoperative assessments, the study developed an algorithm that can help determine the need for patellar resurfacing. The efficiency of the algorithm was tested using HSS PFA score at 3 years. The study's results demonstrate the algorithm's potential to improve clinical outcomes and reduce anterior knee pain.
Total knee arthroplasty (TKA) is widely recognized as an effective procedure that offers substantial relief from pain and improved function for individuals with advanced knee arthropathy. Nevertheless, the question of whether to routinely resurface the patella during primary TKA, as well as the criteria for making this decision, continues to generate debate [1].
Anterior knee pain has emerged as a prominent concern in TKAs, sparking significant deliberation regarding the management of the patella. Uncertainty persists regarding whether resurfacing the patella can prevent anterior knee pain and whether such resurfacing is indeed essential [9].
The common approach to patella management in TKA among Orthopaedic surgeons can categorized into three groups when it comes to patella management in TKA: those who advocate routine resurfacing, those who abstain from resurfacing, and those who opt for selective resurfacing [10, 11].
Proponents of patellar resurfacing point to decreased incidences of anterior knee pain, reduced reoperation rates, enhanced cost-effectiveness, and heightened patient satisfaction following surgery [12, 13]. However, patellar resurfacing has been associated with a range of complications, including patellar fracture, osteonecrosis, patellar polyethylene (PE) wear, aseptic loosening, instability, dislocation, overstuffing, extensor mechanism rupture, and patellar clunk syndrome [14]. On the other side, opponents of patellar resurfacing argue that there are no discernible clinical benefits in terms of pain and function improvement [15].
Recent level one evidence supports the use of patellar resurfacing along with total knee replacement (TKR), when compared to not performing the resurfacing. Benefits such as reduced anterior knee pain and lower requirement for additional surgeries were observed [11].
A recent survey conducted among knee surgeons in the UK has revealed that the most commonly employed approach for primary TKA involves selective patellar resurfacing [16]. The decision to resurface the patella is influenced by multiple factors. According to the survey, the top 12 reasons cited by surgeons include the osteoarthritic changes in patella's articular cartilage (61%), the presence of inflammatory arthritis (53%), the thickness of the natural patella (49%), occurrences of anterior knee pain before surgery (47%), the potential for subsequent secondary patellar resurfacing (43%), the movement and tracking of the natural patella during the surgical procedure (40%), the risk of experiencing anterior knee pain after the surgery (38%), the age of the patient (26%), the risk of postoperative complications like patella fracture or extensor mechanism failure (23%), the degree of constraint applied in the TKR (22%), the specific implant used (20%), and the risk of requiring revision surgery due to issues like loosening or failure of the patellar component (11%) [16].
This issue holds significant clinical importance, not only within the UK but also on a global scale. Selective patellar resurfacing stands out as the predominant method for primary total knee replacement (TKR) in numerous other countries worldwide, such as Australia, New Zealand, and Denmark [17, 18].
When it comes to selective patellar resurfacing, there is no decision making algorithm mentioned in literature at present. Our study found significant correlation between HSS PFA score and intra operative cartilage wear requiring patella resurfacing and we were able to demonstrate a significant correlation between the study variables.
Upon scrutinizing the results, it becomes evident that the predictability of patellar resurfacing based on weight bearing Baldini view findings was notably inadequate. No significant correlations were observed between the patellofemoral score and Baldini view findings, including patella tilt (p = 0.517) and displacement (p = 0.277). Also, the assessment of correlation between intraoperative cartilage wear and patellar tilt (p = 0.65) as well as patellar displacement (p = 0.837) did not yield statistically significant results. This was not consistent with findings of Baldini et al. [6] and Gharabieh et al. [25].
It is crucial to retain a minimum of 12–14 mm of the patient's own patellar bone to mitigate the risk of patellar strain and fracture [19, 20]. Conversely, excessive augmentation of the patellofemoral joint by more than 2 mm can result in patellofemoral malalignment, heightened contact and compression pressures, limited range of motion, anterior knee discomfort, and escalated shear forces, ultimately leading to the loosening and failure of the patellar button [21].
Addressing the challenge of reinstating the preoperative patellar thickness becomes particularly intricate in Asian patients, among whom patellae measuring less than 20 mm in thickness are prevalent [22, 23]. Therefore, it is advisable for manufacturers of TKA prosthesis to develop thinner patellar components to accommodate patients with smaller patellae. A previous study conducted by Jhurani et al. [24] reported a 2-year outcome associated with a thinner patellar button (measuring 6.2 mm). However, the mid-term and long-term implications of this button remains uncertain.
In this study, we have devised an algorithm based on pre-operative HSS PFA score and intra-operative cartilage wear for patients with patella size 21 mm or more. For all patellae of size less than 21 mm, we did patelloplasty alone irrespective of the grade of wear.
Our findings collectively contribute to comprehending the intricate interplay between preoperative variables, intraoperative assessments, and the decision-making process regarding selective patellar resurfacing within the context of osteoarthritis in total knee arthroplasty.
Algorithm for selective patellar resurfacing
With this algorithm, we can identify the patients who need patella resurfacing in primary TKA and a deliberate omission can be done when there is no indication. Its principal function is to offer guidance during the intraoperative phase concerning the decision of whether selective patellar resurfacing should be pursued.
From our analysis, it is clear that the prediction of the need for patellar resurfacing can be reliably accomplished using the HSS PFA score prior to surgery. However, the grade of patellar cartilage wear and patellar thickness is more important and the final decision regarding patellar resurfacing should be accomplished by integrating intraoperative evaluation. Hence, our findings regarding the predictive accuracy of HSS PFA score was consistent with that of Baldini et al. [6].
It is important to acknowledge the limitations of this study. The cohort size, though robust, may limit the generalizability of findings across diverse patient populations. Furthermore, the complexity of patellofemoral biomechanics necessitates ongoing research to refine the algorithm's predictive accuracy and scope. Prospective studies with larger cohorts and longer follow-up periods are warranted to validate and potentially refine the algorithm's performance.
Conclusion
In conclusion, the decision regarding patellar resurfacing in TKA remains complex and multifaceted. Selective resurfacing approach, guided by our algorithm based on HSS PFA score and intraoperative cartilage wear assessment, appear to offer a reasonable strategy to optimize clinical success and patient outcomes. Based on our results, we suggest evaluating the HSS PFA score before the surgery. If the score exceeds 50, we advise performing patella resurfacing in the presence of Grade IV wear intra-operatively. Conversely, if the score is below 50, we recommend patella resurfacing for Grade II, III, and IV wear.
The study's findings contribute to understanding the complex relationship between preoperative variables, intraoperative assessments, and the decision-making process for selective patellar resurfacing in total knee arthroplasty for patients with degenerative OA. HSS PFA score, could enhance the precision of clinical outcome assessments for TKA. This scoring system could serve as an additional source of information alongside the existing Knee Society Scoring System (KSS) and Oxford Knee Scores (OKS).
Data availability
All data supporting the findings of this study are available from corresponding author on reasonable request.
Declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tang X, He Y, Pu S, Lei L, Ning N, Shi Y, et al. Patellar resurfacing in primary total knee arthroplasty: A meta-analysis and trial sequential analysis of 50 randomized controlled trials. Orthopaedic Surgery. 2022;15(2):379–399. doi: 10.1111/os.13392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bourlez J, Canovas F, Duflos C, Dagneaux L. Are modern knee outcomes scores appropriate for evaluating patellofemoral degeneration in osteoarthritis? Evaluation of the ceiling and floor effects in knee outcomes scores. Orthopaedics & Traumatology, Surgery & Research. 2019;105(4):599–603. doi: 10.1016/j.otsr.2019.01.018. [DOI] [PubMed] [Google Scholar]
- 3.Bindelglass DF, Cohen JL, Dorr LD. Patellar tilt and subluxation in total knee arthroplasty: Relationship to pain, fixation, and design. Clinical Orthopaedics and Related Research. 1993;286:103–109. doi: 10.1097/00003086-199301000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Shih HN, Shih LY, Wong YC, Hsu RWW. Long-term changes of the nonresurfaced patella after total knee arthroplasty. The Journal of Bone and Joint Surgery - Series A. 2004;86:935–939. doi: 10.2106/00004623-200405000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Patel VV, Hall K, Ries M, Lindsey C, Ozhinsky E, Lu Y, Majumdar S. Magnetic resonance imaging of patellofemoral kinematics with weight-bearing. The Journal of Bone and Joint Surgery - Series A. 2003;85:2419–2424. doi: 10.2106/00004623-200312000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Baldini A, Anderson JA, Zampetti P, Pavlov H, Sculco TP. A new patellofemoral scoring system for total knee arthroplasty. Clinical Orthopaedics and Related Research. 2006;452:150–154. doi: 10.1097/01.blo.0000238847.34047.90. [DOI] [PubMed] [Google Scholar]
- 7.Gomes LSM, Bechtold JE, Gustilo RB. Patellar prosthesis positioning in total knee arthroplasty. A roentgenographic study. Clinical Orthopaedics. 1988;236:72–81. doi: 10.1097/00003086-198811000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Slattery C, Kweon C. Classifications in brief: Outerbridge classification of chondral lesions. Clinical Orthopaedics. 2018;476:2101. doi: 10.1007/s11999.0000000000000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Breugem SJM, Haverkamp D. Anterior knee pain after a total knee arthroplasty: What can cause this pain? World Journal of Orthopaedics. 2014;5(3):163–170. doi: 10.5312/wjo.v5.i3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cankaya D, Inci F, Bilekli AB, Karakus D, Kahve Y, Erdem Y. Patellar resurfacing in total knee arthroplasty leads to better isokinetic performance. Journal of Orthopaedic Science: Official Journal of the Japanese Orthopaedic Association. 2023;28(1):195–199. doi: 10.1016/j.jos.2021.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Grela M, Barrett M, Kunutsor SK, Blom AW, Whitehouse MR, Matharu GS. Clinical effectiveness of patellar resurfacing, no resurfacing and selective resurfacing in primary total knee replacement: Systematic review and meta-analysis of interventional and observational evidence. BMC Musculoskeletal Disorders. 2022;22(23):932. doi: 10.1186/s12891-022-05877-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parsons T, Al-Jabri T, Clement ND, Maffulli N, Kader DF. Patella resurfacing during total knee arthroplasty is cost-effective and has lower re-operation rates compared to non-resurfacing. Journal of Orthopaedic Surgery. 2021;11(16):185. doi: 10.1186/s13018-021-02295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen K, Dai X, Li L, Chen Z, Cui H, Lv S. Patellar resurfacing versus nonresurfacing in total knee arthroplasty: An updated meta-analysis of randomized controlled trials. Journal of Orthopaedic Surgery. 2021;16(1):83. doi: 10.1186/s13018-020-02185-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schiavone Panni A, Cerciello S, Del Regno C, Felici A, Vasso M. Patellar resurfacing complications in total knee arthroplasty. International Orthopaedics. 2014;38(2):313–317. doi: 10.1007/s00264-013-2244-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schindler OS. The controversy of patellar resurfacing in total knee arthroplasty: Ibisne in medio tutissimus? Knee Surgery, Sports Traumatology, Arthroscopy. 2012;20(7):1227–1244. doi: 10.1007/s00167-012-1985-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matharu, G. S., Blom, A. W., Venkatesh, R., Metcalfe, A. J., & Whitehouse, M. R. (2021). Patellar resurfacing practices in primary total knee replacement: A survey of BASK members. Knee, 28, A3–A5.
- 17.Fraser JF, Spangehl MJ. International rates of patellar resurfacing in primary total knee arthroplasty, 2004–2014. Journal of Arthroplasty. 2017;32(1):83–86. doi: 10.1016/j.arth.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 18.Vertullo CJ, Graves SE, Cuthbert AR, Lewis PL. The effect of surgeon preference for selective patellar resurfacing on revision risk in total knee replacement: An instrumental variable analysis of 136,116 procedures from the Australian Orthopaedic Association National Joint Replacement Registry. Journal of Bone and Joint Surgery. American Volume. 2019;101(14):1261–1270. doi: 10.2106/JBJS.18.01350. [DOI] [PubMed] [Google Scholar]
- 19.Reuben JD, McDonald CL, Woodard PL, Hennington LJ. Effect of patella thickness on patella strain following total knee arthroplasty. Journal of Arthroplasty. 1991;6:251–258. doi: 10.1016/S0883-5403(06)80172-5. [DOI] [PubMed] [Google Scholar]
- 20.Lee QJ, Yeung ST, Wong YC, Wai YL. Effect of patellar thickness on early results of total knee replacement with patellar resurfacing. Knee Surgery, Sports Traumatology, Arthroscopy. 2014;22:3093–3099. doi: 10.1007/s00167-014-3235-7. [DOI] [PubMed] [Google Scholar]
- 21.Matz J, Lanting BA, Howard JL. Understanding the patellofemoral joint in total knee arthroplasty. Canadian Journal of Surgery. 2019;62(1):57–65. doi: 10.1503/cjs.001617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim DK, Seo MC, Song SJ, Kim KI. Are Korean patients different from other ethnic groups in total knee arthroplasty? Knee Surgery and Related Research. 2015;27:199–206. doi: 10.5792/ksrr.2015.27.4.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hosseinzadeh, H. R. S., Tarabichi, S., Shahi, A. S., Yeganeh, M. H., Saleh, U. H., Kazemian, G. R., & Masoudi, A. (2013). Special considerations in Asian knee arthroplasty [Internet]. London: IntechOpen [cited 2013 Feb 20]. Available from: https://www.intechopen.com/books/arthroplasty-update/special-considerations-in-asian-knee-arthroplasty.
- 24.Jhurani A, Agarwal P, Aswal M, Saxena P, Singh N. Safety and efficacy of 62 mm patellar button in resurfacing less than 20 mm thin patella: A matched pair analysis. Knee Surgery and Related Research. 2018;30(2):153–160. doi: 10.5792/ksrr.17.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gharaibeh MA, Monk E, Chen DB, MacDessi SJ. Evaluation of the patellofemoral joint in total knee arthroplasty: Validation of the weight bearing merchant radiographic view. The Knee. 2018;25(6):1262–1271. doi: 10.1016/j.knee.2018.08.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data supporting the findings of this study are available from corresponding author on reasonable request.





