Keywords: psychometrics, depression, Indigenous, culturally competent care, cross-cultural psychiatry
Abstract
Cultural adaptation of psychometric measures has become a process aimed at increasing acceptance, reliability, and validity among specific Indigenous populations. We present a systematic scoping review to: (1) identify the depression scales that have been culturally adapted for use among Indigenous populations worldwide, (2) globally report on the methods used in the cultural adaptation of those scales, and (3) describe the main features of those cultural adaptation methods. We included articles published from inception to April 2021, including 3 levels of search terms: Psychometrics, Indigenous, and Depression. The search was carried out in the Ovid Medline, PubMed, Embase, Global Health, PsycINFO, and CINAHL databases, following PRISMA guidelines. We identified 34 reports on processes of cultural adaptation that met the criteria. The scales were adapted for use among Indigenous populations from Africa, Australia, Asia, North America, and Latin America. The most common scales that underwent adaptation were the Patient Health Questionnaire (PHQ-9), the Center for Epidemiologic Studies Depression Scale (CES-D), and the Edinburgh Postnatal Depression Scale (EPDS). Methods of adaptation involved a revision of the measures’ cultural appropriateness, standard/transcultural translation, revision of the administration process, and inclusion of visual supports. Culturally safe administration of scales was reported in some studies. To come to a consensus on most appropriate methods of improving cultural safety of psychometric measurement, most studies utilized qualitative methods or mixed methods to understand the specific community’s needs. Revision of linguistic equivalence and cultural relevance of content, culturally safe administration procedures, qualitative methods, and participatory research were key features of developing safe culturally adapted measures for depressive symptoms among Indigenous populations. While for comparability, uniform scales would be ideal as mental health evaluations, an understanding of the cultural impact of measurements and local depression expressions would benefit the process of developing culturally sensitive psychometric scales. PROSPERO registration ID: CRD42023391439.
Impact statement
Language, context, and methods of administrating psychiatric evaluations may hinder timely and accurate depression evaluation of Indigenous peoples, which may delay or prevent treatment. A potential strategy to close this gap is to develop new or culturally adapted scales that are more sensitive to detecting culturally specific expressions of mental health. While several structured instruments exist to describe methods and phases of adaptation, it remains open how commonly methods of adaptation are used and reported. In this research, we review original work representing all continents and report on the global evidence on the types of adapted scales for use with Indigenous peoples, their qualities, and their methods of adaptation. This is hoped to form a basis for future work in identifying suitable scales for adaptation, and in developing, adapting, and creating culturally sensitive psychometrics for treatment of major depression disorder. Given the need for equal access to safe mental health services for all population groups, it remains to be defined when a culturally safe administration of a standard scale is preferable, when there is a need to invest in a translation or a cultural adaptation of a scale, and to what extent visual supports can complement verbal measurement. This summary of findings on successfully adapted scales as well as acceptance of items in specific scales can support clinicians who need to choose a safe measure for assessing patients from different cultures. Moreover, the importance of inclusion of community members in the process of selecting and adapting the psychometric scales should be recognized in research and clinical work.
Introduction
Indigenous peoples have originally inhabited several geographical regions and formed values, languages, and strong links to these territories. Indigenous people number about 400 million worldwide, belonging to five thousand diverse groups living in more than 90 countries (Indigenous Peoples, 2023; United Nations, 2023). As a result of imperialism and colonialism, the health of Indigenous peoples worldwide is characterized by systematic inequities in health outcomes (Reid et al., 2019). They have experienced varying degrees of racial discrimination and social oppression, evident as health and social marginalization in regard to education, housing, employment, and access to adequate social and health services (Frohlich et al., 2006). It is an alarming fact that such health disparities are still predominant to this day. This is well illustrated by the higher prevalence and morbidity/mortality rate of mental health conditions and suicide among Indigenous people, up to 20 times higher than the general population (Hajizadeh et al., 2019). This emphasizes the need for providing efficient and accessible mental health care, among other procedures, to improve Indigenous populations’ resilience (Davy et al., 2016), and calls for a decolonization of psychological practices (Smallwood et al., 2023). Ensuring the equal accessibility of mental health services requires more than easy reach services; it requires examination of barriers and racist and colonial practices and then implementation of culturally appropriate mental health services (Davy et al., 2016; National Collaborating Centre for Aboriginal Health, 2019).
Accessibility of medical care is traditionally dependent on formal diagnoses by conventional psychiatric professionals. Yet, the traumatic history of colonization has negatively impacted Indigenous populations’ help seeking behavior, trust, and acceptance of Western psychiatric treatment (Chachamovich et al., 2015). Unfortunately, delayed efforts and unfruitful cooperation are common in screening and treating mental health (Leung, 2016). Furthermore, Indigenous people share values and historical experiences that influence their expression of symptoms of depression – cultural expressions not represented in the biomedical conceptualization of psychiatric disorders (Kleinman, 1977; Kirmayer et al., 2008; Nichter, 2010). Use of colonializers’ language and structural barriers have hindered access to good quality mental health and social services (Montreal Urban Aboriginal Health Needs Assessment, 2012). Without adequate levels of cultural safety embedded in current psychiatric practice (e.g., cultural awareness, cultural sensitivity, and cultural competency), there is limited timely and effective response to depression among the Indigenous (Brascoupé and Waters, 2009; Darroch et al., 2017).
Access to psychiatric care is based on diagnostic categories; for example, severe depression is characterized by the symptoms that decrease the ability to function (Aboraya et al., 2018). The ‘gold-standard’ method of psychiatric diagnosis is clinical interviews, where the delivery is through human interaction. However, Indigenous communities, especially remote groups, typically have limited access to personnel with specialized skills (Boksa et al., 2015). To overcome this barrier, screening for psychiatric disorders can be completed through psychometric measures in primary care to guide decision-making in treatment. In instances where psychiatric services are not easily accessible, psychometric measures may be used during follow-ups to detect relapse, and inform self-management and therapeutic interventions (Boksa et al., 2015). The organizational and political need for accurate measurement of a population’s mental health increases when there is a need to allocate resources, plan service, or to improve quality of treatment.
If initial contact for mental health evaluation and treatment includes completing a psychometric screen, it is essential to confirm that this method of evaluation is culturally acceptable. Currently, most available instruments are based on the Diagnostic and Statistical Manual-5 (DSM-5), which was developed based on the literature and contribution of subject experts predominantly from Western societies. Additionally, as the DSM-5 was developed for use in the context of Western psychiatric practices, it does not capture the global expression of mental health conditions (Kleinman, 1977; Haroz et al., 2017). Simultaneously, calls for cultural safety in health care education and services and concurrent adaptation of measures for assessing psychiatric symptoms in Indigenous populations have been made (Brascoupé and Waters, 2009; Baba, 2013; Darroch et al., 2017).
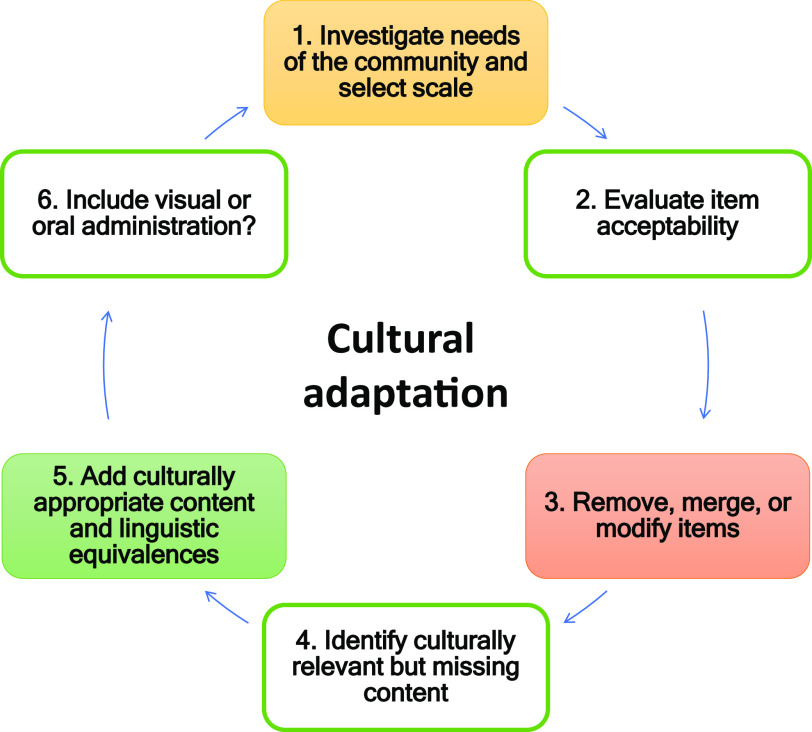
The cultural adaptation of assessment tools has improved acceptance, response rate, and reliability of measures (Arafat et al., 2016; Kral, 2016; Hackett et al., 2019). There has been work on guidelines for the process of cross-cultural adaptations (Beaton et al., 2000; Chávez and Canino, 2005; Sousa and Rojjanasrirat, 2011; Arafat et al., 2016). This process generally involves modifications of instruments with the aim of making them more suitable for a specific population (Wexler et al., 2017; Haroz et al., 2017; Wiltsey Stirman et al., 2019). However, global consensus on guidelines and evaluation criteria for cultural adaptation is not available, and actually used methods remain open.
In this paper, we present a scoping review to synthesize the literature on cultural adaptations of depression measures among Indigenous populations. The rationale of this study is based specifically on a problem identified during the course of our participatory research with Indigenous populations – a critical Indigenous view on conventional, symptom-focused psychometrics (Gomez Cardona et al., 2021). The main objectives of this review were to: (1) identify the depression scales that have been culturally adapted for use among Indigenous populations worldwide, (2) report the methods used in the cultural adaptation of those scales, and (3) describe the main features of used cultural adaptation methods.
Methods
Study design
We conducted a systematic scoping review, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension for Scoping Reviews (PRISMA-ScR) guidelines for scoping reviews (Tricco et al., 2018). The PRISMA-ScR checklist provides a systematic process for reporting title, abstract, introduction, methods, results, discussion, and funding (Tricco et al., 2018). A systematic scoping review design was chosen as this allowed us to present an overview of a large and diverse body of literature pertaining to the broad topic of screening for Indigenous mental health, while carrying out a systematic approach to answering focused objectives.
Search strategy
We used three levels of search terms, which included terminology for depression, psychometrics, and Indigenous (Supplement 1). We searched Ovid Medline, PubMed, PsycINFO, Embase, CINAHL, and Global Health databases for original research articles published between inception of the databases to April 2021. Gray literature searches were complemented through hand-searching on Google Scholar, open access repositories and the reference lists of selected articles. Study researchers (MY, QS) and a librarian created the search strategy and conducted the search. Citations of the search results were uploaded to a citation manager, and the library of references was accessible to all co-authors. The original search was conducted in July 2019, and supplemented by an updated systematic search in April 2021, under the guidance of a McGill University librarian.
Operationalization of search terms
We operationalized the term Indigenous as the original habitants of colonized geographical regions (e.g., European colonization) who have cultural characteristics (e.g., values, languages, strong links to territories) distinct from the dominant societies, self-identify as Indigenous/Aboriginal peoples, and live in their country of origin (United Nations, 2023). However, where possible and to be respectful, we use the terms specified by the specific Nation. We considered cultural adaptation of scales in the form of questionnaires, surveys, or self-reports in culturally distinct populations. Cultural adaptation was operationalized as modifications to increase cultural sensitivity, not solely through – but including – the use of translation. Depression was operationalized in this study as psychological distress or clinical major depression. The search term psychometrics included rating scales, measures, questionnaires, indices, and other related terms and concepts. The final search was confirmed with a professional from the McGill University library.
Study selection
At least two researchers participated independently in each stage of article screening and full-text selection from which we calculated agreement coefficient (kappa = 0.71, substantial; McHugh, 2012). We included studies that adapted standard validated psychometric measures for depression. We searched for articles that were published in English, as this ensured that we included uniform descriptions of adaptation processes in order to synthesize findings. Articles were included if they (1) were a primary source study, (2) included depression measures, (3) described and/or mentioned the cultural adaptation or validation process of an adapted scale, and (4) had an Indigenous population as its target population. Articles were excluded if (1) they did not include information about the cultural adaptation of a scale, (2) they did not specify the Indigenous identity of the population, (3) they presented adapted scales for non-Indigenous populations, (4) adaptations were done to a scale focused on symptomology unrelated to depression, or (5) they were conference abstracts or poster submissions. The only exception is a protocol for an included adaptation study as it provided supportive information (e.g., cultural adaptation methods) and further context for the full study. The final inclusion and exclusion of full-text articles was confirmed by the first author (LGC).
Data collection process and data items
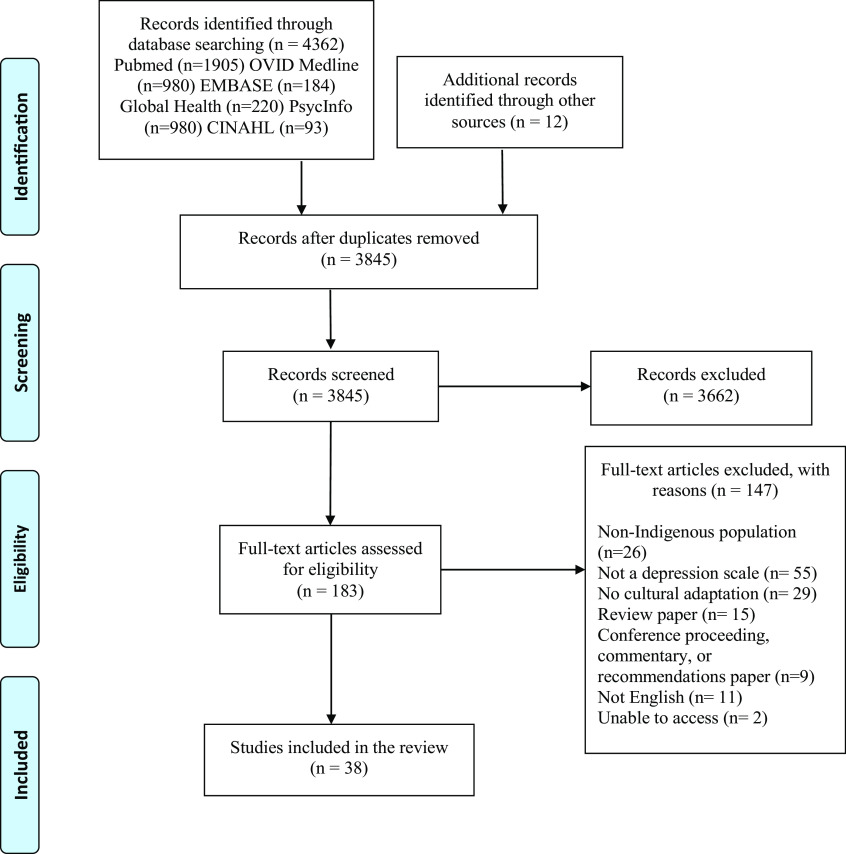
Authors systematically and blindly searched for and screened articles (MY, QS, MK, GV, VN, OL). The inclusion of articles followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension for Scoping Reviews (PRISMA-ScR) guidelines (Tricco et al., 2018) (Figure 1). Data from the selected articles were extracted and summarized by authors (MY, QS, MK, GV, VN) in two tables. Table 1 includes author(s), publication year, study objectives, setting and location of the research, study methods, language in which the scale was presented, population, sample size, and ethnic identity. Table 2 includes methods of cultural adaptation and the main modifications made to the scales. Following a comprehensive data extraction, we conducted a qualitative and narrative synthesis of the themes by collating, summarizing, and reporting on prominent ideas and concepts from the literature data (Arksey and O’Malley, 2005).
Figure 1.
Flowchart of search and screening process.
Table 1.
Characteristics of studies
| Measurement | Authors | Study objective(s) | Setting/Context | Location | Language | Study methods | Population | Indigenous group | Sample size |
|---|---|---|---|---|---|---|---|---|---|
|
Ashaba et al. (2019) |
|
|
|
|
|
|
|
|
|
Armenta et al. (2014) |
|
|
|
|
|
|
|
|
|
Baron et al. (2017) |
|
|
|
|
|
|
|
|
|
Chapleski et al. (1997) |
|
|
|
|
|
|
|
|
|
Kilburn et al. (2018) |
|
|
|
|
|
|
|
|
|
Harry and Crea (2018) |
|
|
|
|
|
|
|
|
|
Andersen et al. (2015) |
|
|
|
|
|
|
|
|
|
Chapla et al. (2019) |
|
|
|
|
|
|
|
|
|
Tiburcio Sainz and Natera Rey (2007) |
|
|
|
|
|
|
|
|
|
Kaaya et al. (2008) |
|
|
|
|
|
|
|
|
|
Bowen and Muhajarine (2006) |
|
|
|
|
|
|
|
|
|
Campbell et al. (2008) |
|
|
|
|
|
|
|
|
|
Ekeroma et al. (2012) |
|
|
|
|
|
|
|
|
|
Fernandes et al. (2011) |
|
|
|
|
|
|
|
|
|
Bass et al. (2008) |
|
|
|
|
|
|
|
|
|
Schneider et al. (2015) |
|
|
|
|
|
|
|
|
|
Ganguli et al. (1999) |
|
|
|
|
|
|
|
|
|
Sarkar et al. (2015) |
|
|
|
|
|
|
|
|
|
Haroz et al. (2014) |
|
|
|
|
|
|
|
|
|
Haroz et al. (2017) |
|
|
|
|
|
|
|
|
|
Bougie et al. (2016) |
|
|
|
|
|
|
|
|
|
Mitchell and Beals (2011) |
|
|
|
|
|
|
|
|
|
Australian Institute of Health and Welfare (2009); McNamara et al. (2014) |
|
|
|
|
|
|
|
|
|
Almeida et al. (2014) |
|
|
|
|
|
|
|
|
|
Marley et al. (2017) |
|
|
|
|
|
|
|
|
|
Denckla et al. (2017) |
|
|
|
|
|
|
|
|
|
Brown et al. (2013) |
|
|
|
|
|
|
|
|
|
Hackett et al. (2016); Hackett et al. (2019) |
|
|
|
|
|
|
|
|
|
Esler et al. (2007); Esler et al. (2008) |
|
|
|
|
|
|
|
|
|
Schantz et al. (2017) |
|
|
|
|
|
|
|
|
|
Gallis et al. (2018) |
|
|
|
|
|
|
|
|
|
Gelaye et al. (2013) |
|
|
|
|
|
|
|
|
|
Husain et al. (2006) |
|
|
|
|
|
|
|
|
|
Caneo et al. (2020) |
|
|
|
|
|
|
|
|
Beck Depression Inventory-II (BDI-II), and Hopkins Symptom Check List (HSCL).
Center for Epidemiologic Studies Depression Scale – 20 items (CES-D-20).
Center for Epidemiologic Studies Depression Scale – 10 items (CES-D-10).
Center for Epidemiologic Studies Depression Scale– 12 items (CES-D-12) and Center for Epidemiologic Studies Depression Scale– 20 items (CES-D-20).
Center for Epidemiologic Studies Depression Scale – 10 items (CES-D-10).
Center for Epidemiologic Studies Depression Scale – 19 items (CES-D-19).
Center for Epidemiologic Studies Depression Scale (CES-D).
Center for Epidemiologic Studies Depression Scale for Children (CES-DC).
Coping Questionnaire (CQ), Symptom Rating Test (SRT), and Depression Scale Center for Epidemiological Studies (CES-D).
Dar-es-Salaam Symptom Questionnaire (DSQ).
Edinburgh Postnatal Depression Scale (EPDS).
Edinburgh Postnatal Depression Scale (EPDS).
Edinburgh Postnatal Depression Scale (EPDSc).
Edinburgh Postnatal Depression Scale (EPDS), Kessler Psychological Distress Scale (K-10).
Edinburgh Postnatal Depression Scale (EPDS), Hopkins Symptom Checklist (HSCL-D).
Functioning Assessment Instrument (FAI), World Health Organization’s Disability Assessment Schedule (WHODAS).
Hindi version of the Geriatric Depression Scale (GDS-H).
Geriatric Depression Scale – 15 items (GDS-15).
Hopkins Symptom Checklist Depression Scale (HSCL-25).
International Depression Symptom Scale-general (IDSS-G).
Kessler Psychological Distress Scale – 10 items (K-10).
Kessler Psychological Distress Scale – 6 items (K-6).
Kessler Psychological Distress Scale – 5 items (K-5).
Kimberley Indigenous Cognitive Assessment of Depression (KICA-dep).
Kimberley Mum’s Mood Scale (KMMS).
Ndetei–Othieno–Kathuku Scale (NOK).
Patient Health Questionnaire – 9 items (PHQ-9).
Patient Health Questionnaire – 16 items (PHQ-16).
Patient Health Questionnaire – 10 items (PHQ-10).
Patient Health Questionnaire – 8 items (PHQ-8).
Patient Health Questionnaire – 9 items (PHQ-9).
Patient Health Questionnaire – 9 items (PHQ-9).
Patient Health Questionnaire – 9 items (PHQ-9).
Patient Health Questionnaire – 2 items (PHQ-2).
Table 2.
Process of cultural adaptation
| Measurement scale | Authors | Methods | Modifications |
|---|---|---|---|
|
Ashaba et al. (2019) |
|
Items Added: ‘having many thoughts’, ‘being desperate’, ‘loss of hope’, ‘self-hatred’, ‘weight loss’, ‘loneliness’, ‘anger’, ‘uselessness’, ‘lack of confidence’, ‘forgetfulness’, ‘lack of peace’, ‘frustration with life’, ‘feeling stressed’, ‘suicidal thoughts’ Items Removed: changes in sleeping patterns, appetite, and/or sexual interest Item Modification:
|
|
Armenta et al. (2014) |
|
Conceptual: recommendation to review notion of loneliness Items Added: recommendation to add somatic difficulties items Items Removed: potential inadequacy of the question ‘I felt everything I did was an effort’ |
|
Baron et al. (2017) |
|
Conceptual: caution about conceptualizing question about hopefulness as a positive affect concept Organizational: reordering the questions, from positive to negative |
|
Chapleski et al. (1997) |
|
Items Removed: concerning interpersonal factors |
|
Kilburn et al. (2018) |
|
Item Removed: recommendation to review the question ‘everything was an effort’ Items Added: Recommendation to include an additional somatic element Conceptual: ‘Hopeful’ may not perfectly align with the conceptualization of positive affect |
|
Harry and Crea (2018) |
|
Items Added: ‘you felt that life was not worth living’ Semantic: pronoun ‘I’ was changed to ‘you’ Response categories change: ‘never or rarely’, ‘sometimes’, ‘a lot of the time’, ‘most of the time/all of the time’ Item Modification:
|
|
Andersen et al. (2015) |
|
Conceptual:
|
|
Chapla et al. (2019) |
|
Semantic/Conceptual: evaluation of the semantic and content equivalence of the scale (details were not reported) |
|
Tiburcio Sainz and Natera Rey (2007) |
|
Semantic:
|
|
Kaaya et al. (2008) |
|
Items added: addition of 30 local idioms for depression and anxiety |
|
Bowen and Muhajarine (2006) |
|
Items Added:
|
|
Campbell et al. (2008) |
|
Semantic changes: alteration of some words and simplification of sentence structures Item Modification:
|
|
Ekeroma et al. (2012) |
|
|
|
Fernandes et al. (2011) |
|
|
|
Bass et al. (2008) |
|
Item Removed:
|
|
Schneider et al. (2015) |
|
Items Added:
|
|
Ganguli et al. (1999) |
|
Item Modification: the item asking whether the individual found life to be exciting was altered to substitute ‘very enjoyable’ |
|
Sarkar et al. (2015) |
|
Not reported |
|
Haroz et al. (2014) |
|
Items Added:
|
|
Haroz et al. (2017) |
|
Items Added: addition of 16 questions on symptoms such as: crying, lonely, social withdrawal, worry, worthless, headaches, stomachaches, general aches and pain, anger, thinking too much, confused, heart weakness, palpitations, heavy heart, heart pain Semantic: participants found items ‘feeling weakness in your heart’ and ‘feeling as though your heart was heavy’ difficult to understand |
|
Bougie et al. (2016) |
|
Not reported |
|
Mitchell and Beals (2011) |
|
Not reported |
|
Australian Institute of Health and Welfare (2009); McNamara et al. (2014) |
|
Item Removed: ‘feel worthless’ was found to be offensive and omitted Semantic: word changes to items to improve their understanding:
|
|
Almeida et al. (2014) |
|
Item modification:
|
|
Marley et al. (2017) |
|
Semantic: rewording of the questions (no further details) |
|
Denckla et al. (2017) |
|
Items Added: 33-items: ‘How much were you distressed by’: ‘feeling as if insects or ants are crawling under your skin’, ‘feeling your heart has fallen down’, ‘feeling a pressure on the top of your head’, ‘getting frequent attacks of malaria’, ‘often having pain in your bones’, ‘feeling your heart is heavy’. |
|
Brown et al. (2013) |
|
Semantic: questions were rephrased Item Modification: certain items were confusing and separated into two elements: ‘psychomotor’, ‘appetite changes’ |
|
Hackett et al. (2016); Hackett et al. (2019) |
|
Items Added: inclusion of seven additional questions assessing: ‘anger’, ‘weakened spirit’, ‘homesickness’, ‘irritability’, ‘excessive worry’, ‘rumination’, ‘drug/alcohol use’ |
| PHQ-10 29 | Esler et al. (2007); Esler et al. (2008) |
|
Semantic: modification of the wording of some questions Items Added: inclusion of one question pertaining to anger (a culturally specific symptom of depression) |
|
Schantz et al. (2017) |
|
Items removed: exclusion of one question about suicide Pragmatic: caution about question ‘difficulty concentrating in reading’ because it is not sensitive to low literacy |
|
Gallis et al. (2018) |
|
Semantic: some difficult Urdu words were replaced by simpler and more frequently used words carrying the same meaning |
|
Gelaye et al. (2013) |
|
Semantic: ensure proper expression and conceptualization of terminologies in local contexts Items added: one additional item (#10) assessing functional impairment |
|
Husain et al. (2006) |
|
Items removed: Psychosexual items in the interview had to be omitted in most female interviews |
|
Caneo et al. (2020) |
|
Not reported |
Beck Depression Inventory-II (BDI-II), and Hopkins Symptom Check List (HSCL).
Center for Epidemiologic Studies Depression Scale– 20 items (CES-D-20).
Center for Epidemiologic Studies Depression Scale – 10 items (CES-D-10).
Center for Epidemiologic Studies Depression Scale– 12 items (CES-D-12) and Center for Epidemiologic Studies Depression Scale– 20 items (CES-D-20).
Center for Epidemiologic Studies Depression Scale – 10 items (CES-D-10).
Center for Epidemiologic Studies Depression Scale – 19 items (CES-D-19).
Center for Epidemiologic Studies Depression Scale (CES-D).
Center for Epidemiologic Studies Depression Scale for Children (CES-DC).
Coping Questionnaire (CQ), Symptom Rating Test (SRT), and Depression Scale Center for Epidemiological Studies (CES-D).
Dar-es-Salaam Symptom Questionnaire (DSQ).
Edinburgh Postnatal Depression Scale (EPDS).
Edinburgh Postnatal Depression Scale (EPDS).
Edinburgh Postnatal Depression Scale (EPDS).
Edinburgh Postnatal Depression Scale (EPDS), Kessler Psychological Distress Scale (K-10).
Edinburgh Postnatal Depression Scale (EPDS), Hopkins Symptom Checklist (HSCL-D).
Functioning Assessment Instrument (FAI), World Health Organization’s Disability Assessment Schedule (WHODAS).
Hindi version of the Geriatric Depression Scale (GDS-H).
Geriatric Depression Scale – 15 items (GDS-15).
Hopkins Symptom Checklist Depression Scale (HSCL-25).
International Depression Symptom Scale- General (IDSS-G).
Kessler Psychological Distress Scale – 10 items (K-10).
Kessler Psychological Distress Scale – 6 items (K-6).
Kessler Psychological Distress Scale – 5 items (K-5).
Kimberley Indigenous Cognitive Assessment of Depression (KICA-dep).
Kimberley Mum’s Mood Scale (KMMS).
Ndetei–Othieno–Kathuku Scale (NOK).
Patient Health Questionnaire – 9 items (PHQ-9).
Patient Health Questionnaire – 16 items (PHQ-16).
Patient Health Questionnaire – 10 items (PHQ-10).
Patient Health Questionnaire – 8 items (PHQ-8).
Patient Health Questionnaire – 9 items (PHQ-9).
Patient Health Questionnaire – 9 items (PHQ-9).
Patient Health Questionnaire – 9 items (PHQ-9).
Patient Health Questionnaire – 2 items (PHQ-2).
Results
Selection of sources of evidence
We identified 3,845 unique articles from the search (following de-duplication) and screened for their titles/abstracts in the first phase. Then, we identified 183 full texts and assessed for eligibility; of these, 37 articles met our inclusion criteria (Chapleski et al., 1997; Ganguli et al., 1999; Bowen and Muhajarine, 2006; Husain et al., 2006; Esler et al., 2007, 2008; Tiburcio Sainz and Natera Rey, 2007; Bass et al., 2008; Campbell et al., 2008; Kaaya et al., 2008; Australian Institute of Health and Welfare, 2009; Fernandes et al., 2011; Mitchell and Beals, 2011; Ekeroma et al., 2012; Brown et al., 2013; Gelaye et al., 2013; Almeida et al., 2014; Armenta et al., 2014; Haroz et al., 2014, 2017; McNamara et al., 2014; Andersen et al., 2015; Sarkar et al., 2015; Schneider et al., 2015; Bougie et al., 2016; Hackett et al., 2016, 2019; Baron et al., 2017; Denckla et al., 2017; Marley et al., 2017; Schantz et al., 2017; Gallis et al., 2018; Harry and Crea, 2018; Kilburn et al., 2018; Ashaba et al., 2019; Chapla et al., 2019; Caneo et al., 2020). Finally, there were 3 cases where the same research team produced two manuscripts detailing adaptation processes; this yielded 34 original reports of cultural adaptation processes included in this review.
Characteristics of the scale measures with a cultural adaptation (Table 1)
In a total of 34 reports of cultural adaptation processes, there were 41 different depression scales adapted (Table 1). The Indigenous groups of the studies were native to Canada or the United States (6/34), Latin America (3/34), Asia (8/34), Africa (9/34), and Australia or New Zealand (8/34). The most commonly adapted scales included the Patient Health Questionnaire (PHQ-9), the Center for Epidemiologic Studies Depression Scale (CES-D), and the Edinburgh Postnatal Depression Scale (EPDS).
Methods of scale modifications
Revision of cultural relevance and transcultural translation
The cultural relevance of the measurement scales, in addition to the linguistic equivalence (language translation), was verified in 19/34 cultural adaptations (Table 2). An example of such a process was asking Indigenous women about the most relevant tasks and activities related to taking care of themselves, their families, and taking care of and participating in the community. The researchers subsequently translated the mentioned categories and constructed a new instrument with items based off the need to cover sufficient domains of functioning.
Some studies spoke more explicitly about transcultural translation, which was described as a process of understanding the meaning of phrases and ensuring that translation maintains cultural nuances. In all these cases, the researchers used qualitative methods to gain insight into the questions and responses presented in the tools and their relevance from the sociocultural point of view of the target population. Participatory qualitative methods were another common characteristic of adaptation processes. This was done in all studies, including through consultations with the Indigenous community focus groups (4/34), qualitative interviews with key community informants (11/34), and or a participatory action research process (1/34) (Table 2). Furthermore, three studies used mixed methods, combining the use of surveys with interviews.
A trend shown by the studies was that significant engagement between researchers/practitioners and Indigenous community members is needed in the process of revising cultural relevance of depression scales. For example, in the cultural adaptation of the Patient Health Questionnaire (PHQ-9) with Indigenous Australian people, focus groups were conducted (Brown et al., 2013). This required the interplay of feedback from bilingual experts and acceptance testing through discussions with community members. The translators, research team members, and Indigenous members discussed the translations to provide linguistic and conceptual equivalences of the adapted scale items, reviewed the difficult items, and identified ways to achieve semantic and cultural equivalence. This process resulted in a modification of words and phrases, as well as division of one initial question into two items that were more precise (e.g., psychomotor changes and appetite changes). Also, seven key features of depression not covered by the standard PHQ-9 but relevant for the local population were identified and added: anger, homesickness, irritability, excessive worry, weakened spirit, drug/alcohol use, and rumination.
Following the involvement of experts and the community to identify needs, different depression scales were adapted in a variety of ways to increase acceptance of their content and use by the Indigenous group, which improves cultural safety. In studies where items were added, the goal was often to incorporate local idioms of distress or of functioning. For example, the most common somatic symptoms (e.g., ‘fatigue’) or positive affect concepts (e.g., ‘hopefulness’) items were added (Baron et al., 2017; Kilburn et al., 2018). Research teams also used a deletion method to remove items perceived as culturally inappropriate or irrelevant to the local constructs of depression. For example, older Australian Aboriginal people perceived the question on the original Kessler Psychological Distress Scale (K-5) concerning feelings of worthlessness as offensive (McNamara et al., 2014). Accordingly, some items about suicidal ideation were subsequently excluded to respect the local sociocultural codes (Gelaye et al., 2013; Schantz et al., 2017). Similarly, the suicidal ideation item was separated into two questions in another study: Have you had thoughts that you would be better off dead? and Have you thought of hurting yourself? (Almeida et al., 2014). Thus, the desire of the community was most important when considering including questions about suicide in depression measures.
Other than through sole use of qualitative methods, some studies adapted scales using quantitative methods. Following interviews with mothers, Bass et al. (2008) compiled a list of identified postpartum symptoms and statistically regressed them on mental health constructs that comprised the measure (Bass et al., 2008). Through this, the authors identified relevant depression-like problems that were meaningful based on both phenomenological insight and objective validation. Subsequently, they reviewed standard post-partum depression screens to identify those that best reflected the local descriptions. Based on this work, they selected, translated, and adapted the EPDS and the Hopkins Symptom Checklist depression section (HSCL-D). This involved adding new questions associated with signs and symptoms that were not part of the original screens but were described by the interviewees.
Language translation
Translation to the respective Indigenous language was completed in 14/34 scales (Table 2). In general, these translations followed a rigorous protocol, informed by guidelines and examples set forth by experts in psychiatry or experts in the field of linguistics (Ganguli et al., 1999; Brown et al., 2013; Almeida et al., 2014). Most translations were done by professional translators with recognized experience in psychiatry; in two cases, non-native translators were fluent in both the original scale language and the Indigenous language (Easton et al., 2017; Schantz et al., 2017). Additionally, the first translated version of certain tools was completed in a blinded manner and through back-translation (14/14). When discrepancies arose, the researchers turned to mental health experts to define the most accurate translation (9/14).
Following a direct transcultural translation, some scale items needed to be rewritten for grammatic purposes. This necessitated reformulation of items (2/14), addition of items (2/14), removal of items (2/14), changes to the order of questions (1/14), and recommendations regarding the wording of items (5/14). To assist in this, some studies compiled a list of Indigenous symptoms or expressions of distress that could be useful for screening for depression. This information was collected through qualitative methods including interviews (4/14) and use of interpreters (1/14). An example of a language translation process is reported by Ganguli et al. (1999). They translated the Geriatric Depression Scale (GDS), originally written in English, into the local Haryanvi dialect of Hindi through a standard approach of iterative back-translation by bilingual clinicians (Ganguli et al., 1999). The researchers also made minimal modifications to the content of the tool to improve cultural appropriateness. The question regarding whether the person found life to be ‘exciting’ was modified to ‘very enjoyable’, as the concept of older people feeling ‘excited’ was found to not be appropriate in rural India. The adapted scale was named the Geriatric Depression Scale-Hindi version (GDS-H).
Visual scales
One study developed a visual scale to accompany the original numerical Likert scale (Marley et al., 2017). In this study, the Kimberley Mum’s Mood Scale (KMMS) was adapted to fit the needs of pregnant and postpartum Indigenous women in Australia. The qualitative methodology relied on multiple focus groups for input on appropriate visual representations, wording, and a protocol for administration of the tool. The resulting visual scale included a water glass pictorial to distinguish different multiple-choice responses, pictographs, and a visual analogue scale comprised of degrees of facial expression indicating valence and magnitude of emotions.
Scale administration
Increasing cultural safety and sensitivity at administration of the scale was often the aim of the studies’ adaptation processes. The context of use as well as the scale administration process were considered by three studies (Table 2). Some authors tried to improve the acceptability, reliability, and utility of the scales, and explored impact of the administration process on this. Increasing acceptability of the tool by the Indigenous community was described as being the process whereby adapted tools were considered sufficiently culturally safe, non-judgmental, and could provide providers with valuable insights into participants’ lived experiences and social, emotional, and cultural well-being. Increasing acceptability also supports the validity of the scale, which is the accuracy of the tool for measuring constructs of depression that align with the Indigenous’ conceptualizations of it.
Esler et al. (2007) investigated attitudes toward depression screening and the components of the PHQ-9 among members of an urban Indigenous community in Australia (Esler et al., 2007). Some focus group participants suggested that involving a family member in the assessment process may improve the accuracy of the screening while other participants shared the opposite point of view. Most participants stated they would prefer an Indigenous health worker as interviewer. Equally, familiarity with the Indigenous community-controlled health service was considered to contribute to the acceptance of the administration of the tool. The need for an initial trusting relationship between the patient and the tool administrator was noted as being particularly important.
In Marley et al.’s (2017) adaptation of the KMMS, the study team created a culturally safe space to conduct the screen with the Indigenous women (Marley et al., 2017). They incorporated a guided questionnaire that allowed the women participants to describe their history in detail, making it easier for researchers and clinicians to identify protective and vulnerability factors. The authors also developed culturally safe training modules for staff administering the tool. Resultingly, the majority of participants reported that completing the KMMS was highly useful and better than the standard instrument (EPDS), as it increased mutual respect, trust, and understanding between the personnel and the participants.
Discussion
We identified 34 reports on cultural adaptation processes including 41 different depression scales. The most commonly adapted scales included the Patient Health Questionnaire (PHQ-9), the Center for Epidemiologic Studies Depression Scale (CES-D), and the EPDS. The review found that cultural adaptation of depression scales is more of an exception than a rule; only 34 reported cultural adaptations were identified, yet the estimated global number of Indigenous groups is over 5,000 (United Nations, 2023). Geographically, the cultural adaptations were mostly conducted in Africa, Australia, and Asia. This finding is consistent with the geographic dispersion of Indigenous populations, as approximately 70% of Indigenous populations live in Asia and the Pacific, 16.3% in Africa, 11.5% in Latin America and the Caribbean, 1.6% in North America, and 0.1% in Europe and Central Asia (Jamil Asilia Centre, 2021). This shows a heightened need for attention to recognizing importance of cultural safety in mental health care for Indigenous populations of these areas.
Four main processes of utilized cultural adaptation of depression scales were identified. The most commonly used non-exclusive methods were revision of cultural appropriateness or transcultural psychiatry, language translation, modifications of the administration process, and complementary visual scales. Most importantly, the approach chosen depended on the context of administration and the specific clinical or research issues to address. Cultural adaptations to scales could increase cultural safety and response rate of psychometrics; however, it remains open when it is appropriate to consider conducting a translation or further cultural adaptation. A careful, shared needs assessment is important before cultural adaptations, given the intensive use of Indigenous resources in the adaptation process.
Importance of cross-cultural translation
Studies found that a rigorous translation of the tool into the native language was important, since the language is a significant identity marker for the community members. As compared to literal equivalence in traditional translation, the main challenges in cultural translation are the complexity of local semantics and the need to guarantee conceptual equivalence, criterion equivalence, and content equivalence (Ghimire et al., 2013). The success of translation processes necessitates several steps and good resources: (1) establishment of a bilingual group of experts, (2) examination of conceptual composition by the experts, (3) translation by an expert, (4) examination of the translation by the experts, (5) examination of the translation by a group representative of the population, (6) blind back-translation by another expert, (7) examination of the blind back-translation by the experts and adjustment of discrepancies, (8) a pilot study to test the tool among the population, and (9) adjustments based on pilot study results (Sartorius and Janca, 1996; Beaton et al., 2000; Sousa and Rojjanasrirat, 2011; Arafat et al., 2016). This process can last up to several months and constitutes the most simple and economical form of adaptation processes.
Importance of qualitative methods
Confirming that a cultural adaptation process is successful and useful to the population is important to support its use (Wiltsey Stirman et al., 2019). In quantitative data collection, completion rates for individual items can provide indirect evidence for the acceptance of a tool. While quantitative research provides a rapid insight into scale-user satisfaction, these methods do not provide concrete information for improvement of cultural sensitivity (Ingersoll-Dayton, 2011). For instance, if items are deemed unclear, researchers must understand culturally relevant ways to modify them. To do this, qualitative methods are necessary, as is following-up on user experiences (Ingersoll-Dayton, 2011). Iterative focus groups, fieldwork, qualitative interviews, and feedback collection with community members and clinicians (among other methods) are appropriate methods to review and improve different iterations of a scale until a final, culturally accepted tool is disseminated for community use (Ingersoll-Dayton, 2011; Brown et al., 2013).
Response options
Colonization, repeated systemic discrimination, and unsafe schools have limited access to resources and conditions necessary to maximize socioeconomic status for many Indigenous groups (Reading and Wien, 2009; Davy et al., 2016; Gall et al., 2021). This disadvantage can be manifested in lower rates of educational attainment, literacy, and familiarity of colonizers’ language, which limit reliability of responses to scales and influence the accuracy of depression screening instruments (Akena et al., 2012). As an example, high rates of missing data on Likert response options have challenged defining the diagnosis (Bell et al., 2005). Conversely, participants’ openness to respond can be compromised when the native language is not used (Borsa et al., 2012; Ghimire et al., 2013; Arafat et al., 2016). Thus, translation, audio recordings of the questions, or administration of the tool verbally can improve reliability.
Indigenous co-leadership in scale development
Seeking Indigenous knowledge to inform decision-making on selection, cultural adaptations, and administration of scales, implies that Indigenous peoples are stakeholders in their own mental health (Latulippe and Klenk, 2020). Reconciliation is about the genuine restructuring and transformation of the relationships between Indigenous and settler people (Hoicka et al., 2021). Reconciliation can take place in cultural adaptation processes that use Indigenous knowledge as ‘expert’ knowledge. In fact, through qualitative interviews to learn about experiences with culturally adapted tools, Indigenous people reported that adapted tools ‘mean something to them’, and that these scales can make Indigenous ‘identify with their own person within’ (Marley et al., 2017).
Prior to cultural adaptation, Indigenous peoples in the studies reported that the original scales created “distrust and questions before you get started, and that confidence is really hard to get back” (Marley et al., 2017). In contrast, inviting Indigenous people in the leadership of their own tools supported trust and mutual respect of researchers/practitioners and Indigenous groups, which allows for confidence in and readiness for cultural adaptations. In this way, the studies illustrated how Indigenous co-leadership in scale development was a determinant of the success of other adaptation methods. This is because this process facilitated collaboration in translation and revision of cultural relevance, as well as established a trusting relationship when Indigenous peoples were invited to focus group discussions, key informant interviews, or consultations.
Indigenous co-leadership in adapting scales requires time and resources from both researchers and the Indigenous community. This is stressing the importance of shared needs assessment before the process of cultural adaptation. The needs assessment has to start from the overall idea of using symptom measures. For symptom measures to be useful, cultural safety cannot compromise utility for the medical approach in evaluation and treatment, necessary to inform mental health services.
Holistic constructs of mental well-being
Some tools were developed to be complementary to the symptom measure scales, considering Indigenous conceptualizations of well-being and honoring the self-determination of the Indigenous group. For example, this was the case of the Functional Assessment Instrument (FAI), developed through free-listing interviews – a particular technique that explores how a group thinks about and defines health domains through engaging communities to identify their shared priorities from the perspective of their own ideologies (Schneider et al., 2015). The researchers adapted this scale to identify tasks and activities that women performed during the perinatal period, which they expressed was more relevant to them than clinical features of post-partum assessments and were more meaningful for healing.
Several Indigenous groups reported feeling that alternatives to symptom measures were more consistent with Indigenous visions of health. This aligns with the literature sharing that Indigenous ideologies embrace a holistic concept of health that reflects physical, spiritual, emotional, and mental dimensions (Reading and Wien, 2009). Accordingly, other than symptom scales adapted by studies included in the review, there exists tools to evaluate distress while considering factors specific to the sociocultural reality of the community and their worldviews (Kinzie et al., 1982). For example, the Native American Cultural Values and Beliefs Scale assesses whether the individual experiences any distress based on their lack of participation in important Dakota, Nakota, and Lakota values and beliefs (Reynolds et al., 2006). Other instruments have moved toward the assessment of more general factors that promote or hinder mental health in a broader sense (e.g., emotional wellness and empowerment) rather than standard clinical measures (Haswell et al., 2010). Moreover, some scales for Indigenous groups have moved away from assessing negative constructs of mental illness, and toward strengths and resources associated with resilience, healing, and recovery (Gee et al., 2023).
Inclusion of local cultural expressions can be particularly important in depression, which is a psychological and experiential phenomenon whose meanings are closely shaped by the sociocultural context. Moreover, measurement scales for Western populations may contain behaviors or experiences considered normal or irrelevant to the local culture of the Indigenous population.
Western symptom measures have been developed based on an individual view of health; cultural adaptation of measures cannot change this fact if the focus is still on symptomology. In contrast, if a screen is to be truly aligned with the local Indigenous concept of health, it is possible that it is developed less as a screen of symptomology but rather developed holistically, recognizing that health is interrelated with and interconnected to their families, community, and lands.
Cultural safety during the adaptation and use of the scale
Researchers have emphasized the importance of an ethnographic approach when assessing global mental health and providing care. The incorporation of qualitative and ethnographic methods in developing assessment tools and interventions is well established and recognized (Campbell et al., 2000; Moreau et al., 2009; Onwuegbuzie et al., 2010). Collaborative-participatory research, commitment of Indigenous peoples, and a relationship of trust and respect with the community are crucial methods for a successful process of cultural adaptation. The ethical principles that regulate the research with Indigenous populations must be respected by the research team. Respecting the national standards as well as the specific standards of the target Indigenous group is necessary and essential to confirm further use of adapted depression screens.
Increasing cultural safety starts in the planning stage for conducting research or developing programs for Indigenous peoples, and inclusion of the target population is essential from the early stages of needs assessment and planning (Kirmayer et al., 2003; Darroch et al., 2017; Yaphe et al., 2019). For example, it is recommended to have research members or service providers of the same ethnic origin as the respondents available to establish a safe space (Rait et al., 1999; Kaiser et al., 2013; Billan et al., 2020). When this is not possible, the administrators of the tools may undergo training in cultural competency through workshops, educational programs, or continuing education to create a culturally sensitive space which correspondingly facilitates communication (Billan et al., 2020). Finally, it is essential to consider institutional discrimination and possible stigma of psychiatric diagnoses in the administration of scales. In cultural adaptation processes, minding the local principles are important as it addresses the ownership of data of adapted scale, as well as the patient’s definition of what safe care means (Baba, 2013).
Unanswered questions and future research
While the final version of a culturally adapted depression psychometric remains specific for the target community, scientifically reporting the process of scale cultural adaptation makes it possible to evaluate methods and make conclusions about culturally specific factors that promote or threaten mental health. Reports also enable accumulation of knowledge on suitable methods not only for culturally sensitive measurement but also to inform treatment.
Deleting unsafe items can also have limitations. The lack of inclusion of ‘idioms of distress’ or ‘cultural concepts of distress’ in the diagnoses developed by the biomedical approach can result in low levels of reliability in the information communicated by people. This can potentially interfere with appropriate diagnoses and securing appropriate mental health services or support (Nichter, 2010; Kohrt et al., 2016; Kidron and Kirmayer, 2019; Lewis-Fernández and Kirmayer, 2019). Thus, it should be noted that adaptations that seem necessary to increase acceptability might compromise other psychometric characteristics and thus, confirming validity, comparability, and clinical utility remains an equally important but separate line of development, where normal guidelines for psychometric evaluation apply.
Currently, selection of populations for cultural adaptation seems to have been arbitrary, dependent on motivation of researchers and community members. Future work may include a needs assessment before devoting external and community resources to a cultural adaptation. A rigorous process of cultural adaptation is challenging and necessitates time and resources. Recognizing the populations where measurement will not be possible without a translation or a more profound cultural adaptation as well as prioritizing populations for adaptation based on a needs assessment might be necessary. Alternatively, focus on culturally safe administration of standard scales might be an option.
Greater focus on including supporting visuals (e.g., pictographs) and auditory materials would extend the accessibility of these tools to low literacy or small populations. Sometimes, valid scales could be modified to avoid the most culturally contradictory items. Research should optimally compare acceptability and validity of pure translations to cultural adaptation of the same scales in the same population and calculate the resources vs. benefit of the process.
Use of cultural knowledge to complement mental health interventions is an interesting approach that should be explored. The process of cultural adaptation, and knowledge about local concepts in mental health and the culture specific resilience, can also indirectly increase cultural safety and respect of minorities.
Strengths and limitations
To our knowledge, this is the first systematic scoping review on methods used for culturally adapting depression measures with Indigenous peoples. Broadly, our analysis contributes to the field of cross-cultural studies and to cultural psychiatry providing well established practices that can guide the process of cultural adaptation of measurement tools, as proposed recently (Arafat et al., 2016). The findings of this review may facilitate further research and more equitable exchanges of knowledge on culturally sensitive measures for not only psychiatry but also resilience and supporting factors. The latter remains a generally unmet need; reports have shown that many psychometric scales can be experienced as unsafe and that empowering approaches to mental health assessment are preferred by several Indigenous groups (Gomez Cardona et al., 2021).
Our search was limited to articles in English. We discarded several articles due to the complexity of the definition of Indigenous peoples and the way this was addressed in the research. In fact, the definition of Indigenous is problematic since the auto-definition of individuals as such is not always rigorously considered by all studies, especially those published before the 2000s. In several cases, Indigenous identity was not specified in the studies or was not used as an inclusion criterion. For consistency, we intentionally excluded studies where the Indigenous community was not living in their country of origin, such as when cultural adaptation was done for immigrants or refugees in another country. In future research, these factors could be considered – particularly, the geographical distribution of Indigenous peoples in identified studies. Moreover, since there are many undertakings of research with Indigenous on mental health assessment, updated searches should be done to support new innovation in culturally safe tools.
Conclusion
Revision of linguistic equivalence and cultural relevance of items, culturally safe administration procedures, and participatory research were key features of improving cultural sensitivity of psychometric measures for depressive symptoms among global Indigenous populations. Participatory qualitative research and methods are appropriate for conducting cultural adaptation of instruments most suitable for the community, but a careful, shared needs assessment is necessary to prioritize resources. Across all studies, increasing cultural safety by translation, changes to content, or modes of administration protocol were found to be empowering and healing. Indigenous reported that the most acceptable scales were culturally safe and able to be integrated into their health services. Use of visual scales and auditory materials are promising in terms of acceptability of the measurement. Finally, empowerment – focused approaches and tools as alternatives to symptom measures should actively be sought for provision of high-quality and culturally sensitive mental health services.
Supporting information
Gomez Cardona et al. supplementary material
Acknowledgements
We would like to thank Ms. Andrea Quaiattini from the McGill University Library for her assistance with our comprehensive systematic search procedure. We also express our gratitude for Indigenous co-authors in other publications and some other community members in Montreal and Kahnawà:ke for introducing us to some basic concepts of their view of health and wellbeing as opposed to symptom measurement.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2023.75.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/gmh.2023.75.
Data availability statement
All additional data is available upon request from authors.
Author contribution
L.G.C., V.N. and O.L. were involved in the conceptualization of the review. Project management was the responsibility of L.G.C. and O.L. Data screening and data analysis were conducted by all authors. All findings were validated by L.G.C. The original draft of the manuscript was written by L.G.C., M.Y., Q.S., and O.L. was reviewed and edited by L.G.C., M.Y., O.L. All co-authors reviewed the final version of the article. Funding was acquired by L.G.C. and O.L.
Financial support
O.L. was funded by grants from FSISSS (#8400958), CIHR (#426678), FRSQ (#252872 and #265693O), the Réseau Québécois sur le suicide, les troubles de l’humeur et les troubles associés, and the Strategic Research Council (SRC) established within the Academy of Finland (#352700). L.G.C. had financial support from the Réseau universitaire intégré de santé et services sociaux (RUISSS) McGill and CIHR grant #430331. Q.S. had funding from McGill University’s Healthy Brains Healthy Lives fellowship (Q.S.). The funders had no role in study design or in later collection and data analysis.
Competing interest
The authors declare none.
References
- Aboraya A, Nasrallah HA, Elswick DE, Ahmed E, Estephan N, Aboraya D, Berzingi S, Chumbers J, Berzingi S, Justice J, Zafar J and Dohar S (2018) Measurement-based care in psychiatry-past, present, and future. Innovations in Clinical Neuroscience 15(11–12), 13–26. [PMC free article] [PubMed] [Google Scholar]
- Akena D, Joska J, Obuku EA, Amos T, Musisi S and Stein DJ (2012) Comparing the accuracy of brief versus long depression screening instruments which have been validated in low and middle income countries: A systematic review. BMC Psychiatry 12(1), 187. 10.1186/1471-244X-12-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida OP, Flicker L, Fenner S, Smith K, Hyde Z, Atkinson D, Skeaf L, Malay R and LoGiudice D (2014) The Kimberley assessment of depression of older indigenous Australians: Prevalence of depressive disorders, risk factors and validation of the KICA-dep scale. PLoS One 9(4), e94983. 10.1371/journal.pone.0094983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2023) About DSM-5-TR. Available at https://www.psychiatry.org/psychiatrists/practice/dsm/about-dsm.
- Amnesty International (2023) Indigenous Peoples. Available at https://www.amnesty.org/en/what-we-do/indigenous-peoples/.
- Andersen L, Kagee A, O’Cleirigh C, Safren S and Joska J (2015) Understanding the experience and manifestation of depression in people living with HIV/AIDS in South Africa. AIDS Care 27(1), 59–62. 10.1080/09540121.2014.951306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arafat SMY, Chowdhury HR, Qusar MMAS and Hafez MA (2016) Cross cultural adaptation & psychometric validation of research instruments: A methodological review. Journal of Behavioral Health 5(3), 129–136. 10.5455/jbh.20160615121755. [DOI] [Google Scholar]
- Arksey H and O’Malley L (2005) Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology 8(1), 19–32. 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Armenta BE, Sittner Hartshorn KJ, Whitbeck LB, Crawford DM and Hoyt DR (2014) A longitudinal examination of the measurement properties and predictive utility of the Center for Epidemiologic Studies Depression Scale among North American indigenous adolescents. Psychological Assessment 26(4), 1347–1355. 10.1037/a0037608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashaba S, Cooper-Vince C, Vořechovská D, Maling S, Rukundo GZ, Akena D and Tsai AC (2019) Development and validation of a 20-item screening scale to detect major depressive disorder among adolescents with HIV in rural Uganda: A mixed-methods study. SSM - Population Health 7, 100332. 10.1016/j.ssmph.2018.100332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare (2009) Measuring the social and emotional wellbeing of Aboriginal and Torres Strait Islander peoples. Australian Institute of Health and Welfare. Available at https://www.aihw.gov.au/reports/indigenous-australians/measuring-the-social-and-emotional-wellbeing/summary.
- Baba L (2013) Cultural safety in First Nations, Inuit and Métis public health: Environmental scan for cultural competency and safety in education, training and health services. National Collaborating Centre for Aboriginal Health. Available at https://www.ccnsa-nccah.ca/docs/emerging/RPT-CulturalSafetyPublicHealth-Baba-EN.pdf.
- Baron EC, Davies T and Lund C (2017) Validation of the 10-item Centre for Epidemiological Studies Depression Scale (CES-D-10) in Zulu, Xhosa and Afrikaans populations in South Africa. BMC Psychiatry 17(1), 6. 10.1186/s12888-016-1178-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass JK, Ryder RW, Lammers M-C, Mukaba TN and Bolton PA (2008) Post-partum depression in Kinshasa, Democratic Republic of Congo: Validation of a concept using a mixed-methods cross-cultural approach. Tropical Medicine & International Health 13(12), 1534–1542. 10.1111/j.1365-3156.2008.02160.x. [DOI] [PubMed] [Google Scholar]
- Beaton DE, Bombardier C, Guillemin F and Ferraz MB (2000) Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 25(24), 3186–3191. 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- Bell RA, Smith SL, Arcury TA, Snively BM, Stafford JM and Quandt SA (2005) Prevalence and correlates of depressive symptoms among rural older African Americans, native Americans, and whites with diabetes. Diabetes Care 28(4), 823–829. 10.2337/diacare.28.4.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billan J, Starblanket D, Anderson S, Legare M, Hagel MC, Oakes N, Jardine M, Boehme G, Dubois E, Spencer O, Hotomani M, McKenna B and Bourassa C (2020) Ethical research engagement with indigenous communities. Journal of Rehabilitation and Assistive Technologies 7, 2055668320922706. 10.1177/2055668320922706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boksa P, Joober R and Kirmayer LJ (2015) Mental wellness in Canada’s aboriginal communities: Striving toward reconciliation. Journal of Psychiatry & Neuroscience 40(6), 363–365. 10.1503/jpn.150309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsa J, Damasio B and Bandeira D (2012) Cross-cultural adaptation and validation of psychological instruments: Some considerations. Paidéia (Ribeirão Preto) 22, 10. [Google Scholar]
- Bougie E, Arim RG, Kohen DE and Findlay LC (2016) Validation of the 10-item Kessler psychological distress scale (K10) in the 2012 aboriginal peoples survey. Health Reports 27(1), 3–10. https://www.ncbi.nlm.nih.gov/pubmed/26788720. [PubMed] [Google Scholar]
- Bowen A and Muhajarine N (2006) Prevalence of antenatal depression in women enrolled in an outreach program in Canada. Journal of Obstetric, Gynecologic, and Neonatal Nursing 35(4), 491–498. 10.1111/j.1552-6909.2006.00064.x. [DOI] [PubMed] [Google Scholar]
- Brascoupé S and Waters C (2009) Cultural safety: Exploring the applicability of the concept of cultural safety to aboriginal health and community wellness. Journal of Aboriginal Health 5, 6–41. [Google Scholar]
- Brown AD, Mentha R, Rowley KG, Skinner T, Davy C and O’Dea K (2013) Depression in aboriginal men in Central Australia: Adaptation of the patient health questionnaire 9. BMC Psychiatry 13, 271. 10.1186/1471-244X-13-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A, Hayes B and Buckby B (2008) Aboriginal and Torres Strait islander women’s experience when interacting with the Edinburgh postnatal depression scale: A brief note. The Australian Journal of Rural Health 16(3), 124–131. 10.1111/j.1440-1584.2007.00930.x. [DOI] [PubMed] [Google Scholar]
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D and Tyrer P (2000) Framework for design and evaluation of complex interventions to improve health. BMJ 321(7262), 694–696. 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caneo C, Toro P and Ferreccio C (2020) Validity and performance of the patient health questionnaire (PHQ-2) for screening of depression in a rural Chilean cohort. Community Mental Health Journal 56(7), 1284–1291. 10.1007/s10597-020-00605-8. [DOI] [PubMed] [Google Scholar]
- Chachamovich E, Kirmayer LJ, Haggarty JM, Cargo M, McCormick R and Turecki G (2015) Suicide among Inuit: Results from a large, epidemiologically representative follow-Back study in Nunavut. Canadian Journal of Psychiatry 60(6), 268–275. 10.1177/070674371506000605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapla A, Prabhakaran A, Ganjiwale J, Nimbalkar S and Kharod N (2019) Validation of the Gujarati version of Center for Epidemiological Studies Depression Scale for children (CES-DC) and prevalence of depressive symptoms amongst school going adolescents in Gujarat, India. Journal of Clinical and Diagnostic Research 13(12), VC06–VC11. 10.7860/JCDR/2019/41001.13377. [DOI] [Google Scholar]
- Chapleski EE, Lamphere JK, Kaczynski R, Lichtenberg PA and Dwyer JW (1997) Structure of a depression measure among American Indian elders: Confirmatory factor analysis of the CES-D scale. Research on Aging 19(4), 462–485. 10.1177/0164027597194004. [DOI] [Google Scholar]
- Chávez LM and Canino G (2005) Toolkit on Translating and Adapting Instruments. The Evaluation HSRI Centre. U.S. Department of Health and Human Services United States of America. https://www.hsri.org/publication/toolkit-on-translating-and-adapting-instruments. [Google Scholar]
- Darroch F, Giles A, Sanderson P, Brooks-Cleator L, Schwartz A, Joseph D and Nosker R (2017) The United States does CAIR about cultural safety: Examining cultural safety within indigenous health contexts in Canada and the United States. Journal of Transcultural Nursing 28(3), 269–277. 10.1177/1043659616634170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davy C, Harfield S, McArthur A, Munn Z and Brown A (2016) Access to primary health care services for indigenous peoples: A framework synthesis. International Journal for Equity in Health 15(1), 163. 10.1186/s12939-016-0450-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denckla CA, Ndetei DM, Mutiso VN, Musyimi CW, Musau AM, Nandoya ES, Anderson KK, Milanovic S, Henderson D and McKenzie K (2017) Psychometric properties of the Ndetei-Othieno-Kathuku (NOK) scale: A mental health assessment tool for an African setting. Journal of Child and Adolescent Mental Health 29(1), 39–49. 10.2989/17280583.2017.1310729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easton SD, Safadi NS, Wang Y and Hasson RG (2017) The Kessler psychological distress scale: Translation and validation of an Arabic version. Health and Quality of Life Outcomes, 15(1), 215. 10.1186/s12955-017-0783-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekeroma AJ, Ikenasio-Thorpe B, Weeks S, Kokaua J, Puniani K, Stone P and Foliaki SA (2012) Validation of the Edinburgh postnatal depression scale (EPDS) as a screening tool for postnatal depression in Samoan and Tongan women living in New Zealand. The New Zealand Medical Journal, 125(1355), 41–49. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med8&NEWS=N&AN=22722214. [PubMed] [Google Scholar]
- Esler D, Johnston F, Thomas D and Davis B (2008) The validity of a depression screening tool modified for use with aboriginal and Torres Strait islander people. Australian and New Zealand Journal of Public Health 32(4), 317–321. 10.1111/j.1753-6405.2008.00247.x. [DOI] [PubMed] [Google Scholar]
- Esler DM, Johnston F and Thomas D (2007) The acceptability of a depression screening tool in an urban, aboriginal community-controlled health service. Australian and New Zealand Journal of Public Health 31(3), 259–263. Available at https://www.ncbi.nlm.nih.gov/pubmed/17679245. [DOI] [PubMed] [Google Scholar]
- Fernandes MC, Srinivasan K, Stein AL, Menezes G, Sumithra R and Ramchandani PG (2011) Assessing prenatal depression in the rural developing world: A comparison of two screening measures. Archives of Women’s Mental Health 14(3), 209–216. 10.1007/s00737-010-0190-2. [DOI] [PubMed] [Google Scholar]
- Frohlich KL, Ross N and Richmond C (2006) Health disparities in Canada today: Some evidence and a theoretical framework. Health Policy 79(2–3), 132–143. 10.1016/j.healthpol.2005.12.010. [DOI] [PubMed] [Google Scholar]
- Gall A, Anderson K, Howard K, Diaz A, King A, Willing E, Connolly M, Lindsay D and Garvey G (2021) Wellbeing of Indigenous Peoples in Canada, Aotearoa (New Zealand) and the United States: A Systematic Review. International Journal of Environmental Research and Public Health, 18(11), 5832. 10.3390/ijerph18115832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallis JA, Maselko J, O’Donnell K, Song K, Saqib K, Turner EL and Sikander S (2018) Criterion-related validity and reliability of the Urdu version of the patient health questionnaire in a sample of community-based pregnant women in Pakistan. PeerJ (San Francisco, CA) 6, e5185. 10.7717/peerj.5185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganguli M, Dube S, Johnston JM, Pandav R, Chandra V and Dodge HH (1999) Depressive symptoms, cognitive impairment and functional impairment in a rural elderly population in India: A Hindi version of the geriatric depression scale (GDS-H). International Journal of Geriatric Psychiatry 14(10), 807–820. . [DOI] [PubMed] [Google Scholar]
- Gee G, Hulbert C, Kennedy H and Paradies Y (2023) Cultural determinants and resilience and recovery factors associated with trauma among aboriginal help-seeking clients from an aboriginal community-controlled counselling service. BMC Psychiatry 23(1), 155. 10.1186/s12888-023-04567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, Wondimagegn D, Lemenhe A, Fann JR, Vander Stoep A and Andrew Zhou XH (2013) Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Research 210(2), 653–661. 10.1016/j.psychres.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghimire DJ, Chardoul S, Kessler RC, Axinn WG and Adhikari BP (2013) Modifying and validating the composite international diagnostic interview (CIDI) for use in Nepal. International Journal of Methods in Psychiatric Research 22(1), 71–81. 10.1002/mpr.1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez Cardona L, Brown K, McComber M, Outerbridge J, Parent-Racine E, Phillips A, Boyer C, Martin C, Splicer B, Thompson D, Yang M, Velupillai G, Laliberté A, Haswell M and Linnaranta O (2021) Depression or resilience? A participatory study to identify an appropriate assessment tool with Kanien’kéha (Mohawk) and Inuit in Quebec. Social Psychiatry and Psychiatric Epidemiology 56(10), 1891–1902. 10.1007/s00127-021-02057-1. [DOI] [PubMed] [Google Scholar]
- Hackett ML, Farnbach S, Glozier N, Skinner T, Teixeira-Pinto A, Askew D, Gee G, Cass A and Brown A (2016) Getting it right: Study protocol to determine the diagnostic accuracy of a culturally-specific measure to screen for depression in aboriginal and/or Torres Strait islander people. BMJ Open 6(12), e015009. 10.1136/bmjopen-2016-015009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackett ML, Teixeira‐Pinto A, Farnbach S, Glozier N, Skinner T, Askew DA, Gee G, Cass A and Brown A (2019) Getting it right: Validating a culturally specific screening tool for depression ( aPHQ‐9) in aboriginal and Torres Strait islander Australians. Medical Journal of Australia 211(1), 24–30. 10.5694/mja2.50212. [DOI] [PubMed] [Google Scholar]
- Hajizadeh M, Bombay A and Asada Y (2019) Socioeconomic inequalities in psychological distress and suicidal behaviours among indigenous peoples living off-reserve in Canada. Canadian Medical Association Journal 191, E325–E336. 10.1503/cmaj.181374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haroz EE, Bass J, Lee C, Oo SS, Lin K, Kohrt B, Michalopolous L, Nguyen AJ and Bolton P (2017) Development and cross-cultural testing of the international depression symptom scale (IDSS): A measurement instrument designed to represent global presentations of depression. Global Mental Health 4, e17. 10.1017/gmh.2017.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haroz EE, Bass JK, Lee C, Murray LK, Robinson C and Bolton P (2014) Adaptation and testing of psychosocial assessment instruments for cross-cultural use: An example from the Thailand Burma border. BMC Psychology 2(1), 31–31. 10.1186/s40359-014-0031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harry ML and Crea TM (2018) Examining the measurement invariance of a modified CES-D for American Indian and non-Hispanic white adolescents and young adults. Psychological Assessment 30(8), 1107–1120. 10.1037/pas0000553. [DOI] [PubMed] [Google Scholar]
- Haswell MR, Kavanagh D, Tsey K, Reilly L, Cadet-James Y, Laliberte A, Wilson A and Doran C (2010) Psychometric validation of the growth and empowerment measure (GEM) applied with indigenous Australians. Australian & New Zealand Journal of Psychiatry 44(9), 791–799. 10.3109/00048674.2010.482919. [DOI] [PubMed] [Google Scholar]
- Hoicka CE, Savic K and Campney A (2021) Reconciliation through renewable energy? A survey of indigenous communities, involvement, and peoples in Canada. Energy Research & Social Science 74, 101897. 10.1016/j.erss.2020.101897. [DOI] [Google Scholar]
- Husain N, Gater R, Tomenson B and Creed F (2006) Comparison of the personal health questionnaire and the self reporting questionnaire in rural Pakistan. The Journal of the Pakistan Medical Association 56(8), 366–370. [PubMed] [Google Scholar]
- Indigenous Peoples (2023) Indigenous Peoples. Amnesty International. https://www.amnesty.org/en/what-we-do/indigenous-peoples/.
- Ingersoll-Dayton B (2011) The development of culturally-sensitive measures for research on ageing. Ageing and Society 31(3), 355–370. 10.1017/s0144686x10000917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamil Asilia Centre (2021) The Indigeneity. Who are Indigenous People? Available at https://jamiiasilia.org/about/indigenous-peoples/.
- Kaaya SF, Lee B, Mbwambo JK, Smith-Fawzi MC and Leshabari MT (2008) Detecting depressive disorder with a 19-item local instrument in Tanzania. International Journal of Social Psychiatry 54(1), 21–33. 10.1177/0020764006075024. [DOI] [PubMed] [Google Scholar]
- Kaiser BN, Kohrt BA, Keys HM, Khoury NM and Brewster A-RT (2013) Strategies for assessing mental health in Haiti: Local instrument development and transcultural translation. Transcultural Psychiatry 50(4), 532–558. 10.1177/1363461513502697. [DOI] [PubMed] [Google Scholar]
- Kidron CA and Kirmayer LJ (2019) Global mental health and idioms of distress: The paradox of culture-sensitive Pathologization of distress in Cambodia. Culture, Medicine and Psychiatry 43(2), 211–235. 10.1007/s11013-018-9612-9. [DOI] [PubMed] [Google Scholar]
- Kilburn K, Prencipe L, Hjelm L, Peterman A, Handa S and Palermo T (2018) Examination of performance of the Center for Epidemiologic Studies Depression Scale Short Form 10 among African youth in poor, rural households. BMC Psychiatry 18(1), 201. 10.1186/s12888-018-1774-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinzie JD, Manson SM, Vinh DT, Tolan NT, Anh B and Pho TN (1982) Development and validation of a Vietnamese-language depression rating scale. The American Journal of Psychiatry 139(10), 1276–1281. 10.1176/ajp.139.10.1276. [DOI] [PubMed] [Google Scholar]
- Kirmayer L, Fletcher C and Watt R (2008) Locating the ecocentric self: Inuit concepts of mental health and illness. In Healing Traditions: The Mental Health of Aboriginal Peoples in Canada. UBC Press, Vancouver, BC, Canada, pp. 289–314. [Google Scholar]
- Kirmayer L, Simpson C and Cargo M (2003) Healing traditions: Culture, community and mental health promotion with Canadian aboriginal peoples. Australasian Psychiatry 11(1_suppl), S15–S23. 10.1046/j.1038-5282.2003.02010.x. [DOI] [Google Scholar]
- Kleinman AM (1977) Depression, somatization and the “new cross-cultural psychiatry”. Social Science & Medicine 11(1), 3–9. 10.1016/0037-7856(77)90138-X. [DOI] [PubMed] [Google Scholar]
- Kohrt BA, Luitel NP, Acharya P and Jordans MJ (2016) Detection of depression in low resource settings: Validation of the patient health questionnaire (PHQ-9) and cultural concepts of distress in Nepal. BMC Psychiatry 16, 58. 10.1186/s12888-016-0768-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kral MJ (2016) Suicide and suicide prevention among Inuit in Canada. Canadian Journal of Psychiatry 61(11), 688–695. 10.1177/0706743716661329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latulippe N and Klenk N (2020) Making room and moving over: Knowledge co-production, indigenous knowledge sovereignty and the politics of global environmental change decision-making. Current Opinion in Environmental Sustainability 42, 7–14. 10.1016/j.cosust.2019.10.010. [DOI] [Google Scholar]
- Leung L (2016) Diabetes mellitus and the aboriginal diabetic initiative in Canada: An update review. Journal of Family Medicine and Primary Care 5(2), 259–265. 10.4103/2249-4863.192362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis-Fernández R and Kirmayer LJ (2019) Cultural concepts of distress and psychiatric disorders: Understanding symptom experience and expression in context. Transcultural Psychiatry 56(4), 786–803. 10.1177/1363461519861795. [DOI] [PubMed] [Google Scholar]
- Marley JV, Kotz J, Engelke C, Williams M, Stephen D, Coutinho S and Trust SK (2017) Validity and acceptability of Kimberley Mum’s mood scale to screen for perinatal anxiety and depression in remote aboriginal health care settings. PLoS One 12(1), e0168969. 10.1371/journal.pone.0168969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh ML (2012) Interrater reliability: The kappa statistic. Biochemia Medica 22(3), 276–282. [PMC free article] [PubMed] [Google Scholar]
- McNamara BJ, Banks E, Gubhaju L, Williamson A, Joshy G, Raphael B and Eades SJ (2014) Measuring psychological distress in older aboriginal and Torres Strait islanders Australians: A comparison of the K-10 and K-5. Australian and New Zealand Journal of Public Health 38(6), 567–573. 10.1111/1753-6405.12271. [DOI] [PubMed] [Google Scholar]
- Mitchell CM and Beals J (2011) The utility of the Kessler screening scale for psychological distress (K6) in two American Indian communities. Psychological Assessment 23(3), 752–761. 10.1037/a0023288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montreal Urban Aboriginal Health Needs Assessment (2012) Montreal Urban Aboriginal Community Strategy Network (NETWORK), pp. 0–54. https://ihct.ca/images/pdf/final-report-health-needs-assessment.pdf
- Moreau N, Hassan G, Rousseau C and Chenguiti K (2009) Perception that “everything requires a lot of effort”: Transcultural SCL-25 item validation. The Journal of Nervous and Mental Disease 197(9), 695–699. 10.1097/NMD.0b013e3181b3af0c. [DOI] [PubMed] [Google Scholar]
- National Collaborating Centre for Aboriginal Health (2019) National Collaborating Centre for Aboriginal Health. L’accès aux services de santé comme un déterminant social de la santé des premièrs nations, des inuits et des métis. https://www.ccnsa.ca/docs/determinants/FS-AccessHealthServicesSDOH-2019-FR.pdf. [Google Scholar]
- Nichter M (2010) Idioms of distress revisited. Culture, Medicine and Psychiatry 34(2), 401–416. 10.1007/s11013-010-9179-6. [DOI] [PubMed] [Google Scholar]
- Onwuegbuzie AJ, Bustamante RM and Nelson JA (2010) Mixed research as a tool for developing quantitative instruments. Journal of Mixed Methods Research 4, 56–78. 10.1177/1558689809355805. [DOI] [Google Scholar]
- Rait G, Burns A, Baldwin R, Morley M, Chew-Graham C, St Leger AS and Abas M (1999) Screening for depression in African-Caribbean elders. Family Practice 16(6), 591–595. 10.1093/fampra/16.6.591. [DOI] [PubMed] [Google Scholar]
- Reading C and Wien D (2009) Health inequalities and social determinants of Aboriginal peoples’ health. Available at https://www.ccnsa-nccah.ca/docs/determinants/RPT-Healthinequalities-Reading-Wien-EN.pdf.
- Reid P, Cormack D and Paine SJ (2019) Colonial histories, racism and health-the experience of Māori and indigenous peoples. Public Health 172, 119–124. 10.1016/j.puhe.2019.03.027. [DOI] [PubMed] [Google Scholar]
- Reynolds WR, Quevillon RP, Boyd B and Mackey D (2006) Initial development of a cultural values and beliefs scale among Dakota/Nakota/Lakota people: A pilot study. American Indian and Alaska Native Mental Health Research 13(3), 70–93. 10.5820/aian.1303.2006.70. [DOI] [PubMed] [Google Scholar]
- Sarkar S, Kattimani S, Roy G, Premarajan KC and Sarkar S (2015) Validation of the Tamil version of short form geriatric depression scale-15. Journal of Neurosciences in Rural Practice 6(3), 442–1446. 10.4103/0976-3147.158800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sartorius N and Janca A (1996) Psychiatric assessment instruments developed by the World Health Organization. Social Psychiatry and Psychiatric Epidemiology 31(2), 55–69. 10.1007/bf00801901. [DOI] [PubMed] [Google Scholar]
- Schantz K, Reighard C, Aikens JE, Aruquipa A, Pinto B, Valverde H and Piette JD (2017) Screening for depression in Andean Latin America: Factor structure and reliability of the CES-D short form and the PHQ-8 among Bolivian public hospital patients. International Journal of Psychiatry in Medicine 52(4–6), 315–327. 10.1177/0091217417738934. [DOI] [PubMed] [Google Scholar]
- Schneider M, Baron E, Davies T, Bass J and Lund C (2015) Making assessment locally relevant: Measuring functioning for maternal depression in Khayelitsha, Cape Town. Social Psychiatry and Psychiatric Epidemiology 50(5), 797–806. 10.1007/s00127-014-1003-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smallwood R, Usher K, Woods C, Sampson N and Jackson D (2023) De‐problematising Aboriginal young peoples’ health and well‐being through their voice: An Indigenous scoping review. Journal of Clinical Nursing 32, 2086–2101. 10.1111/jocn.16308. [DOI] [PubMed] [Google Scholar]
- Sousa V and Rojjanasrirat W (2011) Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. Journal of Evaluation in Clinical Practice 17, 268–274. 10.1111/j.1365-2753.2010.01434.x. [DOI] [PubMed] [Google Scholar]
- Tiburcio Sainz M and Natera Rey G (2007) Adaptación al contexto ñahñú del Cuestionario de Enfrentamientos (CQ), la Escala de Síntomas (SRT) y la Escala de Depresión del Centro de Estudios Epidemiológicos (CES-D). Salud mental (México) 30(3), 48–58. [Google Scholar]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö and Straus SE (2018) PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine 169(7), 467–473. 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- United Nations (2003) Indigenous Peoples and the MDGs. Department of Economic and Social Affairs: Indigenous Peoples. Available at https://www.un.org/development/desa/indigenouspeoples/focus-areas/post-2015-agenda/the-sustainable-development-goals-sdgs-and-indigenous/mdgs.html.
- Wexler L, McEachern D, Difulvio G, Smith C, Graham LF and Dombrowski K (2017) Creating a community of practice to prevent suicide through multiple channels: Describing the theoretical foundations and structured learning of PC CARES. International Quarterly of Community Health Education 36(2), 115–122. 10.1177/0272684x16630886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiltsey Stirman S, Baumann AA and Miller CJ (2019) The FRAME: An expanded framework for reporting adaptations and modifications to evidence-based interventions. Implementation Science 14(1), 58. 10.1186/s13012-019-0898-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaphe S, Richer F and Martin C (2019) Cultural safety training for health professionals working with indigenous populations in Montreal, Québec. International Journal of Indigenous Health 14(1), 60–84. 10.32799/ijih.v14i1.30861. [DOI] [Google Scholar]