Abstract
Talar extrusions are the rare extreme case of talar fractures and dislocations which are associated with high-energy trauma. Given the rarity of talar extrusion, no proper treatment protocol has been established. The earlier treatment outcomes have been poor due to the high rate of infection and avascular necrosis. However, more recent literature advised reimplanting the talus whenever practical, and providing with meticulous cleaning of the talus. In the presence of infection and severe trauma, tibiocalcaneal fusion achieved by the Ilizarov external fixator can be an effective salvage method.
Keywords: Avascular necrosis, Talar extrusion, Tibiocalcaneal fusion, Ilizarov method
Introduction
Talar fractures and dislocations are typically caused by high-energy trauma, and they are generally accompanied by significant displacement, extensive soft-tissue damage, wound contamination, and interruption of the blood supply.1 In the past, talar dislocation was first reported by the German surgeon Fabricius Hildanus in 1680. Talectomy was then used to treat the injury. Van Opstal and Vandeputte2 reported the use of the term "aviator's astragalus” for talar dislocations and fractures in 1919, which was adopted later in 1952.
The talus is made of dense bone, so it can only be shattered by a significant amount of force. As a result, talus fractures are relatively rare, accounting for less than 1% of all fractures.3 Total talar extrusion is the rarest form of talus injuries. Although the true incidence is unknown, it is estimated to be approximately 0.06 % of all dislocations and 2 % of all talar injuries.4 Because of that, there is controversy over how to treat it.1 In this case report, we will discusse our experience in managing a such case.
Case report
A 22-year-old gentleman with underlying Grave's disease has been involved in a motorbike and car accident with an unknown mechanism of injury. He was found unconscious inside a 1 m depth drain. After the trauma, he suffered bleeding from the right ankle with deformity and pain in the right lower limb, causing him unable to move. Otherwise, there was no injury elsewhere.
Upon examination at the casualty, the Glasgow coma scale was 15/15 and the primary survey was uneventful with stable vital signs. There was a shortening of the right lower limb by local examination and the limb rotated externally with noticeable swelling and deformity over the right thigh. There are 80% circumferential laceration in the anterior part of the ankle, which extends laterally to the posterior part of the ankle. The skin on the medial ankle joint is intact, and the extensor digitorum, tibialis anterior, extensor hallucis longus, and bones (Fig. 1). Wound was dirty with no active bleeding. The foot dorsum was grossly swollen and deformed, but the foot compartment was soft. All toes appeared pink with a capillary refill time of less than 2 seconds. Dorsalis pedis artery and posterior tibialis artery pulses were palpable with good volume. The rescuer found the extruded talus and sent it for examination with the patient (Fig. 2). Upon inspection, there was a comminuted fracture over the talar body, and it was heavily covered with soil particles. The bone was irrigated with copious amounts of saline and then covered with moist gauze.
Fig. 1.
Wound condition upon admission.
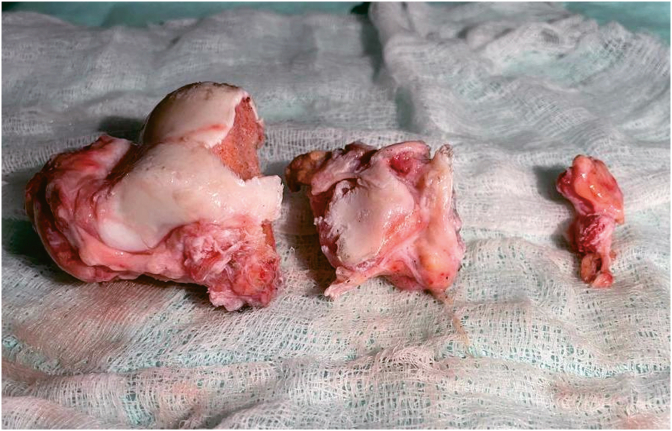
Fig. 2.
Extruded talus after irrigation.
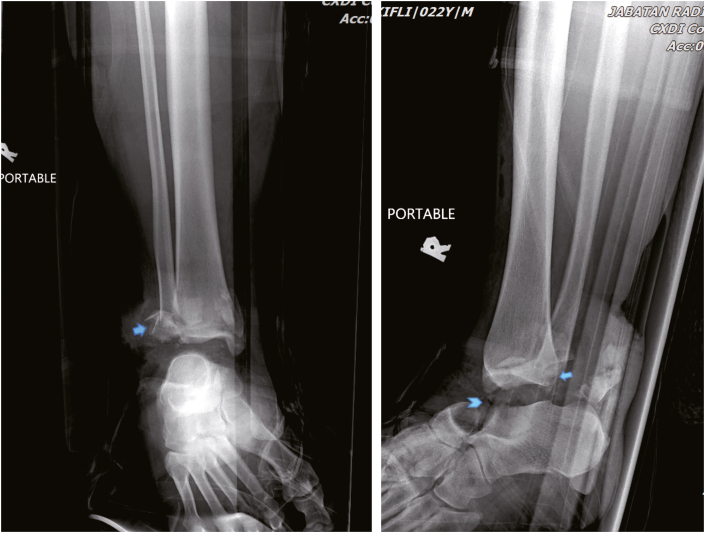
Blood investigations were unremarkable. A plain radiograph of the right ankle showed missing talus with a comminuted fracture of the lateral malleolus (Weber type B) and posterior malleolus fracture (Fig. 3). Meanwhile, a plain radiograph of the right femur showed a comminuted fracture of the midshaft right femur with small butterfly fragment (Winquist classification 1).
Fig. 3.
Plain radiograph of anterior posterior and lateral views of the right ankle showing lateral malleolus and posterior malleolus fractures (blue arrow) and missing talus (chevron arrow).
The patient was brought to the emergency department with a right lower limb splint and cervical collar immobilization. He was stabilized without any life-threatening injury, and intravenous (IV) Cefuroxime 1.5 g stat dose was administered promptly. The right ankle wound was irrigated with copious amount of normal saline, covered and bandaged with moist gauze. Below knee back slab was then applied for temporary stabilization along with skin traction. The patient received 3 L of IV fluid normal saline over 24 h, started on regular analgesics of IV Tramadol 50 mg and took Paracetamol tablet 1 g. Triple antibiotics were started, by given IV Cefuroxime 750 mg, Metronidazole 500 mg, and Gentamicin 160 mg.
He underwent emergent surgical interventions, including extensive wound debridement, cross-ankle external fixator, and gentamicin-impregnated polymethyl methacrylate cement spacer insertion of the right ankle. Intraoperative findings showed a total cut of the peroneus longus, brevis tendon and muscle belly of the extensor digitorum, all of which were finally repaired. The dorsalis pedis artery was macerated, the anterior ankle segmental was lost, the wound was severely contaminated with soil particles, and it was finally decided not to reinsert the extruded talar bone. Postoperatively, the wound was co-managed with plastic surgery, and multiple cycles of vacuum dressing and re-wound debridement were performed. The patient was allowed to mobilize without bearing weight onto the right ankle.
Tibiocalcaneal arthrodesis, the method of treatment was explained to the patient. However, the definitive treatment was delayed due to pin site infection complicated with Staphylococcus aureus bacteremia. He underwent an exchange of antibiotic cement spacer and wound coverage with a split skin graft 3 months later. After negative cultures were obtained, partial weight-bearing ambulation was subsequently started. He eventually underwent definitive operation: bone resection, removal of antibiotic cement spacer, tendoachilles tenotomy, and acute docking right ankle with Ilizarov external fixator 9 months after trauma (Fig. 4). Intraoperatively, the previously grafted skin healed well, without signs of infection such as pus and unhealthy tissues. Bone quality was soft due to diffused osteopenia.
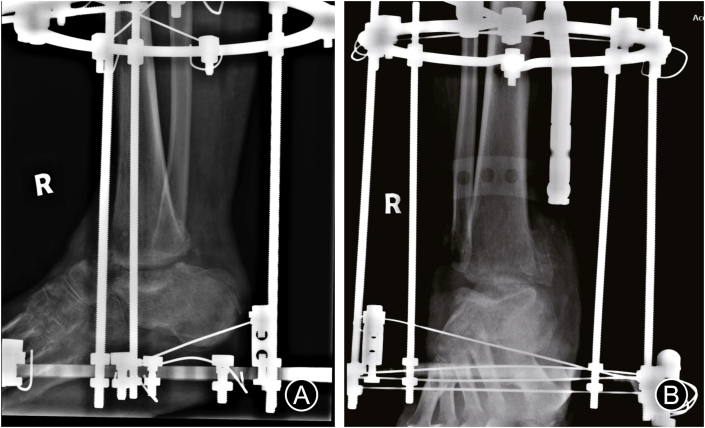
Fig. 4.
Radiograph right ankle post tibiocalcaneal fusion anterior posterior (A) and lateral (B) views.
Bone resection was done via anterolateral approach of ankle. With the loss of talus, navicular and tibiocalcaneal cartilaginous surface were dissected, until subchondral bone was bleeding. Medial malleolus was excised to match the joint fusion, and in this case, tip end of lateral malleolus was already up to the required level of the plafond due to initial injury. If not, an oblique osteotomy should be used to remove the lateral malleolus until the desired level was reached. By doing so, the foot's lateral contour will be improved, and the calcaneus will be better exposed for the fitting of the plafond onto the calcaneus. The shape of the posterior facet of the calcaneus was preserved by sculpting the surfaces of the calcaneus and plafond with osteotomes and a micro-oscillating saw while under saline irrigation. The concave navicular was left undisturbed, since the rounded anterior plafond fitted well with it. Temporary Kirschner wires were inserted through the plantar surface of the calcaneus into the tibia to compress and shorten the contoured bleeding of bone surfaces.
Bone graft was not used in this case, and the fusion was set in mild dorsiflexion. A footplate and a solid tibial ring were used in constructing an Ilizarov frame. We have avoided from drilling a pin from posterior calcaneum because the wound was just freshly healed, and we wanted to leave the area undisturbed. Thus, only 1 pin was drilled into the calcaneus instead of 2 pins.
The patient was discharged on day 2 postoperatively and started on calcium supplements: calcium lactate 300 mg, rocaltrol 0.25 mcg, and Alendronate 75 mg weekly. Partial weight-bearing ambulation was started 3 weeks postoperatively. Fusion was achieved after 3 months postoperatively (Fig. 5) and the wound so far has been healing well without infection (Fig. 6).
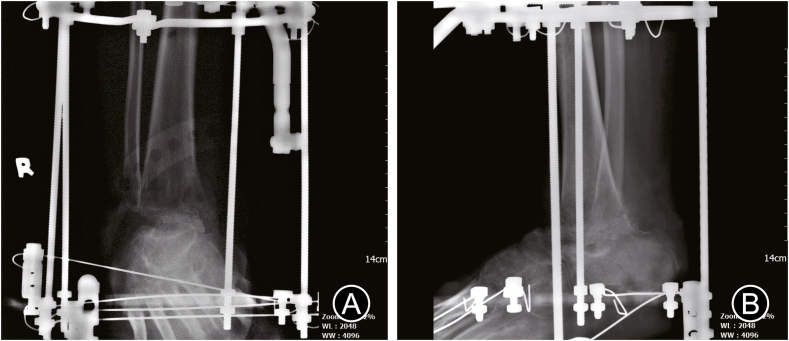
Fig. 5.
Radiograph right ankle 3 months postoperatively, anterior posterior (A) and lateral (B) views, with evidence of fusion.
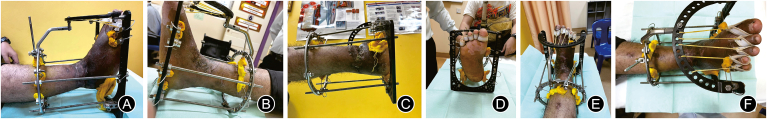
Fig. 6.
Clinical pictures during presentation at 3 months postoperatively. (A) Lateral aspect, (B) medial aspect, (C) posterior aspect and (D) anterior aspect of the ankle. (E) Dorsum aspect, and (F) plantar aspect of the foot.
Discussion
The talus is the sole bone in the lower limb devoid of muscle attachment, and the articular cartilage covers 35% of its surface, thus making the talus susceptible to injury. However, due to the robust support of ligament, talar dislocations are relatively rare.5 The talus will be pushed out of the ankle mortise when the external force surpasses the support of talus structure. With such force and displacement, it is no surprise that the skin is frequently ripped across the anterolateral part of the ankle.6
Due to high incidence of infection and avascular necrosis (AVN), treatment outcomes have been historically dismal. As a result, the earlier recommended treatments comprised talectomy and arthrodesis, or primary arthrodesis.7 However, recent large retrospective case series have demonstrated that AVN and infection rates are lower than previously thought. According to the study of Smith et al.8, none of the 19 patients with open extruded talus injuries developed reimplantation-related infection, and not every patient had poor findings on radiographic after a year follow-up.
Seetharam et al.1 stated in their experience of treating 10 patients with open fracture dislocation of talus and talar body extrusion by reimplantation, none of the 10 patients developed infection during their minimum 3 years of follow-up. AVN of the talus was present in 6 patients, and other 4 patients who had significant lateral ligamentous attachment did not exhibit osteonecrosis signs until in the last follow-up. In 1 case, radiological collapse features were observed. There were no tibiotalar or subtalar arthritic signs. At the 3 years follow-up, none of the patients reported having any hindfoot pain, and only 1 patient had a slight subtalar joint varus. They were all able to ambulate independently. In a distinct retrospective case series reporting 8 patients with talar extrusions, Burston et al.9 summarized the current literatures on talar extrusion and discovered that the prevalence of osteoarthritis was 16% and AVN was 30%, while the overall infection rate for extruded talus injury was 20%.
Based on the aforesaid literatures, the authors advised reimplanting the talus whenever practical, with emphasizing scrupulous cleaning of the talus. Smith et al.8 used a cleansing protocol for the reimplanted talus, which included soaking the talus in a sterile Bacitracin solution, careful intraoperative scrubbing, and 2 or 3 consecutives Bacitracin washes before reimplantation. Therefore, they did not experience any infection related to reimplantation.8 Studies conducted in vitro suggest that different cleaning methods, such as mild cleaning with 10% providone-iodine solution and then a regular saline wash, may achieve the ideal balance between microbial kill and chondrocyte maintenance.10
The advantages of talar reimplantation include maintenance of the normal mechanics and morphology of the hindfoot, as well as bone stock preservation for any future reconstructive surgeries.7 Following reimplantation, the extensive surface area at the site of talar neck fracture provides a far better possibility for the entry of new vascular channels into the talar body than the little area for potential vascular re-entry on the smooth cortical bone of an intact talar neck. In addition, no soft-tissue attachment following a complete extrusion may lead to a decreased in local inflammatory response and much less abrupt collapse. The notorious complication, AVN is not inevitable but if occurs, it is not always results in unfavourable outcomes.1
Decisions should be taken on a case-by-case basis. In our case, we decided not to reinsert the talus because of severe contamination, extensive soft tissue loss, and avascularity. In cases where the talus was extruded and the wound was contaminated, there is a substantial risk of infection. Reimplantation may be disputed if there are no soft tissue attachments due to avascular conditions and talus contamination, which may lead to sequestrum.11 According to the research of Hiraizumi et al.6, the impaired circulation brought on damage to the nearby vascular and lymphatic structures, which contributes to non-healing conditions, subsequently develops infection and makes the patient vulnerable for both acute and chronic bone infections.
The need for subsequent procedures is another concern if we proceeded with talar reimplantation regarding our situation. For some patients, it may be more challenging to establish fusion between the sclerotic talus and the tibia or calcaneus if the talus develops osteonecrosis.8 In our case, the tibiocalcaneal arthrodesis was delayed until the wound condition was optimum and the results of the culture, C-reactive protein, and erythrocyte sedimentation rate tests were all negative. Bone graft was not used in this patient in view of infection. The use of bone grafts to enhance arthrodesis sites is beneficial and even might be necessary in some specific circumstances, such as non-union, malunion, salvage osteomyelitis, and few more other reasons.12 The use of a vascularized medial femoral head autograft or an iliac crest autograft in conjunction with arthrodesis are additional graft options for arthrodesis in addition to the conventional autograft and allograft.13 In general, maintaining or restoring length, correcting angulations, and enhancing or stimulating osseous consolidation are reasons to use bone grafts at arthrodesis sites.12
In the presence of infection, the Ilizarov external fixator can be utilized for achieving tibiocalcaneal fusion. An arthrodesis can be performed with the Ilizarov external fixator without leaving a foreign body at the site of fusion like internal fixation, keeping the utilized pins and wires out of the injury infection zone. Johnson et al.14 described 4 patients had infections following attempted ankle fusions, in whom the talus has been completely or nearly completely destructed. Debridement and deformity correction using an Ilizarov external fixator were performed in the treatment of the patients. Three of the 4 patients had successful tibiocalcaneal fusion, and no recurring deep infections were observed. They discovered that as soon as rigid stability in the external fixator was attained, the sinus tracts stopped draining, and the wounds began to heal.14
Johnson et al.14 used the Ilizarov external fixator to conduct arthrodesis for the first time on a limited case series of 6 patients. Three out of 4 tibiocalcaneal arthrodesis and 2 tibiotalar arthrodesis surgeries were favourable.14 Many studies of ankle arthrodesis employing the Ilizarov external fixator have since been done, and this method is currently recognised as an established standard approach for treating challenging patients, such as those with chronic osteomyelitis, diabetes mellitus, similar conditions like this case, compromised soft tissue and infection.15
Timely identification of talus extrusion is critical since management is time-sensitive and emergent surgical intervention is required. When possible, as an alternative to amputation, reimplantation should be highly pursued because it may help to restore the most physiological joint mechanics, hindfoot height, and bone stock for functional and reconstructive interventions in the future. Tibiocalcaneal arthrodesis using an Ilizarov external fixator can be an effective salvage method for patients who have had a severe traumatic injury. It is also appropriate when there is infection, bone loss, or fragile soft tissue envelope. Good results can be obtained even if the talus has a profound infection or AVN.
Funding
This paper did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical statement
The patient gave the consent to display information related to the case report above to be displayed in a journal article.
Declaration of competing interest
None.
Author contributions
Shukriah Aqilah Zakaria: conceptualization, investigation, writing the original draft, review & editing. Mohd Saiful Adzuwan Mat Rodi: validation, review and supervision.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Seetharam V.B., Sunil B., Preetham M., et al. Extruded talar body: role of reimplatation. Int J Orthop Trauma Surg Sci. 2016;2:137–142. [Google Scholar]
- 2.Van Opstal N., Vandeputte G. Traumatic talus extrusion: case reports and literature review. Acta Orthop Belg. 2009;75:699–704. [PubMed] [Google Scholar]
- 3.Fortin P.T., Balazsy J.E. Talus fractures: evaluation and treatment. J Am Acad Orthop Surg. 2001;9:114–127. doi: 10.5435/00124635-200103000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Ortiz-Cruz J.R., Ojeda Boscana I.L. Talar extrusion, A very rare sequela of trauma: a case report. Am J Case Rep. 2019;20:575–579. doi: 10.12659/AJCR.913576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rochman R., Hutson J.J., Alade O. Tibiocalcaneal arthrodesis using the Ilizarov technique in the presence of bone loss and infection of the talus. Foot Ankle Int. 2008;29:1001–1008. doi: 10.3113/FAI.2008.1001. [DOI] [PubMed] [Google Scholar]
- 6.Hiraizumi Y., Hara T., Takahashi M., et al. Open total dislocation of the talus with extrusion (missing talus): report of two cases. Foot Ankle. 1992;13:473–477. doi: 10.1177/107110079201300808. [DOI] [PubMed] [Google Scholar]
- 7.Lamothe J.M., Buckley R.E. Talus fractures: a current concepts review of diagnoses, treatments, and outcomes. Acta Chir Orthop Traumatol Cech. 2012;79:97–106. [PubMed] [Google Scholar]
- 8.Smith C.S., Nork S.E., Sangeorzan B.J. The extruded talus: results of reimplantation. J Bone Joint Surg Am. 2006;88:2418–2424. doi: 10.2106/JBJS.E.00471. [DOI] [PubMed] [Google Scholar]
- 9.Burston J.L., Isenegger P., Zellweger R. Open total talus dislocation: clinical and functional outcomes: a case series. J Trauma. 2010;68:1453–1458. doi: 10.1097/TA.0b013e3181d03b73. [DOI] [PubMed] [Google Scholar]
- 10.Bruce B., Sheibani-Rad S., Appleyard D., et al. Are dropped osteoarticular bone fragments safely reimplantable in vivo? J Bone Joint Surg Am. 2011;93:430–438. doi: 10.2106/JBJS.J.00793. [DOI] [PubMed] [Google Scholar]
- 11.Choi Y.R., Jeong J.J., Lee H.S., et al. Completely extruded talus without soft tissue attachments. Clin Pract. 2011;1:e12. doi: 10.4081/cp.2011.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Catanzariti A.R. Graft-enhanced arthrodesis. J Foot Ankle Surg. 1996;35:463–473. doi: 10.1016/S1067-2516(96)80068-8. [DOI] [PubMed] [Google Scholar]
- 13.Abdulazim A.N., Reitmaier M., Eckardt H., et al. The Masquelet technique in traumatic loss of the talus after open lateral subtalar dislocation-A case report. Int J Surg Case Rep. 2019;65:4–9. doi: 10.1016/j.ijscr.2019.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson E.E., Weltmer J., Lian G.J., et al. Ilizarov ankle arthrodesis. Clin Orthop Relat Res. 1992;280:160–169. [PubMed] [Google Scholar]
- 15.Reinke C., Lotzien S., Yilmaz E., et al. Tibiocalcaneal arthrodesis using the Ilizarov fixator in compromised hosts: an analysis of 19 patients. Arch Orthop Trauma Surg. 2022;142:1359–1366. doi: 10.1007/s00402-021-03751-0. [DOI] [PMC free article] [PubMed] [Google Scholar]