Abstract
Many states are experiencing a behavioral health workforce crisis, particularly in the public behavioral health system. An understanding of the factors influencing the workforce shortage is critical for informing public policies to improve workforce retention and access to care. The aim of this study was to assess factors contributing to behavioral health workforce turnover and attrition in Oregon. Semistructured qualitative interviews were conducted with 24 behavioral health providers, administrators, and policy experts with knowledge of Oregon’s public behavioral health system. Interviews were transcribed and iteratively coded to reach consensus on emerging themes. Five key themes emerged that negatively affected the interviewees’ workplace experience and longevity: low wages, documentation burden, poor physical and administrative infrastructure, lack of career development opportunities, and a chronically traumatic work environment. Large caseloads and patients’ high symptom acuity contributed to worker stress. At the organizational and system levels, chronic underfunding and poor administrative infrastructure made frontline providers feel undervalued and unfulfilled, pushing them to leave the public behavioral health setting or behavioral health altogether. Behavioral health providers are negatively affected by systemic underinvestment. Policies to improve workforce shortages should target the effects of inadequate financial and workplace support on the daily work environment.
The United States is facing a critical shortage in the behavioral health workforce across a broad range of providers—including psychiatrists, psychologists, nurses, counselors, therapists, case managers, social workers, and peer support specialists—who deliver mental health and substance use services. This shortage has been compounded by inequitable distribution of providers, rising burnout, and challenges with employee recruitment and retention. Workforce expansion is needed as a response to growing population health demands. Approximately one of three U.S. adults experiences a mental health or substance use condition, and behavioral health service gaps are increasing across many states (1). High demand for behavioral health services has been exacerbated by the COVID-19 pandemic, which has been associated with higher prevalence of depression and anxiety symptoms (2) and record rates of overdose deaths and suicide attempts (3). Despite the need for improved access to behavioral health services, one-third of those with any mental illness report unmet needs. These service gaps are even more prevalent among individuals with serious mental illness (including schizophrenia, bipolar disorder, and other mental health conditions causing functional impairment) as well as those with substance use disorders (4).
Access issues are compounded within the public behavioral health system, which provides services and programs to some of the country’s most vulnerable individuals—including a disproportionate share of those with serious mental illness—with limited resources (5). The public behavioral health system is generally financed through a combination of Medicaid payments and local, state, and federal grants. The system is composed of community health clinics, school and community-based organizations, and state mental health hospitals, jails, and other entities (6). In many ways, the public behavioral health system acts as a safety net by serving low-income populations, including people receiving Medicaid, people without insurance, and people at high risk for behavioral health problems (7, 8). High turnover and attrition of providers are notable problems in the public behavioral health system, with an annual industry turnover average of about 30% (9, 10). Turnover results in loss of expertise and institutional knowledge, high costs for recruitment and training of replacement providers, and care disruptions and delays for patients (11).
Addressing workforce shortages is a high priority for state and federal policy makers. In recent years, a number of policy proposals have been developed or implemented to address behavioral health workforce shortages across states, including efforts to raise reimbursement rates for behavioral health services (12, 13), increase support for telehealth (14, 15), expand loan forgiveness and recruitment programs for trainees (16, 17), and establish stable funding mechanisms for behavioral health programs through the certified community behavioral health clinics (CCBHCs) overseen by the Centers for Medicare and Medicaid Services (18). The success of these policies relies on an understanding of the factors contributing to behavioral health provider turnover and attrition in public behavioral health systems. Although a body of literature has examined factors contributing to provider burnout across various training stages (19) and settings (20), including acute care hospitals (21) and primary care (22, 23), little recent work has examined which factors contribute to shortages of behavioral health providers in public health systems.
The well-being and stability of the clinical workforce, particularly in the public behavioral health system, are crucial to the U.S. health system. In this study, we conducted qualitative interviews with providers, administrators, and policy experts with knowledge of the public behavioral health system in Oregon, which (like many states) is facing a workforce shortage and high rates of unmet behavioral health needs (24). Our objective was to assess factors contributing to workforce turnover and attrition in Oregon’s public behavioral health system, with a focus on challenges in the clinical work environment. This study was designed to expand the limited qualitative data on this topic and shed light on the perspectives of behavioral health professionals with firsthand experience of working in the field.
METHODS
Setting
Owing to high need and inadequate treatment access, Oregon ranked 49th out of 50 states and the District of Columbia for unmet behavioral health needs among adults (25). Nearly 6% of the state’s 4 million residents have a serious mental illness. In Oregon, between 2017 and 2019, only about four of 10 adults with any mental health condition received mental health services (26).
Oregon’s public behavioral health system is primarily composed of its state inpatient psychiatric hospital, which predominantly serves justice-involved persons (27), and its community mental health centers. Community mental health centers are typically outpatient programs that are heavily reliant on public funds and provide mental health care for individuals with moderate-to-serious mental health conditions, including schizophrenia, bipolar disorder, and other conditions causing functional impairment. These services are usually covered by Oregon’s Medicaid program, but patients ineligible for Medicaid may qualify for sliding-scale treatment programs. Patients with private insurance usually make up a minority of the patient population at these sites (7). Community mental health centers in Oregon include federally qualified health centers (FQHCs), CCBHCs, and community mental health programs (CMHPs). In each of Oregon’s 36 counties, CMHPs provide a variety of clinical and rehabilitative community-based safety-net services via contract with the Oregon Health Authority (OHA) or a local mental health authority.
Recruitment and Sampling
Interviews were conducted as part of a larger evaluation funded through House Bill 2086, which was passed by the Oregon State Legislature in 2021 to provide recommendations for achieving a living wage for behavioral health workers (28). Key informants were identified in collaboration with the OHA, which helped connect us with key representatives of the state’s behavioral health system. We used purposive sampling to ensure representation from various racial-ethnic groups, geographic regions, work settings (e.g., CMHP, CCBHC, FQHC), and job descriptions (e.g., mental health therapists, addiction counselors, peer providers, psychiatrists). The number of interviews (N=24) was largely predetermined by the OHA, on the basis of the study’s budget and scope of work, but was adjusted to ensure saturation. Forty-one potential interviewees were contacted, up to two times via e-mail, from August to October 2021, with a response rate of 59%. Participants were compensated for their time via electronic gift cards. This study was approved by the Oregon Health & Science University Institutional Review Board (number 23375).
Data Collection and Analysis
In this study, we used a phenomenological approach. This kind of approach is commonly used in qualitative research to capture participant experiences and perceptions of a particular phenomenon. In this approach, the analysis includes identifying commonalities across participant experiences that can potentially be translated into general themes (29). The study team developed the semistructured interview guide with input from two behavioral health experts. Two authors (E.H. and D.H.) with qualitative interviewing experience conducted 23 interviews in English between September and November 2021. One interview was conducted in Spanish, with a translated interview guide, by an OHA staff member who was fluent in Spanish. Participants were asked about their roles and experiences within the behavioral health system, including their experiences with wages, reimbursement rates, billing processes, challenges recruiting or retaining staff, and barriers to training and career development. Each interview was conducted via remote teleconferencing and lasted 45–60 minutes. We obtained verbal consent from the participants prior to recording. Audio recordings were professionally transcribed (in one case, transcribed and then translated from Spanish to English) and checked for accuracy.
We used a directed thematic content analysis approach to develop a codebook. Initial codes were based on literature and existing knowledge about workforce turnover and attrition in the behavioral health system. Three authors (E.H., E.S., and V.A.) then independently coded two interviews with the initial codes. Data that could not be coded or that produced conflicting results from different coders were reviewed to determine whether they could be captured or reconciled by creating a new code or by clarifying existing code definitions. After agreement was reached, all interviews were double-coded, by the same three coders, according to the refined codebook. Two coders (E.H. and E.S.) met to reconcile coding differences through discussion and review of the code definitions in order to achieve intercoder agreement for each interview before beginning the analysis. Each of the two coders (E.H. and E.S.) independently reviewed the code reports to generate emerging themes, then met to discuss results and to reach consensus about factors contributing to participants’ workplace experiences. Analyses were conducted by using ATLAS.ti, version 22.
RESULTS
We conducted 24 qualitative interviews with behavioral health providers, program administrators and leaders, state association or agency administrators, and policy experts with knowledge of the public behavioral health system in Oregon (Table 1). Most of the interviewees (N=19, 79%) were current frontline behavioral health providers or had clinical experience but had shifted to an administrative role within the behavioral health field. Findings from the interviews are summarized and presented visually in Figure 1. Interviewees identified various interconnected factors affecting their workplace experience that we designated across three levels: system, organizational, and individual. System-level factors included overarching government policies and societal views on behavioral health; organizational-level factors were those related to infrastructure, administration, and support within an organization or workplace; and individual-level factors encompassed day-to-day experiences affecting an individual’s financial, emotional, or physical well-being. These factors coalesced into direct drivers of turnover and attrition, which we identified as chronic trauma and stress in the workplace, feeling undervalued and unsupported, and lack of fulfillment or sense of purpose. Five major themes emerged from the analysis of the various factors. Example quotations for the five themes are provided in Table 2, and a glossary of terms is available in the online supplement to this article.
TABLE 1.
Characteristics of participants (N524) and their organizations within the public behavioral health system in Oregon
| Characteristic | N | % |
|---|---|---|
| Participant characteristics | ||
| Gender | ||
| Male | 10 | 42 |
| Female | 14 | 58 |
| Race-ethnicitya | ||
| White | 7 | 29 |
| Black or African American | 5 | 21 |
| Latinx or Hispanic | 4 | 17 |
| American Indian or Alaska Native | 1 | 4 |
| Declined to report | 9 | 38 |
| Occupation | ||
| Former provider, transitioned to administrator | 10 | 42 |
| Current provider | 9 | 38 |
| State association or agency leader | 3 | 12 |
| Policy expert | 2 | 8 |
| Current setting | ||
| Inpatient | 1 | 4 |
| Outpatient | 15 | 63 |
| Both | 3 | 12 |
| Nonclinical | 5 | 21 |
| Region of Oregon representedb | ||
| Portland metro | 7 | 29 |
| Willamette Valley and north coast | 6 | 25 |
| Southwestern | 0 | — |
| Central | 2 | 8 |
| Eastern | 2 | 8 |
| Statewide | 5 | 21 |
| Other states/national | 2 | 8 |
| Organization characteristicsc | ||
| Community mental health program | 10 | 42 |
| Certified community behavioral health clinic | 5 | 21 |
| Recovery-support nonprofit | 3 | 12 |
| Government agency | 3 | 12 |
| Nonprofit association | 2 | 8 |
| Health system | 2 | 8 |
| Academic institution | 2 | 8 |
| Federally qualified health center | 1 | 4 |
| Outpatient clinic | 1 | 4 |
Participants self-reported their race-ethnicity and may have selected more than one category.
Regions were defined by the Oregon Department of Transportation.
Organizations could belong to more than one category.
FIGURE 1. Factors influencing turnover and attrition in the public behavioral health system workforce in Oregona.
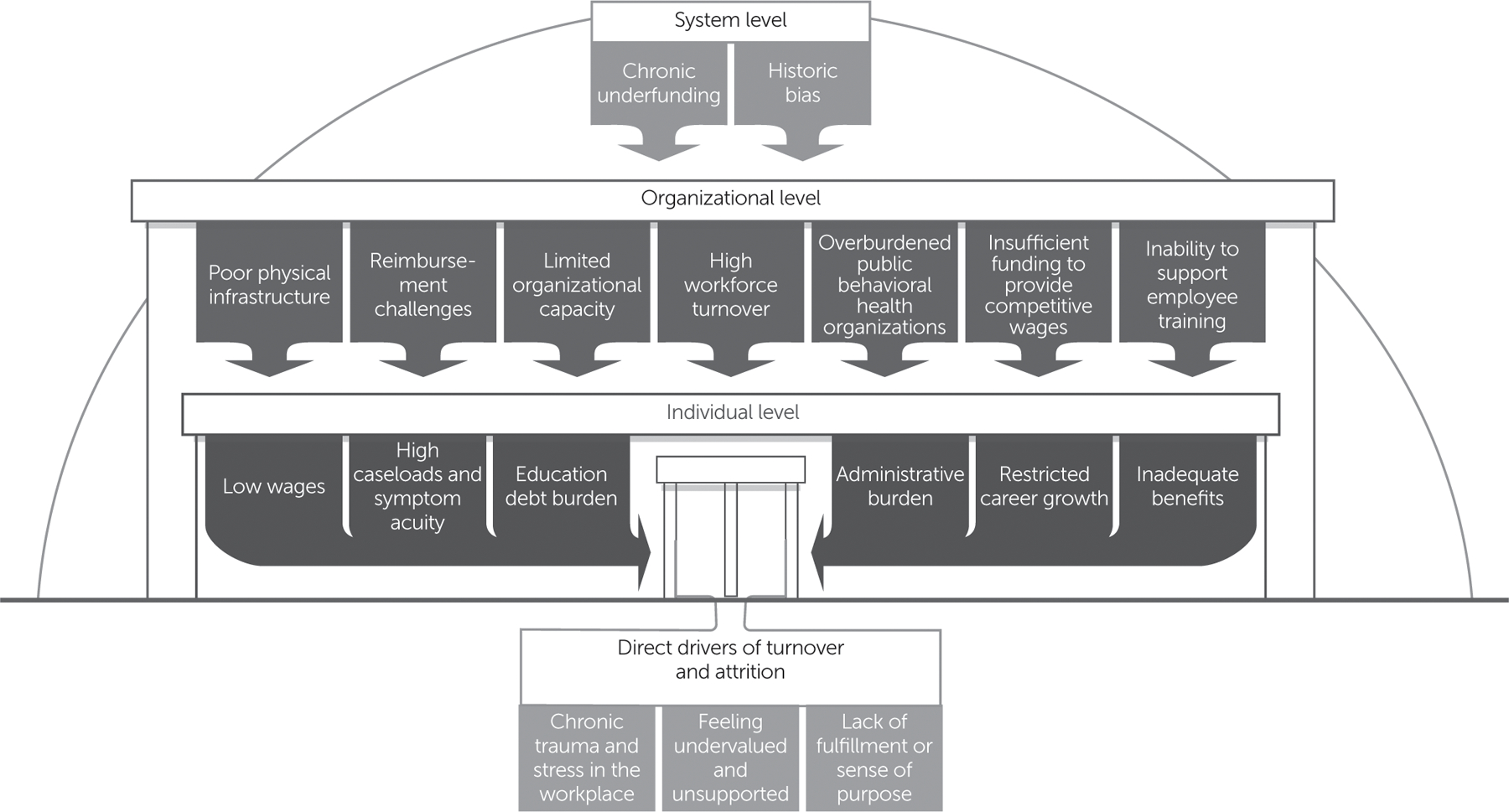
a Interviewees identified factors across three levels—system, organizational, and individual—that contribute to the direct drivers of workforce turnover and attrition.
TABLE 2.
Key themes and representative quotations from interviewees (N524) in the behavioral health system in Oregon
| Theme | Quotation |
|---|---|
| Low wages | “We have a lot of people in the field [who] want to be here … but they can’t afford … this job. They’re trying to put two halves together to make a whole.” (residential treatment director) “There’s no attraction. Why would you want to work here when you can [work] elsewhere and make more than we have the ability to offer?” (community mental health program director) |
| Documentation burden | “How do we have the experience of our workforce be directed at supporting community members, rather than meeting all of the administrative requirements? This work is so hard, and those requirements on top of it [are] wearing our folks down.” (county behavioral health director) “We’re always constantly changing things … [in order to meet reporting standards], which then puts an additional strain on clinicians and staff alike, because they’re trying to run and catch up to things.” (residential treatment director) |
| Poor administrative and physical infrastructure | “I heard it from one of my legislators—he’s saying, ‘What about all the new money?’ Well, it doesn’t cover [current needs]. [The] infrastructure that hasn’t been dealt with. You can slap a coat of paint on something that is not working well, but … you may need to replace it or you may need to take it down to bare wood.” (community mental health program director) “We have different funders for every activity that we do as a behavioral health business. There is no flexibility in any of the funding streams.” (behavioral health association administrator) “[Billing for dual-diagnosis clients is really difficult], because you either have to bill [service delivery] on the substance use disorder side or you have to bill it on the mental health side. It’s as if a person is split down the middle. It’s just this constant battle for billing.” (certified community behavioral health clinic director) |
| Lack of opportunities for career development | “Peers do so much across the state. How can that movement be in a positive direction for peers to not only be able to know that they can advance, but also have a track that they can grow incrementally, education-wise, and be incentivized by the pay structure?” (former peer provider, current administrator) “It has to be a system that allows people to leave work to be trained. Right now, folks are so busy with making sure they’re seeing the people they’re supposed to see [to] generate the revenue that their organizations need. There isn’t time to be able to move away from that grind to actually be engaged in ongoing training.” (state agency administrator) |
| Chronically traumatic work environment | “In our setting [county behavioral health], we tend to see people who are very ill for very long times; we don’t have the satisfaction of seeing people get better. The community is taking care of people who 10 years ago would have been in a hospital. It’s putting out fires almost every single day. You can only do that for so long [before] you are going to be burned out.” (community mental health program director) “The amount of work and … trauma this workforce goes through is immense, [including] enormous caseloads because of a shortage of other staff. [They are] having to work … longer and harder, because they don’t have that access to the higher level [of care]. So, they are enduring all the stress and trauma and burnout and overwork.” (former peer provider, current administrator) |
Theme 1: Low Wages
Participants generally agreed that the public behavioral health field requires high educational investment but offers low financial return, with several participants attributing low wages to historical reliance on provider goodwill. Across the state, several participants reported that wages for entry-level behavioral health positions were on par with or lower than those at fast-food restaurants in their locales. In addition, insufficient supervisory and leadership roles limited opportunities for promotion and wage progression. As a result, participants reported more difficulty alleviating debt burdens compared with peers in medical professions with higher entry-level wages.
A frequent observation was that public behavioral health organizations could not compete, in wages or benefits, with national telehealth companies or large hospitals at any level of staffing. Five participants reported leaving their employer or turning down otherwise desired positions because of low wages or inadequate benefits (e.g., lack of affordable health insurance). Eight participants reported that in recent years, their organizations had not offered cost-of-living increases, differential pay for language skills or other additional service provision, or supplemental benefits (e.g., professional development funds).
Participants felt that low reimbursement rates for services directly limited the salaries and benefits offered by their employers. Several participants believed that lower reimbursement rates—particularly compared with those for general medical services—were a remnant of historical bias toward the behavioral health field, which resulted in persistent stigma and financial undervaluing of behavioral health services. A state association administrator said, “The behavioral health system has been underfunded for decades. You can’t pay people more than [an organization] gets paid to do the work.” Participants felt that low salaries actively pushed employees out of the public behavioral health system or out of behavioral health completely, contributing to workforce shortages.
Theme 2: Documentation Burden
Many participants shared that documentation and reporting burdens often exceeded what they could feasibly complete in a standard work week and felt that this burden significantly contributed to provider-level stress, burnout, and turnover in the public behavioral health system. A director of a community mental health organization reflected, “[A] leading reason … people leave the public behavioral health system is administrative burden. It seems meaningless. It doesn’t make them happy.” Participants felt that documentation burden directly reduced time available for patient care. For example, a program manager at an outpatient mental health clinic described a near-continuous communication loop with insurers to receive prior authorizations for basic services and to get claims approved; some claims were ultimately denied because of formatting issues. Funding streams were often fragmented between different entities with incompatible documentation requirements, demanding hours of staff time to receive full reimbursement for services.
Many participants perceived the public behavioral health system as held to a higher standard of reporting and accountability compared with the general medical health system. Several participants believed that policy makers and state leaders expected evidence of financial cost savings or documentation of treatment efficacy in behavioral health, which exceeded standards in general medical health. For example, to receive full reimbursement, providers were often required to conduct an assessment, write a treatment plan, and make a diagnosis before providing any services to a potential client. Other providers struggled to meet the changing reporting metrics required to maintain the CCBHC or evidence-based program designation and associated funding. Nonintegrated health information technology systems made it difficult for staff to track clients across settings and locations and to locate the historical documents necessary for these assessments and reports.
Theme 3: Poor Administrative and Physical Infrastructure
Much frustration was voiced about inadequate operational support in the public behavioral health system, including poor administrative and physical infrastructure. Regarding administrative support, participants reported that their organizations often had insufficient and inconsistent funding available to hire human resources, administrative, and supervisory staff. Many participants described long delays in hiring and onboarding new employees, which forced them to maintain large caseloads for months at a time.
Multiple participants reported that their small facilities operated in a state of disrepair, which lowered morale and forced staff to operate in outdated buildings that the clinics had outgrown. Organizations with few financial resources often used temporary state or community grants to provide basic services or to hire staff, which limited physical infrastructure investment. A state agency administrator reflected,
How are we paying for the infrastructure to create environments where people feel good about where they work? How do we ensure that they have data systems that support their work? All of that gets in the way of retention and recruitment. Who wants to come to work in an environment that isn’t very clean?
Many participants noted a general lack of facilities, especially in rural areas, to treat a spectrum of behavioral health needs.
Participants commented that fragmented, capitated funding streams for behavioral health services left little room for operational flexibility, which necessitated a choice between providing services, increasing wages, or maintaining infrastructure and did not align with the aims of delivering integrated, evidence-based care. Thirteen participants reported pervasive coding and billing limitations and inefficiencies, including considerable limitations regarding types of reimbursable services and provider billing eligibility. For example, a peer services coordinator noted that only five Medicaid codes were available for peer providers to use in billing and that these codes did not reflect the workers’ scope of services or cover the cost of their positions. State and organization-imposed limits on the types and number of services that unlicensed providers could submit for reimbursement created frustration and stress among workers. Complex billing rules also existed for clients with co-occurring mental and substance use disorders.
Theme 4: Lack of Career Development Opportunities
Several participants noted that minimal organizational support, burdensome training requirements, and an ill-defined career ladder contributed to their perception of insufficient career development opportunities. Participants described substantial variation in organizational policies for paid time off or financial assistance for job-related training. Independent of official policies, some participants felt unable to participate in job-related training because of inadequate staffing, large caseloads, and loss of potential billable hours for the organization. A few participants shared that training rarely fit their schedules, was an out-of-pocket cost, or was not offered in their native language. Three participants reported that they were ineligible for many loan repayment programs or other financial support for training because they were part of the unlicensed workforce. Most participants felt that support for efficient training and licensure pathways had not been prioritized at the federal or state system level.
Many participants felt that career advancement opportunities were unclear or nonexistent; specifically, these participants felt that public behavioral health jobs did not have defined career paths with established supervisory or leadership positions. Others described inadequate mentorship from senior providers or behavioral health leaders as a result of the competing burden of daily workloads and lack of financial incentives for mentoring, both of which deprioritized professional development for junior employees. These factors contributed to a sense of disillusionment, with a few participants viewing public behavioral health as an unsustainable career choice in the medium and long term.
Theme 5: Chronically Traumatic Work Environment
Consistently large caseloads, patients with acute symptoms, and a general feeling of insufficient organizational support created a high-stress daily work environment for many participants. These challenges, along with ongoing secondary traumatic stress from caring for people exposed to trauma, were felt by most to directly drive stress and turnover. A child and adolescent psychiatrist said,
Burnout, it’s like a boulder gaining steam. As you have staff attrition and challenges recruiting, the few therapists [who] remain have a higher caseload, perhaps with greater production expectations to make up for that loss of the other providers. That’s almost like a death spiral for the organization from a burnout perspective—how do we stop the bleeding?
In addition to larger caseloads, participants commented on a general rise in patients’ symptom acuity. Multiple participants observed that new graduates who entered the workforce often were not prepared for the level of patients’ symptom severity or complexity in their caseloads and quickly became overwhelmed. The rapid turnover of new providers created additional stressors for remaining providers, who often had to absorb more clients. Providers at CMHPs described having large caseloads of patients with complex symptoms who required services for long periods of time, which they felt was due in part to lack of bed and space availability at the inpatient level of care.
Many participants reported that organizational leaders did not adequately recognize or compensate for the chronic workplace trauma the providers experienced as a result of large caseloads and patients’ high symptom acuity. For example, several participants described challenges in requesting time off and advocating for culturally relevant care or appropriate services for their patients. Certain job duties, such as supervising interns or translating documentation, were routinely uncompensated. Behavioral health providers in understaffed rural areas reported performing more than one job within their organization or working at a level of responsibility above that for which they had been hired. Most participants felt that the taxing work environment disincentivized long-term retention, especially when other settings, such as telehealth or private practice, could offer lower patient symptom acuity, higher wages, and a more flexible work environment.
DISCUSSION
The public behavioral health system serves as a safety net for individuals with mental illness and substance use disorders, many of whom have low incomes (30–32). Entities financed in part or in full by public funds (e.g., county behavioral health sites, CCBHCs, FQHCs, and jails) provide essential emergency services, clinical outpatient and inpatient services, as well as rehabilitation and community support. In recent years, demand for behavioral health services at entities primarily supported by public funds has increased, and employee turnover and workforce shortages have accelerated (33, 34). In interviews with public behavioral health providers, administrators, and policy experts in Oregon, we identified five key themes—low wages, high documentation burden, poor infrastructure, lack of career development opportunities, and a chronically traumatic work environment—that influenced turnover and attrition of the public behavioral health workforce across provider types, work settings, and geographic regions. The persistence of these challenges, which likely have worsened since the COVID-19 pandemic began (35), has important implications for the long-term stability of this essential workforce.
Although we focused on a single state, findings specific to Oregon’s behavioral health workforce challenges are potentially generalizable to other contexts (33). As in other states, Oregon’s public behavioral health system is heavily reliant on the Medicaid program, although health system financing, organization, and delivery differ from those of other state Medicaid programs. Although behavioral health workforce shortages have local and regional footprints, they constitute a national crisis with similar contours. Nearly every U.S. state is facing projected shortages of psychiatrists, psychologists, and other behavioral health providers—all caused by similar systemic issues (36). Thus, the experiences of Oregon’s frontline behavioral health workers add context for policy discussions.
Our findings suggested that multiple interacting factors contribute to job dissatisfaction for the behavioral health workforce. Some of these factors have been documented, such as low reimbursement rates for behavioral health services (37). In response, more than half of all states are implementing rate hikes or planning to raise reimbursement rates during the next 2 years (38). However, our interviews highlighted that other factors—for example, clinical and regulatory burden, chronic stress, and lack of professional development opportunities—also appeared to be important. Many of these factors are recognized predictors of burnout. Although there is a robust body of literature on protective strategies to combat burnout (39–41) (e.g., addressing work satisfaction, organizational respect, employer care, and work-life integration) (42), these strategies were infrequently cited by our interviewees. As such, reimbursement rate hikes are necessary, but likely insufficient, tools for improving workforce capacity, and commensurate attention is needed to address other factors.
Our findings suggested a need for organizational approaches to support workforce capacity and individual job satisfaction in a public behavioral health system. Potentially beneficial strategies may include streamlining hiring processes, providing paid time off to pursue continuing education and professional development training, creating supervisory roles that are compensated for time and effort, and encouraging organizational leaders to consistently recognize both the work that behavioral health providers perform and the chronic trauma that they face in their daily work.
Ultimately, organizational approaches, including positive leadership and workplace support, rely on adequate funding. Much current policy attention and funding at the federal level are directed toward bolstering the behavioral health workforce to meet public health demands. For example, the Consolidated Appropriations Act (43), passed in December 2022, authorized new provisions to address behavioral health workforce shortages, including new psychiatry residency positions, new funds that can be used toward workforce initiatives for peer support providers, and expanded loan repayment programs for behavioral health professionals.
Similar efforts are being made at the state level. During the 2021–2023 biennium, the Oregon State Legislature appropriated $1.35 billion to support large-scale improvements to the state’s behavioral health system (44). The OHA, which administers Medicaid and helps support public behavioral health services in the state, has been tasked with allocating these funds to strengthen infrastructure and to increase access to services. Planned funding includes grants to the state psychiatric hospital to convert temporary positions into permanent jobs, add staff, and offer wage increases (45, 46). Moreover, grants for behavioral health organizations are intended to be used for increasing staff compensation and implementing policies to improve workforce retention and recruitment (47). Many other states, including Virginia and North Carolina, are engaging in their own efforts to address their behavioral health workforce crises through expanded funding (28). These efforts are crucial and should be implemented in conjunction with approaches that address the three direct drivers of turnover and attrition identified by our interviewees.
This study had several limitations. The study sample was small and was restricted to a single state, limiting generalizability of the findings. Although efforts were made to ensure representation across a variety of interviewee characteristics, women were overrepresented at high levels of organizational leadership, and participants from Oregon’s southwestern region were underrepresented. We did not systematically collect data on age or sexual orientation from our participants. In addition, this was a cross-sectional study that assessed participants’ experiences at a time when much of the funding appropriated by the Oregon State Legislature in the 2021–2023 biennium had not yet been distributed. Allocation of this additional funding to public behavioral health organizations has the potential to alter the findings of our study.
CONCLUSIONS
Our findings suggest that turnover and attrition in Oregon’s public behavioral health system are worsened by the chronic trauma and stressors that behavioral health providers experience in their daily work environment. Our participants reported that these stressors are exacerbated by high symptom acuity among patients, substantial administrative burdens, and inadequate workplace support. In the context of the growing gap between behavioral health service demand and delivery, resulting in part from a critical workforce shortage, organizational efforts to improve the work environment and workplace satisfaction are needed, alongside systemic investment in the public behavioral health system.
Supplementary Material
HIGHLIGHTS.
As is the case in many states, the public behavioral health system in Oregon is facing critical workforce shortages, high provider turnover, and poor employee retention, all of which limit patient access to services.
In qualitative interviews with behavioral health providers, administrators, and policy experts in Oregon, five key themes were found to negatively affect workplace experience and employee retention: low wages, documentation burden, poor infrastructure, lack of career development opportunities, and a chronically traumatic work environment.
Policies to improve workforce shortages should target the negative impacts of inadequate financial and workplace support on the daily work environment.
Acknowledgments
This study was funded in part by the Oregon Health Authority through a contract with the Center for Health Systems Effectiveness (Drs. Zhu and McConnell), Oregon Health & Science University. Dr. Zhu was funded by NIMH grant K08MH123624. The authors thank Craig Mosbaek, M.P.H., for assisting with community engagement and interviewee recruitment; Lynnea Lindsey, Ph.D., M.S.C.P., and Sue Skillman, M.S., for providing contextual knowledge; Daniel Garcia, M.S.W., for conducting an interview in Spanish; and the interview participants for sharing their time, experiences, and insight.
Footnotes
These views represent the opinions of the authors and not necessarily those of the Oregon Health Authority. The NIMH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Dr. Howington received contracting fees from the Center for Health Systems Effectiveness for work on this project. Dr. Zhu has received funding from the National Institute for Health Care Management Foundation. The other authors report no financial relationships with commercial interests.
Contributor Information
Eliza Hallett, Center for Health Systems Effectiveness, School of Medicine, Oregon Health & Science University, Portland
Erika Simeon, Center for Health Systems Effectiveness, School of Medicine, Oregon Health & Science University, Portland
Vineeth Amba, Robert Wood Johnson Medical School, Rutgers University, New Brunswick, New Jersey
Devin Howington, Center for Health Systems Effectiveness, School of Medicine, Oregon Health & Science University, Portland
K. John McConnell, Center for Health Systems Effectiveness, School of Medicine, Oregon Health & Science University, Portland
Jane M. Zhu, Division of General Internal Medicine, School of Medicine, Oregon Health & Science University, Portland
REFERENCES
- 1.Olfson M: Building the mental health workforce capacity needed to treat adults with serious mental illnesses. Health Aff 2016; 35: 983–990 [DOI] [PubMed] [Google Scholar]
- 2.Vahratian A, Blumberg SJ, Terlizzi EP, et al. : Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic—United States, August 2020–February 2021. MMWR Morb Mortal Wkly Rep 2021; 70:490–494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spencer MR, Miniño AM, Warner M: Drug Overdose Deaths in the United States, 2001–2021. NCHS Data Brief no 457 Hyattsville, MD, National Center for Health Statistics, 2022. https://stacks.cdc.gov/view/cdc/122556. Accessed Mar 21, 2023 [Google Scholar]
- 4.Key Substance Use and Mental Health Indicators in the United States: Results From the 2020 National Survey on Drug Use and Health HHS pub no PEP21-07-01-003 Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2021https://www.samhsa.gov/data/sites/default/files/reports/rpt35325/NSDUHFFRPDFWHTML-Files2020/2020NSDUHFFR1PDFW102121.pdf [Google Scholar]
- 5.America’s Health Care Safety Net: Intact But Endangered Edited by Lewin ME, Altman S. Washington, DC, National Academies Press, 2000 [PubMed] [Google Scholar]
- 6.Miller JE: Too Significant to Fail: The Importance of State Behavioral Health Agencies in the Daily Lives of Americans With Mental Illness, for Their Families, and for Their Communities Alexandria, VA, National Association of State Mental Health Program Directors, 2012 [Google Scholar]
- 7.Willging CE, Sommerfeld DH, Aarons GA, et al. : The effects of behavioral health reform on safety-net institutions: a mixed-method assessment in a rural state. Adm Policy Ment Health 2014; 41:276–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waitzkin H, Williams RL, Bock JA, et al. : Safety-net institutions buffer the impact of Medicaid managed care: a multi-method assessment in a rural state. Am J Public Health 2002; 92:598–610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brabson LA, Harris JL, Lindhiem O, et al. : Workforce turnover in community behavioral health agencies in the USA: a systematic review with recommendations. Clin Child Fam Psychol Rev 2020; 23:297–315 [DOI] [PubMed] [Google Scholar]
- 10.Report to Congress on the Nation’s Substance Abuse and Mental Health Workforce Issues Rockville, MD, Substance Abuse and Mental Health Services Administration, 2013 [Google Scholar]
- 11.Paris M, Hoge MA: Burnout in the mental health workforce: a review. J Behav Health Serv Res 2010; 37:519–528 [DOI] [PubMed] [Google Scholar]
- 12.Support Our Direct Care Workforce. NC HB914, 2021–2022 Reg Sess. Raleigh, North Carolina General Assembly, 2021. https://ncleg.gov/BillLookUp/2021/H914
- 13.Relating to Behavioral Health OR HB3046, 2021 Reg Sess. Salem, Oregon State Legislature, 2021. https://olis.oregonlegislature.gov/liz/2021R1/Measures/Overview/HB3046 [Google Scholar]
- 14.Goldman ML, Druss BG, Horvitz-Lennon M, et al. : Mental health policy in the era of COVID-19. Psychiatr Serv 2020; 71: 1158–1162 [DOI] [PubMed] [Google Scholar]
- 15.Chu RC, Peters C, De Lew N, et al. : State Medicaid Telehealth Policies Before and During the COVID-19 Public Health Emergency. Issue brief no HP-2021-17 Washington, DC, US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation, 2021. https://aspe.hhs.gov/sites/default/files/2021-07/medicaid-telehealth-brief.pdf [Google Scholar]
- 16.Massachusetts Loan Repayment Program for Health Professionals: Program Guide. Boston, Massachusetts League of Community Health Centers, 2022. https://www.massleague.org/Programs/WorkforceDevelopment/2022MLRPGuide.pdf
- 17.DSRIP Statewide Investments Student Loan Repayment Program. Boston, Massachusetts League of Community Health Centers, 2021. https://massleague.org/Programs/DSRIPStatewideInvestments/SLRPInfoforApplicants.pdf
- 18.FY 2022 Certified Community Behavioral Health Clinic Planning, Development, and Implementation Grant: Notice of Funding Opportunity Rockville, MD, Substance Abuse and Mental Health Services Administration, 2022. https://www.samhsa.gov/sites/default/files/grants/pdf/fy-22-ccbhc-pdi-nofo.pdf [Google Scholar]
- 19.Mongrain K, Simmons A, Shore I, et al. : Side-by-Side: a one-on-one peer support program for medical students. Acad Med 2022; 97:1170–1174 [DOI] [PubMed] [Google Scholar]
- 20.Dyrbye LN, West CP, Sinsky CA, et al. : Physicians’ experiences with mistreatment and discrimination by patients, families, and visitors and association with burnout. JAMA Netw Open 2022; 5: e2213080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahoney ST, Strassle PD, Schroen AT, et al. : Survey of the US surgeon workforce: practice characteristics, job satisfaction, and reasons for leaving surgery. J Am Coll Surg 2020; 230:283–293 [DOI] [PubMed] [Google Scholar]
- 22.Hodkinson A, Zhou A, Johnson J, et al. : Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ 2022; 378:e070442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nadkarni A, Biswas J: Gender disparity in cognitive load and emotional labor—threats to women physician burnout. JAMA Psychiatry 2022; 79:745–746 [DOI] [PubMed] [Google Scholar]
- 24.United States Senate Committee on Finance: Mental Health Care in the United States: The Case for Federal Action Washington, DC, US Government Publishing Office, 2022 [Google Scholar]
- 25.Reinert M, Fritze D, Nguyen T: The State of Mental Health in America 2022 Alexandria, VA, Mental Health America, 2021. https://mhanational.org/sites/default/files/2022%20State%20of%20Mental%20Health%20in%20America.pdf [Google Scholar]
- 26.Behavioral Health Barometer: Oregon, Volume 6. HHS pub no SMA-20-Baro-19-OR Rockville, MD, Substance Abuse and Mental Health Services Administration, 2020. https://www.samhsa.gov/data/sites/default/files/reports/rpt32854/Oregon-BH-Barometer_Volume6.pdf [Google Scholar]
- 27.Botkin B: Amid Oregon State hospital problems, health systems go to court. The Lund Report 2022. https://www.thelundreport.org/content/amid-oregon-state-hospital-problems-health-systems-go-court
- 28.Zhu JM, Howington D, Hallett E, et al. : Behavioral Health Workforce Report to the Oregon Health Authority and State Legislature. Portland, Oregon Health & Science University, Center for Health Systems Effectiveness, 2022. https://www.oregon.gov/oha/ERD/SiteAssets/Pages/Government-Relations/Behavioral%20Health%20Workforce%20Wage%20Study%20Report-Final%20020122.pdf
- 29.Tuffour I: A critical overview of interpretative phenomenological analysis: a contemporary qualitative research approach. J Healthc Commun 2017; 2:52 [Google Scholar]
- 30.Zur J, Musumeci M, Garfield R: Medicaid’s Role in Financing Behavioral Health Services for Low-Income Individuals San Francisco, Kaiser Family Foundation, 2017. https://www.kff.org/report-section/medicaids-role-in-financing-behavioral-health-services-for-low-income-individuals-issue-brief. Accessed Mar 3, 2023 [Google Scholar]
- 31.Nguyen OK, Makam AN, Halm EA: National use of safety-net clinics for primary care among adults with non-Medicaid insurance in the United States. PLoS One 2016; 11:e0151610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosenbaum S, Shin P, Sharac J, et al. : Medicaid and Safety-Net Providers: An Essential Health Equity Partnership New York, The Commonwealth Fund, 2022. https://www.commonwealthfund.org/publications/fund-reports/2022/apr/medicaid-safety-net-providers-equity-partnership. Accessed Mar 3, 2023 [Google Scholar]
- 33.State-Level Projections of Supply and Demand for Behavioral Health Occupations: 2016–2030 Rockville, MD, Health Resources and Services Administration, National Center for Health Workforce Analysis, 2018. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/state-level-estimates-report-2018.pdf [Google Scholar]
- 34.2020: Oregon’s Licensed Health Care Workforce Supply Portland, Oregon Health Authority, Office of Health Analytics, 2021. https://www.oregon.gov/oha/HPA/ANALYTICS/HealthCareWorkforceReporting/2021-Workforce-Supply-for-web.pdf [Google Scholar]
- 35.Druss BG, Cohen AN, Brister T, et al. : Supporting the mental health workforce during and after COVID-19. Psychiatr Serv 2021; 72:1222–1224 [DOI] [PubMed] [Google Scholar]
- 36.Covino NA: Developing the behavioral health workforce: lessons from the states. Adm Policy Ment Health 2019; 46:689–695 [DOI] [PubMed] [Google Scholar]
- 37.Zhu JM, Renfro S, Watson K, et al. : Medicaid reimbursement for mental health services: comparisons across states and to Medicare. Health Aff 2023; 42:556–565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saunders H, Guth M, Eckart G: A Look at Strategies to Address Behavioral Health Workforce Shortages: Findings From a Survey of State Medicaid Programs San Francisco, Kaiser Family Foundation, 2023. https://www.kff.org/medicaid/issue-brief/a-look-at-strategies-to-address-behavioral-health-workforce-shortages-findings-from-a-survey-of-state-medicaid-programs. Accessed Feb 7, 2023 [Google Scholar]
- 39.Cordes CC: From surviving to thriving: strategies to cultivate individual and organizational resilience in the health care workforce. Fam Syst Health 2022; 40:433–435 [DOI] [PubMed] [Google Scholar]
- 40.Boyes A: How to get through an extremely busy time at work. Harvard Business Review 2019. https://hbr.org/2019/03/how-to-get-through-an-extremely-busy-time-at-work
- 41.Saunders EG: 6 causes of burnout, and how to avoid them. Harvard Business Review 2019. https://hbr.org/2019/07/6-causes-of-burnout-and-how-to-avoid-them
- 42.Parker GB, Hyett MP: Measurement of well-being in the workplace: the development of the Work Well-Being Questionnaire. J Nerv Ment Dis 2011; 199:394–397 [DOI] [PubMed] [Google Scholar]
- 43.Consolidated Appropriations Act, 2023. PL 117–328, HR 2617, 117th Cong Washington, DC, US Government Publishing Office, 2022. https://www.congress.gov/117/bills/hr2617/BILLS-117hr2617enr.pdf [Google Scholar]
- 44.Key Behavioral Health Investments (21–23 Biennium) Expected to Increase Resources and Improve Outcomes for the Population Needing Intensive Services Salem, Oregon Health Authority, 2022. https://www.oregon.gov/oha/HSD/AMH/docs/BH-Investment-Update-Q322.pdf [Google Scholar]
- 45.Jones P: Oregon Legislature Passed Many New Investments in Behavioral Health Lynnwood, WA, State of Reform, 2021. https://stateofreform.com/featured/2021/06/oregon-legislature-behavioral-health. Accessed June 2, 2023 [Google Scholar]
- 46.Emergency Board Advances Millions in Funding to Support Health Care and Behavioral Health Workforces [press release] Salem, Oregon State Legislature, House Majority Office, 2022. https://www.oregonlegislature.gov/housedemocrats/Documents/Emergency%20Board%20Advances%20Millions%20in%20Funding%20to%20Support%20Health%20Care%20and%20Behavioral%20Health%20Workforces.pdf [Google Scholar]
- 47.Relating to Financial Resources Available to Provide Care, and Declaring an Emergency OR HB 4004, 2022 Reg Sess. Salem, Oregon State Legislature, 2022. https://olis.oregonlegislature.gov/liz/2022R1/Downloads/MeasureDocument/HB4004 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


