Abstract
Study Objective:
We sought to describe diagnosis rates and compare common process outcomes between geriatric EDs (GEDs) and non-GEDs participating in the American College of Emergency Physicians (ACEP) Clinical Emergency Data Registry (CEDR).
Methods:
We conducted an observational study of ED visits in calendar year 2021 within the CEDR by older adults. The analytic sample included 6,444,110 visits at 38 GEDs and 152 matched non-GEDs, with GED status determined by linkage to ACEP’s GED Accreditation Program. Stratified by age, we assessed diagnosis rates (X/1000) for four common geriatric syndrome conditions and a set of common process outcomes including ED length of stay, discharge rates, and 72-hour revisit rates.
Results:
Across all age categories, GEDs had higher diagnosis rates than non-GEDs for three of the four geriatric syndrome conditions of interest: UTI, dementia, and delirium / altered mental status. Median ED site-level length of stay for older adults was lower at GEDs compared to non-GEDs, while 72-hour revisit rates were similar across all age categories. GEDs exhibited a median discharge rate of 67.5% for adults 65–74 years of age, 60.8% for adults 75–84 years of age, and 55.6% for adults greater than 85 years of age. Comparatively, the median discharge rate at non-GED sites was 69.0% for adults 65–74 years of age, 64.2% for adults 75–84 years of age, and 61.3% for adults greater than 85 years of age.
Conclusion:
GEDs had higher geriatric syndrome diagnosis rates, lower ED lengths of stay, and similar discharge and 72-hour revisit rates when compared to non-GEDs in the CEDR. These findings provide the first benchmarks for emergency care process outcomes in GEDs compared to non-GEDs.
Introduction
Background
Emergency department (ED) visits by older adults are increasing given the aging population and the expanded role the emergency care setting is playing in the evaluation of acute illnesses in undifferentiated older patients.1 In response, Geriatric Emergency Department Guidelines were published in 2014,2 and the American College of Emergency Physicians (ACEP) launched the Geriatric ED Accreditation (GEDA) Program in 2018 to recognize EDs committed to emergency care delivery to the older adult population.3 The GEDA Program has three levels of accreditation, including Level 1 (gold), Level 2 (silver), and Level 3 (bronze) according to implemented best practices and protocols. Now, less than a decade after the Geriatric ED Guidelines were proposed, there are over 400+ accredited Geriatric EDs (GEDs) in the United States. Prior work has described the implementation of the GEDA program within individual healthcare systems and the broader reach of the GEDA program,4,5 with included EDs almost exclusively in urban areas. Currently, little is known about whether EDs participating in geriatric efforts systematically differ in geriatric patient populations, structure, or common process outcomes for older adults compared to non-GEDs.
Importance
The GEDA Program has exhibited considerable growth in participation since inception. The recent launch and growth of the ACEP Clinical Emergency Data Registry (CEDR)6 offers a unique opportunity to capture ED visit-level electronic health record data to examine patterns of emergency care for older adults. Of those EDs captured in the CEDR, many have also been identified as GEDs through the GEDA Program.3 This analysis will advance the field of emergency medicine in two primary ways. First, understanding variation in care and utilization practices between GEDs and non-GEDs allows for identification of modifiable sources of variation for quality improvement. Second, this data will provide current benchmarks for emergency care in GEDs and non-GEDs for older adults.
Goals of this Investigation
We sought to describe diagnosis rates and compare common process outcomes, including ED length of stay, discharge rates, and 72-hour revisit rates, between GEDs and non-GEDs participating in the CEDR.
Methods
Study Design
We conducted an observational study of ED visits included in a national emergency medicine clinical quality registry with data from January 1, 2021 through December 31, 2021. Our study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.7
Study Setting and Datasets
Data were drawn from the CEDR, a Centers for Medicare & Medicaid Services Qualified Clinical Data Registry for emergency clinicians and health systems nationwide to voluntarily collect and report quality data that is maintained by ACEP.6 CEDR data have been used to conduct research regarding opioid use disorder,8 mental health conditions,9 and broader emergency conditions during the COVID-19 pandemic,10,11 and has several advantages including: 1) unique operational and clinical EHR data elements (e.g. time stamps, diagnoses), 2) representative sample of community EDs often absent from larger registry data collaboratives, and 3) data linkage capabilities.
The ACEP’s CEDR is the largest data registry of emergency care visits in the US, including over 944 EDs and 18 million ED visits in 2021. Reporting EDs use a variety of electronic health record (EHR) platforms and are located across 48 states, thereby providing a diverse sample of ED EHR data to provide insights into the current state of geriatric emergency care. Data at the ED visit-level included International Classification of Disease-Tenth Edition-Clinical Modification (ICD-10-CM) diagnosis codes, patient age, gender, insurance payor(s), ED disposition, ED billing codes, among others. We grouped visits by age into three categories for older adults: aged 65–74, 75–84, and 85 and older. We included ED visits of those aged 45–64 years as a comparison group.
ED sites within CEDR were linked to the publicly available list of ACEP’s GEDA Program to determine GED or non-GED accreditation status.3 ED sites were also linked to the most recent 2020 American Hospital Association Annual Survey data to characterize hospital-based EDs in the sample according to their rural-urban status, teaching status (an Accreditation Council for Graduate Medical Education accredited program), and critical access hospital status.12
Outcomes
We assessed a set of outcomes among GEDs and non-GEDs. This included ED visit-level diagnosis rates (X/1000) across age categories and between GEDs and non-GEDs for four common geriatric syndrome conditions of interest: falls, urinary tract infection (UTI), dementia, delirium / altered mental status. ICD-10-CM ED diagnosis codes were used to identify ED visits related to the four geriatric syndrome conditions (Supplemental Table 1).13,14 Diagnosis rates were presented at the ED visit-level to obtain a more granular estimate of geriatric syndrome conditions. We also assessed ED site-level process outcomes of ED length of stay, discharge rates, and 72-hour revisit rates across age categories and between GEDs and non-GEDs. Consistent with prior literature,15–17 ED length of stay was determined using ED arrival and ED departure time stamps within CEDR. ED site-level analyses were conducted for these outcomes to reduce the impact of high volume EDs with a potential greater likelihood for outlier values which may have biased results. ED visit-level analyses are presented for the three process outcomes: ED length of stay, discharge rates, and 72-hour revisit rates in Supplemental Table 2.
Dataset Development
Raw EHR extracts were reviewed for completeness, and those sites with inconsistent coding of key ED data fields (time stamps, age, diagnoses, dispositions) were removed from the analytic sample. Summary statistics across ages, diagnoses, and dispositions were reviewed for red flag patterns for each individual site as quality measure reporting might require an ED site in CEDR to only report on a subset of their ED visits with certain diagnoses. Those ED sites with <95% data fidelity across variables of interest for the analyses were removed. After this step, there were a total of 512 CEDR EDs with complete and available data for 2021. Of these, 38 ED sites were identified as accredited GEDs, which were subsequently matched in a 4:1 fashion to like non-GEDs within CEDR using a previously derived and validated nearest neighbor matching algorithm and probabilistic linkage.18,19 Sites were matched on six variables including teaching status, freestanding ED status, region (Midwest, Northeast, South, West), ED visit volume, urbanicity (metropolitan, micropolitan, rural), and proportion of ED visits for those >65 years of age.
Analysis
We tabulated ED site and ED visit characteristics for the GEDs and the matched non-GEDs within the CEDR. We describe outcomes by median and interquartile range (IQR) for continuous variables and percentages for categorical variables. Analyses were performed in R (4.0.2). Access to the CEDR data is restricted by agreement with ACEP, given potentially identifying features, and the study was classified as exempt by the Institutional Review Board at Yale University.
Results
Characteristics of the Analytic Sample
The analytic sample of 38 GEDs (Level 1 – 1 ED; Level 2 – 3 EDs; Level 3 – 34 EDs) and 152 matched non-GEDs within CEDR were similar with regards to U.S. census region, urbanicity, critical access hospital status, AHA teaching status, free standing status, and ED visit volume. There was a total of 6,444,110 visits at the included ED sites, including 1,320,057 (20.5%) at GEDs and 5,124,053 (79.5%) at non-GEDs. Across GEDs, the median proportion of visits by older adults 65–74 years of age was 11.3%, 75–84 years of age was 8.1%, and greater than 85 years of age was 4.6%. These proportions at the ED site-level were similar for non-GEDs (Table 1), and the remainder of GED characteristics were comparable to 118 GEDs not included in CEDR upon review of available data within the AHA survey (Supplemental Table 3).
Table 1.
Emergency department analytic sample characteristics
| Matched non-GEDs (n=152) | GEDs (n=38) | |
|---|---|---|
| U.S. Census Region | ||
| Northeast | 40 (26.3%) | 12 (31.6%) |
| Midwest | 34 (22.4%) | 8 (21.1%) |
| South | 31 (20.4%) | 7 (18.4%) |
| West | 47 (30.9%) | 11 (28.9%) |
| CBSA | ||
| Metro | 146 (96.1%) | 37 (97.4%) |
| Micro | 6 (3.9%) | 1 (2.6%) |
| Rural | 0 (0%) | 0 (0%) |
| Critical Access | 7 (4.6%) | 2 (5.3%) |
| AHA Teaching Status | 145 (95.4%) | 36 (94.7%) |
| Free Standing Status | 84 (55.3%) | 16 (42.1%) |
| ED Visit volume, 2021 | ||
| <20k | 34 (22.4%) | 12 (31.6%) |
| 20–40k | 71 (46.7%) | 12 (31.6%) |
| 40–60k | 38 (25.0%) | 9 (23.7%) |
| 60–80k | 6 (3.9%) | 4 (10.5%) |
| 80k+ | 3 (2.0%) | 1 (2.6%) |
| Female (%, median [IQR]) | 54.2% [51.6%–55.5%] | 54.8% [51.6%–56.6%] |
| Visits Age 65+ (%, median [IQR]) | ||
| 65–74 | 11.5% [10.1%–13.0%] | 11.3% [10.4%–12.7%] |
| 75–84 | 8.5% [6.6%–10.0%] | 8.1% [6.9%–9.9%] |
| 85+ | 4.8% [3.3%–6.6%] | 4.6% [3.8%–5.9%] |
Abbreviations: AHA – American Hospital Association; CBSA – Core-based statistical area; GED – geriatric emergency department
Geriatric Syndrome Diagnosis Rates
Across all age categories, GEDs had higher diagnosis rates than non-GEDs for three of the four geriatric syndrome conditions of interest: UTI, dementia, and delirium / altered mental status (Table 2). As an example, UTI diagnosis rates (per 1,000 ED visits) in GEDs were 49.9 for adults 65–74 years of age, 76.6 for adults 75–84 years of age, and 93.7 for adults greater than 85 years of age. In non-GEDs, UTI diagnosis rates (per 1,000 ED visits) were 36.7 for adults 65–74 years of age, 52.9 for adults 75–84 years of age, and 73.6 for adults greater than 85 years of age. Fall diagnosis rates (per 1,000 ED visits) in GED were 5.6 for adults 65–74 years of age, 9.7 for adults 75–84 years of age, and 16.3 for adults greater than 85 years of age. Diagnosis rates of falls were similar across age categories at non-GEDs (Table 2).
Table 2.
Emergency department diagnosis rates per 1,000 ED visits
| Matched non-GEDs (n=152) | GEDs (n=38) | |
|---|---|---|
| Delirium / AMS | ||
| 45–64 | 2.77 | 3.83 |
| 65–74 | 4.57 | 6.31 |
| 75–84 | 6.89 | 9.87 |
| 85+ | 9.40 | 13.42 |
| Fall | ||
| 45–64 | 2.47 | 1.83 |
| 65–74 | 6.68 | 5.62 |
| 75–84 | 10.25 | 9.68 |
| 85+ | 17.63 | 16.28 |
| UTI | ||
| 45–64 | 23.06 | 32.48 |
| 65–74 | 36.69 | 49.87 |
| 75–84 | 52.92 | 76.59 |
| 85+ | 73.59 | 93.68 |
| Dementia | ||
| 45–64 | 2.23 | 2.37 |
| 65–74 | 13.01 | 17.41 |
| 75–84 | 39.40 | 50.88 |
| 85+ | 81.66 | 90.72 |
Note – Diagnosis rates were pooled at the ED visit-level across all EDs within a group (GEDs or non-GEDs).
Abbreviations: AMS – altered mental status; GED – geriatric emergency department; UTI – urinary tract infection
ED Length of Stay
Across all age categories, median ED site-level length of stay was lower at GEDs compared to non-GEDs (Table 3). The median of the median length of stay at GEDs was 3.5 hours for adults 65–74 years of age, 3.8 hours for adults 75–84 years of age, and 4.0 hours for adults greater than 85 years of age, respectively compared to 4.0 hours, 4.2 hours, and 4.4 hours for older adults provided emergency care in non-GEDs.
Table 3.
Emergency department process outcome measures
| Matched non-GEDs (n=152) | GEDs (n=38) | |
|---|---|---|
| LOS Median (hours, median [IQR]) | ||
| 45–64 | 3.6 [3.0–4.3] | 3.2 [2.8–3.7] |
| 65–74 | 4.0 [3.4–4.7] | 3.5 [3.3–4.4] |
| 75–84 | 4.2 [3.6–4.9] | 3.8 [3.5–4.6] |
| 85+ | 4.4 [3.7–5.2] | 4.0 [3.7–4.9] |
| 72-hour ED Revisit (%, median [IQR]) | ||
| 45–64 | 3.3% [2.6%–4.3%] | 3.2% [2.6%–4.2%] |
| 65–74 | 3.0% [2.3%–3.9%] | 2.8% [2.3%–3.5%] |
| 75–84 | 2.9% [2.2%–3.6%] | 2.7% [2.4%–3.2%] |
| 85+ | 2.5% [1.8%–3.5%] | 2.5% [2.0%–2.9%] |
| Discharge Disposition (%, median [IQR]) | ||
| 45–64 | 81.2% [72.1%–90.8%] | 79.0% [74.4%–87.3%] |
| 65–74 | 69.0% [60.7%–83.8%] | 67.5% [61.1%–79.4%] |
| 75–84 | 64.2% [51.7%–83.0%] | 60.8% [52.5%–75.9%] |
| 85+ | 61.3% [44.8%–79.1%] | 55.6% [45.2%–72.3%] |
Note – Process outcome measures were assessed at the ED site-level. For example, each non-GED had a distribution for LOS (in hours) of their ED visits, with the medians across all non-GEDs then summarized using median and IQRs. To avoid the impact of outlier EDs, the proportion with a 72-hour revisit rate and a discharge disposition are summarized in a similar manner.
Abbreviations: GED – geriatric emergency department; LOS – length of stay
Discharge Rates
Overall ED site-level discharge rates were similar between GEDs and non-GEDs for the population 65–74 years of age, but slightly higher for non-GEDs when assessing populations greater than 75 years of age. GEDs exhibited a median discharge rate of 67.5% for adults 65–74 years of age, 60.8% for adults 75–84 years of age, and 55.6% for adults greater than 85 years of age. Comparatively, the median discharge rate at non-GED sites was 69.0% for adults 65–74 years of age, 64.2% for adults 75–84 years of age, and 61.3% for adults greater than 85 years of age (Table 3 & Figure 1).
Figure 1.
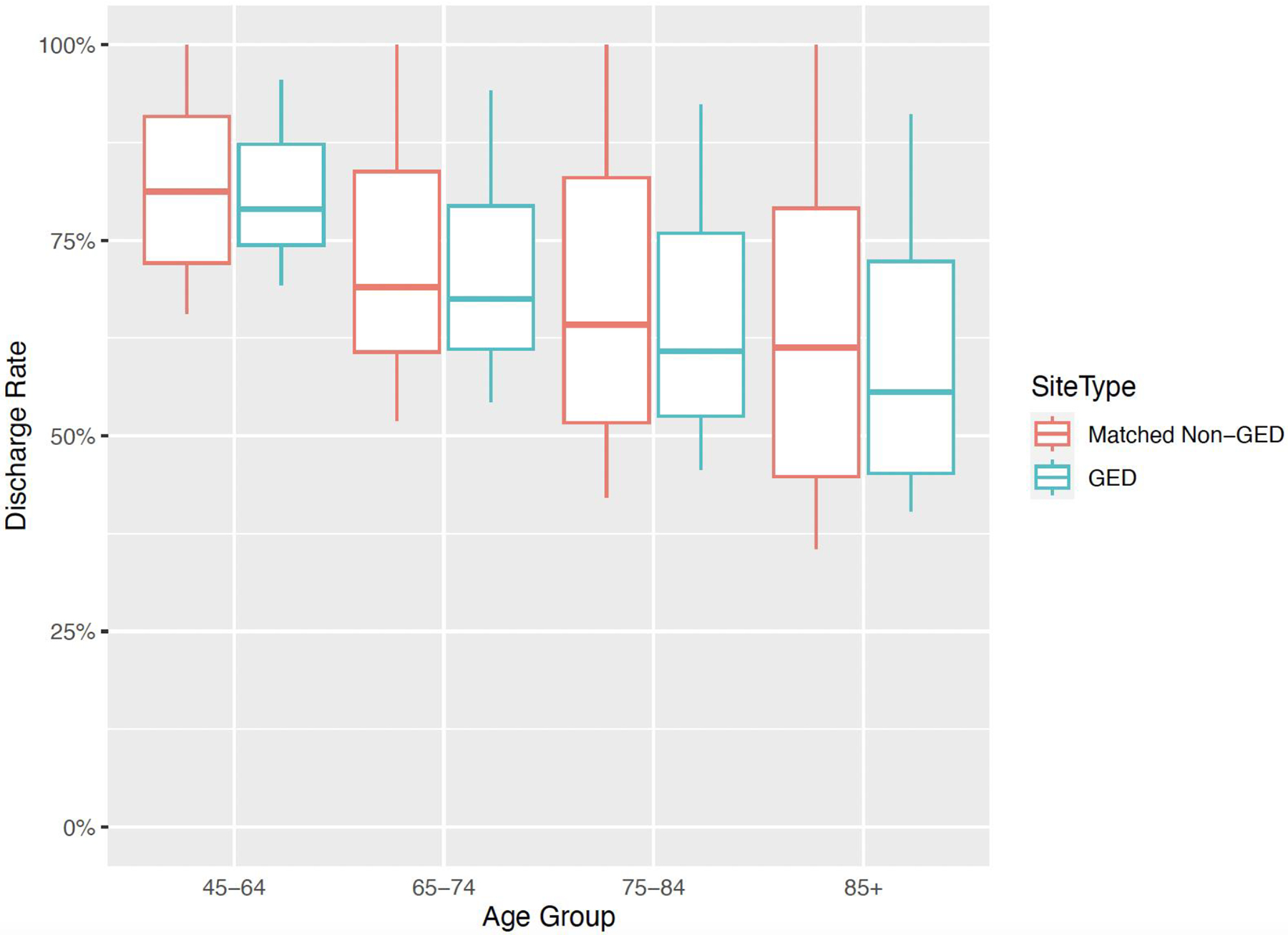
Emergency department discharge rates within geriatric and non-geriatric EDs
Note – Discharge rates were assessed at the ED site-level.
Note - The box plots depict median (thick horizontal line) discharge rates with 25th and 75th percentiles for each box, while vertical lines provide the range (from minimum to maximum).
For the geriatric syndrome conditions of interest, discharge rates were lower for GEDs across age categories (Table 4). Of note, GEDs exhibited a median discharge rate for delirium / AMS of 32.7% for adults 65–74 years of age, 29.6% for adults 75–84 years of age, and 30.0% for adults greater than 85 years of age. Comparatively, the median discharge rate for delirium / AMS at non-GED sites was 47.4% for adults 65–74 years of age, 44.3% for adults 75–84 years of age, and 48.3% for adults greater than 85 years of age. Despite a smaller sample size, discharge rates were markedly more consistent at GEDs, as evidenced by comparatively more narrow interquartile ranges.
Table 4.
Emergency department discharge rates for geriatric syndrome conditions of interest Note – Discharge rates were assessed at the ED site-level.
| Matched non-GEDs (n=152) | GEDs (n=38) | |
|---|---|---|
| Median [IQR] | Median [IQR] | |
| Delirium / AMS | ||
| 45–64 | 50.0% [28.6%–68.9%] | 29.6% [22.3%–37.5%] |
| 65–74 | 47.4% [26.7%–83.3%] | 32.7% [22.8%–43.2%] |
| 75–84 | 44.3% [25.3%–77.1%] | 29.6% [21.4%–38.6%] |
| 85+ | 48.3% [25.0%–68.3%] | 30.0% [20.0%–47.4%] |
| Falls | ||
| 45–64 | 50.0% [32.6%–87.1%] | 35.4% [22.6%–47.8%] |
| 65–74 | 44.4% [24.8%–75.7%] | 27.9% [13.8%–46.6%] |
| 75–84 | 40.6% [26.9%–79.1%] | 22.2% [11.4%–47.2%] |
| 85+ | 38.9% [24.0%–75.0%] | 26.9% [16.4%–40.2%] |
| UTI | ||
| 45–64 | 74.0% [58.1%–91.5%] | 67.1% [59.6%–75.9%] |
| 65–74 | 63.0% [43.8%–88.0%] | 53.9% [39.0%–64.8%] |
| 75–84 | 57.2% [36.6%–87.7%] | 45.1% [32.6%–55.3%] |
| 85+ | 48.9% [31.1 %–73.1%] | 38.4% [27.8%–53.3%] |
| Dementia | ||
| 45–64 | 62.7% [33.7%–94.8%] | 41.2% [24.3%–52.8%] |
| 65–74 | 56.5% [36.7%–94.1%] | 38.6% [30.0%–56.0%] |
| 75–84 | 56.2% [35.7%–89.8%] | 37.3% [28.8%–51.9%] |
| 85+ | 52.1% [31.3%–84.4%] | 41.5% [27.6%–49.9%] |
Abbreviations: AMS – altered mental status; GED – geriatric emergency department; UTI – urinary tract infection
72-Hour Revisit Rates
Between GEDs and non-GEDs, 72-hour ED revisit rates were similar (Table 3). The median 72-hours revisit rate at GEDs was 2.8% for adults 65–74 years of age, 2.7% for adults 75–84 years of age, and 2.5% for adults greater than 85 years of age, respectively compared to 3.0%, 2.9%, and 2.5% for older adults provided emergency care in non-GEDs.
Limitations
Our results should be interpreted within the confines of our study design and dataset. First, inherent limitations exist with the use of diagnosis codes and may have resulted in slightly elevated diagnosis rates for UTI, as one example, if instead we required urine culture positivity for diagnosis. Within CEDR, all diagnoses from the encounter are included and do not differentiate between ‘primary’ and ‘secondary’ diagnoses. Our diagnosis rates therefore reflect if the geriatric syndrome diagnoses of interest were coded in any position for the encounter. However, we do not believe that GEDs or non-GEDs would systematically have been impacted by either of these two limitations, thereby reducing the potential for biased results. Third, all levels of GEDs were aggregated for analysis given the sample size, and therefore we were unable to differentiate differences between Level 1, 2, and 3 accredited GEDs. Overall, we were limited by the number of GEDs reporting within CEDR and recognize that subsequent evaluations using alternative data sources or methodologic approaches will be critical within future analyses. It is possible that EDs participating in geriatric accreditation and reporting within CEDR may have unique characteristics, processes in place, or motivations that are not reflective of GEDs nationwide. Fourth, while EDs were matched across several variables, we did not individually risk adjust our ED-level analyses for ED available resources such as ancillary staff, access to outpatient follow-up, or GED-specific protocols and policies in place that likely differed between EDs. These opportunities were instead thought of under the umbrella of resources potentially available and implemented within the category of GEDs, broadly reflecting the key differentiating factor of interest between EDs. We also were unable to adjust for encounter-level factors that may be associated with the assessed outcomes including older adult socioeconomic status, frailty, and triage acuity. Finally, we opted to present discharge rates rather than admission rates given limitations in data standards and ability to differentiate non-discharge dispositions such as ED observation, inpatient observation, and transfers.
Discussion
In this cross-sectional analysis of over 6 million visits at 38 GEDs and 152 matched non-GEDs, we performed the first direct comparison of its kind assessing diagnosis rates and other common process outcomes, including ED site-level length of stay, discharge rates, and 72-hour revisit rates. Our study has three major findings. First, GEDs had higher diagnosis rates than non-GEDs across age categories for encounters related to UTI, dementia, and delirium / altered mental status. Second, ED site-level length of stay was slightly lower at GEDs compared to non-GEDs, while 72-hour revisit rates were similar between GEDs and non-GEDs. Third, overall ED site-level discharge rates were comparable between GEDs and non-GEDs. Discharge rates were higher at non-GEDs, yet less consistent, when specifically analyzing the four geriatric syndrome conditions of interest across age categories.
Our work builds upon the existing literature in a number of ways. Early observational studies evaluating geriatric emergency care have almost exclusively been conducted at single center ED sites not yet formally accredited as GEDs.20,21 Subsequent GED intervention-based studies have also shown the potential benefit of novel models of service delivery (e.g. telephone follow-up, nurse-led comprehensive geriatric assessment) on care coordination, costs, admission rates, hospital length of stay within academic centers,22–28 yet similarly often have been analyses of local initiatives. A unique strength of our analysis is our ability to compare ED visit outcomes among a national sample of GEDs and similar non-GEDs, with this work serving as the first of its kind.
There are several factors which may have contributed to the findings related to diagnosis rates. To be accredited within the GEDA Program, GEDs must meet criteria regarding staffing, education, policies and procedures, quality improvement initiatives, and the physical environment. Higher diagnosis rates at GEDs for UTI, dementia, and delirium / altered mental status may be a result of increased awareness from local education or standardized screening processes regarding these geriatric syndrome conditions of interest. Falls were a unique geriatric syndrome condition of interest in that diagnosis rates were similar between GEDs and non-GEDs. One hypothesis for this similarity in fall diagnosis rates is the national quality focus on falls screening, identification, and treatment that has permeated emergency care culture and resulted in quality measure efforts centered on this diagnosis. Within the Quality Payment Program of the Centers for Medicare & Medicaid Services (CMS), two quality measures (#155 and #318) within the 2022 performance year specifically address falls. Despite not being included within the Emergency Medicine Specialty Set of quality measures, quality measure #318 (Falls: Screening for Future Fall Risk) was reported by 18,066 emergency clinicians in the 2018 Merit-based Incentive Payment System,29 making it the overall third-most common quality measure reported by emergency clinicians and providing supporting evidence for its similarity between GEDs and non-GEDs.
Separate factors also may have played a role in the care process outcome results we identified. First, the majority of GEDs in the analytic sample (and nationally) are Level 3, which may indicate interest and entry-level structures but not the organizational infrastructure and resources required to implement complex interventions potentially more likely to influence the studied process outcomes. With the majority of included GEDs being Level 3, it is possible that our findings were biased towards the null hypothesis of finding no difference in outcomes between GEDs and non-GEDs as opposed to an analysis that included a more even GED Level distribution across the three categories. However, this would require a considerable transition of current Level 3 GEDs to Level 2 and 1. Second, ED length of stay was lower in GEDs compared to non-GEDs. It is possible that streamlined approaches to nursing assessments, diagnostic testing, and support services are present in GEDs that facilitate this finding. However, it is also possible that decreased ED length of stays in GEDs are a result of clinicians quickly recognizing that an individual older adult is not fit to be discharged (hence the lower discharge rates), with the further evaluation and treatment care plan continuing once hospitalized. Third, when looking at the four geriatric syndrome conditions of interest, discharge rates were higher among non-GEDs across all age categories. One difference worth highlighting was the rather high discharge rate for older adults at non-GEDs with a diagnosis of delirium / AMS. Often the only sign of a serious underlying medical condition, ED detection of delirium has been suggested to require further hospitalization to adequately evaluate and treat,30,31 as seen within our population of GEDs. The broader finding of slightly higher discharge rates among non-GEDs may also be due to the fact that analyses were matched, but were unable to be risk-adjusted, which may more closely remove potential ED visit-level or ED site-level confounders. A second possibility is that the modestly lower discharge rates among GEDs may reflect high value geriatric observation care, in which additional testing is being completed, but would not be identified as an ED discharge disposition. A final contributor in the identified discharge rates may be that 55% of non-GEDs in this sample were freestanding EDs, reflecting a slight increase from the matched GED sample in which 42% were freestanding. In prior literature involving patients of all ages,32 freestanding EDs have been shown to discharge more patients in comparison to hospital-based EDs.
Our work has substantial implications and also can serve as a foundation for future research and administrative efforts to improve geriatric emergency care. Most notably, the return on investment of GEDs must be continued to be studied, including health outcomes, quality of care, and experiences of older adults as well as the potential cost savings to the healthcare system. GEDs have previously shown reduced hospital readmissions,25 reduced hospital lengths of stay,33 and reduced costs to Medicare,23 whereas conflicting studies note that is unclear if the increased staffing and resources required to operate a GED program outweigh any cost savings.34 Ultimately, the decision to invest resources into a GED program may depend on a variety of factors aside from the published literature, including the needs of the local population, potential cost savings, and increasing value-based payment arrangements. Numerous efforts within the past decade have primarily focused on the older adult population through new payment models developed by CMS as well as private payers in the Medicare Advantage program to reduce low-value hospitalizations through alternative payment models.35,36 In the future, it stands to reason that GEDs may be integrated within multispecialty networks and as part of accountable care organizations aiming to provide the resources and supports that older adults require to improve outcomes in a cost-effective manner.
In summary, GEDs had higher diagnosis rates than matched non-GEDs across age categories for encounters related to UTI, dementia, and delirium / altered mental status. In comparison to non-GEDs, GEDs exhibited lower ED site-level lengths of stay and similar discharge and 72-hour revisit rates. These findings provide the first benchmarks for emergency care process outcomes in GEDs compared to non-GEDs and also highlight the need to understand operational impacts of new GED care models.
Supplementary Material
Grant/Financial Support:
Dr. Gettel is a Pepper Scholar with support from the Claude D. Pepper Older Americans Independence Center at Yale School of Medicine (P30AG021342) and the National Institute on Aging (NIA) of the National Institutes of Health (NIH; R03AG073988). Dr. Hwang is supported by the NIA (R33AG058926, R61A069822), the John A Hartford Foundation, West Health Institute, and the Dolby Family Foundation. Dr. Janke reports being supported by the Veterans Affairs (VA) Office of Academic Affiliation through the VA/National Clinician Scholars Program and the University of Michigan. Dr. Venkatesh reports support by the American Board of Emergency Medicine National Academy of Medicine Anniversary fellowship during this work and prior support from the Yale Center for Clinical Investigation grant KL2 TR000140 from the National Center for Advancing Translational Science (NCATS/NIH). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meetings:
This work has been accepted for presentation at the 2023 American Geriatric Society annual meeting in Long Beach, CA and the 2023 Society for Academic Emergency Medicine annual meeting in Austin, TX.
Declaration of Conflicting Interests:
Dr. Gettel is a reviewer for the Geriatric Emergency Department Accreditation (GEDA) process. Drs. Gettel and Venkatesh serve on the American College of Emergency Physicians (ACEP) Clinical Emergency Data Registry Committee and Drs. Gettel, Hwang, and Venkatesh serve on the ACEP Quality and Patient Safety Committee. Dr. Schenider is the Senior Vice President of Clinical Affairs at ACEP, and Dr. Goyal is the Senior Vice President of Quality at ACEP.
References:
- 1.National Center for Health Statistics. Emergency Department Visits Among Adults Aged 60 and Over: United States, 2014–2017. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/databriefs/db367-h.pdf [Google Scholar]
- 2.Carpenter CR, Bromley M, Caterino JM, et al. Optimal older adult emergency care: introducing multidisciplinary geriatric emergency department guidelines from the American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, and Society for Academic Emergency Medicine. Acad Emerg Med. 2014;21(7):806–809. [DOI] [PubMed] [Google Scholar]
- 3.Geriatric Emergency Department Accreditation Program. American College of Emergency Physicians. Accessed September 17, 2022. https://www.acep.org/geda/
- 4.Liberman T, Roofeh R, Herod SH, Maffeo V, Biese K, Amato T. Dissemination of geriatric emergency department accreditation in a large health system. J Am Coll Emerg Physicians Open. 2020;1(6):1281–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kennedy M, Lesser A, Israni J, et al. Reach and Adoption of a Geriatric Emergency Department Accreditation Program in the United States. Ann Emerg Med. 2022;79(4):367–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clinical Emergency Data Registry. American College of Emergency Physicians. https://www.acep.org/cedr/
- 7.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–577. [DOI] [PubMed] [Google Scholar]
- 8.Taylor A, Kinsman J, Hawk K, et al. Development and testing of data infrastructure in the American College of Emergency Physicians’ Clinical Emergency Data Registry for opioid-related research. J Am Coll Emerg Physicians Open. 2022;3(5):e12816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Venkatesh AK, Janke AT, Kinsman J, et al. Emergency department utilization for substance use disorders and mental health conditions during COVID-19. PLoS One. 2022;17(1):e0262136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Venkatesh AK, Janke AT, Shu-Xia L, et al. Emergency Department Utilization for Emergency Conditions During COVID-19. Ann Emerg Med. 2021;78(1):84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Janke AT, Jain S, Hwang U, et al. Emergency department visits for emergent conditions among older adults during the COVID-19 pandemic. J Am Geriatr Soc. 2021;69(7):1713–1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.AHA Annual Survey Database. American Hospital Association. https://www.ahadata.com/aha-annual-survey-database
- 13.Centers for Medicare & Medicaid Services. Chronic Conditions. Chronic Conditions Data Warehouse Accessed February 13, 2022. https://www2.ccwdata.org/web/guest/condition-categories-chronic
- 14.American Academy of Professional Coders. ICD-10-CM Codes Lookup. Accessed February 14, 2022. https://www.aapc.com/codes/icd-10-codes-range/
- 15.Yiadom MYAB, Napoli A, Granovsky M, et al. Managing and Measuring Emergency Department Care: Results of the Fourth Emergency Department Benchmarking Definitions Summit. Acad Emerg Med. 2020;27(7):600–611. [DOI] [PubMed] [Google Scholar]
- 16.Wiler JL, Welch S, Pines J, Schuur J, Jouriles N, Stone-Griffith S. Emergency department performance measures updates: proceedings of the 2014 emergency department benchmarking alliance consensus summit. Acad Emerg Med. 2015;22(5):542–553. [DOI] [PubMed] [Google Scholar]
- 17.Chang AM, Lin A, Fu R, McConnell KJ, Sun B. Associations of Emergency Department Length of Stay With Publicly Reported Quality-of-care Measures. Acad Emerg Med. 2017;24(2):246–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ho DE, Imai K, King G, Stuart EA. Matching as Nonparametric Preprocessing for Reducing Model Dependence in Parametric Causal Inference. Polit Anal. 2007;15(3):199–236. [Google Scholar]
- 19.Ho D, Imai K, King G, Stuart EA. MatchIt: Nonparametric Preprocessing for Parametric Causal Inference. J Stat Softw. 2011;42:1–28. [Google Scholar]
- 20.Foo CL, Siu VWY, Tan TL, Ding YY, Seow E. Geriatric assessment and intervention in an emergency department observation unit reduced re-attendance and hospitalisation rates. Australas J Ageing. 2012;31(1):40–46. [DOI] [PubMed] [Google Scholar]
- 21.Conroy SP, Ansari K, Williams M, et al. A controlled evaluation of comprehensive geriatric assessment in the emergency department: the “Emergency Frailty Unit.” Age Ageing. 2014;43(1):109–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wallis M, Marsden E, Taylor A, et al. The Geriatric Emergency Department Intervention model of care: a pragmatic trial. BMC Geriatr. 2018;18(1):297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hwang U, Dresden SM, Vargas-Torres C, et al. Association of a Geriatric Emergency Department Innovation Program With Cost Outcomes Among Medicare Beneficiaries. JAMA Netw Open. 2021;4(3):e2037334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morse L, Xiong L, Ramirez-Zohfeld V, Dresden S, Lindquist LA. Tele-Follow-Up of Older Adult Patients from the Geriatric Emergency Department Innovation (GEDI) Program. Geriatrics. 2019;4(1). doi: 10.3390/geriatrics4010018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dresden SM, Hwang U, Garrido MM, et al. Geriatric Emergency Department Innovations: The Impact of Transitional Care Nurses on 30-day Readmissions for Older Adults. Acad Emerg Med. 2020;27(1):43–53. [DOI] [PubMed] [Google Scholar]
- 26.Marsden E, Taylor A, Wallis M, et al. Effect of the Geriatric Emergency Department Intervention on outcomes of care for residents of aged care facilities: A nonrandomised trial. Emerg Med Australas. 2020;32(3):422–429. [DOI] [PubMed] [Google Scholar]
- 27.Huang HH, Chang JCY, Tseng CC, et al. Comprehensive geriatric assessment in the emergency department for the prediction of readmission among older patients: A 3-month follow-up study. Arch Gerontol Geriatr. 2021;92:104255. [DOI] [PubMed] [Google Scholar]
- 28.Huded JM, Lee A, Song S, et al. Association of a geriatric emergency department program with healthcare outcomes among veterans. J Am Geriatr Soc. 2022;70(2):601–608. [DOI] [PubMed] [Google Scholar]
- 29.Gettel CJ, Han CR, Granovsky MA, et al. Emergency clinician participation and performance in the Centers for Medicare & Medicaid Services Merit-based Incentive Payment System. Acad Emerg Med. 2022;29(1):64–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carpenter CR, Hammouda N, Linton EA, et al. Delirium Prevention, Detection, and Treatment in Emergency Medicine Settings: A Geriatric Emergency Care Applied Research (GEAR) Network Scoping Review and Consensus Statement. Acad Emerg Med. 2021;28(1):19–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee S, Angel C, Han JH. Succinct Approach to Delirium in the Emergency Department. Curr Emerg Hosp Med Rep. 2021;9(2):11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Simon EL, Shakya S, Muir M, Fertel BS. Differences in patient population and length of stay between freestanding and hospital-based emergency departments. Am J Emerg Med. 2019;37(9):1738–1742. [DOI] [PubMed] [Google Scholar]
- 33.Keene SE, Cameron-Comasco L. Implementation of a geriatric emergency medicine assessment team decreases hospital length of stay. Am J Emerg Med. 2022;55:45–50. [DOI] [PubMed] [Google Scholar]
- 34.Southerland LT, Savage EL, Muska Duff K, et al. Hospital Costs and Reimbursement Model for a Geriatric Emergency Department. Acad Emerg Med. 2020;27(10):1051–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gettel CJ, Tinloy B, Nedza SM, et al. The future of value-based emergency care: Development of an emergency medicine MIPS value pathway framework. J Am Coll Emerg Physicians Open. 2022;3(2):e12672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Biese K, Lash TA, Kennedy M. Emergency Department Care Transition ProgramsValue-Based Care Interventions That Need System-Level Support. JAMA Netw Open. 2022;5(5):e2213160. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


