Abstract
A well-accessible healthcare system is an important measure of the progress of a country, as access to adequate healthcare is one of everyone's very basic human rights. When a community lives below the poverty line, unfortunately, it gets deprived of the basic human rights like healthcare, which is a reality to many resource-constrained communities around the world. The number of such resource-constrained communities in developing countries is large. Orphans present a prominent example in this regard in the context of Bangladesh. Orphans suffer greatly from many diseases due to their resource-constrained environment of livings and they are unable to take a minimum care of their own health. Their lack of resources, inadequate literacy skills, and limited (or no) access to technology leave them in such a position that they are ignorant of healthcare services available for them directly or through technological means. Considering all these unavoidable real aspects and the fact that such resource-constrained communities are very little focused in the literature for aiding them in getting bare minimum healthcare services, in this study, we leverage technology and relevant appropriate intermediaries to bridge the gap between the orphans in the orphanages and healthcare services offered by medical doctors. To accomplish so, we conduct a series of field studies over the intended communities. The orphanage teachers and administrators, being in proximity, are the most effective ones to operate as intermediaries for the orphan children, as revealed through our field studies. Therefore, we use these intermediaries to help the orphans to get basic healthcare services via an Android healthcare app called ‘Shastho-sheba’. We also use our findings from the field study to specifically tailor and modify the application for intermediaries to use on behalf of the orphans so that health professionals can provide direct healthcare services to them over the Internet. Finally, we look into our proposed techno-social solution in the context of HCI to ensure that the service is used more effectively.
Keywords: Healthcare, Bangladesh, Orphans, Intermediary, Low-resource, Techno-social solution, Semi-structured survey
1. Introduction
There exist several ‘Resource-Constrained Communities’ (or RCCs) all over the world. There is often a commonality among the resource-constrained communities such as orphans, beggars, slum-dwellers, etc., and the commonality is the fact that the number is noticeably higher in the third-world or developing countries. For example, more than 7,00,000 begging people live in Bangladesh, a growing developing country, together with 4,00,000 orphan children. The nation's capital, Dhaka, has around 25 orphanages scattered throughout the city with approximately 1,000,000 beggars [1]. The orphanages host a vast number of orphan children.
By nature, children are generally at the highest risk of suffering the negative consequences of different types of crises and conflicts, such as social, political, etc., which occur worldwide. For example, according to a study, forced child begging is a noteworthy problem worldwide affecting solely the children, and the masterminds employ many methods to catch the toddlers within the net [2]. However, of the 7 billion people on the planet, 2.2 billion are children, and 143 to 210 million are orphans. Asia, Africa, Latin America, and the Middle East are the continents where orphans are most prevalent [3]. The communities are deprived of the bare necessary fundamental human rights such as access to healthcare. To address this issue, in this paper, we intend to develop a techno-social solution for making it easier to provide healthcare support to resource-constrained communities (with a particular focus on orphans in orphanages). Our primary focus is providing healthcare services via technological adaptation. To better fit this process, we designed our user studies. In the way of achieving our primary focus, necessary enhancement of the mobile application came in.
1.1. Healthcare services available for resource-constrained communities worldwide in current scenario
Varying nations and regions of the world have different conditions for communities with limited resources. Worldwide, initiatives like ‘RAMED’, ‘Clickhealth’, ‘Healthshare’, and ‘GiveMed’ have been implemented to give healthcare to communities with limited resources and the homeless [4], [5], [6], [7]. Children who become orphans because of war, invasion, natural catastrophes, conflict, persistent poverty, and fatal illnesses like AIDS are defenseless and without anyone to look after them [8], [9]. Children in these situations suffer multiple risks because of the chaos in the crisis-affected areas, including human trafficking, forced adoption, recruitment as child soldiers, child labor, begging gangs, prostitution, and drug misuse. According to UNICEF research, India has the highest number of orphan children, and Bangladesh is in fourth place. UNICEF identifies the sub-Saharan African nations as having the highest risk of orphans contracting AIDS [3]. Every child has the right to freedom, an education, access to healthcare, a place to call home, and safety from physical and psychological abuse. The international society, including UNICEF and WHO, conducts several campaigns to uphold these fundamental rights for children and to safeguard them against maltreatment.
1.2. Healthcare services available for resource-constrained communities in Bangladesh in current scenario
One obvious distinction between the underserved populations in other parts of the world—for instance, homeless people in the USA—is that these groups in Bangladesh have almost no access to technology, as our field study has confirmed. In Bangladesh, several healthcare treatments are available for beggars and other disadvantaged individuals, although they are typically unknown to the intended communities [10]. Bangladesh Rural Advancement Committee (BRAC) uses human resources for local patients' well-being in a limited resource context in rural and slum areas of Bangladesh [11], [12]. Finding a low-cost healthcare option is always the beggars' top priority when they become ill. When beggars in Dhaka city were interviewed for the field-level survey reported in ‘Dakter Bari’ [13], it was discovered that none of them visited doctors' private chambers. Most of them, typically without a prescription from a doctor, visit the closest drugstore and purchase certain medications from the pharmacy owner or shop personnel by describing the symptoms on their own. Few beggars choose to receive their medical care at government hospitals since they are the least expensive choice. To the best of our knowledge, ‘Dakter Bari’ was the first field survey revealing these behaviors among beggars in Bangladesh. On the other hand, some hospitals and organizations offer the underprivileged access to affordable and occasionally accessible healthcare treatments. For instance, Shikder Medical College and Hospital offers free medical care and treatment to the underprivileged every Friday [13]. Dhaka Medical College provides free medication along with daily treatment for just 10 BDT (0.12 USD). ‘Dakter Bari’ tried to resolve this problem by providing information on nearby available hospitals through an app with the help of intermediaries such as tea-stall men, pharmacists, etc., who are well connected to beggars.
1.3. Our proposed solution and research focus
Since there is a significant barrier between the relevant healthcare services and the intended poor recipients, the aforementioned circumstance provides a unique problem in the field of HCI (orphans in our context). We took the idea of intermediaries for our research on orphans from ‘Dakter Bari’. On the other hand, in ‘Dakter Bari’ tea stalls, men, pharmacists, and others acted as intermediaries with the beggars. ‘Dakter Bari’ provides beggars with information about nearby available hospitals via an app. In contrast, we used a mobile internet healthcare application called ‘Shastho-sheba’ [14] and updated this ‘Shastho-sheba’ app for our service, targeting in-house intermediaries to overcome the health-care situation in orphanages. To accomplish this, we worked with renowned medical professionals and prospective intermediaries willing to take time out of their busy schedules to offer online advice to orphans in orphanages. Our research involves intermediation in technology intervention for orphans in orphanages, which can be used later for other resource-constrained communities (RCCs) in further studies.
Initially, ‘Shastho-sheba’ was created to help people access healthcare during a lockdown when the COVID-19 attack was imminent throughout Bangladesh. This service was made available to provide online healthcare so that people would not have to leave their homes in such perilous situations. We customized the software for our online healthcare purpose to achieve our goal of providing online healthcare services to orphans in orphanages. Our proposal proposed the concept of internal intermediaries, essentially orphanage administrators. Our research questions in this study are three-fold:
RQ1: What is the present situation of healthcare services in orphanages in Bangladesh? How can we improve that using technological intervention?
To answer this question, we conduct a field survey over the orphans and orphanage administrators in the orphanages of Dhaka city to reveal the healthcare situation of the orphan children. Our survey contained a questionnaire about adopting technological interventions to this phenomenon. After addressing this question, we shift our attention to the following research question:
RQ2: How can we connect medical doctors with orphans and relevant orphanage communities through technological interventions?
To answer this question, we conduct semi-structured interviews with orphans and Orphanage Administrators (OAs) and discover that orphanage administrators and teachers can act as intermediaries for orphans in the same way that shopkeepers and pharmacists mentioned in the ‘Daktar Bari’ act for beggars in Bangladesh. We also survey medical doctors to get their opinion about our idea and implementation and, most importantly, their spontaneous participation. Then we move to our next research question:
RQ3: What could be the expected features for such technological interventions?
To address RQ3, we conduct a comprehensive examination of the key features and functionalities of the existing ‘Sastho-sheba’ app. As our plan involves adding intermediation as a layer to provide healthcare services, we made necessary modifications to these features, as detailed in Section 5.1. Subsequently, we engaged the intended users in the piloting phase to validate these features.
1.4. Our contributions in this study
How effectively and efficiently we can handle the problem of insufficient healthcare services for orphans in orphanages is the leading research focus of this study. We offer the following contributions to answer these research questions and achieve the study's aim.
-
•
We perform an online survey of doctors to let them know about our plan and to get their feedback about their contribution we intend to provide to the orphans in orphanages. Due to the rising cases of COVID-19, we could not do the field survey over them, and we perform the survey over the Internet.
-
•
To explore sustainability, we conducted a field survey building on the ‘Daktar Bari’ concept, which involved structured interviews with intermediaries of ‘Dakter Bari.’ Previous research highlighted the limited use of electronic devices among RCCs. Recognizing the potential for direct healthcare assistance through intermediaries, we surveyed individuals like salesmen in pharmacies and grocery shops who had previously used the ‘Daktar Bari’ app on their mobile devices. These intermediaries were not in-house, leading to challenges in sustained support. Based on these findings, we chose to survey over ‘in-house’ intermediaries.
-
•
We perform a field survey based on in-person structured and semi-structured interviews with orphans in orphanages in three different places in Bangladesh: Mirpur, Mohammadpur, and Azimpur. We also perform similar studies over related ‘in-house’ intermediaries - Orphanage Administrators (teachers, workers, nurses, etc.). We refer Orphanage Administrators as OAs in this paper.
-
•
Based on the survey findings, we have directed our attention towards a techno-social solution to deliver healthcare services to orphans in orphanages. Within this framework, we place a primary emphasis on the integration of technology into the existing resource limitations. Our approach involves enhancing and customizing an Android mobile application, ‘Shastho-sheba patient,’ intended for intermediaries such as orphanage administrators and nurses. Through this application, orphans can access medical consultations over the Internet with the help of intermediaries. To facilitate this bidirectional communication, we also improve another Android application, ‘Shastho-sheba doctor,’ designed for healthcare professionals. We undertake these modifications to offer the intended healthcare services through technological adaptation to benefit the orphans in the orphanages.
-
•
We deploy our solution in the surveyed orphanages, and further deployment is still ongoing. In the meantime, we also perform some post-deployment monitoring.
2. Related work
2.1. Studies on status of resource-constrained communities
Resource-constrained communities (RCCs), characterized by low-income and social marginalization factors, encompass various disadvantaged groups globally. One of the most underprivileged and stigmatized social groups worldwide is that of beggars [15]. An investigative field survey in Amroha city, India, provides insights into the socioeconomic status of beggars and government poverty alleviation schemes [16]. One study in Nigeria revealed that communities' understanding of their healthcare options was poor [17]. Morocco's ‘RAMED’ program, offering free access to hospital care for the most vulnerable, has demonstrated positive outcomes in enhancing healthcare access [4]. In Bangladesh, densely populated slum areas are hotspots for water-borne and unsanitary diseases. Residents in Dhaka and Rajshahi slums exhibit subpar hygiene standards [18]. According to studies [19], [20], pregnant women and infants, particularly in Dhaka's slums, face heightened vulnerability. The social-demographic research revealed that the Indian refugees were denied access to fundamental rights and that their health was noticeably poor [21]. Communities of the homeless and female homeless people exhibit a significant healthcare access gap. One article examines ways of empowering women providers such as nurses and midwives who facilitate healthcare services to distressed women [22]. The role of human resources in providing healthcare services to resource-constrained communities has been studied several times [23], [24]. Researchers discovered that efforts should be made to enhance health through biological, educational, environmental, and policy initiatives for those who are homeless with higher rates of disease and [25], [26].
As we intend to focus on orphan health as well, we find some related studies to get known to their socio-economic and health status worldwide and in the context of Bangladesh. Three orphanages in Dhaka city—Rayarbazar Rahamania Etimkhana, Sir Salimullah Muslim Etimkhana, and Bawniabad Islamia Etimkhana—were the subject of a cross-sectional study. The study's main goal was to determine the orphanages' healthcare resources and each individual's nutritional status, which was heavily influenced by eating habits [27]. Semi-structured interviews in Sylhet City revealed the cruel treatment of orphan children and beggars and their precarious health [8]. An investigation into the socio-demographic characteristics of India's orphans was conducted [9]. Moreover, sub-Saharan African nations, including Kenya, Nigeria, and Uganda, grapple with severe health challenges, necessitating action from governments and international organizations [28], [29], [30], [31], [32], [33], [34], [35]. Our study focuses on providing good healthcare to a group of people with resource constraints living in orphanages.
2.2. Impacts of HCI on resource-constrained communities
The design of interactive systems for inclusion [36], learning [37], and marginalized communities [38] has also been studied in various HCI studies. Significant psychological discomfort, such as post-traumatic stress disorder, affects refugees. The first step in treating them is diagnosing the disease, and in a study, some Bangladeshi researchers used an EEG gadget and hand sketches to do so [39], [40]. Numerous studies have been conducted to offer solutions for various homeless populations, such as young homeless, homeless moms, and urban homeless communities in multiple nations [41], [42], [43], [44], [45], [46]. Access to knowledge is recognized as crucial, as demonstrated by implementing free Wi-Fi in underserved areas in South Africa [47]. In Bangladesh, street children represent a vulnerable group, and a study suggests mechanisms to facilitate communication among stakeholders and donors [48].
Developed systems that use mobile technologies to encourage communication among young, jobless, and homeless people [49], [50], [51]. Utilizing interactive voice and video systems, as well as various social media platforms, for a variety of services such as educational support [52], [53], financial management, cultural integration, and agricultural support [54], [55], among others, are additional systems that aim to improve the lives of resource-constrained communities.
HCI's contribution to the healthcare sector in resource-constrained communities is substantial. Doctors have adopted telemedicine to deliver healthcare services in Africa [56]. Another Android app that assists the homeless in finding the closest medical facility is called ‘ClickHealth’ [5]. Text messages have been embraced for healthcare purposes among homeless populations [57]. The prevalence of digital devices among resource-constrained communities is nonexistent in developing countries like Bangladesh [58]. For those who wish to donate their unneeded medications to the underprivileged or needy who require them, several researchers in Bangladesh have created the ‘GiveMed’ web platform [6]. ‘HealthShare,’ a web-based system, aids in identifying and contacting homeless individuals for healthcare services in USA [7]. Rural Kenya faces healthcare challenges, leading to the development of a USSD-based system for feedback on community health worker services [59]. Our study contributes to HCI by designing a techno-social solution to connect medical professionals with orphans and communities in orphanages.
2.3. Intermediaries as bridges to empower people
According to research by Sambasivan et al. [60], and Parikh & Ghosh [61], intermediated interaction is a common style of technology interaction in the developing world. It makes it possible for people to look for and use information that would otherwise be unavailable to them because of their lack of literacy, numeracy, technology operation skills, or financial limitations that prevent them from owning technology. These works provide interfaces for shared technology use, building on the argument for human infrastructure in developing and using technology. A proxy primary user, or intermediary, having the necessary access rights and operating skills assists those who would otherwise have only limited or no access to the technology [60]. Intermediaries, who link producers and customers by disseminating information and making product recommendations to their real-world social contacts, are a crucial group of individuals facilitating market transactions on e-commerce platforms [62]. The role of successful intermediaries has been researched in previous work to facilitate improved promotional services in sales. Utilizing this idea of mediation, previous research in the HCI and ICTD literature produced tools for social media access [63], apps for financial management systems, and more [64], [65] to function in resource-constrained contexts. To mediate online services and help recipients with limited resources [66], [67], [68], issues relating to deployment difficulties [69], [70], [71], trust, and sustainability of these intermediary-based systems have also been studied. Such intermediaries empower beneficiaries by enhancing their technological knowledge and proficiency [71], [72], [73]. The critical component of systems incorporating technological exchange is shared and unequal use of the technology. Here, Parikh & Ghosh further the intermediary as the primary user and the beneficiary as the secondary user. Our work is unique in that we concentrate on providing individuals with healthcare access who have little to no technology experience and who lack the means to do so. Information intermediary, also known as an infomediary, is a phrase used to describe a person who is “interested in enabling access to information from numerous sources and active in informing, aggregating, assembling, and signaling information” [74]. Prior research on ICT engagement with infomediaries [75], [76], [77], [78] has a strong emphasis on enhancing their current beneficiary contacts through technology for deeper penetration of information systems. In the context of technology transfer, research has explored the role of internal intermediaries [79]. Previous work in Bangladesh, as seen in ‘Dakter Bari,’ examined intermediaries as bridges for providing healthcare to beggars [13]. Our study applies the concept of intermediaries as a means to provide healthcare access to resource-constrained communities, particularly orphans, who lack technological experience and resources.
2.4. Healthcare interventions in HCI domain
HCI has been instrumental in designing systems for healthcare service delivery. Research has explored personalized voice and web-based feedback to support community health workers [80]. IoT-based healthcare platforms have integrated existing technologies to provide assisted living mobile healthcare services [81]. Text messages are being used to promote healthy living, provide appointment reminders, and deliver just-in-time interventions to prevent risky behavior [82]. mHealth solutions have gained traction in developing nations, with research focusing on factors influencing adoption and sustainability [83], [84], [85]. Studies [85] revealed a knowledge gap, necessitating the creation and validation of an appropriate model for evaluating the sustainability of mHealth systems in underdeveloped nations. The study of mHealth's impact on Bangladeshi seniors is an example of HCI's involvement in the sector [86]. In this study, we improve the current mobile app and investigate its features to give orphans access to healthcare.
3. Methodology
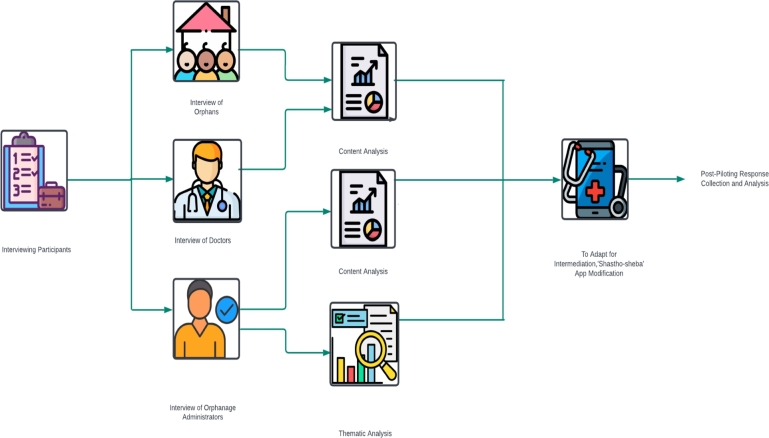
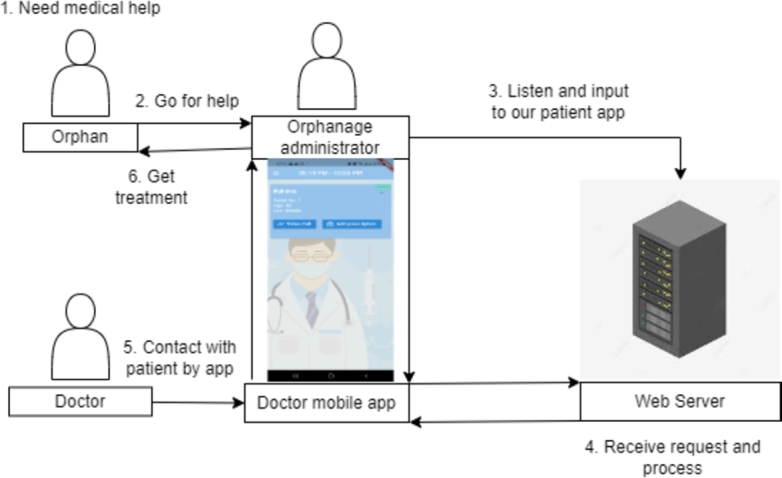
We plan to use Orphanage Administrators (OAs) as Intermediaries to provide healthcare services via technological interventions to the orphans in the orphanages. In the process of our research study, we conducted interviews and fieldwork with doctors, OAs, and orphans. Fig. 1 shows an overview of our methodology.
Figure 1.
Methodology of Our Study.
3.1. Participant recruitment
The survey with the doctors was carried out between May 2021 and January 2022, during which we encountered challenges in recruiting doctors due to the constraints imposed by the COVID-19 pandemic. As a result, we had to opt for an online mode of survey administration. A total of 14 doctors participated in our study, recruited through three distinct sources. Initially, we reached out to doctors in our close network via email. Subsequently, these initial contacts assisted in further recruitment by reaching out to their own professional connections [87]. Finally, we utilized social media platforms to disseminate information about our study, attracting doctors from our online social network.
Before outlining our research plan with Orphanage Administrators (OAs) as intermediaries, we conducted site visits to the orphanages. During informal discussions with the OAs, we identified their close proximity to the orphaned individuals within the orphanages. This proximity validated our decision to employ OAs as intermediaries, and we headed to the semi-structured interviews with them. Throughout our research, we remained committed to acquiring comprehensive insights while prioritizing the safety and well-being of our participants. These principles influenced sample sizes for both orphans and intermediaries. Amid the challenges posed by the COVID-19 pandemic, we selected four orphanages within a 1 to 6 km radius of our residential area, ensuring practical accessibility established by the orphanage authorities. It is worth noting that within the context of Bangladesh, there is a shortage of OAs, such as nurses, teachers, and supervisors, relative to the number of orphan students in some institutions. For instance, the Markazul Quran Jannatun Nisa Orphanage accommodates approximately 30-35 students but only has two OAs. We collected data from 10 intermediaries out of a potential 15-20. Our analysis revealed recurring themes and sentiments in the intermediary responses, signifying that our sample adequately represents the perspectives of the broader group [88].
For the orphans, we conducted 17 detailed questionnaire-based interviews across the four orphanages from April 2021 to May 2022, collectively hosting approximately 250 orphans. To foster a comfortable and interactive environment, one of our researchers engaged in in-depth sessions during the interviews, and another one meticulously recorded the responses in our prepared and carried questionnaires in hardcopy format. Each interview extended over a duration of approximately 5 to 25 minutes. As the interviews progressed, a discernible pattern of recurring responses emerged, indicative of data saturation. Consequently, the 17 interviews collectively provide a representative snapshot of the broader orphan population's experiences and challenges [88], [89].
3.2. Interview protocols
3.2.1. Information gathering via online interviews with doctors
We recruited doctors in our user study because doctors are the ones who will provide healthcare to orphans using our mobile application. In this regard, their thoughts, and suggestions about our research design were paramount. The primary objective of this phase was to secure their consent to participate in our research and to assess the effectiveness of our initial research plan before introducing the intermediary layer. During this stage, we specifically focused on gathering their opinions about online consultations for resource-constrained communities in a broader context. The detailed examination of the intermediary layer was deferred to a subsequent phase of our research plan, where we intend to conduct in-depth, semi-structured interviews to obtain comprehensive feedback on its implementation in future work. We asked them 24 questions, including about the consent, expectations, and confidence regarding the platform we plan to build alongside other basic demographic questions. We have used a five-point Likert scale [90], [91] in our interview questionnaire for questions like “To what extent, you are confident that our idea will be a realistic one?”, “In case there would be a facility for physically attending and examining the patients (beggars) in a voluntary manner at your convenient time and place instead of the online consultation over the Internet, what will be the extent of your interest in participating there?”, etc. (details are in supplementary materials). There were different responses from the participants, which we discussed in the findings later. There were some open-ended questions about what facilities they expect from the online platform in providing consultation over the Internet, how many hours a week they generally want to spend providing services, their preferred schedule for online consultation, and their opinion on physically attending to the patients. Finally, we wanted to know their suggestion or any comment about our idea - “What are your suggestion(s), comment(s), and/or critique(s) regarding our idea? How can it be improved/shaped up?” Among the responses, different types of suggestions came up. We acknowledged their valuable opinions and incorporated those in the mobile application design.
3.2.2. Fieldwork with the orphanage administrators (OAs) as intermediaries
In our journey to bridge the gap in healthcare accessibility for orphaned students, we recognized the pivotal role that intermediaries could play, and, in our case, these intermediaries were the OAs. Our survey, conducted with a dual purpose in mind, sought to introduce our vision and objectives while assessing the availability of these intermediaries. The initial phase of our field study started in April 2021 when we separated into groups and ventured into various orphanages to gain a firsthand understanding of their conditions and the extent of support we could expect. Later, in October 2021, we started taking semi-structured interviews with the intermediaries. By this time, we had worked on preparing the semi-structured interview questions and refining them to better fit our research focus. We interviewed teachers, nurses, staff, and supervisors who work in the orphanages to know their interest and cooperation in providing healthcare services to their orphan students. Each interview took 30-40 minutes to complete. We started our questionnaire with demographic questions and their technological skill with the devices. Our questionnaire included how the administration takes care of the health care expenses of the students there and how they deal with this. We inquired into the everyday health challenges faced by orphaned students and probed into the reasons underlying the apparent gaps in their access to existing healthcare services within the orphanages. The administrators shared invaluable insights, responding to questions like,- “What are the health issues orphan students here face so that you have to search for medical services?” “Do you have any opinion or comment regarding the treatment your orphan students are receiving? If so, please mention” and “How much do you have to spend on an average per month regarding health issues of the orphan students?”. We asked questions about their eagerness to support the orphans as intermediaries. They gave their valuable opinion on how practical and realistic our online platform would be, according to which we stepped into our next task.
3.2.3. Fieldwork with resource-constrained communities
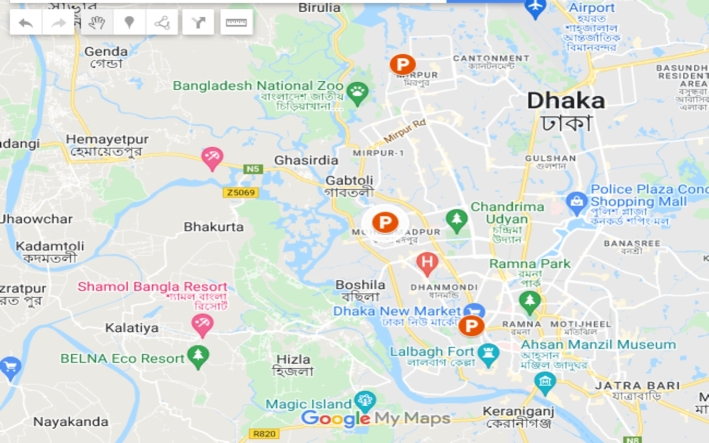
As mentioned in section 1.3, we conducted our field study in different areas of Bangladesh, namely Mirpur, Mohammadpur, and Azimpur. We offer a high-level overview of the sites investigated in Fig. 4. Some of the orphans' pictures are shown in Fig. 2. Fig. 3(a), and 3(b) shows some orphanages we visited for fieldwork and deployed our mobile Application later.
Figure 4.
Snapshot of Chosen Locations for Our Survey (P Marked).
Figure 2.

Orphans in the Orphanages.
Figure 3.
Orphanages in Mirpur, Mohammadpur, and Azimpur Area.
We conducted the interview in Bengali, recognizing that the orphans under study are native Bengali speakers. The fieldwork involved the presence of two researchers from our team, each assigned specific roles to ensure a conducive and comfortable environment for the orphans. One researcher played a pivotal role in establishing a friendly and reassuring atmosphere, fostering a sense of ease and willingness among the orphans to respond to our inquiries. To ensure an accurate record of the interviews, the other researcher documented the conversations and notations on hardcopy questionnaires, which we printed and carried to the field. Later, this researcher transcribed the recorded interactions, cross-checking for any omissions or inaccuracies in the notes and facilitating the translation of the conversations from Bengali to English.
Specific questions were tailored to gauge their likely responses and acceptance of our proposed online healthcare service. For example, we inquired about their experiences in seeking medical treatment and asked them to rate their satisfaction with their current course of treatment, employing a five-point Likert scale. The orphans were presented with scenarios and questions to evaluate their receptiveness to the envisioned online healthcare service. An example query was “Do you find difficulties in searching hospitals to get treatment?” We probed their preferences for engaging with healthcare services online, asking - “If you get a chance to get free health service online via an app to contact a doctor through video calling helped by someone, what medium will be more helpful?”
3.3. Data analysis
The interviews with the doctors, orphans, and a subset of the intermediaries underwent a content analysis process [92], [93], [94]. As we mentioned earlier, one of the researchers recorded the interviews and transcribed them. This researcher subsequently conducted the content analysis. The insights extracted from these interviews played a pivotal role in guiding the progression of our research plan, which we discuss later.
In the case of the Intermediary interview, we used thematic analysis [95], [96]. Following data collection, two team members independently coded each interview, building the codebook incrementally. This iterative process involves re-coding previously coded interviews as the codebook evolves. Once all interviews are coded, the team members compare their codes, reconciling any discrepancies to generate the final codes used for thematic analysis. This rigorous approach ensures the validity and reliability of our findings, providing a robust foundation for our subsequent analyses and recommendations.
3.4. Ethical concerns and approval
This work was conducted with reference to the online medical consultation for resource-constrained communities in Bangladesh, and the work has received ethics approval number - Est/Ta-4/Ref-3388. The Ethics Committee run by Bangladesh University of Engineering and Technology Institutional Review Board (IRB) approved all the methods and procedures involving human subjects for this study. The participants have consented to the inclusion in this research.
4. Findings from interviews
In this section, we present the key insights and observations drawn from our interviews and field studies with resource-constrained communities, doctors, and intermediaries. We present a comprehensive overview of the outcomes from multiple vantage points.
4.1. Outcomes from online survey over doctors
Our data collection involved interviews with doctors from diverse backgrounds and regions of our country, as summarized in Table 1. Of the 14 participants, 12 expressed their voluntary commitment to provide free healthcare consultations to resource-constrained communities via the Internet. Below, we highlight the significant findings derived from this survey.
Table 1.
Demographic Table of the Participants.
| Participant Group | Variable | Classification | Frequency |
|---|---|---|---|
| Doctors (N=14) |
Age (years) |
<25 | 1 |
| 25-35 | 9 | ||
| 36-45 | 1 | ||
| 56-65 |
3 |
||
| Gender |
Male | 7 | |
| Female |
7 |
||
| Education |
MBBS | 9 | |
| MPHIL | 1 | ||
| FCPS | 1 | ||
| MD | 1 | ||
| PHD |
2 |
||
| Designation |
Medical officer | 9 | |
| Consultant | 1 | ||
| Associate professor | 1 | ||
| Professor | 1 | ||
| Founder and Managing | 1 | ||
| Director | 1 | ||
| Orphanage Administrators (N=10) |
Age (years) |
<25 | 2 |
| 25-30 | 1 | ||
| 31-35 | 2 | ||
| 41-45 | 4 | ||
| 51-55 |
1 |
||
| Gender |
Male | 8 | |
| Female |
2 |
||
| Education |
H.S.C | 5 | |
| B.S.C | 4 | ||
| M.S.C |
1 |
||
| Electronic Device Usage |
Mobile | 10 | |
| Television | 10 | ||
| Others | 10 | ||
| Orphans (N=17) | Age (years) |
6-10 | 8 |
| 11-15 | 8 | ||
| 16-20 |
1 |
||
| Gender |
Male | 4 | |
| Female |
13 |
||
| Education |
Below class-1 | 1 | |
| Class 1-2 | 3 | ||
| Class 3-4 | 3 | ||
| Class 5-6 | 3 | ||
| Class 7-8 | 1 | ||
| Class 9-10 | 2 | ||
| Hifz | 3 | ||
| Najera |
1 |
||
| Electronic Device Usage | Mobile | 0 | |
| Television | 13 | ||
| None | 4 | ||
4.1.1. Problem-driven application enhancements
Our representative doctors suggest a variety of design modifications for the application that are driven by the generation of specific problems. These suggestions have contributed to the development of a streamlined application. Notably, a suggestion to offer the patient app in Bengali, with intermediation, was well-received and recognized as a potential avenue for future work. Selected feedback is provided below, with further insights detailed in Section 5.4:
P13: “The system should be as simple as possible.”
P14: “I think you can make the app Bangla.”
P12: “Obviously, it's a very good idea. After starting this activity, problem-based solutions and modifications will be helpful.”
4.1.2. Effectiveness and realism of online consultation
We found mixed reactions about the effectiveness of our plan. P6, P11, P13, and P14 are very confident that our idea ends up being a realistic one, whereas P3, P7, and P8 feel less confident. P1, P2, P10, and P12 are neutral about their opinion. The rest of the participants think our plan is never going to be a realistic one. Selected comments reflect this diversity of perspectives:
P3: “I personally don't prefer online platforms for managing patients. Otherwise, it's a good initiative for the targeted population... like something is better than nothing.”
P4: “Because in a country like ours, it's impossible for beggars to use the internet, whereas most poor people don't even have any smartphone.”
P9: “It might not be effective because of lack of logistic support, awareness, Doctor-Patient relationship in view of virtual and real Clinical scenario and historical differentiation.”
P10: “If the convenience of the doctors, especially junior doctors, is identified, then it can be a good initiative.”
4.1.3. Field-work for the resource-constrained communities (RCCs)
We inquired whether doctors were interested in conducting physical examinations of RCCs as an alternative to online consultations. Only three respondents expressed interest, while five were uninterested, and the remaining participants maintained a neutral stance. The surge of COVID-19 affected their responses at that time. Moreover, doctors who expressed interest in fieldwork preferred locations in proximity to their residences. Some of their comments are as follows:
P3: “The place can be in a diagnostic center or any place but easily accessible.”
P1: “Not interested in field camp unless Covid situation improves. Otherwise, at the Hospital.”
P10: “Any suitable place nearby my residence.”
4.2. Outcomes from the interviews with the intermediaries
The in-house intermediaries in our system are orphanage administrators, such as teachers, nurses, workers, and supervisors in the orphanages. We found various interesting findings from the field survey that we present in statistics and themes.
All of the OAs express their interest in being intermediaries. We could reveal that the intermediaries are proficient enough to use smartphones and internet technologies to adopt our proposed techno-social service on behalf of the orphan students, as shown in the Table 2. We asked them about the sources of financial support needed as expenses for the orphans' healthcare services. We found two of the four orphanages can support their financial expenses with the grant they get from the government. Two other orphanages have only three OAs in total, and they have to rely on donations from others. We also find that these two orphanages hardly afford money for healthcare services. In response to the mode of online consultation over the Internet, all of the OAs prefer to use intermediation. Although most of them didn't discuss in detail about their rationale, however, we would like to highlight three comments here:
Table 2.
Intermediary Interview Results.
| Category | Frequency |
|---|---|
| Proficiency in Technology | |
| Smart Phone | Proficient (5), Good (4) |
| Internet | Expert (1), Proficient (5), Good (3) |
| Financial Supports | |
| Government Grant | 2 orphanages |
| Public Donation | 2 orphanages |
| Mode of Preferred Online Consultation | |
| Helped by the orphanage administration | 10 |
| Helped by Volunteers | 0 |
OA3: “Orphans do not communicate properly, they hide their disease, and they have a lot of female healthcare problems as it is a mohila orphanage, so female worker here is good for them.”
OA5: “Most of the students are females, there is the privacy issue.”
OA8: “We remain here 24/7.”
From the detailed answers transcribed from the conversations with the OAs, we could extract themes. We present the emergent themes, each supported by direct quotes from participants, providing a nuanced understanding of the healthcare ecosystem within orphanages. We distilled three predominant themes that encapsulate the challenges in ensuring adequate healthcare for orphans. These themes are detailed in Table 3.
Table 3.
Summary of Thematic Analysis Results.
| Theme | Brief Description |
|---|---|
| Lack of Money | Financial constraints limiting access and quality of healthcare for orphans. |
| Lack of Proper Treatment | Concerns over quality, potential stigma, and gender-specific healthcare needs. |
| Lack of Availability | Challenges in providing continuous and round-the-clock healthcare. |
4.2.1. Lack of money
Financial constraints emerged as a significant barrier to accessing healthcare services for orphans. OA3 articulated these challenges, stating,
“Their family doesn't spend money; we also do not have the financial sufficiency to proceed.”
This sentiment was echoed by OA2 and OA10, who emphasized the inability to afford essential healthcare services. The recurring mention of these financial challenges underscores the critical need for sustainable and cost-effective healthcare solutions tailored for orphanages, as these constraints not only limit access but also influence the quality of healthcare received by orphans.
4.2.2. Lack of proper treatment
Concerns related to the quality and appropriateness of medical treatment received by orphans were evident. OA2's response highlighted potential stigma and challenges:
“I get bad treatment from the doctor when they see we have come from an orphanage.” He further elaborated on the communication barriers and unique healthcare needs, especially for female orphans, stating,
“Orphans do not communicate properly, they hide their disease, and they have a lot of female healthcare problems as it is a female orphanage, so a female doctor is good for them.”
These insights indicate the importance of gender-sensitive healthcare interventions and the need to address potential biases in medical treatment.
4.2.3. Lack of availability
Ensuring continuous and round-the-clock healthcare for orphans poses challenges for orphanages. OA4 succinctly captured this challenge, stating,
“We try our best to provide, but 24/7 is not possible.”
This highlights the need for scalable solutions, such as telemedicine platforms or partnerships with local healthcare providers, to ensure timely medical intervention and consistent medical support.
4.3. Outcomes from the interviews with the orphans
We discuss the findings from our field study with the orphans in the orphanages. We dig down into their situation in the socio-economic contexts, dig down into their health conditions and availability of healthcare services, and inquire about their opinion on the intermediation process.
4.3.1. Access to the technologies
According to the table of demographic information of the orphans (Table 1), we can see all the seventeen orphan students of orphanages are children. Their discrete relationship with technologies suggests that they are in a resource-constrained environment, and a self-perform online mode of healthcare consultation is inaccessible to them. Four orphans have no relationship with any kind of electronic device, and none have access to a mobile phone. They mostly use others' phones for communication purposes, while two of them even do not have access to others' phones.
4.3.2. Health conditions
When the orphans were asked about their current status of illness and diseases, we found that 11 of the orphans were sick, and two of them were not sure about their current health condition. We found the diseases they encounter, and here, we present the number of participants for each disease inside the bracket. The most common diseases they usually suffer from are cough (5), headaches (4), fever (4), and respiratory problems (3), such as pneumonia (1), asthma (1), menstrual problems (2), stomach pain (2), waterborne diseases (1), eye problems (1), malnutrition (1), pox (1), etc. We present all the information in Table 4. Some of the diseases occur frequently, as one orphan mentioned that:
Table 4.
Orphan Interview Results.
| Category | Frequency |
|---|---|
| Health Conditions | |
| Sick | 11 |
| Not Sure | 2 |
| Not Sick | 4 |
| Health Issues | |
| Cough | 5 |
| Headache | 4 |
| Fever | 4 |
| Respiratory Problems | 3 |
| Menstrual Problems | 2 |
| Stomach Pain | 2 |
| Eye Problem | 1 |
| Waterborne Diseases | 1 |
| Nearby Healthcare Services | |
| Pharmacy | 8 |
| Hospital | 4 |
| Doctor Visits Orphanage | 7 |
| None | 1 |
| Mode of Preferred Online Consultation | |
| Helped by the orphanage administration | 15 |
| Helped by Volunteers | 2 |
P14: “I have to go through severe stomach pain every morning.”
Some of the diseases are interconnected to each other; P3 talks about how his/her headache is connected with severe coughing problems:
P3: “When I have heavy cough for 2 to 3 days, headache also increases.”
4.3.3. Availability of healthcare services
The results in Table 4 reveal that most of them go to the pharmacy to seek healthcare services without prescriptions, which is a significant risk to anyone's health. Other than that, doctors visit their respective orphanages twice/thrice a week in Sir Salimullah Muslim Orphanage, which is one of the largest orphanages in Bangladesh. In the case of severe issues or emergencies, the orphans from most of the orphanages go to the nearest government hospitals to get healthcare services at a cheaper cost. Most of the time, they are neglected due to being orphans. The results also reveal that the healthcare services they are availing currently are not continuous, and they do not get the services whenever they need them. Therefore, healthcare support is still at stake.
Shaheed Suhrawardy Medical College is the nearest government hospital to Mohammadpur, and the hospital's distance from the orphanage is about 500 meters. When it is an emergency case (like an accident or something else very serious), they go to the nearest hospital. They are satisfied by the treatment they get from the hospital in emergency cases. They gave different opinions on whether they get proper medicines from a pharmacy. Six of them find it easy to get medicines, but the other two do not. According to the reason for finding medicines difficult, One student said,
P5: “One day, I went to the pharmacy, but there was a scarcity of medicines I needed for myself as per doctor's prescription.” Sometimes, when there was lockdown all around the country, they could not go to hospitals and felt that if they could get medical service sitting at the orphanage.
4.3.4. Opinion about mode of intermediation in online healthcare consultation
We described and showed them the prototype of an online healthcare mobile application and asked them what they would prefer as a medium if they get a chance to get free health service online via an app to contact a doctor through video calling helped by someone. They felt that help by the orphanage administration would be more helpful (Table 4). Regarding their suggestion on our proposed method, one of the female students said,
P1: “I face menstrual problems sometimes but can not reveal my problem to the orphanage administration because of uncomfortable feeling, if I can consult with any female doctor over the phone, it would be very suitable and comfortable for me.”
5. Redesign, enhancement, modification, and deployment of ‘Shastho-sheba’ mobile application
We had an existing online healthcare app named ‘Shastho-sheba,’ developed for providing medical services through video calls and e-prescription. We redesigned and enhanced the application to fit it with our research plan. Our new app model is mainly divided into two parts: one is for doctors, and the other is for orphan students who get healthcare services through OAs. As orphans in orphanages are resource-constrained, they are mostly unfamiliar with using mobile devices and have limited access to technology. As a result, adding a layer of intermediation is helpful for them [13].
5.1. App enhancement for our study
We used the MongoDB server for the database as development tools. We chose NodeJS, a JavaScript-based framework for the back-end. The programming language Dart is used with the Flutter framework for front-end development. In the subsequent sections, we provide details about our app enhancement progressions.
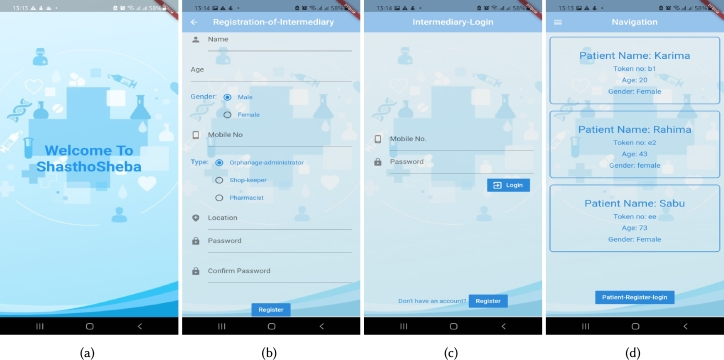
5.1.1. Introducing registration of the intermediaries in ‘Shastho-sheba patient’ app
In the previous model of the app, no intermediary was introduced. But in our system, the intermediaries play a vital role in connecting orphan patients and doctors by being go-betweens in handling the technology. To meet the role, intermediaries must register as users in the app and then log into the app as verified users (Fig. 5(b), and (c)). After successful login, intermediaries can make the patients (orphan students) log in to the app. In this way, certain patients can be under one intermediary that can be shown as a list. Fig. 5 shows an overview of this whole system design. Fig. 5(a) shows the welcome page. The users' information (patients and intermediaries) is saved to the database. Through API calling from the back-end to the front-end, the saved data info of users can be accessed in the app.
Figure 5.
Different Interfaces of Enhanced ‘Shastho-sheba’ App for Intermediary (a) Welcome Page, (b) Registration Page, (c) Login Page, and (d) List of the Patients under the Assigned Intermediary along with the Register-login Button.
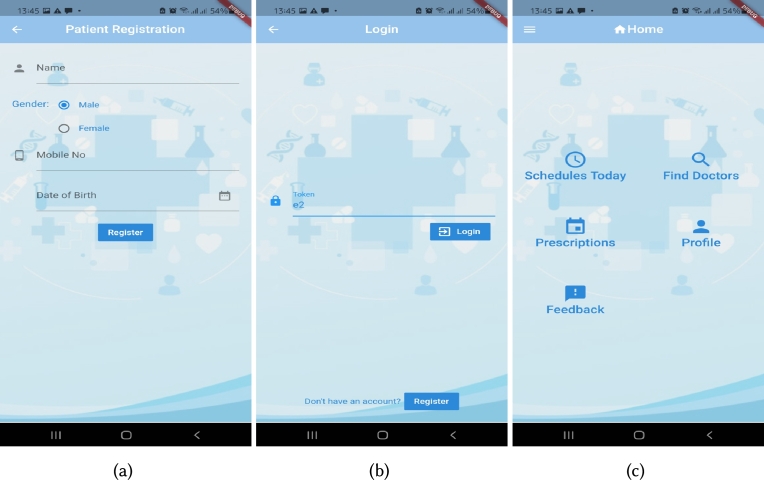
5.1.2. Login and authentication with patient token in ‘Shastho-sheba patient’ app
According to the previous design, users had to log in to the app with a specific mobile number and password. As the new design involves intermediary registration and registration of patients via intermediaries, the complexity of the process is expected to be less possible. We found that the intermediaries are not experts in technology usage, and orphans have almost zero knowledge about technology; the most straightforward design we could think of is just using a token to make the patients log in to the system by the intermediaries. After intermediary login, an intermediary can register as many patients as possible (Fig. 6(a)). After that, each registered patient gets an automatically generated token stored as a list in a table in the app (Fig. 5(d)). Later, a token is used to further login for a particular patient (Fig. 6(b)). Fig. 6 shows an overview of the system design using the idea of a user-friendly patient token. Unique token numbers can be produced each time in the NodeJS framework.
Figure 6.
Different Interfaces of Enhanced ‘Shastho-sheba patient’ App for an Intermediary (a) Registration Page for the Patient, (b) Login Page for the Patient, and (c) Home Page of the Patient after Login with Necessary Features.
5.1.3. Removing the process of taking appointment in ‘Shastho-sheba patient’ app
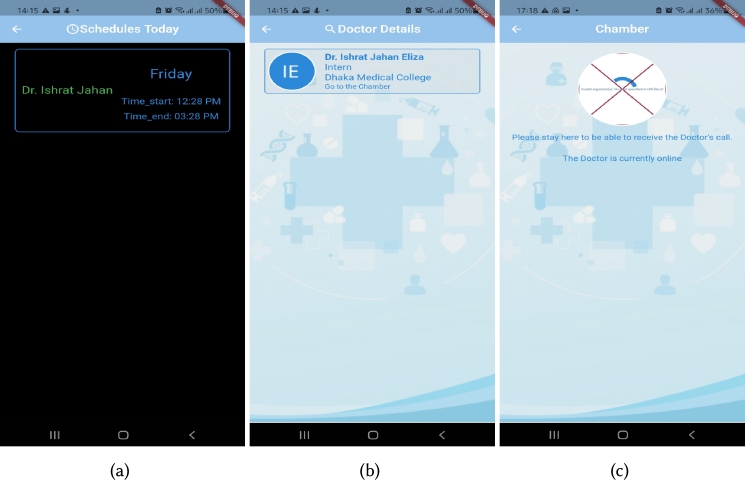
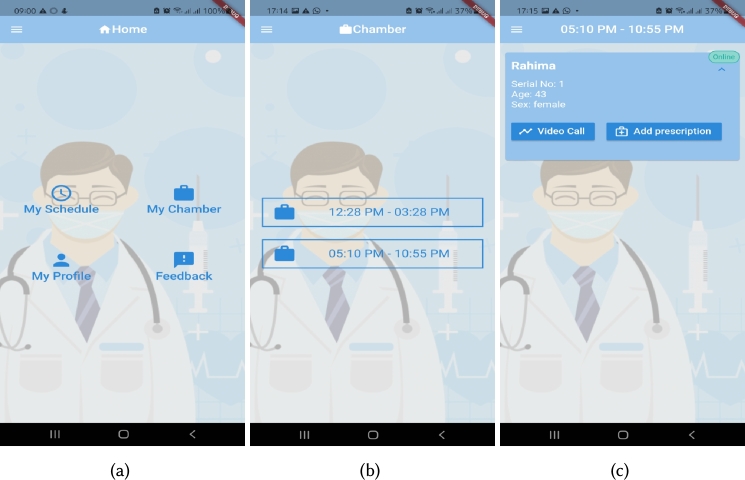
The previous design had an appointment feature. We acknowledge that it would be challenging to make appointments for every patient as it would be a complex, lengthy process. To ease this problem, we have removed the appointment process. After proper login and verification, patients can see that day's schedules in the “Schedules Today” option from the home page (Fig. 6(c)) and can see the scheduled doctor's details (Fig. 7(a), and (b)). Then the patient can enter the particular doctor's chamber when it is their turn. After entering the chamber, a patient can see if the doctor is online or offline (Fig. 7(c)). Fig. 7 demonstrates the system that works accordingly without taking an appointment for a particular doctor. The user had to click on the “Take appointment” button in a prior version of the current code. However, in the modified version, the button has been deleted, and this appointment feature has been added silently in the chamber module, so when the user enters the chamber, an appointment will be established automatically in the background based on the user's unique chamber ID which the user can't see explicitly. Conversely, in the doctor app, the doctor can enter their chamber on the scheduled time frame. Upon seeing the patient online, they can establish a video call. Fig. 8 shows how the simplified version of the developed system looks from the doctor's end. The doctor can find all of their configured schedules in his/her homepage (Fig. 8(a)), he/she can enter to their chamber (Fig. 8(b)) and can see the appointed patients are online or offline (Fig. 8(c)).
Figure 7.
Different Interfaces of Enhanced ‘Shastho-sheba patient’ App for Intermediary (a) Page Containing All the Schedules of a Particular Day on the Particular Time Frame Page after Pressing Schedules Today Option in Home Page, (b) Doctor Details Page after Selecting a Schedule Card, and (c) Chamber of the Doctor Page Indicating if the Doctor is Online or Offline.
Figure 8.
Different Interfaces of Enhanced ‘Shastho-sheba doctor’ App for Health Professionals (a) Home Page for Doctors with My Chamber Option, (b) Page Containing All the Schedules of a Particular Day, and (c) Chamber of the Doctor Page Indicating if the Patients are Online or Offline.
5.1.4. Removing the transaction section in both apps
Our healthcare platform intends to work voluntarily with the patients. In the previous commercial version, there was a transaction part to collect fees. But now, no more transaction is needed for payment as doctor's fee as the doctors gave their consent to give treatment at free of cost. Thus, we have removed the transaction process from the previous app model. Fig. 9 shows the simplified version of creating a new schedule without fee information on the doctor's end.
Figure 9.
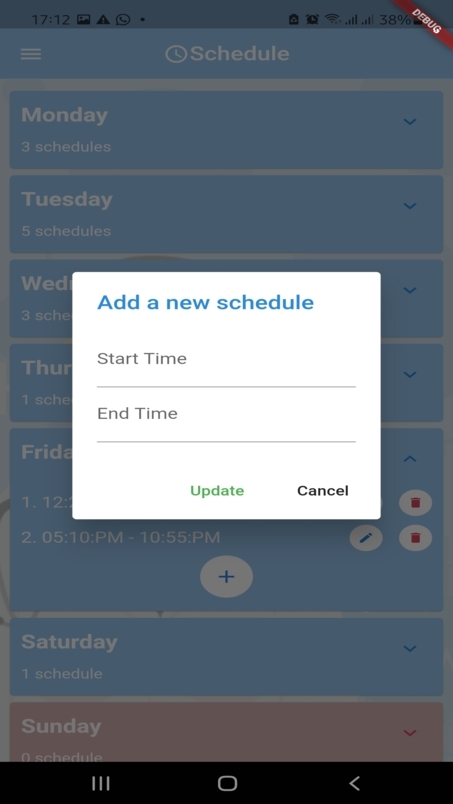
‘Shastho-sheba Doctor’ App for Doctors with Add New Schedule Page without Fee Information.
5.1.5. Turn server added for video call in both app
To establish the video call between patients and doctors, a turn server is a must in Flutter. The TURN (Traversal Using Relays around NAT) server is meant to bypass the Symmetric NAT restriction by opening a connection with a TURN server and relaying all information through that server [97]. In the previous app system, the turn server was free and not working at all. We ran into a few snags while setting up a video call on the app. Initially, only the user's face could be seen on the app's video camera, but the user on the other side could not, and the audio was not working. We needed to fix the problem, so we changed servers, but the app only operated in the same network, not in separate ones. We bought a server in AWS to set up the turn server. We set up the turn server on an EC2 instance. We needed a domain, so we purchased shasthosheba.live from name.com and installed it on the EC2 server. The turn and stun servers, turn.shasthosheba.live, and stun.shasthosheba.live, are added to the domain. We checked if the turn server was operational. We initially received an error, but after some troubleshooting, turn/stun began to operate in the appropriate port number. We requested an SSL certificate and received it within 24 hours. Using instructions, we added the certificate-encoded values to the EC2 server. After inserting the certificate encoded values, we checked using Trickle and discovered that the turn and stun ports were open. The information of the turn server was added to the signaling file [98], [99], [100].
5.2. Experimental setup
The system model of our proposed solution is presented in Fig. 10. We now briefly explain what our setup looks like. To do so, we present a scenario of the use case of the enhanced mobile application:
Figure 10.
System Model of Our Proposed Solution.
“Rahima, a teacher at an orphanage, is considered an intermediary who is interested in helping her orphanage children. She teaches about 8-10 children in the orphanage. She installs our app into her smartphone and registers as an intermediary. After registration, she logs in to the app and registers the students individually as patients. For each student, one token is produced uniquely via our system, and there is no chance of token duplication. She can see the auto-generated tokens for each patient in a list format, and later, she uses the tokens to make the orphan students log in as patients with no password. Rahima enters the registration info for the sick orphan, Mahbuba, Fatema and Atia. After all of them are registered, Rahima gets a table with a token generated for everyone. Now, on a specific day, Mahbuba is sick and needs to consult a doctor. Rahima logs into the system as an intermediary and can see the token for Mahbuba. Then, she enters the token for Mahbuba to log her in as a patient. After logging in to the system, Rahima clicks on the “Schedules Today” option to find the doctors. Among different schedules of doctors, she finds suitable schedule timing as per convenience and clicks on the schedule. Mahbuba now waits in the virtual doctor's chamber. Rahima clicks on the chamber option and waits for the doctor to call on behalf of Mahbuba.
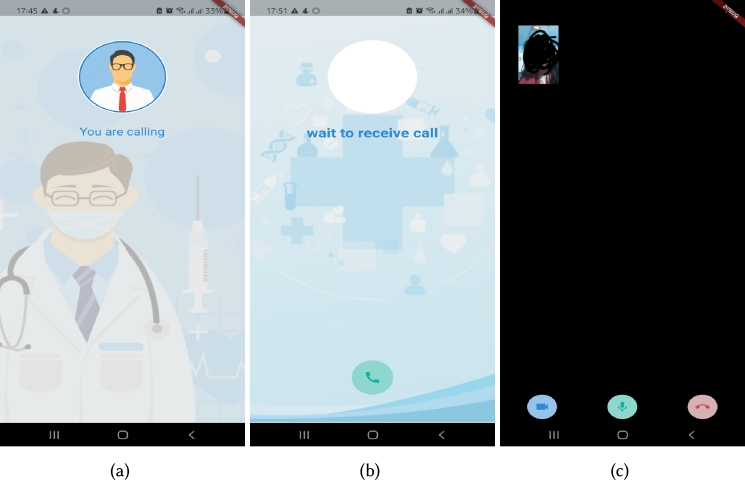
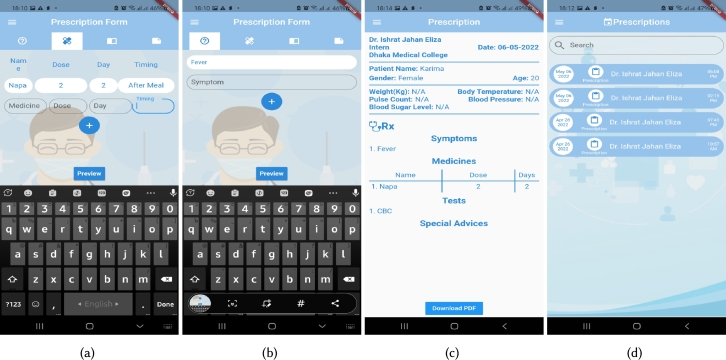
Dr. Disha registers as a verified doctor via the Doctor app and, using a mobile number, password logs in to the system. She enters into the “My Schedule” section where she can edit and create her new schedule. Therefore, she makes a new schedule for patients. After schedule settings, she comes back to the home page and clicks on the “My chamber” section of the preferred time at which she wants to give treatment. Instead, whenever Mahbuba waits in the chamber, automatically, an appointment is created in the back-end, and a serial number is also shown for the patient in the doctor app. Dr. Disha can observe her patients waiting in the chamber online, and according to the demonstrated serial, she clicks on the video call option to establish the call (Fig. 11(a)). Mahbuba sees on her end that Dr. Disha is calling and she receives the call (Fig. 11(b)). Dr. Disha can talk with the patient on the video call. The video call session from both ends is portrayed in Fig. 11(c). After the conversation ends, the doctor comes back to the chamber screen and found the “Add Prescription” section where she can add medicines with dosage, timing (before/after meal), medical tests (Fig. 12(a)), symptoms (Fig. 12(b)), and particular advice (Fig. 12(c)). Then after all of these are appropriately entered, she presses the save button (Fig. 12(c)).
Figure 11.
Different Interfaces of Enhanced ‘Shastho-sheba doctor’ App (a) Doctor Calling Patient, (b) Patient Receiving the Call, and (c) Established Video Call (identity of the user is not revealed so face in the video is marked as black).
Figure 12.
Different Interfaces of Enhanced ‘Shastho-sheba doctor and patient’ App (a) Doctor Adding Medicines, (b) Doctor Adding Symptoms, (c) Preview of Prescription, and (d) Prescription Page from Patient's End.
After the prescription is saved into the database successfully, on the patient's end, Mahbuba can find her prescription in the intermediary app from the patient's prescription module (Fig. 12(d)). Rahima downloads the prescription and passes the information about medications to Mahbuba.”
5.3. Piloting the app among the real users
After the Completion of the app, we intended to test the app services among the targeted users and wanted to know their feedback. We prepared an APK link to the app. Before sending it to the stakeholders, we tested the functionality of our devices. We emailed the APK link to the doctors and sent the APK to orphanage administrators via email, What's App.
We contacted the orphanages in Mirpur, Mohammadpur, and Azimpur, where we had already done our survey previously mentioned in Section 3.2.2. We went to the orphanages to make them understand how to install the app. They inquired about their doubts about different aspects of the app, such as login, video call, feedback, etc. We gave the OAs a demo on how to install and use the features of our app for the patients. The users pointed out some confusion about the features of the app. Based on these concerns, we again worked to update some of the features.
We first went to a female orphanage named ‘Jannatun Nisa’ on 25th April, 2022 to pilot our application. Our intermediary in the orphanage was the Arabic teacher who had installed our app on her phone through our assistance before. On the day of the health checkup by the doctor via online, the teacher did all the steps to get into the call for her orphan patient. At first, the patient was nervous and felt uneasy talking with the doctor. However, the intermediary was very helpful and made her feel comfortable. The patient described that she had been suffering from toothache problems for a couple of days. The doctor examined her condition through a video screen and also prescribed her some medicines via the e-prescription of the app.
Our second patient was a female child in the same orphanage. She had been suffering from coughing for long days. In fact, she had been diagnosed with pneumonia before. After hearing about her problems online, the doctor prescribed some medicines for her in e-prescription. The intermediary received each of the two prescriptions in the prescription section in the patient app. The Figs. 13(a), (b), and (c) portray the video call session between doctor and patient in the orphanages.
Figure 13.
Real-time Deployment of App in (a) Jannatun Nisa Female Orphanage, (b) Sir Salimullah Orphanage, and (c) Dhaka Ahsania Mission Female Orphanage.
On July 14, 2022, we went to ‘As Sunnah Hafizia Lillah Board Madrasa’ which is an orphanage situated in the Matikata area at Dhaka Cantonment. One of the orphanage students was sick, and one of our volunteer doctors gave him treatment via our system.
5.4. User feedback after piloting
We went to ‘Sir Salimullah Muslim Orphanage’ to see if they were able to use the app's services. We talked with students and one of the intermediaries, the nurse in the orphanage. She gave us her valuable feedback on using our app -
“Patient app is feasible and easy to use. The features are also easy to understand. If we get services through the app for our orphans, this would be really beneficial for us.”
One of our doctors, who is an intern doctor at Chittagong Medical College, gave her feedback on the basis of using the doctor app -
P13: “I have used the app to give treatment to orphans, and the features are quite easy to use. I felt comfortable while using this. However, the video call gets disrupted if the net connection is weak. It creates issues in the continuity of the video call.” Another doctor who used our app provided useful comments on the doctor app. He said,
P2: “I am unable to change the prescription when I attempt to do so. It is inconvenient, and you can include an amending option in the prescription.”
6. Discussion
In the aforementioned parts, we attempt to give readers a thorough understanding of the orphans living in orphanages, their means of survival, way of life, social connections, and availability of technology. We carefully explained how the chosen populations face substantial challenges when it comes to healthcare, given the study's focus on healthcare and factors like cost and a lack of knowledge and reading abilities. Additionally, we provided comprehensive findings from our rigorous field research and app deployment. We now discuss how the findings address the RQs in Section 1.3 and the significance, congruence, and differences between our findings and those of the previous studies.
6.1. Understanding the contexts of resource-constrained communities (RCCs) and intermediaries in the orphanages of Bangladesh
Our techno-social approach takes the idea of incorporating middlemen from the existing study ‘Dakter Bari’ [13] to help avail one of the basic human rights to the orphans. The intermediaries of the ‘Dakter Bari’ could not continue the service because they relocated. In our solution, to overcome this problem, we have introduced in-house intermediaries. In this regard, the service is continuous, and the risk of discontinuation due to relocation has decreased. Orphans can consult with doctors anytime, any day. This strengthens the existing service provided in the orphanages. On the other side, intermediaries are regarded as acting as a middleman in other developing nations to help the underprivileged groups become financially included [101], [102]. As we include intermediaries to assist orphans, which is one of the communities with resource constraints, our study is in line with these other studies in this area.
On the other hand, no research has been done on healthcare interventions for orphans in orphanages in Bangladesh. However, there are already studies on improved healthcare access for orphans and vulnerable children in other nations [103]. The orphans are already at risk of not receiving basic entitlements like health care. That was discovered in numerous South African nations by numerous investigations [28], [29], [31], [32]. Although Bangladesh is among the top ten countries with the highest number of cases of orphan children, there is little research about the socio-demographic status of orphans there [8], [27]. Despite the studies' findings that orphans are vulnerable, no more research has been done on how orphan administrators can support them by acting as a conduit for their rights. By bringing orphan administrators, such as teachers, nurses, and other professionals, into the loop, we contribute to this particular sector. According to our study, the majority of orphans reside in orphanages and lack access to quality healthcare. The administrators and teachers at the orphanage look after them and fulfill their duties; in certain instances, they even take on the role of guardians. The orphanage teachers gave their consent to let their phones be used on behalf of students while receiving online treatment from doctors. This notion of volunteerism, referring to work enacted in service of others for doing good [104], provides an explanation for the helping and philanthropic intent of our intermediary partners [105].
The findings from the field study with orphans shed light on the current state of healthcare services available to orphans in orphanages in Bangladesh, highlighting the potential benefits of intermediation, given the students' comfort with this approach. This comprehensive understanding helps address RQ1. The findings from the intermediary field study strongly advocate the provision of continuous and cost-free healthcare services in resource-constrained settings, particularly for orphans who are our representatives of resource-constrained communities. Notably, the orphans' comfort and trust in Orphanage Administrators (OAs), who maintain a continuous presence, lend further credence to the pivotal role of these administrators as intermediaries in delivering healthcare services to the orphans. This valuable insight effectively addresses RQ2. This natural affinity and proximity make the presence of OAs as intermediaries indispensable in facilitating healthcare services within orphanages.
6.2. Tailoring a techno-social solution to fit the context of orphanages in Bangladesh
Our system relies heavily on simplicity. In our study, we focus on orphans living in orphanages who lack access to basic rights, technology interventions, and in-house intermediates who aren't financially stable. For the benefit of the care of the orphan students, the orphanage administrator has their own tasks to complete. We design our system with this in mind, especially since the administrators are in charge of using it and have some experience using technology compared to the orphans, who have virtually no experience with it. Thus, we have designed our system in a way that it can be used easily. Compared to what Sambasivan et al. [60] and Parikh & Ghosh [61] suggested, this is radically different. They recommended designing systems with dual-user phenomena in mind for best performance. However, the intermediation intended to give recipients access to technology is the main subject of their investigations. Contrarily, we only want healthcare services to be made available to the targeted group through volunteerism from internal intermediaries utilizing the tools they already utilize. Volunteers must be available in order for technology to be mediated through volunteerism. By placing our system where orphanages have less access to resources and where the administrator is more likely to support them, we boost availability. The services they receive from the doctors will help them to prevent diseases in the future as the prescription will always be in the app, even though the orphans may prefer to go to nearby government hospitals for chronic conditions like accident operations or there are no doctors available. On the other hand, based on the results of the previous study [106], we can confirm that this idea of e-prescription will also assist in the treatment of common illnesses at any time for anyone. The potential for collaborative technology and social assistance in many circumstances has been demonstrated by CSCW and HCI researchers who have examined the techno-social intervention in health crises [107], [108]. Our techno-social solution fundamentally supports these sorts of interventions in the context of orphans in Bangladesh.
Our findings from the doctor survey indicate that doctors are genuinely enthusiastic about contributing to community welfare. However, RCCs as direct users of online systems might not be effective as they have no access to devices. Consequently, adding a layer of intermediation is yet an area to be explored in the shake of sustainability. The online model is deemed more suitable for RCCs, as doctors may encounter hurdles during fieldwork, and that possibly lead to discontinuity in the future. These findings answer our RQ2. Our approach to enhancing the mobile app to add a layer of intermediation lets us dive into RQ3, and the comments regarding the system feature drive us to the potential future works.
6.3. Comparisons with traditional NGO-based healthcare services
In the context of healthcare services in Bangladesh, the presence of NGO-based initiatives designed to serve resource-constrained communities, both in rural and urban areas, is well-documented. However, these services often face accessibility challenges, primarily due to geographical distance [109]. Additionally, studies suggest that the consistency of these services can be a concern. In contrast, our research places a specific emphasis on the aspect of continuity. By offering a free, online-based system facilitated through relevant intermediaries, our approach addresses the issue of inaccessibility more effectively. It's worth noting that BRAC, being the county's leading international developing organization, has a predominant focus on women and children, mainly through free programs related to maternal, neonatal, and child health [11]. While there may be some overlap with our objectives, as we also consider child health, our study takes a broader approach by concentrating on the healthcare of orphans residing in Bangladesh's orphanages. This encompasses both male and female orphans. To the best of our knowledge, organizations like Grameen Healthcare Services LTD. (GHS) have endeavored to provide quality healthcare services at affordable costs, with a specific focus on rural areas. However, GHS primarily emphasizes eye care and eye health programs across four districts in the country. What distinguishes our study from many of the existing affordable healthcare models is our exclusive techno-social design to provide free healthcare services to orphaned individuals residing in orphanages.
6.4. Contribution to HCI for resource-constrained communities
The communities with little resources make up a growing section of our society. Since they cannot afford expensive therapy, they hardly ever receive proper healthcare when they need it. Bangladesh had a number of lengthy lockdowns during COVID-19, which brought about a halt to people's lives. People could already sense the need for online medical services at that time, and they quickly gained attention. Online healthcare is accessible to those with simple access to technology and devices. Contrarily, the complexity of the lockdown was greater for those with restricted resources and restrictions. Our suggested system helps to address such issues. Various research has attempted to help the destitute, homeless, and refugee groups around the world using technology-based solutions [39], [40], [41], [46], [48]. In leveraging technology to deliver healthcare, our study complements those studies. Research on HCI-based Systems that leverage mobile technology to help communities with limited resources live better has previously been done in this area [46], [49], [52], [53], [54], [110], [111]. In the case of orphans in orphanages, our smartphone app substantially contributes to the current era of the emergence of mobile technology penetration in their support. Additionally, there have been numerous studies on the use of technology in low-resource communities [44], [57], [112], including ‘ClickHealth’ [5], ‘GiveMed’ [6], ‘HealthShare’ [7]. Other telemedicine services to deliver healthcare to underserved communities in various developing and industrialized nations [56]. Our study contributes to this field because the orphans in our system may obtain healthcare quickly, easily, and effectively because of our system's mHealth characteristics. Our techno-social solution is open to voluntary contributions from doctors everywhere in the world. We created our online healthcare software in a simple manner because the consumers are pretty ordinary individuals like orphanage teachers, nurses, etc. HCI has broadened from its original emphasis on individual and general user behavior to include social and organizational computing, accessibility for the elderly, physically and cognitively disabled, and for everyone, as well as for the broadest range of human experiences and activities, known as the three basic user focus. Our research on adapting systems for user needs and comfort adds to the three user emphasis areas in the field of HCI.
6.5. Challenges and limitations
In both fieldwork and app-level enhancement, we confronted numerous challenges and limitations. For starters, we were unable to do the field study for a long time due to the lockdown and rising COVID-19 cases in Bangladesh from May 2021 to August 2021. As a result, we had to start surveying health professionals online because they could participate in an online survey. However, resource-strapped communities are unable to participate in online surveys. Therefore, we had to wait a long time for the COVID-19 situation to improve. Secondly, we perform our research in a few specific places in Dhaka. We found it simple to conduct our study in Dhaka primarily because we live in the city. Furthermore, this type of research necessitates extensive fieldwork, and for an extended period of time, it was only us - the two girls who went for the field survey; we found it very difficult to conduct a rapid field study by ourselves due to other social concerns in our society and culture. Later, we sought assistance from other male classmates, and thus, the other authors were included in the study. Thirdly, we found it challenging to locate probable intermediaries for the beggar communities based on the ‘Daktar Bari’ survey results due to the relocation of their shops. While providing the demographic information in the first place, the intermediaries were excessively concerned about our identification. However, after some informal conversation, they agreed to cooperate with us.
The majority of the issues we encountered when modifying the application are linked to the turn server setup. When the callee and caller were on two distinct network connections, the video calling module did not perform correctly. We fixed the problem by setting up our own turn server on AWS, as discussed before. The constraint here is that the server is the cheapest on AWS. Our backend server is hosted on Heroku, which is a free service as well. If we had adequate financial assistance, we could raise the server's capacity. The feature reduction and simplification of the old ‘Shastho-sheba’ app was a tough challenge. We had to rebuild various previous modules because it was not working effectively to make them operational. We had to debug the application to make it functional on an actual Android device, and we had to make it compatible with any Android version.
Another drawback of our app is that discussing taboo topics like menstrual difficulties with doctors might still be awkward using this app method. The children would not address intermediaries, which requires more development. We acknowledge that emergency cases like operations can not be done using this service, but doctors can still suggest if emergency treatment is needed via our app. Another limitation is that this study did not include other sections of the population. The remaining portions differ significantly from the circumstances of our chosen places. Furthermore, if we travel to another region of the world, there may be considerable differences in technology, socio-cultural factors, religious beliefs, and other practical concerns that may limit the applicability of our solution. As a result, if we use our solution in any other scenario, we must evaluate, realize, and solve these contextual factors.
7. Conclusion and future research scope
Many third-world countries, such as Bangladesh, have vast populations of resource-constrained communities that are severely lacking in basic needs, such as healthcare. The limited existence of continuously available services meant to deliver healthcare to resource-constrained populations is one of the key reasons for being deprived of healthcare services. Due to a lack of resources, awareness, and the vast distance from free service locations, the orphans in orphanages in Bangladesh are unable to access healthcare specialists when they are necessary. In this study, we provide a new approach to bridge the gap between orphans and healthcare professionals in order to obtain relevant healthcare services, with Bangladesh (primarily focusing on its capital, Dhaka) as our research context. Our technology recognizes and considers practical circumstances and responds to them in a consistent manner, allowing different stakeholders in the envisioned healthcare service ecosystem to collaborate. To do so, we propose a techno-social method in which healthcare services are delivered to orphans via an online platform over the Internet with the assistance of competent intermediaries. It's worth noting that we don't offer the communities any direct technology-based solutions because they're generally disconnected from technology (smartphones or the Internet). Rather, we reveal relevant intermediates who do have the needed technology penetration to operate a smartphone application. This intermediary is mostly in touch with the orphans, who are in direct contact with orphanage administrators and teachers virtually 24/7. We design and modify the application, deploy it, and do post-deployment outreach to its stakeholders. We have done a trial of the application at one orphanage so far, and the orphans have benefited from it. In addition to providing contributions to HCI theory, we are continuously working on revealing numerous new findings and demonstrating real-world implications. Nonetheless, our approach allows us to provide better healthcare to a large disenfranchised community on the way to reaching the SDGs and the humanitarian growth of our civilization. In the future, we plan to use the system in two ways. We will work to expand our operations beyond Dhaka first. We intend to spread our online healthcare service outside Dhaka's urban areas and to the rural areas. We have already contacted some doctors living in different countries to scale the usage of our app so that orphans and the relevant communities can get healthcare services in a continuous manner. If our project is funded, we intend to migrate our app server to a more long-term cloud hosting solution. We plan to perform more testing of our app among intermediaries and patients in order to gather more feedback and execute design iteration and improvements in response to user feedback. In fact, in addition to Bangladesh, we plan to incorporate other underprivileged countries in our online healthcare service. In terms of technology, socio-cultures, adoption, and other subjects, we would like to reach out to other countries. Finally, our future work will include attempting to forge partnerships with established private companies and government agencies to build the system from the bottom up while also considering the current condition of the system's security, privacy, and trust components.
Originality
The authors state that the information presented in this research work is entirely original and has not been previously published, nor is it currently under consideration for publication elsewhere, either in full or in part. We have taken the necessary steps to acknowledge and cite all relevant published work throughout the paper. We ensured the integrity of the research by following ethical standards.
Declaration of generative AI and AI-assisted technologies in the writing process
During the preparation of this work the author(s) used ChatGPT in order to rephrase some of the paragraphs to improve readability and language. After using this tool/service, the author(s) reviewed and edited the content as needed and take(s) full responsibility for the content of the publication.
CRediT authorship contribution statement
Ishrat Jahan Eliza: Writing – review & editing, Writing – original draft, Visualization, Software, Project administration, Methodology, Formal analysis, Data curation, Conceptualization. Mobasshira Akter Urmi: Writing – review & editing, Writing – original draft, Software, Project administration, Methodology, Formal analysis, Data curation, Conceptualization. Md Tousif Tanjim Anan: Writing – review & editing, Writing – original draft. Md Tanveer Hossain Munim: Writing – review & editing, Writing – original draft, Methodology, Formal analysis. Fattah-Zul-Ikram Galib: Writing – review & editing. A.B.M. Alim Al Islam: Writing – review & editing, Writing – original draft, Supervision, Project administration, Investigation, Conceptualization.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary material related to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e23100.
Appendix A. Supplementary material
The following is the Supplementary material related to this article.
Survey on orphans about online healthcare support for the orphans.
Survey over administrators of orphanages about online healthcare support for orphans.
Survey on voluntary participation in online healthcare consultation for resource-constrained communities (RCCs).
Data availability
The data that has been used in this study is confidential. Due to the sensitive nature of the research, the supporting data is not publicly available.
References
- 1.Kamruzzaman Md, Hakim Md. Social, biology and economic life of children links on street-begging in Bangladesh: a cross-cultural multivariate analysis. Math. Lett. 01 2017;3:107–114. [Google Scholar]
- 2.Khan Naushad, Fahad Shah. Social Science Research Network; 02 2020. Begging negative impact on the world community. [Google Scholar]
- 3.Kavak Hafize Zehra. 07 2014. Report on world's orphans. Informing humanitarians worldwide 24/7. [Google Scholar]
- 4.Cottin Raphael. 2018. Free health care for the poor: a good way to achieve universal health coverage? Evidence from Morocco. [Google Scholar]
- 5.Song Erin, Maheshwari Puja, Lewis Daniel, Figueira Silvia. ACM DEV '16. Association for Computing Machinery; New York, NY, USA: 2016. ClickHealth, an app to provide info on healthcare to the homeless. [Google Scholar]
- 6.Islam Muhammad Nazrul, Zavin Ashratuz, Srabanti Sanjana, Ferdous Chowdhury Nawrin, Suha Sayma Alam, Afroze Lameya, Shawon Nafin, Refath Naznin Sultana. 2017 IEEE Region 10 Humanitarian Technology Conference (R10-HTC) 2017. GiveMed: a webportal for medicine distribution among poverty-stricken people; pp. 294–299. [Google Scholar]
- 7.Pierce James J., Engelhardt Ashley E., Yim Jung Youn. Homeless HealthShare: connecting health professionals and the homeless. CHI '08 Extended Abstracts on Human Factors in Computing Systems; CHI EA '08; New York, NY, USA: Association for Computing Machinery; 2008. pp. 3861–3866. [Google Scholar]
- 8.Roy Rana, Chowdhury Mitu, Sarker Rupa, Yasmin Khadeza, Sarker Tanwne. Education and health status of child beggars in Sylhet city. 10 2019;4:58–66. [Google Scholar]
- 9.Kumar Anant, Schofield Toni. Orphan and vulnerable children - health policy interventions in India. J. Health Dev. 12 2008;4:21–32. [Google Scholar]
- 10.Uddin J., Koehlmoos T.P., Saha N.C. Strategies for providing healthcare services to street-dwellers in Dhaka city: evidence from an operations research. Health Res. Policy Syst. 06 2012;10 doi: 10.1186/1478-4505-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marcil L., Afsana K., Perry H.B. First steps in initiating an effective maternal, neonatal, and child health program in urban slums: the BRAC Manoshi project's experience with community engagement, social mapping, and census taking in Bangladesh. J. Urban Health. 2016;93(01) doi: 10.1007/s11524-016-0026-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmed Toufiq, Shirahada Kunio. Toward a sustainable healthcare service system in a limited resource context: case study of Bangladesh rural advancement committee's healthcare system. Int. J. Healthc. Manag. 2017 [Google Scholar]
- 13.Rahman Md. Aminur, Rashed Rayhan, Purabi Sharmin Akther, Ulfat Noshin, Chellappan Sriram, Alim Al Islam A.B.M. Dakter Bari: introducing intermediary to ensure healthcare services to extremely impoverished people. Proc. ACM Hum.-Comput. Interact. apr 2021;5(CSCW1) [Google Scholar]
- 14.Waqar Hassan Khan, Md Al Imran, Ahmed Nafis Fuad, Mohammed Latif Siddiq, A.B.M. Alim Al Islam, Shashthosheba dissecting perception of Bangladeshi people towards telemedicine apps through the lens of features of the apps, 2022.
- 15.Jelili Musibau Omoakin. Street-begging in cities: unveiling the global situations and issues to be addressed. 11 2013;1 [Google Scholar]
- 16.Sultana Dr, Alam Zaid. Analysis of socio-economic profile of beggars in Amroha city: a case study. Int. J. Res. Soc. Sci. 06 2018;8:667–684. [Google Scholar]
- 17.Salami Kabiru, Olugbayo Aishat. Health-seeking behavior of migrant beggars in Ibadan, southwestern Nigeria. Health. 01 2013;05:792–804. [Google Scholar]
- 18.Alam Md. Zahanggir, Rahman Md, Firoz Md. Water supply and sanitation facilities in urban slums: a case study of Rajshahi city corporation slums. Am. J. Civ. Eng. Archit. 01 2013;1:1–6. [Google Scholar]
- 19.Afsana Kaosar, Wahid Syed. Health care for poor people in the urban slums of Bangladesh. Lancet. 11 2013;382 doi: 10.1016/S0140-6736(13)62295-3. [DOI] [PubMed] [Google Scholar]
- 20.Rahman Mohammad, Helal Abdullah. Slum women and their socio-economic characteristics: a study in Dhaka city. Int. J. Humanit. Soc. Sci. 02 2017;12:1–15. [Google Scholar]
- 21.Bhatia Shushum, Dranyi Tsegyal, Rowley Derrick. A social and demographic study of Tibetan refugees in India. Soc. Sci. Med. (1982) 03 2002;54:411–422. doi: 10.1016/s0277-9536(01)00040-5. [DOI] [PubMed] [Google Scholar]
- 22.Krubiner Carleigh B., Salmon Marla, Synowiec Christina, Lagomarsino Gina. Investing in nursing and midwifery enterprise: empowering women and strengthening health systems—a landscaping study of innovations in low- and middle-income countries. Nursing Outlook. 2016;64(01) doi: 10.1016/j.outlook.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Taderera Bernard Hope, Hendricks Stephen James Heinrich, Pillay Yogan. Human resource for health policy interventions towards health sector reform in a Zimbabwean peri-urban community: a decision space approach. Int. J. Healthc. Manag. 2018;11(4):289–297. [Google Scholar]
- 24.Taderera Bernard Hope. Community health volunteers and their role in health system strengthening in peri-urban areas: a qualitative study of Epworth, Zimbabwe. Int. J. Healthc. Manag. 2021;14(2):349–357. [Google Scholar]
- 25.Frankish C.J., Hwang S.W., Quantz D. Homelessness and health in Canada: research lessons and priorities. Can. J. Public Health. 2005;96:23–29. doi: 10.1007/BF03403700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheung A.M., Hwang S.W. Risk of death among homeless women: a cohort study and review of the literature. Can. Med. Assoc. J. 2004;170(8):1243–1247. doi: 10.1503/cmaj.1031167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huq A.K. Obidul, Chowdhury Tanni, Roy Provat, Haque K., Hossain M., Huq Dr. Health care facilities and nutritional status of orphans residing in selected orphanage in capital city of Bangladesh. Int. J. Curr. Microbiol. Appl. Sci. 01 2013;2:118–125. [Google Scholar]
- 28.Schenk Katie, Michaelis Annie, Sapiano Tobey, Brown Lisanne, Weiss Ellen. Improving the lives of vulnerable children: implications of horizons research among orphans and other children affected by AIDS. Public Health Rep. (Washington, D.C.: 1974) 03 2010;125:325–336. doi: 10.1177/003335491012500223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Biemba Godfrey, Njoka John, Simon Jonathon, Costello Jill, Beard Jen, Brooks Bram. Center for Global Health and Development; 08 2009. Kenya research situation analysis on orphans and other vulnerable children. [Google Scholar]
- 30.Goodman Michael, Kaberia Reegan, Morgan Robert, Keiser Philip. Health and livelihood outcomes associated with participation in a community-based empowerment program for orphan families in semirural Kenya: a cross-sectional study. Vulnerable Child. Youth Stud. 07 2014;9:365–376. [Google Scholar]
- 31.Bryant Malcolm, Beard Jennifer, Sabin Lora, Brooks Mohamad, Scott Nancy, Larson Bruce, Biemba Godfrey, Miller Candace, Simon Jonathon. PEPFAR's support for orphans and vulnerable children: some beneficial effects, but too little data, and programs spread thin. Health Aff. (Project Hope) 07 2012;31:1508–1518. doi: 10.1377/hlthaff.2012.0230. [DOI] [PubMed] [Google Scholar]
- 32.Bamgboye Elijah, Odusote Temitayo, Olusanmi Iyabode, Nwosu Joanna, Phillips Ononye Tessie, Akpa Onoja, Yusuf Oyindamola, Adebowale Ayo, Todowede Olamide, Ladipo Oladapo. Vulnerable children and youth studies school absenteeism among orphans and vulnerable children in Lagos State, Nigeria: a situational analysis school absenteeism among orphans and vulnerable children in Lagos State, Nigeria: a situational analysis. Vulnerable Child. Youth Stud. 04 2017 [Google Scholar]
- 33.Tagurum Yetunde, Chirdan Oluwabunmi, Bello Danjuma, Afolaranmi Tolulope, Hassan Zuwairai, Iyaji A., Idoko Lucy. Situational analysis of orphans and vulnerable children in urban and rural communities of plateau state. Ann. Afr. Med. 01 2015;14:18–24. doi: 10.4103/1596-3519.148714. [DOI] [PubMed] [Google Scholar]
- 34.Chima Victor. Socio-demographic determinants of health support services among orphans and vulnerable children in Nigeria. J. Public Health Epidemiol. 2018;10(5):165–170. [Google Scholar]
- 35.Aspaas Helen Ruth. Aids and orphans in Uganda: geographical and gender interpretations of household resources. Soc. Sci. J. 1999;36(2):201–226. [Google Scholar]
- 36.Garzotto Franca, Schelhowe Heidi. Marginalized young people: inclusion through ICT. Proceedings of the 7th International Conference on Interaction Design and Children; IDC '08; New York, NY, USA: Association for Computing Machinery; 2008. pp. 101–104. [Google Scholar]
- 37.Wyche Susan P., Oreglia Elisa, Ames Morgan G., Hoadley Christopher, Johri Aditya, Sengers Phoebe, Steinfield Charles. Learning from marginalized users: reciprocity in HCI4D. Proceedings of the ACM 2012 Conference on Computer Supported Cooperative Work Companion; CSCW '12; New York, NY, USA: Association for Computing Machinery; 2012. pp. 27–28. [Google Scholar]
- 38.Almohamed Asam, Vyas Dhaval. DIS '16 Companion. Association for Computing Machinery; New York, NY, USA: 2016. Designing for the marginalized: a step towards understanding the lives of refugees and asylum seekers; pp. 165–168. [Google Scholar]
- 39.Shahid Farhana, Rahman Wasifur, Islam Anika Binte, Paul Nipi, Khan Nabila, Rahman Mohammad Saifur, Haque Md Munirul, Alim Al Islam A.B.M. Two tell-tale perspectives of PTSD: neurobiological abnormalities and Bayesian regulatory network of the underlying disorder in a refugee context. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. sep 2019;3(3) [Google Scholar]
- 40.Shahid Farhana, Rahman Wasifur, Rahman M. Saifur, Purabi Sharmin Akther, Seddiqa Ayesha, Mostakim Moin, Feroz Farhan, Soron Tanjir Rashid, Hossain Fahmida, Khan Nabila, Islam Anika Binte, Paul Nipi, Hoque Ehsan, Alim Al Islam A.B.M. Leveraging free-hand sketches for potential screening of PTSD. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. sep 2020;4(3) [Google Scholar]
- 41.Woelfer J.P., Hendry D.G. Designing ubiquitous information systems for a community of homeless young people: precaution and a way forward. Pers. Ubiquitous Comput. 2011;15:565–573. [Google Scholar]
- 42.Woelfer Jill Palzkill, Hendry David G. Homeless young people and living with personal digital artifacts. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; CHI '11; New York, NY, USA: Association for Computing Machinery; 2011. pp. 1697–1706. [Google Scholar]
- 43.Woelfer Jill Palzkill, Iverson Amy, Hendry David G., Friedman Batya, Gill Brian T. Improving the safety of homeless young people with mobile phones: values, form and function. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; CHI '11; New York, NY, USA: Association for Computing Machinery; 2011. pp. 1707–1716. [Google Scholar]
- 44.Le Dantec Christopher A. Life at the margins: assessing the role of technology for the urban homeless. Interactions. sep 2008;15(5):24–27. [Google Scholar]
- 45.Le Dantec Christopher A., Farrell Robert G., Christensen Jim E., Bailey Mark, Ellis Jason B., Kellogg Wendy A., Edwards W. Keith. Publics in practice: ubiquitous computing at a shelter for homeless mothers. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; CHI '11; New York, NY, USA: Association for Computing Machinery; 2011. pp. 1687–1696. [Google Scholar]
- 46.Mohan Nisha, Sarma Abhraneel, Toyama Kentaro. Food-availability SMS system for U.S. homeless communities. Proceedings of the Tenth International Conference on Information and Communication Technologies and Development; ICTD '19; New York, NY, USA: Association for Computing Machinery; 2019. [Google Scholar]
- 47.Budree Adheesh, Chacko Sheril, Fourie Louis Ch. 2017 7th International Conference on Cloud Computing, Data Science Engineering - Confluence. IEEE Xplore; 2017. Implementing free Wi-Fi in underprivileged communities: A case study of Project Isizwe; pp. 687–692. [Google Scholar]
- 48.Ishmam Alvi Md., Sabique Md. Raihan, Alim Al Islam A.B.M. 2017 IEEE Region 10 Humanitarian Technology Conference (R10-HTC) 2017. BONDHON: an integrated organization hub for facilitating street children of Bangladesh; pp. 769–772. [Google Scholar]
- 49.Samuel M., Taylor J., Winschiers-Theophilus H., Nieminen M. Proceedings of the 8th International Conference on Communities and Technologies. Association for Computing Machinery; New York, NY, USA: 2017. Improving the flow of livelihood information among unemployed youth in an informal settlement of Windhoek, Namibia; pp. 256–265. [Google Scholar]
- 50.Medhi Indrani, Patnaik Somani, Brunskill Emma, Gautama S.N. Nagasena, Thies William, Toyama Kentaro. Designing mobile interfaces for novice and low-literacy users. ACM Trans. Comput.-Hum. Interact. may 2011;18(1) [Google Scholar]
- 51.Raza Agha Ali, Saleem Bilal, Randhawa Shan, Tariq Zain, Athar Awais, Saif Umar, Rosenfeld Roni. Baang: a viral speech-based social platform for under-connected populations. Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems; CHI '18; New York, NY, USA: Association for Computing Machinery; 2018. pp. 1–12. [Google Scholar]
- 52.Vashistha Aditya, Brady Erin, Thies William, Cutrell Edward. ACM DEV-5 '14. Association for Computing Machinery; New York, NY, USA: 2014. Educational content creation and sharing by low-income visually impaired people in India; pp. 63–72. [Google Scholar]
- 53.Raza Agha Ali, Ul Haq Farhan, Tariq Zain, Pervaiz Mansoor, Razaq Samia, Saif Umar, Rosenfeld Roni. CHI '13. Association for Computing Machinery; New York, NY, USA: 2013. Job opportunities through entertainment: virally spread speech-based services for low-literate users; pp. 2803–2812. [Google Scholar]
- 54.Jain Mohit, Kumar Pratyush, Bhansali Ishita, Liao Q. Vera, Truong Khai, Patel Shwetak. FarmChat: a conversational agent to answer farmer queries. dec 2018;2(4) [Google Scholar]
- 55.Riaz Waleed, Durrani Haris, Shahid Suleman, Raza Agha Ali. ICT intervention for agriculture development: designing an IVR system for farmers in Pakistan. Proceedings of the Ninth International Conference on Information and Communication Technologies and Development; ICTD '17; New York, NY, USA: Association for Computing Machinery; 2017. [Google Scholar]
- 56.Brauchli K. University of Basel, Faculty of Science; 2006. Telemedicine for Improving Access to Health Care in Resource-Constrained Areas: from Individual Diagnosis to Strengthening Health Systems. [Google Scholar]
- 57.Asgary R., Sckell B., Alcabes A., Naderi R., Adongo P., Ogedegbe G. Perceptions, attitudes, and experience regarding mHealth among homeless persons in New York city shelters. J. Health Commun. 2015;20(12):1473–1480. doi: 10.1080/10810730.2015.1033117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Islam Muhammad Nazrul, Inan Toki Tahmid. Exploring the fundamental factors of digital inequality in Bangladesh. SAGE Open. 2021;11(2) [Google Scholar]
- 59.Okeke Fabian, Wasunna Beatrice, Amulele Mercy, Holeman Isaac, Dell Nicola. Including the voice of care recipients in community health feedback loops in rural Kenya. Proc. ACM Hum.-Comput. Interact. nov 2019;3(CSCW) [Google Scholar]
- 60.Sambasivan Nithya, Smyth Thomas. The human infrastructure of ICTD. Proceedings of the 4th ACM/IEEE International Conference on Information and Communication Technologies and Development; ICTD '10; New York, NY, USA: Association for Computing Machinery; 2010. [Google Scholar]
- 61.Parikh J.S., Ghosh Kaushik. Understanding and designing for intermediated information tasks in India. IEEE Pervasive Comput. 2006;5(2):32–39. [Google Scholar]
- 62.Chen Zhilong, Cao Hancheng, Xu Fengli, Cheng Mengjie, Wang Tao, Li Yong. Understanding the role of intermediaries in online social e-commerce: an exploratory study of Beidian. Proc. ACM Hum.-Comput. Interact. oct 2020;4(CSCW2) [Google Scholar]
- 63.Medhi-Thies Indrani, Ferreira Pedro, Gupta Nakull, O'Neill Jacki, Cutrell Edward. CSCW '15. Association for Computing Machinery; New York, NY, USA: 2015. Krishipustak: a social networking system for low-literate farmers; pp. 1670–1681. [Google Scholar]
- 64.Mehra Apurv, Muralidhar Srihari, Satija Sambhav, Dhareshwar Anupama, O'Neill Jacki. CHI '18. Association for Computing Machinery; New York, NY, USA: 2018. Prayana: intermediated financial management in resource-constrained settings; pp. 1–13. [Google Scholar]
- 65.Mehra Apurv, Satija Sambhav, O'Neill Jacki. ICTD '17. Association for Computing Machinery; New York, NY, USA: 2017. Prayana: a journey towards financial inclusion. [Google Scholar]
- 66.Ghosh Ishita. Contextualizing intermediated use in the developing world: findings from India & Ghana. Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems; CHI '16; New York, NY, USA: Association for Computing Machinery; 2016. pp. 355–359. [Google Scholar]
- 67.Hersberger Julie. Everyday information needs and information sources of homeless parents. New Rev. Inf. Behav. Res. 01 2001;2:119–134. [Google Scholar]
- 68.Hersberger Julie. Are the economically poor information poor? Does the digital divide affect the homeless and access to information? Can. J. Inf. Libr. Sci. 09 2002;27:44–63. [Google Scholar]
- 69.Dombrowski Lynn, Brubaker Jed R., Hirano Sen H., Mazmanian Melissa, Hayes Gillian R. It takes a network to get dinner: designing location-based systems to address local food needs. Proceedings of the 2013 ACM International Joint Conference on Pervasive and Ubiquitous Computing; UbiComp '13; New York, NY, USA: Association for Computing Machinery; 2013. pp. 519–528. [Google Scholar]
- 70.Dombrowski Lynn, Hayes Gillian R., Mazmanian Melissa, Voida Amy. E-government intermediaries and the challenges of access and trust. ACM Trans. Comput.-Hum. Interact. feb 2014;21(2) [Google Scholar]
- 71.Dombrowski Lynn, Voida Amy, Hayes Gillian R., Mazmanian Melissa. CHI '12. Association for Computing Machinery; New York, NY, USA: 2012. The labor practices of service mediation: a study of the work practices of food assistance outreach; pp. 1977–1986. [Google Scholar]
- 72.Ehrlich Kate, Cash Debra. The invisible world of intermediaries: a cautionary tale. Comput. Support. Coop. Work. 1999;8(1–2):147–167. [Google Scholar]
- 73.Ramirez Fred. Technology and parental involvement. Clear. House: J. Educ. Strategies Issues Ideas. 2001;75(1):30–31. [Google Scholar]
- 74.Paula England, Merging theories of care work, 2005 [last accessed December 12, 2021].
- 75.Ramachandran Divya, Canny John, Das Prabhu Dutta, Cutrell Edward. Mobile-izing health workers in rural India. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; CHI '10; New York, NY, USA: Association for Computing Machinery; 2010. pp. 1889–1898. [Google Scholar]
- 76.Ramachandran Divya, Goswami Vivek, Canny John. Research and reality: using mobile messages to promote maternal health in rural India. Proceedings of the 4th ACM/IEEE International Conference on Information and Communication Technologies and Development; ICTD '10; New York, NY, USA: Association for Computing Machinery; 2010. [Google Scholar]
- 77.Molapo Maletsabisa, Marsden Gary. Software support for creating digital health training materials in the field. Proceedings of the Sixth International Conference on Information and Communication Technologies and Development: Full Papers - Volume 1; ICTD '13; New York, NY, USA: Association for Computing Machinery; 2013. pp. 205–214. [Google Scholar]
- 78.Katule Ntwa, Densmore Melissa, Rivett Ulrike. Leveraging intermediated interactions to support utilization of persuasive personal health informatics. Proceedings of the Eighth International Conference on Information and Communication Technologies and Development; ICTD '16; New York, NY, USA: Association for Computing Machinery; 2016. [Google Scholar]
- 79.Albers Albert, Bursac Nikola, Maul Ludwig, Mair Marius. The role of in-house intermediaries in innovation management – optimization of technology transfer processes from cross-industry. 24th CIRP Design ConferenceProc. CIRP. 2014;21:485–490. [Google Scholar]
- 80.DeRenzi Brian, Dell Nicola, Wacksman Jeremy, Lee Scott, Lesh Neal. Supporting community health workers in India through voice- and web-based feedback. Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems; CHI '17; New York, NY, USA: Association for Computing Machinery; 2017. pp. 2770–2781. [Google Scholar]
- 81.Pace P., Aloi G., Caliciuri G., Gravina R., Savaglio C., Fortino G., Ibanez-Sanchez G., Fides-Valero A., Bayo-Monton J., Uberti M., Corona M., Bernini L., Gulino M., Costa A., De Luca I., Mortara M. 2019 IEEE 5th World Forum on Internet of Things (WF-IoT) 2019. Inter-health: an interoperable IoT solution for active and assisted living healthcare services; pp. 81–86. [Google Scholar]
- 82.Patil Dhanraj A. Mobile for health (mHealth) in developing countries: application of 4 Ps of social marketing. J. Health Inform. Dev. Ctries. Dec. 2011;5(2) [Google Scholar]
- 83.Fiordelli M., Diviani N., Schulz P.J. Mapping mHealth research: a decade of evolution. 2013;15 doi: 10.2196/jmir.2430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zapata Belén, Fernández-Alemán José, Idri Ali, Toval Ambrosio. Empirical studies on usability of mHealth apps: a systematic literature review. J. Med. Syst. 02 2015;39:182. doi: 10.1007/s10916-014-0182-2. [DOI] [PubMed] [Google Scholar]
- 85.Muhambe Titus Mukisa, Daniel Orwa Ochieng, Peter Wagacha Waiganjo, Evaluating the sustainability of mhealth systems in developing countries: the knowledge gap, 2017.
- 86.Hoque Md. Rakibul, Sorwar Golam. Factors influencing mHealth acceptance among elderly people in Bangladesh. 2016. arXiv:1606.00874 [abs]
- 87.Goodman Leo A. Snowball sampling. Ann. Math. Stat. 1961;32(1):148–170. [Google Scholar]
- 88.Guest Greg, Bunce Arwen, Johnson Laura. How many interviews are enough?: an experiment with data saturation and variability. Field Methods. 2006;18(1):59–82. [Google Scholar]
- 89.Onwuegbuzie Anthony, Collins Kathleen M.T. A typology of mixed methods sampling designs in social science research. Qual. Rep. 06 2007;12:281–316. [Google Scholar]
- 90.Pal Dinesh Kumar, Joshi Ankur. Likert scale: explored and explained. 2015;07:396–403. [Google Scholar]
- 91.Kraig Finstad, Response interpolation and scale sensitivity: evidence against 5-point scales, 2010, pp. 104–110.
- 92.Elo Satu, Kyngäs Helvi. The qualitative content analysis process. J. Adv. Nurs. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 93.Krippendorff Klaus. Sage Publications; 2018. Content Analysis: An Introduction to Its Methodology. [Google Scholar]
- 94.Vrij Aldert. Criteria-based content analysis: a qualitative review of the first 37 studies. Psychol. Public Policy Law. 2005;11(1):3. [Google Scholar]
- 95.Braun Virginia, Clarke Victoria. American Psychological Association; 2012. Thematic Analysis. [Google Scholar]
- 96.Clarke Victoria, Braun Virginia, Hayfield Nikki. Qualitative Psychology: A Practical Guide to Research Methods. 3. 2015. Thematic analysis; pp. 222–248. [Google Scholar]
- 97.https://medium.com/@otacorporation0520/set-up-stun-turn-server-for-the-video-chat-app-ee8dc6fb9b15 Turn server kernel description.
- 98.https://ourcodeworld.com/articles/read/1175/how-to-create-and-configure-your-own-stun-turn-server-with-coturn-in-ubuntu-18-04 Turn-EC2 EC2 server setup.
- 99.https://www.name.com/support/articles/230050067-generating-a-certificate-signing-request-csr-through-cpanel Turn-SSL certificate EC2 server setup.
- 100.https://docs.aws.amazon.com/AWSEC2/latest/UserGuide/SSL-on-amazon-linux-2.html Turn-SSL certificate EC2 server setup and SSL certificate.
- 101.Okello Candiya Bongomin George, Munene John C., Yourougou Pierre. Examining the role of financial intermediaries in promoting financial literacy and financial inclusion among the poor in developing countries: lessons from rural Uganda. Cogent Econ. Finance. 2020;8(1) [Google Scholar]
- 102.Okello Candiya Bongomin George, Ntayi Joseph Mpeera, Munene John C., Akol Charles Malinga. Financial intermediation and financial inclusion of poor households: mediating role of social networks in rural Uganda. Cogent Econ. Finance. 2017;5(1) [Google Scholar]
- 103.Goodman M.L., Seidel S.E., Kaberia R., Keiser P.H. How can we improve healthcare access and general self-rated health among orphans and vulnerable children? Findings from a Kenyan cross-sectional study. Int. J. Public Health. 07 2015;60(5):589–597. doi: 10.1007/s00038-015-0681-z. [DOI] [PubMed] [Google Scholar]
- 104.England Paula. Emerging theories of care work. Annu. Rev. Sociol. 2005;31:381–399. [Google Scholar]
- 105.Ellie Harmon, Matthias Korn, Amy Voida. Proceedings of the 2017 ACM Conference on Computer Supported Cooperative Work and Social Computing. 2017. Supporting everyday philanthropy: care work in situ and at scale; pp. 1631–1645. [Google Scholar]
- 106.Porterfield A., Engelbert K., Coustasse A. Electronic prescribing: improving the efficiency and accuracy of prescribing in the ambulatory care setting. Perspect. Health Inf. Manag. 03 2014;11 [PMC free article] [PubMed] [Google Scholar]
- 107.Slovák Petr, Theofanopoulou Nikki, Cecchet Alessia, Cottrell Peter, Altarriba Bertran Ferran, Dagan Ella, Childs Julian, Isbister Katherine. “I just let him cry...: designing socio-technical interventions in families to prevent mental health disorders. nov 2018;2(CSCW) [Google Scholar]
- 108.Nikkhah Sarah, John Swaroop, Yalamarti Krishna Supradeep, Mueller Emily L., Miller Andrew D. Helping their child, helping each other: parents' mediated social support in the children's hospital. Companion Publication of the 2021 Conference on Computer Supported Cooperative Work and Social Computing; CSCW '21; New York, NY, USA: Association for Computing Machinery; 2021. pp. 140–143. [Google Scholar]
- 109.Ahmed N.U., Alam M.M., Sultana F., Sayeed S.N., Pressman A.M., Powers M.B. Reaching the unreachable: barriers of the poorest to accessing NGO healthcare services in Bangladesh. J. Health Popul. Nutr. 2006;24(4) [PMC free article] [PubMed] [Google Scholar]
- 110.Pearson Jennifer, Robinson Simon, Jones Matt. Exploring low-cost, Internet-free information access for resource-constrained communities. ACM Trans. Comput.-Hum. Interact. dec 2016;23(6) [Google Scholar]
- 111.Schmidt Clifford, Gorman Trina Jean, Bayor Andrew Azaabanye, Gary Michael Shayne. Impact of low-cost, on-demand, information access in a remote Ghanaian village. Proceedings of the 4th ACM/IEEE International Conference on Information and Communication Technologies and Development; ICTD '10; New York, NY, USA: Association for Computing Machinery; 2010. [Google Scholar]
- 112.Le Dantec Christopher A., Christensen Jim E., Bailey Mark, Farrell Robert G., Ellis Jason B., Danis Catalina M., Kellogg Wendy A., Edwards W. Keith. DIS '10. Association for Computing Machinery; New York, NY, USA: 2010. A tale of two publics: democratizing design at the margins; pp. 11–20. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Survey on orphans about online healthcare support for the orphans.
Survey over administrators of orphanages about online healthcare support for orphans.
Survey on voluntary participation in online healthcare consultation for resource-constrained communities (RCCs).
Data Availability Statement
The data that has been used in this study is confidential. Due to the sensitive nature of the research, the supporting data is not publicly available.