Abstract
Background and purpose
We conducted a systematic review and meta-analysis of RSA studies to investigate the early and long-term migration patterns of acetabular cups and the influence of implant factors on cup migration over time.
Methods
We performed a systematic search of PubMed, Embase, and Scopus databases to identify all RSA studies of cup migration following primary total hip replacement (THR). Proximal migration at 3 and 6 months, 1, 2, 5, and 10 years were considered for analysis. Implant factors investigated included fixation type, head size, bearing surface, uncemented coating design, and the decade of RSA introduction.
Results
47 studies reported the proximal migration of 83 cohorts (2,328 cups). Besides 1 threaded cup design, no implant factor investigated was found to significantly influence proximal migration. The mean pooled 2-year proximal migration of cemented cups (0.14 mm, 95% confidence interval [CI] 0.08–0.20) was not significantly different from uncemented cups (0.12 mm, CI 0.04–0.19). The mean pooled proximal migration at 6 months was 0.11 mm (CI 0.06–0.16) and there was no significant increase between 6 months and 2 years (0.015 mm, CI 0.000–0.030). 27 of 75 cohorts (36%) reported mean proximal migration greater than 0.2 mm at 2 years, which has previously been identified as a predictor of implants at risk of long-term loosening.
Conclusion
Our meta-analysis demonstrated that the majority of cup migration occurs within the first 6 months. With one exception, no implant factors influenced the 2-year proximal migration of acetabular cups. 36% of studies with 2-year migration were considered at risk of long-term loosening. Further investigation and comparison against long-term survivorship data would validate 6-month and/or 1-year proximal migration measurements as an earlier predictor of long-term loosening than the current 2-year threshold.
Aseptic loosening of the acetabular cup is one of the main causes for revision of primary total hip replacement (THR). The 2022 annual report from the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) and the 2022 annual report of the Dutch Arthroplasty Register indicated that in 2021, 21% and 34% respectively of revision in primary THR was caused by loosening of the implant [1,2]. Early migration of the acetabular cup has been shown to have an association with long-term risk of revision due to aseptic loosening [3]. Radiostereometric analysis (RSA) is the most sensitive technique to measure in vivo cup migration and is suggested to be used as an early qualitative tool for the phased introduction of new orthopedic hip implants internationally [4-6].
The current RSA migration threshold for predicting future loosening of acetabular cups used at primary THR was established in 2012 when a systematic review compared 49 long-term survivorship studies against 26 RSA studies of cup migration [3]. Acetabular cups that migrated greater than 1.0 mm proximally at 2 years were associated with poor survivorship at 10-years (> 5% revision) and classified as “unacceptable.” Mean proximal cup migration between 0.2 mm and 1.0 mm proximally at 2 years was classified as “at risk” because some cup designs had poor long-term survivorship in this range. Currently, RSA measurements at 2 years are 1 of 2 validated surrogate methods to predict long-term outcomes [6]. Identifying migration thresholds earlier than the current 2-year timepoint would be advantageous for the orthopedic community. Earlier assessment of new implant designs is beneficial as it can minimize the risk of patients receiving poor performing implants whilst also promoting continuous development of new implant designs.
As new acetabular cup designs continue to be introduced to the clinical setting, the number of RSA studies evaluating early and long-term cup migration have subsequently increased over time. Often RSA studies investigate only the migration of 1 cup design, which makes comparison of the migration pattern difficult between different designs. It is important to investigate the migration patterns of acetabular cups and identify the period where most migration occurs as this allows the ideal time point at which cups stabilize to be identified.
Therefore, the primary aim of our systematic review and meta-analysis was to investigate the early and long-term migration patterns of acetabular cups using RSA. The secondary aim was to investigate whether implant factors influence early migration patterns of the acetabular cup.
Methods
Search, screening, and selection
This systematic review is reported in accordance with the PRISMA statement [7]. A systematic literature search was conducted on February 28, 2022 and the following databases were used: PubMed, Embase, and Scopus. Articles in languages spoken by the review team were considered (English, German, Dutch, French, Italian, Spanish, and Korean). The search strategy consisted of the following components, each defined by a combination of controlled vocabulary and corresponding mesh terms: (1) hip replacement, (2) acetabular cup, (3) migration, and (4) RSA (see Appendix 1 in Supplementary data).
Covidence systematic review management software (https://www.covidence.org/) was used to export the searches to conduct a blinded review on the inclusion of the studies. The title and abstract screening were performed by 4 reviewers (CHC, AR, BP, and AB) independently. If the reviewers disagreed, the study remained eligible, and the full text was screened. The full texts of the eligible studies were screened by the same 4 reviewers and any disagreements were resolved by discussion or after consulting with 2 referees (SC and BP).
The inclusion criteria were any studies that reported: (1) primary THR, (2) migration measured using RSA, (3) proximal migration pattern of acetabular cup. A migration pattern was defined as the reporting of cup migration at 2 or more follow-up moments [8,9]. Studies were excluded if they did not report acetabular implant migration; reported on fewer than 5 acetabular cups; acetabular implant migration was not measured using RSA; the cohorts integrated the migration of acetabular cups used at revision THR; the studies were conference proceedings, thesis manuscript, or used languages not spoken by the review team; the studies used in vitro or animal models; the studies did not separate acetabular cup migration via implant types (Figure 1). Proximal cup migration was chosen as the primary outcome because it is the most commonly reported; has the best resolution; and has previously been associated with late aseptic loosening in primary acetabular cups [3]. The references of the records assessed for full-text review were also examined for additional inclusion of studies.
Figure 1.
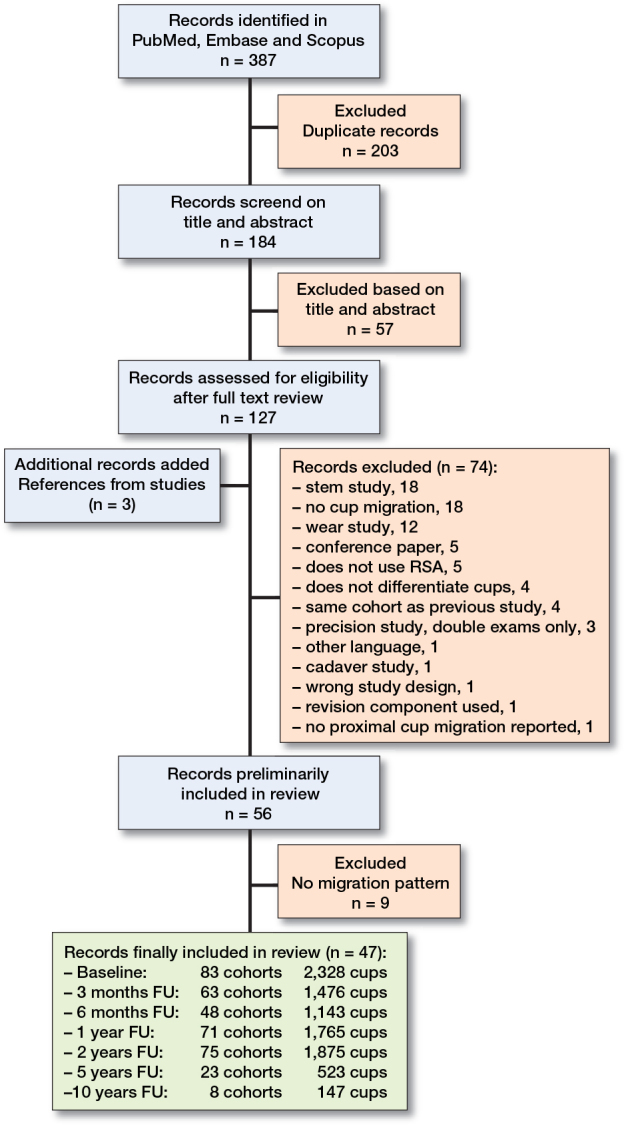
PRISMA flowchart for inclusion and exclusion of the literature.
Data extraction
Data was extracted by 4 reviewers (CHC, AR, BP. and RK). Any disagreements were resolved by discussion or after consulting with a referee (SC and BP). Data that was extracted included the year of publication, number of hips at each timepoint, implant fixation, surgical factors, RSA factors, and proximal migration (mm) of the acetabular implant at all timepoints. The mean proximal migration with corresponding standard deviation (SD) was extracted or calculated from reported median, interquartile range (IQR), or range using internationally accepted methodology [10]. When the data was represented only through a graph, Webplotdigitizer (version 4.6) (https://automeris.io/WebPlotDigitizer/) was used to extract the data [11]. In the rare case that only the mean migration was given without range, IQR, SE, or SD, the SD was calculated as the average SD from similar studies [8,9]. The rationale for this is that it is more important to include data that can later be subjected to sensitivity analyses, rather than to exclude data, which could lead to bias [9]. If multiple studies re-reported on the same cohort’s acetabular migration only the original study was included. Cohorts in this systematic review were separated by the type of acetabular implant and their implant factors. Data concerning patient demographics, RSA technique, and prosthesis characteristics (i.e., type of prosthesis, fixation, uncemented coating designs, and bearing surfaces) was extracted to allow for sub-cohort analyses. The year of initial patient recruitment of the first RSA study of each implant was extracted and categorized into “decade of RSA introduction” for further analysis.
Migration pattern was defined as the reporting of cup migration at 2 or more follow-up timepoints post-operation [8,9]. For example, a study with a migration pattern is when the study reports the mean proximal cup migration at 2 or more timepoints following a baseline postoperative measurement, e.g., “3 months” and “2 years” and/or other timepoints. A study without a migration pattern is when the study reports proximal migration at 1 timepoint following a baseline postoperative measurement, e.g., only “3 months” or only “2 year” timepoint. Studies without a migration pattern were not further analyzed, to minimize the effect of possible reporting bias in the literature.
Data synthesis and analysis
A study cohort was defined as a predefined set of patients that reported the mean cup migration collectively to investigate a study question. The cohorts investigated in each study are also presented in Appendix 3 (see Supplementary data). A study cohort typically represents the treatment cohort of a trial. For example, a trial comparing conventional polyethylene (PE) cups versus highly crossed-linked PE cups has 2 study cohorts. Up to 2-year follow-up we determined and plotted the 10th, 25th, 50th, 75th, and 90th percentile of the means (there were not enough study cohorts with follow-up beyond 2 years to reliably determine the percentiles).
A random effects model was used to pool the proximal migration of individual study cohorts in order to estimate the overall proximal migration for each follow-up and its associated 95% confidence interval (CI) [8,9]. Random effects meta-regression on study level covariates such as cup fixation, PE type, and the starting date of RSA studies was employed. Proximal migration at 2 years was used for this meta-regression because it was the most reported value and there was not enough data at later time points. Although proximal migration at 3 and 6 months, 1, 2, 5, and 10 years was considered for analysis, pooled analysis could not be performed after 5 years due to the small number of long-term RSA studies. All analyses were performed using Metafor Package R statistics [12].
Ethics, registration, data sharing, funding, and disclosure
No ethical approval was required for this study as the data was retrieved from previous published studies. A request for the compiled review can be made by contacting the corresponding author and will be available upon reasonable request. The protocol of this review was not registered. The study was not funded by any external or internal party. There are no conflicts of interest for any of the authors. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.24580
Results
Inclusion of RSA studies
After full text assessment, 56 studies were included in this systematic review [13-69]. However as 9 studies did not report a migration pattern at more than 1 follow-up timepoint (Appendix 2 in Supplementary data)) only 47 studies were analyzed (Figure 1). Overall, there were 83 study cohorts and 2,328 cups from 28 different cup designs that were followed up at least at 2 timepoints (Figure 1). The median percentage of female patients in each study cohort was 54% (range 11–100). The median percentage of patients with primary osteoarthritis (OA) was 100% (0–100). 47 study cohorts were restricted to primary OA. The mean age of the study cohorts varied between 47 and 77 years with a median of 64 years. Of the 47 studies, there were 11 single-cohort studies (see Appendix 3 in Supplementary data). The remaining 36 studies had 2 or more cohorts investigating the effects of surgical techniques, surgical factors, and/or implant factors on cup migration (see Appendix 3 in Supplementary data). 10 studies compared the migration of different acetabular cup designs, 8 of which compared new cups against a well-documented and recognized control implant. Interestingly, only 1 study investigated the effect of patient factors (BMD) on the migration (see Appendix 3 in Supplementary data) [22].
Reported precision
The mean precision of each study was reported as the CI (SD x 1.96) of the difference between 2 examinations taken on the same day. 30 of 47 RSA studies reported original precision data as determined by double examinations within each study. The average precision was 0.14 mm of proximal migration (range 0.00–0.39).
Migration results
Early migration in percentiles of the 83 study cohorts is depicted in Figure 2. The majority of the mean pooled proximal migration was recorded at 6 months with a mean of 0.11 mm (CI 0.06–0.16). The pooled increase in proximal migration between 6 months and 1 year was 0.007 mm based on 43 study cohorts. The pooled increase in proximal migration between 1 year and 2 years was 0.015 mm (CI 0.001–0.028) based on 63 study cohorts. The pooled increase in proximal migration between 6 months and 2 years was 0.015 mm (CI 0.000–0.030) based on 43 study cohorts. The proximal migration pattern of 2 known poorly performing acetabular cups (the Link V cup and the ReCap [metal-on-metal] hydroxyl-apatite coated cup) are plotted in Figure 2. Only 8 cohorts presented 10-year data on acetabular cup migration (Figure 3). Although the majority of the migration of acetabular cup occurred within the first 6 months, 3 of the 8 studies showed an increasing migration pattern greater than 0.1 mm between 5 and 10 years (Figure 3).
Figure 2.
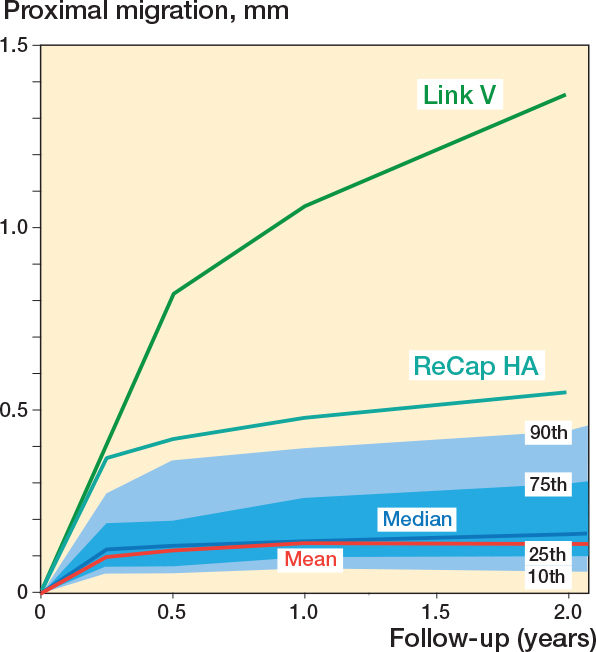
Early migration in percentiles of 83 study cohorts, 2,328 cups. The migration of 2 known acetabular cup failures is also plotted as they were outliers: the Link V cup and the ReCap hydroxyapatite coated cup.
Figure 3.
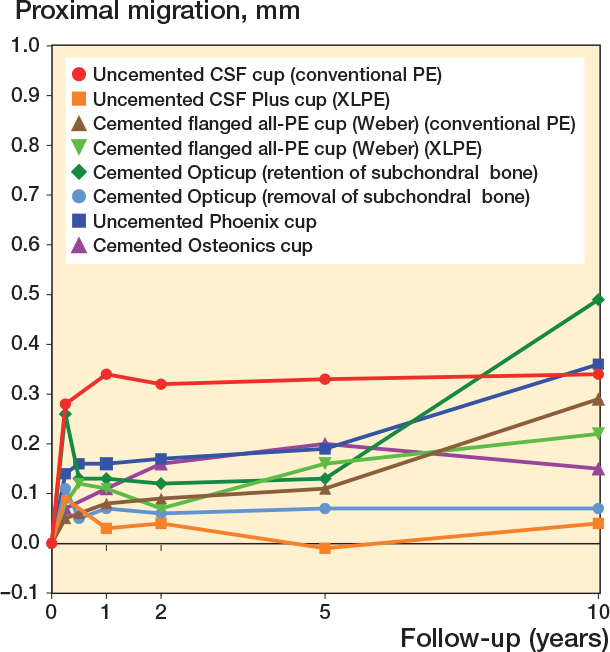
Long-term migration of 8 study cohorts. A significant number of patients are often lost at long-term follow-up (10 years); therefore the mean migration may be significantly influenced by an outlier. For example, a patient in the cemented Opticup cohort (retention of sub-subchondral bone) had been radiologically diagnosed with acetabular cup loosening, which may have significantly influenced the mean migration of the cohort. PE = standard polyethylene liner, XLPE = crosslinked-polyethylene liner, CSF = cancellous screw fit.
Notably, of 75 cohorts that reported 2-year proximal migration, 27 cohorts (36%) were considered at risk (> 0.2mm at 2 years). 64 cohorts reported the mean proximal migration of acetabular cups at both the 1-year and 2-year timepoint (Figure 4). There were 25 cohorts that were considered at risk at 2 years. 22 of the 25 cohorts were already above the threshold at 1 year. Of the 64 cohorts, 43 cohorts also reported the mean proximal migration at 6 months. 12 of the 43 cohorts that were above the threshold at 2 years also reported 6-month proximal migration results, 11 of which were already above the recommended threshold at 6 months (92%) (Figure 4).
Figure 4.
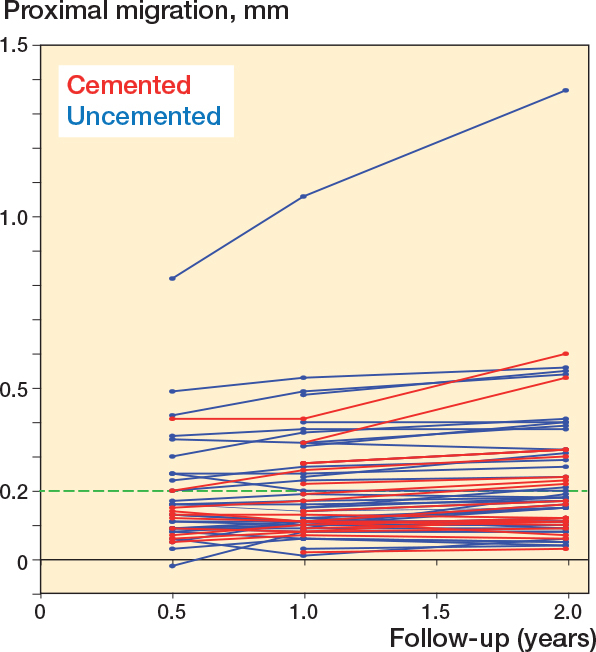
Reported mean proximal migration from RSA studies that reported proximal migration at 6 months, 1 year, and 2 years. The green dashed line represents the 0.2 mm threshold.
Implant fixation, head size, and liner
The pooled 2-year proximal migration of cemented cups and uncemented cups was 0.14 mm (CI 0.08–0.20) and 0.12 mm (CI 0.04–0.19), respectively (Figure 5). There were 4 different types of uncemented cups identified in this review (Figure 6). At 2 years, proximal migration of threaded cups was 1.4 mm (CI 0.27–2.5), porous coated cups 0.17 mm (CI 0.08–0.25), hydroxyapatite coated cups 0.11 mm (CI 0.02–0.19), and hydroxyapatite tricalcium phosphate (TCP) coated cups 0.13 mm (CI –0.24 to 0.50) (Figure 6). The RSA study that used the Link V threaded cup (smooth surface) reported the highest amount of proximal migration [58].The pooled mean 2-year proximal migration of acetabular cups first studied with RSA in the 1990s was 0.15 mm (CI 0.05–0.25), in the 2000s was 0.11mm (CI 0.05–0.17), and in the 2010s was 0.16 mm (CI 0.07–0.26) (Figure 7).
Figure 5.
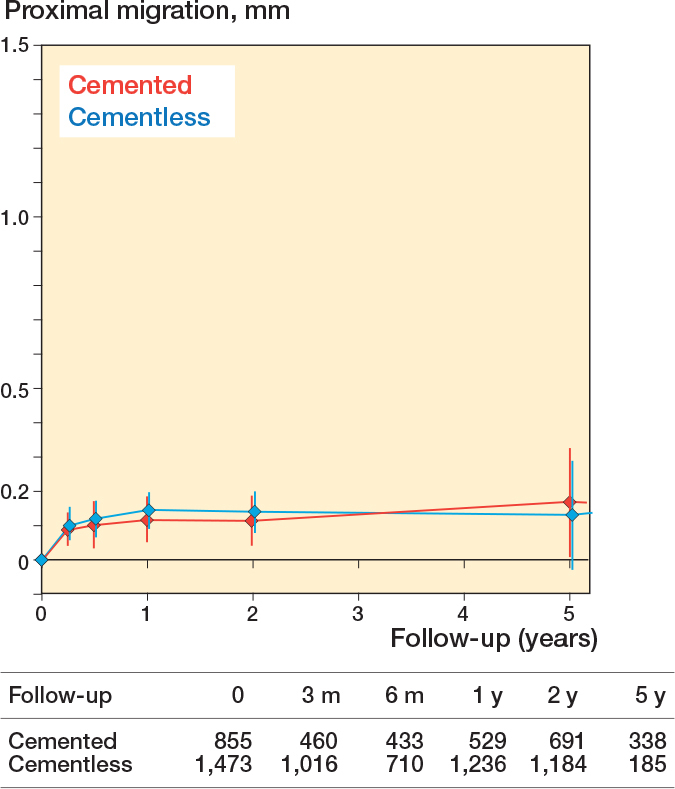
The mean pooled migration overtime (CI) for cemented and cementless acetabular cups.
Figure 6.
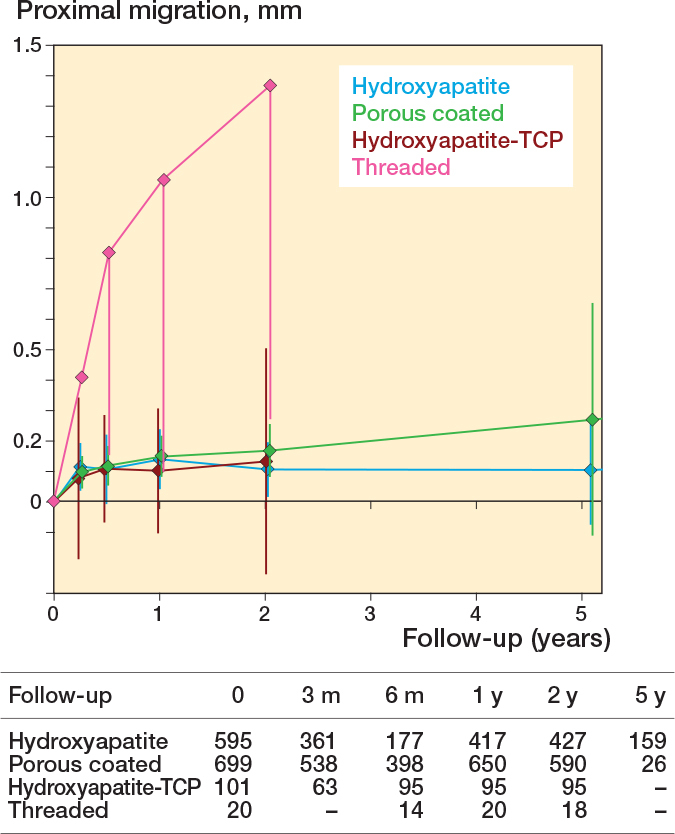
Mean pooled migration overtime (CI) according to the cementless cup surface type. The threaded cup is only 1 study cohort comprising the Link V cup. TCP = tricalcium phosphate.
Figure 7.
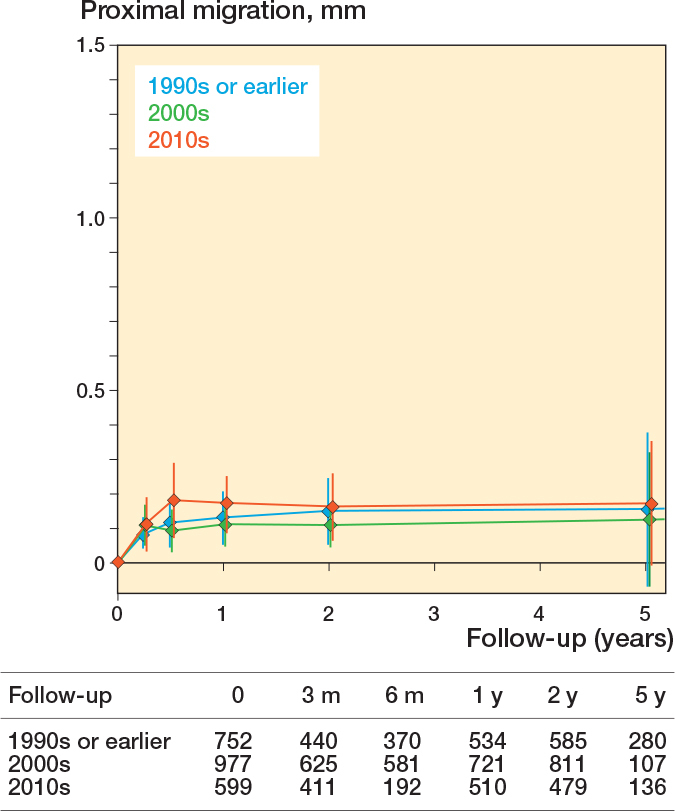
Mean pooled migration overtime (CI) by decade of RSA introduction (1990s, 2000s, and 2010s).
There were 4 different head sizes, 36 mm, 32 mm, 28 mm, and 22 mm, identified in the review. The 2-year proximal migration of acetabular cups with different head sizes was 0.15 mm (CI –0.21 to 0.50], 0.14 mm (CI 0.04–0.23), 0.10 mm (CI 0.02–0.18), and 0.22 mm (CI –0.02 to 0.45), respectively (Figure 8). The 2-year proximal migration for non-crosslinked (non-XLPE) was 0.16 mm (CI 0.07–0.25), for crossed-linked (XLPE) 0.11 mm (CI 0.02–0.20), and for crossed-linked with antioxidants (XLPE+AO) 0.18 mm (CI 0.05–0.32) (Figure 9). The migration of patients in RCTs did not differ from patients in observational studies (Figure 10).
Figure 8.
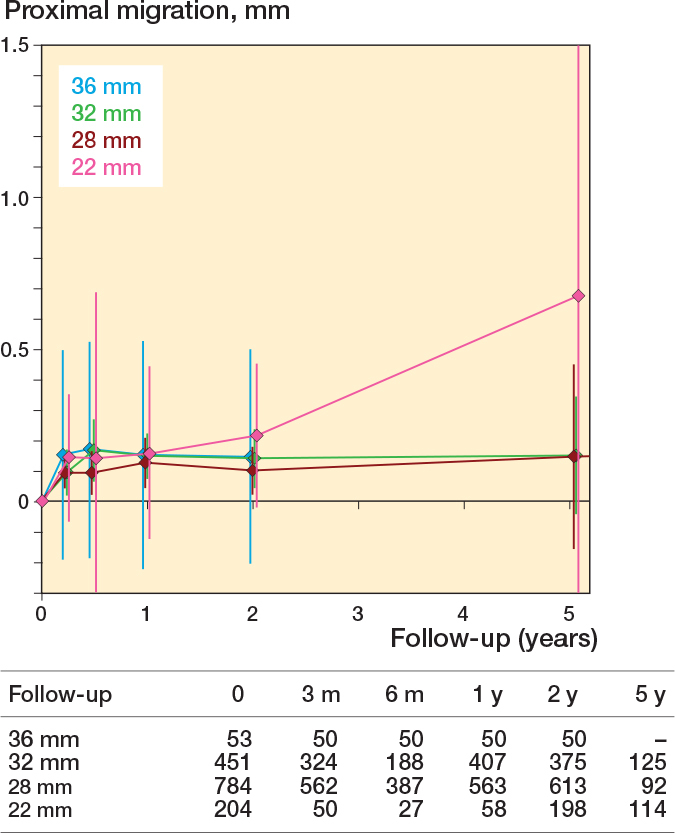
Mean pooled migration overtime (CI) according to femoral head size.
Figure 9.
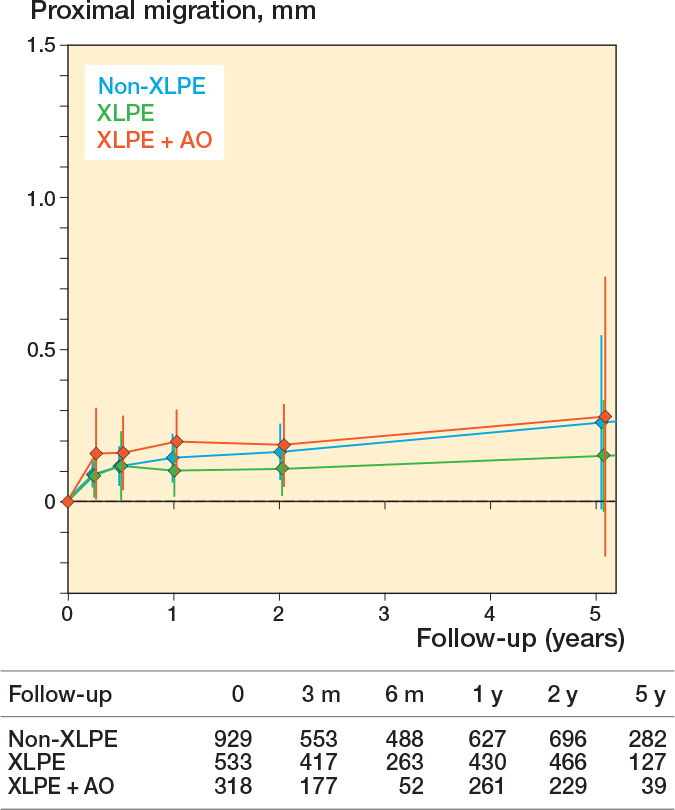
Mean pooled migration overtime (CI) according to PE type. XLPE = crosslinked polyethylene, AO = antioxidant.
Figure 10.
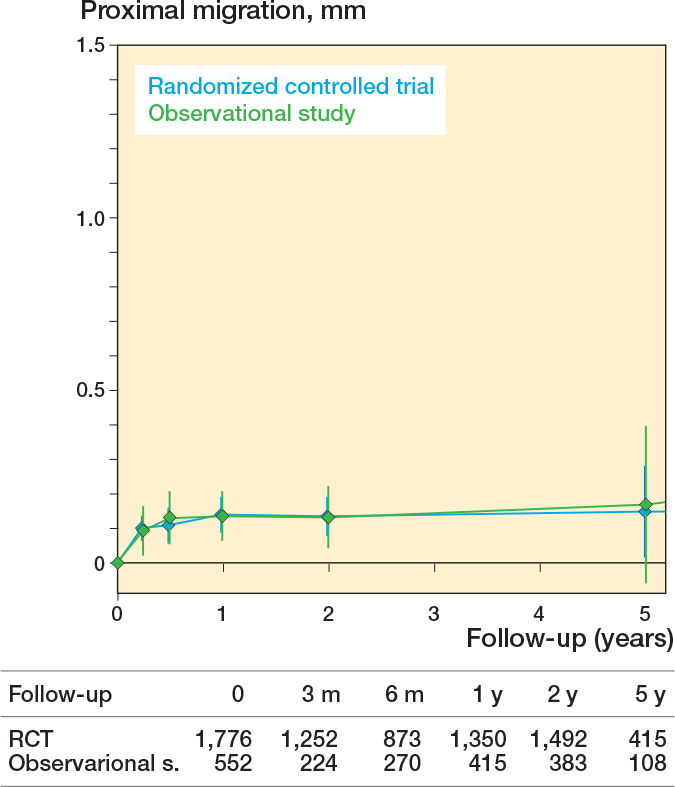
Mean pooled migration overtime (CI) according to study design. RCT = randomized controlled trial
Discussion
The earliest validated RSA timepoint to predict long-term acetabular cup loosening is 2 years post-surgery [3]. RSA cup migration studies have increased in the last decade. For example, in our systematic review, we identified 2,328 cups from 83 study cohorts compared with 700 cups and 26 study cohorts in the previous RSA cup review [3]. Our meta-analysis showed that the majority of acetabular cup migration occurs in the first 6 months. Besides the higher migration of 1 threaded cup design, none of the investigated implant factors had a significant influence on migration within the first 5 years. Given the small difference in pooled migration at 6 months, 1 year, and 2 years, there is the potential to validate an earlier timepoint than the current 2-year threshold. Earlier assessment of new implant designs may reduce the risk of patients receiving a poor performing implant and encourage ongoing implant design improvement.
Our review demonstrated that 27 of 75 study cohorts (36%) reported proximal migration at 2 years that would classify them as “at risk” (> 0.2 mm proximal migration at 2 years) [3]. Further analysis of these cohorts is required to determine the association with long-term survivorship in clinical studies or registry reports. Additionally, we found that most of the acetabular cups that were “at risk” at 2 years were already above the recommended threshold at both 6 months and 1 year. Further investigation is required to confirm the use of these earlier timepoints as a benchmark in the future.
Despite the majority of migration occurring early, it is still important to monitor implant stabilization over time as continuing migration may be suggestive of loosening. Hence the continued cup stability beyond 2 years can be used as an extra safeguard during the phased introduction of THR implants. Unfortunately, we were unable to analyze pooled proximal migration beyond the 5-year timepoint as only 8 RSA studies reported proximal migration at 10 years. 3 of the 8 long-term cohorts reported increasing migration between 5 and 10 years [19,25,31], suggesting that more long-term RSA studies are required to investigate the patterns of continued migration.
Initially, implant factors and fixation methods were hypothesized to influence early cup migration. However, the results of this meta-analysis suggested that implant factors and the majority of fixation methods did not influence the early migration of acetabular cups. Of the uncemented cups, one threaded cup with a known history of poor performance (Link V) was observed to have greater early migration than porous, hydroxyapatite, and TCP coated cups. As cemented and uncemented acetabular cups did not have a significant difference in migration pattern in the first 5 years, this allowed the pooled analysis of migration patterns of all cups regardless of fixation type. While the early proximal migration patterns were similar in this study, there may be differences in migration patterns between cup fixation methods in translational and/or rotational axes not investigated in this meta-analysis. In addition, future migration thresholds may also differ between cup fixation methods due to differences in cup long-term registry loosening rates. This was evident in a previous threshold validation study where only 1 of 6 cemented cups investigated had “acceptable” migration at 2 years [3].
Our meta-analysis found similar early migration patterns independent of bearing surface. In contrast, long-term registry results report an improved survivorship of THR with XLPE bearings and it is likely this benefit will only be seen in long-term RSA migration studies. The use of larger heads did not result in increased migration; however, there was only one randomized RSA study to investigate the influence of larger heads on cup migration [66]. In our study, 22-mm heads were the only head size that had increasing migration between 2 and 5 years. However, 22-mm heads are no longer commonly used in THR and confounding factors such as the type of liner material and cup design limited statistical comparison between head sizes. This is supported by the finding of no migration difference between cups introduced with RSA in the 1990s, 2000s, and 2010s, although the authors acknowledge there may be improved stability of new cup designs within the pooled results.
It is important to note that the mean proximal migration of each cohort was analyzed and not individual cup migration. Only 8 RSA studies reported individual cup migration [23,29,31,32,35-37,44]. Reporting the mean migration of a cohort may not be representative of the individual outliers within the cohort and different interpretation of individual results against thresholds is required. For example, Aspenberg et al. have indicated that excessive migration of acetabular cups is a product of a dichotomy and only a small proportion of cups that are identified at risk of loosening may require revision surgery [70].
The majority of RSA studies investigate implant or surgical factors and only 1 study investigated the effects of patient factors on proximal migration of acetabular cups. Therefore, future RSA studies should investigate the effects of patient factors on the migration of cups. However, it is not feasible for all future RSA studies to report migration by factors for each patient as this can result in excessive manuscript length. Nonetheless, a thorough analysis of individual patient factors would require inclusion of larger patient cohorts, more resources, and associated costs. Such an analysis would preferably be based on a meta-analysis like ours if information on an individual level were to have been available.
Limitations
Our review has several limitations. First, we investigated only pooled proximal migration as it was the most reported measurement, and it has previously been used to predict loosening of acetabular cups [3]. We did not investigate the maximum total point motion (MTPM) or other axes of translation and rotation. Second, 45 of 47 RSA studies reported the migration as signed proximal values, which is acknowledged to result in a lower mean when compared with absolute values. Signed migration values are important as distal (negative proximal) migration can occur in cases that lose superior fixation [71]. RSA guidelines recommend reporting signed values to minimize methodological errors [72]. Third, it would be advantageous to investigate the individual cup migration patterns as this will allow further investigation of patient factors that may influence cup migration. The outliers and the different number of patients included at each follow-up timepoint in RSA studies may influence mean migration [70,73,74]. Currently, it is difficult to determine the full extent of the influence of patient factors on cup migration with the mean of the cohorts as there is already significant variability of patient factors (age, sex, BMD, bone quality, and the rate of activity). Many RSA studies have recruited patients with OA who may not have equal bone quality to those diagnosed with other conditions such as rheumatoid arthritis or fractured neck of femur. As the majority of the RSA studies did not report the BMD of individual patients or their comorbidities, it is difficult to assess the effect of bone density on implant migration. Therefore, the results of this systematic review may not be equal under different bone quality and healing conditions. It was not possible to perform subgroup meta-analysis to directly compare implant or surgical factors (e.g., to perform meta-analysis between studies that only randomized the same cup with different head sizes) as there were not enough RSA studies. Additionally, in our review, there were not enough studies of the same cup design to allow comparison of the migration patterns measured using different RSA techniques. Only 1 study investigated the effect of RSA methods on cup migration and found significantly higher migration when using model-based RSA compared with marker-based RSA [55]. Finally, we did not compare our results with the long-term survivorship studies of the same acetabular cup designs. Therefore, we were not able validate whether 6-month or 1-year RSA measurements could be used as a surrogate method to predict long-term loosening. However, this initial meta-analysis of cup migration patterns was required to identify the period where most migration occurs prior to the validation of new thresholds. A strength of this meta-analysis is that all the phases of the review have been completed by 2 to 4 reviewers and a relatively large number of studies were identified.
Conclusion
This meta-analysis suggests that the majority of the proximal migration of acetabular cups used at primary THR occurs within the first 6 months. Besides higher migration of 1 threaded cup design, no implant factors influenced the 2-year proximal migration of acetabular cups. Pooled analysis of acetabular cup migration beyond 5 years was not possible due to the limited amount of RSA studies. Further investigation and comparison against long-term survivorship data is required to determine whether 6-month and/or 1-year proximal migration measurements may be used as a predictor of long-term loosening.
Supplementary data
Appendices 1–3 are available as Supplementary data on the article page, doi: 10.2340/17453674.2023.24580
Supplementary Material
CHC, BP, LBS, JMA, and SC contributed to study design and manuscript production. CHC, RK, AH, and AB contributed to review and data extraction. The same authors cross-checked the data to ensure the accuracy of the data extraction. BP performed data analysis. CHC, BP, LBS, JMA, and SC participated in interpretation of the results. CHC, BP, and SC wrote the initial manuscript. All authors discussed the manuscript and contributed to the final manuscript.
The authours would like to acknowledge the University of Adelaide’s research librarian Vikki Langton for her assistance with the literature search. Stuart Callary held an EMCR Fellowship from The Hospital Research Foundation Group during the time of this study.
Handling co-editors: Ivan Hvid and Robin Christensen
Acta thanks Hannu T Aro and Johan Kärrholm for help with peer review of this manuscript.
References
- 1.AOANJRR . Australian Orthopaedic Association National Joint Replacement Registry Annual Report 2022. Adelaide: Australian Orthopaedic Association; 2022. [Google Scholar]
- 2.LROI . LROI annual report 2022. Netherlands: Dutch Arthroplasty Register; 2022. [Google Scholar]
- 3.Pijls B G, Nieuwenhuijse M J, Fiocco M, Plevier J W, Middeldorp S, Nelissen R G, et al. Early proximal migration of cups is associated with late revision in THA: a systematic review and meta-analysis of 26 RSA studies and 49 survival studies. Acta Orthop 2012; 83(6): 583-91. doi: 10.3109/17453674.2012.745353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasan S, Marang-van de Mheen P J, Kaptein B L, Nelissen R, Pijls B G.RSA-tested TKA implants on average have lower mean 10-year revision rates than non-RSA-tested designs. Clin Orthop Relat Res 2020; 478(6): 1232-41. doi: 10.1097/corr.0000000000001209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nelissen R G, Pijls B G, Kärrholm J, Malchau H, Nieuwenhuijse M J, Valstar E R. RSA and registries: the quest for phased introduction of new implants. J Bone Joint Surg Am 2011; 93(Suppl. 3): 62-5. doi: 10.2106/jbjs.K.00907. [DOI] [PubMed] [Google Scholar]
- 6.Malak T T, Broomfield J A, Palmer A J, Hopewell S, Carr A, Brown C, et al. Surrogate markers of long-term outcome in primary total hip arthroplasty: a systematic review. Bone Joint Res 2016; 5(6): 206-14. doi: 10.1302/2046-3758.56.2000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liberati A, Altman D G, Tetzlaff J, Mulrow C, Gøtzsche P C, Ioannidis J P, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009; 62(10): e1-e34. doi: [DOI] [PubMed] [Google Scholar]
- 8.Hasan S, van Dijk L A, Nelissen R G, Plevier J W, Blankevoort L, Pijls B G. RSA migration of unicondylar knee arthroplasties is comparable to migration of total knee arthroplasties: a meta-analysis. J ISAKOS 2022; 7(3): 17-23. doi: 10.1016/j.jisako.2021.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Pijls B G, Plevier J W M, Nelissen R. RSA migration of total knee replacements. Acta Orthop 2018; 89(3): 320-8. doi: 10.1080/17453674.2018.1443635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hozo S P, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005; 5(1): 13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drevon D, Fursa S R, Malcolm A L. Intercoder reliability and validity of WebPlotDigitizer in extracting graphed data. Behav Modif 2017; 41(2): 323-39. doi: 10.1177/0145445516673998. [DOI] [PubMed] [Google Scholar]
- 12.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw 2010; 36(3): 1-48. doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- 13.Baad-Hansen T, Kold S, Nielsen P T, Laursen M B, Christensen P H, Soballe K. Comparison of trabecular metal cups and titanium fiber-mesh cups in primary hip arthroplasty: a randomized RSA and bone mineral densitometry study of 50 hips. Acta Orthop 2011; 82(2): 155-60. doi: 10.3109/17453674.2011.572251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bergvinsson H, Sundberg M, Flivik G. Polyethylene wear with ceramic and metal femoral heads at 5 years: a randomized controlled trial with radiostereometric analysis. J Arthroplasty 2020; 35(12): 3769-76. doi: 10.1016/j.arth.2020.06.057. [DOI] [PubMed] [Google Scholar]
- 15.Bergvinsson H, Zampelis V, Sundberg M, Flivik G. Highly cross-linked polyethylene still outperforms conventional polyethylene in THA: 10-year RSA results. Acta Orthop 2021; 92(5): 568-74. doi: 10.1080/17453674.2021.1932140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bergvinsson H, Zampelis V, Sundberg M, Tjörnstrand J, Flivik G. Vitamin E infused highly cross-linked cemented cups in total hip arthroplasty show good wear pattern and stabilize satisfactorily: a randomized, controlled RSA trial with 5-year follow-up. Acta Orthop 2022; 93: 249-55. doi: 10.2340/17453674.2022.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bourne R B, McCalden R W, Naudie D, Charron K D, Yuan X, Holdsworth D W. The next generation of acetabular shell design and bearing surfaces. Orthopedics 2008; 31(12 Suppl. 2). doi: [PubMed] [Google Scholar]
- 18.Carlsson L V, Albrektsson B E J, Albrektsson B G, Albrektsson T O, Jacobsson C M, Macdonald W, et al. Stepwise introduction of a boneconserving osseointegrated hip arthroplasty using RSA and a randomized study: I. Preliminary investigations—52 patients followed for 3 years. Acta Orthop 2006; 77(4): 549-58. doi: 10.1080/17453670610012601. [DOI] [PubMed] [Google Scholar]
- 19.Digas G, Kärrholm J, Thanner J, Malchau H, Herberts P. Highly cross-linked polyethylene in cemented THA: randomized study of 61 hips. Clin Orthop Relat Res 2003. (417): 126-38. doi: 10.1097/01.blo.0000096802.78689.45. [DOI] [PubMed] [Google Scholar]
- 20.Digas G, Kärrholm J, Thanner J, Malchau H, Herberts P. The Otto Aufranc Award. Highly cross-linked polyethylene in total hip arthroplasty: randomized evaluation of penetration rate in cemented and uncemented sockets using radiostereometric analysis. Clin Orthop Relat Res 2004. (429): 6-16. doi: [PubMed] [Google Scholar]
- 21.Digas G, Thanner J, Anderberg C, Kärrholm J. Bioactive cement or ceramic/porous coating vs. conventional cement to obtain early stability of the acetabular cup: randomised study of 96 hips followed with radiostereometry. J Orthop Res 2004; 22(5): 1035-43. doi: 10.1016/j.orthres.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 22.Finnilä S, Moritz N, Svedströ M E, Alm J J, Aro H T. Increased migration of uncemented acetabular cups in female total hip arthroplasty patients with low systemic bone mineral density: a 2-year RSA and 8-year radiographic follow-up study of 34 patients. Acta Orthop 2016; 87(1): 48-54. doi: 10.3109/17453674.2015.1115312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Flatøy B, Rydinge J, Dahl J, Röhrl S M, Nordsletten L. Low wear, high stability: promises of success in a moderately cross-linked cup? Hip Int 2015; 25(3): 199-203. doi: 10.5301/hipint.5000230. [DOI] [PubMed] [Google Scholar]
- 24.Flivik G, Kristiansson I, Ryd L. Positive effect of removal of subchondral bone plate for cemented acetabular component fixation in total hip arthroplasty: a randomised RSA study with ten-year follow-up. Bone Joint J 2015; 97-b(1): 35-44. doi: 10.1302/0301-620x.97b1.34391. [DOI] [PubMed] [Google Scholar]
- 25.Flivik G, Sanfridsson J, Önnerfält R, Kesteris U, Ryd L. Migration of the acetabular component: effect of cement pressurization and significance of early radiolucency. Acta Orthop 2005; 76(2): 159-68. doi: 10.1080/00016470510030526. [DOI] [PubMed] [Google Scholar]
- 26.Galea V P, Rojanasopondist P, Laursen M, Muratoglu O K, Malchau H, Bragdon C. Evaluation of vitamin E-diffused highly crosslinked polyethylene wear and porous titanium-coated shell stability: a seven-year randomized control trial using radiostereometric analysis. Bone Joint J 2019; 101-b(7): 760-7. doi: 10.1302/0301-620x.101b7.Bjj-2019-0268.R1. [DOI] [PubMed] [Google Scholar]
- 27.Hjorth M H, Lorenzen N D, Søballe K, Jakobsen S S, Stilling M. Equal primary fixation of resurfacing stem, but inferior cup fixation with anterolateral vs posterior surgical approach: a 2-year blinded randomized radiostereometric and dual-energy x-ray absorptiometry study of metal-on-metal hip resurfacing arthroplasty. J Arthroplasty 2017; 32(11): 3412-20. doi: 10.1016/j.arth.2017.05.034. [DOI] [PubMed] [Google Scholar]
- 28.Hjorth M H, Søballe K, Jakobsen S S, Lorenzen N D, Mechlenburg I, Stilling M. No association between serum metal ions and implant fixation in large-head metal-on-metal total hip arthroplasty. Acta Orthop 2014; 85(4): 355-62. doi: 10.3109/17453674.2014.922731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Howie D W, Holubowycz O T, Callary S A, Robertson T S, Solomon L B. Highly Porous tantalum acetabular components without ancillary screws have similar migration to porous titanium acetabular components with screws at 2 years: a randomized controlled trial. J Arthroplasty 2020; 35(10): 2931-7. doi: 10.1016/j.arth.2020.05.049. [DOI] [PubMed] [Google Scholar]
- 30.Itayem R, Arndt A, McMinn D J, Daniel J, Lundberg A. A five-year radiostereometric follow-up of the Birmingham Hip Resurfacing arthroplasty. J Bone Joint Surg Br 2007; 89(9): 1140-3. doi: 10.1302/0301-620x.89b9.18367. [DOI] [PubMed] [Google Scholar]
- 31.Jacobsen A, Seehaus F, Hong Y, Cao H, Schuh A, Forst R, et al. Model-based roentgen stereophotogrammetric analysis using elementary geometrical shape models: 10 years results of an uncemented acetabular cup component. BMC Musculoskelet Disord 2018; 19(1): 335. doi: 10.1186/s12891-018-2259-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jørgensen P B, Daugaard H, Jakobsen S S, Lamm M, Søballe K, Stilling M. Higher early proximal migration of hemispherical cups with electrochemically applied hydroxyapatite (BoneMaster) on a porous surface compared with porous surface alone: a randomized RSA study with 53 patients. Acta Orthop 2020; 91(1): 26-32. doi: 10.1080/17453674.2019.1687860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kadar T, Hallan G, Aamodt A, Indrekvam K, Badawy M, Skredderstuen A, et al. Wear and migration of highly cross-linked and conventional cemented polyethylene cups with cobalt chrome or Oxinium femoral heads: a randomized radiostereometric study of 150 patients. J Orthop Res 2011; 29(8): 1222-9. doi: 10.1002/jor.21389. [DOI] [PubMed] [Google Scholar]
- 34.Kjærgaard K, Ding M, Jensen C, Bragdon C, Malchau H, Andreasen C M, et al. Vitamin E-doped total hip arthroplasty liners show similar head penetration to highly cross-linked polyethylene at five years: a multi-arm randomized controlled trial. Bone Joint J 2020; 102-b(10): 1303-10. doi: 10.1302/0301-620x.102b10.Bjj-2020-0138.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klaassen A D, Schäffer E A, Willigenburg N W, Van Beers L, Scholtes V A B, Van der Hulst V P M, et al. Comparison of early migration patterns between a ceramic and polyethylene liner in uncemented Trabecular Titanium cups: a 2-year randomized controlled trial of 52 hips using radiostereometric analysis. Acta Orthop 2022; 93: 451-8. doi: 10.2340/17453674.2022.2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laende E K, Richardson C G, Dunbar M J. Migration and wear of a dual mobility acetabular construct at 3 years measured by radiostereometric analysis. J Arthroplasty 2020; 35(4): 1109-16. doi: 10.1016/j.arth.2019.11.010. [DOI] [PubMed] [Google Scholar]
- 37.Lazarinis S, Milbrink J, Mattsson P, Mallmin H, Hailer N P. Bone loss around a stable, partly threaded hydroxyapatite-coated cup: a prospective cohort study using RSA and DXA. Hip Int 2014; 24(2): 155-66. doi: 10.5301/hipint.5000104. [DOI] [PubMed] [Google Scholar]
- 38.Lindalen E, Dahl J, Nordsletten L, Snorrason F, Høvik Ø, Röhrl S. Reverse hybrid and cemented hip replacement compared using radiostereometry and dual-energy X-ray absorptiometry: 43 hips followed for 2 years in a prospective trial. Acta Orthop 2012; 83(6): 592-8. doi: 10.3109/17453674.2012.742393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Minten M J, Heesterbeek P J, Spruit M. No effect of additional screw fixation of a cementless, all-polyethylene press-fit socket on migration, wear, and clinical outcome. Acta Orthop 2016; 87(4): 363-7. doi: 10.1080/17453674.2016.1190244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Munzinger U, Guggi T, Kaptein B, Persoon M, Valstar E, Doets H C. A titanium plasma-sprayed cup with and without hydroxyapatite-coating: a randomised radiostereometric study of stability and osseointegration. Hip Int 2013; 23(1): 33-9. doi: 10.5301/hip.2013.10598. [DOI] [PubMed] [Google Scholar]
- 41.Naudie D D, Somerville L, Korczak A, Yuan X, McCalden R W, Holdsworth D, et al. A randomized trial comparing acetabular component fixation of two porous ingrowth surfaces using RSA. J Arthroplasty 2013. ; 28(8 Suppl.): 48-52. doi: 10.1016/j.arth.2013.06.041. [DOI] [PubMed] [Google Scholar]
- 42.Nilsson K G, Theodoulou A, Mercer G, Quinn S J, Krishnan J. Midterm migration of a cementless, porous acetabular cup: a 5 year radiostereometric analysis. J Orthop 2017; 14(4): 454-60. doi: 10.1016/j.jor.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nivbrant B, Kärrholm J, Röhrl S, Hassander H, Wesslén B. Bone cement with reduced proportion of monomer in total hip arthroplasty: preclinical evaluation and randomized study of 47 cases with 5 years’ follow-up. Acta Orthop Scand 2001; 72(6): 572-84. doi: 10.1080/000164701317268987. [DOI] [PubMed] [Google Scholar]
- 44.Onsten I, Bengnér U, Besjakov J. Socket migration after Charnley arthroplasty in rheumatoid arthritis and osteoarthritis: a roentgen stereophotogrammetric study. J Bone Joint Surg Br 1993; 75(5): 677-80. doi: 10.1302/0301-620x.75b5.8376420. [DOI] [PubMed] [Google Scholar]
- 45.Onsten I, Carlsson A S. Cemented versus uncemented socket in hip arthroplasty: a radiostereometric study of 60 randomized hips followed for 2 years. Acta Orthop Scand 1994; 65(5): 517-21. doi: 10.3109/17453679409000904. [DOI] [PubMed] [Google Scholar]
- 46.Onsten I, Carlsson A S, Sanzén L, Besjakov J. Migration and wear of a hydroxyapatite-coated hip prosthesis: a controlled roentgen stereophotogrammetric study. J Bone Joint Surg Br 1996; 78(1): 85-91. doi: [PubMed] [Google Scholar]
- 47.Pakvis D, Luites J, van Hellemondt G, Spruit M. A cementless, elastic press-fit socket with and without screws. Acta Orthop 2012; 83(5): 481-7. doi: 10.3109/17453674.2012.720116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Palm L, Olofsson J, åström S-E, Ivarsson I. No difference in migration or wear between cemented low-profile cups and standard cups: a randomized radiostereographic study of 53 patients over 3 years. Acta Orthop 2007; 78(4): 479-84. doi: 10.1080/17453670710014112. [DOI] [PubMed] [Google Scholar]
- 49.Röhrl S, Nivbrant B, Mingguo L, Hewitt B. In vivo wear and migration of highly cross-linked polyethylene cups: a radiostereometry analysis study. J Arthroplasty 2005; 20(4): 409-13. doi: 10.1016/j.arth.2004.09.040. [DOI] [PubMed] [Google Scholar]
- 50.Röhrl S M, Li M G, Nilsson K G, Nivbrant B. Very low wear of non-remelted highly cross-linked polyethylene cups: an RSA study lasting up to 6 years. Acta Orthop 2007; 78(6): 739-45. doi: 10.1080/17453670710014509. [DOI] [PubMed] [Google Scholar]
- 51.Röhrl S M, Li M G, Pedersen E, Ullmark G, Nivbrant B. Migration pattern of a short femoral neck preserving stem. Clin Orthop Relat Res 2006. ; 448: 73-8. doi: 10.1097/01.blo.0000224000.87517.4c. [DOI] [PubMed] [Google Scholar]
- 52.Röhrl S M, Nivbrant B, Nilsson K G. No adverse effects of submelt-annealed highly crosslinked polyethylene in cemented cups: an RSA study of 8 patients 10 years after surgery. Acta Orthop 2012; 83(2): 14852. doi: 10.3109/17453674.2011.652889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Röhrl S M, Nivbrant B, Ström H, Nilsson K G. Effect of augmented cup fixation on stability, wear, and osteolysis: a 5-year follow-up of total hip arthroplasty with RSA. J Arthroplasty 2004; 19(8): 962-71. doi: 10.1016/j.arth.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 54.Salemyr M, Muren O, Eisler T, Bodén H, Chammout G, Stark A, et al. Porous titanium construct cup compared to porous coated titanium cup in total hip arthroplasty: a randomised controlled trial. Int Orthop 2015; 39(5): 823-32. doi: 10.1007/s00264-014-2571-z. [DOI] [PubMed] [Google Scholar]
- 55.Shareghi B, Johanson P E, Kärrholm J. Clinical evaluation of model-based radiostereometric analysis to measure femoral head penetration and cup migration in four different cup designs. J Orthop Res 2017; 35(4): 760-7. doi: 10.1002/jor.23177. [DOI] [PubMed] [Google Scholar]
- 56.Sillesen N H, Greene M E, Nebergall A K, Nielsen P T, Laursen M B, Troelsen A, et al. Three year RSA evaluation of vitamin e diffused highly cross-linked polyethylene liners and cup stability. J Arthroplasty 2015; 30(7): 1260-4. doi: 10.1016/j.arth.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 57.Sköldenberg O G, Rysinska A D, Chammout G, Salemyr M, Mukka S S, Bodén H, et al. A randomized double-blind noninferiority trial, evaluating migration of a cemented vitamin E-stabilized highly crosslinked component compared with a standard polyethylene component in reverse hybrid total hip arthroplasty. Bone Joint J 2019; 101-b(10): 1192-8. doi: 10.1302/0301-620x.101b10.Bjj-2019-0456.R2. [DOI] [PubMed] [Google Scholar]
- 58.Snorrason F, Kärrholm J. Primary migration of fully-threaded acetabular prostheses: a roentgen stereophotogrammetric analysis. J Bone Joint Surg Br 1990; 72(4): 647-52. doi: 10.1302/0301-620x.72b4.2199453. [DOI] [PubMed] [Google Scholar]
- 59.Tabori-Jensen S, Mosegaard S B, Hansen T B, Stilling M. Inferior stabilization of cementless compared with cemented dual-mobility cups in elderly osteoarthrosis patients: a randomized controlled radiostereometry study on 60 patients with 2 years’ follow-up. Acta Orthop 2020; 91(3): 246-53. doi: 10.1080/17453674.2020.1720978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thanner J, Freij-Larsson C, Kärrholm J, Malchau H, Wesslén B. Evaluation of Boneloc: chemical and mechanical properties, and a randomized clinical study of 30 total hip arthroplasties. Acta Orthop Scand 1995; 66(3): 207-14. doi: 10.3109/17453679508995525. [DOI] [PubMed] [Google Scholar]
- 61.Thanner J, Kärrholm J, Herberts P, Malchau H. Hydroxyapatite and tricalcium phosphate-coated cups with and without screw fixation: a randomized study of 64 hips. J Arthroplasty 2000; 15(4): 405-12. doi: 10.1054/arth.2000.2963. [DOI] [PubMed] [Google Scholar]
- 62.Thanner J, Kärrholm J, Malchau H, Wallinder L, Herberts P. Migration of press-fit cups fixed with poly-L-lactic acid or titanium screws: a randomized study using radiostereometry. J Orthop Res 1996; 14(6): 895-900. doi: 10.1002/jor.1100140608. [DOI] [PubMed] [Google Scholar]
- 63.Thien T M, Ahnfelt L, Eriksson M, Strömberg C, Kärrholm J. Immediate weight bearing after uncemented total hip arthroplasty with an anteverted stem: a prospective randomized comparison using radiostereometry. Acta Orthop 2007; 78(6): 730-8. doi: 10.1080/17453670710014491. [DOI] [PubMed] [Google Scholar]
- 64.Thien T M, Thanner J, Kärrholm J. Fixation and bone remodeling around a low-modulus stem: seven-year follow-up of a randomized study with use of radiostereometry and dual-energy X-ray absorptiometer. J Arthroplasty 2012; 27(1): 134-42. e1. doi: [DOI] [PubMed] [Google Scholar]
- 65.Thoen P S, Nordsletten L, Pripp A H, Röhrl S M. Results of a randomized controlled trial with five-year radiostereometric analysis results of vitamin E-infused highly crosslinked versus moderately crosslinked polyethylene in reverse total hip arthroplasty. Bone Joint J 2020; 102-b(12): 1646-53. doi: 10.1302/0301-620x.102b12.Bjj-2020-0721.R1. [DOI] [PubMed] [Google Scholar]
- 66.Tsikandylakis G, Mortensen K R L, Gromov K, Troelsen A, Malchau H, Mohaddes M. The use of porous titanium coating and the largest possible head do not affect early cup fixation: a 2-year report from a randomized controlled trial. JB JS Open Access 2020; 5(4). doi: 10.2106/jbjs.Oa.20.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.von Schewelov T, Sanzén L, Onsten I, Carlsson A. Catastrophic failure of an uncemented acetabular component due to high wear and osteolysis: an analysis of 154 omnifit prostheses with mean 6-year follow-up. Acta Orthop Scand 2004; 75(3): 283-94. doi: 10.1080/00016470410001213. [DOI] [PubMed] [Google Scholar]
- 68.von Schewelov T, Sanzén L, Onsten I, Carlsson A, Besjakov J. Total hip replacement with a zirconium oxide ceramic femoral head: a randomised roentgen stereophotogrammetric study. J Bone Joint Surg Br 2005; 87(12): 1631-5. doi: 10.1302/0301-620x.87b12.16873. [DOI] [PubMed] [Google Scholar]
- 69.Zhou Z K, Li M G, Börlin N, Wood D J, Nivbrant B. No increased migration in cups with ceramic-on-ceramic bearing: an RSA study. Clin Orthop Relat Res 2006; 448: 39-45. doi: 10.1097/01.blo.0000223999.10389.c9. [DOI] [PubMed] [Google Scholar]
- 70.Aspenberg P, Wagner P, Nilsson K G, Ranstam J. Fixed or loose? Dichotomy in RSA data for cemented cups. Acta Orthopaedica 2008; 79(4): 467-73. doi: 10.1080/17453670710015445. [DOI] [PubMed] [Google Scholar]
- 71.Abrahams J M, Callary S A, Munn Z, Jang S W, Huang Q, Howie D W, et al. Acetabular component migration measured using radiostereometric analysis following revision total hip arthroplasty: a scoping review. JBJS Rev 2020; 8(4): e0170. doi: 10.2106/jbjs.Rvw.19.00170. [DOI] [PubMed] [Google Scholar]
- 72.Valstar E R, Gill R, Ryd L, Flivik G, Börlin N, Kärrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005; 76(4): 563-72. doi: 10.1080/17453670510041574. [DOI] [PubMed] [Google Scholar]
- 73.de Vries L M, van der Weegen W, Pilot P, Stolarczyk P A, Sijbesma T, Hoffman E L. The predictive value of radiostereometric analysis for stem survival in total hip arthroplasty: a systematic review. Hip Int 2014; 24(3): 215-22. doi: 10.5301/hipint.5000102. [DOI] [PubMed] [Google Scholar]
- 74.Finnilä S, Löyttyniemi E, Aro H T. Denosumab in cementless total hip arthroplasty: multivariate reanalysis of 3D femoral stem migration and the influence on outliers. JBMR Plus 2022; 6(2): e10588. doi: 10.1002/jbm4.10588. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


