Abstract
Falls and osteoporotic fractures are a major public health problem, particularly among older adults. A third of individuals aged 65 years and over fall at least once each year, with up to 20 % of these resulting in serious injury, including fracture. In conjunction with regular exercise, the importance of diet for musculoskeletal health has largely focused upon calcium, vitamin D, and protein, particularly in the context of preventing falls and fractures. Whilst there is evidence for the benefits of these nutrients for musculoskeletal health, other aspects of the diet remain largely underexplored. For example, vegetables are rich sources of macro- and micronutrients that are essential for muscle function and bone health, which are key factors in the prevention of falls and fractures. Recent work has highlighted the importance of nutrients such as vegetable-derived nitrate and vitamin K1 in optimising muscle strength, physical function, and bone quality. In the context of dietary patterns, vegan/plant-based diets have recently gained popularity due to perceived health benefits, animal welfare, or to tackle climate change. The elimination and/or substitution of animal-based products for plant foods (without careful planning and/or expert dietary guidance) could, however, have long-term negative musculoskeletal consequences; a trend uncovered by recent evidence. Within the overarching theme of nutrition for fall and fracture prevention in older populations, the aim of this review is to (i) summarise the current evidence for calcium, vitamin D and protein; (ii) describe the importance of vegetables and selected nutrients, such as nitrate and vitamin K1, for muscle function and bone structural integrity; and (iii) highlight current evidence around different dietary patterns (e.g., plant-based, diet quality, data driven approaches) and their impact on musculoskeletal health.
Keywords: Diet, Bone, Muscle strength, Physical function, Osteoporosis, Vitamin K1, Nitrate, Vegetables
Highlights
-
•
Dietary factors beyond vitamin D, calcium and protein benefit muscle and bone
-
•
Vegetable-derived nitrate and vitamin K1 may reduce fall and/or fracture risk.
-
•
Evidence supports a balanced diet (e.g., Mediterranean) for musculoskeletal health.
-
•
Vegan/plant-only diets should be carefully planned to limit fracture risk.
1. Introduction
There are physiological decreases in muscle function and bone strength with age. In conjunction with other risk factors (e.g., compromised vision, chronic disease) this contributes towards an individual's propensity to fall and fracture (Montero-Odasso et al., 2022; Ambrose et al., 2013). Close to a third of individuals aged 65 years and over fall at least once each year, with fracture being a major consequence. It has been estimated that up to 95 % of hip fractures result from falls (Stevens and Olson, 2000). Falls and related injuries are clearly a significant global public health problem (James et al., 2020; Wu et al., 2021), with a large economic burden to healthcare systems. In 2015 in the United States, medical costs attributed to falls among older adults were estimated to be $50 billion, and this number is set to increase over the next decade with an aging population (Florence et al., 2018). Fall-related injuries have serious long-term consequences, including increased disability, loss of independence, reduced quality of life and mortality (James et al., 2020; Wu et al., 2021). There is a clear need to promote primary prevention strategies to support musculoskeletal health across the life-course and reduce the burden and morbidity of falls and fractures in older adults.
Risk factors for falls and fractures are multifactorial, including various modifiable and non-modifiable factors. Notably, low bone mineral density (BMD) is a strong predictor of fracture risk, whilst muscle weakness and reduced physical function increase risk of falls and fractures (Montero-Odasso et al., 2022). Healthy lifestyle behaviours, such as regular exercise and maintaining a well-balanced diet, play an important role in optimising musculoskeletal health (Daly et al., 2014; Rizzoli et al., 2021). There is strong evidence that exercise, specifically resistance and balance exercise, can reduce the risk of falls and fractures (Sherrington et al., 2017; de Souto et al., 2019; Hoffmann et al., 2022). Calcium, vitamin D and protein are often recommended to support bone and muscle health, and there is growing evidence that a wider range of nutrients could also play an important role. The 2022 World Guidelines for Falls Prevention and Management for Older Adults also recommends, in addition to traditional fall assessments, a nutritional assessment, including a review of vitamin D status and protein intake (Montero-Odasso et al., 2022). Less information regarding diet is, however, available in other areas, such as vegetables and their nutrients, and the implication of different dietary patterns for musculoskeletal outcomes. As such, the aim of this review is to (i) summarise the latest evidence for calcium, vitamin D and protein; (ii) describe the importance of vegetables and selected nutrients, such as nitrate and vitamin K1, for musculoskeletal health; and (iii) highlight current evidence around different dietary patterns (e.g., plant-based, diet quality, data driven approaches) and their impact on musculoskeletal health.
2. Vitamin D & calcium
Vitamin D and calcium work together synergistically to promote musculoskeletal health (Ringe, 2012). Vitamin D is essential for the intestinal absorption of calcium, as an active vitamin D metabolite (1,25-dihydroxyvitamin D; 1,25[OH]2D) binds to the vitamin D receptor in the intestinal cell, thereby enabling the active calcium transport from the intestine to the circulation (Lips, 2012). The International Osteoporosis Foundation defines vitamin D deficiency and insufficiency as a circulating vitamin D (25OHD) level of <50 nmol/l (<20 ng/ml) and 50 to 74 nmol/l (20–29 ng/ml) (International Osteoporosis Foundation, 2023). This is supported by the Institute of Medicine indicating that 25OHD levels above 50 nmol/l would protect 97.5 % of the population against adverse musculoskeletal outcomes such as falls and fractures (Institute of Medicine, 2010). Notably, both the Endocrine Society and the International Osteoporosis Foundation recommend targeting a higher circulating 25OHD level of 75 nmol/l in older adults (Dawson-Hughes et al., 2010; Holick et al., 2011). The recommended daily intake (RDI) for vitamin D and calcium are 600–800 IU (15–20 μg) (Holick et al., 2011; Lips et al., 2010) and 1000–1200 mg (Lips et al., 2010; Cormick and Belizán, 2019) for older adults. Dietary vitamin D only accounts for ∼10–20 % of 25OHD, with the majority (∼80–90 %) being generated via endogenous skin synthesis resulting from direct sun exposure (Herrmann et al., 2017). Consequently, the amount of dietary vitamin D required likely differs based upon sun exposure due to geographic location and can also be influenced by seasonal changes (summer vs. winter) and skin pigmentation. Specifically, melanin pigment reduces the ultraviolet radiation available for 25OHD synthesis in the skin. In terms of sex differences, studies regarding differences in 25OHD levels between males and females are inconsistent, and are most likely influenced by geographic location (Wierzbicka and Oczkowicz, 2022). When considering the RDI for calcium, this can easily be achieved by consuming a cup of milk (∼276 mg) and yoghurt (∼338 mg), with half a cup (∼60 g) of cheese (∼438 mg) each day. Comparatively, a single 75 g serve of vegetables would provide substantially less calcium. For example, one serve of spinach, kale and broccoli provide ∼108 mg, ∼41 mg or ∼ 30 mg of calcium. Of importance, yoghurt, milk, tofu and Chinese cabbage (Bok Choy) represent good sources of calcium with higher absorption rates, as described in detail (Titchenal and Dobbs, 2007).
Suboptimal circulating 25OHD may have an indirect impact on bone by contributing to a reduction in absorption of ingested calcium, which, in turn, can result in low serum calcium levels. Such events may elicit an increase in parathyroid hormone (PTH) secretion, which acts to regain calcium homeostasis by resorbing mineralised bone (Ringe, 2012). Over time, this can lead to reduced bone mineral density (BMD) as bone formation is unable to equal rates of resorption, thus increasing the risk of osteoporosis and fractures (Lips et al., 2010; Ceglia and Harris, 2013). Adequate circulating 25OHD and calcium levels are not only important for bone health, but also play an important role in muscle physiology and function (see Lewis et al., 2019 for review). Vitamin D insufficiency is associated with impairments in physiological and neuropsychological function thus affecting muscle strength, balance and function, all of which increase the risk of falls in older adults (Ceglia and Harris, 2013; Bischoff-Ferrari, 2009; Bischoff-Ferrari, 2012; Pfeifer et al., 2002; Remelli et al., 2019). Vitamin D supplementation is a common strategy to improve 25OHD status, but the greatest benefits for muscle function appear to be in deficient persons (25OHD <40 nmol/l), with a lack of benefit in those with sufficient 25OHD (≥75 nmol/l) (Dawson-Hughes, 2017). This is an important consideration when interpretating nutrition-related interventions, where the greatest (or any) benefits are likely to be observed when intake is inadequate, or a deficiency exists. Nutritional supplementation is unlikely to result in further improvements once RDIs are met and maintained.
The importance of maintaining adequate 25OHD was also demonstrated in 1348 community-dwelling older women (∼75 years of age) from Western Australia (latitude 32°S, which is typically associated with higher sun exposure). Circulating 25OHD of ≥75 nmol/l, independent of total daily calcium intake, was associated with better physical function (6 % faster timed-up-and-go [TUG]), higher hip and femoral neck BMD (3.3 % and 3.9 %), as well as a lower risk for a fall (24 %) (Sim et al., 2021a) and fracture (30 %) that required hospitalization (Zhu et al., 2019), compared to women with low 25OHD (<50 nmol/l). In addition to attaining adequate sun exposure, this highlights the benefit of consuming whole foods rich in vitamin D and calcium (e.g., dairy products) for musculoskeletal health (Li et al., 2021). This is supported by a recent dairy supplementation cluster randomised controlled trial reporting lower fall (11 %) and fracture (33 %) risks in 7920 adults (68 % female, mean age ∼ 86 years) residing across 60 aged-care facilities over two years (Iuliano et al., 2021). The additional supplementation of dairy through milk, yoghurt and cheese ensured residents attained a total daily intake of ∼1142 mg of calcium and 69 g (1.1 g/kg body weight) of protein. Further, a Bayesian meta-analysis including nine studies reported that compared to those consuming dairy products, individuals following a vegan diet had 6 % (95 % CI 2–9 %) lower BMD at the hip and spine (which we discuss in subsequent sections) (Ho-Pham et al., 2009). This effect on BMD was more pronounced among vegans than among vegetarians who consume dairy and eggs (Ho-Pham et al., 2009). To this end, a whole foods approach should be promoted where possible as it provides other nutrients such as protein that is found in many vitamin D and calcium-rich foods (dairy, eggs, oily fish, etc.) (Geiker et al., 2020); a factor often overlooked in single (often pharmaceutical) nutrient trials.
3. Protein
In addition to calcium and vitamin D, protein has been established as an important contributor to musculoskeletal health (Iuliano et al., 2021; Deutz et al., 2014). Well recognised for its effects on muscle, protein has also been shown to be important for bone health (Kagawa et al., 1980; Kerstetter et al., 2011). Dietary protein intake guidelines globally typically recommend adults consume 0.8–1.0 g/kg body weight daily (United States Department of Agriculture (USDA) and United States Department of Health and Human Services, 2020; National Health and Medical Research Council, 2006; World Health Organisation, 2007), although it is becoming increasingly clear that older adults require a higher amount (∼1.0–1.5 g/kg/day) to help optimally preserve muscle (Deutz et al., 2014; Bauer et al., 2013; Volpi et al., 2013).
Several recent systematic reviews and meta-analyses have reported on the association between or effects of dietary protein intake on BMD and fracture risk in healthy adults (Darling et al., 2019; Darling et al., 2009; Shams-White et al., 2017; Wallace and Frankenfeld, 2017; Wu et al., 2015). These analyses reported that protein intake was positively associated with BMD for nearly all bone sites (Darling et al., 2009; Shams-White et al., 2017), was inversely associated with hip fracture risk (11–16 %) (Wallace and Frankenfeld, 2017; Wu et al., 2015), or had no association with lumbar spine or femoral neck BMD or osteoporotic fracture risk (Darling et al., 2019). Notably, none of these analyses suggest any detrimental effects on bone health, at least within the protein intakes of studies included (typically up to ∼1.4 g/kg/day or 110 g/day). It is important to note that the studies included in these meta-analyses varied widely in terms of the protein intake of participants, the units used to describe protein intake (e.g., absolute grams per day, relative to body weight, percentage of daily energy intake), as well as the way data was analysed (e.g., protein intake as a continuous variable, comparing categories of protein intake), which limits clear interpretation about optimal protein requirements for bone health and fracture prevention.
Positive effects of dietary protein on bone outcomes appear to be dependent upon having sufficient calcium intake (Sahni et al., 2010; Dargent-Molina et al., 2008; Dawson-Hughes and Harris, 2002). Among 3656 men and women (mean age 55 years) from the Framingham Offspring Cohort, those with the highest tertile of animal protein intake (median 60 g/day) had an 85 % lower hip fracture risk compared with the lowest tertile (median 34 g/day; HR 0.15, 95 % CI 0.02–0.92) when calcium intake was high (≥800 mg/day), but 184 % higher risk of hip fracture (HR 2.84, 95 % CI 1.20–6.74) when calcium intake was low (<800 mg/day) (Sahni et al., 2010). In 36,217 postmenopausal women from the E3N cohort study, a higher fracture risk was shown for the highest quartile of total dietary protein intake (>1.71 g/kg/day; RR 1.46, 95 % CI 1.03–2.06) compared to the lowest quartile (<1.15 g/kg/day), but only when combined with low calcium intake (lowest quartile; <749 mg/day) (Dargent-Molina et al., 2008). A 3-year randomised controlled trial comparing calcium citrate malate and vitamin D supplementation to placebo in 342 older adults (≥65 years of age) partially supports these findings (Dawson-Hughes and Harris, 2002). The primary analyses reported a significant interaction between treatment group (supplement or placebo) and protein intake for total body BMD, but not femoral neck or lumbar spine BMD. Within the supplemented group, participants in the highest tertile of protein intake (20.1 % of total energy intake) had a greater positive change in femoral neck BMD (∼2.5 % increase) compared with both the lowest (13.8 % of total energy intake) and middle (16.7 % of total energy intake) tertiles (∼0.4 % decrease and ∼ 0.3 % increase, respectively), whereas no such differences were observed within the placebo group. These within-group results should be interpreted with caution given there was no significant interaction at the femoral neck and change in lumbar spine BMD did not show a consistent pattern across protein intake tertiles. Collectively, the literature generally supports the recent results from the dairy supplementation trial (Iuliano et al., 2021) described in the section above.
Protein intake is proposed to directly influence bone by increasing insulin-like growth factor-1 (IGF-1) production (Kerstetter et al., 2011; Darling et al., 2009; Calvez et al., 2012; Dawson-Hughes et al., 2004), which is suggested to promote bone formation by stimulating osteoblast proliferation and differentiation (Darling et al., 2009; Calvez et al., 2012; Siddiqui and Partridge, 2016; Yakar et al., 2018). An increase in IGF-1 with higher protein intake is also suggested to increase circulating 25OHD levels and to suppress PTH, leading to an increase in intestinal calcium absorption and a decrease in bone resorption (Darling et al., 2009; Bonjour, 2016; Conigrave et al., 2008), and may also play a role in osteocytes in mediating the osteogenic response to mechanical stimuli (Yakar et al., 2018). Protein may also act upon bone indirectly via its effects on muscle (Heaney and Layman, 2008; Wolfe, 2006). Given the close anatomical link of bone and muscle, it is suggested that there is an increase in the force exerted on bone by muscle contractions when muscle mass is higher, therefore providing a greater osteogenic stimulus (Wolfe, 2006; Szulc et al., 2005). Furthermore, the inverse association between protein intake and fracture risk may also be in part due to positive effects on muscle outcomes that could reduce the risk of falls (Ambrose et al., 2013; Moreland et al., 2004).
High dietary protein intakes (∼100–180 g/day) can increase urinary calcium excretion and decrease urine pH (Calvez et al., 2012), which has previously been thought to increase bone resorption, according to the acid-ash hypothesis (Calvez et al., 2012; Bonjour, 2013). This has, however, been largely dispelled, with no direct evidence of a detrimental association between protein intake and BMD or fracture risk. In addition, studies using alkalinising diets have not reported any changes in bone related outcomes (Calvez et al., 2012; Bonjour, 2013; Rizzoli et al., 2018). It is now generally accepted that there are no adverse skeletal complications of high protein intakes (typically up to ∼1.5 g/kg/day in most studies), and that the consequences of insufficient dietary protein are likely more severe than those of excessive protein intake (Rizzoli et al., 2018).
Dietary protein-derived essential amino acids provide an anabolic stimulus for muscle protein synthesis (van Vliet et al., 2015a; Witard et al., 2016). It has been reported that higher compared to lower dietary protein intakes (1.2 g/kg/day vs 0.8 g/kg/day) (Houston et al., 2008) and protein supplementation (ranging from 10 to 106 g/day) compared to placebo/no supplementation (Gielen et al., 2021; Wirth et al., 2020), can attenuate age-related declines in lean mass in middle-aged and older adults. Whether dietary protein intake is positively associated with muscle strength and function is less clear, with the evidence to date suggesting benefits may only be observed when combined with resistance exercise training (Gielen et al., 2021; Nunes et al., 2022). Although not the focus of this review, it is critical to acknowledge the importance of exercise, specifically progressive resistance training, for both muscle and bone health (O’Bryan et al., 2022). The greatest musculoskeletal benefits are likely achieved with optimal nutrition (including protein) to support the effects of regular exercise (Daly et al., 2014). In meta-analyses of randomised controlled trials, protein supplementation (typically ranging from 10 to 35 g/day) is shown to enhance resistance-exercise induced gains in lean mass (mean difference 0.3 kg (Morton et al., 2018); standardised mean difference 0.6 (Liao et al., 2017) and one-repetition maximum strength (mean difference 2.5 kg (Morton et al., 2018); standardised mean difference 0.7) among healthy adults (Morton et al., 2018) or older adults specifically (Liao et al., 2017). There is limited evidence, however, investigating the effect of protein intake on falls, with the few prospective studies to date generally reporting that protein intake is not associated with falls (Larocque et al., 2015; Sandoval-Insausti et al., 2019; Zoltick et al., 2011). Higher dietary protein intake (mean 1.31 g/kg/d) has, however, been shown to preserve lean mass more effectively (mean difference 0.45 kg, 95%CI 0.20–0.71) than lower protein intake (mean 0.79 g/kg/day) after energy-restriction induced weight loss in adults over 50 years of age (Kim et al., 2016). Inverse associations have been reported between protein intake and risk of falling among older adults following unintentional weight loss (Sandoval-Insausti et al., 2019; Zoltick et al., 2011).
Differing amino acid profiles in different types of protein are thought to have varying effects on muscle protein synthesis, and subsequently muscle and bone outcomes (van Vliet et al., 2015a; Gilbert et al., 2011). Animal proteins (e.g., dairy, meat, fish, poultry, eggs) contain all essential amino acids, whereas many sources of plant protein (e.g., vegetables, soybeans, grains, nuts) contain insufficient amounts of some, but not all, essential amino acids (van Vliet et al., 2015a; Gilbert et al., 2011). For example, lysine but not methionine content is particularly low in wheat-derived plant proteins, whereas legumes have sufficient lysine but are low in methionine (van Vliet et al., 2015a). Therefore, consuming greater amounts and a wide variety of plant protein sources together can help improve the protein quality of a plant-based meal by providing a more balanced amino acid profile (van Vliet et al., 2015a). Further, the digestion and absorption kinetics appear to be lower in plant protein as compared with animal-based protein (van Vliet et al., 2015b), which have also been suggested to be important for muscle (van Vliet et al., 2015a; Gilbert et al., 2011). The available evidence in middle-aged and older adults does not, however, show any consistent differences in the effect of animal or plant protein on lean mass and muscle strength (Gilbert et al., 2011; Lim et al., 2021), or falls (Larocque et al., 2015; Zoltick et al., 2011). Most intervention studies provided animal protein to their participants, limiting the ability for meta-analyses to compare the effects of animal and plant protein on muscle outcomes (Wirth et al., 2020; Nunes et al., 2022). Whether the effects on bone and fracture differ by protein type also remains unclear. A meta-analysis comparing animal and plant protein for bone outcomes in healthy adults reported no differences between protein type on BMD at any site, although the quality of evidence was limited, largely due to only 2–4 studies being included in the analysis for each bone site (Shams-White et al., 2018). While sub-group analyses from previous meta-analyses have also consistently shown no differences in the effects of animal and plant protein intakes on bone health outcomes (Darling et al., 2019; Darling et al., 2009; Wallace and Frankenfeld, 2017; Wu et al., 2015), these results are also limited by the small number of included studies reporting outcomes based on protein type. Overall, achieving the total recommended daily protein (1.2–1.5 g/kg) and calcium (1000–1200 mg) intakes from a variety of sources as part of a balanced diet, appears optimal for musculoskeletal health (e.g., BMD, lean mass, fracture risk) in older adults.
4. Vegetables to support muscle and bone health: is nutrient diversity key?
Despite the benefits of greater vegetable intake for cardiovascular health being studied extensively (see Blekkenhorst et al., 2018 for review), its impact upon the musculoskeletal system remains unclear. Recently, this was studied in a cohort of community-dwelling older Australian women (≥70 years, n = 1429). Compared to women with low vegetable intake (<2 serves/day), daily consumption of ≥3 serves/day of vegetables (75 g/serve), specifically of the cruciferous (broccoli, cauliflower, cabbage, Brussel sprouts) and allium (onion, garlic) varieties, was associated with lower risk for an injurious fall (41 %) (Sim et al., 2018a), any fracture (27 %) and hip fracture-related hospitalisations (39 %) (Blekkenhorst et al., 2017) over 14.5 years. Results remained significant after adjusting for a range of lifestyle factors (e.g., smoking, physical activity, socioeconomic status, diet quality). Furthermore, higher vegetable consumption (≥3 serves/day) was associated with 31 % lower odds for both weak grip strength (<22 kg) and slow TUG (Sim et al., 2018a). Another interesting finding was that vegetable diversity (per increase in one different vegetable/day) was associated with between 8 % and 9 % lower risk for an injurious fall and fracture, respectively (Sim et al., 2018b), with the greatest benefit observed in women with habitually low vegetable intake (e.g., <165 g/day equating to <2.2 serves/day) (Sim et al., 2018b).
The aforementioned data suggests that consuming a diverse range of vegetables is likely to be most beneficial for health (see Blekkenhorst et al., 2018 for review). Further, synergistic effects likely exist between nutrients obtained from vegetables. For example, green leafy vegetables (e.g., kale, spinach) are a rich source of non-heme iron and vitamin C, with the latter known to facilitate iron absorption (Heffernan et al., 2017). This is especially important, since iron deficiency anemia is a known risk factor for poor muscle function (Neidlein et al., 2021) and low trauma fractures often associated with osteoporosis (Lee et al., 2019). This should be considered when interpreting results from clinical trials adopting single nutrient interventions, as opposed to a whole foods approach. For reference, a successful whole foods approach was recently demonstrated in the previously discussed multicentre trial reporting lower falls (11 %) and fracture (33 %) rates among older aged residential care residents through the provision of additional dairy-based foods (e.g., milk, yoghurt and cheese) (Iuliano et al., 2021). Numerous studies have reported that lower vegetable intake, assessed by circulating carotenoid levels, were independently associated with impaired muscle strength and the development of walking disability (for a mini-review of these studies, please see Semba et al., 2007). Potential mechanisms include the impact carotenoids may have on fatty acid metabolism, dysregulation of mitochondrial ATP production, increased production of reactive oxygen species, and telomere shortening (see Bartali and Semba, 2021 for review). In-vivo evidence also indicates that glucosinolates, such as sulforaphane, which are commonly found in allium and cruciferous vegetables, are important when considering muscle function (e.g., muscular dystrophy,) and bone strength in older adults (see Connolly et al., 2021 for review). This raises an important question as to what other nutrients within vegetables might contribute towards musculoskeletal health. It is beyond the scope of this review to provide a detailed discussion of all vegetable-derived nutrients linked to musculoskeletal health, instead we focus upon the emerging evidence around dietary vitamin K and nitrate, as they are primarily found in the cruciferous and green leafy vegetables that have been favourably linked to musculoskeletal health (Sim et al., 2018a; Blekkenhorst et al., 2017).
4.1. Nitrate
Since the discovery of the nitrate-nitrite-NO pathway, medical research has typically studied nitrate for its benefits relating to cardiovascular health (see Khatri et al., 2017 for review). This is supported by studies reporting that acute beetroot juice supplementation improves endothelial function (Lara et al., 2016), whilst higher habitual dietary nitrate intake, especially from vegetables (e.g., spinach, kale, arugula, beet root) has been associated with up to 37 % lower incidence of cardiovascular-related mortality (Liu et al., 2019). In 2007, nitrate was first shown to improve the oxygen costs associated with a submaximal cycling task (Larsen et al., 2007). Since then, a plethora of research in this area has emerged, with the performance benefits of nitrate supplements being recognised (Peeling et al., 2018), including by the International Olympic Committee (Maughan et al., 2018). Although the exact mechanism responsible for these benefits remains unclear, nitrate's influence on enhancing physical performance may include greater contractile efficiency, greater perfusion and/or oxygenation and improved mitochondrial function of the skeletal muscle (Jones et al., 2018). It has also been suggested that higher nitrate intake enhances nitric oxide production, thereby improving endothelial function (e.g., vasodilation), thus facilitating transport and uptake of oxygen by the muscle (see Jones et al., 2018 for review). Unsurprisingly, the benefits to muscle strength and power have led to nitrate being studied in older and clinical populations with some positive results (Coggan et al., 2015a; Coggan et al., 2015b; Haider and Folland, 2014).
When considering clinical populations, such as those with heart failure, a detailed review reported mixed findings for the potential benefits for nitrate supplements on the vasculature and physical performance (Ferguson et al., 2021). Nevertheless, in a small clinical trial that included heart failure patients (n = 9, mean age 57 years), high dosage acute beetroot juice supplementation (approximately 700 mg of nitrate) resulted in increased peak knee extensor power (∼10 %) and knee extension velocity (∼12 %) (Coggan et al., 2015b). Similarly, faster knee extension velocity (11 %) and power (6 %) was reported after providing the same beetroot juice supplement to 12 healthy middle-aged adults (Coggan et al., 2015a). Although these studies provide proof of concept for the benefits of acute nitrate supplements on muscle function, the dosages adopted were large and are typically unattainable through diet alone. Specifically, beetroot juice supplements provide ∼5–6 times the levels of nitrate typically ingested as part of a usual diet (Zhong et al., 2022).
In 2019, Sim et al. (2019) were the first to report greater hand grip strength and faster TUG performance in community-dwelling older women (n = 1429, ≥70 years) with higher habitual dietary nitrate intake, coming predominantly from vegetables. In this cross-sectional study, women in the highest tertile of nitrate intake (>84 mg/day) had 35 % and 28 % lower odds for weak grip strength (<22 kg) and slow TUG (>10.2 s) compared to those with the lowest nitrate intake (tertile 1, <65 mg/day). This is especially relevant because compromised grip strength and TUG are well established risk factors for injurious falls (Sim et al., 2019) and mortality (Sim et al., 2018d). Subsequently, when nitrate intake was assessed over 12 years in another cohort of 3759 healthy adults (aged 25-85 years, 44 % male), individuals with the highest nitrate intake (tertile 3, median ~90 mg/day), had 11 % (2.6 kg) stronger knee extension strength and 4% (0.24 s) faster TUG performance, compared to those with the lowest intake (tertile 1, 47 mg/day), irrespective of physical activity status or sex (Sim et al., 2021b). Most importantly, such nitrate intakes can easily be attained by consuming a daily serve (one cup, 75 g) of raw spinach (providing ∼135 mg of nitrate), arugula (∼362 mg), or lettuce (∼154 mg) (Zhong et al., 2022).
Meta-analyses of double-blinded placebo controlled, randomised crossover experiments (with low bias for selection/detection and performance) in healthy adults have also reported benefits for nitrate supplements (e.g., beet root juice) on the contractile properties of skeletal muscle, with a small improvement in peak (n = 8 studies, SMD = 0.25, p = 0.030) and mean power output (n = 6 studies, SMD = 0.28, p = 0.034) (Esen et al., 2022). When studied at an individual patient level in healthy adults (19 studies, 268 participants, 81.3 % male), approximately 5 % increased maximal muscle power after nitrate supplementation has also been reported (Coggan et al., 2021). Evidence also exists for the benefits of organic nitrates (used to treat angina) to be associated with lower odds for fractures (11 %) and hip fractures (15 %) in a pharmaco-epidemiological case-control study comprising of 124,655 Danish individuals (median [IQR] age, 42 [17–68] years) who had sustained a fracture in a year (cases) as well as 373,962 age- and sex-matched controls (Rejnmark et al., 2006). Contradictory results have, however, also been reported when considering organic nitrate, BMD and fractures (Golchin et al., 2016; Jamal et al., 2013; Pouwels et al., 2010). To our knowledge, no study has examined the relationship between higher habitual dietary nitrate intake, BMD, muscle function, falls and fracture risk; making this relevant for further investigation.
4.2. Vitamin K
Over the last decade, vitamin K has gained considerable attention for its potential role in musculoskeletal health (Alonso et al., 2022). Previously, vitamin K was primarily considered for its role in coagulation, and inadequate vitamin K intake has been linked with cardiovascular disease (see Palmer et al., 2020 for review). Vitamin K exists in two main forms, vitamin K1 (phylloquinones), found primarily in vegetables (especially green leafy and cruciferous varieties, including their oils), and vitamin K2 (menaquinones 4–13), found primarily in animal products (e.g., dairy, cheese, eggs and meat) (Palmer et al., 2021). About 90 % of total vitamin K intake comes from vitamin K1 (Schurgers and Vermeer, 2000). As reviewed in detail previously (Palmer et al., 2020), the bioavailability of vitamin K1 from cooked vegetables is reported to be quite low (up to 10 %), increasing slightly in the presence of dietary lipids. In contrast, vitamin K1 absorption from oils is much higher. Long-chain vitamin K2 (MK-7, MK-8, and MK-9) have higher bioaccessibility and absorption rates (close to 100 %) from dietary sources such as natto, cheese, and egg yolk, and have a longer half-life than K1 and MK-4 (Akbari and Rasouli-Ghahroudi, 2018). Whilst there is ambiguity regarding which form of vitamin K (K1 vs. K2) is most beneficial for health (Halder et al., 2019), for this section we will focus upon vitamin K1, keeping with the theme around vegetables for musculoskeletal health.
Currently, the National Institute of Health highlights uncertainty regarding the benefits of vitamin K for fracture prevention (National Institue for Health, 2021), although pharmaceutical vitamin K2 has been approved in Japan for the treatment of osteoporosis since 1995 (Orimo et al., 2012); despite concerns having been raised regarding the scientific integrity of vitamin K supplementation trials in this area (Kupferschmidt, 2018). Of note, a meta-analysis of 19 randomised controlled trials (n = 6759 participants) reported no benefits of vitamin K2 supplementation on BMD and vertebral fractures in women (Huang et al., 2015). However, in subgroup analysis comprising post-menopausal or osteoporotic women, lower risk for presenting with any clinical fracture was evident. Of importance, this meta-analysis included large pharmaceutical dosages of vitamin K2, which differs substantially to a multi-nutrient whole foods approach, whilst also indicating between-study heterogeneity, small sample sizes and selection bias. Vitamin K is known to play a vital role in the γ-carboxylation of osteocalcin (OC), a vitamin K dependant protein (VKDP) associated with bone integrity, that is produced by osteoblasts (Sim et al., 2020). Consequently, the ratio of undercarboxylated OC to total OC (ucOC:tOC) is considered a biomarker for vitamin K status. A lower ucOC:tOC is associated with higher dietary vitamin K intake (Sim et al., 2020). Smith et al. (2021) previously reported that higher ucOC:tOC (>0.47), indicating poorer vitamin K status, was associated with a 31 % greater risk for an injurious fall in older women (n = 1261, mean age ∼ 75 years). Higher ucOC:tOC was also associated with greater fear of falling and poorer TUG, including its 5-year decline. Other VKDP's, such as higher desphospho-uncarboxylated matrix Gla protein (de-ucMGP, approximately >270 pmol/l), have also been implicated in lower grip strength (by 1.1 kg) and smaller calf circumference (by 0.5 cm) (van Ballegooijen et al., 2018), as well as between 62 and 75 % greater odds for frailty risk over 13 years (Machado-Fragua et al., 2020). Collectively, these data suggest vitamin K supports musculoskeletal health.
Despite the importance of the aforementioned findings, the optimal amount of vitamin K (or form) to support the carboxylation of VKDP remains unclear. Recent work has demonstrated a linear relationship between dietary vitamin K1, primarily derived from vegetables, and ucOC:tOC (Sim et al., 2022), and that higher vitamin K1 intakes were associated with lower hazards for an injurious fall (Sim et al., 2023), fracture and hip fracture (Sim et al., 2022) in older women (n = 1348, mean age 75 years). Most importantly, a nadir in the relative hazards for both falls and fractures was uncovered with intakes of ≥100 μg/day of vitamin K1. Specifically, compared to women with the lowest intakes (quartile 1, 60 μg/day), those with the highest intakes (>100 μg/day) had approximately 27 % and 49 % lower hazards for a fall and hip fracture, respectively. These data were independent of lifestyle factors (diet quality, smoking, physical activity) and circulating vitamin D status (plasma 25OHD) (Sim et al., 2022; Sim et al., 2023). Of interest, no relationship between vitamin K2 and falls was recorded. Collectively, these are important findings that support current vitamin K nutrition guidelines in the USA promoting vitamin K intakes of approximately 90 and 120 μg/day for women and men (United States Department of Agriculture USDA, 2015). Comparable findings have been reported in older Norwegian individuals, where low vitamin K1 intake (<53 μg/day) was associated with 57 % greater hazard for a hip fracture over ∼10 years, compared to those with higher intakes (>109 μg/day) (Apalset et al., 2011). Similar results have been reported from the Framingham Heart Study (n = 888, mean age ∼ 75 years, 62.2 % women) (Booth et al., 2000) and the Nurses Health Study (n = 72,327 women, aged 38–63 years) (Feskanich et al., 1999), but not in a cohort of Chinese individuals (≥65 years, 55.5 % male), possibly due to the low fracture incidence (e.g., hip fractures ∼1.6 %) and/or very high median intake of vitamin K1 (∼240 μg/day) (Chan et al., 2012). The aforementioned benefits are supported by a meta-analysis reporting higher vitamin K1 intake was associated with 22 % lower fracture risk (n = 80,982, highest vs. the lowest intake, RR 0.78 95 % CI 0.56–0.99; I2 = 59.2 %, p-heterogeneity = 0.04).
To this end, consuming a minimum of one to two serves per day (75–150 g/day) of vitamin K1-rich vegetables, especially those of the green leafy and cruciferous varieties, would be an effective strategy to meet daily vitamin K1 intakes of >100 μg/day (Palmer et al., 2021). Whilst the form of vitamin K (K1 vs. K2) for musculoskeletal health remains less clear, public health messaging should consider the well-established health benefits associated with higher vegetable intake. Specifically, any messages around vitamin K nutrition should promote its intake through healthy foods, such as vegetables, which are often lacking in the typical Western diet. From this perspective, promoting vegetable consumption to support adequate vitamin K nutrition appears as a preferable choice.
5. Dietary patterns and musculoskeletal health: an underestimated strategy for fall and fracture prevention?
Healthy diets are nutrient-dense, which can play a role in limiting any age-induced loss of bone and muscle, thereby decreasing the risk of sarcopenia and osteoporosis, which are key risk factors for falls and fracture (Warensjö Lemming and Byberg, 2020). Studying dietary patterns is important, as they encompass the physiological effects of several foods and nutrients beyond calcium, vitamin D and protein acting independently and/or synergistically on musculoskeletal health (Webster et al., 2021). This section discusses the evidence on plant-based diets, diet quality indices, and finally data-derived dietary patterns, in-relation to musculoskeletal health.
5.1. Plant-based diets
Plant-based diets are becoming more widely adopted in developed countries due to potential health benefits, as well as for environmental and ethical reasons (Stewart et al., 2021). Whilst it is common for fruits and vegetables to be linked to better health outcomes, animal-based products, such as meat and dairy, are abundant in several nutrients related to bone and/or muscle health; their omission could negatively impact musculoskeletal health (Chan et al., 2021a). Similarly, vegetarian diets can vary widely from person to person and can be nutrient-dense or nutrient deficient, just like diets that include animal products (Gallagher et al., 2022). Recent epidemiological evidence suggests poorer musculoskeletal health in vegetarians (meat- and fish-free diets) and vegans (diets free of any product derived from animals), with consistent prospective evidence demonstrating that such diets are associated with a higher risk of fractures (Tong et al., 2020; Webster et al., 2022; Thorpe et al., 2021). Three recently published, large prospective cohort studies have explored potential differences in fracture risk between vegetarians and meat-eaters, including the Oxford branch of the European Prospective Investigation into Cancer (EPIC-Oxford, UK) (Tong et al., 2020), UK Women's Cohort Study (UKWCS) (Webster et al., 2022), and Adventist Health Study-2 (AHS-2, US) (Thorpe et al., 2021). All three studies predominantly included Caucasian women; were well-powered with between 3818 and 15,499 vegetarians and 679 to 945 confirmed hip fractures (confirmed using hospital records in both UK studies); and had follow-up durations ranging from 8.4 to 22.1 years. Consistent evidence across the three cohorts indicated that ‘strict’ vegetarians were at a greater risk of hip fracture than meat-eaters (17–33 %), though the difference was non-significant in the AHS-2. The magnitude of the risk difference in both UK cohorts was similar after adjustment for potential confounders (UKWCS: 1.33 [1.03, 1.71] and EPIC-Oxford: 1.25 [1.04, 1.50], equivalent to 2.9 [0.9, 5.2] additional hip fractures per 1000 people over 10 years).
The EPIC-Oxford and AHS-2 studies further explored risk differences between vegans and meat-eaters; vegans were at the greatest risk of hip fracture. In the EPIC-Oxford study, the risk difference for vegans versus meat-eaters was 2.30 (1.66, 3.22) for hip fracture, equivalent to 14.9 (7.9, 24.5) additional cases per 1000 people over 10 years. This would indicate a clinically significant risk increase for vegans. The associations reported in these studies are, however, unlikely to be free from residual confounding, healthy participant selection bias, and dietary measurement error, as well as changes in eating patterns over time. The only other study comparing fracture risk between vegetarians, vegans, and meat-eaters was one small prospective study of 210 Vietnamese women (including 105 vegans and 10 fracture cases in total) (Ho-Pham et al., 2012), which reported no significant difference in total fracture incidence between vegans and meat-eaters over two years (Tong et al., 2020).
Mechanisms underpinning potential risk differences are unclear, though a higher risk of all fractures in vegetarians and vegans could be due to poorer musculoskeletal structure (Iguacel et al., 2019a) and function (Chan et al., 2021b) compared to omnivores. Vegetarians and vegans face greater challenges in achieving sufficient intakes of several nutrients important to bone and muscle health, including protein, calcium, vitamin D, and vitamin B12, among other factors that are abundant in animal products (Tucker, 2014; Davey et al., 2003). These nutrients are less abundant and less bioavailable in plants, which reduces digestion and absorption kinetics compared to that of animal-sourced nutrients (van Vliet et al., 2015b). Further, chronic iron deficiency has also been linked to increased risk of osteoporosis (Toxqui and Vaquero, 2015), potentially via altered bone homeostasis (Balogh et al., 2018), and risk of falls (Kim and Kim, 2022). Vegetarians and vegans may consequently have lower body mass index, fat-free mass, fat mass, BMD, and lower IGF-1 levels (Tong et al., 2018; Barnard et al., 2015; Allen et al., 2002), which are each independently associated with a higher risk of fractures (Kim et al., 2018; Gonnelli et al., 2014; Yuan et al., 2021). A meta-analysis of cross-sectional studies reported that among adults over 50 years of age, vegetarians and vegans had lower BMD compared to omnivores, though between-study heterogeneity was high (Iguacel et al., 2019b). There is a paucity of prospective evidence on the topic and it is unclear if differences might be clinically relevant (Iguacel et al., 2019a). Muscle strength and physical function may also differ in those on plant-based versus omnivorous diets (Chan et al., 2021b; Tong et al., 2018), though it is unclear if differences are due to dietary factors, such lower protein intake and/or quality (see section on protein). This warrants further investigation.
More large-scale, long-term prospective cohort studies with repeated diet measurements and access to hospital data are needed to confirm if vegetarians and vegans are at a greater risk of fractures than meat-eaters, particularly in vegans, men, and in non-European populations, for whom there is a lack of research. Further research elucidating factors responsible for potential risk differences is needed given the increasing popularity of these diets, and the growing need to devise public health interventions and policy guidelines to reduce risk of fractures in those on plant-based diets.
5.2. Diet quality indices
Studies have investigated associations between diet quality and fracture risk by assigning scores that reflect adherence to pre-defined diets, based upon foods and nutrients that are considered healthy or unhealthy. To date, a consistent pattern has been shown with increased adherence to the Mediterranean diet (MD) and lower fracture risk (Malmir et al., 2018; Benetou et al., 2018; Jennings et al., 2020; Byberg et al., 2016; Benetou et al., 2013; Haring et al., 2016). The MD is characterised by high intake of olive oil, fruit, vegetables, cereals, legumes, nuts, and oily fish; moderate intake of poultry, eggs, dairy, and red wine; and low intake of red and processed meat and sweets (Davis et al., 2015). The MD can be scored in multiple ways, with the most common being from a 0–9 scale, and higher scores indicating greater adherence. A 2018 meta-analysis of three large cohort studies and a pooling project of eight EPIC-cohorts reported that a 1-unit increase in MD score was associated with a 5 % reduction in hip-fracture risk, with low between-study heterogeneity (HR: 0.95, 95 % CI's: 0.92, 0.98, I2 = 0 %) (Malmir et al., 2018). Similar results are reported in 140,775 European and US adults (≥60 years, n = 5454 hip fractures) where a 2-unit increase in MD score was associated with a 4 % lower risk of hip fracture (Benetou et al., 2018). The EPIC-Norfolk cohort of middle-aged to older adults also reported a lower risk of both total (23 %) and hip fracture risk (21 %) in the highest vs lowest quintile of MD adherence over an average of 17.4 years of follow-up (Jennings et al., 2020).
Benefits between other indices of diet quality and lower risk of fractures have also been reported, but with less consistency across studies than for the MD (Fung et al., 2018; Panahande et al., 2019; Dai et al., 2014; Veronese et al., 2018). A meta-analysis including three cohort studies and a case-control study in the US (Haring et al., 2016; Fung et al., 2018), China (Dai et al., 2014) and Singapore (Zeng et al., 2014), including 6938 incident hip fractures, reported that increased adherence to the alternative healthy eating index (AHEI) was related to lower hip fracture risk (31 % for highest vs lowest adherence comparison) (Panahande et al., 2019). Two large US cohorts showed similar associations between increased adherence to an alternative MD score, the AHEI, and the Dietary Approaches to Stop Hypertension (DASH) score with lower hip fracture risk in women under 75 years, but not in older women or in men (Fung et al., 2018). Inconsistencies in results across studies may be due to variations in both the diet quality index used and in defining its scoring system, which depends upon the study population and available dietary data (Warensjö Lemming and Byberg, 2020). For example, high dairy consumption is considered beneficial in the alternative MD index but is considered harmful in the traditional MD index. As such, an individual with a low calcium intake, may present with a higher traditional MD score, but an unfavourable alternative MD index (Warensjö Lemming and Byberg, 2020; Davis et al., 2015).
Generally, there appears to be a protective role for diet quality on musculoskeletal health, especially when considering hip fractures. Separate meta-analyses (Noori et al., 2022; Coelho-Júnior et al., 2021) concluded that higher MD adherence was associated with higher BMD at various sites, including the hip, lumbar spine, femoral neck, and whole-body; and with walking speed and isometric knee muscle strength, but not handgrip strength, in older adults. This is an important finding as a combination of higher BMD and/or muscle function are likely to substantially reduce the risk of falls and resulting injuries such as fracture. It is important to acknowledge, however, that evidence is limited to small cross-sectional studies. Further investigation through well-powered long-term clinical trials is warranted.
5.3. Data-driven dietary patterns
Observational studies (Fabiani et al., 2019; Rogers et al., 2018; Monma et al., 2010; Langsetmo et al., 2011; Zeng et al., 2013; de Jonge et al., 2017; Warensjö Lemming et al., 2017) have investigated relationships between dietary patterns and fracture risk using a posteriori data-driven approaches, such as principal component or cluster analyses. These methods aim to group foods and/or nutrients consumed together in a specific population into collapsed exposure variables. For example, high intakes of red and processed meat (≥1–2 serves/day) and refined grains (≥2–3 serves/day) may be collapsed into an exposure variable (Fabiani et al., 2019). A systematic review of observational studies investigating data-derived dietary patterns, low BMD and fracture risk in adults (≥ 50 years of age) identified three dietary patterns of importance; (i) Healthy Diet, involving high intakes of fruits and vegetables, fish and seafood, poultry, and wholegrains; (ii) Meat/Western, involving high intakes of red and processed meat, eggs, refined grains, and sweets; and (iii) Milk/dairy, characterised by high intakes of milk and dairy products (Fabiani et al., 2019). Increased adherence to the Healthy Diet was associated with a lower risk of fractures, whilst the opposite was observed with the Western Diet. Both the Healthy and Milk/dairy rich diets were associated with lower risk of low BMD. The Meat/Western diet was linked with lower BMD risk. Similarly, in a cohort of older US men, greater adherence to a prudent dietary pattern (abundant in vegetables, salad, and non-fried fish) attenuated total hip but not femoral neck BMD loss over 4 years; however the Western dietary pattern was not significantly associated with change in BMD (Rogers et al., 2018). Other results also indicate that a healthy diet is associated with lower risk of fractures (Monma et al., 2010; Langsetmo et al., 2011; Zeng et al., 2013; de Jonge et al., 2017; Warensjö Lemming et al., 2017), and increased bone and muscle health (Fabiani et al., 2019; Bloom et al., 2018; Denova-Gutiérrez et al., 2018; Samadi et al., 2021). Another systematic review concluded that healthier data-derived diets may be associated with better muscle mass outcomes and lower declines in muscle strength and physical performance, though the quality of evidence was considered weak and/or inconsistent (Bloom et al., 2018). Future work should examine how these data-driven dietary patterns might be related to falls.
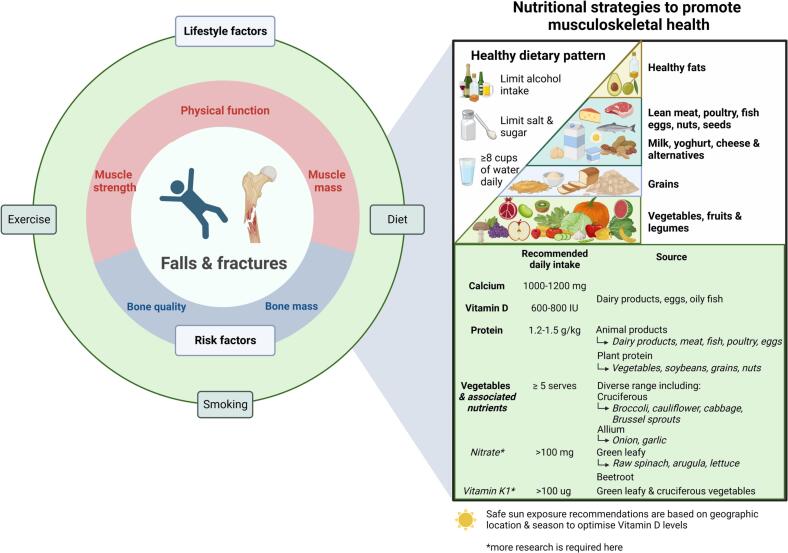
As highlighted consistently in these sections, it is apparent that a balanced diet rich in fruits, vegetables, unprocessed meat as well as oily fish and dairy are likely to best meet the overall nutrient requirements to optimise musculoskeletal health; as summarised in Fig. 1. Most importantly, current evidence suggests that vegetarian and vegan diets (unless carefully planned and ideally supported by a dietician), may not provide adequate amounts of some of the key nutrients (e.g., calcium, protein, vitamin D, vitamin B12, docosahexaenoic acid [DHA]) essential to musculoskeletal health. The message is not that plant-based foods are detrimental, instead an optimal diet includes a combination of plant and animal-based foods consumed in appropriate amounts, specifically an increase in the former and a decrease in the latter. This is particularly relevant in the context of the typical Western diet, which is low in vegetables, representing an area that can be vastly improved to support musculoskeletal health.
Fig. 1.
A conceptual framework based on vegetable-derived nutrients as part of dietary patterns covered in this review highlighting the importance of nutrition to optimise musculoskeletal health for preventing falls and fractures. Lifestyle factors (outer ring) can negatively influence musculoskeletal factors (middle ring) that can contribute to falls and fractures (inner circle). Created with BioRender.com
6. Conclusion
This review highlights the importance of diet in optimising musculoskeletal health for fall and fracture prevention beyond just dietary vitamin D, calcium, and protein; a key message that should be communicated through public health messaging and promoted by clinicians to the community. Current guidelines recommending the consumption of least five serves per day of vegetables, including different varieties (e.g., three colours of vegetables with each meal) are likely to optimise musculoskeletal health. From a public health perspective, the inclusion of one to two serves of green leafy and cruciferous vegetables each day, as part of overall vegetable consumption, likely represents a novel and simple strategy to increase nitrate and vitamin K1 intake, in conjunction with a plethora of other nutrients, to optimise muscle function and bone integrity. The next step could be for clinical trials to determine if habitual consumption of such vegetables is a strategy capable of optimising muscle function to lower fall and fracture risk. Current evidence suggests that vegan (plant-only) diets may be detrimental for musculoskeletal health. The increasing trend for eliminating and/or replacing animal products (e.g., plant-based milk, especially if unfortified, for dairy-based milk) could have long-term negative impacts for muscle and bone that we are yet to fully understand. This would be especially relevant to the diets of teenagers and younger adults (<30 years) as part of the acquisition of peak bone mass and subsequent long-term risk of osteoporosis, an area that warrants further investigation. Therefore, individuals who choose to adopt a vegan/vegetarian diet should carefully consider how they can achieve sufficient intake of key nutrients for musculoskeletal health, ideally under expert guidance (e.g., dietician/nutritionist). Seeking fortified plant-based alternatives could help to improve diet quality. To this end, a balanced diet that includes habitually high intakes of vegetables, in combination with lower amounts of processed and discretionary foods (Fig. 1), comparable to the MD, in conjunction with regular exercise, appears to be the best primary prevention strategy currently available to optimise musculoskeletal health.
CRediT authorship contribution statement
James Webster: Conceptualization, Writing – original draft, Writing – review & editing. Jack Dalla Via: Conceptualization, Writing – original draft, Writing – review & editing. Christina Langley: Writing – original draft, Writing – review & editing, Conceptualization. Cassandra Smith: Conceptualization, Writing – original draft, Writing – review & editing. Craig Sale: Conceptualization, Writing – original draft, Writing – review & editing. Marc Sim: Conceptualization, Writing – original draft, Writing – review & editing.
Declaration of competing interest
All authors declare no conflicts of interest specific to the completion of this article. Craig Sale has, however, received honoraria from the Dairy Council UK the Dairy Council Northern Ireland and nutritional supplement companies to speak at events on topics broadly relevant to the current article.
Acknowledgements
The salary of Marc Sim is supported by a Royal Perth Hospital Research Foundation Fellowship (RPHRF CAF 00/21) and an Emerging Leader Fellowship from the Future Health Research and Innovation Fund (Department of Health, Western Australia). None of the funding agencies had any role in the conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Data availability
No data was used for the research described in the article.
References
- Akbari S., Rasouli-Ghahroudi A.A. Vitamin K and bone metabolism: a review of the latest evidence in preclinical studies. Biomed. Res. Int. 2018;2018 doi: 10.1155/2018/4629383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen N.E., Appleby P.N., Davey G.K., Kaaks R., Rinaldi S., Key T.J. The associations of diet with serum insulin-like growth factor I and its main binding proteins in 292 women meat-eaters, vegetarians, and vegans. Cancer Epidemiol. Biomark. Prev. 2002;11(11):1441–1448. [PubMed] [Google Scholar]
- Alonso N., Meinitzer A., Fritz-Petrin E., Enko D., Herrmann M. Role of vitamin K in bone and muscle metabolism. Calcif. Tissue Int. 2022;1–19 doi: 10.1007/s00223-022-00955-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambrose A.F., Paul G., Hausdorff J.M. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. doi: 10.1016/j.maturitas.2013.02.009. [DOI] [PubMed] [Google Scholar]
- Apalset E.M., Gjesdal C.G., Eide G.E., Tell G.S. Intake of vitamin K1 and K2 and risk of hip fractures: the Hordaland health study. Bone. 2011;49(5):990–995. doi: 10.1016/j.bone.2011.07.035. [DOI] [PubMed] [Google Scholar]
- Balogh E., Paragh G., Jeney V. Influence of iron on bone homeostasis. Pharmaceuticals (Basel) 2018;11(4):107. doi: 10.3390/ph11040107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnard N.D., Levin S.M., Yokoyama Y. A systematic review and meta-analysis of changes in body weight in clinical trials of vegetarian diets. J. Acad. Nutr. Diet. 2015;115(6):954–969. doi: 10.1016/j.jand.2014.11.016. [DOI] [PubMed] [Google Scholar]
- Bartali B., Semba R.D. Carotenoids and Healthy Aging: The Fascination Continues. Oxford University Press; 2021. pp. 259–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer J., Biolo G., Cederholm T., Cesari M., Cruz-Jentoft A.J., Morley J.E., et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE study group. J. Am. Med. Dir. Assoc. 2013;14(8):542–559. doi: 10.1016/j.jamda.2013.05.021. [DOI] [PubMed] [Google Scholar]
- Benetou V., Orfanos P., Pettersson-Kymmer U., Bergström U., Svensson O., Johansson I., et al. Mediterranean diet and incidence of hip fractures in a european cohort. Osteoporos. Int. 2013;24(5):1587–1598. doi: 10.1007/s00198-012-2187-3. [DOI] [PubMed] [Google Scholar]
- Benetou V., Orfanos P., Feskanich D., Michaëlsson K., Pettersson-Kymmer U., Byberg L., et al. Mediterranean diet and hip fracture incidence among older adults: the CHANCES project. Osteoporos. Int. 2018;29(7):1591–1599. doi: 10.1007/s00198-018-4517-6. [DOI] [PubMed] [Google Scholar]
- Bischoff-Ferrari H. Vitamin D: what is an adequate vitamin D level and how much supplementation is necessary? Best Pract. Res. Clin. Rheumatol. 2009;23(6):789–795. doi: 10.1016/j.berh.2009.09.005. [DOI] [PubMed] [Google Scholar]
- Bischoff-Ferrari H.A. Relevance of vitamin D in muscle health. Rev. Endocr. Metab. Disord. 2012;13(1):71–77. doi: 10.1007/s11154-011-9200-6. [DOI] [PubMed] [Google Scholar]
- Blekkenhorst L.C., Hodgson J.M., Lewis J.R., Devine A., Woodman R.J., Lim W.H., et al. Vegetable and fruit intake and fracture-related hospitalisations: a prospective study of older women. Nutrients. 2017;9(5) doi: 10.3390/nu9050511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blekkenhorst L.C., Sim M., Bondonno C.P., Bondonno N.P., Ward N.C., Prince R.L., et al. Cardiovascular health benefits of specific vegetable types: a narrative review. Nutrients. 2018;10(5):595. doi: 10.3390/nu10050595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom I., Shand C., Cooper C., Robinson S., Baird J. Diet quality and sarcopenia in older adults: a systematic review. Nutrients. 2018;10(3) doi: 10.3390/nu10030308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonjour J.P. Nutritional disturbance in acid-base balance and osteoporosis: a hypothesis that disregards the essential homeostatic role of the kidney. Br. J. Nutr. 2013;110(7):1168–1177. doi: 10.1017/S0007114513000962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonjour J.P. The dietary protein, IGF-I, skeletal health axis. Horm. Mol. Biol. Clin. Invest. 2016;28(1):39–53. doi: 10.1515/hmbci-2016-0003. [DOI] [PubMed] [Google Scholar]
- Booth S.L., Tucker K.L., Chen H., Hannan M.T., Gagnon D.R., Cupples L.A., et al. Dietary vitamin K intakes are associated with hip fracture but not with bone mineral density in elderly men and women. Am. J. Clin. Nutr. 2000;71(5):1201–1208. doi: 10.1093/ajcn/71.5.1201. [DOI] [PubMed] [Google Scholar]
- Byberg L., Bellavia A., Larsson S.C., Orsini N., Wolk A., Michaëlsson K. Mediterranean diet and hip fracture in swedish men and women. J. Bone Miner. Res. 2016;31(12):2098–2105. doi: 10.1002/jbmr.2896. [DOI] [PubMed] [Google Scholar]
- Calvez J., Poupin N., Chesneau C., Lassale C., Tomé D. Protein intake, calcium balance and health consequences. Eur. J. Clin. Nutr. 2012;66(3):281–295. doi: 10.1038/ejcn.2011.196. [DOI] [PubMed] [Google Scholar]
- Ceglia L., Harris S.S. Vitamin D and its role in skeletal muscle. Calcif. Tissue Int. 2013;92(2):151–162. doi: 10.1007/s00223-012-9645-y. [DOI] [PubMed] [Google Scholar]
- Chan R., Leung J., Woo J. No association between dietary vitamin K intake and fracture risk in chinese community-dwelling older men and women: a prospective study. Calcif. Tissue Int. 2012;90(5):396–403. doi: 10.1007/s00223-012-9586-5. [DOI] [PubMed] [Google Scholar]
- Chan H.H.L., Ribeiro R., Haden S., Hirani V. Plant-based dietary patterns, body composition, muscle strength and function in middle and older age: a systematic review. J. Nutr. Health Aging. 2021;25(8):1012–1022. doi: 10.1007/s12603-021-1666-7. [DOI] [PubMed] [Google Scholar]
- Chan H., Ribeiro R.V., Haden S., Hirani V. Plant-based dietary patterns, body composition, muscle strength and function in middle and older age: a systematic review. J. Nutr. Health Aging. 2021;25(8):1012–1022. doi: 10.1007/s12603-021-1666-7. [DOI] [PubMed] [Google Scholar]
- Coelho-Júnior H.J., Trichopoulou A., Panza F. Cross-sectional and longitudinal associations between adherence to Mediterranean diet with physical performance and cognitive function in older adults: a systematic review and meta-analysis. Ageing Res. Rev. 2021;70 doi: 10.1016/j.arr.2021.101395. [DOI] [PubMed] [Google Scholar]
- Coggan A.R., Leibowitz J.L., Kadkhodayan A., Thomas D.P., Ramamurthy S., Spearie C.A., et al. Effect of acute dietary nitrate intake on maximal knee extensor speed and power in healthy men and women. Nitric Oxide. 2015;48:16–21. doi: 10.1016/j.niox.2014.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coggan A.R., Leibowitz J.L., Spearie C.A., Kadkhodayan A., Thomas D.P., Ramamurthy S., et al. Acute dietary nitrate intake improves muscle contractile function in patients with heart failure: a double-blind, placebo-controlled, randomized trial. Circ. Heart Fail. 2015;8(5):914–920. doi: 10.1161/CIRCHEARTFAILURE.115.002141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coggan A.R., Baranauskas M.N., Hinrichs R.J., Liu Z., Carter S.J. Effect of dietary nitrate on human muscle power: a systematic review and individual participant data meta-analysis. J. Int. Soc. Sports Nutr. 2021;18(1):1–12. doi: 10.1186/s12970-021-00463-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conigrave A., Brown E., Rizzoli R. Dietary protein and bone health: roles of amino acid-sensing receptors in the control of calcium metabolism and bone homeostasis. Annu. Rev. Nutr. 2008;28:131–155. doi: 10.1146/annurev.nutr.28.061807.155328. [DOI] [PubMed] [Google Scholar]
- Connolly E.L., Sim M., Travica N., Marx W., Beasy G., Lynch G.S., et al. Glucosinolates from cruciferous vegetables and their potential role in chronic disease: investigating the preclinical and clinical evidence. Front. Pharmacol. 2021:2964. doi: 10.3389/fphar.2021.767975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cormick G., Belizán J.M. Calcium intake and health. Nutrients. 2019;11(7):1606. doi: 10.3390/nu11071606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai Z., Butler L.M., van Dam R.M., Ang L.W., Yuan J.M., Koh W.P. Adherence to a vegetable-fruit-soy dietary pattern or the alternative healthy eating index is associated with lower hip fracture risk among Singapore chinese. J. Nutr. 2014;144(4):511–518. doi: 10.3945/jn.113.187955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly R.M., Duckham R.L., Gianoudis J. Evidence for an interaction between exercise and nutrition for improving bone and muscle health. Curr. Osteoporos. Rep. 2014;12(2):219–226. doi: 10.1007/s11914-014-0207-2. [DOI] [PubMed] [Google Scholar]
- Dargent-Molina P., Sabia S., Touvier M., Kesse E., Bréart G., Clavel-Chapelon F., et al. Proteins, dietary acid load, and calcium and risk of postmenopausal fractures in the E3N french women prospective study. J. Bone Miner. Res. 2008;23(12):1915–1922. doi: 10.1359/jbmr.080712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darling A.L., Millward D.J., Torgerson D.J., Hewitt C.E., Lanham-New S.A. Dietary protein and bone health: a systematic review and meta-analysis. Am. J. Clin. Nutr. 2009;90(6):1674–1692. doi: 10.3945/ajcn.2009.27799. [DOI] [PubMed] [Google Scholar]
- Darling A.L., Manders R.J.F., Sahni S., Zhu K., Hewitt C.E., Prince R.L., et al. Dietary protein and bone health across the life-course: an updated systematic review and meta-analysis over 40 years. Osteoporos. Int. 2019;30(4):741–761. doi: 10.1007/s00198-019-04933-8. [DOI] [PubMed] [Google Scholar]
- Davey G.K., Spencer E.A., Appleby P.N., Allen N.E., Knox K.H., Key T.J. EPIC-Oxford: lifestyle characteristics and nutrient intakes in a cohort of 33 883 meat-eaters and 31 546 non meat-eaters in the UK. Public Health Nutr. 2003;6(3):259–269. doi: 10.1079/PHN2002430. [DOI] [PubMed] [Google Scholar]
- Davis C., Bryan J., Hodgson J., Murphy K. Definition of the Mediterranean diet; a literature review. Nutrients. 2015;7(11):9139–9153. doi: 10.3390/nu7115459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson-Hughes B. Vitamin D and muscle function. J. Steroid Biochem. Mol. Biol. 2017;173:313–316. doi: 10.1016/j.jsbmb.2017.03.018. [DOI] [PubMed] [Google Scholar]
- Dawson-Hughes B., Harris S.S. Calcium intake influences the association of protein intake with rates of bone loss in elderly men and women. Am. J. Clin. Nutr. 2002;75(4):773–779. doi: 10.1093/ajcn/75.4.773. [DOI] [PubMed] [Google Scholar]
- Dawson-Hughes B., Harris S.S., Rasmussen H., Song L., Dallal G.E. Effect of dietary protein supplements on calcium excretion in healthy older men and women. J. Clin. Endocrinol. Metab. 2004;89(3):1169–1173. doi: 10.1210/jc.2003-031466. [DOI] [PubMed] [Google Scholar]
- Dawson-Hughes B., Mithal A., Bonjour J.P., Boonen S., Burckhardt P., Fuleihan G.E., et al. IOF position statement: vitamin D recommendations for older adults. Osteoporos. Int. 2010;21(7):1151–1154. doi: 10.1007/s00198-010-1285-3. [DOI] [PubMed] [Google Scholar]
- Denova-Gutiérrez E., Méndez-Sánchez L., Muñoz-Aguirre P., Tucker K.L., Clark P. Dietary patterns, bone mineral density, and risk of fractures: a systematic review and meta-analysis. Nutrients. 2018;10(12) doi: 10.3390/nu10121922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deutz N.E., Bauer J.M., Barazzoni R., Biolo G., Boirie Y., Bosy-Westphal A., et al. Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN expert group. Clin. Nutr. 2014;33(6):929–936. doi: 10.1016/j.clnu.2014.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esen O., Dobbin N., Callaghan M.J. The effect of dietary nitrate on the contractile properties of human skeletal muscle: a systematic review and meta-analysis. J. Am. Nutr. Assoc. 2022:1–12. doi: 10.1080/07315724.2022.2037475. [DOI] [PubMed] [Google Scholar]
- Fabiani R., Naldini G., Chiavarini M. Dietary patterns in relation to low bone mineral density and fracture risk: a systematic review and meta-analysis. Adv. Nutr. 2019;10(2):219–236. doi: 10.1093/advances/nmy073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson S.K., Woessner M.N., Holmes M.J., Belbis M.D., Carlström M., Weitzberg E., et al. Effects of inorganic nitrate supplementation on cardiovascular function and exercise tolerance in heart failure. J. Appl. Physiol. 2021;130(4):914–922. doi: 10.1152/japplphysiol.00780.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feskanich D., Weber P., Willett W.C., Rockett H., Booth S.L., Colditz G.A. Vitamin K intake and hip fractures in women: a prospective study. Am. J. Clin. Nutr. 1999;69(1):74–79. doi: 10.1093/ajcn/69.1.74. [DOI] [PubMed] [Google Scholar]
- Florence C.S., Bergen G., Atherly A., Burns E., Stevens J., Drake C. Medical costs of fatal and nonfatal falls in older adults. J. Am. Geriatr. Soc. 2018;66(4):693–698. doi: 10.1111/jgs.15304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) National Academy of Sciences. Institute of Medicine; Washington, DC: 2010. Dietary Reference Intakes for Calcium and Vitamin D. [Google Scholar]
- International Osteoporosis Foundation . 2023. Nutrition, Vitamin D.https://www.osteoporosis.foundation/health-professionals/prevention/nutrition/vitamin-d Available from. [Google Scholar]
- Fung T.T., Meyer H.E., Willett W.C., Feskanich D. Association between diet quality scores and risk of hip fracture in postmenopausal women and men aged 50 years and older. J. Acad. Nutr. Diet. 2018;118(12):2269–2279. doi: 10.1016/j.jand.2017.11.022. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher C.T., Hanley P., Lane K.E. Pattern analysis of vegan eating reveals healthy and unhealthy patterns within the vegan diet. Public Health Nutr. 2022;25(5):1310–1320. doi: 10.1017/S136898002100197X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geiker N., Mølgaard C., Iuliano S., Rizzoli R., Manios Y., Van Loon L., et al. Impact of whole dairy matrix on musculoskeletal health and aging–current knowledge and research gaps. Osteoporos. Int. 2020;31(4):601–615. doi: 10.1007/s00198-019-05229-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen E., Beckwée D., Delaere A., De Breucker S., Vandewoude M., Bautmans I. Nutritional interventions to improve muscle mass, muscle strength, and physical performance in older people: an umbrella review of systematic reviews and meta-analyses. Nutr. Rev. 2021;79(2):121–147. doi: 10.1093/nutrit/nuaa011. [DOI] [PubMed] [Google Scholar]
- Gilbert J.A., Bendsen N.T., Tremblay A., Astrup A. Effect of proteins from different sources on body composition. Nutr. Metab. Cardiovasc. Dis. 2011;21(Suppl. 2):B16–B31. doi: 10.1016/j.numecd.2010.12.008. [DOI] [PubMed] [Google Scholar]
- Golchin N., Hohensee C., LaCroix A., Gray S.L. Nitrate medications, fractures, and change in bone mineral density in postmenopausal women: results from the Women's Health Initiative. J. Bone Miner. Res. 2016;31(9):1760–1766. doi: 10.1002/jbmr.2838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonnelli S., Caffarelli C., Nuti R. Obesity and fracture risk. Clin. Cases Miner. Bone Metab. 2014;11(1):9–14. doi: 10.11138/ccmbm/2014.11.1.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider G., Folland J.P. Nitrate supplementation enhances the contractile properties of human skeletal muscle. Med. Sci. Sports Exerc. 2014;46(12):2234–2243. doi: 10.1249/MSS.0000000000000351. [DOI] [PubMed] [Google Scholar]
- Halder M., Petsophonsakul P., Akbulut A.C., Pavlic A., Bohan F., Anderson E., et al. Vitamin K: double bonds beyond coagulation insights into differences between vitamin K1 and K2 in health and disease. Int. J. Mol. Sci. 2019;20(4):896. doi: 10.3390/ijms20040896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haring B., Crandall C.J., Wu C., LeBlanc E.S., Shikany J.M., Carbone L., et al. Dietary patterns and fractures in postmenopausal women: results from the Women's Health Initiative. JAMA Intern. Med. 2016;176(5):645–652. doi: 10.1001/jamainternmed.2016.0482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaney R.P., Layman D.K. Amount and type of protein influences bone health. Am. J. Clin. Nutr. 2008;87(5):1567S–1570S. doi: 10.1093/ajcn/87.5.1567S. [DOI] [PubMed] [Google Scholar]
- Heffernan A., Evans C., Holmes M., Moore J. The regulation of dietary iron bioavailability by vitamin C: a systematic review and meta-analysis. Proc. Nutr. Soc. 2017;76(OCE4) [Google Scholar]
- Herrmann M., Farrell C.-J.L., Pusceddu I., Fabregat-Cabello N., Cavalier E. Assessment of vitamin D status–a changing landscape. Clin. Chem. Lab. Med. 2017;55(1):3–26. doi: 10.1515/cclm-2016-0264. [DOI] [PubMed] [Google Scholar]
- Hoffmann I., Kohl M., von Stengel S., Jakob F., Kerschan-Schindl K., Lange U., et al. Exercise and the prevention of major osteoporotic fractures in adults: a systematic review and meta-analysis with special emphasis on intensity progression and study duration. Osteoporos. Int. 2022:1–14. doi: 10.1007/s00198-022-06592-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holick M.F., Binkley N.C., Bischoff-Ferrari H.A., Gordon C.M., Hanley D.A., Heaney R.P., et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011;96(7):1911–1930. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- Ho-Pham L.T., Nguyen N.D., Nguyen T.V. Effect of vegetarian diets on bone mineral density: a bayesian meta-analysis. Am. J. Clin. Nutr. 2009;90(4):943–950. doi: 10.3945/ajcn.2009.27521. [DOI] [PubMed] [Google Scholar]
- Ho-Pham L.T., Vu B.Q., Lai T.Q., Nguyen N.D., Nguyen T.V. Vegetarianism, bone loss, fracture and vitamin D: a longitudinal study in asian vegans and non-vegans. Eur. J. Clin. Nutr. 2012;66(1):75–82. doi: 10.1038/ejcn.2011.131. [DOI] [PubMed] [Google Scholar]
- Houston D.K., Nicklas B.J., Ding J., Harris T.B., Tylavsky F.A., Newman A.B., et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the health, aging, and body composition (Health ABC) study. Am. J. Clin. Nutr. 2008;87(1):150–155. doi: 10.1093/ajcn/87.1.150. [DOI] [PubMed] [Google Scholar]
- Huang Z.-B., Wan S.-L., Lu Y.-J., Ning L., Liu C., Fan S.-W. Does vitamin K2 play a role in the prevention and treatment of osteoporosis for postmenopausal women: a meta-analysis of randomized controlled trials. Osteoporos. Int. 2015;26(3):1175–1186. doi: 10.1007/s00198-014-2989-6. [DOI] [PubMed] [Google Scholar]
- Iguacel I., Miguel-Berges M.L., Gómez-Bruton A., Moreno L.A., Julián C. Veganism, vegetarianism, bone mineral density, and fracture risk: a systematic review and meta-analysis. Nutr. Rev. 2019;77(1):1–18. doi: 10.1093/nutrit/nuy045. [DOI] [PubMed] [Google Scholar]
- Iguacel I., Miguel-Berges M.L., Gómez-Bruton A., Moreno L.A., Julián C. Veganism, vegetarianism, bone mineral density, and fracture risk: a systematic review and meta-analysis. Nutr. Rev. 2019;77(1):1–18. doi: 10.1093/nutrit/nuy045. [DOI] [PubMed] [Google Scholar]
- Iuliano S., Poon S., Robbins J., Bui M., Wang X., De Groot L., et al. Effect of dietary sources of calcium and protein on hip fractures and falls in older adults in residential care: cluster randomised controlled trial. BMJ. 2021;375 doi: 10.1136/bmj.n2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal S., Reid L., Hamilton C. The effects of organic nitrates on osteoporosis: a systematic review. Osteoporos. Int. 2013;24(3):763–770. doi: 10.1007/s00198-012-2262-9. [DOI] [PubMed] [Google Scholar]
- James S.L., Lucchesi L.R., Bisignano C., Castle C.D., Dingels Z.V., Fox J.T., et al. The global burden of falls: global, regional and national estimates of morbidity and mortality from the global burden of disease study 2017. Inj. Prev. 2020;26(Suppl. 2):i3–i11. doi: 10.1136/injuryprev-2019-043286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings A., Mulligan A.A., Khaw K.T., Luben R.N., Welch A.A. A Mediterranean diet is positively associated with bone and muscle health in a non-Mediterranean region in 25,450 men and Women from EPIC-Norfolk. Nutrients. 2020;12(4) doi: 10.3390/nu12041154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A.M., Thompson C., Wylie L.J., Vanhatalo A. Dietary nitrate and physical performance. Annu. Rev. Nutr. 2018;38:303–328. doi: 10.1146/annurev-nutr-082117-051622. [DOI] [PubMed] [Google Scholar]
- de Jonge E.A., Kiefte-de Jong J.C., Hofman A., Uitterlinden A.G., Kieboom B.C., Voortman T., et al. Dietary patterns explaining differences in bone mineral density and hip structure in the elderly: the Rotterdam study. Am. J. Clin. Nutr. 2017;105(1):203–211. doi: 10.3945/ajcn.116.139196. [DOI] [PubMed] [Google Scholar]
- Kagawa Y., Nishimura K., Sato J., Shozawa K., Murakami Y., Iwata H., et al. Omission of breakfast and its effects on the nutritional intake, serum lipids and examination grades of dormitory students. Jpn. J. Nutr. 1980;38(6):283–294. [Google Scholar]
- Kerstetter J.E., Kenny A.M., Insogna K.L. Dietary protein and skeletal health: a review of recent human research. Curr. Opin. Lipidol. 2011;22(1):16–20. doi: 10.1097/MOL.0b013e3283419441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatri J., Mills C.E., Maskell P., Odongerel C., Webb A.J. It is rocket science–why dietary nitrate is hard to ‘beet’! Part I: twists and turns in the realization of the nitrate–nitrite–NO pathway. Br. J. Clin. Pharmacol. 2017;83(1):129–139. doi: 10.1111/bcp.12913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y., Kim J. Relationship between anemia and falls among postmenopausal women in Korea. Int. J. Environ. Res. Public Health. 2022;19(14) doi: 10.3390/ijerph19148242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.E., O'Connor L.E., Sands L.P., Slebodnik M.B., Campbell W.W. Effects of dietary protein intake on body composition changes after weight loss in older adults: a systematic review and meta-analysis. Nutr. Rev. 2016;74(3):210–224. doi: 10.1093/nutrit/nuv065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.H., Yi S.W., Yi J.J., Kim Y.M., Won Y.J. Association between body mass index and the risk of hip fracture by sex and age: a prospective cohort study. J. Bone Miner. Res. 2018;33(9):1603–1611. doi: 10.1002/jbmr.3464. [DOI] [PubMed] [Google Scholar]
- Kupferschmidt K. Tide of lies. Science. 2018;361(6403):636–641. doi: 10.1126/science.361.6403.636. [DOI] [PubMed] [Google Scholar]
- Langsetmo L., Hanley D.A., Prior J.C., Barr S.I., Anastassiades T., Towheed T., et al. Dietary patterns and incident low-trauma fractures in postmenopausal women and men aged ≥ 50 y: a population-based cohort study. Am. J. Clin. Nutr. 2011;93(1):192–199. doi: 10.3945/ajcn.110.002956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara J., Ashor A.W., Oggioni C., Ahluwalia A., Mathers J.C., Siervo M. Effects of inorganic nitrate and beetroot supplementation on endothelial function: a systematic review and meta-analysis. Eur. J. Nutr. 2016;55(2):451–459. doi: 10.1007/s00394-015-0872-7. [DOI] [PubMed] [Google Scholar]
- Larocque S.C., Kerstetter J.E., Cauley J.A., Insogna K.L., Ensrud K., Lui L.Y., et al. Dietary protein and vitamin D intake and risk of falls: a secondary analysis of postmenopausal women from the study of osteoporotic fractures. J. Nutr. Gerontol. Geriatr. 2015;34(3):305–318. doi: 10.1080/21551197.2015.1054574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen F., Weitzberg E., Lundberg J., Ekblom B. Effects of dietary nitrate on oxygen cost during exercise. Acta Physiol. 2007;191(1):59–66. doi: 10.1111/j.1748-1716.2007.01713.x. [DOI] [PubMed] [Google Scholar]
- Lee E.A., Shin D.W., Yoo J.H., Ko H.Y., Jeong S.M. Anemia and risk of fractures in older korean adults: a Nationwide population-based study. J. Bone Miner. Res. 2019;34(6):1049–1057. doi: 10.1002/jbmr.3675. [DOI] [PubMed] [Google Scholar]
- Lewis J.R., Sim M., Daly R.M. The vitamin D and calcium controversy: an update. Curr. Opin. Rheumatol. 2019;31(2):91–97. doi: 10.1097/BOR.0000000000000584. [DOI] [PubMed] [Google Scholar]
- Li S., Xi C., Li L., Long Z., Zhang N., Yin H., et al. Comparisons of different vitamin D supplementation for prevention of osteoporotic fractures: a bayesian network meta-analysis and meta-regression of randomised controlled trials. Int. J. Food Sci. Nutr. 2021;72(4):518–528. doi: 10.1080/09637486.2020.1830264. [DOI] [PubMed] [Google Scholar]
- Liao C.-D., Tsauo J.-Y., Wu Y.-T., Cheng C.-P., Chen H.-C., Huang Y.-C., et al. Effects of protein supplementation combined with resistance exercise on body composition and physical function in older adults: a systematic review and meta-analysis. Am. J. Clin. Nutr. 2017;106(4):1078–1091. doi: 10.3945/ajcn.116.143594. [DOI] [PubMed] [Google Scholar]
- Lim M.T., Pan B.J., Toh D.W.K., Sutanto C.N., Kim J.E. Animal protein versus plant protein in supporting lean mass and muscle strength: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2021;13(2) doi: 10.3390/nu13020661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lips P. Interaction between vitamin D and calcium. Scand. J. Clin. Lab. Invest. 2012;72(sup243):60–64. doi: 10.3109/00365513.2012.681960. [DOI] [PubMed] [Google Scholar]
- Lips P., Bouillon R., Van Schoor N.M., Vanderschueren D., Verschueren S., Kuchuk N., et al. Reducing fracture risk with calcium and vitamin D. Clin. Endocrinol. 2010;73(3):277–285. doi: 10.1111/j.1365-2265.2009.03701.x. [DOI] [PubMed] [Google Scholar]
- Liu A.H., Bondonno C.P., Russell J., Flood V.M., Lewis J.R., Croft K.D., et al. Relationship of dietary nitrate intake from vegetables with cardiovascular disease mortality: a prospective study in a cohort of older australians. Eur. J. Nutr. 2019;58(7):2741–2753. doi: 10.1007/s00394-018-1823-x. [DOI] [PubMed] [Google Scholar]
- Machado-Fragua M.D., Hoogendijk E.O., Struijk E.A., Rodriguez-Artalejo F., Lopez-Garcia E., Beulens J.W., et al. High dephospho-uncarboxylated matrix gla protein concentrations, a plasma biomarker of vitamin K, in relation to frailty: the longitudinal aging study Amsterdam. Eur. J. Nutr. 2020;59(3):1243–1251. doi: 10.1007/s00394-019-01984-9. [DOI] [PubMed] [Google Scholar]
- Malmir H., Saneei P., Larijani B., Esmaillzadeh A. Adherence to Mediterranean diet in relation to bone mineral density and risk of fracture: a systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2018;57(6):2147–2160. doi: 10.1007/s00394-017-1490-3. [DOI] [PubMed] [Google Scholar]
- Maughan R.J., Burke L.M., Dvorak J., Larson-Meyer D.E., Peeling P., Phillips S.M., et al. IOC consensus statement: dietary supplements and the high-performance athlete. Int. J. Sport Nutr. Exerc. Metab. 2018;28(2):104–125. doi: 10.1123/ijsnem.2018-0020. [DOI] [PubMed] [Google Scholar]
- Monma Y., Niu K., Iwasaki K., Tomita N., Nakaya N., Hozawa A., et al. Dietary patterns associated with fall-related fracture in elderly japanese: a population based prospective study. BMC Geriatr. 2010;10:31. doi: 10.1186/1471-2318-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montero-Odasso M., van der Velde N., Martin F.C., Petrovic M., Tan M.P., Ryg J., et al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing. 2022;51(9) doi: 10.1093/ageing/afac205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreland J.D., Richardson J.A., Goldsmith C.H., Clase C.M. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J. Am. Geriatr. Soc. 2004;52(7):1121–1129. doi: 10.1111/j.1532-5415.2004.52310.x. [DOI] [PubMed] [Google Scholar]
- Morton R.W., Murphy K.T., McKellar S.R., Schoenfeld B.J., Henselmans M., Helms E., et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. Br. J. Sports Med. 2018;52(6):376–384. doi: 10.1136/bjsports-2017-097608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health and Medical Research Council . National Health and Medical Research Council; Canberra: 2006. Australian Government Department of Health and Ageing. New Zealand Ministry of Health. Nutrient Reference Values for Australia and New Zealand. [Google Scholar]
- National Institue for Health . 2021. Vitamin K Fact Sheet for Health Professionals. [Google Scholar]
- Neidlein S., Wirth R., Pourhassan M. Iron deficiency, fatigue and muscle strength and function in older hospitalized patients. Eur. J. Clin. Nutr. 2021;75(3):456–463. doi: 10.1038/s41430-020-00742-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noori M., Jayedi A., Khan T.A., Moradi S., Shab-Bidar S. Mediterranean dietary pattern and bone mineral density: a systematic review and dose-response meta-analysis of observational studies. Eur. J. Clin. Nutr. 2022;76(12):1657–1664. doi: 10.1038/s41430-022-01093-7. [DOI] [PubMed] [Google Scholar]
- Nunes E.A., Colenso-Semple L., McKellar S.R., Yau T., Ali M.U., Fitzpatrick-Lewis D., et al. Systematic review and meta-analysis of protein intake to support muscle mass and function in healthy adults. J. Cachexia. Sarcopenia Muscle. 2022;13(2):795–810. doi: 10.1002/jcsm.12922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Bryan S.J., Giuliano C., Woessner M.N., Vogrin S., Smith C., Duque G., et al. Progressive resistance training for concomitant increases in muscle strength and bone mineral density in older adults: a systematic review and meta-analysis. Sports Med. 2022;52(8):1939–1960. doi: 10.1007/s40279-022-01675-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orimo H., Nakamura T., Hosoi T., Iki M., Uenishi K., Endo N., et al. Japanese 2011 guidelines for prevention and treatment of osteoporosis—executive summary. Arch. Osteoporos. 2012;7(1):3–20. doi: 10.1007/s11657-012-0109-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer C.R., Blekkenhorst L.C., Lewis J.R., Ward N.C., Schultz C.J., Hodgson J.M., et al. Quantifying dietary vitamin K and its link to cardiovascular health: a narrative review. Food Funct. 2020;11(4):2826–2837. doi: 10.1039/c9fo02321f. [DOI] [PubMed] [Google Scholar]
- Palmer C.R., Koch H., Shinde S., Blekkenhorst L.C., Lewis J.R., Croft K.D., et al. Development of a vitamin K database for commercially available food in Australia. Front. Nutr. 2021;8 doi: 10.3389/fnut.2021.753059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panahande B., Sadeghi A., Parohan M. Alternative healthy eating index and risk of hip fracture: a systematic review and dose-response meta-analysis. J. Hum. Nutr. Diet. 2019;32(1):98–107. doi: 10.1111/jhn.12608. [DOI] [PubMed] [Google Scholar]
- Peeling P., Binnie M.J., Goods P.S.R., Sim M., Burke L.M. Evidence-based supplements for the enhancement of athletic performance. Int. J. Sport Nutr. Exercise Metab. 2018;28(2):178–187. doi: 10.1123/ijsnem.2017-0343. [DOI] [PubMed] [Google Scholar]
- Pfeifer M., Begerow B., Minne H. Vitamin D and muscle function. Osteoporos. Int. 2002;13(3):187–194. doi: 10.1007/s001980200012. [DOI] [PubMed] [Google Scholar]
- Pouwels S., Lalmohamed A., van Staa T., Cooper C., Souverein P., Leufkens H.G., et al. Use of organic nitrates and the risk of hip fracture: a population-based case-control study. J. Clin. Endocrinol. Metab. 2010;95(4):1924–1931. doi: 10.1210/jc.2009-2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rejnmark L., Vestergaard P., Mosekilde L. Decreased fracture risk in users of organic nitrates: a nationwide case-control study. J. Bone Miner. Res. 2006;21(11):1811–1817. doi: 10.1359/jbmr.060804. [DOI] [PubMed] [Google Scholar]
- Remelli F., Vitali A., Zurlo A., Volpato S. Vitamin D deficiency and sarcopenia in older persons. Nutrients. 2019;11(12):2861. doi: 10.3390/nu11122861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ringe J.D. The effect of vitamin D on falls and fractures. Scand. J. Clin. Lab. Invest. 2012;72(sup243):73–78. doi: 10.3109/00365513.2012.681965. [DOI] [PubMed] [Google Scholar]
- Rizzoli R., Biver E., Bonjour J.-P., Coxam V., Goltzman D., Kanis J.A., et al. Benefits and safety of dietary protein for bone health—an expert consensus paper endorsed by the european Society for Clinical and Economical Aspects of osteopororosis, osteoarthritis, and musculoskeletal diseases and by the international osteoporosis foundation. Osteoporos. Int. 2018;29(9):1933–1948. doi: 10.1007/s00198-018-4534-5. [DOI] [PubMed] [Google Scholar]
- Rizzoli R., Biver E., Brennan-Speranza T.C. Nutritional intake and bone health. Lancet Diabetes Endocrinol. 2021;9(9):606–621. doi: 10.1016/S2213-8587(21)00119-4. [DOI] [PubMed] [Google Scholar]
- Rogers T.S., Harrison S., Judd S., Orwoll E.S., Marshall L.M., Shannon J., et al. Dietary patterns and longitudinal change in hip bone mineral density among older men. Osteoporos. Int. 2018;29(5):1135–1145. doi: 10.1007/s00198-018-4388-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahni S., Cupples L.A., Mclean R.R., Tucker K.L., Broe K.E., Kiel D.P., et al. Protective effect of high protein and calcium intake on the risk of hip fracture in the Framingham offspring cohort. J. Bone Miner. Res. 2010;25(12):2770–2776. doi: 10.1002/jbmr.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samadi M., Khosravy T., Azadbakht L., Rezaei M., Mosafaghadir M., Kamari N., et al. Major dietary patterns in relation to muscle strength status among middle-aged people: a cross-sectional study within the RaNCD cohort. Food Sci Nutr. 2021;9(12):6672–6682. doi: 10.1002/fsn3.2617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandoval-Insausti H., Pérez-Tasigchana R.F., López-García E., Banegas J.R., Rodríguez-Artalejo F., Guallar-Castillón P. Protein intake and risk of falls: a prospective analysis in older adults. J. Am. Geriatr. Soc. 2019;67(2):329–335. doi: 10.1111/jgs.15681. [DOI] [PubMed] [Google Scholar]
- Schurgers L.J., Vermeer C. Determination of phylloquinone and menaquinones in food. Pathophysiol. Haemost. Thromb. 2000;30(6):298–307. doi: 10.1159/000054147. [DOI] [PubMed] [Google Scholar]
- Semba R.D., Lauretani F., Ferrucci L. Carotenoids as protection against sarcopenia in older adults. Arch. Biochem. Biophys. 2007;458(2):141–145. doi: 10.1016/j.abb.2006.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shams-White M.M., Chung M., Du M., Fu Z., Insogna K.L., Karlsen M.C., et al. Dietary protein and bone health: a systematic review and meta-analysis from the National Osteoporosis Foundation, 2. Am. J. Clin. Nutr. 2017;105(6):1528–1543. doi: 10.3945/ajcn.116.145110. [DOI] [PubMed] [Google Scholar]
- Shams-White M.M., Chung M., Fu Z., Insogna K.L., Karlsen M.C., LeBoff M.S., et al. Animal versus plant protein and adult bone health: a systematic review and meta-analysis from the National Osteoporosis Foundation. PLoS One. 2018;13(2) doi: 10.1371/journal.pone.0192459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherrington C., Michaleff Z.A., Fairhall N., Paul S.S., Tiedemann A., Whitney J., et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br. J. Sports Med. 2017;51(24):1750–1758. doi: 10.1136/bjsports-2016-096547. [DOI] [PubMed] [Google Scholar]
- Siddiqui J.A., Partridge N.C. Physiological bone remodeling: systemic regulation and growth factor involvement. Physiology. 2016;31(3):233–245. doi: 10.1152/physiol.00061.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim M., Blekkenhorst L.C., Lewis J.R., Bondonno C.P., Devine A., Zhu K., et al. Vegetable and fruit intake and injurious falls risk in older women: a prospective cohort study. Br. J. Nutr. 2018;120(8):925–934. doi: 10.1017/S0007114518002155. [DOI] [PubMed] [Google Scholar]
- Sim M., Blekkenhorst L., Lewis J., Bondonno C., Devine A., Zhu K., et al. Vegetable diversity, injurious falls, and fracture risk in older women: a prospective cohort study. Nutrients. 2018;10(8):1081. doi: 10.3390/nu10081081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim M., Prince R., Scott D., Daly R., Duque G., Inderjeeth C., et al. Utility of four sarcopenia criteria for the prediction of falls-related hospitalization in older Australian women. Osteoporos. Int. 2019;30(1):167–176. doi: 10.1007/s00198-018-4755-7. [DOI] [PubMed] [Google Scholar]
- Sim M., Prince R.L., Scott D., Daly R.M., Duque G., Inderjeeth C.A., et al. Sarcopenia definitions and their associations with mortality in older Australian women. J. Am. Med. Dir. Assoc. 2018;20(1):76–82. doi: 10.1016/j.jamda.2018.10.016. [DOI] [PubMed] [Google Scholar]
- Sim M., Lewis J.R., Blekkenhorst L.C., Bondonno C.P., Devine A., Zhu K., et al. Higher dietary nitrate intake is associated with better muscle function in older women. J. Cachexia. Sarcopenia Muscle. 2019;10(3):601–610. doi: 10.1002/jcsm.12413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim M., Lewis J.R., Prince R.L., Levinger I., Brennan-Speranza T.C., Palmer C., et al. The effects of vitamin K-rich green leafy vegetables on bone metabolism: a 4-week randomised controlled trial in middle-aged and older individuals. Bone Rep. 2020;12 doi: 10.1016/j.bonr.2020.100274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim M., Zhu K., Lewis J.R., Hodgson J.M., Prince R.L. Association between vitamin D status and long-term falls-related hospitalization risk in older women. J. Am. Geriatr. Soc. 2021;69(11):3114–3123. doi: 10.1111/jgs.17442. [DOI] [PubMed] [Google Scholar]
- Sim M., Blekkenhorst L.C., Bondonno N.P., Radavelli-Bagatini S., Peeling P., Bondonno C.P., et al. Dietary nitrate intake is positively associated with muscle function in men and women independent of physical activity levels. J. Nutr. 2021;151(5):1222–1230. doi: 10.1093/jn/nxaa415. [DOI] [PubMed] [Google Scholar]
- Sim M., Smith C., Bondonno N.P., Radavelli-Bagatini S., Blekkenhorst L.C., Dalla Via J., McCormick R., Zhu K., Hodgson J.M., Prince R.L., Lewis J.R. Higher dietary Vitamin K intake is associated with better physical function and lower long-term injurious falls risk in community-dwelling older women. J. Nutr. Health Ageing. 2023;27:38–45. doi: 10.1007/s12603-022-1866-9. [DOI] [PubMed] [Google Scholar]
- Sim M., Strydom A., Blekkenhorst L.C., Bondonno N.P., McCormick R., Lim W.H., et al. Dietary vitamin K1 intake is associated with lower long-term fracture-related hospitalization risk: the Perth longitudinal study of ageing women. Food Funct. 2022;13(20):10642–10650. doi: 10.1039/d2fo02494b. [DOI] [PubMed] [Google Scholar]
- Smith C., Lewis J.R., Sim M., Lim W.H., Lim E.M., Blekkenhorst L.C., et al. Higher undercarboxylated to Total osteocalcin ratio is associated with reduced physical function and increased 15-year falls-related hospitalizations: the Perth longitudinal study of aging women. J. Bone Miner. Res. 2021;36(3):523–530. doi: 10.1002/jbmr.4208. [DOI] [PubMed] [Google Scholar]
- de Souto Barreto P., Rolland Y., Vellas B., Maltais M. Association of Long-term Exercise Training with Risk of falls, fractures, hospitalizations, and mortality in older adults: a systematic review and meta-analysis. JAMA Intern. Med. 2019;179(3):394–405. doi: 10.1001/jamainternmed.2018.5406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens J.A., Olson S. Reducing falls and resulting hip fractures among older women. Home Care Provid. 2000;5(4):134–141. doi: 10.1067/mhc.2000.109232. [DOI] [PubMed] [Google Scholar]
- Stewart C., Piernas C., Cook B., Jebb S.A. Trends in UK meat consumption: analysis of data from years 1–11 (2008–09 to 2018–19) of the National Diet and nutrition survey rolling programme. Lancet Planet. Health. 2021;5(10):e699–e708. doi: 10.1016/S2542-5196(21)00228-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szulc P., Beck T.J., Marchand F., Delmas P.D. Low skeletal muscle mass is associated with poor structural parameters of bone and impaired balance in elderly men—the MINOS study. J. Bone Miner. Res. 2005;20(5):721–729. doi: 10.1359/JBMR.041230. [DOI] [PubMed] [Google Scholar]
- Thorpe D.L., Beeson W.L., Knutsen R., Fraser G.E., Knutsen S.F. Dietary patterns and hip fracture in the adventist health study 2: combined vitamin D and calcium supplementation mitigate increased hip fracture risk among vegans. Am. J. Clin. Nutr. 2021;114(2):488–495. doi: 10.1093/ajcn/nqab095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titchenal C.A., Dobbs J. A system to assess the quality of food sources of calcium. J. Food Compos. Anal. 2007;20(8):717–724. [Google Scholar]
- Tong T.Y., Key T.J., Sobiecki J.G., Bradbury K.E. Anthropometric and physiologic characteristics in white and british indian vegetarians and nonvegetarians in the UK biobank. Am. J. Clin. Nutr. 2018;107(6):909–920. doi: 10.1093/ajcn/nqy042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong T.Y.N., Appleby P.N., Armstrong M.E.G., Fensom G.K., Knuppel A., Papier K., et al. Vegetarian and vegan diets and risks of total and site-specific fractures: results from the prospective EPIC-Oxford study. BMC Med. 2020;18(1):353. doi: 10.1186/s12916-020-01815-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toxqui L., Vaquero M.P. Chronic iron deficiency as an emerging risk factor for osteoporosis: a hypothesis. Nutrients. 2015;7(4):2324–2344. doi: 10.3390/nu7042324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker K.L. Vegetarian diets and bone status. Am. J. Clin. Nutr. 2014;100(Suppl. 1):329s–335s. doi: 10.3945/ajcn.113.071621. [DOI] [PubMed] [Google Scholar]
- United States Department of Agriculture (USDA) United States Department of Health and Human Services. The United States Department of Agriculture, 2015–2020 Dietary Guidelines for Americans. 2015. Washington D.C. [Google Scholar]
- United States Department of Agriculture (USDA) United States Department of Health and Human Services . 9th edition. 2020. Dietary Guidelines for Americans, 2020-2025. December. [Google Scholar]
- van Ballegooijen A.J., van Putten S.R., Visser M., Beulens J.W., Hoogendijk E.O. Vitamin K status and physical decline in older adults—The longitudinal aging study Amsterdam. Maturitas. 2018;113:73–79. doi: 10.1016/j.maturitas.2018.04.013. [DOI] [PubMed] [Google Scholar]
- Veronese N., Stubbs B., Koyanagi A., Hébert J.R., Cooper C., Caruso M.G., et al. Pro-inflammatory dietary pattern is associated with fractures in women: an eight-year longitudinal cohort study. Osteoporos. Int. 2018;29(1):143–151. doi: 10.1007/s00198-017-4251-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Vliet S., Burd N.A., van Loon L.J. The skeletal muscle anabolic response to plant- versus animal-based protein consumption. J. Nutr. 2015;145(9):1981–1991. doi: 10.3945/jn.114.204305. [DOI] [PubMed] [Google Scholar]
- van Vliet S., Burd N.A., van Loon L.J. The skeletal muscle anabolic response to plant-versus animal-based protein consumption. J. Nutr. 2015;145(9):1981–1991. doi: 10.3945/jn.114.204305. [DOI] [PubMed] [Google Scholar]
- Volpi E., Campbell W.W., Dwyer J.T., Johnson M.A., Jensen G.L., Morley J.E., et al. Is the optimal level of protein intake for older adults greater than the recommended dietary allowance? J. Gerontol. A Biol. Sci. Med. Sci. 2013;68(6):677–681. doi: 10.1093/gerona/gls229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace T.C., Frankenfeld C.L. Dietary protein intake above the current RDA and bone health: a systematic review and meta-analysis. J. Am. Coll. Nutr. 2017;36(6):481–496. doi: 10.1080/07315724.2017.1322924. [DOI] [PubMed] [Google Scholar]
- Warensjö Lemming E., Byberg L. Is a healthy diet also suitable for the prevention of fragility Fractures? Nutrients. 2020;12(9) doi: 10.3390/nu12092642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warensjö Lemming E., Byberg L., Melhus H., Wolk A., Michaëlsson K. Long-term a posteriori dietary patterns and risk of hip fractures in a cohort of women. Eur. J. Epidemiol. 2017;32(7):605–616. doi: 10.1007/s10654-017-0267-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster J., Rycroft C.E., Greenwood D.C., Cade J.E. Dietary risk factors for hip fracture in adults: an umbrella review of meta-analyses of prospective cohort studies. PLoS One. 2021;16(11) doi: 10.1371/journal.pone.0259144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster J., Greenwood D.C., Cade J.E. Risk of hip fracture in meat-eaters, pescatarians, and vegetarians: results from the UK Women's cohort study. BMC Med. 2022;20(1):275. doi: 10.1186/s12916-022-02468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wierzbicka A., Oczkowicz M. Sex differences in vitamin D metabolism, serum levels and action. Br. J. Nutr. 2022;128(11):2115–2130. doi: 10.1017/S0007114522000149. [DOI] [PubMed] [Google Scholar]
- Wirth J., Hillesheim E., Brennan L. The role of protein intake and its timing on body composition and muscle function in healthy adults: a systematic review and meta-analysis of randomized controlled trials. J. Nutr. 2020;150(6):1443–1460. doi: 10.1093/jn/nxaa049. [DOI] [PubMed] [Google Scholar]
- Witard O.C., Wardle S.L., Macnaughton L.S., Hodgson A.B., Tipton K.D. Protein considerations for optimising skeletal muscle mass in healthy young and older adults. Nutrients. 2016;8(4):181. doi: 10.3390/nu8040181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe R.R. The underappreciated role of muscle in health and disease. Am. J. Clin. Nutr. 2006;84(3):475–482. doi: 10.1093/ajcn/84.3.475. [DOI] [PubMed] [Google Scholar]
- World Health Organisation Protein and amino acid requirements in human nutrition: report of a joint WHO/FAO/UNU expert consultation. World Health Organ. Tech. Rep. Ser. 2007;935:1. [PubMed] [Google Scholar]
- Wu A.-M., Sun X.-L., Lv Q.-B., Zhou Y., Xia D.-D., Xu H.-Z., et al. The relationship between dietary protein consumption and risk of fracture: a subgroup and dose-response meta-analysis of prospective cohort studies. Sci. Rep. 2015;5:9151. doi: 10.1038/srep09151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu A.-M., Bisignano C., James S.L., Abady G.G., Abedi A., Abu-Gharbieh E., et al. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990–2019: a systematic analysis from the global burden of disease study 2019. Lancet Healthy Longev. 2021;2(9):e580–e592. doi: 10.1016/S2666-7568(21)00172-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yakar S., Werner H., Rosen C.J. Insulin-like growth factors: actions on the skeleton. J. Mol. Endocrinol. 2018;61(1):T115–T137. doi: 10.1530/JME-17-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan S., Wan Z.H., Cheng S.L., Michaëlsson K., Larsson S.C. Insulin-like growth Factor-1, bone mineral density, and fracture: a mendelian randomization study. J. Clin. Endocrinol. Metab. 2021;106(4) doi: 10.1210/clinem/dgaa963. e1552-e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng F.F., Wu B.H., Fan F., Xie H.L., Xue W.Q., Zhu H.L., et al. Dietary patterns and the risk of hip fractures in elderly chinese: a matched case-control study. J. Clin. Endocrinol. Metab. 2013;98(6):2347–2355. doi: 10.1210/jc.2013-1190. [DOI] [PubMed] [Google Scholar]
- Zeng F.F., Xue W.Q., Cao W.T., Wu B.H., Xie H.L., Fan F., et al. Diet-quality scores and risk of hip fractures in elderly urban chinese in Guangdong, China: a case-control study. Osteoporos. Int. 2014;25(8):2131–2141. doi: 10.1007/s00198-014-2741-2. [DOI] [PubMed] [Google Scholar]
- Zhong L., Blekkenhorst L.C., Bondonno N.P., Sim M., Woodman R.J., Croft K.D., et al. A food composition database for assessing nitrate intake from plant-based foods. Food Chem. 2022;394 doi: 10.1016/j.foodchem.2022.133411. [DOI] [PubMed] [Google Scholar]
- Zhu K., Lewis J.R., Sim M., Prince R.L. Low vitamin D status is associated with impaired bone quality and increased risk of fracture-related hospitalization in older australian women. J. Bone Miner. Res. 2019;34(11):2019–2027. doi: 10.1002/jbmr.3818. [DOI] [PubMed] [Google Scholar]
- Zoltick E.S., Sahni S., McLean R.R., Quach L., Casey V.A., Hannan M.T. Dietary protein intake and subsequent falls in older men and women: the Framingham study. J. Nutr. Health Aging. 2011;15(2):147–152. doi: 10.1007/s12603-011-0028-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was used for the research described in the article.