Abstract
Live attenuated human immunodeficiency virus type 1 (HIV-1) vaccines are considered unsafe because faster-replicating pathogenic virus variants may evolve after vaccination. We previously presented a conditional-live HIV-1 variant of which replication can be switched off as an alternative vaccination strategy. To improve the safety of such a vaccine, we constructed a new HIV-1 variant that depends not only on doxycycline for gene expression but also on the T20 peptide for cell entry. Replication of this virus can be limited to the level required to induce the immune system by transient administration of doxycycline and T20. Subsequent withdrawal of these inducers efficiently blocks viral replication and evolution.
Human immunodeficiency virus type 1 (HIV-1) vaccines based on a live attenuated virus have shown some promise in the simian immunodeficiency virus (SIV)-macaque model but are generally considered unsafe for use in humans (1, 9, 13, 14, 23). The major problem is the persistence of the attenuated virus, and ongoing replication may eventually lead to the selection of fitter and more pathogenic virus variants (2, 3, 8). Ideally, one would like to restrict virus replication to the time that is needed to provide full protection. Several approaches have been reported that address this issue. For instance, virus replication can be stopped after vaccination by administration of antiviral drugs (19). Whereas this may be a good strategy for in vitro studies, application in humans seems problematic because long-term virus inhibition will require continuous drug administration and the virus may develop drug resistance. An alternative approach is the construction of a “single-cycle” virus that can execute only a single round of replication. However, it is questionable whether such limited replication will be sufficient for the induction of protective immunity.
We and others previously presented a unique genetic approach that uses a conditional-live HIV-1 virus (7, 10, 11, 24, 25). In this HIV-rtTA virus, the Tat-TAR regulatory mechanism that controls viral gene expression and replication was inactivated by mutation of both the Tat gene and the TAR RNA structure and functionally replaced by the Tet system for inducible gene expression (6). The rtTA gene encoding a man-made transcriptional activator was inserted in place of the nef gene, and the tet operator (tetO) DNA binding sites were inserted into the long terminal repeat promoter. Since the rtTA protein can only bind tetO and activate transcription in the presence of doxycycline (DOX), the HIV-rtTA variant replicates exclusively when DOX is administered. Upon vaccination with this virus, replication can be temporarily activated and controlled to the extent needed for induction of the immune system by transient DOX administration. The initial HIV-rtTA virus has been improved significantly by virus evolution (12, 21, 22), and we have shown efficient and DOX-dependent replication not only in vitro in T-cell lines but also ex vivo in human lymphoid tissue (18). However, additional safety features may be required before such a vaccine virus can be considered for use in humans.
We recently came across another way to control HIV-1 replication by a nontoxic drug. An HIV-1 patient within the Academic Medical Center (University of Amsterdam, Amsterdam, The Netherlands) entered a clinical trial with the entry inhibitor T20 (also called enfuvirtide and fuzeon) in 2001. T20 is a 36-mer peptide that mimics part of the HR2 domain of the envelope gp41 protein (Env-gp41), which is intrinsically involved in the fusion of the viral and cellular membranes (4). Although viral replication was successfully inhibited initially, a gradual increase in the viral load suggested the emergence of T20-resistant HIV-1 variants, and we set out to perform a detailed genotypic and phenotypic analysis (5). An initial amino acid change (Val-554-Ala [Env coordinates]) within the HR1 portion of Env-gp41 was found to provide resistance to T20 (26). Most intriguingly, an additional change (Asn-642-Lys) within HR2 was observed that improved the level of resistance yet abolished the ability of the virus to replicate in the absence of T20. In other words, this double mutant is dependent on the T20 peptide for replication, and a mechanistic model was presented to explain T20-induced viral entry (5).
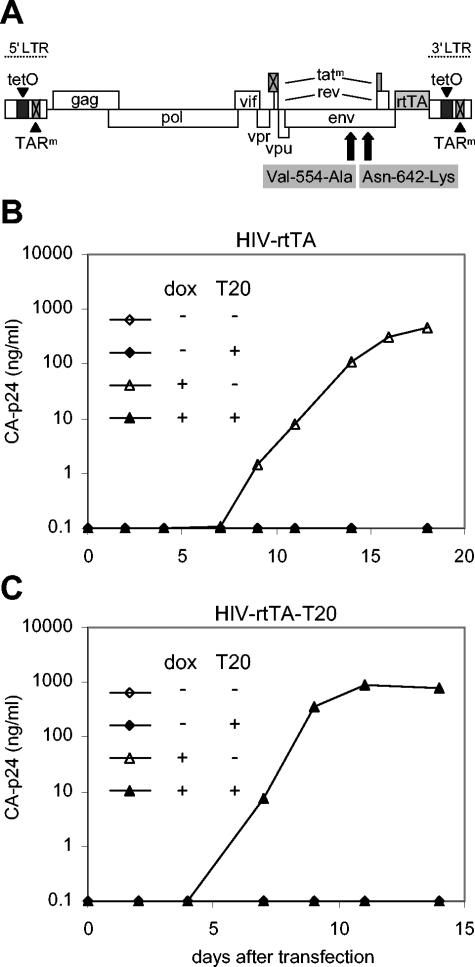
We decided to construct an HIV-1 virus that replicates only in the presence of both T20 and DOX by introducing the observed gp41 changes into HIV-rtTA. These mutations had been introduced earlier into a molecular clone of the CXCR4-tropic HIV-1 LAI isolate (5). The DraI-BamHI Env fragment of this clone was used to replace the corresponding sequences in the optimized HIV-rtTA construct that contains the 2ΔtetO configuration (21) and the rtTA-F86Y variant with greatly improved DOX sensitivity (12) (Fig. 1A). This HIV-rtTA-T20 plasmid was transfected into the SupT1 T-cell line, and viral replication was assayed in the presence or absence of DOX and T20. We used the parental HIV-rtTA virus as a control. This virus requires only DOX for replication and is effectively inhibited by the antiviral peptide T20 (Fig. 1B). HIV-rtTA-T20 replicates exclusively in the presence of both DOX and T20 (Fig. 1C). Addition of a single inducer, either DOX or T20, is not sufficient to support replication of this new HIV-1 variant.
FIG. 1.
Conditional-live HIV-1 variants. (A) In the HIV-rtTA virus, the Tat-TAR axis of transcription regulation has been inactivated by mutation of both Tat and TAR (crossed boxes), and transcription and replication of the virus was made DOX dependent by introducing tetO elements in the long terminal repeat (LTR) promoter region and replacing the Nef gene with the rtTA gene. A T20-dependent HIV-rtTA-T20 variant was constructed by introduction of the Val-554-Ala and Asn-642-Lys mutations in the Env-gp41 domain. This construction caused an additional Asn-641-Ser mutation that does not affect virus replication (5) (unpublished results). (B and C) Replication of HIV-rtTA and HIV-rtTA-T20. SupT1 T cells were transfected with 1 μg of the molecular clones and cultured in the presence (+) or absence (-) of 100 ng of DOX/ml and 500 ng of T20/ml (as described previously [5, 12]). Virus replication was monitored by CA-p24 enzyme-linked immunosorbent assay (ELISA) on culture supernatant samples. A typical experiment is shown. Similar results were obtained in independent experiments that were started by either infection or transfection of SupT1 cells.
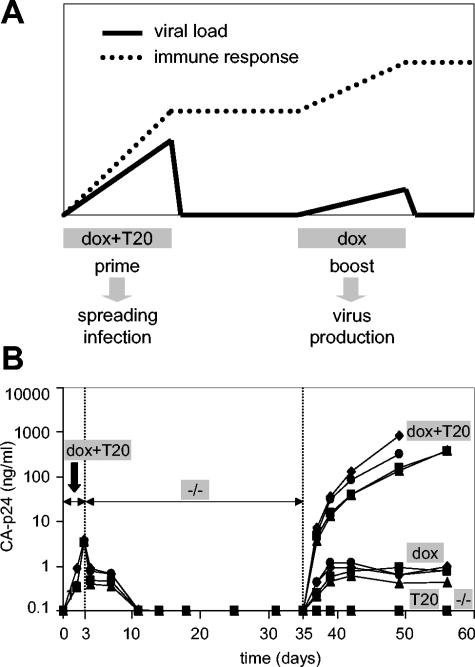
Because DOX and T20 control different steps of the HIV-1 replication cycle, additional manipulation seems possible. For instance, the sole addition of DOX to cells carrying the integrated HIV-rtTA-T20 provirus will result in another round of virus production, yet the infection of new cells and virus spread will be blocked in the absence of T20. In fact, this plus-DOX-no-T20 regimen seems to be an ideal strategy for booster vaccination without further virus spread (Fig. 2A). Repeated DOX administration will not only boost the immune system but may also lead to the removal of antigen-expressing cells by the immune system. This elimination of provirus-containing cells will further improve the safety of the vaccine. To test this scenario, we started four cultures of HIV-rtTA-T20 in SupT1 cells in the presence of both DOX and T20 (Fig. 2B). Viral replication resulted in the detection of CA-p24 and the appearance of syncytia in the culture. At day 3 we washed out both inducers, which resulted in silencing of viral replication, and the CA-p24 level dropped below the level of detection around day 11. At day 35, each culture was split in four samples that were treated differently. Addition of both DOX and T20 induced a spreading infection with high CA-p24 levels and large syncytia. Addition of only DOX did activate a modest level of virus production, but did not result in a spreading infection. The untreated control and the sample that received only T20 did not produce any virus.
FIG. 2.
Vaccination strategy with the DOX- and T20-dependent HIV-1 virus. (A) Upon prime vaccination with HIV-rtTA-T20, replication can be temporarily activated and controlled to the extent that is needed for induction of the immune system by transient DOX and T20 administration. After priming of the immune system, DOX and T20 are withdrawn to stop virus replication. If this priming is not sufficient to confer protective immunity, or if it is necessary to refresh immunological memory, a booster vaccination can be achieved by the administration of DOX, which will activate virus production in cells carrying the integrated HIV-rtTA-T20 provirus, yet the infection of new cells and virus spread will be blocked in the absence of T20. (B) To simulate this vaccination scenario, SupT1 cells were transfected with HIV-rtTA-T20 and cultured in the presence of both DOX and T20 (different symbols represent different cultures). At day 3, the culture medium was replaced with medium without DOX and T20 (-/-). At day 35, each culture was split in four samples, to which either DOX (100 ng/ml), T20 (500 ng/ml), DOX plus T20, or no inducer (-/-) was added. Virus production was monitored by CA-p24 ELISA on culture supernatant samples.
We have described the construction of an HIV-1 variant that is dependent for its replication on the antibiotic DOX and the antiviral peptide T20. This double dependency clearly improves the safety of this virus as a conditional-live virus vaccine. Since the T20-dependent phenotype is the product of natural virus evolution, one could wonder whether the same evolution process may hamper the proposed vaccine approach. For instance, HIV-rtTA-T20 could evolve to a T20-resistant or wild-type-like T20-sensitive phenotype. T20 resistance would require a Lys-642-Asn reversion in HR2, and we could try to limit this escape route by introducing an alternative Lys codon (or perhaps even an alternative amino acid) that needs multiple nucleotide substitutions to convert into an Asn codon. Evolution to the wild-type phenotype is more difficult, because it requires an additional Ala-554-Val reversion in HR1. The alternative with an initial change in HR1 seems impossible, because a virus that carries only the HR2 mutation does not replicate (5). These evolutionary possibilities will be addressed in future studies. However, we emphasize that the DOX control of viral gene expression provides an efficient and independent means to prevent HIV-rtTA-T20 evolution, as the virus cannot evolve if it does not replicate. Nevertheless, we realize that the efficacy and safety of this vaccine approach requires further testing in the SIV-macaque model, and we recently managed to construct a DOX-dependent version of SIVmac239 for this purpose (unpublished results). It will be of interest to test if the T20-dependent phenotype can also be transferred onto the Env protein of SIVmac239. This may not be straightforward, because T20 is not an effective inhibitor of SIV. However, more potent inhibitor peptides with a broader-activity spectrum have been developed, e.g., T1249, although its clinical development was recently suspended (15-17, 20). Future virus evolution and selection experiments with such compounds may provide means to control SIV entry into the cell by a nontoxic drug. Finally, the phenotype of T20-dependent virus entry and DOX-dependent gene expression provides a nice research tool to dissect multiple steps in viral replication, and it may provide a means to synchronize HIV-1 viruses or HIV-based lentiviral vectors at the level of gene expression or infection.
Acknowledgments
We thank Xue Zhou for help in some of the experiments and Stephan Heynen for the CA-p24 ELISA.
The HIV-rtTA vaccine research is sponsored by the Technology Foundation STW (Applied Science Division of NWO and the Technology Program of the Ministry of Economic Affairs, Utrecht, The Netherlands).
REFERENCES
- 1.Almond, N., K. Kent, M. Cranage, E. Rud, B. Clarke, and E. J. Stott. 1995. Protection by attenuated simian immunodeficiency virus in macaques against challenge with virus-infected cells. Lancet 345:1342-1344. [DOI] [PubMed] [Google Scholar]
- 2.Baba, T. W., Y. S. Jeong, D. Penninck, R. Bronson, M. F. Greene, and R. M. Ruprecht. 1995. Pathogenicity of live, attenuated SIV after mucosal infection of neonatal macaques. Science 267:1820-1825. [DOI] [PubMed] [Google Scholar]
- 3.Baba, T. W., V. Liska, A. H. Khimani, N. B. Ray, P. J. Dailey, D. Penninck, R. Bronson, M. F. Greene, H. M. McClure, L. N. Martin, and R. M. Ruprecht. 1999. Live attenuated, multiply deleted simian immunodeficiency virus causes AIDS in infant and adult macaques. Nat. Med. 5:194-203. [DOI] [PubMed] [Google Scholar]
- 4.Baldwin, C. E., R. W. Sanders, and B. Berkhout. 2003. Inhibiting HIV-1 entry with fusion inhibitors. Curr. Med. Chem. 10:1633-1642. [DOI] [PubMed] [Google Scholar]
- 5.Baldwin, C. E., R. W. Sanders, Y. Deng, S. Jurriaans, J. M. Lange, M. Lu, and B. Berkhout. 2004. Emergence of a drug-dependent HIV-1 variant during therapy with the T20 fusion inhibitor. J. Virol. 78:12428-12437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baron, U., and H. Bujard. 2000. Tet repressor-based system for regulated gene expression in eukaryotic cells: principles and advances. Methods Enzymol. 327:401-421. [DOI] [PubMed] [Google Scholar]
- 7.Berkhout, B., G. Marzio, and K. Verhoef. 2002. Control over HIV-1 replication by an antibiotic; a novel vaccination strategy with a drug-dependent virus. Virus Res. 82:103-108. [DOI] [PubMed] [Google Scholar]
- 8.Berkhout, B., K. Verhoef, J. L. B. van Wamel, and B. Back. 1999. Genetic instability of live-attenuated human immunodeficiency virus type 1 vaccine strains. J. Virol. 73:1138-1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blancou, P., N. Chenciner, F. R. Ho Tsong, V. Monceaux, M. C. Cumont, D. Guetard, B. Hurtrel, and S. Wain-Hobson. 2004. Simian immunodeficiency virus promoter exchange results in a highly attenuated strain that protects against uncloned challenge virus. J. Virol. 78:1080-1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Das, A. T., K. Verhoef, and B. Berkhout. 2004. A conditionally replicating virus as a novel approach toward an HIV vaccine. Methods Enzymol. 388:359-379. [DOI] [PubMed] [Google Scholar]
- 11.Das, A. T., X. Zhou, M. Vink, B. Klaver, and B. Berkhout. 2002. Conditional live virus as a novel approach towards a safe live attenuated HIV vaccine. Expert Rev. Vaccines 1:293-301. [DOI] [PubMed] [Google Scholar]
- 12.Das, A. T., X. Zhou, M. Vink, B. Klaver, K. Verhoef, G. Marzio, and B. Berkhout. 2004. Viral evolution as a tool to improve the tetracycline-regulated gene expression system. J. Biol. Chem. 279:18776-18782. [DOI] [PubMed] [Google Scholar]
- 13.Desrosiers, R. C. 1992. HIV with multiple gene deletions as a live attenuated vaccine for AIDS. AIDS Res. Hum. Retrovir. 8:411-421. [DOI] [PubMed] [Google Scholar]
- 14.Desrosiers, R. C. 1998. Prospects for live attenuated HIV. Nat. Med. 4:982. [DOI] [PubMed] [Google Scholar]
- 15.Eron, J. J., R. M. Gulick, J. A. Bartlett, T. Merigan, R. Arduino, J. M. Kilby, B. Yangco, A. Diers, C. Drobnes, R. DeMasi, M. Greenberg, T. Melby, C. Raskino, P. Rusnak, Y. Zhang, R. Spence, and G. D. Miralles. 2004. Short-term safety and antiretroviral activity of T-1249, a second-generation fusion inhibitor of HIV. J. Infect. Dis. 189:1075-1083. [DOI] [PubMed] [Google Scholar]
- 16.Feinberg, J. 2003. Meeting notes from the 43rd Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC). T-1249 for T-20 salvage. AIDS Clin. Care 15:95-96. [PubMed] [Google Scholar]
- 17.Huff, B. 2003. T-1249 development suspended. GMHC Treat. Iss. 17:6. [PubMed] [Google Scholar]
- 18.Kiselyeva, Y., Y. Ito, R. Lima, J.-C. Grivel, A. T. Das, B. Berkhout, and L. B. Margolis. 2004. Depletion of CD4 T lymphocytes in human lymphoid tissue infected ex vivo with doxycycline-dependent HIV-1. Virology 328:1-6. [DOI] [PubMed] [Google Scholar]
- 19.Lifson, J. D., J. L. Rossio, M. Piatak, Jr., T. Parks, L. Li, R. Kiser, V. Coalter, B. Fisher, B. M. Flynn, S. Czajak, V. M. Hirsch, K. A. Reimann, J. E. Schmitz, J. Ghrayeb, N. Bischofberger, M. A. Nowak, R. C. Desrosiers, and D. Wodarz. 2001. Role of CD8+ lymphocytes in control of simian immunodeficiency virus infection and resistance to rechallenge after transient early antiretroviral treatment. J. Virol. 75:10187-10199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martin-Carbonero, L. 2004. Discontinuation of the clinical development of fusion inhibitor T-1249. AIDS Rev. 6:61. [PubMed] [Google Scholar]
- 21.Marzio, G., K. Verhoef, M. Vink, and B. Berkhout. 2001. In vitro evolution of a highly replicating, doxycycline-dependent HIV for applications in vaccine studies. Proc. Natl. Acad. Sci. USA 98:6342-6347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marzio, G., M. Vink, K. Verhoef, A. de Ronde, and B. Berkhout. 2002. Efficient human immunodeficiency virus replication requires a fine-tuned level of transcription. J. Virol. 76:3084-3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mills, J., R. Desrosiers, E. Rud, and N. Almond. 2000. Live attenuated HIVvaccines: proposal for further research and development. AIDS Res. Hum. Retrovir. 16:1453-1461. [DOI] [PubMed] [Google Scholar]
- 24.Smith, S. M., M. Khoroshev, P. A. Marx, J. Orenstein, and K. T. Jeang. 2001. Constitutively dead, conditionally live HIV-1 genomes. Ex vivo implications for a live virus vaccine. J. Biol. Chem. 276:32184-32190. [DOI] [PubMed] [Google Scholar]
- 25.Verhoef, K., G. Marzio, W. Hillen, H. Bujard, and B. Berkhout. 2001. Strict control of human immunodeficiency virus type 1 replication by a genetic switch: Tet for Tat. J. Virol. 75:979-987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wei, X., J. M. Decker, H. Liu, Z. Zhang, R. B. Arani, J. M. Kilby, M. S. Saag, X. Wu, G. M. Shaw, and J. C. Kappes. 2002. Emergence of resistant human immunodeficiency virus type 1 in patients receiving fusion inhibitor (T-20) monotherapy. Antimicrob. Agents Chemother. 46:1896-1905. [DOI] [PMC free article] [PubMed] [Google Scholar]