Abstract
Background
High‐quality cardiopulmonary resuscitation (CPR) is associated with improved survival from out‐of‐hospital cardiac arrest and includes chest compression depth, chest compression rate, and chest compression fraction within international guideline recommendations. Previous studies have demonstrated divergent results of real‐time feedback on CPR performance and patient outcomes. This study investigated the association between emergency medical service CPR quality and real‐time CPR feedback for out‐of‐hospital cardiac arrest.
Methods and Results
This study collected out‐of‐hospital cardiac arrest data within the Capital Region of Denmark and compared CPR quality delivered by ambulance personnel. Data were collected in 2 consecutive phases from October 2018 to February 2020. Median chest compression depth was 6.0 cm (no feedback) and 5.9 cm (real‐time feedback) (P=0.852). Corresponding proportion of guideline‐compliant chest compressions for depth was 16.6% and 28.7%, respectively (P<0.001). Median chest compression rate per minute was 111 and 109 (P<0.001), respectively. Corresponding guideline adherence proportion for compression rate was 65.4% compared with 80.4% (P<0.001), respectively. Chest compression fraction was 78.9% compared with 81.9% (P<0.001), respectively. The combination of guideline‐compliant chest compression depth and chest compression rate simultaneously was 8.5% (no feedback) versus 18.8% (feedback) (P<0.001). Improvements were not significant for return of spontaneous circulation (odds ratio [OR], 1.08 [95% CI, 0.84–1.39]), sustained return of spontaneous circulation (OR, 1.00 [95% CI, 0.77–1.31]), or survival to hospital discharge (OR, 0.91 [95% CI, 0.64–1.30]).
Conclusions
Real‐time feedback was associated with improved guideline compliance for chest compression depth, rate, and fraction but not return of spontaneous circulation, sustained return of spontaneous circulation, or survival to hospital discharge.
Registration
URL: https://www.clinicaltrials.gov; Unique identifier: NCT04152252.
Keywords: cardiopulmonary resuscitation, cardiopulmonary resuscitation quality, emergency medical services, out‐of‐hospital cardiac arrest, real‐time feedback
Subject Categories: Cardiopulmonary Arrest, Cardiopulmonary Resuscitation and Emergency Cardiac Care
Nonstandard Abbreviations and Acronyms
- CCD
chest compression depth
- CCDiT
chest compression depth in target
- CCF
chest compression fraction
- CCR
chest compression rate
- CCRiT
chest compression rate in target
- CCiT
combined compressions in target
- OHCA
out‐of‐hospital cardiac arrest
- ROSC
return of spontaneous circulation
- sROSC
sustained return of spontaneous circulation
Clinical Perspective.
What Is New?
Despite median chest compression depth (in centimeters) not changing significantly between control and intervention groups in this study, the proportion of compressions within guideline recommendations almost doubled when paramedics were exposed to real‐time feedback.
Although median chest compression depth (in centimeters) and median chest compression rate (in compressions per minute) were within guidelines in both groups, the proportion of compressions delivered according to guidelines improved significantly with real‐time feedback.
When combining guideline‐adherent depth and rate simultaneously for every compression delivered, cardiopulmonary resuscitation quality was generally low but more than doubled with real‐time feedback.
What Are the Clinical Implications?
During resuscitation, the challenge in achieving guideline compliance must not be underestimated; even with real‐time feedback, combining correct depth and rate in 1 compression is difficult.
During chest compressions, the compressor should not be assigned other tasks or focus on tasks other than performing compressions.
When measuring cardiopulmonary resuscitation quality, resuscitation officers and researchers should use combined parameters and measure guideline in proportion compliance and not the current mean/median measurements.
Out‐of‐hospital cardiac arrest (OHCA) is a major health problem in Europe, with ≈275 000 cases treated by emergency medical services (EMS) each year. 1 Overall survival is ≈8% to 10%, but significant variation exists across countries. 2 , 3 Survival depends on optimal performance in the chain of survival, with guideline‐adherent chest compressions being a key performance component in cardiopulmonary resuscitation (CPR). 4 Current resuscitation guidelines from the European Resuscitation Council and the American Heart Association recommend a chest compression depth (CCD) of 5 to 6 cm, a chest compression rate (CCR) of 100 to 120 compressions per minute, a chest compression fraction (CCF) of at least 60% (American Heart Association guidelines state 80%), a full release of the force exerted to the chest (recoil), ventilations with a duration of 1 second, and a tidal volume of 500 to 600 mL per breath. 4 , 5 Real‐time CPR feedback is available in several automated external defibrillators and professional EMS monitors. However, previous studies have reported divergent relationships between real‐time feedback and CPR quality and patient outcome when EMS attend OHCA. 6 , 7 , 8
OHCA occurs ≈5400 times each year in Denmark, with a quadrupling in survival from 4% to 16% since 2001. 9 Improvement initiatives have been driven by implementing the 10‐step OHCA survival strategy advocated by the Global Resuscitation Alliance and Resuscitation Academy. 10 Initiatives implemented include a continuously updated national OHCA register, telephone‐assisted CPR, artificial intelligence to improve OHCA recognition, and dispatch of volunteer responders in suspected OHCA. 9 , 11 Furthermore, the 10 steps recommend high‐performance CPR and the continuous measurement of professional resuscitation.
This study investigated whether real‐time feedback for chest compressions was associated with improved EMS CPR quality (chest compression depth, rate, and fraction) and patient outcomes (return of spontaneous circulation [ROSC], sustained ROSC [sROSC], and 30‐day survival) in an EMS system that has already improved OHCA survival.
Methods
Study Design
This study was conducted as a prospective cohort study and registered on https://clinicaltrials.gov/ (NCT04152252). The study consists of 2 consecutive phases. Phase 1 (no feedback) was an 8‐month phase from October 1, 2018, to May 25, 2019. Phase 2 (real‐time feedback) was a 9‐month phase from May 26, 2019, to February 19, 2020. This study is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology Statement. 12
Because of the sensitive nature of the data collected for this study, requests to access the data set from qualified researchers trained in human subject confidentiality protocols may be sent to the corresponding author.
Setting
Demographics
The study was conducted in the Capital Region of Denmark. The region covers 2561 km2 and is a mix of urban and rural areas and includes 1.82 million inhabitants with a population density of 709.7 inhabitants/km2. 13 The region has 9 hospitals with emergency departments, with 2 being designated OHCA receiving facilities.
EMS and OHCA in Study Setting
Copenhagen EMS is a public organization responsible for providing EMS to the population in the region. Copenhagen EMS operates the 1‐1‐2 medical triage of health‐related calls and 5 physician‐staffed mobile critical care units. Two independent companies provide ambulances: Falck and the Greater Copenhagen Fire Department. 14 Copenhagen EMS handles >120 000 1‐1‐2 emergency calls annually. Of these, 2.7% were categorized as unresponsive adults/suspected cardiac arrests. 15 Copenhagen EMS use artificial intelligence to aid the recognition of OHCA, dispatch volunteer responders by app, and provide telephone or video‐assisted CPR to the caller. 11 , 16 , 17 The standard clinical response to OHCA is dispatch of the nearest ambulance and mobile critical care unit.
Participants and Selection
We included adults aged ≥18 years in OHCA who received CPR from EMS providers with a ZOLL X‐Series defibrillator (ZOLL Medical Corporation, Chelmsford, MA) attached to the patient. Patients and cases were excluded on the basis of the following: (1) age <18 years, (2) if no EMS physician was involved, (3) if no CPR quality data remained after editing the case, (4) unidentifiable CPR quality pattern, or (5) corrupted data.
Data Collection and Management
EMS initiates resuscitation on unconscious patients with no or abnormal breathing and where no do not resuscitate document is presented. Resuscitation attempts are continued until an emergency physician, present or by telephone, finds the resuscitation attempt to be futile. This approach did not change during study phases.
Data on CPR quality were recorded using a ZOLL X‐Series Defibrillator, which records chest compression data when paramedics attach an accelerometer‐based sensor to the patient's chest. The sensor is a pressure pad situated between the provider's hands and the patient's chest. The sensor recorded thoracic movement and presented data as real‐time feedback on the defibrillator screen in a CPR feedback dashboard (Figure S1). Paramedics manually transferred data to CaseReview (ZOLL Medical Corporation), a software allowing for review, editing, and exporting of cardiac arrest data.
CPR quality data were reviewed case by case and, if indicated, edited by 1 researcher (R.M.O.) according to a predefined set of criteria and a procedure developed by the researchers (Data S1 and Figure S2). Selected cases were reviewed by another researcher (R.M.L.) for verification or to make a final decision for complex patterns.
CPR quality data from CaseReview were merged with regional verified OHCA data on patient characteristics and outcomes and analyzed using STATA version 17 (StataCorp; 2021; Stata Statistical Software: Release 17; College Station, TX).
Before the initiation of our study, paramedics were equipped with LifePack 15 defibrillators only delivering metronome audio guidance.
Exposure
During the no‐feedback phase, paramedics attached the sensor to the patient's chest, but the CPR feedback dashboard (Figure S1) on the defibrillator was disengaged and not visible to paramedics.
In the real‐time feedback phase, real‐time feedback was displayed on the defibrillator screen, presenting compression depth as a numerical value with color. Green indicated guideline compliance, and yellow indicated noncompliant compression depth. The compression rate was presented the same way. Furthermore, a metronome provided audible rate guidance. A bar indicated the release of force exerted to the chest. Before the real‐time feedback phase, paramedics attended a 45‐minute introduction to the feedback dashboard, including a 10‐minute simulated OHCA scenario.
Outcomes
The following variables were collected from CaseReview: CCD in target (CCDiT) (proportion of all compressions delivered within the recommended 5–6 cm depth), CCD (mean in centimeters), CCR (frequency mean), CCR in target (CCRiT) (proportion of all compressions delivered within the recommended 100–120 compressions per minute), CCF (proportion of the total resuscitation time with chest compressions being performed), combined compressions in target (CCiT) (proportion of guideline‐adherent compression depth [in centimeters] and rate in compressions per minute delivered simultaneously), and patient social security number.
The primary outcome was CCDiT. Secondary outcomes were CCD, CCRiT, CCR, CCF, CCiT, and ROSC at any time during resuscitation, sROSC (ROSC at hospital handover), and 30‐day survival. All CPR quality measurements were calculated from the first registered compression to the last registered compression.
Other Variables
From the regional cardiac arrest database, the following variables were collected: sex, age, location of OHCA, OHCA witnessed by bystander, bystander defibrillation, EMS defibrillation, EMS response time, OHCA witnessed by EMS, first observed rhythm by EMS, bystander CPR, ROSC, sROSC, 30‐day survival, and patient social security number.
Sample Size and Power
With an estimated 115 OHCA cases each month in Copenhagen, 6‐month data collection phases were planned to allow for the potential inclusion of 690 OHCA cases in each of the 2 phases. Potential causes for data loss were incomplete data, unidentifiable patients, and technical issues. Data loss was estimated to be 5%, which allowed for 655 OHCA cases in each phase.
The power of the study was calculated on the basis of the primary outcome (CCDiT) with a 5% significance level and a total of 1310 patients, with 655 in each group using a formula for detection of a difference between 2 means and a 2‐sided test. The mean and SD of CCDiT in the nonfeedback phase was expected to be 36.9±30.6%.
In consultation with clinical experts within cardiology and medical education and simulation, a consensus was reached that an improvement should be at least 15% to be clinically significant (ie, mean and SD of CCDiT in the real‐time feedback phase at 42.435±30.6%). A systematic review by Lyngby et al 7 supported this, as the mean improvements in performance for guideline‐adherent compression depth, rate, and fraction were 9.6%, 9.9%, and 9.8%, respectively, when real‐time feedback intervention was used. The 9.6% to 9.9% improvement was insufficient to detect changes in patient outcomes in the included studies. This suggested a CPR quality improvement of at least 10% and possibly higher to translate into changes in patient outcomes.
On the basis of the above parameter values, a power of 90% was estimated.
Analysis Population
The intention‐to‐treat population was defined as those who fulfilled the inclusion criteria. The as‐observed population was defined as those for whom CPR quality and regional OHCA data had been recorded. No imputation was performed. The as‐observed population was the main analysis population.
Statistical Analysis
Baseline characteristics are presented as numbers with corresponding percentages for binary and ordinal variables. Continuous variables are presented as means with corresponding SDs or medians with interquartile ranges.
Shapiro‐Wilk test was used to evaluate a normal distribution of the 5 outcome variables.
The association between CCDiT and real‐time feedback was tested using Wilcoxon rank‐sum test.
The association between the continuous secondary outcomes (CCD, CCR, CCRiT, CCiT, and CCF) and real‐time feedback was also tested using Wilcoxon rank‐sum test. Logistic regression analyses were used to test the association between the binary outcome (ROSC, sROSC, and 30‐day survival) and real‐time feedback. We did not adjust for any confounders as the study phases were controlled by date and hence not affected by potential confounders and thereby not eligible for adjustment. However, a semiadjusted and fully adjusted analysis did not change our results. The adjusted analysis can be found in Table S1.
Results
Participants
A total of 1697 patients were eligible for enrollment. CPR quality data were available for 1065 (62.8%) patients. Pairing CPR quality data with the regional cardiac arrest database resulted in a total of 951 cases. After applying the exclusion criteria, 38 cases were excluded, leaving 913 cases included (Figure 1).
Figure 1. Study flowchart.
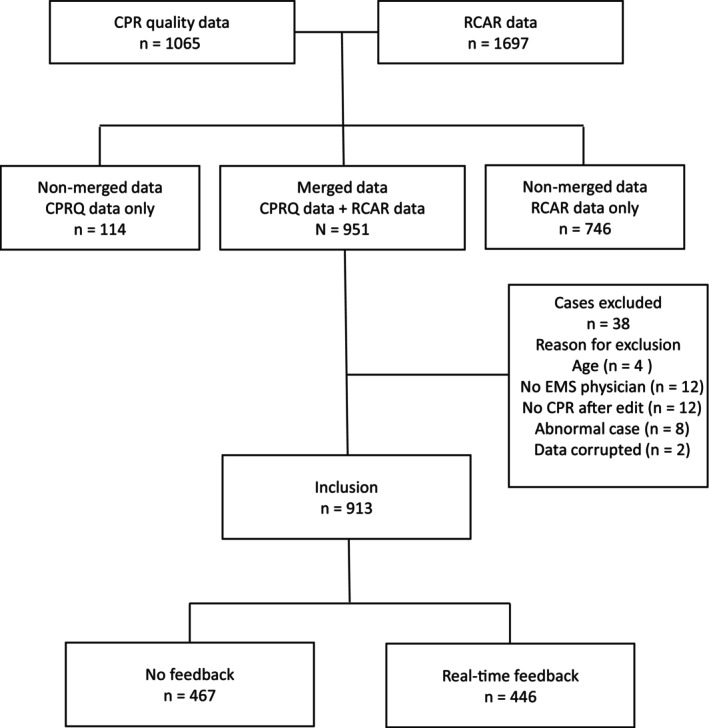
CPR indicates cardiopulmonary‐resuscitation; CPRQ, CPR quality; EMS, emergency medical services; and RCAR, regional cardiac arrest database.
Of the 913 patients included, 467 (51.2%) were in the no‐feedback phase, and 446 (48.9%) were in the real‐time feedback phase. The median (interquartile range) age was 74.0 (63.0–82.0) years, with 64.5% (n=589) being men. The OHCA primarily occurred in private homes (78.9%; n=720), with 48.9% (n=446) witnessed by relatives or bystanders. Bystander CPR was initiated in 68.1% (n=621) of the cases, with bystander defibrillation in 10.1% (n=92) of all cases. Paramedics witnessed the arrest in 9.8% (n=89) of the cases and initiated defibrillation in 27.4% (n=250) of all arrests. Mean (SD) EMS response time was 7.4 (5.4) minutes (Table 1 and Table S2).
Table 1.
Baseline Characteristics
| Out‐of‐hospital cardiac arrest characteristics | ||||
|---|---|---|---|---|
| No feedback | Real‐time feedback | Total | Missing values | |
| Total, N (%) | 467 (51.2) | 446 (48.9) | 913 (100) | … |
| Age, median (IQR), y | 74.0 (62.0–83.0) | 74.5 (63.0–82.0) | 74.0 (63.0–82.0) | 0 |
| Male sex, n (%) | 305 (65.3) | 282 (63.9) | 589 (64.5) | 0 |
| Location: private, n (%)* | 378 (80.9) | 342 (76.9) | 720 (78.9) | 0 |
| First EMS‐recorded rhythm: shockable, n (%) | 81 (17.8) | 77 (17.6) | 158 (17.7) | 22 (2.4) |
| Witnessed by bystander, n (%) | 218 (46.7) | 228 (51.1) | 446 (48.9) | 0 |
| Bystander CPR, n (%) | 332 (71.1) | 289 (64.9) | 621 (68.1) | 1 (<1) |
| Bystander defibrillation, n (%) | 49 (10.5) | 43 (9.6) | 92 (10.1) | 0 |
| Witnessed by EMS, n (%) | 43 (9.2) | 46 (10.3) | 89 (9.8) | 0 |
| EMS defibrillation, n (%) | 129 (27.6) | 121 (27.1) | 250 (27.4) | 0 |
| EMS response time, mean (SD), min | 7.4 (5.9) | 7.3 (4.8) | 7.4 (5.4) | 28 (3.1) |
Baseline characteristics of patients with out‐of‐hospital cardiac arrest included in the study. CPR indicates cardiopulmonary‐resuscitation; EMS, emergency medical services; and IQR, interquartile range.
Location was classified as either private or public.
Primary Outcome
The real‐time feedback group had a statistically significant higher proportion of correct chest compression depth (28.7%) compared with the no‐feedback group (16.6%) (P<0.001) (Figure 2A and Table 2).
Figure 2. Chest compression quality.
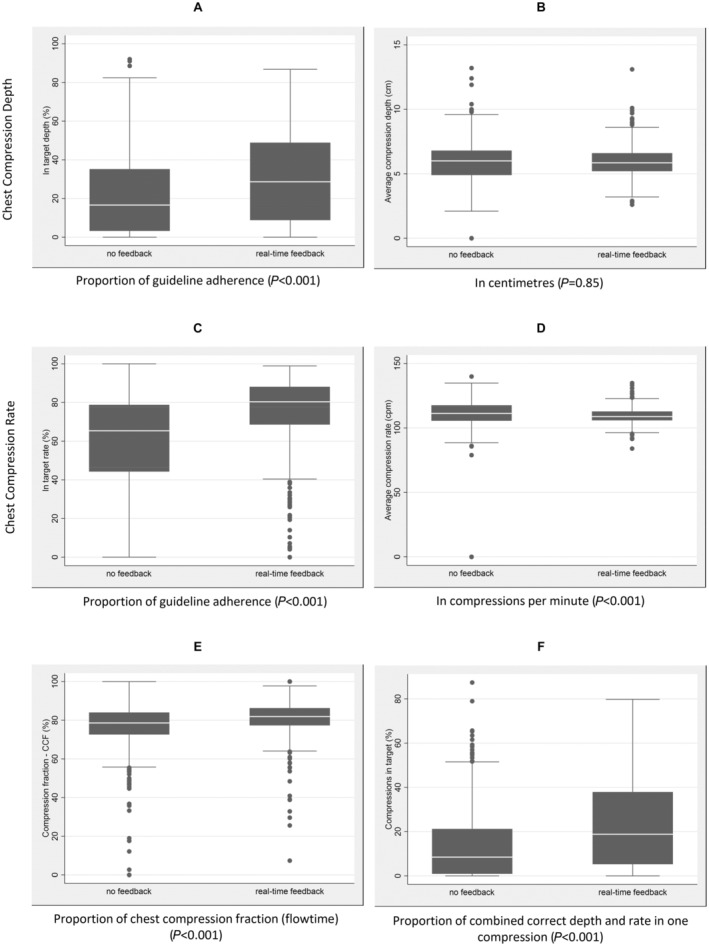
A, Box plots of the proportion of chest compression depth in target. B, Box plots of chest compression depth in centimeters. C, Box plots of the proportion of chest compression rate in target. D, Box plots of chest compression rate in cpm. E, Box plots of CCF (flow time). F, Box plots of combined chest compression depth and rate proportion in target. CCF indicates chest compression fraction; and cpm, compressions per minute.
Table 2.
Outcome Descriptives and Significance
| No feedback | Real‐time feedback | Significance | |||
|---|---|---|---|---|---|
| Variable | No. | Descriptives | No. | Descriptives | probability |
| CCD, median (IQR), cm | 467 | 6.0 (4.9–6.8) | 446 | 5.9 (5.2–6.6) | 0.852 |
| CCDiT, median (IQR), % | 467 | 16.6 (3.3–35.2) | 446 | 28.7 (8.8–48.9) | <0.001 |
| CCR, median (IQR), compressions/min | 467 | 111.3 (105.6–117.6) | 446 | 108.8 (105.9–112.8) | <0.001 |
| CCRiT, median (IQR), % | 467 | 65.4 (44.3–78.8) | 446 | 80.4 (68.6–88.1) | <0.001 |
| CCF, median (IQR), % | 467 | 78.9 (72.6–84.0) | 446 | 81.9 (77.3–86.3) | <0.001 |
| CCiT, median (IQR), % | 467 | 8.5 (0.9–21.2) | 446 | 18.8 (5.3–37.9) | <0.001 |
CCD indicates chest compression depth; CCDiT, CCD in target; CCF, chest compression fraction; CCiT, combined compressions in target; CCR, chest compression rate; CCRiT, CCR in target; and IQR, interquartile range.
Secondary CPR Performance Outcomes
We found a nonsignificant difference between the no‐feedback and the real‐time feedback group for CCD (P=0.85) (Figure 2B and Table 2). The results for CCRiT (P<0.001) (Figure 2C), CCR (P<0.001) (Figure 2D), CCF (P<0.001) (Figure 2E), and CCiT (P<0.001) (Figure 2F) were all significant (Table 2).
Secondary Patient‐Centered Outcome
We found no significant differences in the real‐time feedback group compared with the no‐feedback group for the following: ROSC 31.8% (n=142) versus 33.2% (n=155) (P=0.66), sROSC 23.9% (n=106) versus 27.0% (n=126) (P=0.27), and 30‐day survival 11.5% (n=51) versus 13.7% (n=64) (P=0.30), respectively. Odds ratios are presented in Table 3.
Table 3.
OR and Proportion for Patient‐Centered Outcomes
| Patient‐centered outcome | Phase | No. | Events, n (%) | OR (95% CI) |
|---|---|---|---|---|
| ROSC | No feedback | 467 | 155 (33.2) | 1 (Reference) |
| Real‐time feedback | 446 | 142 (31.8) | 0.94 (0.71–1.24) | |
| sROSC | No feedback | 467 | 126 (27.0) | 1 (Reference) |
| Real‐time feedback | 445 | 106 (23.9) | 0.85 (0.63–1.14) | |
| 30‐d Survival | No feedback | 467 | 64 (13.7) | 1 (Reference) |
| Real‐time feedback | 445 | 51 (11.5) | 0.81 (0.55–1.20) |
OR indicates odds ratio; ROSC, return of spontaneous circulation; and sROSC, sustained ROSC.
Discussion
This study investigated the effect on CPR quality and patient outcome using real‐time feedback for EMS‐attended OHCA. The main study findings are as follows: (1) Despite median chest compression depth in centimeters (CCD) not changing significantly between the groups, the proportion of compressions within guideline recommendations (CCDiT) almost doubled when paramedics were exposed to real‐time feedback. (2) Although median chest compression depth in centimeters (CCD) and median chest compression rate in compressions per minute (CCR) were within guidelines in both groups, the proportion of compressions delivered according to guidelines improved significantly (CCDiT and CCRiT) with real‐time feedback. (3) When combining guideline‐adherent depth and rate simultaneously for every compression delivered (CCiT), CPR quality was generally low but more than doubled with real‐time feedback. Nevertheless, the improvement in CPR quality found with real‐time feedback did not translate into improved ROSC or 30‐day survival; however, our study was not powered for patient outcomes.
Chest Compression Depth and Rate
Interestingly, our study demonstrated that when looking at the median CCD and CCR for the entire resuscitation attempt, these values were within guideline recommendations in both study groups. However, when CCD and CCR were investigated individually for every single compression delivered, only 1 of 6 compressions for depth (CCDiT) and 2 of 3 compressions for rate (CCRiT) were high quality without real‐time feedback. In comparison, the guideline adherence for CCDiT almost doubled, and CCRiT improved by 15% in the real‐time feedback period.
As CPR is associated with a reduction of 60% to 90% of the normal cardiocerebral blood flow, patients with OHCA require each compression throughout the resuscitation to be of high quality to ensure stable hemodynamics. 18 Combining CCDiT and CCRiT into 1 combined CPR compression quality score (CCiT) revealed that only 1 in 11 compressions were of high quality. Intervening with real‐time feedback improved guideline adherence significantly to 1 in 5 compressions for CCiT. Our finding suggests that real‐time feedback can improve CPR quality for depth and rate, both as individual variables and in combination, despite performance already appearing to meet guideline recommendations for high quality when measured as mean centimeters and compressions per minute across the entire resuscitation attempt. Current guidelines recommend compliant depth and rate as individual parameters for high quality but do not emphasize the importance of them being delivered simultaneously in each compression, which our study showed was rarely the case.
The CCDiT and CCRiT improvement and coherent lack of improvement in CCD and CCR could be explained by the approach to OHCA management. European guidelines dictate a change of compressor every 2 minutes to avoid rescuer exhaustion. 4 The change of compressor allows providers to compensate for a team member's noncompliant performance, leading to a better final overall performance. This tendency was seen in some cases where 1 provider performed below guideline recommendations, whereas another team member performed above guideline recommendations. This translated to an average CCD/CCR within guideline recommendations, although CCDiT/CCRiT remained low. In contrast, CCD/CCR could be outside guideline recommendations, whereas CCDiT/CCRiT were high.
Our findings demonstrated an almost identical CCD (−0.1 cm) when providers were exposed to real‐time feedback. This differs from previous studies, where prehospital intervention with real‐time feedback (defibrillator displayed) was reported to improve chest compression depth. 19 , 20 , 21 , 22 Hostler et al was the only study reporting findings as significant. 22 However, to detect an improvement in any measured variable, the starting point is required to allow for an improvement. As paramedics in our study already performed guideline‐adherent CCD without real‐time feedback, this variable did not allow for any improvement. The same tendency was seen for CCR. In contrast, other OHCA studies reported real‐time feedback to improve CCR performance, 19 , 20 , 21 , 22 with both Hostler et al and Lakomen et al reporting findings as significant. 20 , 21 , 22
As previously mentioned, when combining guideline‐adherent chest compression depth and chest compression rate delivered simultaneously in 1 compression (CCiT), we found that only 1 in 11 compressions in the no‐feedback group were within guideline recommendations for both rate and depth delivered in the same compression. This improved to 1 in 5 for the real‐time feedback group. This suggests that CPR quality, measured in centimeters, and compressions per minute as individual variables may be an incomplete measurement for CPR quality. Furthermore, this finding may contribute to understanding the lack of translation of CPR quality improvement into improved patient outcomes in our and previous studies.
Chest Compression Fraction
Our study found a minor but still significant improvement in CCF following real‐time feedback. This finding is supported by Sainio and colleagues 23 but is in contrast to several other studies, 19 , 20 , 21 , 22 , 24 which reported nonsignificant changes favoring both feedback and no feedback. These nonconclusive findings correspond with what could be expected by feedback in real‐time. As real‐time feedback prompts a change in performance during the resuscitation, and CCF is calculated retrospectively, it cannot reasonably be expected to influence providers' performance during the resuscitation attempt. Furthermore, CCF is affected by natural breaks and CCR. If CCR increases, so do the number of ventilation breaks according to the guideline‐recommended 30:2 compression/ventilation ratio. The CCR delivered and potentially guided by real‐time feedback, therefore, affects CCF. In our study, the CPR feedback dashboard displayed a timer activated after a few seconds without chest compressions, which counted the lapsed time without compressions. This feature could explain why we found CCF to improve, as the timer could have directed the providers' attention toward minimizing periods without chest compressions.
Patient‐Centered Outcomes
For the patient‐centered outcomes, we found no significant changes. Similar findings were reported by Bobrow et al and Hostler et al. 19 , 22 OHCA is a multifactor event where the outcome depends on several variables. This could explain our finding as the improvements achieved by intervening with real‐time feedback may not be sufficient to influence clinical outcome despite their statistical significance. Furthermore, performing only 1 in 5 compressions according to guidelines may not be sufficient to affect outcomes. Finally, our study was not powered to detect ROSC or survival benefits.
Technology
The high‐quality CPR recommendations stated by the European Resuscitation Council are based on an average size adult, making CPR a one‐size‐fits‐all approach. Real‐time feedback holds limitations, and circumstances may arise where providers should deviate from the feedback received (eg, in obese or underweight patients, or patients on soft surfaces). In such circumstances, real‐time feedback may inhibit the provider in delivering efficient compressions by providing feedback that either advises to compress deeper (in underweight patients) or informs those compressions are too deep (in obese patients or on soft surfaces). In such incidents, compressions would be registered as non–guideline compliant while they in fact were effective as they were conducted according to patient size. However, current guidelines do not recommend individualized CPR and still recommend an approach based on an average size adult.
Comparing the technology in our study with other technologies was outside the scope of this study but may be a factor in validating the results of our study. In a systematic review by Wang et al, 25 the authors found that outcomes relied on the type of defibrillator used, which may indicate that either technology or presentation of real‐time feedback may be an important factor in real‐time feedback studies. An in‐depth description of the various feedback technologies is described elsewhere. 26
Limitations
Several limitations should be considered when interpreting our results. First, we cannot rule out that our results originate from providers changing practice merely because of knowledge of the observation, also known as the Hawthorne effect; however, if this were the case, it would affect both the no‐feedback and the feedback phases of the study. 27
Unfortunately, it was impossible to do the study as a randomized clinical trial as the setup of the defibrillator did not allow for rapid change of feedback function (on/off), nor was it possible for all ambulances to bring 2 defibrillators, 1 with real‐time feedback and 1 without. The turnover between services and stations was estimated to be ≈25% to 30%, which would have caused a substantial risk of a carryover effect between intervention and control groups; hence, a stepped‐wedge randomized cluster trial was abandoned.
Our study was conducted using a before/after study design. Previous studies have found that well‐designed cohort studies do not introduce a higher risk of bias compared with poor randomized clinical trial designs, which argued for a cohort design despite its limitations.
Our study is also limited by the technology used. We cannot determine the surface on which compressions were delivered. Therefore, if providers have adapted their compression depth to compensate for a soft compressible surface under the patient (eg, a bed), their compressions would be registered as too deep by the sensor and would thereby, despite being clinically correct, be registered as outside guidelines recommendations. This phenomenon is referred to as the mattress effect. 28 , 29 Furthermore, if paramedics were adapting compression depth to patient size with deeper compressions to compensate (individualized CPR), this would be registered as noncompliant compressions. Data were collected using the manufacturer's software. Our data extraction and analysis were limited by the functionality of the software and accessibility to compression‐by‐compression data.
The dynamics of an OHCA includes an initial chaos phase, where it can be suspected that real‐time feedback may provide better support than later in the arrest. However, we did not have access to data on the duration of the arrest. Therefore, we could not perform a time‐specific analysis of the different stages of the arrests or compare the duration and study phases to assess the strength of the association in the different stages of an arrest. Furthermore, we cannot rule out that the use of metronome guidance before our study caused an undetectable carryover effect.
Finally, our estimates were too optimistic in calculating data loss, and we did not reach the required sample size.
Conclusions
On the basis of 916 patients, real‐time feedback was associated with improved chest compression depth, chest compression rate (individually and combined), and chest compression fraction guideline compliance. Overall quality for combined depth and rate was low but doubled with real‐time feedback. Furthermore, our study indicates that current measurements of CPR quality should not be limited to average centimeters and compressions per minute for chest compression depth and chest compression rate but expanded to contain proportion within guideline recommendations both as individual variables and in combination.
Sources of Funding
This work was supported by TrygFonden, Denmark (grant number 125963). CaseReview software was provided free of charge by ZOLL Medical Corporation for the duration of the study.
Disclosures
None.
Ethical Approval
We applied for ethical approval from The Danish National Committee on Health Research Ethics (H‐18016462). The committee waived formal approval. Permission to collect data was obtained from the Danish Data Protection Agency (P‐2021‐670). Permission to store data was obtained from the Centre for Regional Development (R‐2005114). According to Danish legislation, the study was regarded and conducted as quality assurance, which does not require patient consent.
Supporting information
Data S1
Acknowledgments
The authors wish to thank Lyra Clark and Annemarie Silver from ZOLL Medical Corporation for providing technical support throughout the study. Author contributions: Rasmus Meyer Lyngby: funding acquisition, project administration, conceptualization, investigation, methods, formal analysis, data curation, and writing (original draft, review, and editing); Tom Quinn: conceptualization, methods, supervision, and writing (review and editing); Julie Samsoee Kjoelbye: writing (review and editing); Mads Tofte Gregers: writing (review and editing); Annette Kjaer Ersbøll: methods, formal analysis, and writing (review and editing); Roselil Maria Oelrich: data curation, validation, and review and editing; Dimitra Nikoletou: methods, supervision, and writing (review and editing); Fredrik Folke: conceptualization, funding acquisition, project administration, supervision, formal analysis, methods, and writing (review and editing).
This article was sent to Saket Girotra, MD, SM, Associate Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.123.029457
For Sources of Funding and Disclosures, see page 10.
References
- 1. Gräsner J‐T, Lefering R, Koster RW, Masterson S, Böttiger BW, Herlitz J, Wnent J, Tjelmeland IBM, Ortiz FR, Maurer H, et al. EuReCa ONE 27 nations, ONE Europe, ONE registry: a prospective one month analysis of out‐of‐hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004 [DOI] [PubMed] [Google Scholar]
- 2. Dyson K, Brown SP, May S, Smith K, Koster RW, Beesems SG, Kuisma M, Salo A, Finn J, Sterz F, et al. International variation in survival after out‐of‐hospital cardiac arrest: a validation study of the Utstein template. Resuscitation. 2019;138:168–181. doi: 10.1016/j.resuscitation.2019.03.018 [DOI] [PubMed] [Google Scholar]
- 3. Gräsner J‐T, Herlitz J, Tjelmeland IBM, Wnent J, Masterson S, Lilja G, Bein B, Böttiger BW, Rosell‐Ortiz F, Nolan JP, et al. European resuscitation council guidelines 2021: epidemiology of cardiac arrest in Europe. Resuscitation. 2021;161:61–79. doi: 10.1016/j.resuscitation.2021.02.007 [DOI] [PubMed] [Google Scholar]
- 4. Olasveengen TM, Semeraro F, Ristagno G, Castren M, Handley A, Kuzovlev A, Monsieurs KG, Raffay V, Smyth M, Soar J, et al. European resuscitation council guidelines 2021: basic life support. Resuscitation. 2021;161:98–114. doi: 10.1016/j.resuscitation.2021.02.009 [DOI] [PubMed] [Google Scholar]
- 5. Semeraro F, Greif R, Böttiger BW, Burkart R, Cimpoesu D, Georgiou M, Yeung J, Lippert F, S Lockey A, Olasveengen TM, et al. European resuscitation council guidelines 2021: systems saving lives. Resuscitation. 2021;2021(161):80–97. doi: 10.1016/j.resuscitation.2021.02.008 [DOI] [PubMed] [Google Scholar]
- 6. Lyngby RM, Clark L, Kjoelbye JS, Oelrich RM, Silver A, Christensen HC, Barfod C, Lippert F, Nikoletou D, Quinn T, et al. Higher resuscitation guideline adherence in paramedics with use of real‐time ventilation feedback during simulated out‐of‐hospital cardiac arrest: a randomised controlled trial. Resuscitation Plus. 2021;5:100082. doi: 10.1016/j.resplu.2021.100082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lyngby RM, Händel MN, Christensen AM, Nikoletou D, Folke F, Christensen HC, Barfod C, Quinn T. Effect of real‐time and post‐event feedback in out‐of‐hospital cardiac arrest attended by EMS—a systematic review and meta‐analysis. Resuscitation Plus. 2021;6:100101. doi: 10.1016/j.resplu.2021.100101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Olasveengen TM, Mancini ME, Perkins GD, Avis S, Brooks S, Castrén M, Chung SP, Considine J, Couper K, Escalante R, et al. Adult basic life support: international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A35–A79. doi: 10.1016/j.resuscitation.2020.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gantzel Nielsen C, Andelius LC, Hansen CM, Blomberg SNF, Christensen HC, Kjølbye JS, Tofte Gregers MC, Ringgren KB, Folke F. Bystander interventions and survival following out‐of‐hospital cardiac arrest at Copenhagen international airport. Resuscitation. 2021;162:381–387. doi: 10.1016/j.resuscitation.2021.01.039 [DOI] [PubMed] [Google Scholar]
- 10. Nadarajan GD, Tiah L, Ho AFW, Azazh A, Castren MK, Chong SL, El Sayed MJ, Hara T, Leong BS, Lippert FK, et al. Global resuscitation alliance utstein recommendations for developing emergency care systems to improve cardiac arrest survival. Resuscitation. 2018;132:85–89. doi: 10.1016/j.resuscitation.2018.08.022 [DOI] [PubMed] [Google Scholar]
- 11. Andelius L, Malta Hansen C, Lippert FK, Karlsson L, Torp‐Pedersen C, Kjær Ersbøll A, Køber L, Collatz Christensen H, Blomberg SN, Gislason GH, et al. Smartphone activation of citizen responders to facilitate defibrillation in out‐of‐hospital cardiac arrest. J Am Coll Cardiol. 2020;76:43–53. doi: 10.1016/j.jacc.2020.04.073 [DOI] [PubMed] [Google Scholar]
- 12. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 13. Denmark TCRo . Demographics 2019. Capital Region of Denmark. 2019. Accessed August 6, 2019. https://www.regionh.dk/om‐region‐hovedstaden/fakta/geografi/Sider/Geografi.aspx.
- 14. Denmark TCRo . Emergency Medical Services 2019. 2019. Accessed 10 September 2019. https://www.regionh.dk/english/Healthcare‐Services/Emergency‐Medical‐Services/Copenhagen‐Emergency‐medical‐services/Pages/Ambulances.aspx.
- 15. Denmark TCRo . Årsrapport 2020. 2020. Accessed 2 June 2021. https://www.regionh.dk/til‐fagfolk/Om‐Region‐H/region‐hovedstadens‐akutberedskab/Akutberedskabets‐aktivitetsdata‐/Documents/Akutbedredskabet_aaarsrapport_2020.pdf.
- 16. Blomberg SN, Christensen HC, Lippert F, Ersbøll AK, Torp‐Petersen C, Sayre MR, Kudenchuk PJ, Folke F. Effect of machine learning on dispatcher recognition of out‐of‐hospital cardiac arrest during calls to emergency medical services: a randomized clinical trial. JAMA Netw Open. 2021;4:e2032320. doi: 10.1001/jamanetworkopen.2020.32320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Linderoth G, Rosenkrantz O, Lippert F, Østergaard D, Ersbøll AK, Meyhoff CS, Folke F, Christensen HC. Live video from bystanders’ smartphones to improve cardiopulmonary resuscitation. Resuscitation. 2021;168:35–43. doi: 10.1016/j.resuscitation.2021.08.048 [DOI] [PubMed] [Google Scholar]
- 18. Meaney PA, Bobrow BJ, Mancini ME, Christenson J, Caen AR, Bhanji F, Abella BS, Kleinman ME, Edelson DP, Berg RA, et al. Cardiopulmonary resuscitation quality: improving cardiac resuscitation outcomes both inside and outside the hospital. Circulation. 2013;128:417–435. doi: 10.1161/CIR.0b013e31829d8654 [DOI] [PubMed] [Google Scholar]
- 19. Bobrow BJ, Vadeboncoeur TF, Stolz U, Silver AE, Tobin JM, Crawford SA, Mason TK, Schirmer J, Smith GA, Spaite DW. The influence of scenario‐based training and real‐time audiovisual feedback on out‐of‐hospital cardiopulmonary resuscitation quality and survival from out‐of‐hospital cardiac arrest. Ann Emerg Med. 2013;62:47–56.e41. doi: 10.1016/j.annemergmed.2012.12.020 [DOI] [PubMed] [Google Scholar]
- 20. Lakomek F, Lukas R‐P, Brinkrolf P, Mennewisch A, Steinsiek N, Gutendorf P, Sudowe H, Heller M, Kwiecien R, Zarbock A, et al. Real‐time feedback improves chest compression quality in out‐of‐hospital cardiac arrest: a prospective cohort study. PLoS One. 2020;15:e0229431. doi: 10.1371/journal.pone.0229431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lakomek F, Lukas R‐P, Brinkrolf P, Mennewisch A, Steinsiek N, Gutendorf P, Sudowe H, Heller M, Kwiecien R, Zarbock A, et al. Correction: real‐time feedback improves chest compression quality in out‐of‐hospital cardiac arrest: a prospective cohort study. PLoS One. 2020;15:e0232672. doi: 10.1371/journal.pone.0232672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hostler D, Everson‐Stewart S, Rea TD, Stiell IG, Callaway CW, Kudenchuk PJ, Sears GK, Emerson SS, Nichol G. Effect of real‐time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster‐randomised trial. BMJ. 2011;342:d512. doi: 10.1136/bmj.d512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sainio M, Kämäräinen A, Huhtala H, Aaltonen P, Tenhunen J, Olkkola KT, Hoppu S. Real‐time audiovisual feedback system in a physician‐staffed helicopter emergency medical service in Finland: the quality results and barriers to implementation. Scand J Trauma Resusc Emerg Med. 2013;21:50. doi: 10.1186/1757-7241-21-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Leis CC, González VA, Hernandez RDE, Sanchez O, Martin JLM, Hermosa EJM, Torres EC. Feedback on chest compression quality variables and their relationship to rate of return of spontaneous circulation. Emergencias. 2013;25:99–104. [Google Scholar]
- 25. Wang S‐A, Su C‐P, Fan H‐Y, Hou W‐H, Chen Y‐C. Effects of real‐time feedback on cardiopulmonary resuscitation quality on outcomes in adult patients with cardiac arrest: a systematic review and meta‐analysis. Resuscitation. 2020;155:82–90. doi: 10.1016/j.resuscitation.2020.07.024 [DOI] [PubMed] [Google Scholar]
- 26. Digna MG‐O, Ruiz S, De G, Jesus MR, José Julio G, Purificación S, Mikel L. Audiovisual feedback devices for chest compression quality during CPR. In: Theodoros A, ed Resuscitation Aspects. Rijeka: IntechOpen; 2017. [Google Scholar]
- 27. Wickström G, Bendix T. The "Hawthorne effect"–what did the original Hawthorne studies actually show? Scand J Work Environ Health. 2000;26:363–367. doi: 10.5271/sjweh.555 [DOI] [PubMed] [Google Scholar]
- 28. Hellevuo H, Sainio M, Huhtala H, Olkkola KT, Tenhunen J, Hoppu S. The quality of manual chest compressions during transport–effect of the mattress assessed by dual accelerometers. Acta Anaesthesiol Scand. 2014;58:323–328. doi: 10.1111/aas.12245 [DOI] [PubMed] [Google Scholar]
- 29. Hellevuo H, Sainio M, Tenhunen J, Hoppu S. The quality of manual chest compressions during transport–can we handle mattress effect with feedback devices. Resuscitation. 2012;83:e47. doi: 10.1016/j.resuscitation.2012.08.119 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1


