Abstract
Background:
Prenatal diagnosis of congenital heart disease (CHD) often leads to anxiety, depression, and traumatic stress in expectant mothers, with long-term implications for the child and family. However, psychosocial intervention is rarely incorporated into prenatal care. HEARTPrep is a virtually-delivered psychosocial intervention aimed at reducing distress and social isolation and increasing parenting self-efficacy and hope for mothers expecting a baby with CHD to promote long-term child/family wellbeing. This study evaluated the feasibility and acceptability of HEARTPrep.
Materials and Methods:
Participants were mothers receiving cardiology care for a fetal CHD diagnosis. Partners could participate with the mother. HEARTPrep was delivered through a mobile app and telehealth. Feasibility was assessed through enrollment/retention rates. Acceptability was assessed through 20 Likert-scale and five open-ended questions.
Results:
Of 39 recruited mothers, 35 (90%) enrolled. Half of partners (48%) also participated. Twenty-seven of 35 enrolled mothers (77%) completed HEARTPrep. On a scale from 0 (Not at All) to 4 (Very), mean item acceptability scores ranged from 3.5 – 3.9. Mothers reported HEARTPrep helped them feel less distressed (mean: 3.74), less alone (3.84), more prepared (3.89), and more hopeful (3.84). Opportunities to process emotions, develop coping skills, learn with their partner, navigate relationships, understand they are not alone, connect with peer support, access resources, and prepare for stressors were described as helpful.
Conclusions:
HEARTPrep is feasible and acceptable for mothers expecting a baby with CHD. Future research will evaluate its efficacy in preventing/reducing maternal mental health problems and improving postnatal clinical outcomes.
Keywords: fetal, prenatal diagnosis, pregnancy, mental health, parent, family
Introduction
Congenital heart disease (CHD) is the most common birth defect, affecting nearly 1% of births.1 Approximately 25% of infants born with CHD will require cardiac surgery within their first year of life, often during the neonatal period.2 Due to advancements in fetal imaging, CHD is increasingly diagnosed prenatally.3 Prenatal diagnosis of CHD allows for prenatal counseling, parental education and support, and careful planning for delivery and postnatal care.4 Prenatal diagnosis of CHD is associated with better neonatal outcomes including improved oxygenation, less cardiac dysfunction, and fewer neurologic sequelae by allowing for rapid intervention and stabilization after birth.4–6
There is growing recognition of the psychosocial impact of prenatal CHD diagnosis on expectant parents.7,8 Pregnancy is a vulnerable time for mental health, with elevated rates of stress, anxiety, and depression even in women carrying a healthy fetus (10–25%).9,10 However, when a fetus is diagnosed with CHD, rates of stress, anxiety, and depression can be 2 to 3 times higher (22–65%).11,12 Traumatic stress symptoms (e.g., intrusive thoughts, hyperarousal) are also common (39%) after learning that the fetus has a life-threatening heart condition.12 Qualitative research on the lived experiences of families who received a prenatal diagnosis of CHD indicate that many expectant parents feel terrified, isolated, hopeless, and emotionally unprepared, which can lead to long-term parental mental health difficulties.13
There is a large body of research linking perinatal mental health with fetal and child outcomes. In the general population, maternal stress and trauma during pregnancy have been associated with preterm birth, low birthweight, developmental delays, neurocognitive impairments, and emotional and behavioral difficulties.14 Importantly, these associations seem to be stronger among certain high-risk groups, such as those with social disadvantage (e.g., low income) or greater severity of maternal mental health difficulties.15 A recent study of mothers carrying a fetus with CHD found that maternal stress during pregnancy was associated with smaller fetal hippocampal and cerebellar volumes.11 Other studies have shown associations between maternal mental health and neurodevelopmental and psychosocial outcomes for children with CHD,16–18 with maternal mental health often serving as a stronger predictor of child psychosocial outcomes than medical and surgical factors.18
Despite this evidence, formal psychosocial interventions are rarely provided after prenatal diagnosis of a birth defect, including CHD. Parents of children with CHD identified a lack of preparation for the emotional impacts of CHD (e.g., potential for parental anxiety, depression, and traumatic stress reactions, impact of stress on family relationships) as a critical unmet need.19 Among parents whose child was diagnosed with CHD prenatally, most reported needing, but not receiving, psychosocial intervention during the pregnancy (88% of mothers and 80% of fathers).20 Yet to date, there are no published data on the actual feasibility and acceptability of psychosocial intervention for mothers expecting a baby with CHD.
Recently, a team of multidisciplinary healthcare professionals and parent stakeholders from eight pediatric health systems (PEDSnet21) co-designed HEARTPrep, a virtually-delivered, psychosocial intervention aimed at reducing distress and social isolation and increasing parenting self-efficacy and hope among mothers expecting a baby with CHD to promote long-term family and child wellbeing.13 This paper reports on a pilot study of HEARTPrep, examining its acceptability and feasibility within one health system.
Material and Methods
Participants
This study was reviewed and approved by the Nemours Children’s Health Institutional Review Board. Participants were expectant mothers receiving cardiology care for a fetal diagnosis of CHD through Nemours Children’s Health. Partners could participate with the expectant mother. To be eligible, expectant mothers and partners had to be age 18 or older and fluent in English. Expectant mothers who had an older child with CHD were excluded, as their experiences and needs likely differ from those receiving their first fetal CHD diagnosis. The anticipated infant care plan had to include cardiac surgery at Nemours Children’s Health at less than 12 months of age. Genetic and congenital comorbidities were permitted, with the exception of those associated with a life expectancy of less than one year (e.g., Trisomy 18).
Mothers had to be referred for study participation by 30 weeks gestation to ensure sufficient time for HEARTPrep prior to the birth. Mothers who transferred care to another health system after enrollment were no longer considered eligible, as HEARTPrep was delivered through the Nemours app, which is currently specific to one health system.
Recruitment and Enrollment
Recruitment spanned approximately one year, beginning at Nemours Children’s Hospital-Delaware in Wilmington, DE (NCH-D) in August 2021. Nemours Children’s Hospital-Florida in Orlando, FL (NCH-F) was added in May 2022. Eligible expectant mothers were informed about the study by their perinatal nurse coordinator during a fetal cardiology appointment or by phone. Those who expressed interest were referred for study participation and were contacted by phone to conduct informed consent. Expectant mothers who enrolled were encouraged to invite their partner to participate. The decision regarding whether to invite the partner was left to the expectant mother. Informed consent for both mothers and partners was documented via DocuSign.
Intervention
HEARTPrep is a virtually-delivered, psychosocial intervention for women expecting a baby with CHD. HEARTPrep consists of 3–6 live telehealth sessions (45–60 minutes each) delivered through the Nemours App (a mobile app supported by the health system and used by both NCH-D and NCH-F). HEARTPrep focuses on six core components: 1) normalizing and processing emotions, 2) developing coping skills, 3) engaging a supportive network, 4) connecting with peer-to-peer support, 5) accessing supportive resources, and 6) exploring the role of cultural beliefs and faith. The initial co-design of HEARTPrep was described previously (Sood et al., 2022).
HEARTPrep was conducted by a licensed clinical psychologist or a psychology fellow, each with experience working in a pediatric cardiac center. The psychology providers for HEARTPrep were based at NCH-D but were familiar with the care team and model of care at NCH-F and provided HEARTPrep to participants in both locations. HEARTPrep sessions were conducted individually with each family (expectant mother or mother/partner dyad). Flexibility was prioritized when determining number of sessions and spacing of sessions to meet the individual needs of families. Participants were told that most families complete between 3–6 sessions on an every-other week basis during the pregnancy, but more frequent sessions or additional sessions beyond six (up to 12) could be scheduled when needed or requested. Telehealth sessions were scheduled Monday through Friday during business hours or evenings, based on family and provider availability. Expectant mothers could participate from anywhere that was convenient for them (e.g., home, parked car). Partners participated in telehealth sessions together with the expectant mother, either from the same room or conferenced in from a separate location (e.g., workplace). Participants were paid $10 per completed session via reloadable debit card for their time dedicated to the study.
Measures
Maternal and fetal clinical and demographic characteristics were extracted from the electronic medical record. Area Deprivation Index (national percentile rankings from 1 [lowest level of disadvantage] to 100 [highest level of disadvantage]) was determined based on street address.22 Rates of enrollment and completion, number of sessions, and reasons for non-enrollment and non-completion were tracked as measures of feasibility. Expectant mothers completed the HEARTPrep Evaluation Survey (Online Resource 1) via REDCap23 after session 3 and again after the final session for those who completed six or more sessions. This survey consists of 4-point Likert-Scale items assessing perceived acceptability (16 items; e.g., “I have been satisfied with HEARTPrep”) and helpfulness (4 items; e.g., “HEARTPrep has helped me feel less distressed”). Five open-ended questions were also included (e.g., “What are the most helpful parts of HEARTPrep?”). The HEARTPrep Evaluation Survey was modified from an existing measure used to assess the perceived acceptability of a virtually-delivered psychosocial intervention for parents of children with cancer.24 Participants were paid $25 per completed survey as compensation for their time.
Analysis
Measures of feasibility were evaluated using descriptive statistics (e.g., percent enrolled, mean/median number of sessions, percent completed). Likert-scale responses to the HEARTPrep Evaluation Survey were also analyzed using descriptive statistics. For expectant mothers who completed the survey twice (i.e., those who completed six or more sessions), responses to the second survey were used for analyses to incorporate their perspectives on their full participation. Open-ended responses across all surveys completed (1–2 per participant) were categorized by theme using qualitative methods.
Results
Feasibility: Rates of Enrollment and Sample Diversity
Perinatal nurse coordinators approached 39 eligible expectant mothers. All approached mothers expressed interest and were referred for study participation. Four additional expectant mothers were not able to be reached by phone by a perinatal nurse coordinator and were therefore not informed about the study. Prenatal CHD diagnosis after 30 weeks gestation was the most common reason for exclusion among expectant mothers carrying a fetus with CHD anticipated to undergo infant cardiac surgery at Nemours Children’s Health.
Of the 39 expectant mothers contacted by a member of the study team, 35 (90%) enrolled. Participants were diverse with regard to age (ranging from 19 – 41 years), race, ethnicity, insurance type, and fetal cardiac diagnosis. Those who initially expressed interest but chose not to enroll indicated that they were doing well coping with the CHD diagnosis (N = 2), were already working with a mental health professional and felt their needs were being met (N = 1), or were too busy (N = 1). Mean gestational age was 25.6 weeks (range 17 – 32) at time of enrollment and 26.6 weeks (range 21 – 32) at time of first telehealth session.
Feasibility: Intervention Engagement and Completion
Twenty-seven of the 35 enrolled expectant mothers (77%) completed HEARTPrep (Figure 1). Three-quarters of these mothers attended between 3–6 telehealth sessions (10 attended three sessions, 9 attended four, and 1 attended six), whereas one-quarter attended additional telehealth sessions (3 attended seven and 4 attended between 8–12 sessions) due to new stressors (e.g., new genetic diagnosis, significant life changes) or family perceptions that additional sessions would be helpful leading up to the birth. Reasons for non-completion were being too busy (N = 3), transferring care to a different health system (N = 2), scheduling difficulties (N = 1), early delivery (N = 1), and fetal demise (N = 1
Fig. 1. HEARTPrep Enrollment and Completion Rates.
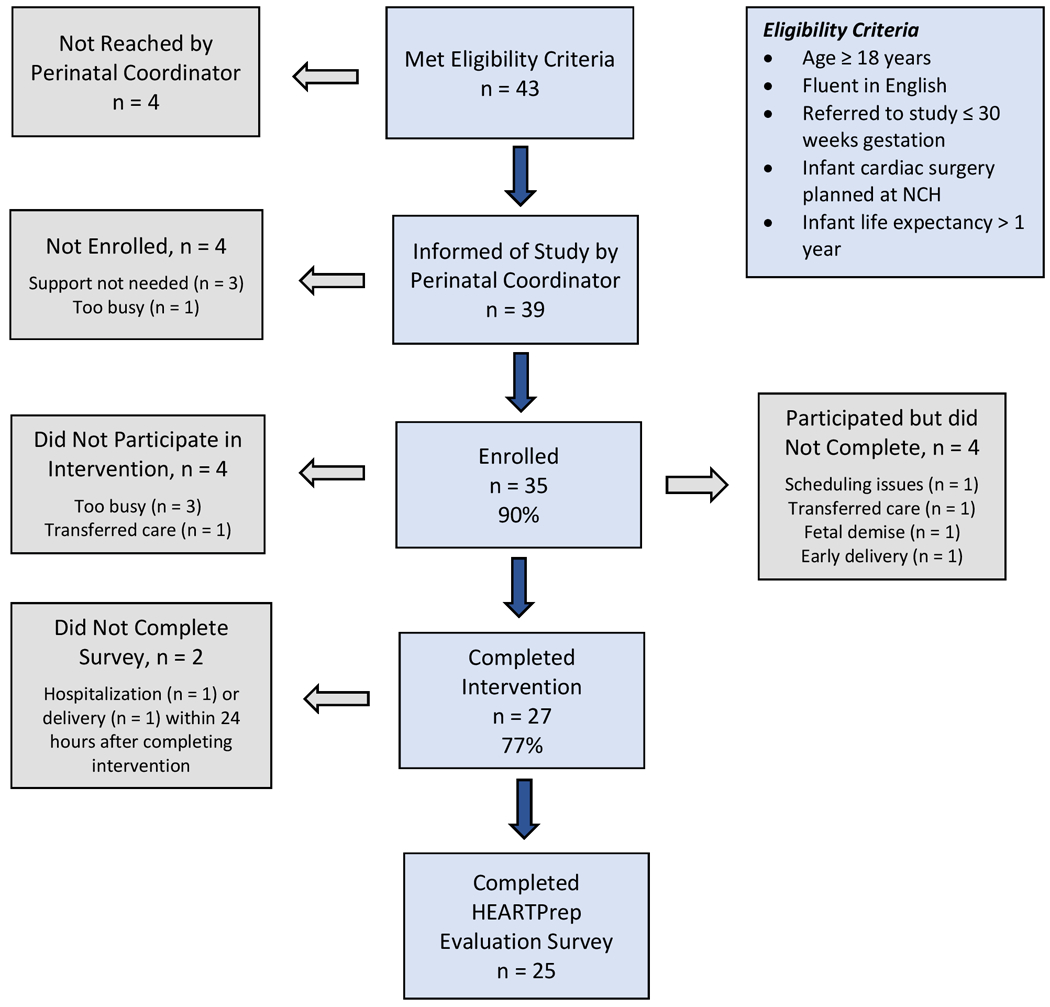
Ninety percent of recruited mothers chose to enroll and 77% of enrolled mothers completed HEARTPrep, indicating that HEARTPrep is feasible for mothers expecting a baby with congenital heart disease.
Note. CHD = congenital heart disease, NCH = Nemours Children’s Health
Clinical and sociodemographic characteristics did not differ between those who did and did not complete HEARTPrep, including Area Deprivation Index (51.4 ± 17.3 vs. 49.5 ± 19.8). Although the proportions of mothers who identified as Black or African-American and had Medicaid insurance were somewhat lower and the proportion of mothers carrying a fetus with single-ventricle physiology was somewhat higher among those who completed as compared to those who did not, these differences did not reach statistical significance (ps > 0.2) (Table 1).
Table 1.
Maternal and Fetal Characteristics
| Maternal/Fetal Characteristic a | Completers (N = 27) | Non-Completers (N = 8) b |
|---|---|---|
| Maternal Age (Years) | ||
| 18–24 | 6 (22.2%) | 3 (37.5%) |
| 25–29 | 7 (25.9%) | 2 (25%) |
| 30–34 | 9 (33.3%) | 1 (12.5%) |
| 35–41 | 5 (18.5%) | 2 (25%) |
| Maternal Race/Ethnicity | ||
| Non-Hispanic White | 17 (63%) | 4 (50%) |
| Hispanic/Latina | 4 (14.8%) | 1 (12.5%) |
| Black or African American | 5 (18.5%) | 3 (37.5%) |
| Asian | 1 (3.7%) | 0 |
| Maternal Insurance Type | ||
| Private/Military | 20 (74.1%) | 4 (50%) |
| Medicaid | 7 (25.9%) | 4 (50%) |
| Area Deprivation Index c | 51.4 ± 17.3 | 49.5 ± 19.8 |
| Fetal Diagnoses | ||
| Single-Ventricle Physiology d | 8 (29.6%) | 1 (12.5%) |
| Down Syndrome | 4 (14.8%) | 1 (12.5%) |
| Extracardiac Anomaly | 2 (7.4%) | 0 |
Most characteristics reported as N (%).
No group differences reached statistical significance.
Area Deprivation Index reported as mean percentile ± standard deviation. Higher percentiles reflect a higher level of disadvantage.
Confirmed or suspected single-ventricle physiology. All others had confirmed or suspected biventricular physiology.
Fifteen partners participated with the expectant mother, representing 48% of families who participated in or completed HEARTPrep. Nine of 15 participating partners (60%) attended 3 or more sessions (ranging from 3–10 sessions). The most common reasons provided for partner non-participation or non-completion were work schedules or competing demands.
Acceptability
Twenty-five expectant mothers completed the HEARTPrep Evaluation Survey (2 missing due to hospitalization or delivery within 24 hours of third session). Figure 2 displays results of the 16-item scale assessing perceived acceptability (mean item scores ranged from 3.5 – 3.9 on a 0 – 4 scale).
Fig. 2. Perceived Acceptability of HEARTPrep.
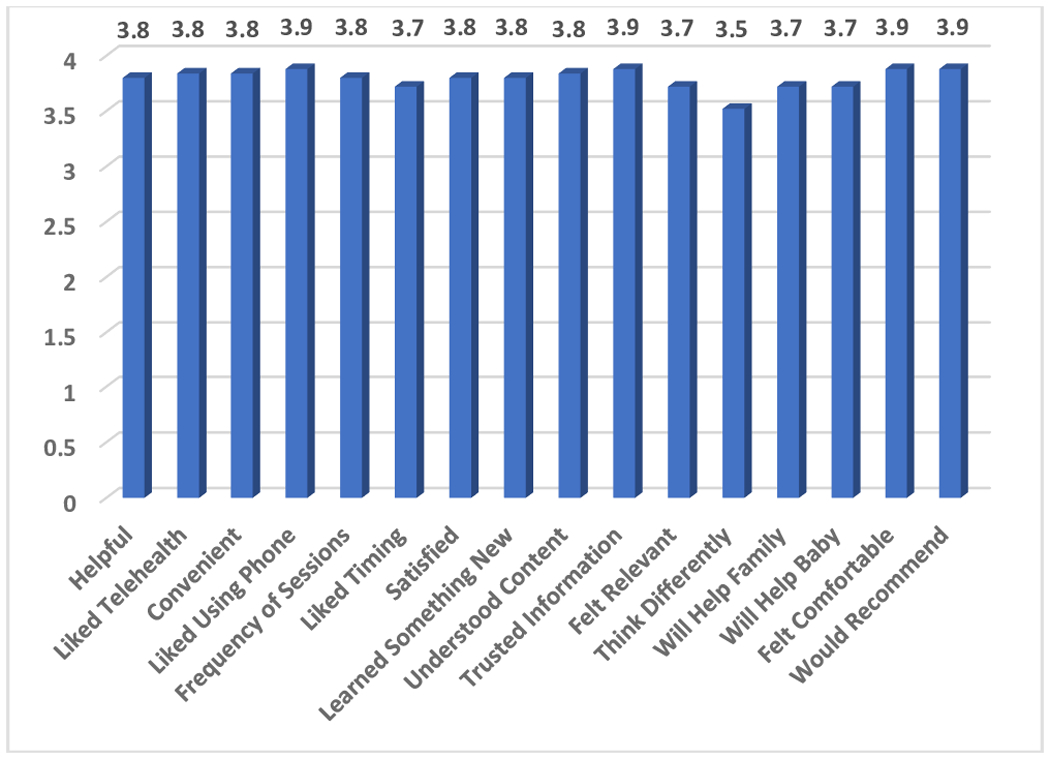
The HEARTPrep Evaluation Survey assessed mothers’ perceptions regarding the acceptability of HEARTPrep. Mean item scores ranged from 3.5 – 3.9 on a 0 (Not At All True) to 4 (Very True) scale, indicating that HEARTPrep is perceived as acceptable to mothers expecting a baby with congenital heart disease.
Note. Full survey questions displayed in Online Resource 1.
Perceived acceptability did not differ significantly between mothers who completed 3 telehealth sessions (mean ± SD = 3.75 ± 0.51) versus 6 or more sessions (3.87 ± 0.34). Expectant mothers perceived that HEARTPrep helped them feel less distressed (3.74 ± 0.45), less alone (3.84 ± 0.37), more informed and prepared (3.89 ± 0.32), and more hopeful (3.84 ± 0.37) (Figure 3).
Fig. 3. Perceived Helpfulness of HEARTPrep.
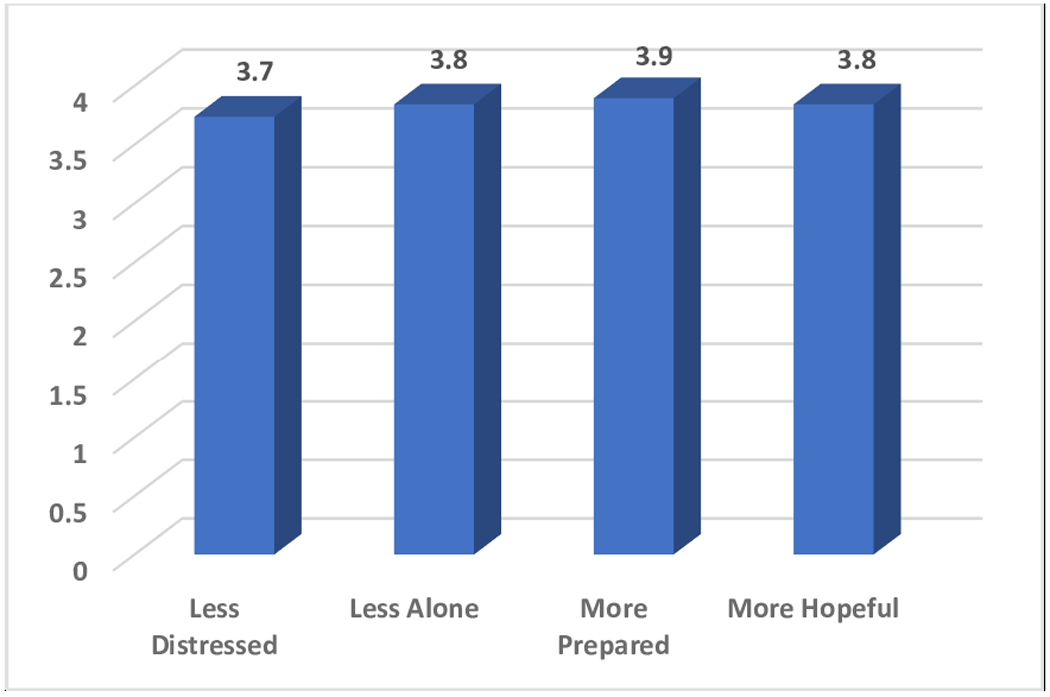
The HEARTPrep Evaluation Survey assessed mothers’ perceptions regarding the helpfulness of HEARTPrep in reducing distress and social isolation and increasing parenting self-efficacy and hope. On a 0 – 4 scale, mothers perceived that HEARTPrep helped them feel less distressed and alone and more prepared, and hopeful, providing preliminary evidence that HEARTPrep may improve maternal outcomes.
Note. Survey prompt was “HEARTPrep has helped me feel…”
Themes from maternal responses to open-ended survey questions are displayed in Table 2. Responses indicated that the opportunity to process emotions and have their feelings validated, develop coping skills, learn together with their partner, navigate relationships, understand that they are not alone in this experience, connect with peer-to-peer support, access relevant resources, and prepare for stressors after the birth were perceived as helpful. Some participants recommended more opportunities for peer-to-peer support, more information on what to expect after the birth, and continuity of psychosocial support in the postnatal period. The delivery of HEARTPrep through the Nemours app was described by the vast majority of mothers as convenient and accessible, although one mother stated that she would have liked the opportunity to also meet in person.
Table 2.
Themes and Representative Quotes from Survey Responses
| Helpful Aspects of HEARTPrep | |
|---|---|
| Themes | Representative Quotes |
| Processing emotions and having feelings validated | This program has helped me process emotions and prepare for this life changing event. I feel more supported than I ever have before in motherhood. Giving families the tools they need to process emotions and move through heavy news during pregnancy is important. |
| Developing coping skills | Talking out my feelings and coming up with strategies to cope. |
| Learning together with partner | Being able to do this with my husband has been very valuable in making sure we keep that line of communication open and we are learning together! [HEARTPrep] made us feel like we had someone in our corner and could ask for help anytime. |
| Navigating relationships | Exploring my feelings and how my husband and I are handling it different. |
| Understanding they are not alone | It’s been helpful realizing there is a whole community of people in similar situations and that there is a plethora of resources at our disposal. |
| Connecting with peer-to-peer support | I really like that I was given the opportunity to connect with another parent with a child that has my son’s condition. |
| Accessing relevant resources | All the resources we have received to this point have been amazing and I [am] feeling more connected and learning more about this particular condition. |
| Preparing for stressors after the birth | It was super helpful to get lots of tips and info on what to expect. |
| Recommendations to Improve HEARTPrep | |
| Themes | Representative Quotes |
| More opportunities for peer-to-peer support | Connecting with other families is so helpful and makes this process a little bit easier. It would be nice to have a local group you could join and talk with. |
| More information on what to expect after the birth | Explaining the steps after babies are born in more detail, meaning appointments and how Nemours continues to monitor after surgery for developmental aspects. |
| Continuity of psychosocial support after the birth | Maybe extending HEARTPrep even after birth or creating a program that extends from HEARTPrep to the experiences you have after the birth of the baby. |
Discussion
Despite growing recognition of the psychosocial impact of a prenatal CHD diagnosis on expectant parents,7,8 formal psychosocial intervention is rarely incorporated into prenatal care for women carrying a fetus with CHD. The present study provides initial evidence that virtually-delivered psychosocial intervention can be feasibly implemented to diverse mothers expecting a baby with CHD and their partners. HEARTPrep was perceived by expectant mothers as relevant, convenient, and helpful for reducing distress and social isolation and increasing parenting self-efficacy and hope.
Enrollment rates were very high (90%). Rates of enrollment across prior studies of psychosocial intervention for families affected by critical or chronic illness vary widely, with most in the range of 20 – 70%.25,26 Some parents in prior studies have expressed reluctance to participate in interventions focused on their own wellbeing, which they worry could divert time and attention away from their child’s care.20,27 However, when the child is in-utero, expectant mothers likely understand that their own wellbeing is intrinsically linked to their child’s wellbeing,7 potentially accepting psychosocial intervention at higher rates. Additionally, having the study introduced by perinatal nurse coordinators directly involved in fetal cardiology care likely facilitated recruitment. Lastly, barriers to providing parent-focused psychosocial intervention in a children’s hospital setting are minimized when the mother is the patient, as in the setting of fetal cardiology care. It is important to note that financial barriers to psychosocial intervention (e.g., co-payments, health insurance claim denials) are removed within the context of research funding. While psychologists can often bill for mental health services associated with the management of health conditions (e.g., health and behavior codes), reimbursement rates vary.28 Expectant mothers interested in participating in psychosocial intervention may face financial barriers outside the research context unless alternative sources of funding are identified.
Rates of intervention completion (77%) were also high, and many expectant mothers chose to participate in more sessions than required for completion. Open-ended survey responses suggested that the core components of HEARTPrep (e.g., normalizing and processing emotions, developing coping skills, connecting with peer-to-peer support, accessing supportive resources) were perceived as meaningful and impactful to expectant mothers. The virtual and flexible nature of HEARTPrep was also perceived as convenient and no recommendations were given to improve the convenience or accessibility of HEARTPrep. Many participants engaged in telehealth sessions through the Nemours app while caring for other children, engaging in family routines (e.g., cooking or eating dinner), or during a break at work. No difficulties delivering HEARTPrep to expectant mothers receiving care in Florida by interventionists located in Delaware were noted. Recent legislation (i.e., Psychology Interjurisdictional Compact29) has reduced regulatory barriers to psychologists practicing across state lines via telehealth and could facilitate psychosocial intervention for this population of expectant mothers, even within the context of limited psychology resources at many children’s hospitals. It should also be noted that perceived acceptability of HEARTPrep did not differ between mothers who completed 3 telehealth sessions versus 6 or more sessions, which could have important implications for delivering prenatal psychosocial intervention at hospitals with limited resources.
While partners were not the primary focus of this study, they participated with mothers in about half of cases. Some mothers noted that it was helpful to participate in HEARTPrep with their partner as it facilitated communication and helped them learn together. The extent to which HEARTPrep is helpful for the partner and how it helps was not evaluated in this pilot study. Prior research indicates that fathers of children with CHD experience unique stressors that may require targeted supports (e.g., societal expectations for fatherhood, feeling overlooked as a partner in care).30,31 Future research is needed to determine if and how prenatal psychosocial intervention is helpful for partners and what may need to be added to address their unique needs.
Of note, a HEARTPrep custom dashboard within the Nemours app was in the process of being developed and refined at the same time as this study. This dashboard is organized into 3 modules (Adjusting, Connecting, and Preparing), each of which consists of a) patient education aimed at normalizing emotional reactions and providing tips for coping, b) recorded videos of other parents sharing their experiences with CHD and offering words of hope to expectant parents, and c) information about and links to relevant resources. Because current participants did not have access to this dashboard, its development and testing is outside of the scope of this study. Future research will evaluate the use and impact of the HEARTPrep dashboard in addition to scheduled telehealth sessions. In the current study, otherwise eligible mothers who received a prenatal CHD diagnosis after 30 weeks gestation were excluded due to the concern that they would not receive the full intervention prior to the birth. However, the ability for mothers to access intervention components through a mobile dashboard on their own time may facilitate intervention for a broader group of mothers.
Study Limitations
Non-English speaking families were not included in this initial pilot study. Research is underway to evaluate the feasibility and acceptability of HEARTPrep when delivered by a bilingual interventionist to Spanish-speaking mothers, who may experience more barriers to a virtually-delivered psychosocial intervention.32 A sample size of 35 is typically considered sufficient for pilot studies evaluating feasibility and acceptability prior to a larger efficacy trial.33 However, this sample size, in conjunction with a high completion rate, limits power to identify factors associated with intervention engagement and completion. The extent to which socioeconomic status and digital literacy affect engagement in HEARTPrep should be explored in future studies. Additionally, future research should examine how preexisting maternal mental health conditions affect HEARTPrep engagement and how HEARTPrep can augment other mental health therapies that mothers may be receiving. Lastly, this pilot study was conducted within one health system with a longstanding history of psychosocial research and it is not known whether results would differ across health systems.
HEARTPrep is feasible and acceptable for diverse mothers expecting a baby with CHD. These promising pilot results support the need for future multi-site research examining the impact of HEARTPrep on prenatal and postnatal outcomes, including long-term maternal mental health, maternal-child bonding, family functioning, and child neurodevelopment. This model of intervention could ultimately be applied across health systems and also adapted for other birth defects, given commonalities in maternal stress reactions after a prenatal diagnosis34,35 and a lack of formal interventions addressing family psychosocial needs.
Supplementary Material
Acknowledgements:
We thank Samantha Butler, PhD, Jo Ann Davis, CPNP-AC, Allison Divanovic, MD, Lindsay Edwards, MD, Colette Gramszlo, PhD, Nadine Kasparian, PhD, Sarah Kelly, PsyD, Trent Neely, MEd, Cynthia Ortinau, MD, Alejandra Perez Ramirez, Latoya Romeus, Salvadore Ruiz-Esparza, and Amanda Shillingford, MD for their contributions to the design of HEARTPrep.
This study was funded by the Research Expanding Access to Child Health (REACH) Center of Biomedical Research Excellence supported by National Institute of General Medical Sciences of the National Institutes of Health [1P20GM144270-01] and institutional funds from Nemours Children’s Health, Delaware through the PEDSnet Scholars Program.
Footnotes
Statements and Declarations:
Competing Interests: The authors do not have any financial or non-financial conflicts of interest.
Protection of Human Subjects: This study was reviewed and approved by the Nemours Children’s Health Institutional Review Board and all participants provided informed consent prior to study procedures.
References
- 1.van der Linde D, Konings EE, Slager MA, et al. (2011) Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol 58:2241–2247. [DOI] [PubMed] [Google Scholar]
- 2.Oster ME, Lee KA, Honein MA, Riehle-Colarusso T, Shin M, Correa A (2013) Temporal trends in survival among infants with critical congenital heart defects. Pediatrics 131:e1502–e1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quartermain MD, Pasquali SK, Hill KD, et al. (2015) Variation in Prenatal Diagnosis of Congenital Heart Disease in Infants. Pediatrics 136:e378–e385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Donofrio MT, Moon-Grady AJ, Hornberger LK, et al. (2014) Diagnosis and treatment of fetal cardiac disease: a scientific statement from the American Heart Association. Circulation 129:2183–2242. [DOI] [PubMed] [Google Scholar]
- 5.Weber RW, Stiasny B, Ruecker B, et al. (2019) Prenatal Diagnosis of Single Ventricle Physiology Impacts on Cardiac Morbidity and Mortality. Pediatr Cardiol 40:61–70. [DOI] [PubMed] [Google Scholar]
- 6.Bonnet D (2021) Impacts of prenatal diagnosis of congenital heart diseases on outcomes. Transl Pediatr 10:2241–2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kasparian NA (2019) Heart care before birth: A psychobiological perspective on fetal cardiac diagnosis. Prog Pediatr Cardiol 54:101142. [Google Scholar]
- 8.Espinosa KM, Julian M, Wu Y, et al. (2022) “The Mental Health Piece is Huge”: perspectives on developing a prenatal maternal psychological intervention for congenital heart disease. Cardiol Young 32:1268–1275. [DOI] [PubMed] [Google Scholar]
- 9.Dennis CL, Falah-Hassani K, Shiri R (2017) Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry 210:315–323. [DOI] [PubMed] [Google Scholar]
- 10.Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG (2017) A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord 219:86–92. [DOI] [PubMed] [Google Scholar]
- 11.Wu Y, Kapse K, Jacobs M, et al. (2020) Association of Maternal Psychological Distress With In Utero Brain Development in Fetuses With Congenital Heart Disease. JAMA Pediatr 174:e195316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rychik J, Donaghue DD, Levy S, et al. (2013) Maternal psychological stress after prenatal diagnosis of congenital heart disease. J Pediatr 162:302–307.e1. [DOI] [PubMed] [Google Scholar]
- 13.Sood E, Gramszlo C, Perez Ramirez A, et al. (2022) Partnering With Stakeholders to Inform the Co-Design of a Psychosocial Intervention for Prenatally Diagnosed Congenital Heart Disease. J Patient Exp 9:23743735221092488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howard LM, Khalifeh H (2020) Perinatal mental health: a review of progress and challenges. World Psychiatry 19:313–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Madigan S, Oatley H, Racine N, et al. (2018) A Meta-Analysis of Maternal Prenatal Depression and Anxiety on Child Socioemotional Development. J Am Acad Child Adolesc Psychiatry 57:645–657.e8. [DOI] [PubMed] [Google Scholar]
- 16.Roberts SD, Kazazian V, Ford MK, et al. (2021) The association between parent stress, coping and mental health, and neurodevelopmental outcomes of infants with congenital heart disease. Clin Neuropsychol 35:948–972. [DOI] [PubMed] [Google Scholar]
- 17.Ernst MM, Marino BS, Cassedy A, et al. (2018) Biopsychosocial Predictors of Quality of Life Outcomes in Pediatric Congenital Heart Disease. Pediatr Cardiol 39:79–88. [DOI] [PubMed] [Google Scholar]
- 18.DeMaso DR, Labella M, Taylor GA, et al. (2014) Psychiatric disorders and function in adolescents with d-transposition of the great arteries. J Pediatr 165:760–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gramszlo C, Karpyn A, Christofferson J, et al. Meeting Parents’ Needs for Education and Preparation following Congenital Heart Disease Diagnosis: Recommendations from a Crowdsourced Study. Am J Perinatol. Published online Sept 12, 2022. https://www.thieme-connect.com/products/ejournals/abstract/10.1055/a-1906-8786 [DOI] [PMC free article] [PubMed]
- 20.Gramszlo C, Karpyn A, Demianczyk AC, et al. (2020) Parent Perspectives on Family-Based Psychosocial Interventions for Congenital Heart Disease. J Pediatr 216:51–57.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Forrest CB, Margolis PA, Bailey LC, et al. (2014) PEDSnet: a National Pediatric Learning Health System. J Am Med Inform Assoc 21:602–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kind AJH, Buckingham W (2018) Making Neighborhood Disadvantage Metrics Accessible: The Neighborhood Atlas. N Engl J Med 378:2456–2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harris PA, Taylor R, Minor BL, et al. (2019) The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Canter KS, Deatrick JA, Hilgart MM, et al. (2019) eSCCIP: A psychosocial ehealth intervention for parents of children with cancer. Clin Pract Pediatr Psychol 7:44–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kasparian NA, Kan JM, Sood E, Wray J, Pincus HA, Newburger JW (2019) Mental health care for parents of babies with congenital heart disease during intensive care unit admission: Systematic review and statement of best practice. Early Hum Dev 139:104837. [DOI] [PubMed] [Google Scholar]
- 26.Song L, Qan’ir Y, Guan T, et al. (2021) The Challenges of Enrollment and Retention: A Systematic Review of Psychosocial Behavioral Interventions for Patients With Cancer and Their Family Caregivers. J Pain Symptom Manage 62:e279–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hocking MC, Kazak AE, Schneider S, Barkman D, Barakat LP, Deatrick JA (2014) Parent perspectives on family-based psychosocial interventions in pediatric cancer: a mixed-methods approach. Support Care Cancer 22:1287–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Drotar D (2012) Introduction to the Special Section: Pediatric Psychologists’ Experiences in Obtaining Reimbursement for the Use of Health and Behavior Codes. J Pediatr Psychol 37:479–485. [DOI] [PubMed] [Google Scholar]
- 29.Psychology Interjurisdictional Compact. http://www.psypact.org. Accessed 18 February 18 2023.
- 30.Sood E, Karpyn A, Demianczyk AC, et al. (2018) Mothers and Fathers Experience Stress of Congenital Heart Disease Differently: Recommendations for Pediatric Critical Care. Pediatr Crit Care Med 19:626–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoffman MF, Karpyn A, Christofferson J, et al. (2020) Fathers of Children With Congenital Heart Disease: Sources of Stress and Opportunities for Intervention. Pediatr Crit Care Med 21:e1002–e1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nouri S, Khoong EC, Lyles CR, Karliner L (2020) Addressing Equity in Telemedicine for Chronic Disease Management During the Covid-19 Pandemic. NEJM Catal Innov Care Deliv. https://catalyst.nejm.org/doi/pdf/10.1056/CAT.20.0123
- 33.Teresi JA, Yu X, Stewart AL, Hays RD (2022) Guidelines for Designing and Evaluating Feasibility Pilot Studies. Med Care 60:95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sreejith VP, Arun V, Devarajan AP, Gopinath A, Sunil M (2018) Psychological effect of prenatal diagnosis of cleft lip and palate: a systematic review. Contemp Clin Dent 9:304–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rofail D, Maguire L, Kissner M, Colligs A, Abetz-Webb L (2013) A review of the social, psychological, and economic burdens experienced by people with spina bifida and their caregivers. Neurol Ther 2:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


