Abstract
Background
Individuals with type 2 diabetes mellitus (T2DM) are more vulnerable to social disconnection compared with the general population; however, there are few relevant studies investigating this issue.
Aims
To investigate whether social isolation or loneliness may be associated with subsequent risk of developing major adverse cardiovascular events, whether these associations vary according to fatal and non-fatal outcomes and how behavioural, psychological and physiological factors mediate these associations.
Methods
This longitudinal analysis included data from 19 360 individuals with T2DM at baseline (2006–2010) from the UK Biobank. Social isolation and loneliness were measured using self-report questionnaires. The study outcomes included the first events of myocardial infarction (MI) or stroke (n=2273) and all-cause (n=2820) or cardiovascular disease-related mortality through linked hospital data or death registries.
Results
Over a median follow-up of 12.4 years (interquartile range (IQR): 11.6–13.3 years), participants who were more socially isolated (most social isolation vs least social isolation) experienced increased risks for all-cause (hazard ratio (HR) : 1.33, 95% confidence interval (CI): 1.19 to 1.47) and cardiovascular disease (HR: 1.36, 95% CI: 1.17 to 1.59) mortality but not first MI or stroke. Loneliness (yes vs no) was associated with a greater risk for a composite of incident MI or stroke (HR: 1.37, 95% CI: 1.19 to 1.57) but not mortality. Social isolation was associated with fatal MI and stroke, whereas loneliness was associated with non-fatal MI and stroke. The significant associations of social isolation and loneliness with outcomes were mainly mediated by behavioural factors (mediating proportion: 17.8%–28.2% and 17.6%–17.8%, respectively).
Conclusions
Among individuals with T2DM, social isolation and loneliness are associated with a greater risk of developing major adverse cardiovascular events, with differences in both risks stratified according to fatal and non-fatal events and underlying mediating factors.
Keywords: Social Isolation, Epidemiologic Studies, Mortality, Mental Health, Risk Factors
WHAT IS ALREADY KNOWN ON THIS TOPIC
Social isolation and loneliness are two important social determinants that affect cardiometabolic health. However, it remains unknown whether social isolation and loneliness are associated with cardiovascular diseases among individuals with type 2 diabetes mellitus, who are vulnerable to social disconnection.
WHAT THIS STUDY ADDS
Social isolation was associated with a higher risk for fatal cardiovascular outcomes and mortality, whereas loneliness was associated with non-fatal cardiovascular outcomes. These associations were mainly mediated by behavioural factors.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Our findings underscore the potential of enhancing social networks to prevent diabetes-related cardiovascular disease and mortality risks. This is particularly relevant considering the increasing social isolation and loneliness rates following the coronavirus disease 2019 (COVID-19) pandemic.
Introduction
Social determinants have been increasingly recognised as risk factors for multiple diseases and related mortality and have great potential for preventing these events.1 2 Social disconnection is a promising social determinant affecting cardiometabolic health3 4 and mental health5 that was highlighted during the coronavirus disease 2019 (COVID-19) pandemic.6 Social disconnection can be classified into two weakly correlated but distinct components: objective (social isolation) and subjective (loneliness) social disconnections.4 Social isolation refers to a lack of objective contacts or relationships with family, friends, or others, or simply living alone. Loneliness occurs when individuals perceive themselves as socially isolated, even when there is sufficient contact with others. Social isolation appears to be more consistently associated with fatal cardiovascular outcomes,7 8 while loneliness is associated with the risk of developing cardiovascular disease (CVD) in the general population.9 10 A recent scientific statement from the American Heart Association further urges the field to understand the independent effects of social isolation and loneliness on cardiometabolic health in vulnerable populations (eg, individuals with diabetes or CVD).4
Less attention has been devoted to individuals with type 2 diabetes mellitus (T2DM), who are more vulnerable to social disconnection compared with the general population.11 First, social disconnection is notably more common among individuals with T2DM (22%–38%)11 than in the general population (7%–10%).12 Second, recent research has suggested that a lack of social networks or loneliness is associated with an increased risk for T2DM.13 Third, social disconnection often occurs concomitantly with other traditional risk factors for T2DM or CVD, for example, unhealthy lifestyles, depression or anxiety, and inflammation.4 14 More importantly, in individuals with diabetes, social disconnection decreases their ability to control the disease, possibly due to increasing psychological stress, restricted access to healthcare services and poor medication adherence.3 As a result, previous studies have found that social isolation or loneliness was associated with worse glycaemic control15 and a higher risk of developing macrovascular (ie, coronary heart disease9 16 17) or microvascular (ie, chronic kidney disease18) complications and mortality19 among individuals with diabetes. Interventions, such as socialisation, have potential benefits in reducing glycated haemoglobin levels.20 These previous studies have implied that social disconnection may play a critical role in the poor prognosis among individuals with T2DM. However, it remains largely unknown whether social isolation and loneliness are associated with major adverse cardiovascular events (MACE) and mortality in this vulnerable population. Furthermore, if such associations exist, identifying potential mediating factors may help develop novel management strategies to reduce these risks.
Therefore, in this large cohort of individuals with T2DM, using individual-level data from the UK Biobank, the present study aimed to investigate the following: whether social isolation or loneliness was associated with subsequent risk for developing MACE, including myocardial infarction (MI), stroke and all-cause and CVD-related mortality; whether these associations varied according to fatal and non-fatal outcomes; and how behavioural, psychological and physiological factors mediated these associations.
Methods
Study population
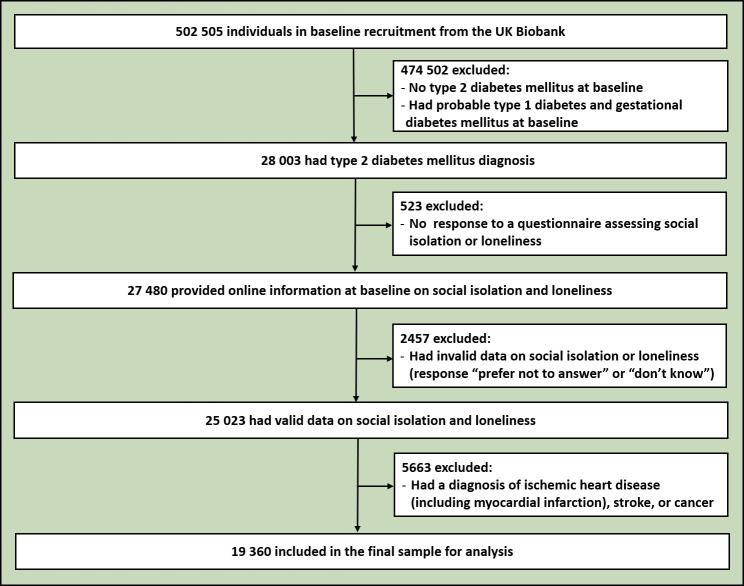
The UK Biobank is a large population-based longitudinal study that includes over 500 000 adults aged 40–69 years recruited from one of 22 assessment centres across the UK between 2006 and 2010. Each participant completed verbal interviews and touchscreen questionnaires, underwent multiple physical measurements and provided biological samples. A flowchart and a detailed description of the current study’s inclusion and exclusion are presented in figure 1 and online supplemental eText 1.
Figure 1.
Flowchart of participant selection.
gpsych-2023-101153supp001.pdf (563KB, pdf)
Exposures and outcomes
Social isolation was assessed using a validated questionnaire. The social isolation index score was derived from three questions: (1) ‘How often do you visit friends or family or have them visit you?’ (1 point was given for answering about once a month, once every few months, never or almost never, or no friends or family outside the household); (2) ‘Which of the following (sports club or gym, pub or social club, religious group, adult education class, other group activity) do you engage in once a week or more often?’ (1 point was given for answering none of the above); and (3) ‘Including yourself, how many people are living together in your household?’ (1 point was given for living alone). Using the scoring method implemented in previous studies,7 8 we constructed a social isolation index score (range: 0–3), with a higher score indicating a higher level of social isolation. We then divided social isolation into three levels: least social isolation (score=0), moderate social isolation (score=1) and most social isolation (score=2 or 3). The two items of social isolation were ‘contact with family/friends/groups’ (questions 1 and 2) and ‘living alone’ (question 3).
Loneliness was measured by the short-term University of California Los Angeles (UCLA) Loneliness Scale.21 The two questions used were: (1) ‘Do you often feel lonely?’ (1 point was given for answering yes) and (2) ‘How often are you able to confide in someone close to you?’ (1 point was given for answering never or almost never). The loneliness index score (range: 0–2) was calculated using the previously described scoring method.8 We defined the presence of loneliness as an index score of 2.8 The item ‘lonely’ was assessed by the first question, while the item ‘able to confide’ was assessed by the second question.8 More details about the assessment of social isolation and loneliness are shown in online supplemental eText 2.
The study outcomes were MACE, including all-cause mortality, CVD mortality and first MI or stroke (a composite endpoint) with a censor date of November 12, 2021. Data on the date and cause of death were collected from death certificates from the National Health Service Information Centre (England and Wales) and the National Health Service Central Register Scotland (Scotland). We ascertained CVD mortality based on the International Classification of Diseases 10th Revision (ICD-10) code (I00–I99). We determined the occurrence of the composite of the first MI or stroke using death registry records or hospital admission data. The diagnosis of the first cardiovascular event was determined by having a primary or secondary diagnosis (hospital admission records) or underlying/contributory cause of death (death register) with the following ICD-10 codes: MI (I21–I23, I24.1 or I25.2) and stroke (I60–I64, I69). We then subdivided first MI and stroke into fatal and non-fatal subtypes. Notably, fatal MI or stroke refers to death due to MI or stroke without hospital admission or occurring on the first day of hospital admission.7 The person-years were calculated from the date of entry to the UK Biobank to the date of death, first event or cessation, whichever occurred first.
Covariates
Information on covariates was collected at baseline (see online supplemental eText 3 and eTable 1): (1) demographic factors, including age, gender, ethnicity and assessment centres; (2) socioeconomic factors, including current employment status, education and Townsend Deprivation Index; (3) behavioural factors, including smoking, alcohol consumption, physical activity, TV watching time, healthy diet score and sleep duration; (4) psychological factors, including seeking help from physicians due to anxiety or depressive symptoms; (5) physiological factors, including obesity, grip strength, systolic blood pressure, diastolic blood pressure, hyperlipidaemia and estimated glomerular filtration rate; (6) diabetes-related factors, including family history of diabetes, haemoglobin A1c (HbA1c) level, diabetes duration and diabetes medication use; and (7) comorbidities, including chronic kidney disease, diabetes-related microvascular disease, neurodegenerative disease, respiratory disease, digestive disease, rheumatic arthritis and osteoarthritis.
Statistical analysis
The baseline characteristics are displayed as n (%) if categorical or mean (standard deviation (SD)) or median (interquartile range (IQR)) if continuous. To maximise the statistical power, multiple imputations were performed to impute missing data using the ‘mice’ R package (see online supplemental eText 4). Detailed information is provided in online supplemental eTable 2. Cox proportional hazards models were constructed to calculate hazard ratios (HRs) and 95% confidence intervals (CIs) for the associations between social isolation, loneliness and their subitems with the risk of each study outcome. Three levels of adjustment were performed within the multivariate Cox models: model 1 (age and gender), model 2 (model 1 additionally adjusted for ethnicity, assessment centres, socioeconomic factors, behavioural and psychological factors and most of the physiological factors, such as obesity status, grip strength, systolic blood pressure, diastolic blood pressure and hyperlipidaemia) and model 3 (model 2 additionally adjusted for estimated glomerular filtration rate, diabetes-related factors and comorbidities). Mutual adjustment for social isolation or loneliness was applied to models 2 and 3. Joint analyses were conducted to estimate the combined effects of social isolation and loneliness on the risk of developing vascular events or death among the T2DM population. Causal mediation analyses were conducted to examine whether the associations between exposure and outcome were mediated by the potential mediators.
Several sensitivity and subgroup analyses were performed to demonstrate the robustness of our findings: (1) using the dataset where invalid data of exposures were imputed (see online supplemental eText 4); (2) excluding participants with missing covariate data; (3) excluding death or first events occurring within 2 years after baseline and after December 31, 2019 (this date was considered the start of the COVID-19 pandemic in the UK); (4) separating study events within the first and last six years to explore whether social isolation and loneliness exerted longer term impacts on outcomes; (5) using Fine-Grey subdistribution hazards for the composites of the first MI or stroke to account for possible bias arising from competing risks across groups; (6) subgroup analyses; and (7) including the cross-product terms of social isolation and loneliness in the models to rule out the impacts of their interaction on independent associations.
All statistical analyses were performed using the R software V.4.2.2 (R Development Core Team, Vienna, Austria). A two-sided p value <0.05 was considered statistically significant.
Results
The characteristics of the study sample were comparable to those of the overall sample in the UK Biobank (see online supplemental eTable 3). The study sample comprised 19 360 individuals with T2DM (mean age (SD): 59.4 (7.0) years; 61.1% were male). During an average follow-up of 12.4 years (IQR: 11.6–13.3 years) representing 234 002 person-years, 2820 (14.6%) all-cause deaths occurred; 1377 (7.1%) were CVD-cause. A total of 2273 (11.7%) patients had first events of MI or stroke (MI=1503; stroke=922), with 152 patients experiencing both MI and stroke. Among them, 170 (0.9%) patients with T2DM experienced fatal MI or stroke (MI=134; stroke=37), while 2108 (10.9%) experienced non-fatal MI or stroke (MI=1369; stroke=885). As displayed in table 1, compared with the participants with least social isolation, those who experienced moderate or most social isolation or loneliness were more likely to be younger and have unhealthy lifestyles and comorbid conditions.
Table 1.
Baseline characteristics of patients with type 2 diabetes mellitus in the UK Biobank
| Characteristics | Total (n=19 360) |
Social isolation | Loneliness | |||
| Least social isolation (n=7409) |
Moderate social isolation (n=8147) |
Most social isolation (n=3804) |
No loneliness (n=17 873) |
Loneliness (n=1487) |
||
| Age, mean (SD), years | 59.4 (7.0) | 60.0 (6.9) | 59.3 (7.1) | 58.6 (7.1) | 59.6 (7.0) | 58.0 (7.2) |
| Gender, male, n (%) | 11 820 (61.1) | 4594 (62.0) | 4811 (59.1) | 2415 (63.5) | 10 884 (60.9) | 936 (62.9) |
| Ethnicity, white, n (%) | 17 057 (88.1) | 6587 (88.9) | 7162 (87.9) | 3308 (87.0) | 15 746 (88.1) | 1311 (88.2) |
| Assessment centre, n (%) | ||||||
| England | 17 237 (89.0) | 6549 (88.4) | 7295 (89.5) | 3393 (89.2) | 15 925 (89.1) | 1312 (88.2) |
| Scotland | 1233 (6.4) | 481 (6.5) | 495 (6.1) | 257 (6.8) | 1124 (6.3) | 109 (7.3) |
| Wales | 890 (4.6) | 379 (5.1) | 357 (4.4) | 154 (4.0) | 824 (4.6) | 66 (4.4) |
| Currently employed, n (%) | 8545 (44.1) | 3135 (42.3) | 3680 (45.2) | 1730 (45.5) | 7937 (44.4) | 608 (40.9) |
| College or university degree, n (%) | 4776 (24.7) | 1888 (25.5) | 1945 (23.9) | 943 (24.8) | 4485 (25.1) | 291 (19.6) |
| Townsend Deprivation Index* | −0.5 (3.4) | −1.2 (3.1) | −0.4 (3.4) | 0.5 (3.6) | −0.6 (3.3) | 0.4 (3.6) |
| Current smokers, n (%) | 2228 (11.5) | 638 (8.6) | 946 (11.6) | 644 (16.9) | 1974 (11.0) | 254 (17.1) |
| Alcohol consumption status, n (%) | ||||||
| Not current | 2867 (14.8) | 935 (12.6) | 1222 (15.0) | 710 (18.7) | 2572 (14.4) | 295 (19.8) |
| Less than three times a week | 10 545 (54.5) | 3770 (50.9) | 4552 (55.9) | 2223 (58.4) | 9713 (54.3) | 832 (56.0) |
| Three or more times a week | 5948 (30.7) | 2704 (36.5) | 2373 (29.1) | 871 (22.9) | 5588 (31.3) | 360 (24.2) |
| Physical activity (MET score), mean (SD) | 9.6 (5.1) | 10.3 (4.9) | 9.5 (5.1) | 8.8 (5.2) | 9.7 (5.0) | 8.7 (5.3) |
| TV watching time (hours/day), mean (SD) | 3.4 (2.0) | 3.3 (1.7) | 3.5 (1.9) | 3.8 (2.4) | 3.4 (1.9) | 4.0 (2.5) |
| Healthy diet score, median (IQR) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 3 (2–3) | 3 (2–4) | 2 (2–3) |
| Sleep duration, n (%) | ||||||
| Short (<7 hours/day) | 5382 (27.8) | 1754 (23.7) | 2326 (28.6) | 1302 (34.2) | 4771 (26.7) | 611 (41.1) |
| Normal (7–8 hours/day) | 11 719 (60.5) | 4746 (64.1) | 4893 (60.1) | 2080 (54.7) | 11 043 (61.8) | 676 (45.5) |
| Long (>8 hours/day) | 2259 (11.7) | 909 (12.3) | 928 (11.4) | 422 (11.1) | 2059 (11.5) | 200 (13.4) |
| Anxiety, n (%) | 89 (0.5) | 24 (0.3) | 43 (0.5) | 22 (0.6) | 78 (0.4) | 11 (0.7) |
| Depression, n (%) | 296 (1.5) | 66 (0.9) | 135 (1.7) | 95 (2.5) | 240 (1.3) | 56 (3.8) |
| Ever seeking help from physicians due to anxiety or depressive symptoms, n (%) | 6797 (35.1) | 2298 (31.0) | 2954 (36.3) | 1545 (40.6) | 5982 (33.5) | 815 (54.8) |
| Obesity status (kg/m2) | ||||||
| Underweight or normal weight, n (%) | 1893 (9.8) | 713 (9.6) | 812 (10.0) | 368 (9.7) | 1776 (9.9) | 117 (7.9) |
| Overweight, n (%) | 6548 (33.8) | 2697 (36.4) | 2702 (33.2) | 1149 (30.2) | 6141 (34.4) | 407 (27.4) |
| Obese, n (%) | 10 919 (56.4) | 3999 (54.0) | 4633 (56.9) | 2287 (60.1) | 9956 (55.7) | 963 (64.8) |
| Grip strength (kg), mean (SD) | 30.6 (11.1) | 31.1 (11.1) | 30.4 (11.0) | 30.1 (11.0) | 30.7 (11.0) | 29.6 (11.2) |
| Systolic blood pressure (mm Hg), mean (SD) | 145 (18) | 145 (18) | 145 (18) | 144 (19) | 145 (19) | 142 (18) |
| Diastolic blood pressure (mm Hg), mean (SD) | 83 (10) | 83 (10) | 83 (10) | 83 (11) | 83 (10) | 83 (10) |
| Hyperlipidaemia, n (%) | 13 265 (68.5) | 5129 (69.2) | 5558 (68.2) | 2578 (67.8) | 12 217 (68.4) | 1048 (70.5) |
| Estimated glomerular filtration rate, mean (SD), mL/min/1.73 m2 | 89.8 (15.6) | 89.5 (15.1) | 90.0 (15.7) | 90.3 (16.2) | 89.7 (15.5) | 91.2 (16.3) |
| Family history of diabetes, n (%) | 7061 (36.5) | 2690 (36.3) | 3034 (37.2) | 1337 (35.1) | 6484 (36.3) | 577 (38.8) |
| HbA1c, median (IQR), % | 6.8 (6.2–7.5) | 6.7 (6.1–7.4) | 6.8 (6.2–7.5) | 6.8 (6.2–7.7) | 6.7 (6.2–7.5) | 6.9 (6.2–7.7) |
| Diabetes duration, median (IQR), years | 4.0 (1.0–8.0) | 4.0 (1.0–8.0) | 4.0 (1.0–8.0) | 4.0 (1.0–8.0) | 4.0 (1.0–8.0) | 4.1 (1.0–9.0) |
| Diabetes medication use, n (%) | ||||||
| Neither | 7227 (37.3) | 2877 (38.8) | 3007 (36.9) | 1343 (35.3) | 6752 (37.8) | 475 (31.9) |
| Oral antidiabetic drug only | 9584 (49.5) | 3628 (49.0) | 4036 (49.5) | 1920 (50.5) | 8822 (49.4) | 762 (51.2) |
| Insulin | 2549 (13.2) | 904 (12.2) | 1104 (13.6) | 541 (14.2) | 2299 (12.9) | 250 (16.8) |
| Chronic kidney disease, n (%) | 328 (1.7) | 107 (1.4) | 141 (1.7) | 80 (2.1) | 298 (1.7) | 30 (2.0) |
| Diabetes-related microvascular disease, n (%) | 321 (1.7) | 102 (1.4) | 145 (1.8) | 74 (1.9) | 290 (1.6) | 31 (2.1) |
| Neurodegenerative disease, n (%) | 52 (0.3) | 15 (0.2) | 19 (0.2) | 18 (0.5) | 43 (0.2) | 9 (0.6) |
| Respiratory disease, n (%) | 717 (3.7) | 227 (3.1) | 301 (3.7) | 189 (5.0) | 627 (3.5) | 90 (6.1) |
| Digestive disease, n (%) | 269 (1.4) | 78 (1.1) | 118 (1.4) | 73 (1.9) | 243 (1.4) | 26 (1.7) |
| Rheumatoid arthritis, n (%) | 318 (1.6) | 124 (1.7) | 135 (1.7) | 59 (1.6) | 289 (1.6) | 29 (2.0) |
| Osteoarthritis, n (%) | 2130 (11.0) | 774 (10.4) | 882 (10.8) | 474 (12.5) | 1927 (10.8) | 203 (13.7) |
*Positive values of the index indicate areas with high material deprivation, whereas those with negative values indicate relative affluence.
HbA1c, haemoglobin A1c; IQR, interquartile range; MET, metabolic equivalent of task; SD, standard deviation.
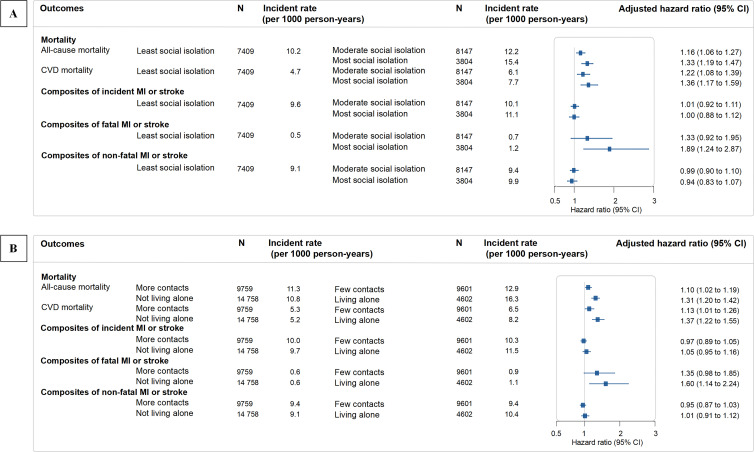
As shown in figure 2 and online supplemental eTable 4, social isolation was substantially associated with a greater risk for fatal but not non-fatal MACE. After full adjustment for demographic and socioeconomic factors, behavioural, psychological and physiological factors, diabetes-related factors and comorbidities, a higher level of social isolation (most social isolation vs least social isolation) was associated with an increased risk for both all-cause (HR: 1.33, 95% CI: 1.19 to 1.47) and CVD-cause mortality (HR: 1.36, 95% CI: 1.17 to 1.59) (figure 2A). However, a weak association was found between social isolation (most social isolation vs least social isolation) and incident MI or stroke (model 1: HR: 1.26 (95% CI: 1.13 to 1.41); model 3: HR: 1.00 (95% CI: 0.88 to 1.12)). When MI or stroke was subclassified into fatal and non-fatal subtypes, in the fully adjusted model, social isolation showed a substantial association with a greater risk of incident fatal MI or stroke (most social isolation vs least social isolation: HR: 1.89, 95% CI: 1.24 to 2.87) but had a weak association with the non-fatal subtype (HR: 0.94, 95% CI: 0.83 to 1.07) (figure 2A). The pattern was generally similar when MI and stroke outcomes were separated (see online supplemental eTable 4). Regarding the subitems, living alone was associated with a higher risk for all-cause mortality (HR: 1.31, 95% CI: 1.20 to 1.42), CVD mortality (HR: 1.37, 95% CI: 1.22 to 1.55) and fatal MI or stroke (HR: 1.60, 95% CI: 1.14 to 2.24) (figure 2B). A similar association was found between ‘contact with family/friends/groups’ and all-cause mortality (HR: 1.10, 95% CI: 1.02 to 1.19), CVD mortality (HR: 1.13, 95% CI: 1.01 to 1.26) and fatal MI or stroke (HR: 1.35, 95% CI: 0.98 to 1.85), but with lower HRs (figure 2B).
Figure 2.
Association of social isolation (A) and its items (B) with subsequent risk for major adverse cardiovascular events, including mortality, MI or stroke following type 2 diabetes mellitus. HRs were adjusted for demographic behavioural, psychological, physiological and diabetes-related factors, and comorbidities. CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; MI, myocardial infarction.
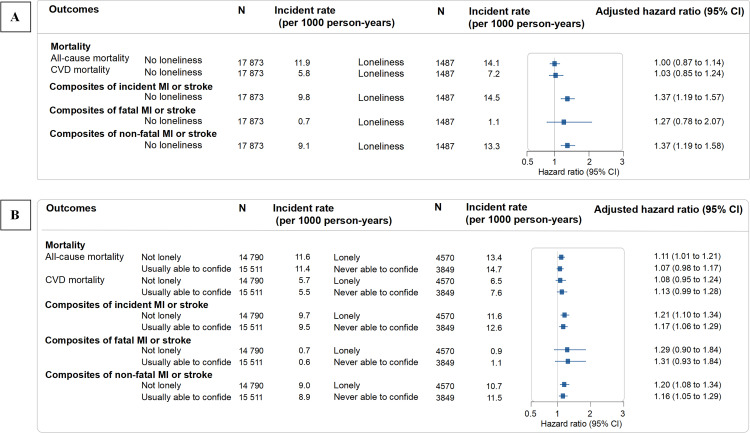
In contrast to social isolation, loneliness was mainly associated with an increased risk for non-fatal MACE (figure 3 and online supplemental eTable 5). Loneliness was not independently associated with an increased risk for all-cause (HR: 1.00, 95% CI: 0.87 to 1.14) and CVD (HR 1.03, 95% CI: 0.85 to 1.24) mortality (figure 3A). Participants with loneliness showed a substantially higher risk for incident MI or stroke (HR: 1.37, 95% CI: 1.19 to 1.57) in the fully adjusted model. Loneliness increased the risk for the first non-fatal MI or stroke (HR: 1.37, 95% CI: 1.19 to 1.58) by 37%; it was not significantly associated with fatal MI or stroke as the first event (HR: 1.27, 95% CI: 0.78 to 2.07), however, with a wider CI for the fatal outcome than the non-fatal outcome (figure 3A). A small number of events may account for the wide CI. Similar patterns were observed when separately considering MI and stroke as outcomes. ‘Lonely’ was associated with a greater risk for all-cause mortality (HR: 1.11, 95% CI: 1.01 to 1.21) and composites of incident MI or stroke (HR: 1.21, 95% CI: 1.10 to 1.34), which were mainly driven by their non-fatal subtypes (HR: 1.20, 95% CI: 1.08 to 1.34) (figure 3B). A similar pattern was found for ‘able to confide’ (figure 3B).
Figure 3.
Associations of loneliness (A) and its items (B) with subsequent risk for major adverse cardiovascular events, including mortality, MI or stroke following type 2 diabetes mellitus. HRs were adjusted for demographic behavioural, psychological, physiological and diabetes-related factors, and comorbidities. CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; MI, myocardial infarction.
Joint analyses showed that social isolation and loneliness might have additive effects. Individuals with a combination of social isolation and loneliness were generally at the highest risk for developing cardiovascular events or death compared with those with the other five combinations (combinations of no loneliness and least, moderate or most isolation, and combinations of loneliness and least or moderate social isolation) (see online supplemental eTable 6).
The major results remained robust when the complete dataset was used (see online supplemental eTables 7 and 8), when the invalid exposure data were imputed (see online supplemental eTables 9 and 10) and when study events occurring within the first 2 years (see online supplemental eTables 11 and 12) and after December 31, 2019 (see online supplemental eTables 13 and 14) were excluded. The results were largely consistent using the whole sample for the first 6 years (see online supplemental eTables 15–18).
For mediation analyses (see online supplemental eTable 19), the effects of social isolation on mortality and composites of fatal MI or stroke were mainly mediated by behavioural factors (range of mediating proportion: 17.8%–28.2%), followed by physiological factors (6.5%–7.6%), comorbidities (7.3%–8.4%) and diabetes-related factors (4.6%–5.6%), while the effects of loneliness on outcomes were mainly mediated by behavioural (range of mediating proportion: 17.6%–17.8%) and physiological factors (6.0%–6.7%), followed by diabetes-related factors (7.2%–7.7%) and comorbidities (4.1%–4.9%).
The Fine-Grey subdistribution hazards models showed a similar pattern (see online supplemental eTable 20). Most of the results of the subgroup analyses were consistent when stratified according to age, gender, socioeconomic deprivation, smoking, alcohol consumption, physical activity, obesity and HbA1c (all p>0.05) (see online supplemental eTables 21 and 22). Social isolation and loneliness were not statistically interacted regarding any outcome (all pinteraction>0.1) (see online supplemental eTable 23). These independent associations remained robust after adjusting for the interaction.
Discussion
Main findings
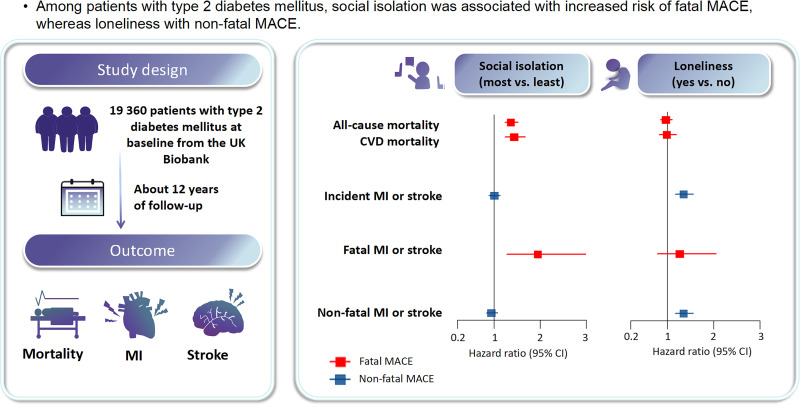
There were several noteworthy findings in this analysis of data from the UK Biobank, including 19 360 individuals with T2DM (234 002 person-years) (figure 4). First, social isolation and loneliness were distinctly associated with fatal and non-fatal outcomes among patients with T2DM. Social isolation was associated with an increased risk for all-cause and CVD-related mortality and the first fatal MI or stroke, which directly resulted in death without associated hospital admission. In contrast, loneliness was associated with an increased risk for non-fatal MI or stroke (hospital admission as the first event without death) but had little effect on fatal MACE. Second, the main findings were robust across various sensitivity and subgroup analyses. Finally, the association of social isolation on mortality and composites of fatal MI or stroke was mainly mediated by behavioural factors, whereas the effects of loneliness on the composites of incident MI or stroke and composites of non-fatal MI or stroke were mainly mediated by behavioural and physiological factors.
Figure 4.
Social isolation, loneliness and subsequent risk for major adverse cardiovascular events, including mortality, myocardial infarction or stroke following type 2 diabetes mellitus. Social isolation was associated with a higher risk of fatal events, including mortality and fatal MI or stroke. Conversely, the association of loneliness with the risk of first MI or stroke was mainly driven by non-fatal events. CI, confidence interval; CVD, cardiovascular disease; MACE, major adverse cardiovascular events; MI, myocardial infarction.
Although previous studies have revealed a link between social isolation, loneliness and vascular events in patients with diabetes, they have reported inconsistent findings. Several cohort studies have consistently reported that social isolation—rather than loneliness—was significantly associated with an increased risk for mortality among the general population8 or in patients with existing CVDs.22 Conversely, a recent study from the UK Biobank by Wang et al reported that loneliness—instead of social isolation—was associated with an increased risk of developing cardiovascular events among individuals with diabetes.9 Other studies have found that social isolation and loneliness were both potential risk factors for CVD or mortality.23 24 These inconsistencies are perhaps due to these studies which did not differentiate between fatal and non-fatal outcomes. Recently, a longitudinal study classified CVD outcomes into fatal or non-fatal events and demonstrated that social isolation had little impact on new-onset non-fatal CVD but was more related to fatal events directly leading to death before arriving at hospitals.7 However, a similar study by Wang et al 9 overlooked fatal outcomes. Instead, we alluded to these previous studies by showing that the associations of social isolation and loneliness with diabetic vascular events differed substantially between fatal and non-fatal subtypes among patients with T2DM. Our study is clinically important because it expands the literature by selecting a high-risk population (ie, patients with T2DM) who are vulnerable to both social disconnection and CVD. Collectively, these findings underscore the necessity of separately considering the effects of social isolation and loneliness on cardiometabolic health in future research.
Our findings corroborate the results of earlier studies in this field, reporting a modest association between unsatisfactory social relationships, for example, smaller network size,16–19 less social support,16 17 higher social strain17 or loneliness,9 and the risk of vascular complications in patients with diabetes. We also advanced the literature by reporting that social isolation was as important as loneliness in increasing the risk of a poor T2DM prognosis. Notably, several methodological concerns in previous studies may have limited their ability to measure causal inference and generalisability, including their cross-sectional design,16 small sample size,16 highly selected samples (eg, postmenopausal women with diabetes treated,17 patients from an ongoing trial18) or recall bias (eg, self-reported outcomes17). Moreover, we extend previous studies by revealing the potentially additive effect(s) of social isolation and loneliness on diabetes-related vascular risks and mortality. These findings suggest that patients with diabetes, who are subjected to both social isolation and loneliness, should devote particular attention to preventing future vascular events and death.
To the best of our knowledge, this is the first study to illustrate the mediating pathways linking social isolation or loneliness with vascular events or mortality among the diabetic population, in which social isolation leads to fatal outcomes largely via maladaptive behavioural factors, whereas loneliness leads to non-fatal outcomes mainly via maladaptive behavioural and physiological factors. These speculations are supported by previous studies demonstrating that associations of social isolation and loneliness with mortality or dementia were mediated by lifestyle, depressive symptoms or biological factors.8 25 Previous evidence has suggested that the risk of fatal events or mortality associated with social isolation is likely due to the lack of immediate help from another individual in seeking emergency care.7 Our finding that living alone was associated with a greater risk for fatal MI or stroke and mortality further supports this speculation. Meanwhile, feelings of loneliness do not necessarily mean that individuals do not live with other people; instead, they may be eager for contact or attention from others.26
Beyond these differential pathways, social isolation and loneliness may share common underlying pathways, including elevated activities of the hypothalamic–pituitary–adrenal axis and sympathetic nervous system,27 a higher degree of proinflammatory response and oxidative stress.28 These pathophysiological changes may lead to poor glycaemic control, accelerated atherosclerosis and increased peripheral pressure and promote the development of cardiovascular complications in patients with diabetes.
Given the rapidly increasing rates of social isolation and loneliness, particularly post COVID-19 pandemic, our findings may be important for policy and clinical application. First, early screening for both social isolation and loneliness should be encouraged to detect excess cardiovascular risk following diabetes. For patients with T2DM who are socially isolated or living alone, it is necessary to enhance emergency care by providing personal emergency alarms. Intervention frameworks across individuals, communities and other levels of society29 are needed to support socially isolated patients in improving their behaviours. Meanwhile, for those feeling lonely, mental health professionals are encouraged to aid in diabetes management by offering psychological therapies to lower the mental distress of loneliness.26 29 In addition, interventions targeting mediating factors, such as unhealthy behaviours, depressive symptoms or other physiological factors, could generate extra benefits for the prevention of vascular events or premature death in this vulnerable population.
The current study has several strengths, such as its longitudinal design, the large sample size enabling the classification of CVD events into fatal and non-fatal groups and the concurrent consideration of social isolation and loneliness in a vulnerable population. Additionally, the current study is one of the few studies to compare the potentially distinct associations of objective and subjective social disconnections on CVD outcomes. We found that social isolation and loneliness were associated with a greater risk of developing MACE, with differences in risk stratified according to fatal and non-fatal events and underlying mediating factors.
Limitations
Some limitations should be considered when interpreting these findings. First, the UK Biobank cohort mainly comprises participants of European descent, limiting our findings’ generalisability to other ethnic groups. Second, social isolation and loneliness were assessed using simple questionnaires, which may have induced recall bias. The social isolation questionnaire only considered in-person contact and did not include virtual connections or other aspects of social relationships. Loneliness was defined using only two items from the UCLA scale, which may have led to an underestimation of loneliness. However, the current definitions of social isolation and loneliness have been widely adopted by several previous studies involving different cohorts.7–9 24 27 Third, we were unable to delineate time-varying associations because we used a single time point measure of social isolation and loneliness in the UK Biobank. Nevertheless, a previous meta-analysis suggested that these traits were stable across patient lifespans.30 Fourth, participants who experienced social isolation were more likely to die alone, thereby not contributing to a known cause of death. This study may have underestimated the rate of fatal MI or stroke, which may have rendered the estimated association null. Finally, residual confounding was inevitable owing to the observational design of the study. The time lag analysis, which excluded events occurring in the first two years, yielded robust results, suggesting that the documented associations were less likely to be biased by reverse causality. Nevertheless, we could only infer an association, not causation.
Implications
In a large population-based sample of individuals with T2DM, social isolation and loneliness were associated with fatal and non-fatal MACE, respectively. The associations between social isolation on mortality and fatal MACE were mediated mainly by behavioural factors. In contrast, the effects of loneliness on overall and non-fatal MACE were primarily mediated by behavioural and physiological factors.
Acknowledgments
This research was conducted using the UK Biobank Resource (application number: 59117). We sincerely thank the participants and staff who contributed to the UK Biobank.
Biography
Yannis Yan Liang is currently an attending physician and assistant researcher at The Affiliated Brain Hospital of Guangzhou Medical University in China. She obtained her PhD in Medical Science from The Chinese University of Hong Kong in 2018. After graduation, she worked as an attending physician in the Department of Neurology of The First Affiliated Hospital of Jinan University in China. She was a postdoctoral fellow at Guangdong Cardiovascular Institute, Guangdong Provincial People's Hospital in China, from 2020 to 2023. She has published 16 science citation-indexed papers as first or corresponding author in journals including Nature Communications, Journals of the American College of Cardiology: Heart Failure, Journal of Sport and Health Science, European Journal of Preventive Cardiology, etc. Dr Liang has obtained several national grants from the National Natural Science Foundation of China and the China Postdoctoral Science Foundation. Her main research interests include psychosomatic medicine, mental stress-related cardiovascular or metabolic diseases, and neuroimaging.

Footnotes
Contributors: All authors reviewed and approved the final manuscript. YYL and SA were responsible for conceptualisation. YYL and HF helped with the data curation. YYL and YC contributed to the formal analysis. HF, QYHA, LY, HX, and YN helped with the software and methodology. YYL had the primary responsibility for writing—original draft with the help of HX, JM and JZ. All the authors helped with writing—review and editing. YYL had full access to all data in the study. SA was responsible for validation and supervision as the guarantor.
Funding: This study was funded by the National Natural Science Foundation of China (32100880), Guangzhou Municipal Key Discipline in Medicine (2021–2023), Guangzhou High-level Clinical Key Specialty and Guangzhou Research-oriented Hospital.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data may be obtained from a third party and are not publicly available. Individual-level data from the UK Biobank are not publicly available due to their policy, but the data will be made available after the application to the UK Biobank (https://www.ukbiobank.ac.uk/).
Ethics statements
Patient consent for publication
Obtained.
Ethics approval
This study involves human participants and the Northwest Multicenter Research Ethics Committee approved the UK Biobank Study (reference: 16/NW/0274). Participants gave informed consent to participate in the study before taking part.
References
- 1. Wang F, Gao Y, Han Z, et al. A systematic review and meta-analysis of 90 cohort studies of social isolation, loneliness and mortality. Nat Hum Behav 2023;7:1307–19. 10.1038/s41562-023-01617-6 [DOI] [PubMed] [Google Scholar]
- 2. Xu X, Mishra GD, Holt-Lunstad J, et al. Social relationship satisfaction and accumulation of chronic conditions and multimorbidity: a national cohort of Australian women. Gen Psychiatr 2023;36:e100925. 10.1136/gpsych-2022-100925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schram MT, Assendelft WJJ, van Tilburg TG, et al. Social networks and type 2 diabetes: a narrative review. Diabetologia 2021;64:1905–16. 10.1007/s00125-021-05496-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cené CW, Beckie TM, Sims M, et al. Effects of objective and perceived social isolation on cardiovascular and brain health: a scientific statement from the American heart Association. J Am Heart Assoc 2022;11:e026493. 10.1161/JAHA.122.026493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang X, Chen J. Isolation and mental health: challenges and experiences from China. Gen Psychiatr 2021;34:e100565. 10.1136/gpsych-2021-100565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Holt-Lunstad J, Perissinotto C. Social isolation and loneliness as medical issues. N Engl J Med 2023;388:193–5. 10.1056/NEJMp2208029 [DOI] [PubMed] [Google Scholar]
- 7. Smith RW, Barnes I, Green J, et al. Social isolation and risk of heart disease and stroke: analysis of two large UK prospective studies. Lancet Public Health 2021;6:e232–9. 10.1016/S2468-2667(20)30291-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Elovainio M, Hakulinen C, Pulkki-Råback L, et al. Contribution of risk factors to excess mortality in isolated and lonely individuals: an analysis of data from the UK Biobank cohort study. Lancet Public Health 2017;2:e260–6. 10.1016/S2468-2667(17)30075-0IF:50.0Q1B1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang X, Ma H, Li X, et al. Joint association of loneliness and traditional risk factor control and incident cardiovascular disease in diabetes patients. Eur Heart J 2023;44:2583–91. 10.1093/eurheartj/ehad306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Liang YY, Chen Y, Feng H, et al. Association of social isolation and loneliness with incident heart failure in a population-based cohort study. JACC Heart Fail 2023;11:334–44. 10.1016/j.jchf.2022.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chao AM, Wadden TA, Clark JM, et al. Changes in the prevalence of symptoms of depression, loneliness, and insomnia in U.S. older adults with type 2 diabetes during the COVID-19 pandemic: the look AHEAD study. Diabetes Care 2022;45:74–82. 10.2337/dc21-1179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Surkalim DL, Luo M, Eres R, et al. The prevalence of loneliness across 113 countries: systematic review and meta-analysis. BMJ 2022;376:e067068. 10.1136/bmj-2021-067068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Henriksen RE, Nilsen RM, Strandberg RB. Loneliness increases the risk of type 2 diabetes: a 20 year follow-up - results from the hunt study. Diabetologia 2023;66:82–92. 10.1007/s00125-022-05791-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Santini ZI, Jose PE, York Cornwell E, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health 2020;5:e62–70. 10.1016/S2468-2667(19)30230-0 [DOI] [PubMed] [Google Scholar]
- 15. Shin SM, Oh TJ, Choi SH, et al. Effects of social distancing on diabetes management in older adults during COVID-19 pandemic. Diabetes Metab J 2021;45:765–72. 10.4093/dmj.2021.0096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Brinkhues S, Dukers-Muijrers NHTM, Hoebe CJPA, et al. Social network characteristics are associated with type 2 diabetes complications: the Maastricht Study. Diabetes Care 2018;41:1654–62. 10.2337/dc17-2144 [DOI] [PubMed] [Google Scholar]
- 17. Miao Jonasson J, Hendryx M, Shadyab AH, et al. Social support, social network size, social strain, stressful life events, and coronary heart disease in women with type 2 diabetes: a cohort study based on the women's health initiative. Diabetes Care 2020;43:1759–66. 10.2337/dc19-2065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dunkler D, Kohl M, Heinze G, et al. Modifiable lifestyle and social factors affect chronic kidney disease in high-risk individuals with type 2 diabetes mellitus. Kidney Int 2015;87:784–91. 10.1038/ki.2014.370 [DOI] [PubMed] [Google Scholar]
- 19. Han H, Cao Y, Feng C, et al. Association of a healthy lifestyle with all-cause and cause-specific mortality among individuals with type 2 diabetes: a prospective study in UK Biobank. Diabetes Care 2022;45:319–29. 10.2337/dc21-1512 [DOI] [PubMed] [Google Scholar]
- 20. Spencer-Bonilla G, Ponce OJ, Rodriguez-Gutierrez R, et al. A systematic review and meta-analysis of trials of social network interventions in type 2 diabetes. BMJ Open 2017;7:e016506. 10.1136/bmjopen-2017-016506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hughes ME, Waite LJ, Hawkley LC, et al. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging 2004;26:655–72. 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yu B, Steptoe A, Chen L-J, et al. Social isolation, loneliness, and all-cause mortality in patients with cardiovascular disease: a 10-year follow-up study. Psychosom Med 2020;82:208–14. 10.1097/PSY.0000000000000777 [DOI] [PubMed] [Google Scholar]
- 23. Golaszewski NM, LaCroix AZ, Godino JG, et al. Evaluation of social isolation, loneliness, and cardiovascular disease among older women in the US. JAMA Netw Open 2022;5:e2146461. 10.1001/jamanetworkopen.2021.46461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hakulinen C, Pulkki-Råback L, Virtanen M, et al. Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK Biobank cohort study of 479 054 men and women. Heart 2018;104:1536–42. 10.1136/heartjnl-2017-312663 [DOI] [PubMed] [Google Scholar]
- 25. Shen C, Rolls ET, Cheng W, et al. Associations of social isolation and loneliness with later dementia. Neurology 2022;99:e164–75. 10.1212/WNL.0000000000200583 [DOI] [PubMed] [Google Scholar]
- 26. Brown V, Morgan T, Fralick A. Isolation and mental health: thinking outside the box. Gen Psychiatr 2021;34:e100461. 10.1136/gpsych-2020-100461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cacioppo JT, Cacioppo S, Capitanio JP, et al. The neuroendocrinology of social isolation. Annu Rev Psychol 2015;66:733–67. 10.1146/annurev-psych-010814-015240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Li H, Xia N. The role of oxidative stress in cardiovascular disease caused by social isolation and loneliness. Redox Biol 2020;37:101585. 10.1016/j.redox.2020.101585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Holt-Lunstad J. Why social relationships are important for physical health: a systems approach to understanding and modifying risk and protection. Annu Rev Psychol 2018;69:437–58. 10.1146/annurev-psych-122216-011902 [DOI] [PubMed] [Google Scholar]
- 30. Mund M, Freuding MM, Möbius K, et al. The stability and change of loneliness across the life span: a meta-analysis of longitudinal studies. Pers Soc Psychol Rev 2020;24:24–52. 10.1177/1088868319850738 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
gpsych-2023-101153supp001.pdf (563KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data may be obtained from a third party and are not publicly available. Individual-level data from the UK Biobank are not publicly available due to their policy, but the data will be made available after the application to the UK Biobank (https://www.ukbiobank.ac.uk/).