Abstract
Objectives
To describe the experiences of patients who have postacute sequelae SARS-CoV-2 infection with internal vibrations and tremors as a prominent component, we leveraged the efforts by Survivor Corps, a grassroots COVID-19 patient advocacy group, to gather information from individuals belonging to its Facebook group with a history of COVID-19 suffering from vibrations and tremors.
Setting and design
A narrative analysis was performed on 140 emails and 450 social media comments from 140 individuals collected as a response to a call to >180 000 individuals participating in Survivor Corps between 15 July and 27 July 2021. We used common coding techniques and the constant comparative method for qualitative data synthesis and categorising emails. Coded data were entered into NVivo V.12 to identify recurrent themes, theme connections and supporting quotations. Comments were analysed using Word Clouds, generated with R V.4.0.3 using quanteda, wordcloud and tm packages.
Main outcome measures
Patient-reported long COVID symptom themes and domains related to internal tremors and vibration.
Results
The respondents’ emails represented 22 themes and 7 domains pertaining to their experience with internal tremor and vibrations. These domains were as follows: (1) symptom experience, description and anatomic location; (2) initial symptom onset; (3) symptom timing; (4) symptom triggers or alleviators; (5) change from baseline health status; (6) experience with medical establishment and (7) impact on individuals’ lives and livelihood. There were 22 themes in total, each corresponding to one of the broader domains. Among the responses, many described symptoms that varied in location, timing and triggers, occurred soon after their COVID-19 infection, and were markedly debilitating. There were often frustrating experiences with the healthcare system.
Conclusions
This study describes key themes and experiences among a group of people reporting long COVID and having a prolonged and debilitating symptom complex that prominently features internal tremors and vibrations.
Keywords: COVID-19, NEUROLOGY, REGISTRIES
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study investigated self-reported symptom experiences from the patient perspective from a convenience sample of patients experiencing internal tremors and vibration symptoms as postacute sequelae of SARS-CoV-2.
We used common coding techniques for qualitative data and the constant comparative qualitative data analysis method to identify themes from patients’ experiences.
This study represents a convenience sample and therefore cannot provide information on the incidence and prevalence of these symptoms.
This study contributes to the literature an understanding of the patient perspective regarding internal tremor and vibrations, a potentially important cluster of similar symptoms reported by people with long COVID.
Introduction
Post-acute sequelae of SARS-CoV-2 infection, also known as long COVID, is a condition that is marked by protean manifestation that varies considerably among individuals.1–4 Common symptoms among long COVID patients encompass a range of respiratory, metabolic, neuropsychiatric and pain-related disorders, including postexertional malaise, fatigue, dizziness, brain fog and gastrointestinal symptoms.5 The heterogeneity of long COVID necessitates attention to specific clusters of individuals who are suffering from similar symptoms. Proper clustering may enable efforts to identify biological, cognitive and behavioural signatures of long COVID that help elucidate underlying mechanisms to guide the development of diagnostic and therapeutic strategies.
Some individuals with long COVID manifest symptoms that they describe as internal tremors and vibrations. To date, these symptoms, as experienced by patients, have not yet been well described. There are reports of patients with myoclonus, but they are described from the perspective of clinicians.6–13 Although no underlying cause of the myoclonus episodes among patients with long COVID has been identified, other studies have reported cases of myoclonus episodes following COVID-19.14–16
To understand the perspective of patients who have long COVID with tremors and vibrations as a prominent component, we leveraged the efforts by Survivor Corps, a grassroots COVID-19 patient advocacy group, to gather information from individuals with long COVID who belong to its Facebook group and suffer from these symptoms.17–19 We conducted a qualitative analysis of responses and organised them according to prominent themes. The goal of this study was to characterise the patient perspective and identify a potentially important cluster of similar symptoms that individuals with long COVID are reporting.
Methods
Study design and sample
This study was a narrative analysis of emails and Facebook comments that were received from members of Survivor Corps, a long COVID patient advocacy group where members interact in a Facebook group. The concept for the study originated with the experience of Heidi Ferrer and the initiative of her husband, NG. Heidi had severe manifestations of the sensations of vibrations and exhibited tremors with onset early in the pandemic. Heidi Ferrer ultimately committed suicide as she found the symptoms intolerable. NG spoke with Survivor Corps, which initiated a call for individuals in its Facebook group of over 180 000 individuals to report their experience with vibrations and tremors among those with long COVID via emails and Facebook comments (online supplemental table 1). The qualitative approach was chosen because previous literature characterising the patient perspective on these symptoms is limited.20 In addition, a study participant, LF, was involved as a coauthor in the study design and analysis by reviewing themes before final analysis and providing feedback on the manuscript. This study received an exemption from the Yale Institutional Review Board because the comments had been posted publicly.
bmjopen-2023-077389supp001.pdf (269.9KB, pdf)
Data collection
Data were collected from unstructured responses that included 140 emails and 450 Facebook comments that occurred in response to Survivor Corps’ calls for information in July 2021. Exact dates and names were removed and replaced with month/year and five year age brackets to protect anonymity. Any information about testing and timing of acute COVID infection were based on self-report.
Survivor Corps collected data for this study in three steps. First, on 27 June 2021, the Survivor Corps founder (DBG), posted a Facebook poll, titled ‘Vibration/Buzzing/Pain Poll,’ in the Survivor Corps Facebook group (online supplemental table 1). Responses were in a multiple-choice answer format, where respondents could select multiple answers and also add their own answer choices. There were 20 answer choices, each a statement relevant to vibration, tingling, buzzing and neuropathic sensations (online supplemental table 1). The research team included all poll responses as of 16 July 2021, which totalled 769. In addition, there were 162 Facebook comments posted by group members below the poll as of 16 July 2021, which were all included in data analysis.
Next, Survivor Corps member NG posted in the Survivor Corps Facebook group on 14 July 2021, requesting that anyone with long COVID in the group who had experienced ‘tremors or internal vibrations’ and was interested in participating in a study comment below his post (online supplemental figure 1). By 16 July 2021, there were 288 comments from group members in response to his post, all of which were included in data analysis for this study. In response to members’' comments, NG and DBG requested that commenters share their symptom stories via email with Survivor Corps for the study, with subjects’ consent to use their deidentified emails for research.
Finally, the Survivor Corps newsletter in July 2021 also included a request for ‘Long Haulers’ with ‘neurological tremors or internal vibrations’ to send details of their symptoms to Survivor Corps via email for this study (online supplement 1). Survivor Corps received 140 emails for this study between 15 July through 27 July 2021. All emails were included in data analysis. Including the Facebook comments from the initial poll and the comments from NG’s post, 450 Facebook comments were analysed in this study.
Patient and public involvement
Members of the patient advocacy group, Survivor Corps (DBG, NG, SPS and LF) played a central role in this research, actively engaging through social media and emails to disseminate surveys, collect responses and offer insightful feedback on comprehensive analysis drafts. The development of research questions was profoundly influenced by the patients’ priorities, experiences and preferences, facilitated through multiple interactive sessions that prioritised domain and theme shaping.
Data analysis
Emails
Email data were analysed using common coding techniques for qualitative data and the constant comparative method of qualitative data analysis.21 Coding of the data was accomplished in iterative steps. An initial code list was generated after evaluation of the data by research team members (HMK and DM) (online supplement 2). The initial code list was created in three steps. First, each reviewer separately read the 140 emails (with names and exact dates redacted). Next, each reviewer separately read the 140 emails while creating themes based on the contents of each email, until each statement about internal tremors or vibrations in every email had been assigned to a theme. The reviewers then met to discuss shared themes and reached a consensus on the list of themes. The reviewers then grouped the themes into seven larger domains. At this point, the full research team reviewed the code structure, including a study participant (LF), for logic and breadth.
Using this final version of the code structure, members of the research team (HMK and DM) independently coded all transcripts, then met to code in several joint sessions, achieving consensus and assigning codes to observations by a negotiated, group process. Coded data were entered into NVivo (V.12 (Lumivero, Denver, CO)) to assist in reporting recurrent themes, links among the themes, and supporting quotations.
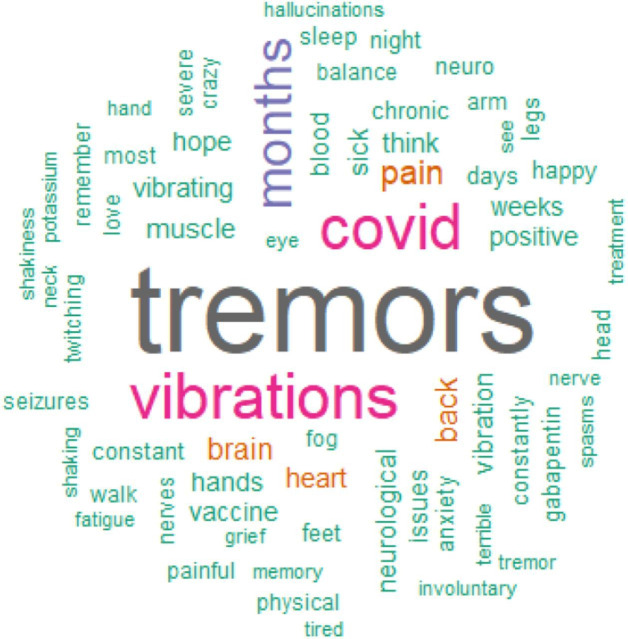
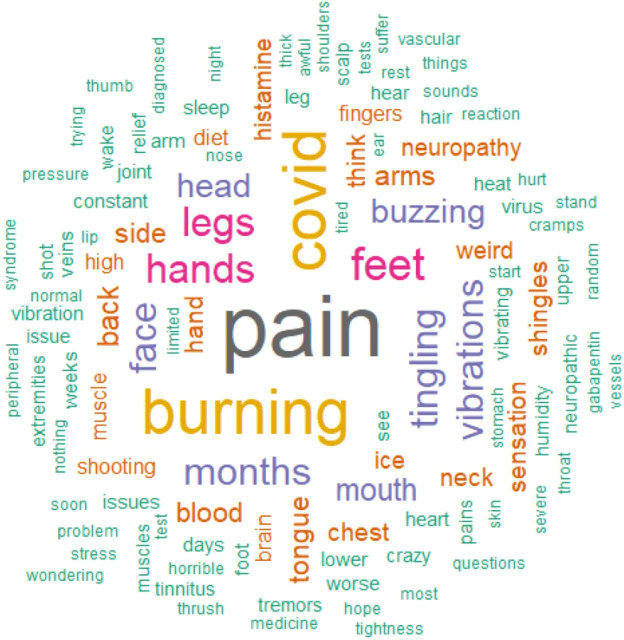
Facebook comments
We used Word Cloud methodology to visualise the prevalence of terms (online supplement 3). A Word Cloud is a visual representation of word frequency derived from written text. The more often the word appears within the passage being analysed, the larger it appears in the image generated. We set the minimum frequency of words to be included in the Word Cloud to 3, the maximum number of words to 200 and removed extraneous filler words. Word Clouds were generated using the quanteda, wordcloud and tm packages in R v4.0.3 (R Development Core Team, Vienna, Austria).22 23
Results
Email data
After review of the email data, respondents’ comments reflected seven domains related to their experience with vibrations and tremors. These domains were as follows: (1) symptom experience, description and anatomic location; (2) initial symptom onset; (3) symptom timing; (4) symptom triggers or alleviators; (5) change from baseline health status; (6) experience with medical establishment and (7) impact on people’s lives and livelihood. There were 22 themes total, each corresponding to one of the broader domains. Sample quotations are listed to illustrate the themes (online supplemental figure 2).
Symptom experience, description and anatomic location
Theme 1: vibrations and tremors were described concomitantly, with descriptions of internal vibrations, visible tremors and some people experiencing both
Example 1
Sometimes my entire body feels like it’s humming and trembling. It’s like I’m sitting on a huge speaker with the volume all the way up. Through the progression of the last few months, the complete body humming has slowed down, but still happens 5–8 times a month. My hands and legs also began tremoring about the same time as the whole body. My legs bop up and down aggressively at times. I’m not cold, I’m not restless, but my legs visibly move up and down like I’m tapping my foot. My hands have been the worst of it. I felt like they had improved a few months ago, but they’re back with a vengeance. I’m not hungry ever. I know I need to eat, and my go-to has been soup. By the time I get the spoon 4 inches above the bowl, and close to my mouth, all of the broth has been ‘shaken’ off. My handwriting. awful. Sometimes I absolutely cannot stand myself and just go to bed. That happens more often than not. I usually try to hide my hands in my pockets or under the table, but am not always able to do that. When my whole body is tremoring, I find it a lot more difficult to focus and to get anything accomplished.’
Example 2
Internal vibrations started about 3 weeks after. They started in my back and back of upper thighs. It felt like I was sitting on a vibration massage chair. They never went away but would vary in intensity. February 2021 I started having restless left arm at bedtime where my left arm would flap until I fell asleep. On (May 2021) it progressed to full body myoclonic movements lasting up to 30 minutes.
Theme 2: vibration or tremor site varied, from the entire body to localisation in extremities, chest, abdomen and other locations
Example 1
I experience daily internal tremors/vibrations all over but mainly inside my brain and chest. I have external tremors in my legs, arms and chest.
Example 2
Still suffering with symptoms. One of which is tremors and internal vibrations primarily in the legs and feet but do sometimes occur in arms.
Theme 3: vibrations and tremors occurred with other symptoms of varying number
Example 1
I also experience relentless headaches. I have had the same one, in varying degrees, since October. Crushing fatigue. Vivid dreams. And the worst, word retrieval.
Example 2
Here is a list of my current symptoms that I have over a year after my acute infection: 1. Extreme Fatigue 2. Exercise Intolerance/Post-Exertion Malaise (Physical and Mental) 3. Short-Term Memory Loss. Must carry a notebook to remember things 4. Brain Fog 5. Muscle Weakness 6. Dizziness. Can’t Drive 7. Seizures 8. Headaches/Migraines 9. High Blood Pressure 10. Cold Hands and Feet 11. Ringing in Ears Tinnitus 12. Hoarseness/Loss of Voice 13. Loss of Coordination in Hands 14. Burning Sensation on Skin Lower Torso.
Theme 4: vibrations and tremors could cause severe pain
Example 1
My brain shakes after a few hours inside my head, my face starts to tingle and numb, and then the full head shaking seizures start. I have severe head pain and nausea constantly from all the seizures.
Example 2
That week of unrelieved spasms left my body barely able to move. Like paralyzed. I had 3 natural child births. I could not fake such 10/10 pain. I have never felt such intense pain, I thought my back would break and my right arm would be completely dislocated twisted out of socket. I could not breathe at times due to the Laryngeal spasms and diaphragm spasms.
Initial symptom onset
Theme 5: vibration and tremor initial onset varied, from the day of initial infection to weeks or even months later
Example 1
Symptoms started on (July). About 3 weeks later, I developed tremors. I've had them ever since.
Example 2
I contracted COVID from an ICU patient in May 2020. A few days later terrible headaches, loss smell, lung, cardio, eye damage. Ongoing problems fatigue, Headaches, Migraines, Imbalance, Dizzy, Vertigo, SOB, COPD, Brady/Tachycardia, SVT, chest pain, Gastric, swallow, voice, cognitive, exercise intolerance, several leaves of absences off work. I had many scans, tests, labs with both normal results and damage results. I have all Records. Then few months later unrelenting Neuro issues vibrations, ripples, tremors, became intense foot cramps, painful ankle, foot drop, leg spasms started mostly r foot. I had to wear ankle brace use cane. Very difficult to sleep. Husband could see ripples under skin and feel the vibrations at times. Body is constantly ‘on’, pain, numb, burning, briar patch, walking on nails, spikes r foot, can't put r foot flat. Also forearms, hands, r side worse.
Theme 6: vibrations and tremors occurred following or during acute COVID-19 infections that varied from mild to severe
Example 1
I was diagnosed with COVID-19 in July of 2020. I spent 2 months in the ICU and 9 days on ECMO.
Example 2
I had a moderate case of Covid in November of 2020 with multiple symptoms. I was never hospitalized. I was recovered one week before my first Long Covid symptom of shortness of breath began.
Symptom timing
Theme 7: vibration and tremor episodes could be brief, or could be prolonged, even constant
Example 1
The internal tremors in my chest generally only last for about 5 seconds or so and then completely subside. The ones in my abdomen are more rare and have lasted for longer, but still less than a minute or so in general.
Example 2
Now here at almost 8 months post covid, I have dealt with these horrible tremors daily. They are constant, they don’t come and go. They are 24/7. I feel them more when I am still and resting or at night and early morning, or during naps. If I can just get up and get going most days, I don’t notice them much, unless the intensity increases and I get breakthrough pain or headaches. But the night time always reminds me they are still there.
Theme 8: vibration and tremor episodes could occur constantly, daily or only when relapses occurred
Example 1
The tremors and the dizziness are daily challenges.
Example 2
Tremors and ‘vibrations’ are a few of the many ongoing symptoms. The tremors I notice in my hands and toes. It lasts for about 10 seconds or less about every 2 to 3 days. The vibrations I notice when I first lay down for bed at night. It lasts about seconds.
Theme 9: vibration and tremor symptoms could completely resolve temporarily and could return up to months later
Example 1
Even now, almost eight months out in July, I still occasionally experience these. They do not occur daily, but do generally happen in conjunction with the relapse of other symptoms, such as mild chest, throat, and back pressure/tightness, and tingling in my extremities.
Example 2
Sometimes my entire body feels like it’s humming and trembling. It’s like I'm sitting on a huge speaker with the volume all the way up. Through the progression of the last few months, the complete body humming has slowed down, but still happens 5–8 times a month. My hands and legs also began tremoring about the same time as the whole body. My legs bop up and down aggressively at times. I'm not cold, I'm not restless, but my legs visibly move up and down like I'm tapping my foot. My hands have been the worst of it. I felt like they had improved a few months ago, but they're back with a vengeance.
Theme 10: people experienced vibrations and tremors over different time periods (even if they were episodic), and some did not have improvement in symptoms after more than a year
Example 1
I got tremors on (December 2020) the day I got covid & it increased to where I had it in my whole body vibrating on head as well increasing during activity. It’s been very debilitating & frustrating. I have been a patient in Rochester Minnesota Mayo Covid Clinic and my symptoms have lessened. However, it is now it is (July) and the tremors have not subsided.
Example 2
I had Covid in early February 2020. I did not know I had it. Severe Headache, sore throat, rash and crushing fatigue. Got better in a flash. 5 months later, the floor dropped out. By early October, hand tremors started. They have diminished and come back intermittently. It is now 18 Months after the initial infection.
Symptom triggers or alleviators
Theme 11: exercise and activity were associated for some with onsets of tremors and vibrations
Example 1
Since then I notice that if I get my heart rate up too high (which could be anything above 110–15) the tremors and vibrations are made worse.
Example 2
I have had long covid for 6 months now, and I get tremors/vibrations/buzzing nerves whenever I overextend myself.
Theme 12: a variety of self-treatment strategies, such as diet modifications and humming, were used to alleviate tremors and vibrations
Example 1
Regarding the nerve issues, I have found very recently that humming in the morning helps me to stop the vibrations faster. I suspect our vagus nerve is being affected.
Example 2
I have experimented with supplements, removing medicines, and diet. Removing all sugar and processed foods from my diet has reduced the internal vibrations. If I ever slip up, the intensity is extreme.
Change from baseline health status
Theme 13: people with vibrations and tremors had varying health states before their COVID-19 infection, from those who were completely healthy to those with pre-existing conditions
Example 1
I was a healthy (30–35 year-old) marathon runner. Now I’m a (30–35 year-old) individual who is grieving who the person was, figuring out how this new body works, realizing it still works differently day-to-day, while also having physicians refuse to treat me.
Example 2
I am an extremely physically active (50–55 year-old) peri-menopausal Canadian female with no pre-existing conditions except for being a migraine sufferer all my adult life.
Experience with medical establishment
Theme 14: medical testing failed to reveal the mechanism of either tremors or vibrations
Example 1
Had a brain CT & brain MRI (all normal). 2. After a short duration of sleep or a nap (15–30 min), upon waking I feel that my heart is racing, like palpitations. I feel shaky…as if there is a fast motor running inside me. I've now learned to sit up slowly and give it a few minutes and then it goes away. Diagnostic cardiac/pulmonary tests I’ve had: EKGs, CT Thoracic Stress test, Echocardiogram, Pulmonary Function & Blood Oxygen Stress (all normal). Had over 50 lab/blood tests and all normal.
Example 2
Had MRI that showed micro clots and white matter. Had an EEG but do not know results.
Theme 15: tremor and vibration symptoms were sometimes doubted or dismissed by doctors
Example 1
Some doctors have been very dismissive and charted that ‘she just prefers not to walk.’ When I arrived at ER, my previous Neurology MD requested Pysch consult.this delayed medical evaluation. They did not believe my pain nor that I could not breathe as my husband begged them to roll me to my side as they tied me flat to the bed. Most of the time I could barely speak as spasms affected my mouth. The previous Neurologist told me to ‘dumb myself down as a nurse and quit researching and causing myself stress’.
Example 2
In August 2020, when my heart started racing for hours, I tried to speak to my pulmonologist, and they had a local doctor call who was running a test site, and wanted to assure me it wasn't possible for me to have Covid because (1) it wasn't in our area yet, but I was in Boston the day before they announced an outbreak, (2) that symptoms only last 2 weeks max, and I explained Long Covid. (3) That I shouldn't read research that I can't understand, but I used to work in a med related field, trained in pre-med/vet including epidemiology, was part of a 2010–2015 pandemic task force related group, and currently work in genetics research, so then she said that (4) this is all in my head and I just need to get over myself and get back to work full time (I was) and that work makes people better (fatigue says no). She yelled at me for over 2 hours. She now is in charge of home bound patient care and tells people they need to have compassion for Long Covid as it can take ‘a few weeks to recover’ and then tells stories about people who recover quickly being examples of ‘good people’ while insinuating that those who stay ill don't want to heal. My doctors have run the gamut of not believing me; to finally agreeing that Long Covid is real but that since I don't have a positive test, I can't have it; to even if I have Long Covid, they don't have treatment, so short of an ER admit, I just need to suck it up.
Theme 16: the vaccine was associated with both improvement in symptoms for some people, and a relapse in symptoms for others
Example 1
I had slight tremors in my hands after originally getting sick in June 2020 and after my second vaccine, on (May 2021) (two days later) I started having more seizure-like symptoms.
Example 2
I had the internal vibrations intensely during my year of long haul. Since the vaccine most of my symptoms have abated or significantly diminished. I do still have some of the internal vibration though, especially after exertion.
Theme 17: medications have been provided for tremor symptoms, with varying results
Example 1
They tried Gabapentin but it didn’t stop them. From March through (July) I had 5–9 seizures trying to fall asleep every night, but they only happened at night. Since the Gabapentni wasn’t working they switched me to Topamax. I was ramping into Topamax throughout June but it wasn’t working either. My family and I got sick again at the end of June with something viral (multiple negative Covid, Flu, and Strep tests that week). The same time they adjusted my Topamax dosage up again. Something changed again. Suddenly I was having non-stop seizures back to back and was hospitalized (July) and also again on (July) at two different hospitals for uncontrolled seizures. My EEG showed normal and they switched meds again to Keppra. So far I am on 500 mg Keppra 2x day and ramping up, but my seizures are uncontrolled. The meds work only for a few hours and I have had to go on Short Term Disability from work.
Example 2
He also put me on the very lowest dose gabapentin 3x per day. I began the medication the same night. The next day I had a terrible headache but something felt different. I continued the meds 3x per day like directed. After 1 week I began to be able to get up and move a little. I began doing dishes and light house work. My family was rejoicing. I was improving. After a few weeks of being on the medication I could tell it was helping with all the pain. The tremors were still there, but were farther in the background, if that makes sense?.as if they had been put on soft mute. The meds weren't stopping the tremors but calmed them I guess.
Impact on people’s lives and livelihood
Theme 18: vibrations and tremors were associated with mental health effects, including anxiety, depression and suicidal thoughts
Example 1
The psychologist who saw me for 30 minutes gaslit me saying I need to exercise more as my severe depression could be the cause of my symptoms when I called him on that he said he noted in his report ‘as tolerated’ that my chronic fatigue syndrome could also be the cause but he doesn't deal with that only psychological causes. My therapist says I am clearly depressed because of my fatigue from what she has seen for a year. Being in constant pain, unable to participate in life day after day, month after month is depressing. Of course I feel useless. Of course I feel things might not get better. I haven't been functioning for 16 months!
Example 2
I could not sleep and went 15 days straight with no sleep. I was suicidal in addition to all the other Covid symptoms, thus one showed up two months after my acute Covid.
Theme 19: vibration and tremor symptoms caused disability for some people
Example 1
I am writing to advise that I am one of the Covid long-haulers who is experiencing hand tremors. I feel them in my arms also and occasionally in my voice and breathing. The tremors in my hands are so severe that I cannot grip or hold a pen for any length of time before my hand writing deteriorates to chicken scratch. I have also resorted to dictating many of my emails and messages because my fingers don’t hit the right keys. I don’t know if tinnitus qualifies as internal vibration but I do have it and it is getting louder all the time. It causes me great anxiety and I have not been able to discover a treatment or solution.
Example 2
Since March, I have had limited mobility as my legs give way and do not have the strength to walk unassisted. I have to use a chair to shower and walk with a cane. I cannot walk across the room without falling into things and struggle with balance. I have felt internal tremors that feel like a fizzing/bubbling that moves through my trunk and extremeties. My arms and legs shake and I have problems even with holding my fork still to feed myself. My mind doesn't cooperate most days and I have speech issues with slurred speaking and stuttering.
Theme 20: vibrations and tremors could disturb or prevent sleep
Example 1
Mostly Every morning waking up, there is an electrical zap from the top of my spine to mid back. Before I knew what the correct term was, I was telling doctors I buzz like a battery. This sensation happens first when I’m opening my eyes in the morning. It’s the first conscious feeling in the morning every day. If I try and go back to sleep the vibrations get more intense and more upsetting. So the best thing to do on waking up is just get up and go on about my day. If I take a nap during the day. No problem, no vibrations. But there is a limit that I can sleep at any time, so if I do nap When I wake up, I don’t try and sleep more. There is I feel, a component of the vibrations That affect my sleep. I am very tired and feel most nights that my brains at war with itself and I don’t feel refreshed when waking up. Sometimes, not very often, I will get a whole body tremor feeling it’s unpleasant but, doesn’t last very long. I would say the ones that wake me up in the morning are more bothersome because I do not wake up gently or quietly. It really is internal torture.
Example 2
Just when I thought I was done developing new symptoms in March this started, every time I start to fall asleep I get shooting pain and immense pressure in my arms, legs and spine. It wakes me up instantly. Imagine all the times you doze off a little in the day, times that by 20 if you are on medications that make you sleepy and try to imagine how torturous that symptom is when it happens to you 20 times a day. No one knows what this is or how to stop it. I'm forced to take muscle relaxers, lyrica, and Ativan to try to get to sleep before the symptom starts.
Theme 21: vibration and tremor symptoms could prevent people from working or carrying out daily life activities
Example 1
I am not the person I was before Covid. I used to paint, refinish furniture, hang out with girlfriends, dance, golf, bike, travel, date. Now I barely have the energy to help my patient which is the only reason I have a roof over my head. If I can't do it at any point, he needs to replace me and I lose my place to stay. I have no income and I couldn't possibly work.
Example 2
I got covid (September 2020). I’m a nurse practitioner and cared for patients with Covid. I tried to go back to work. And after my psych Neuro testing I was found to have cognitive decline and severe memory recall and other memory issues. I was pulled from work (March), and then let go (May).
Theme 22: vibration and tremor symptoms could cause financial stress, through a combination of medical care costs and loss of income from medical leave
Example 1
Before the pandemic was looking for another part time job so could live in a better place Now am drowning in medical debt with no relief in sight or ability to hold a job This has devastated my life Now am stuck living in an old garage without plumbing Hauling water back and forth from a garden hose and dumping dirty water takes what little energy have.
Example 2
I got Covid (September 2020) and continue to have daily debilitating symptoms that have prevented me from going back to work. Side note: is there any government funding for those of us who are long haulers and can’t get back to work yet? My short term disability ran out beginning of April and I’ve been without any income since. It’s getting really tough.
For all 450 comments combined, the 10 most frequent terms were tremors (64%), COVID (55%), pain (51%), vibrations (43%), months (36%), burning (29%), feet (24%), hands (22%), legs (21%) and back (20%). Two Word Clouds were generated based on prevalent terms related to the themes found in emails.
The first Word Cloud (figure 1) analysed 288 comments in response to a post that requested people experiencing tremors or internal vibrations to comment. This Word Cloud revealed that the five most common words used in comments were as follows: tremors, COVID, vibrations, months and pain. Words included also indicated that symptoms ranged in presentation and severity, and vibrations were mentioned, as were seizures, shaking and twitching. This Word Cloud also included other long COVID symptoms including brain fog, fatigue and anxiety. Words indicating timing and duration of symptoms included months, days and constantly. The only medication captured was gabapentin. Finally, similar to the email responses, comments included mentions of sleep and being tired.
Figure 1.
Word Cloud from comments in response to a post.
The second Word Cloud (figure 2) was created based on 162 comments to a Survivor Corps poll that asked respondents about vibration or buzzing sensations and neuropathic pain. This Word Cloud revealed that pain, burning, COVID, legs, hands and feet were the most common terms mentioned in comments. This Word Cloud included terms related to sensations such as burning and symptoms such as shingles and thrush.
Figure 2.
Word Cloud from comments on a Survivor Corps poll.
Discussion
This study describes key themes and experiences among a group of individuals reporting long COVID and a prolonged and debilitating symptom complex that prominently involves internal tremors and vibrations. While symptom experiences were heterogeneous—in symptom timing, medical history and initial infection, for instance—there were also common themes in how individuals described these symptoms and their effects. Individuals also reported how diagnostic evaluation and medical care have not yet identified possible mechanisms or successful treatment for these symptoms.
Although the causal pathway remains unclear from these patient reports alone, these patient experiences demonstrate the prolonged and debilitating symptom complex associated with long COVID. Many of the themes identified in this analysis demonstrate physical suffering, including due to severe pain (theme 2), constancy of the tremor episodes (theme 7) and tremors lasting for months or even over a year after initial infection (theme 10). Our findings, importantly, also demonstrate how the suffering from this symptom complex invades peoples’ lives, livelihood and psychological well-being. Themes included effects on mental health such as anxiety, depression and suicidality (theme 18) aligning with recent studies,5 24–26 and effects on daily functioning including inability to exercise (theme 11), sleep deprivation (theme 20) and even disability (theme 19). The cumulative toll of these limits on daily functioning and well-being led some people to have to quit or pause working and household or family responsibilities (theme 21) and to fall into subsequent debt or financial distress (theme 22). Each individual’s experience with these symptoms was different, and not all experienced the most severe effects. However, the reports revealed a pattern that these symptoms could cause immense pain and disruption to daily lives and livelihood.
This study extends the literature in several ways. Previous literature consists of case series that provide preliminary reports of patients’ clinical presentation, course of care and outcomes, but information on people’s experience with tremors more broadly has not been described in relation to long COVID.6–13 In addition, the literature describes symptoms from the point of view of healthcare providers, but not from patients. Previous case-series reports included a total of 16 people previously infected with SARS-CoV-2 who suffered from myoclon us-ataxia syndrome between 3 days and 6 weeks after acute, often mild or moderate, infection.5–12 Our report attempts to add a larger, broader overview of experiences of these symptoms. Our analysis expands on the sensorimotor symptoms described to date. Furthermore, we describe symptoms experienced by individuals who might not have sought formal medical care.
This study, although limited in scope, is an effort to channel the perspective of patients for a condition that has yet to be defined. The utility of this study is that it may enable more formal and structured data collection for individuals with this syndrome. These experiences should be more rigorously characterised to develop hypotheses and understand mechanisms.
There are several key implications of the work. First, internal vibrations and tremors cause severe suffering, both physically and mentally, for a group of individuals after self-reported SARS-CoV-2 infection. Second, while the overall scale of these symptoms is still unknown, this group of people experiencing the symptoms have neither recovered from the symptoms nor have they received specific diagnoses or been given treatment that completely alleviates their suffering. Third, the descriptions of feeling internal vibrations and tremor symptoms were similar across this group of patients and independent of one another’s responses as the emails were not seen by the other participants.
This study has several limitations. Respondents were a convenience sample with minimal information about their demographic or clinical characteristics, including laboratory-confirmed infection with COVID-19. Any information about testing is based on self-report. As such, we cannot determine whether these symptoms were caused by their infection with SARS-CoV-2, or whether the symptoms reported by different people were the same symptom complex or of the same aetiology. We also cannot determine whether the sample is representative of the source population experiencing these symptoms. The data are self-reported and cross-sectional; information was limited to what individuals provided in their initial communication and there was no follow-up. This limited the scope of findings and may have excluded information that medical professionals would have found relevant. This sample may have been skewed towards individuals healthy enough to be active members of a patient community (Survivor Corps) and to email a response to the group. Finally, this study cannot provide information on the incidence and prevalence of these symptoms.
In conclusion, some individuals report experiencing internal vibration and tremor symptoms, often causing intense suffering, after a self-reported history of SARS-CoV-2 infection. The symptoms had some common features but there was variability in timing, concomitant symptoms and impact. Further research is needed to understand and alleviate this suffering by studying the extent and scope of these symptoms, possible mechanisms, and potential treatment.
Supplementary Material
Footnotes
Twitter: @MitsuakiSawano, @cesarcaraballoc, @hmkyale
Contributors: DM and MS served as first coauthors. DM played a key role in planning, designing, analysing data and drafting the manuscript. MS critically reviewed the manuscript and took charge of the major revisions after peer review, contributing significantly as a first coauthor. Other contributors, ADB, DBG, NG, SPS, LF, CBG, CC, TZ, RS and HMK, played crucial roles in carefully evaluating the manuscript. DBG and NG were involved in designing the project and collecting data. CBG, responsible for data analysis and manuscript drafting, contributed substantially to the revision process. HMK, in addition to planning and drafting, provided valuable supervision and is responsible for the overall content as the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: In the past 3 years, Dr Krumholz reported receiving personal fees from Massachusetts Medical Society, UpToDate, Element Science, Eyedentify and F-Prime. He is a cofounder of HugoHealth, Refactor Health and Ensight-AI. He is associated with grants and/or contracts, through Yale New Haven Hospital, from the Centers for Medicare & Medicaid Services and through Yale University from Johnson & Johnson Consumer, Janssen and Pfizer. The other authors report no potential conflicts.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Deidentified data in the present study are available upon reasonable request to the authors.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants, but the Yale Institutional Review Board exempted this study. Subjects consented to their email being used for research by responding ‘yes’ to an email from Survivor Corps group members asking if their deidentified email could be shared with researchers. No consent was obtained for the publicly shared Facebook comments and stories. As indicated in the Ethics Approval section, while this study involves human participants, it was granted exemption by the Yale Institutional Review Board.
References
- 1.Groff D, Sun A, Ssentongo AE, et al. Short-term and long-term rates of Postacute sequelae of SARS-Cov-2 infection: a systematic review. JAMA Netw Open 2021;4:e2128568. 10.1001/jamanetworkopen.2021.28568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davis HE, Assaf GS, McCorkell L, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021;38:101019. 10.1016/j.eclinm.2021.101019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carfì A, Bernabei R, Landi F, et al. Persistent symptoms in patients after acute COVID-19. JAMA 2020;324:603–5. 10.1001/jama.2020.12603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. The Lancet 2021;397:220–32. 10.1016/S0140-6736(20)32656-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thaweethai T, Jolley SE, Karlson EW, et al. Development of a definition of Postacute sequelae of SARS-Cov-2 infection. JAMA 2023;329:1934–46. 10.1001/jama.2023.8823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Przytuła F, Błądek S, Sławek J. Two COVID-19-related Video-accompanied cases of severe ataxia-myoclonus syndrome. Neurol Neurochir Pol 2021;55:310–3. 10.5603/PJNNS.a2021.0036 [DOI] [PubMed] [Google Scholar]
- 7.Schellekens MMI, Bleeker-Rovers CP, Keurlings PAJ, et al. Reversible myoclonus-ataxia as a Postinfectious manifestation of COVID-19. Mov Disord Clin Pract 2020;7:977–9. 10.1002/mdc3.13088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Emamikhah M, Babadi M, Mehrabani M, et al. Opsoclonus-myoclonus syndrome, a post-infectious neurologic complication of COVID-19: case series and review of literature. J Neurovirol 2021;27:26–34. 10.1007/s13365-020-00941-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah PB, Desai SD. Opsoclonus myoclonus ataxia syndrome in the setting of COVID-19 infection. Neurology 2021;96:33. 10.1212/WNL.0000000000010978 [DOI] [PubMed] [Google Scholar]
- 10.Dijkstra F, Van den T, Willekens B, et al. Myoclonus and cerebellar ataxia following Coronavirus disease 2019 (COVID-19). Mov Disord Clin Pract 2020;7:974–6. 10.1002/mdc3.13049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grimaldi S, Lagarde S, Harlé J-R, et al. Autoimmune encephalitis concomitant with SARS-Cov-2 infection: insight from (18)F-FDG PET imaging and neuronal Autoantibodies . J Nucl Med 2020;61:1726–9. 10.2967/jnumed.120.249292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foucard C, San-Galli A, Tarrano C, et al. Acute cerebellar ataxia and myoclonus with or without Opsoclonus: a para-infectious syndrome associated with COVID-19. Eur J Neurol 2021;28:3533–6. 10.1111/ene.14726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wright D, Rowley R, Halks-Wellstead P, et al. Abnormal Saccadic Oscillations associated with severe acute respiratory syndrome Coronavirus 2 encephalopathy and ataxia. Mov Disord Clin Pract 2020;7:980–2. 10.1002/mdc3.13101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan JL, Murphy KA, Sarna JR. Myoclonus and cerebellar ataxia associated with COVID-19: a case report and systematic review. J Neurol 2021;268:3517–48. 10.1007/s00415-021-10458-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Della Corte M, Delehaye C, Savastano E, et al. Neuropsychiatric syndrome with myoclonus after SARS-Cov-2 infection in a Paediatric patient. Clin Neurol Neurosurg 2022;213:107121. 10.1016/j.clineuro.2022.107121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anand P, Zakaria A, Benameur K, et al. Myoclonus in patients with Coronavirus disease 2019: A multicenter case series. Crit Care Med 2020;48:1664–9. 10.1097/CCM.0000000000004570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Massey D, Berrent D, Krumholz H. Breakthrough symptomatic COVID-19 infections leading to long COVID: report from long COVID facebook group poll. Epidemiology [Preprint]. 10.1101/2021.07.23.21261030 [DOI]
- 18.Lambert NJ, Survivor Corps . ‘COVID-19‘long Hauler’ symptoms survey report 2020’. n.d. Available: https://dig.abclocal.go.com/wls/documents/2020/072720-wls-covid-symptom-study-doc.pdf
- 19.Lambert N, Corps S, El-Azab SA, et al. COVID-19 survivors’ reports of the timing, duration, and health impacts of post-acute sequelae of SARS-cov-2 (PASC) infection. Infectious Diseases (except HIV/AIDS) [Preprint]. 10.1101/2021.03.22.21254026 [DOI]
- 20.Crabtree BF, Miller WL. Doing qualitative research. Thousand Oaks, Calif: Sage Publications, 1999: 406. [Google Scholar]
- 21.Miles MB, Huberman AM. Qualitative data analysis:An expanded sourcebook. Thousand Oaks: Sage Publications, 1994. [Google Scholar]
- 22.Benoit K, Watanabe K, Wang H, et al. An R package for the quantitative analysis of textual data. JOSS 2018;3:774. 10.21105/joss.00774 [DOI] [Google Scholar]
- 23.Feinerer I, Hornik K, Meyer D. Text mining infrastructure in R. J Stat Softw 2008;25:1–54. 10.18637/jss.v025.i05 [DOI] [Google Scholar]
- 24.Gasnier M, Choucha W, Radiguer F, et al. Comorbidity of long COVID and psychiatric disorders after a Hospitalisation for COVID-19: a cross-sectional study. J Neurol Neurosurg Psychiatry 2022. 10.1136/jnnp-2021-328516 [DOI] [PubMed] [Google Scholar]
- 25.Wang S, Quan L, Chavarro JE, et al. Associations of depression, anxiety, worry, perceived stress, and loneliness prior to infection with risk of post-COVID-19 conditions. JAMA Psychiatry 2022;79:1081–91. 10.1001/jamapsychiatry.2022.2640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xie Y, Xu E, Al-Aly Z. Risks of mental health outcomes in people with COVID-19: cohort study. BMJ 2022;376:e068993. 10.1136/bmj-2021-068993 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-077389supp001.pdf (269.9KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Deidentified data in the present study are available upon reasonable request to the authors.