Abstract
Purpose
To evaluate online, self-reported pudendal nerve or perineal injuries related to the use of a perineal post during hip arthroscopy.
Methods
Public posts on Reddit and the Health Organization for Pudendal Education were searched to identify anonymous individuals reporting symptoms of pudendal nerve or perineal injury following hip arthroscopy. Included posts were by any individual with a self-reported history of hip arthroscopy who developed symptoms of pudendal nerve injury or damage to the perineal soft tissues. Demographic information and details about a person’s symptoms and concerns were collected from each post. Descriptive statistics were used to analyze the data.
Results
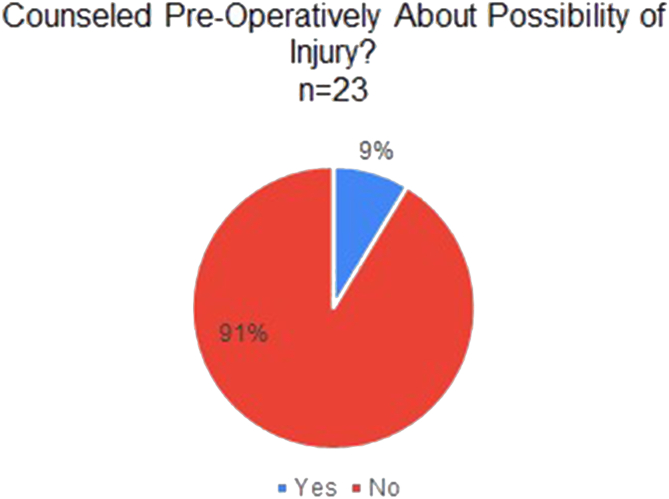
Twenty-three online posts reported on a perineal post-related complication following hip arthroscopy. Sex information was available in 16 (70%) posts (8 male, 8 female). Twenty-two posts reported a sensory injury, and 4 posts reported a motor injury with sexual consequences (sexual dysfunction, dyspareunia, impotence). Symptom duration was available in 15 (65%) posts (8 temporary, 7 permanent). Permanent symptoms included paresthesia of the perineum or genitals (7) and sexual complaints (5). Two posts stated they were counseled preoperatively about the possibility of this injury. Zero patients reported that a postless hip arthroscopy alternative was an option made available to them before surgery.
Conclusions
A high incidence of permanent pudendal nerve, perineal skin, and genitourinary/sexual complications are self-reported and discussed online by patients who have undergone post-assisted hip arthroscopy. These patients report being uninformed and undereducated about the possibility of sustaining a post-related complication. No patient reported being informed of postless hip arthroscopy preoperatively.
Clinical Relevance
Identifying and evaluating self-reported patient information in online medical forums can provide important information about patient experiences and outcomes.
Arthroscopic hip-preservation surgery, also known as hip arthroscopy, continues to rapidly grow in terms of international volume of cases performed, complexity of clinical practice, research, education, and innovation.1, 2, 3, 4, 5, 6 Labral preservation, correction of femoroacetabular impingement syndrome pathomorphology, and capsular management are all accepted surgical indications when paired with appropriate clinical decision-making.1,4 Most hip arthroscopy clinical outcomes evidence is based on a perineal post-assisted technique to achieve distraction. Unfortunately, by nature of the post and human anatomy, pressure-related injury can occur with excessive traction time or excessive force of traction. Although most publications report these complications to be low in incidence and temporary, with several even reporting 0% incidence or 0% permanence, these are likely underestimates.7, 8, 9 Thus, postless hip arthroscopy has emerged due to its elimination of post-related soft-tissue and nerve complications.10
Rates of post-related complications have been reported to be as high as 46%, and this is one of the most common complications associated with hip arthroscopy.7,9,11,12 Post-related complications to reproductive organs have been reported to be as high as 25%.10 Despite multiple advancements to aid in joint distraction while reducing perineal pressure (e.g., increased post diameter and padding, post lateralization, Trendelenburg patient positioning, use of air arthrogram, adequate muscle relaxation), post-related complications still occur.13, 14, 15, 16 Manifestations of post-related complications include soft-tissue damage (male and female genitourinary organs and the perineum) and nerve injury (pudendal, anterior branch of obturator, genitofemoral, ilioinguinal, iliohypogastric, cluneal nerves). The resulting nerve damage can cause numbness and/or paresthesias to the perineum, medial thigh, and reproductive organs, sexual dysfunction, dyspareunia, impotence, hypoorgasmia, anorgasmia, erectile dysfunction, increased or decreased urinary frequency, urinary incontinence, and skin damage. The possibility of pudendal neuropraxia or perineal soft-tissue injury is generally not mentioned on the websites of professional orthopaedic surgery organizations, with the possibility of nerve damage briefly mentioned in the patient education section on 2 webpages.17, 18, 19, 20, 21
Once a post-related complication occurs, due to the sensitive location and manifestations of injuries to the perineum or pudendal nerve, patients may be reluctant to disclose this information to their surgeon. These injuries often are reported to be temporary and likely overlooked. Previous evidence has demonstrated a positive tone on social media when discussing hip arthroscopy but did not provide explanations of why negative or neutral tones are present.22 Patients may be more likely to bring up sensitive complications like these online to see whether other patients have had a similar outcome before, or instead of, talking with their surgeon. However, due to the lack of anonymity through social media, patients may be reluctant to share their experience regarding such a sensitive issue. The purpose of this study is to evaluate online, self-reported pudendal nerve or perineal injuries related to the use of a perineal post during hip arthroscopy. The authors hypothesized that there would be a greater number of permanent post-related complications on anonymous online forums compared with peer-reviewed published hip arthroscopy literature.
Methods
Study Design
This cross-sectional study identified anonymous online discussion platforms with deidentified, free, and publicly available information; therefore, ethical approval was not sought. Any online discussion platform with personal identifying information, password protection(s), or pay-per-use was not used. No identifying information was obtained from any post for this study. Search strategies were performed relevant to each webpage. Included posts were by any individual with a history of hip arthroscopy who developed symptoms of pudendal nerve injury or damage to the perineal soft tissues. Excluded posts were those in which the poster did not undergo hip arthroscopy, or who had preexisting symptoms related to pudendal nerve pathology and could not be solely linked to their surgical procedure. Two authors (B.M.H. and A.E.W.) agreed upon all posts through formal discussion for inclusion before statistical analysis.
Anonymous Online Discussion Forums
Reddit is a free discussion website publicly viewable to all and requires an account to post content. Reddit is divided into “subreddits,” which are created by users to discuss areas of interest and are identified by the convention “r/.” For example, r/HipImpingement is a group dedicated to discussing hip impingement and labral tears. To help focus content, r/HipImpingement and r/ChronicPain were identified as 2 subreddits likely to yield posts for analysis. r/HipArthroscopy was of interest to include for analysis but does not exist and therefore could not be evaluated. Initially, the entire Reddit website was searched using combinations of the terms genital numbness, numbness, and nerve with hip, hip surgery, and hip impingement. The search was repeated on r/HipImpingement and r/ChronicPain to ensure no relevant posts were missed for evaluation.
The Health Organization for Pudendal Education website provides an anonymous online forum available to anyone who creates an account and was identified through a Google search using “support group, pudendal nerve” with the goal of identifying an additional message board for analysis. All posts are publicly viewable without an account. An account is only required to create a post. The forum provides a search function that was searched with the following terms: hip arthroscopy, hip surgery, perineal post, complications, nerve, and arthroscopic.
Data Collection
Discussion posts were identified through the search on both Reddit and Health Organization for Pudendal Education forums that met inclusion criteria for further analysis. Data regarding the following variables were extracted from each post: sex, original post or reply to a post, age, pudendal nerve injury–sensory, pudendal nerve injury–motor, skin injury (perineal or genital areas), genitourinary dysfunction, sexual dysfunction, duration of symptoms, severity of symptoms, and preoperative counseling on possibility of the complication. When present, the duration to resolution was classified as temporary or permanent based on the description provided in the post being evaluated. The incidence of permanent pudendal nerve, perineal skin injury, or sexual dysfunction was extracted from the largest synthetic reviews in the literature and was a combined 0%.7,9,23, 24, 25 The following symptoms were sought: paresthesias, numbness, burning, stinging, tingling, prickling, painful cold, itching, “pins and needles,” “electric shock” of labia, penis, scrotum, perineum, groin, or medial thigh, erectile dysfunction, sexual dysfunction, impotence, hypoorgasmia, anorgasmia, dyspareunia, pain with sexual intercourse, urinary frequency, urinary incontinence, urinary retention, and dysuria. In addition, we assessed for the presence of mental health, psychological, or psychiatric impact the injury has/had on their life (fear, scared, depressed, exhausted, confused, sad, desperate, hopeless, hopeful, sleep disturbance, social withdrawal, among others). Concise quotes about the impact on their life were extracted for qualitative analysis. Lastly, patient posts identifying a specific health care worker (surgeon, nurse, physician assistant) counseling them were evaluated for an understanding of the source of their symptoms, their expectations related to the duration of symptoms (temporary or permanent and one of the following: days/weeks/months/years), and when they received this counseling (preoperative or postoperative). All associated posts (i.e., the entire thread of messages containing included patient posts) were evaluated to identify physicians offering explanations regarding the cause of the patient’s reported symptoms. Descriptive statistics were performed based on the collected information. Posts were analyzed for the presence or absence of the collected variables.
Results
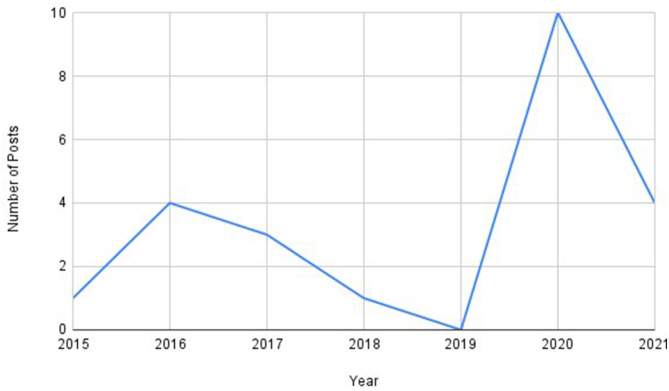
Twenty-three posts met inclusion criteria and were available for analysis (Table 1). The patient posts analyzed were created between July 2015 and June 2021 (Fig 1). Eleven (48%) were original posts, and 12 (52%) were replies to original posts. The sex of the poster was reported in 16 posts (70%): 8 posters stated they were male, and 8 stated they were female. Eight posters reported temporary symptoms, and 7 reported permanent symptoms. Permanent symptoms included (some individuals reported more than 1 permanent symptom): paresthesia of the perineum (6), labia (2), and scrotum (1), with sexual dysfunction (2), dyspareunia (2), and impotence/hypoorgasmia (1). Symptoms of depression were the most common specific emotions mentioned (Table 2). The perineum was the most common anatomic location for sensory injury (Table 3). Significant problems with sexual intercourse were the most common motor deficits mentioned (Table 4). The only patient who reported urinary dysfunction presented as urinary incontinence. Two posters stated they were counseled preoperatively about the possibility of their injury (Fig 2). One poster stated that they were counseled preoperatively about the potential severity of their injury.
Table 1.
Overall Data Extracted From Anonymous Online Forums on Post-Related Pudendal Nerve Injury Following Hip Arthroscopy
| Element Analyzed from Anonymous Online Forums | |
|---|---|
| Sensory injury | 22 |
| Sex | 16 |
| Duration of symptoms | 15 |
| Emotion stated | 10 |
| Motor injury | 4 |
| Counseled on possibility of injury | 2 |
| Counseled on potential severity of injury | 1 |
Fig 1.
Number of anonymous online forum posts identified per year regarding pudendal nerve injury after post-assisted hip arthroscopy.
Table 2.
Emotions and Example Quotations From Anonymous Online Forums Regarding Post-Related Pudendal Nerve Injury and Impact on Their Life
| Emotion | Frequency | Example Quote from Anonymous Online Forums |
|---|---|---|
| Sad, depressed, hopeless | 4 | I feel like this has taken away a lot of my happiness and life. |
| Fear, scared | 4 | It feels as if I simply don't have a penis anymore and I’m very scared. |
| Activity, identity | 2 | I went from a high-level athlete to a couch potato. Will I ever be active again? |
| I don't recognize myself anymore. | ||
| Hopeful | 1 | Hopeful |
| Exhausted, confused | 1 | It has definitely changed who I am as a person, it’s mentally all-consuming when I let it be. |
| Devastation, distrust | 1 | The perineal post is barbaric. I’m a woman who was not warned of the risk by the surgeon I had trusted. I was castrated in 2012 age 34 and have never orgasmed since, it has been devastating. I am sharing my story to create awareness. |
| Anger | 1 | When I asked my surgeon why I was in excruciating pain in my clitoral area after my op, there was no explanation, no reassurance, he shouted “I told you there’d be bruising.” No he hadn’t. I had no idea this post was used. My surgeon knew of the risks yet neglected to advise me. |
Table 3.
Sensory Injury Commentary on Post-Related Pudendal Nerve Injury Following Hip Arthroscopy
| Sensory injury | 22 |
| Perineum | 9 |
| Penis | 8 |
| Medial thigh | 7 |
| Scrotum | 5 |
| Labia | 3 |
Table 4.
Motor Injury Commentary on Post-Related Pudendal Nerve Injury Following Hip Arthroscopy
| Motor injury | 4 |
| Dyspareunia | 4 |
| Sexual dysfunction | 2 |
| Impotence | 1 |
| Hypoorgasmia | 1 |
| Urinary incontinence | 1 |
Fig 2.
Frequency of anonymous online forum posts that mentioned preoperative counseling regarding the potential for post-related injury during hip arthroscopy.
Health Care Worker Counseling
Zero included patient posts mentioned they were informed of postless hip arthroscopy as an alternative option available to them before surgery. Seven patients (30%) received postoperative counseling with a health care worker (surgeon—6, nurse—1, physician assistant—1; one individual received counseling from more than 1 health care worker). Three patients (43%) receiving health care worker counseling incorrectly identified traction alone (duration—1, intensity—1, unspecified—1) as the source of their symptoms. One patient (14%) stated the post in combination with the duration and intensity of traction was the source of his/her symptoms, whereas 2 (29%) of the remaining posts offered no explanation and a final patient post (14%) stated only that his/her surgery was “botched” (Appendix Table 1, available at www.arthroscopyjournal.org). The lone patient who mentioned the perineal post as the cause of his/her symptoms informed the surgeon of symptoms at a postoperative follow-up visit and received counseling. In one (0.8%) post, the individual identified as a physician (urologist). His/her response stated they had researched the problem to offer an explanation and reported the stretch due to traction had put the nerves to sleep.
Discussion
The most important finding of this study is that permanent pudendal nerve, perineal skin, and genitourinary/sexual dysfunction complications may occur following post-assisted hip arthroscopy, and patients post this sensitive information on publicly available discussion platforms in a deidentified manner. This supports the authors’ hypothesis that the incidence of permanent post-related complications may be underrepresented in currently published original research publications and synthetic (systematic reviews, meta-analyses) reviews. Patients identified by the present study reported they were not informed about the possibility of sustaining a post-related complication. No patient reported they were informed of a postless alternative before surgery.
Pudendal nerve injuries often are labeled in the literature as transient/temporary and low incidence. However, there are reports of patients with permanent complications due to the perineal post.10,26, 27, 28 The contrast in reports related to the duration of symptoms may be due to selection and recall biases in conjunction with the sensitive nature of the complication. A retrospective studies’ post-related complication incidence was a significant underestimate of the true incidence (1.4% vs 7.1%, respectively).10,26, 27, 28 The importance of postless hip arthroscopy is emphasized by literature reporting a zero percent incidence with the postless technique during hip arthroscopy compared with 30% incidence of groin numbness with a perineal post.10,28,29
Pudendal nerve injury following hip arthroscopy was described more than 25 years ago.30 Despite increased research efforts in hip arthroscopy, there are still patients being interviewed who report their preoperative education did not match their postoperative patient experience.28,31 If verified in future studies, this represents a significant problem that has ethical and medicolegal implications. Most importantly, patient distress is likely to be intensified in situations in which patients do not feel their preoperative counseling and/or expectations accurately reflects their postoperative experience. As trainees and young surgeons gain experience, they must also gain understanding of their patients’ experiences, which should be a powerful educator to minimize the morbidity of hip arthroscopy.31,32 This unique and anecdotal, online forum-based investigation represents experiences with a complication that deserves further investigation because of the potential impact on our patients’ lives.
Frandsen et al.33 reported an incidence of groin numbness after hip arthroscopy of almost 1 in 4 (22 of 100 patients). Three patients in this cohort experienced their symptoms for longer than 2 months. There are several studies acknowledging the association of pudendal nerve injury with intraoperative risk factors, such as patient positioning and duration of traction.14,34, 35, 36, 37, 38, 39, 40, 41 In a prospective study, Dippmann et al.11 reported on 9 patients (of 50 total; 18%) with postoperative groin numbness up to 6 weeks after post-assisted hip arthroscopy, and 1 subject had erectile dysfunction for 7 weeks. In another prospective post-assisted hip arthroscopy study, Reda and Wong12 reported on 37 patients (of 221 total; 17%) with postoperative groin and genital numbness, with 57% still present at 6 weeks and 32% at 6 months. In another prospective post-assisted hip arthroscopy study, Kern et al.42 reported on 9 patients (of 100 total; 9%) with postoperative pudendal nerve injury with resolution at 2.1 ± 1.7 weeks in all patients. In a systematic review that analyzed 7 hip arthroscopy studies using a perineal post, Habib et al.43 reported a 4.3% incidence of postoperative pudendal nerve injury. Moreover, surgeon experience is critical during hip arthroscopy to minimize complications, as greater hip arthroscopy case volume has shown a reduced risk of reoperations.44,45 Thus, it stands to reason that with increasing experience, both traction time and total surgery time should decrease, with resultant lower time with pudendal/perineal compression if using a post.
Alternatively, recent orthopaedic literature reports elimination of pudendal nerve and perineal soft-tissue complications with the postless technique.12,46,47 Just as the cam correction and labral repair require skillful, accurate, and precise technique to optimize outcome and reduce the incidence of complications, so does the application of traction.48 Both post-assisted and postless techniques can be very safe and highly effective if used appropriately. In more than 20 years and more than 7,000 cases of hip arthroscopy, a surgeon has had zero known pudendal neuropraxia or perineal skin breakdown.48 This is due to skillful technique—post lateralization to minimize pressure over the medial ischial tuberosity, use of 5 to 10° of Trendelenburg, capsule and joint venting, neutral (as opposed to abduction) limb positioning, and minimization of both traction force and duration. The presented investigation reinforces the idea that hip-preservation surgeons, as a community, should continue considering available avenues for improvement in the care provided to our patients. Incorporating the possibility of pudendal or perineal soft-tissue injury into clinical patient education could improve patient experience for surgeons who use a perineal post.
The paucity of orthopaedic literature describing overall positive tones on other social media platforms (Twitter, Instagram), including hip arthroscopy, was not found in this study.22,49, 50, 51, 52, 53 The contrast described between previous studies and the present study is not limited to social media. Sochacki et al.54 reported a comparable trend (public database compared with original research). Anonymous (public database) data reported significantly greater complication rates than original research.54 The described findings must prompt hip-preservation specialists to pursue an understanding of the elements creating dichotomy in reported results. If a post is used, the authors recommend surgeons inquire about development of this complication in the form of survey or clinical interaction at a postoperative visit in order to characterize patient-reported outcomes related to this problem. These modifications in communication have the potential to improve surgeon recognition of the condition, subsequent patient management and, most importantly, patients’ experiences.
Limitations
This observational study is not without limitations. Included posts do not come from verified patients in an electronic medical record associated with a health system and treating surgeons. These posts are publicly available, and any individual can post anything they want. The data may only pertain to a small percentage of people undergoing hip arthroscopy. An unquantifiable number of private posts may provide a larger sample for analysis. Our current investigation did not seek to gain access in password-protected private social media “groups” (e.g., Facebook). An unquantifiable number of private posts may provide a larger sample for analysis. More popular social media platforms (e.g., Instagram, Twitter, Facebook, Snapchat) do not present information in a deidentified fashion, and patients may be reluctant to publicly declare such sensitive issues to their followers.55 Social media propels users to emphasize positive representations of the content they generate, as response bias potentially alienates patients experiencing negative outcomes.
Conclusions
A high incidence of permanent pudendal nerve, perineal skin, and genitourinary/sexual complications are self-reported and discussed online by patients who have undergone post-assisted hip arthroscopy. These patients report being uninformed and undereducated about the possibility of sustaining a post-related complication. No patient reported being informed of postless hip arthroscopy preoperatively.
Data Availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Disclosure
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: R.C.M. reports royalties or licenses and consulting fees from Stryker; leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid: American Academy of Orthopaedic Surgeons, International Society of Hip Arthroscopy, and North Carolina Orthopaedic Association; and stock or stock options from Pattern Health. M.J.K. reports leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid: Arthroscopy. J.D.H. reports royalties or licenses from SLACK Incorporated and Thieme Medical Publishers; consulting fees from Smith & Nephew; leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid: American Academy of Orthopaedic Surgeons, American Orthopaedic Society for Sports Medicine, Arthroscopy Association of North America, Arthroscopy, International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine, and Orthopaedic Research Society; and stock or stock options from PatientPop. All other authors (B.M.H., A.E.W., J.C., D.P., A.E.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Bozic K.J., Chan V., Valone F.H., 3rd, Feeley B.T., Vail T.P. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28(8 suppl):140–143. doi: 10.1016/j.arth.2013.02.039. [DOI] [PubMed] [Google Scholar]
- 2.Cvetanovich G.L., Chalmers P.N., Levy D.M., et al. Hip arthroscopy surgical volume trends and 30-day postoperative complications. Arthroscopy. 2016;32:1286–1292. doi: 10.1016/j.arthro.2016.01.042. [DOI] [PubMed] [Google Scholar]
- 3.Duchman K.R., Westermann R.W., Glass N.A., Bedard N.A., Mather R.C., 3rd, Amendola A. Who is performing hip arthroscopy? An analysis of the American Board of Orthopaedic Surgery Part-II Database. J Bone Joint Surg Am. 2017;99:2103–2109. doi: 10.2106/JBJS.17.00342. [DOI] [PubMed] [Google Scholar]
- 4.Martin H.D., Palmer I.J., Champlin K., Kaiser B., Kelly B., Leunig M. Physiological changes as a result of hip arthroscopy performed with traction. Arthroscopy. 2012;28:1365–1372. doi: 10.1016/j.arthro.2012.04.139. [DOI] [PubMed] [Google Scholar]
- 5.Montgomery S.R., Ngo S.S., Hobson T., et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013;29:661–665. doi: 10.1016/j.arthro.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Sing D.C., Feeley B.T., Tay B., Vail T.P., Zhang A.L. Age-related trends in hip arthroscopy: A large cross-sectional analysis. Arthroscopy. 2015;31:2307–2313.e2. doi: 10.1016/j.arthro.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Harris J.D., McCormick F.M., Abrams G.D., et al. Complications and reoperations during and after hip arthroscopy: A systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29:589–595. doi: 10.1016/j.arthro.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Kollmorgen R.C., Ellis T., Lewis B.D., Harris J.D. Achieving post-free distraction in hip arthroscopy with a pink pad patient positioning device using standard hip distraction tables. Arthrosc Tech. 2019;8:e363–e368. doi: 10.1016/j.eats.2018.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weber A.E., Harris J.D., Nho S.J. Complications in hip arthroscopy: A systematic review and strategies for prevention. Sports Med Arthrosc Rev. 2015;23:187–193. doi: 10.1097/JSA.0000000000000084. [DOI] [PubMed] [Google Scholar]
- 10.Mei-Dan O., Kraeutler M.J., Garabekyan T., Goodrich J.A., Young D.A. Hip distraction without a perineal post: A prospective study of 1000 hip arthroscopy cases. Am J Sports Med. 2018;46:632–641. doi: 10.1177/0363546517741704. [DOI] [PubMed] [Google Scholar]
- 11.Dippmann C., Thorborg K., Kraemer O., Winge S., Hölmich P. Symptoms of nerve dysfunction after hip arthroscopy: An under-reported complication? Arthroscopy. 2014;30:202–207. doi: 10.1016/j.arthro.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 12.Reda B., Wong I. Postoperative numbness: A survey of patients after hip arthroscopic surgery. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118771535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hodax J.D., Flores S.E., Cheung E.C., Zhang A.L. Use of air arthrograms to aid in joint distraction during hip arthroscopic surgery decreases postoperative pain and opioid requirements. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119837389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lall A.C., Saadat A.A., Battaglia M.R., et al. Perineal pressure during hip arthroscopy is reduced by use of Trendelenburg: A prospective study with randomized order of positioning. Clin Orthop Relat Res. 2019;477:1851–1857. doi: 10.1097/CORR.0000000000000804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mei-Dan O., McConkey M.O., Young D.A. Hip arthroscopy distraction without the use of a perineal post: Prospective study. Orthopedics. 2013;36:e1–e5. doi: 10.3928/01477447-20121217-10. [DOI] [PubMed] [Google Scholar]
- 16.Papavasiliou A.V., Bardakos N.V. Complications of arthroscopic surgery of the hip. Bone Joint Res. 2012;1:131–144. doi: 10.1302/2046-3758.17.2000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Orthopaedic Society for Sports Medicine https://www.sportsmed.org/aossmimis/
- 18.American Academy of Orthopaedic Surgeons For Patients and the Public. https://www.aaos.org/about/for-patients-public--the-media/
- 19.ISHA - International Society for Hip Arthroscopy Information for Patients. https://ishasoc.net/information-for-patients/ Published August 31, 2020.
- 20.International Society of Arthroscopy Knee Surgery and Orthopaedic Sports Medicine. https://www.isakos.com/
- 21.Arthroscopy Association of North America Understanding the Risks. https://www.aana.org/AANAIMIS/Members/For_Patients/Understanding_the_Risks/Members/For-Patients/Potential-Risks.aspx?hkey=978acba4-a2d6-4f97-9411-3a142db0ff96&WebsiteKey=10f6eed0-bcab-4019-8f57-18dad8aaf2d7
- 22.Haeberle H.S., Bartschat N.I., Navarro S.M., et al. Hip arthroscopy: A social media analysis of patient perception. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119854188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Sa D., Stephens K., Parmar D., et al. A comparison of supine and lateral decubitus positions for hip arthroscopy: A systematic review of outcomes and complications. Arthroscopy. 2016;32:716–725.e8. doi: 10.1016/j.arthro.2015.12.028. [DOI] [PubMed] [Google Scholar]
- 24.Gupta A., Redmond J.M., Hammarstedt J.E., Schwindel L., Domb B.G. Safety measures in hip arthroscopy and their efficacy in minimizing complications: A systematic review of the evidence. Arthroscopy. 2014;30:1342–1348. doi: 10.1016/j.arthro.2014.04.103. [DOI] [PubMed] [Google Scholar]
- 25.Kowalczuk M., Bhandari M., Farrokhyar F., et al. Complications following hip arthroscopy: A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1669–1675. doi: 10.1007/s00167-012-2184-2. [DOI] [PubMed] [Google Scholar]
- 26.Kraeutler M.J., Fasulo S.M., Harris J.D., Mei-Dan O., Scillia A.J. Current trends in the use of postless hip arthroscopy: A survey of the International Society for Hip Arthroscopy Membership. Orthop J Sports Med. 2022;10 doi: 10.1177/23259671221143353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dumont G.D., Cohn R.M., Gross M.M., Menge T.J., Battle N.C., Thier Z.T. The learning curve in hip arthroscopy: Effect on surgical times in a single-surgeon cohort. Arthroscopy. 2020;36:1293–1298. doi: 10.1016/j.arthro.2019.11.121. [DOI] [PubMed] [Google Scholar]
- 28.Wininger A.E., Mei-Dan O., Ellis T.J., et al. Post-related complications in hip arthroscopy are reported significantly greater in prospective versus retrospective literature: A systematic review. Arthroscopy. 2022;38:1658–1663. doi: 10.1016/j.arthro.2021.11.045. [DOI] [PubMed] [Google Scholar]
- 29.Kraeutler M.J., Fasulo S.M., Dávila Castrodad I.M., Mei-Dan O., Scillia A.J. A Prospective comparison of groin-related complications after hip arthroscopy with and without a perineal post. Am J Sports Med. 2023;51:155–159. doi: 10.1177/03635465221130768. [DOI] [PubMed] [Google Scholar]
- 30.Byrd J.W. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275–280. doi: 10.1016/s0749-8063(05)80111-2. [DOI] [PubMed] [Google Scholar]
- 31.Wininger A.E., Dabash S., Ellis T.J., Nho S.J., Harris J.D. The key parts of hip arthroscopy for femoroacetabular impingement syndrome: implications for the learning curve. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211018703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carreira D.S., Kruchten M.C., Emmons B.R., Startzman A.N., Martin R.L. A characterization of sensory and motor neural dysfunction in patients undergoing hip arthroscopic surgery: Traction- and portal placement-related nerve injuries. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118797306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Frandsen L., Lund B., Grønbech Nielsen T., Lind M. Traction-related problems after hip arthroscopy. J Hip Preserv Surg. 2017;4:54–59. doi: 10.1093/jhps/hnw044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clarke M.T., Arora A., Villar R.N. Hip arthroscopy: Complications in 1054 cases. Clin Orthop Relat Res. 2003;(406):84–88. doi: 10.1097/01.blo.0000043048.84315.af. [DOI] [PubMed] [Google Scholar]
- 35.Funke E.L., Munzinger U. Complications in hip arthroscopy. Arthroscopy. 1996;12:156–159. doi: 10.1016/s0749-8063(96)90004-3. [DOI] [PubMed] [Google Scholar]
- 36.Griffin D.R., Villar R.N. Complications of arthroscopy of the hip. J Bone Joint Surg Br. 1999;81:604–606. doi: 10.1302/0301-620x.81b4.9102. [DOI] [PubMed] [Google Scholar]
- 37.Larson C.M., Clohisy J.C., Beaulé P.E., et al. Intraoperative and early postoperative complications after hip arthroscopic surgery: A prospective multicenter trial utilizing a validated grading scheme. Am J Sports Med. 2016;44:2292–2298. doi: 10.1177/0363546516650885. [DOI] [PubMed] [Google Scholar]
- 38.Lo Y.P., Chan Y.S., Lien L.C., Lee M.S., Hsu K.Y., Shih C.H. Complications of hip arthroscopy: Analysis of seventy three cases. Chang Gung Med J. 2006;29:86–92. [PubMed] [Google Scholar]
- 39.Sampson T.G. Complications of hip arthroscopy. Clin Sports Med. 2001;20:831–835. doi: 10.1016/s0278-5919(05)70288-x. [DOI] [PubMed] [Google Scholar]
- 40.Simpson J., Sadri H., Villar R. Hip arthroscopy technique and complications. Orthop Traumatol Surg Res. 2010;96(8 Suppl):S68–S76. doi: 10.1016/j.otsr.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 41.Smart L.R., Oetgen M., Noonan B., Medvecky M. Beginning hip arthroscopy: Indications, positioning, portals, basic techniques, and complications. Arthroscopy. 2007;23:1348–1353. doi: 10.1016/j.arthro.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 42.Kern M.J., Murray R.S., Sherman T.I., Postma W.F. Incidence of nerve injury after hip arthroscopy. J Am Acad Orthop Surg. 2018;26:773–778. doi: 10.5435/JAAOS-D-17-00230. [DOI] [PubMed] [Google Scholar]
- 43.Habib A., Haldane C.E., Ekhtiari S., et al. Pudendal nerve injury is a relatively common but transient complication of hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2018;26:969–975. doi: 10.1007/s00167-017-4783-4. [DOI] [PubMed] [Google Scholar]
- 44.Degen R.M., Pan T.J., Chang B., et al. Risk of failure of primary hip arthroscopy—a population-based study. J Hip Preserv Surg. 2017;4:214–223. doi: 10.1093/jhps/hnx018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mehta N., Chamberlin P., Marx R.G., et al. Defining the learning curve for hip arthroscopy: A threshold analysis of the volume–outcomes relationship. Am J Sports Med. 2018;46:1284–1293. doi: 10.1177/0363546517749219. [DOI] [PubMed] [Google Scholar]
- 46.Schaver A.L., Mattingly N., Glass N.A., Willey M.C., Westermann R.W. Hip arthroscopy with and without a perineal post: A comparison of early postoperative pain. Arthroscopy. 2021;37:2840–2845. doi: 10.1016/j.arthro.2021.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Welton K.L., Garabekyan T., Kraeutler M.J., et al. Effects of hip arthroscopy without a perineal post on venous blood flow, muscle damage, peripheral nerve conduction, and perineal injury: A prospective study. Am J Sports Med. 2019;47:1931–1938. doi: 10.1177/0363546519849663. [DOI] [PubMed] [Google Scholar]
- 48.Larson C.M. Editorial Commentary: Minimizing traction force and time as well as application of specific technical pearls might trump the importance of choosing between post or postless hip arthroscopy with regards to complications. Arthroscopy. 2023;39:748–750. doi: 10.1016/j.arthro.2022.11.017. [DOI] [PubMed] [Google Scholar]
- 49.Ng J.P., Tarazi N., Byrne D.P., Baker J.F., McCabe J.P. Scoliosis and the social media: Facebook as a means of information exchange. Spine Deform. 2017;5:102–108. doi: 10.1016/j.jspd.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 50.Ramkumar P.N., La T., Jr., Fisch E., et al. Integrating social media and anterior cruciate ligament surgery: An analysis of patient, surgeon, and hospital use. Arthroscopy. 2017;33:579–585. doi: 10.1016/j.arthro.2016.08.021. [DOI] [PubMed] [Google Scholar]
- 51.Ramkumar P.N., Navarro S.M., Haeberle H.S., Chughtai M., Flynn M.E., Mont M.A. Social media and total joint arthroplasty: An analysis of patient utilization on Instagram. J Arthroplasty. 2017;32:2694–2700. doi: 10.1016/j.arth.2017.03.067. [DOI] [PubMed] [Google Scholar]
- 52.Rizkalla J.M., Holderread B., Hotchkiss W., et al. Instagram and spine fusion: An analysis of social media and its relationship to patient perception of surgery. Global Spine J. 2023;13:617–620. doi: 10.1177/21925682211001814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yu J.S., Carr J.B., 2nd, Thomas J., et al. Trends in patient, physician, and public perception of ulnar collateral ligament reconstruction using social media analytics. Orthop J Sports Med. 2021;9 doi: 10.1177/2325967121990052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sochacki K.R., Jack R.A., 2nd, Safran M.R., Nho S.J., Harris J.D. There is a significant discrepancy between "big data" database and original research publications on hip arthroscopy outcomes: A systematic review. Arthroscopy. 2018;34:1998–2004. doi: 10.1016/j.arthro.2018.01.018. [DOI] [PubMed] [Google Scholar]
- 55.Pew Research Center Social Media Use in 2021. https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/ Published April 7, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.