Abstract
The coeliac trunk, the first anterior branch, often originates at the level of the T12 vertebral body, right below the aortic hiatus, as the first ventral branch of the abdominal aorta. It commonly divides into the left gastric, common hepatic, and splenic arteries. We report a rare variation in the branching pattern and course of branches of the coeliac trunk in two donated female cadavers during routine abdominal dissection. It is essential to understand the coeliac trunk and the distinctions in its origin and branching pattern to perform efficient upper abdominal surgical and radiological procedures and to adopt novel interventional and treatment options for hepatic cancers. As anatomists, we are also attempting to link our study’s variations to their embryological genesis.
Keywords: Coeliac trunk, hepatic artery, gastric artery, unusual, variation
Abstract
İlk ön dal olan çölyak trunkus, abdominal aortanın ilk ventral dalı olarak genellikle T12 vertebral cisim seviyesinde, aortik hiatusun hemen altından çıkar. Genellikle sol gastrik, ortak hepatik ve splenik arterlere ayrılır. Bu yazıda, bağışlanan iki kadın kadavrada, rutin abdominal diseksiyon sırasında çölyak trunkusun dallanma paterninde ve seyrinde görülen nadir bir varyasyon sunulmaktadır. Etkin üst abdominal cerrahi ve radyolojik prosedürler gerçekleştirmek ve karaciğer kanserleri için yeni girişimsel ve tedavi seçeneklerini benimsemek için çölyak trunkusu ve kökenindeki ve dallanma paternindeki farklılıkları anlamak çok önemlidir. Anatomi uzmanları olarak biz de çalışmamızdaki varyasyonları embriyolojik oluşumlarıyla ilişkilendirmeye çalışmaktayız.
Keywords: Çölyak trunkusu, hepatik arter, gastrik arter, olağandışı, varyasyon
INTRODUCTION
In pancreatic and hepatobiliary procedures, where direct visualization of the relevant field is complex, the arterial architecture of the coeliac trunk (CT) is extremely valuable. CT is the first ventral branch of the abdominal aorta (AA). CT commences at the level of the T12 and L1 vertebrae. The spleen, lower end of the esophagus, stomach, liver, and proximal section of the duodenum are supplied by CT1. Typically, the CT gives three branches: the left gastric artery (LGA), the common hepatic artery (CHA), and the splenic artery (SA). Haller2 described this traditional branching pattern for the first time as Tripus Halleri in 1756.
Unusual vascular variations may arise because of the preservation of some parts of the longitudinal channels between primitive vessels that ordinarily disappear or because of the disappearance of parts that generally persist3,4. For effective surgical and radiological interventions of the upper abdomen and for implementing innovative interventional and therapy options for hepatic malignancies, it is mandatory to have a firm knowledge of the coeliac axis and the differences pertaining to its origin and branching pattern3. Here, we describe two cadaveric cases with rare variant branching patterns of CT.
CASE REPORTS
An unusual branching pattern of CT and/or its branches in two formalin-embalmed female cadavers was observed during routine dissection of the abdomen for medical undergraduates. Following the instructions in Cunningham’s dissection procedure, the abdomen was dissected, the lesser omentum was reflected, and the origin of CT and its main branches (i.e., LGA, SA, and CHA) was traced neatly5. A detailed study was conducted and photographs were taken. The branching pattern of CT exhibited a variant pattern that was distinct in each case.
Case 1: In a 72-year-old female cadaver, CT was seen trifurcating soon after its origin from the AA into LGA, CHA, and SA and was directed forward and toward the right. From its upper part, LGA arose that was running upwards and to the left and took a U-turn anteroinferiorly at the level of the gastroesophageal junction where it gave an esophageal branch to supply the lower end of the esophagus. Subsequently, along the proximal part of the lesser curvature (LC) of the stomach, LGA divided into anterior and posterior branches to supply the corresponding surfaces of the body of the stomach (Figure 1A, B). The right gastric artery (RGA), which is normally a relatively small artery that usually arises from the hepatic artery proper (HAP), was absent, and the entire stomach was supplied by the LGA.
Figure 1A.

Findings observed in Case 1. Coeliac trunk (CT) was seen trifurcating soon after its origin from the abdominal aorta (AA) into left gastric (LGA), common hepatic artery (CHA) and splenic artery (SA). LGA after taking a ‘U’ turn giving an esophageal branch (OB). CHA in this case is the largest branch of CT which if giving rise to smaller gastro duodenal artery (GDA) and larger hepatic artery proper (HAP). Cystic artery (CA) took origin from HAP ran towards the gall bladder (GB) crossed the common bile duct (CBD) anteriorly which is variant type of relation. Right gastric artery (RGA) is absent in this case.
GDA: Gastroduodenal artery, SPDA: Superior pancreatico duodenal artery, RLL: Right lobe of liver, LLL: Left lobe of liver, RHA: Right hepatic artery, LHA: Left hepatic artery, RGEA: Right gastro epiploic artery, PV: Portal vein, SMV: Superior mesenteric vein, SV: Splenic vein, PB: Pancreatic body, SB: Stomach body, Py: Pylorus
Figure 1B.

Findings observed in Case 1. Hepatic artery proper (HAP) gives rise to three hepatic branches: one to the left lobe [left hepatic artery (LHA)] and two to the right lobe [right hepatic artery 1 & 2 (RHA1 & RHA2)]. RHA2 is again divided into two branches [Branch 1 (Br1) and Branch 2 (Br2)]. Gall bladder is removed in this image.
CHA: Common hepatic artery, PV: Portal vein
CHA in this case was the largest branch of CT, which after origin ran upwards and toward the right. Right free margin of the lesser omentum in front of the portal vein (PV) and common bile duct (CBD), divided into two branches. The smaller branch, Gastroduodenal artery (GDA), just above the first part of the duodenum, is divided into the right gastroepiploic and superior pancreaticoduodenal arteries. Both these arteries followed the usual pattern. The larger branch, ‘HAP’ or proper hepatic artery (PHA) ran upwards toward the porta hepatis (PH) of the liver and soon divided into 4 branches, the cytostic artery (CA) and 3 hepatic branches, one to the left lobe [left hepatic artery (LHA)] and two to the right lobe [right hepatic artery 1 & 2-(RHA1 & RHA2)]. CA, after its origin from the right side of the HAP and ran toward the gall bladder (GB), crossed the CBD anteriorly, which is a variant type of relation. Reaching near the neck of GB, CA split into anterior and posterior branches to supply GB. RHA1 entered the liver passing superficially to PV and CBD through the left end of PH, whereas RHA2 was seen passing deep to PV and CHD through the right end of PH and right lobe of the liver (Figure 1A,B).
Case 2: In another 79-year-old female cadaver, we observed a very short CT, which divided into three divisions soon after, i.e., LGA, hepatosplenic trunk (HST), and a small branch to the left triangular ligament. The LGA was a thinner branch after its origin ran upwards and split into an ascending hepato-gastric artery (HGA) and a descending branch to the LC. HGA ran along the upper end of LC toward the lower end of the esophagus and was divided into the superior and inferior branches. The superior branch was seen entering the PH, and the inferior branch had a somewhat tortuous course and reached the anterior surface of the stomach. In the present case, instead of giving an independent SA, CT gave rise to a larger branch HST with a caliber size similar to that of CT. HST ran towards the right and gave a branch CHA, then took a sinuous course towards the left, lying behind the pancreas’ body and reaching the spleen’s hilum. CHA ascended towards the PH with convexity upwards, giving a descending branch, GDA and its continuation as HAP, which ascended towards the PH of the liver, dividing it into two divisions before entering the PH. RGA and CA were absent in this case. The third and smallest branch directly from CT was a branch to the left triangular ligament of the liver (Figure 2).
Figure 2.

Findings observed in Case 2.
CT: Coeliac trunk, HST: Hepato splenic trunk, SA: Splenic arter, CHA: Common hepatic artery, HAP: Hepatic artery proper, GDA: Gastro duodenal artery, LGA: Left gastric artery, HGA: Hepato gastric artery, Sup Br: Superior branch, Inf br: Inferior branch, LC Br: Lesser curvature branch, Asterisk: An aberrant ranch to the left triangular ligament, LC: Lesser curvature, PB (ref): Pancreatic body reflected, GB: Gall bladder, PH: Porta hepatis, SB: Stomach body
DISCUSSION
The typical trifurcation pattern, as reported by Haller2, is observed in approximately 89% of individuals, irrespective of gender6. In 1917, Lipschutz proposed the first classification, failing to mention the possibility of an absent CT and coeliomesenteric trunk7. Following him, several other researchers have investigated these variants of CT since the 20th century and have proposed their classification (Tables 1, 2)8,9,10. Nevertheless, because each of these authors classified their data, none of their research could include all of the variances. After a systematic review, Panagouli et al.11 established a new categorization encompassing all reported CT abnormalities (Table 3).
Table 1. Michels’ classification of variations of coeliac trunk (CT)8.

Table 2. Adachi’s Classification of variations of coeliac trunk9.

Table 3. Panagouli’s Classification of variations of coeliac trunk11.
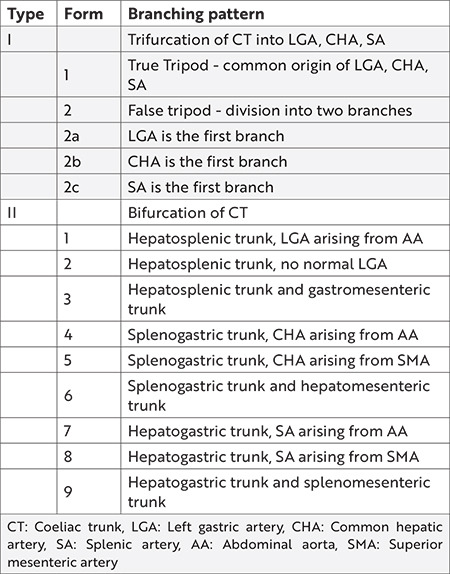
In case 1, there is normal trifurcation (true tripod; type 1, form one of Panagouli Classification) of CT. Instead of bifurcating, the PHA has four branches: Two going to the right lobe of the liver, one to the left lobe, and one as CA12. Ranaweera et al.12 documented four hepatic branches arising directly from the AA supplying the liver. It takes considerable understanding of the hepatic vascular pattern to ligate or embolize hepatic arteries to treat liver damage, tumors, and transplantation. To prevent unnecessary post-operative complications in upper abdominal procedures and liver transplants, these additional hepatic arteries should consistently be carefully recognized and considered9. After its origin from the right side of the PHA, CA ran toward the GB and crossed the common hepatic duct (CBD) anteriorly, which is a variant type of relation. Most often, the CA passes posterior to the CHD1. The development of laparoscopic cholecystectomy has rekindled interest in the architecture of the hepatic artery and bile duct13.
In the second case, there is a trifurcation of CT into LGA, HST, and an aberrant branch, which ultimately reaches the left triangular ligament of the liver, which has not been previously described in the literature. HST, which is divided into CHA and SA, had an ordinary course and distribution. However, LGA bifurcation into descending and ascending branches is not commonly reported in the literature. The superior branch from LGA supplied the liver by entering via PH and gave a branch to GB. In a study by Naidich et al.13, 2.8% of LGA arose directly from the AA and primarily supplied the liver with minor contributions to the stomach14. Gayretli et al.14 reported multiple variations of LGA, where LGA divides into three branches, one going to the liver, another to the stomach, and the last to the esophagus15. In another study, LGA resulted in an aberrant hepatic artery in the left lobe of the liver4. The presence of additional hepatic arteries has profound consequences for surgical interventions such as CBD explorations, laparoscopic cholecystectomy, Whipples’ operation, radical hepatic surgery, liver transplantation, and endovascular procedures in the liver, such as chemoembolization9. LGA variations are significant for perivascular lymphadenectomy. Another interesting point to note in this case is that a small branch arising from CT supplies the left triangular ligament. Gao and Roberts16 reported the presence of aberrant bile ducts in 80-89% of cadavers and rudimentary liver cells in 62-65% of cadavers within the left triangular ligament. We also observed an unusual variation in absent RGA in both cases. Although different origins of RGA from PHA, RHA, LHA, and CHA have been reported, absence of RGA has rarely been documented4.
With the folding of the embryo, the right and left vitelline plexus merge to generate several main arteries, which are anastomosed with the ventral surface of the dorsal aorta. A series of unpaired segmental and ventral splanchnic arteries developed at the end of the fourth week. Ventral longitudinal anastomosing channels link these arteries. Many ventral splanchnic branches vanish, and only three trunks-the celiac trunks, superior mesenteric artery, and inferior mesenteric artery-remain. Any modification to this longitudinal anastomosis may alter the branching pattern of CT3.
Acknowledgments
Our profound gratitude goes to the cadaver’s family for donating their loved one’s body for study.
Footnotes
Ethics
Informed Consent: All cadavers used in this study were donated to the department with written and informed consent for performing whole-body dissection for educational and research purposes.
Peer-review: Externally peer-reviewed.
Author Contributions
Concept: A.K., R.M., M.C., Design: A.K., R.M., M.C., Data Collection and/or Processing: A.K., R.M., M.C., Analysis and/or Interpretation: A.K., R.M., M.C., Literature Search: A.K., R.M., M.C., Writing: A.K., R.M., M.C.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The author declared that this study has received no financial support.
References
- 1.Tubbs RS. Posterior abdominal wall and retroperitoneum. In: Standring S, editor. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 42nd ed. China: Elsevier. 2021;. p.:1219–20. [Google Scholar]
- 2.Haller AV. Icones anatomicae in quibus aliquae partes corporis humani delineatae proponuntur et arteriaum potissimum historia continuter. Gottingen. 1756. [Google Scholar]
- 3.Tandler J. Uber die Varietaten der Arteia coeliaca and deren Ent wicklung. Anat. Hefte.1904;25:473–500. [Google Scholar]
- 4.Ariyanachi K, Ravindra Deshmukh V, Nagaraj S. The origin and formation of gastrosplenic trunk and the common hepatic artery: surgical and embryological basis: a case report. Int J Anat Res. 2018;6:5256–60. [Google Scholar]
- 5.Koshi R. Cunningham’s Manual of Practical Anatomy. Thorax and Abdomen. Oxford University Press. 2017. [Google Scholar]
- 6.Araujo Neto SA, Franca HA, de Mello Júnior CF, et al. Anatomical variations of the celiac trunk and hepatic arterial system: an analysis using multidetector computed tomography angiography. Radiol Bras. 2015;48:358–62. doi: 10.1590/0100-3984.2014.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lipshutz B. A composite study of the coeliac axis artery. Ann Surg. 1917;65:159–69. doi: 10.1097/00000658-191702000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Michels NA. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg. 1966;112:337–47. doi: 10.1016/0002-9610(66)90201-7. [DOI] [PubMed] [Google Scholar]
- 9.Adachi B. Das Arteriensystem der Japaner. Verlag der Kaiserlich - Japanischen Universitat zu Kyoto. 1928;. p.:18–71. [Google Scholar]
- 10.Rajini T, Mokhasi V, Geethanjali BS, Sivacharan PV, Shashirekha M. Coeliac trunk and its branches: anatomical variations and clinical implications. Singapore Med J. 2012;53:329–31. [PubMed] [Google Scholar]
- 11.Panagouli E, Venieratos D, Lolis E, Skandalakis P. Variations in the anatomy of the celiac trunk: A systematic review and clinical implications. Ann Anat. 2013;195:501–11. doi: 10.1016/j.aanat.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 12.Ranaweera L, Withana K, Weerasingha S. A rare morphological variation of the coeliac trunk in a Sri Lankan cadaver. Int J Complement Alt Med. 2020;13:215–7. [Google Scholar]
- 13.Naidich JB, Naidich TP, Sprayregen S, Hyman RA, Pudlowski RM, Stein HL. The origin of the left gastric artery. Radiology. 1978;126:623–6. doi: 10.1148/126.3.623. [DOI] [PubMed] [Google Scholar]
- 14.Gayretli Ö, Çetiner Kale A, Kocabıyık N, Ozan H, Yalçın B. Multivariations of the Left Gastric Artery: A Case Report. Balkan Med J. 2010;27:420–3. [Google Scholar]
- 15.Lippert H, Pabst R. Arterial variations in man: classification and frequency. In: Verlag JFB, editor. Munchen. 1985;. p.:71–3. [Google Scholar]
- 16.Gao XH, Roberts A. The left triangular ligament of the liver and the structures in its free edge (appendix fibrosa hepatis) in Chinese and Canadian cadavers. Am Surg. 1986;52:246–52. [PubMed] [Google Scholar]


