ABSTRACT
Acute gastroenteritis (AGE) caused by rotavirus (RV) remains a public health issue in China. To accelerate the mass rotavirus vaccination, it is important to inform the policy maker, and the public of the economic burden caused by rotavirus infection. A meta-analysis was conducted applying standardized algorithms. Articles published before January 1, 2023, in English and Chinese were searched through PubMed, CNKI, and WanFang Data. Studies with cost analysis of RV AGE were included. A random-effects model was applied to synthesize the total cost of RV AGE from the societal perspective. A prospective survey aimed to measure the cost of RV AGE was conducted in 2021 and 2022 in Shaoxing city, Zhejiang province, that can represent the developed region. The cost data was applied as deviation indicator, in comparison with the pooled estimate generated from meta-analysis. Totally 286 articles were identified, and eventually 12 studies were included. The pooled total social cost of RV AGE was US$282.1 (95%CI: US$213.4–350.7). The pooled private cost of RV AGE was US$206.4 (95%CI: US$155.2–257.5). RV AGE hospitalized and RV AGE incurred in developed regions caused remarkable higher burden (US$631.2 [95%CI: US$512.6–749.8], and US$333.6 [95%CI: US$234.1–433.2] respectively), compared to RV AGE treated at outpatient, and incurred in less developed regions. Our study demonstrates that RV AGE causes a significant economic burden in China. Given the promising effectiveness and highly cost-effective, introduction of rotavirus vaccines in national immunization programs could substantially reduce the economic burden in China.
KEYWORDS: Rotavirus, acute gastroenteritis, economic burden, China
Introduction
Acute gastroenteritis (AGE) caused by rotavirus remains a public health issue worldwide.1 Annually, rotavirus infection is estimated to cause 110 million children under the age of 5 suffer from diarrhea every year. Of these, around 25 and 2 million children require treatment in outpatient and ward respectively, and eventually lead to 350,000–590,000 deaths.2 Notabely, 82% of deaths incur in developing countries.3 In China, the annual incidence rate of AGE due to rotavirus infection is around 50 cases/1,000 children/year.4 Moreover, rotavirus is the most common etiology being responsible for moderate and severe diarrhea in children less than 5 years of age.5 Currently, there is no specific and effectious small molecular anti-viral agent, such as paxlovid for Covid-19, to treat rotavirus AGE, vaccine is the sole measure against rotavirus infection, and thus is recommended to be included in all national immunization programmes and considered a priority.6 According to China’s immunization program mechanism, rotavirus vaccines are classified as non-Expanded Program on Immunization (EPI) vaccines and are provided through the private market at a high out-of-pocket cost (280 RMB per dose, 3 doses for the full course). This has led to low national vaccine coverage, and there are potential disparities in vaccine uptake and health outcomes.7,8 So far, there has been limited research in China evaluating the cost-effectiveness of incorporating rotavirus vaccines into the immunization plan. Due to uncertainties in local parameters (vaccine efficacy, pricing, etc.) during the research and limited available data on rotavirus vaccine coverage in the current situation, this might have overestimated the cost-effectiveness of the immunization strategy. In Taiwan, rotavirus causes diseases of health insurance costs $1–30 million.9 Hong Kong statistics show that rotavirus causes disease. The social burden is $4.3 million, and the direct medical cost is $4 million, with each family bearing about $20US dollars.10 The article published by Wang11et al estimated that the average direct and indirect medical costs were $13.51 and $108.96 respectively. In 2004, statistics showed that there were 13 million cases of diarrhea symptoms caused by rotavirus infection in China. Among them, 2.5 million people received outpatient treatment at a cost of $9.49–$36.78 USD, while 230,000 people required hospitalization with costs ranging from $97.57 to $284.69 USD. The estimated average outpatient treatment cost for rotavirus across the nation was $14.83 USD per person, and the average hospitalization cost per person was $124.43 USD.12
It is further emphasized that introduction of rotavirus vaccine should be accompanied by measures to ensure high vaccination coverage and timely administration of each dose. Two rotavirus vaccines, namely RotaTeq and Lanzhou lamb rotavirus (LLR), were licensed in China many years ago. However, the coverage of full course is still surprisingly low, even in well-developed region, such as Shanghai.13 So far, there has been limited research in China evaluating the cost-effectiveness of incorporating rotavirus vaccines into the immunization plan. In order to promote the implementation of rotavirus vaccines in China, we believe that, it is important to inform the public of the disease burden caused by rotavirus infection, especially to make the public aware of the economic burden. To this end, we analyzed and synthesized the cost-of-illness (COI) including the direct costs of health care services for rotavirus-specific diarrhea, indirect costs, and intangible costs to the individual patients due to rotavirus infection in Chinese children employed a meta-analysis, adjusting by a prospective COI survey based on catchment design in Shaoxing, Zhejiang province.
Materials and methods
To estimate the incidence rate of rotavirus infection, clinical characteristics
and the COI due to rotavirus infection, population-based prospective surveillance was conducted in Shaoxing city. At the same time, we employ a meta-analysis to collect data about COI caused by rotavirus from previous study in China. There are two methods of data collection, meta-analysis and prospective study. In population-based prospective surveillance, we employ clinical characteristics and COI in 2021 and 2022 in Shaoxing city and verify whether the data aligns with the cost composition of rotavirus disease burden in previously economically developed regions. This set of data serves as a supplement for the previous rotavirus disease burden data from meta-analysis. As one of the sources of prospective screening in meta-literature, we merge the previously retrieved literature and conduct the meta-analysis again to explore RV COI in different patients and development regions.
Meta-analysis
Search strategy and selection criteria
Studies on the cost-of-illness of rotavirus infections in Chinese children (<5 years of age), published before January 1, 2023, were identified following PRISMA guidelines for systematic reviews.14 Scientific articles published in English and Chinese languages were sought through searching PubMed, China National Knowledge Internet (CNKI) and WanFang Data (A Chinese Literature Service platform). Standardized medical subject heading (MeSH) terms, rotavirus; disease burden; costs; cost analysis; cost-of-illness; and freeword “China,” were established for searching. Prior to the literature search, a pilot study was conducted to refine the MeSH terms and combinations thereof, especially when the terms were translated to Chinese.
Review strategy
Endnote® (version 20, Thomson, Inc., Philadelphia, U.S.A.) bibliographic software was used to create an electronic library of citations identified in the database searches, and duplicate records were deleted. All remaining duplications were eliminated manually during the following screening. Each study was assigned a unique identification code to enable tracking of reviews and analysis after title/abstract screening. Authors named XLF and ZL performed the title/abstract screening, full text screening, appraisal of quality, and thereafter data extraction independently. Inclusion criteria included: 1) studies reported from mainland China; 2) studies provided laboratory diagnosed RV infection; and 3) studies included children less than 5 years of age. Exclusion criteria included: 1) studies did not provide aggregatable data on direct medical costs, direct non-medical costs, and indirect costs; 2) studies did exclusively pertain to descriptive research and review, and did not provided extractable data on costs.
Prospective cost-of-illness survey based on catchment design
Shaoxing city locates in Zhejiang province, and composes of three districts, namely Yuecheng, Keqiao and Shangyu, and Yuecheng is the downtown possessing two major pediatric clinics in the city, namely Shaoxing People’s Hospital and Maternal and Child Health Hospital. A preliminary healthcare facility utilization survey was conducted to facilitate the catchment design, and it indicated around 80% infants living in Yuecheng district sought healthcare in these two hospitals when experiencing AGE. In this case, a catchment design based on these two hospitals was conducted in consecutive epidemic seasons (October through March) in 2021 and 2022. During the study period, children sought healthcare due to AGE in these two hospitals, and living in Yuecheng district were recruited after informed consenting, including patient treated in outpatient and inpatient. Demographic information, clinical manifestation, indirect costs, direct non-medical costs, as well as stool specimens were collected from each enrolled patient, while the direct medical costs was exported from Hospital Information System (HIS). Stool specimens was used for RV RT-PCR diagnosis.15 A rotavirus vaccination history of each enrolled patient was matched with EPI database in Shaoxing Center for Disease Control and Prevention (CDC), and a vaccinated patient was excluded from the COI analysis.
Definition
To facilitate identification of reports, a suspected case of RV AGE was defined as a child less than 5 years old who sought treatment to a healthcare facility. A confirmed case of RV AGE was defined as a child for whom rotavirus infection was proven by means of either an enzyme immunoassay, or a RT-PCR test performed on stool specimens. The estimated cost of a RV AGE episode includes the sum of direct medical, direct non-medical, and indirect costs.16 Direct medical costs included cost of consultation fees, hospitalization, laboratory tests, and medicines. Non-medical direct costs included costs on transportation, special foods and drinks, accommodation while receiving treatment. Indirect costs are defined as productivity loss due to illness.16 COI were estimated from two perspectives, social costs (total direct cost + total indirect cost) and private costs (0.5 × direct medical cost + direct non-medical cost + total indirect cost). Evidently, the insurance coverage ratio stood at 0.5, equivalent to half of the direct medical expenses. This amount was billed to the parents’ employers or the local Medical Insurance Bureau in accordance with the local health insurance policy.17 In this study, the patients were not of working age so productivity loss was calculated based on the work time loss of caregivers due to care-taking during the illness. The “human capital” approach18 was used for the calculation of productivity loss due to work absence.
Data extraction and analytical strategy
All case report forms (CRFs) derived from both systematic review study and prospective hospital-based COI survey were entered into a custom-made study data management systemdouble (EpiData version 3.1). Combined meta-analysis and prospective study data on the basis of patient type (inpatient or outpatient) and different economic region. For systematic review, considering the variance of COI caused by the economical level across different regions, the costs analysis was stratified by economic development level. According to statistics of the Gross Domestic Product (GDP) per capita in 2022,19 all provinces and regions in China were grouped into economically developed regions and economically less developed region in terms of the average GDP that was 85,698 Yuan. With regard to this cutoff value, the economically developed region included Beijing, Shanghai, Jiangsu, Fujian, Zhejiang, Tianjin, Guangdong, Inner Mongolia, Hubei, Chongqing, Shandong, while the economically less developed region included Shanxi, Anhui, Shanxi, Hunan, Jiangxi, Ningxia, Xinjiang, Liaoning, Sichuan, Hainan, Henan, Yunnan, Qinghai, Tibet, Hebei, Jilin, Guizhou, Guangxi, and Gansu. Due to inflation, the real purchasing power of currencies with equal values in different years varied widely, therefore, the average Consumer Price Index (CPI) between 2005 (the earliest publications included in the final analysis) and 2022 derived from the National Bureau of Statistics20 was employed to unify the costs for different years to the price level in 2022. Between 2003 and 2022, the average annual CPI in China was 2.49%. considering the large publication time span of the included literatures would lead to a substantial heterogeneity, the random-effects model was used to summarize the pooled costs, as well as 95% confidence intervals. In order to detect potential bias introduced by the heterogeneous quality of publications, if the proportion of high-quality articles (mean score per question ≥ 3.0) was less than two-thirds (~66%), then the pooled costs from all studies and high-quality articles (mean score per question ≥ 3.0) would be calculated and compared. If there was significant difference, outputs derived from high-quality articles would be presented.21
For catchment design study, the costs were measured from societal perspective. For societal perspective, all direct costs were measured as out-of-pocket expenditure of social. For indirect cost, an average wage of Chinese currency (Renminbi, RMB) 236 per day22 multiplied by number of days lost to estimate costs associated with lost productivity. To understand the potential impact factors of RV COI, a multiple linear regression model was employed, total costs were log10 transformed and regressed with independent variables, to compare with non-RV AGE, and demographic information, clinical manitestation, and therapy were included. We have checked the model assumptions by examining the normality, heteroscedasticity and multicollinearity. When the models were under these assumptions, the costs were retransformed to the original scales adjusted by a smearing factor.23
In addition, Shaoxing is one of the most economically developed cities in China, and it ranked 29th among cities in terms of GDP in 2022,24 and thus was applied as indicator of COI in well-developed region in 2022, in order to assess the reliability of those COIs coverted by average CPI in abovementioned meta-analysis.
All analyses were performed using STATA version 14.0 (Stata Corp, College Station, Texas, USA). Statistical significance was assessed using P < .05. All costs were analyzed from patient perspectidve, and reported in US$ using the exchange rate of 2022 [1 US$ = 7.18 Chinese RMB].25 This study was reviewed and approved by the Institutional Review Board of Institutes of Biomedical Sciences, Fudan University.
Results
Summary of studies
For meta-analysis, a total of 286 articles published were identified after systematically searching multiple data sources. After removing duplicates, 273 articles went through title/abstract, and full text screening, and eventually, 12 peer-reviewed articles were included in final analysis (Figure 1). Majority (66.7%) were published in Chinese, and 4 studies (33.3%) were published in English. Out of 12 studies, 10 (83.3%) articles are classified as high quality. More data (66.7%) were generated from economically developed region, such as Beijing, Shanghai, Jiangsu province, etc., four studies (33.3%) were reported from Gansu and Hebei province which belong to the economically less developed region.
Figure 1.
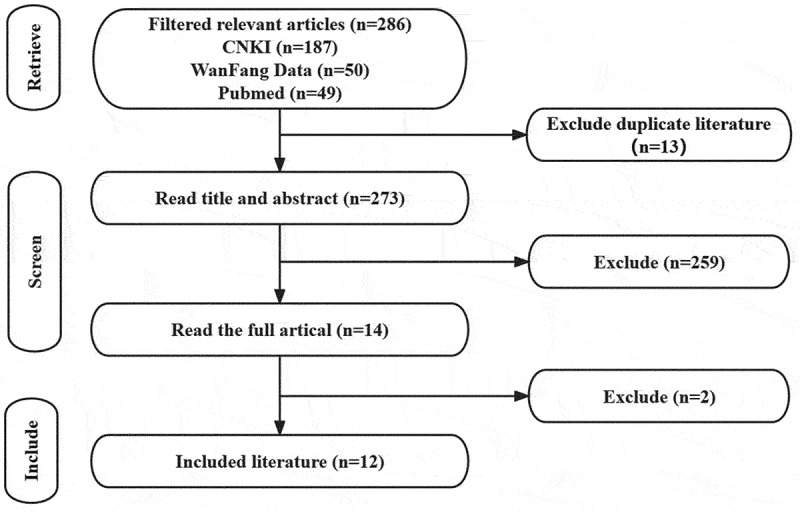
Study selection for inclusion in the meta-analysis.
For catchment design, 643 AGE patients were eventually enrolled during the epidemic season in 2021 and 2022. In total, 45 patients (7.0%; 95%CI:5.0%-9.0%) were identified as RV AGE, with 42 G8P[8] and 3 G1P[8] genotypes. The average age month was 15.0 and 15.3 for AGE and RV AGE respectively. Out of 643 AGE cases, 499 cases (77.6%) were treated at outpatient, and 144 cases (22.4%) treated as inpatient. 32 and 13 RV AGE cases were identified from outpatient and inpatient, resulted in a detection rate of 6.4% and 9.0% respectively (p > .05). The average month at onset was 14.9 months and 15.3 months for non-RV AGE, and RV AGE respectively (p = .41).
Significant difference on clinical manitestation of AGE was observed in RV AGE patients, in comparison with that of Non-RV AGE (Table 1). The Vesikari Score was 7.3 (95%CI: 6.2–8.5) and 6.2 (95%CI: 6.0–6.5) in RV AGE and Non-RV AGE patients respectively (p < .05). Particularly, the maximum episodes of vomiting in any 24 hours, and duration of vomiting were dramatically high in RV AGE patients, compared to Non-RV AGE patients (p < .05). Furthermore, more severe vomiting occurred in those hospitalized RV AGE patients, in addition, rehydration and the watery diarrhea became more common in hospitalized RV AGE patients, eventually, resulted in a average Vesikari Score of 12.0 (95%CI: 9.6–14.4) in hospitalized RV AGE patients.
Table 1.
Clinical manifestation of RV AGE and non-RV AGE.
| Clinical characteristic | RV | Non-RV | P-Value |
|---|---|---|---|
| Mean (95%CI) | Mean (95%CI) | ||
| n = 45 cases | n = 598 cases | ||
| Age (months) | 15.3 (11.7–18.9) | 14.9 (14.0–15.9) | .41 |
| Maximum number of stools per day; n (%) | 4.5 (3.9–5.2) | 4.7 (4.5–4.9) | .32 |
| Duration of diarrhea (days) | 3.7 (2.9–4.6) | 3.8 (3.4–4.2) | .44 |
| Duration of vomiting (days) | 0.9 (0.4–1.4) | 0.4 (0.3–0.5) | <.05 |
| Maximum number of vomiting episodes per day; n (%) | 1.7 (0.8–2.7) | 0.7 (0.6–0.9) | <.05 |
| Temperature (℃) | 37.1 (36.9–37.3) | 37.1 (36.9–37.3) | .41 |
| Rehydration; n (%) | 33.3 (15/45) | 19.6 (117/598) | <.05 |
| Water stool proportion | 62.2 (28/45) | 49.3 (295/598) | <.05 |
| Vesikari scale | 7.3 (6.2–8.5) | 6.2 (6.0–6.5) | <.05 |
Cost analysis
For Shaoxing prospective survey, overall, the social costs due to RV AGE and non-RV AGE were US$219.0 (95%CI: US$173.4–264.6) and US$ 131.9 (95%CI: US$122.6–140.9) respectively, a significant difference on the costs between RV AGE and non-RV AGE was observed (p < .05). Moreover, for those hospitalized RV AGE cases, a significant higher social cost was calculated, which was US$649.9 (95%CI: US$599.7–700.1), compared to the costs of RV AGE cases treated at outpatient (US$51.3; 95%CI: US$41.8–60.9) (p < .05). In the composition of total social costs, direct costs accounted for over 60%. Private need to undertake more than 70% of total social costs. In addition, among the direct costs, direct medical costs contributed the most, especially for those hospitalized RV AGE, which reached 77.7%. Multiple linear regression analysis indicated that, the significant impact factors on the total cost included hospitalization, presentation with vomiting, and RV AGE (Table 2).
Table 2.
Potential predictor variables included in the multiple regression analysis.
| Variables | Costs of illness |
||||
|---|---|---|---|---|---|
| B | β | t | P-Value | OR | |
| Constant | 339.112 | 5.150 | <.001 | ||
| Age | −6.733 | −0.048 | −2.283 | .023 | 0.953 |
| Hospitalization | 3326.709 | 0.843 | 33.557 | <.001 | 2.323 |
| Rehydration | 71.306 | 0.017 | 0.666 | .506 | 1.017 |
| Diarrhea duration | −3.049 | −0.008 | −0.398 | .691 | 0.992 |
| Vomiting | 85.808 | 0.022 | 0.968 | .334 | 1.022 |
| Adjusted R2 | 0.778 | ||||
After converting the costs reported in literatures to the costs under purchasing power in 2022 using CPI, in terms of meta-analysis, cost summarized from economically developed regions indicated that, the total social cost was US$272.6 (95%CI: 206.5–338.8). Of these, direct medical cost and indirect cost were US$146.5 and US$89.9 with a ratio of 53.7% and 33.0% respectively. Direct medical cost account for 80.2% of direct cost. Whereas, based on the Shaoxing prospective survey, the total social cost was US$219.0 (95%CI: 173.4–264.6). The direct medical cost and indirect cost were US$98.9 and US$84.1 with a ratio of 45.2% and 38.4% respectively. Again, the direct medical cost account for 73.3% of direct cost. Moreover, when cost data were stratified by outpatient/inpatient, similar proportions of direct and indirect, direct medical and direct non-medical was measured between Shaoxing prospective survey and developed regions in meta-analysis (Table 3). Thereafter, cost data derived from Shaoxing prospective survey and meta-analysis were merged to quantity the cost-of-illness due to RV AGE.
Table 3.
Comparison on the composition of costs due to RV AGE derived from Shaoxing prospective survey and developed regions in meta-analysis.
| Cost (US $) | Outpatient |
Inpatient |
||||||
|---|---|---|---|---|---|---|---|---|
| Shaoxing prospective survey | Percentage | Meta-analysisx (developed regions) | Percentage | Shaoxing prospective survey | Percentsage | Meta-analys is (developed regions) | Percentage | |
| n = 32 cases | (%) | n = 2630 cases | (%) | n = 13 cases | (%) | n = 1542 cases | (%) | |
| Direct costs (Mean, 95%CI) | 27.8 (24.0–31.7) | 54.2% | 42.1 (34.9–49.3) | 50.5% | 451.7 (422.3–481.0) | 69.5% | 452.2 (371.1–533.2) | 66.4% |
| Direct medical costs (Mean, 95%CI) | 17.0 (14.8–19.0) | 61.0% | 23.9 (20.4–27.5) | 57.0% | 350.8 (330.1–371.6) | 77.7% | 353.6 (303.5–403.7) | 73.1% |
| Direct non-medical costs (Mean, 95%CI) | 10.8 (8.5–13.2) | 39.0% | 18.0 (11.5–24.4) | 43.0% | 100.8 (82.6–119.0) | 22.3% | 123.3 (92.0–154.6) | 26.9% |
| Indirect costs (Mean, 95%CI) | 23.5 (17.1–29.9) | 45.8% | 41.2 (31.0–51.4) | 49.5% | 198.3 (166.2–230.4) | 30.5% | 223.0 (158.1–287.9) | 33.6% |
| Total social costs (Mean, 95%CI) | 51.3 (41.8–60.9) | 100% | 83.3 (66.5–100.1) | 100% | 649.9 (599.7–700.1) | 100% | 630.6 (491.8–769.5) | 100% |
| Total private costs (Mean, 95%CI) | 42.8 (25.7–60.0) | 83.4% | 71.3 (55.3–87.4) | 85.6% | 474.5 (384.2–564.8) | 73.0% | 453.8 (336.6–571.1) | 72.0% |
*Data are reflected as mean (95%CI) using US$ as measurements unit. The currency exchange rate is 1US $ to 7.18 RMB.
#The percentages of direct and indirect costs in total costs were calculated, as well as the percentages of direct medical costs and direct non-medical costs in direct costs.
According to the per capita GDP in 2022, overall, the pooled total cost from the social’s perspective was US$282.1 (95%CI: 213.4–350.7) and the pooled total cost from the private perspective was US$206.4 (95%CI: 155.2–257.5). Direct medical cost and direct non-medical cost from a societal perspective were US$151.4 and US$50.8 respectively. The indirect cost of societal perspective was US$99.3. Compared to RV AGE treated at outpatient room, hospitalization incurred 7–fold higher social cost, and the overall increase was more attributed to increase of direct cost (~10–fold), especially the increase of direct medical costs (12.3–fold) (Table 4). Compared to the costs of RV AGE between developed regions and less developed regions, significant differences are observed in general expenses in the range of outpatient, inpatients and total patients. Compared to the social costs of RV AGE (US$148.1; 95%CI: US$96.1–200.0) derived from less developed regions, the cost of RV AGE (US$333.6; 95%CI: US$234.1–433.2) was double from developed regions (p < .05) and the overall increase was more attributed to increase of direct cost (~2.3–fold), especially the increase of direct non-medical costs (7–fold). Similar pattern was observed between the costs in developed regions and less developed regions when the costs of RV AGE were further stratified by inpatient and outpatient (Figure 2).
Table 4.
Pooled costs due to RV AGE treated at outpatient and inpatient.
| Cost (US $) | Outpatient | Inpatient | Total |
|---|---|---|---|
| n = 3328 cases | n = 2757 cases | n = 6085 cases | |
| Direct costs (Mean, 95%CI) | 38.7 (32.8–44.6) | 387.7 (315,9–459.5) | 193.8 (144.5–243.1) |
| Direct medical costs (Mean, 95%CI) | 25.1 (21.4–28.9) | 309.2 (263.0–355.5) | 151.4 (112.2–190.6) |
| Direct non-medical costs (Mean, 95%CI) | 16.8 (12.2–21.4) | 89.7 (62.2–117.1) | 50.8 (35.8–65.8) |
| Indirect costs (Mean, 95%CI) | 38.3 (31.4–45.2) | 117.8 (126.8–228.8) | 99.3 (73.4–125.3) |
| Total social costs (Mean, 95%CI) | 73.2 (6.3–86.1) | 543.2 (426.8–659.7) | 282.1 (213.4–350.7) |
| Total private costs (Mean, 95%CI) | 6.6 (48.6–72.6) | 388.6 (292.6–484.7) | 206.4 (155.2–257.5) |
Data are reflected as mean (95%CI) using US$ as measurements unit. The currency exchange rate is 1US $ to 7.18 RMB.
Figure 2.
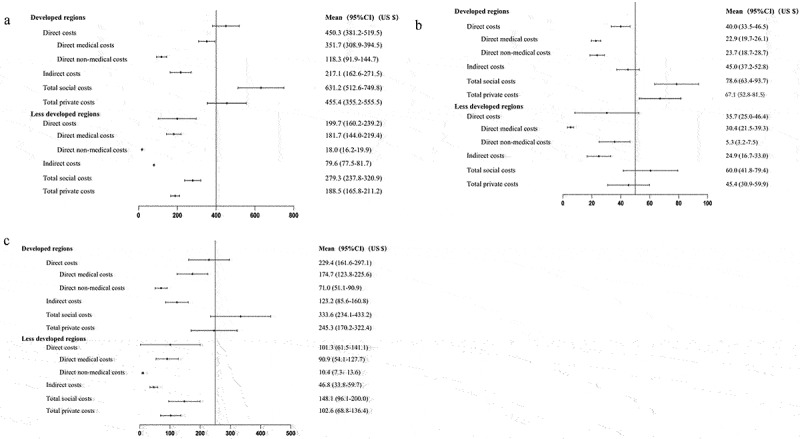
Analysis of the cost of illness by GPD per capita.
A: Inpatient B: Outpatient C: Total.
With an average of 79.29 million births occurring during the 5–year period of 2017–2022 (17.23 million births in 2017, 15.23million births in 2018, 14.65 million births in 2019,12.00 million births in 2020, 1062 million births in 2021, 9.56 million births in 2022). RV detection rate in hospitalized diarrhea among U5 children (34.0%) from a systematic review.26 The corresponding estimates for the annual social costs and the annual private expenditure are US $76.05 billion (79.29 million × 34.0% × US $282.1) and US $55.64 billion (79.29 million × 34.0% × US $206.4) respectively.
Discussion
Globally, rotavirus was the leading cause of severe, dehydrating diarrhea in children aged <5 years, and infected nearly every child by the age of 3–5 years, resulting in an estimated 215 000 (range, 197 000–233 000) childhood deaths in 2013,27 accompanied by considerable economic burden.28 Similar disease burden due to RV AGE in China was summarized,4,29 while the estimate of economic burden was sparse. We had measured the burden of RV AGE in rural northern China using population-based surveillance, resulted in an overall incidence rate of 61.4 cases per 1000 children per year, accompanied by a total cost of US$49 (95%CI: US$22.10–US$38.00) from the societal perspective.3 Another study conducted in eastern China estimated that, on average, the total cost ranged from US $54.64 for outpatients to US $454.24 for inpatients when children suffered from rotavirus infection.17 Since a diversity of economic level existed among regions, the cost-of-illness varied widely over China. To advocate RV vaccines being included into national immunization program, the current estimates derived from the abovementioned individual studies could not satisfy the policy maker, a average estimate on national level, as well as estimates stratified by economic zone is desirable. Therefore, we synthesized the national economic burden caused by RV AGE which was US$206.4 (95%CI: US$155.2–257.5) in 2022 from the societal perspective. In terms of national annual statistics in 2022, the per capita disposable income (PCDI) was US$5136.9,30 thus, the expenditure of treatment for RV infection accounted for 4.7% of PCDI. Moreover, when looking at the composition of PCDI, the per capita healthcare consumption expenditure was only US$295.3, accounted for 5.7% of PCDI.30 In another word, the total cost of RV AGE almost equaled to per capita healthcare consumption expenditure. Therefore, the significant importance of the economic burden caused by RV AGE was undoubtedly demonstrated. Up to date, specific antiviral therapy is not available against rotaviruses. Rotavirus vaccines provide a crucial means for effectively preventing rotavirus infections. Wang31et al estimated that including Rotateq in the NIP was projected to prevent 348 million RVGE cases (62.6% reduction) and 4251 deaths (72.6% reduction) compared to the status quo. Rotarix through the NIP would prevent 48.7% of cases and LLR would avert 20.3% of cases. In uncertainty analyses, the reduction of vaccine prices and the incorporation of herd immunity further improved the cost- effectiveness of the NIPs, especially Rotateq or Rotarix.
The global impact of RV vaccine is evident from the 40% reduction in RV infection following the introduction, and highly cost-effective or even cost-saving was measured in most low- and middle-income countries when compared to no vaccination.3,6
The number of past studies on the disease burden caused by rotavirus diarrhea based on population data obtained through literature searches is very limited, and all studies were conducted before 2016. The relevance of these studies to the current situation has been influenced by various factors. Our study was conducted in 2021 and focused on Shaoxing City, which had not previously been studied for rotavirus disease burden, as a representative case. We aimed to explore the current disease burden caused by rotavirus diarrhea and expand and supplement the disease burden information of provinces and cities nationwide. From the perspective of the cost composition of disease burden, considering the time value of money, we conducted a meta-analysis that systematically integrated data from both hospitalized and outpatient rotavirus patients in regions with different levels of economic development. It can be concluded that the economic situation of a region has a significant impact on the disease burden caused by rotavirus, and this is an important factor to consider in the process of widespread vaccination against rotavirus.
Two impact factors on the cost of RV AGE were detected. Firstly, after stratifying by economic zone, the total cost was US$245.3 (95%CI: US$170.2–322.4) and US$102.6 (95%CI: US$68.8–136.4) incurred in developed and less developed region respectively. Undoubtedly, the cost of RV AGE is directly associated with the economic level of the region that the patient coming from. Two reasons might be responsible for such a significant gap between developed and less developed regions. In one hand, PCDI affected patients’ ability to pay. In terms of national annual statistics in 2022, the PCDI was US$6549.9 and US$4150.8 in developed and less developed regions respectively.30 This payment ability was reflected in the composition of the total cost. Compared to developed region, more reduction on direct non-medical and indirect cost were observed, rather than reduction on direct medical in less developed region. In another hand, regional variance on medical service prices might also affect the cost-of-illness. Published studies indicated that a significant higher price was founded in developed region.32,33 For instance, the cost of laparoscopic cholecystectomy performed in tertiary hospital was US$1665.8 and US$1068.7 in Shanghai and Kunming respectively, while, the gap of cost came from surgical service fees.34 Secondly, another impact factor on cost-of-illness was clinical manitestation. Compared to dehydration, the duration of diarrhea and vomiting made significant contribution to the total cost of RV AGE, while in typical cases, following an incubation period of 1–3 days, the onset of disease is abrupt, with fever and vomiting followed by watery diarrhea.6
Our study has couple of limitations. First, only 12 studies included in the final synthesis, which covered 9 (26.5%) provinces/municipalities. Of these, four studies came from less developed region. Findings regarding the economic burden of RV AGE might not be a ideal representative for total 34 provinces/municipalities over China. Nevertheless, compared to the estimate generated from individual study, the pooled cost-of-illness is unlikely to bring any systematic error that might result in a directional bias. Second, using CPI to correct inflation may result in data distortion, as CPI data is obtained through sampling surveys and the measurement range is too small. In addition, the selection of elements (a fixed basket of products) and element weights during CPI calculation can not be updated in a real-time manner, which may also lead to a deviation. Therefore, we used the cost derived from the prospective survey conducted in Shaoxing city that can represent the developed region as deviation indicator, in comparison with the pooled estimate generated from meta-analysis, and did not detect notable difference, in terms of the percentages and range of costs between components of total cost. In our study, the detection rate of rotavirus in this study was 6.9%, significantly lower than the rates reported in previous years. Amidst improving medical conditions and the continuous rise in rotavirus vaccination rates, the uncontrolled spread of the novel coronavirus may interfere with the occurrence of rotavirus during the peak season. Because of the global spread of the COVID-19 pandemic, which influenced the circulation of rotavirus during the winter season. To curb the transmission of COVID-19, reduced outdoor gatherings and effective protective measures may have further slowed down the spread of rotavirus during the peak season. Research from the Jading District Disease Control Center in Shanghai35 showed that COVID-19 prevention and control measures have affected the incidence rates of different legally notifiable infectious diseases in Jading District. In 2020, the incidence rate of infectious diseases transmitted through the fecal-oral route was 10.27%, while in 2021, it was 15.64%. The average incidence rate from 2017 to 2019 was 25.21%, which is significantly different from the incidence rate during the pandemic period (p < .001).
In conclusion, our study demonstrates that RV AGE is not only associated with substantial infection among children less than five years of age, but also causes a significant economic burden in China. Given the promising effectiveness and highly cost-effective of rotavirus vaccine immunization demonstrated in those countries with mass immunization in infants, introduction of rotavirus vaccines in national immunization programs could substantially reduce the economic burden in China.
Acknowledgments
Supported in part by a research grant from Investigator-Initiated Studies Program of MSD. The opinions expressed in this paper are those of the authors and do not necessarily represent those of MSD.
We thank Shaoxing Institute of Infection Disease for specimens and questionnaire collection
Funding Statement
This work was funded by MSD R&D (CHINA) CO., LTD.
References
- 1.LeClair CE, McConnell KA. Rotavirus. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. PMID: 32644377. [PubMed] [Google Scholar]
- 2.Parashar UD, Hummelman EG, Bresee JS, Miller MA, Glass RI.. Global illness and deaths caused by rotavirus disease in children. Emerg Infect Dis. 2003. May;9(5):565–8. doi: 10.3201/eid0905.020562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang XY, Riewpaiboon A, von Seidlein L, Chen XB, Kilgore PE, Ma JC, Qi SX, Zhang ZY, Hao ZY, Chen JC, et al. Potential cost-effectiveness of a rotavirus immunization program in rural China. Clin Infect Dis. 2009. Oct 15;49(8):1202–10. doi: 10.1086/605632. [DOI] [PubMed] [Google Scholar]
- 4.Wang JX, Zhou HL, Mo ZJ, Wang SM, Hao ZY, Li Y, Zhen SS, Zhang CJ, Zhang XJ, Ma JC, et al. Burden of viral gastroenteritis in children living in rural China: population-based surveillance. Int J Infect Dis. 2020. Jan;90:151–60. doi: 10.1016/j.ijid.2019.10.029. [DOI] [PubMed] [Google Scholar]
- 5.Zhou HL, Bessey T, Wang SM, Mo ZJ, Barclay L, Wang JX, Zhang CJ, Ma JC, Qiu C, Zhao G, et al. Burden and etiology of moderate and severe diarrhea in children less than 5 years of age living in north and south of China: prospective, population-based surveillance. Gut Pathog. 2021. May 24;13(1):33. doi: 10.1186/s13099-021-00428-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO . Rotavirus vaccines: WHO position paper – July 2021. 16 JULY 2021, 96th YEAR. No 28, 2021, 96, 301–320.
- 7.Zheng Y, Rodewald L, Yang J, Qin Y, Pang M, Feng L, Yu H. The landscape of vaccines in China: history, classification, supply, and price. BMC Infect Dis. 2018;18(1). doi: 10.1186/s12879-018-3422-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Y, Yue C, Li Y, Wang Y, Li S-L, Jiang X-Y. Analysis of vaccination situation of orial live attenuated rotavirus vaccine (LLR strain) among children in 6 provinces of China. Chin J Prev Med. 2018;52(3):282–6. doi: 10.4103/0366-6999.223851. [DOI] [PubMed] [Google Scholar]
- 9.Kilpatrick AM, Kramer LD, Campbell SR, Alleyne EO, Dobson AP, Daszak P. West Nile virus risk assessment and the bridge vector paradigm. Emerg Infect Dis. 2005. Mar;11(3):425–9. doi: 10.3201/eid1103.040364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mostashari F, Kulldorff M, Hartman JJ, Miller JR, Kulasekera V. Dead bird clusters as an early warning system for West Nile virus activity. Emerg Infect Dis. 2003;9(6):64 1–6. doi: 10.3201/eid0906.020794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang B, Fang ZY, Gao Q, Zhang LJ, Wu QB, Sun LW. The study of diseaseburden on rotavirus diarrhea in China. Chin J Vaccines Immun. 2005;11(Supp l):15–17. [Google Scholar]
- 12.Klee AL, Maid B, Edwin B, Poshni I, Mostashari F, Fine A, Layton M, Nash D. Long-term prognosis for clinical West Nile virus infection. Emerg Lnfect Dis. 2004;10(8):1405–11. doi: 10.3201/eid1008.030879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu J, Guan BC, Zhang LP, Mei KW, Lu XY, Lu YH. Rotavirus vaccination rate of children in the birth cohort in Minhang District, Shanghai, 2013-2020. Chin J Vaccines Immun. 2021;27:695–9. [Google Scholar]
- 14.Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021. Mar 29;372:n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gentsch J, Gray J, Iturriza Gómara M, et al. Manual of rotavirus detection and characterization methods. S Afr Med J= Suid-Afrikaansetydskrif vir geneeskunde. 2009;46(7):245-6. doi: 10.1007/BF02790641. [DOI] [Google Scholar]
- 16.World Health Organization (WHO) . Generic protocols (i) hospital- based surveillance to estimate the burden of rotavirus gastroenteritis in children and (ii) a community-based survey on utilization of health care services for gastroenteritis in children. 2002. [accessed 2004 Jan 5]. http://www.path.org/vaccineresources/details.php?ip513.
- 17.Jin H, Wang B, Fang Z, Duan Z, Gao Q, Liu N, Zhang L, Qian Y, Gong S, Zhu Q, et al. Hospital-based study of the economic burden associated with rotavirus diarrhea in eastern China. Vaccine. 2011. Oct 13;29(44):7801–6. doi: 10.1016/j.vaccine.2011.07.104. [DOI] [PubMed] [Google Scholar]
- 18.Kobelt G. Health economics: an introduction to economic evaluation. 2nd. London: Office of Health Economics; 2002. [Google Scholar]
- 19.National Bureau of Statistics . China statistical yearbook[M]. Beijing: China Statistics Press; 2023. [Google Scholar]
- 20.National Bureau of Statistics . Consumer price index[EB/OL]. National Bureau of Statistics; 2023. https://data.stats.gov.cn/ks.htm?cn=C01. [Google Scholar]
- 21.Zhou HL. Molecular epidemiology and variation of Norovirus[D]. Shanghai: Fudan university; 2021. [Google Scholar]
- 22.Shaoxing Municipal People’s Government . 2022 Shaoxing statistical yearbook [M]. Beijing: China Statistics Press; 2023. [Google Scholar]
- 23.Duan N. Smearing estimate: a nonparametric retransformation method. J Am Stat Assoc. 1983;78(383):605–10. doi: 10.1080/01621459.1983.10478017. [DOI] [Google Scholar]
- 24.Zhengzhou Municipal People’s Government . “The 2022 China’s top 100 cities was released” [EB/OL]. Zhengzhou Municipal People’s Government; 2023. https://www.henan.gov.cn/2022/07-04/2480244.html. [Google Scholar]
- 25.State Administration of Foreign Exchange . “The mid-rate of the RMB exchange rate” [EB/OL]. State Administration of Foreign Exchange; 2023. https://www.safe.gov.cn/safe/rmbhlzjj/index.html. [Google Scholar]
- 26.Li J, Wang H, Li D, Zhang Q, Liu N. Infection status and circulating strains of rotaviruses in Chinese children younger than 5-years old from 2011 to 2018: systematic review and meta-analysis. Hum Vaccin Immunother. 2021;17(6):1811–17. doi: 10.1080/21645515.2020.1849519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tate JE, Burton AH, Boschi-Pinto C, Parashar UD, World Health Organization–Coordinated Global Rotavirus Surveillance Network . Global, regional, and national estimates of rotavirus mortality in children <5 years of age, 2000-2013. Clin Infect Dis. 2016. May 1;62(Suppl 2):S96–S105. doi: 10.1093/cid/civ1013. [DOI] [PubMed] [Google Scholar]
- 28.Kawai K, O’Brien MA, Goveia MG, Mast TC, El Khoury AC. Burden of rotavirus gastroenteritis and distribution of rotavirus strains in asia: a systematic review. Vaccine. 2012. Feb 8;30(7):1244–54. doi: 10.1016/j.vaccine.2011.12.092. [DOI] [PubMed] [Google Scholar]
- 29.Zhang J, Duan Z, Payne DC, Yen C, Pan X, Chang Z, Liu N, Ye J, Ren X, Tate JE, et al. Rotavirus-specific and overall diarrhea mortality in Chinese children younger than 5 years: 2003 to 2012. Pediatr Infect Dis J. 2015. Oct;34(10):e233–7. doi: 10.1097/INF.0000000000000799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Bureau of Statistics . Household income and consumption expenditure in 2022[EB/OL]. National Bureau of Statistics; 2023. http://www.stats.gov.cn/sj/zxfb/202302/t20230203_1901715.html. [Google Scholar]
- 31.Wang J, Zhang H, Zhang H, Fang H. Public health impact and cost-effectiveness of rotavirus vaccination in China: comparison between private market provision and national immunization programs. Hum Vaccin Immunother. 2022. Dec 30;18(7):2090162. doi: 10.1080/21645515.2022.2090162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang C, Jiang H, Song XG, Jx OU, Xu ZY, Huang GC, Yao YT, Zhang YN. Research on regional price comparison relationship of medical service projects. Soft Sci Health. 2021;35:41–4. [Google Scholar]
- 33.Tang QM, Xiang L . Influencing factors and regional differences in Chinese residents’ healthcare expenditure. J Financ Rev. 2014;(01):85–98 . [Google Scholar]
- 34.Ye HM, Ling J, Wen J, Teng HF. Comparison of medical costs of laparoscopic cholecystectomy in eastern and western hospitals. Hosp Adm J Chin People’s Liberation Army. 2016;23(7):660–2. [Google Scholar]
- 35.Zhu YF, Zhang SZ, Duan CM. The impact of the prevention and control measures of the novel coronavirus pneumonia epidemic on the incidence of statutory infectious diseases in Jiading District, Shanghai. Dis Surveillance. 2023;38:181–4. [Google Scholar]


