ABSTRACT
Human papillomavirus (HPV) has a great impact on world health. Vaccination is among the most important methods of preventing HPV infection. This study investigated Chinese male college students’ knowledge of, attitude toward, and acceptance of the 9vHPV vaccine and the independent predictors. An online cross-sectional study was conducted among male college students at Chinese colleges and universities from March 12 to March 23, 2022. Based on a literature review of similar studies, a self-questionnaire was designed to investigate the students’ knowledge of, attitude toward, and acceptance of the 9vHPV vaccine. Multivariate logistic regression analysis was performed to identify factors influencing their willingness to be vaccinated. In addition, the structural equation model was constructed. A total of 1,547 male college students completed the survey. Of all the students, 54.95% were unwilling to receive a 9vHPV vaccination, while only 45.05% expressed willingness. Multivariate logistic regression analysis revealed that the male college students willing to receive the vaccine included medical students, those in a romantic relationship, those whose relatives and friends had cervical cancer, those whose relatives and friends had received the 9vHPV vaccine, those supportive of promoting the vaccine for men, and those who would recommend the vaccine to their relatives and friends. Male college students exhibited high hesitancy toward the 9vHPV vaccine. Acceptance of the 9vHPV vaccine by male college students can be improved by deepening their accurate understanding of the vaccine and enhancing their positive attitude toward it.
KEYWORDS: Human papillomavirus, acceptance, knowledge, attitude, vaccine, survey
Background
There are over 200 types of human papillomavirus (HPV).1 Genital HPV types have been subdivided into low-risk types, which are found mainly in genital warts, and high-risk types, which are frequently associated with invasive cervical cancer.2 HPV is considered a crucial pathogenic factor in cervical cancer, and more than 600,000 new cervical cancer cases globally are attributable to HPV infections each year.3,4 HPV is not only associated with cervical cancer, vulvar cancer, and vaginal cancer, but it is the primary cause of head and neck cancer, anal cancer, oral cancer, and penile cancer.2,5–8 Thus, men are also at risk for HPV infection, and HPV vaccination can be considered a crucial protective measure against this risk. The three-dose, 9-valent HPV (9vHPV) vaccination schedule can avoid 90% of cervical cancer and other HPV-related cancers and precancerous lesions.4,9
China has been vigorously promoting the HPV vaccine among women. Many colleges and universities have also started providing the 9vHPV vaccine for free.10 However, the risks of HPV infection and diseases associated with sexual behavior also impose huge disease burdens on men. Therefore, incorporating men into the preventive HPV vaccination program should help to effectively prevent HPV-related diseases in men and significantly reduce disease burdens on women.11 In addition, cost-benefit studies have shown that vaccination for both men and women is more cost-effective than that for women alone.12
On April 28, 2018, the National Medical Products Administration conditionally approved the marketing of the 9vHPV vaccine for cervical cancer prevention. HPV vaccine hesitancy has become an emerging global problem.13 Studies have been published on Chinese female college students’ attitudes toward and acceptance of the HPV vaccine. In a study conducted in eastern, central, and western China from April to September 2019, 11% of the female college students had been vaccinated, and 53.5% of the unvaccinated female students were willing to be vaccinated.14 In a cross-sectional survey of 3,867 female students from seven colleges and universities in mainland China, which was conducted from February 21 to April 30, 2020, 102 (2.64%) of the female students had received the HPV vaccine, and 32.08% of the unvaccinated female students were willing to be vaccinated in the next six months.15 A China (Fujian)-based study conducted from 2019, May 13 to 24, reported that 55.2% of female college students were willing to be vaccinated with the HPV vaccine.16 In 2012, a report based in China, Hunan, found that 44% of female undergraduates were willing to be vaccinated in the future.17 However, relevant data on the willingness of Chinese male college students to receive the HPV vaccine are lacking. Therefore, understanding Chinese male college students’ willingness to be vaccinated with the 9vHPV vaccine and the underlying reasons are important for the promotion of this vaccine in China. In this context, we conducted a cross-sectional study online to investigate Chinese male college students’ knowledge of, attitude toward, and acceptance of the 9vHPV vaccine and to identify the factors influencing male college students’ willingness to be vaccinated with the vaccine.
Methods and materials
Research design and respondents
An online questionnaire survey was conducted at several colleges and universities in China from March 12 to March 23, 2022. Copies of the electronic questionnaire were distributed and recovered through the Questionnaire Star (https://www.wjx.cn/) platform, and relevant data were exported. Male college students were invited to participate in the survey.
Ethical approval
This study was approved by the Medical Ethics Committee, Chaohu Hospital of Anhui Medical University (KYXM-202207-005). All respondents were informed of the study purpose, procedure, and their relevant rights. They were also informed that their personal identity or information would not be disclosed. Oral informed consent was obtained from each respondent before distribution of the questionnaire.
Questionnaire survey
This questionnaire mainly assessed Chinese male college students’ knowledge of, attitude toward, and acceptance of the 9vHPV vaccine. The questionnaire was prepared in Chinese and was designed with improvements based on a literature review of similar studies.18–22 Before large-scale distribution, the questionnaire was sent to 30 respondents as a pilot test, aiming to assess their vaccination willingness. In the pilot study, a total of 30 offline respondents were invited to complete the questionnaire, which took an average of 3.5 minutes. After completing the questionnaire, we interviewed each respondent and asked them about possible problems with the questionnaire. Each respondent discussed the questions in the questionnaire one by one. These interviews took an average of 7.5 min. We found no substantive problems and only modified the description of one problem through the pilot study.
The questionnaire was mainly composed of four parts: (1) Basic information on the respondents: Demographic characteristics (residence, college grade, body mass index, current smoking status, and current drinking status) and basic personal information (whether the respondent was a medical student or in a romantic relationship, whether relatives and friends had cervical cancer, and whether relatives and friends had been vaccinated with the 9vHPV vaccine). (2) Respondents’ knowledge of and attitude toward HPV and the 9vHPV vaccine. The respondents were asked to answer the following questions with “yes” or “no”: “HPV can cause genital warts and certain cancers,” “HPV can only be transmitted through sexual behavior,” “Men can’t be infected with HPV,” “9-valent HPV vaccination can effectively prevent HPV-related cancers,” The best age for receiving 9-valent HPV vaccine is before 26 years old,” Are you in support of promoting the 9-valent HPV vaccine for men?” “Do you think the authorized 9-valent HPV vaccine is safe? “Do you think the 9-valent HPV vaccine could have unexpected side effects?” “Do you think the authorized 9-valent HPV vaccine is effective?” “Would you recommend that your family and friends receive the 9-valent HPV vaccine?”(3) Respondents’ willingness to be vaccinated with the 9vHPV vaccine: whether they were willing to be vaccinated, and the reasons for their willingness or unwillingness.
Sample size estimation
The proportion of men intending to receive the HPV vaccine was assumed to be 48.9% in the calculation of sample size, based on a previous report in Saudi Arabia.23 The sample size was calculated as follows:
where n was the minimum number of respondents required, Z2 was (1.96)2 relative to the 95% confidence interval (CI), P was the prevalence rate estimated in the previous study, and e was the required accuracy (4%). The estimated non-response rate for the present study was 5%, and the minimum sample size was 630.
Data analysis
Data analysis was performed using SPSS version 21.0 (Chicago, IL, USA). The responses of the students to the questionnaire were considered classified data and expressed as numbers and percentages. Univariate analysis was performed to assess the relationships between independent variables (respondents’ basic information, their understanding of HPV and the 9vHPV vaccine, and their attitude toward the vaccine) and the dependent variable (respondents’ willingness to be vaccinated with the 9vHPV vaccine). Variables with a p-value of < .05 in univariate analysis (12 variables) and all variables were further analyzed by multivariate logistic regression to identify independent predictors influencing the willingness of the male college students to be vaccinated. Odds ratio (OR) and 95% CI were used to describe these variables. p < .05 was considered statistically significant. In addition, a structural equation model was used to analyze demographic characteristics and basic information that affect knowledge and attitude.
Results
Respondents’ characteristics and willingness to be vaccinated with the 9vHPV vaccine
A total of 1,550 male college students were invited to participate in the survey. Two male college students completed the questionnaire in less than two minutes, and one did not complete the questionnaire. Therefore, 1,547 were included in the survey, with an overall effective questionnaire recovery rate of 99.81%.
Of the 1,547 respondents, 697 (45.05%) were willing to be vaccinated with the 9vHPV vaccine, whereas 850 (54.95%) were unwilling. Of the respondents, 742 (47.96%) lived in rural areas, and 805 (52.04%) lived in urban areas, 12.15% had a BMI of less than 18.5 (kg/m2), more than half (66.84%) had a BMI between 18.5 and 24 (kg/m2), 16.68% had a BMI between 24 and 28 (kg/m2), and 4.33% had a BMI of more than 28 (kg/m2). Of the respondents, 11.05% (171/1547) were medical students, and 88.95% (1376/1547) were not. One hundred and ninety-seven (12.73%) respondents were current smokers, and 400 (25.86%) were current drinkers (Table 1).
Table 1.
Demographic characteristics and basic information of the participants.
| Item | All participants (N = 1547) |
Intention to receive HPV vaccine |
OR (95%CI) | P-value | |
|---|---|---|---|---|---|
| Vaccine hesitancy (N =850) |
Vaccine acceptance (N = 697) |
||||
| Residence | .863 | ||||
| Rural | 742(47.96%) | 406(47.76%) | 336(48.21%) | Ref | |
| Urban | 805(52.04%) | 444(52.23%) | 361(51.79%) | 0.982(0.804–1.201) | |
| College grade | .001 | ||||
| Freshman | 627(40.53%) | 361(42.47%) | 266(38.16%) | Ref | |
| Sophomore | 572(36.97%) | 330(38.82%) | 242(34.72%) | 0.995(0.791–1.252) | |
| Junior | 223(14.41%) | 108(12.71%) | 115(16.50%) | 1.445(1.063–1.964) | |
| Senior and fifth | 125(8.08%) | 51(6.00%) | 74(10.62%) | 1.969(1.333–2.909) | |
| BMI (kg/m2) | .033 | ||||
| <18.5 | 188(12.15%) | 110(12.94%) | 78(11.19%) | Ref | |
| 18.5–24 | 1034(66.84%) | 548(64.47%) | 486(69.73%) | 1.340(0.97401.843) | |
| 24–28 | 258(16.68%) | 151(17.76%) | 107(15.35%) | 1.073(0.731–1.575) | |
| >28 | 67(4.33%) | 41(4.82%) | 26(3.73%) | 0.725(0.394–1.335) | |
| Are you a medical student? | .001 | ||||
| No | 1376(88.95%) | 777(91.41%) | 599(85.94%) | Ref | |
| Yes | 171(11.05%) | 73(8.59%) | 98(14.06%) | 1.741(1.263–2.401) | |
| Current smoking status | .157 | ||||
| No | 1350(87.27%) | 751(88.35%) | 599(85.94%) | Ref | |
| Yes | 197(12.73%) | 99(11.65%) | 98(14.06%) | 1.241(0.920–1.674) | |
| Current drinking status | .980 | ||||
| No | 1147(74.14%) | 630(74.12%) | 517(74.18%) | Ref | |
| Yes | 400(25.86%) | 220(25.88%) | 180(25.82%) | 0.997(0.793–1.253) | |
| Romantic relationships | <.001 | ||||
| Single, no romance experience | 586(37.88%) | 353(41.53%) | 233(33.43%) | Ref | |
| Single, have romantic experience | 487(31.48%) | 276(32.47%) | 211(30.27%) | 1.158(0.908–1.478) | |
| In a romantic relationship | 474(30.64%) | 221(26.00%) | 253(36.30%) | 1.734(1.358–2.215) | |
| Do you have relatives or friends with cervical cancer? | .001 | ||||
| No | 1479(95.60%) | 827(97.29%) | 652(93.54%) | Ref | |
| Yes | 68(4.40%) | 23(2.71%) | 45(6.46%) | 2.482(1.486–4.144) | |
| Do you have friends or relatives who received 9-valent HPV? | <.001 | ||||
| No | 952(61.54%) | 571(67.18%) | 381(54.66%) | Ref | |
| Yes | 595(38.46%) | 279(32.82%) | 316(45.34%) | 1.697(1.380–2.087) | |
Data are presented as number (percentage). P-values were calculated via univariate analysis between the “vaccine hesitancy” and “vaccine acceptance” groups. OR: odds ratio; CI: confidence interval.
According to Table 1, the willingness to be vaccinated with the vaccine was unrelated to age, residence, current smoking status, or current drinking status. Statistically significant differences (all p < .05) were observed between the vaccine-accepting and vaccine-hesitant groups in terms of college grade, body mass index, specialty, romantic relationships, whether their relatives and friends had cervical cancer, and whether relatives and friends had been vaccinated with the 9vHPV vaccine.
Sources of information on HPV and the 9vHPV vaccine
The most important source of information on HPV and the 9vHPV vaccine for the study respondents was media (such as television, magazines, media, and Internet) (1,134/1,547, and 73.30%), followed by government agencies (1,004/1,547, and 64.90%), medical staff (829/1,547, and 53.59%), relatives and friends (762/1,547, and 49.26%), and other channels (6/1,547, and 0.39%). The source of information for some respondents was unclear (43/1,547, and 2.78%) (Figure 1).
Figure 1.
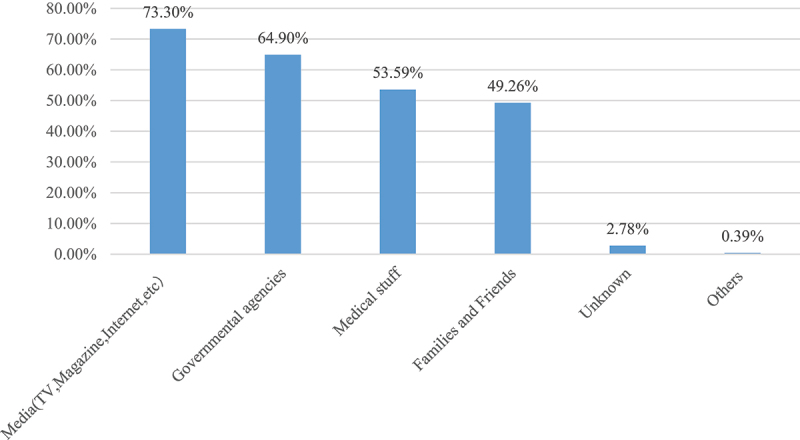
Sources of information about HPV and HPV vaccine (N = 1547).
Knowledge of and attitude toward HPV and the 9vHPV vaccine
Statistical differences were observed between the vaccine hesitancy and vaccine acceptance groups in terms of patients’ knowledge of and attitude toward HPV and the vaccine (Table 2). Among Chinese male college students who knew that HPV could cause genital warts and cancers or that men might also develop HPV infection, believed that men should be vaccinated with the 9vHPV vaccine, and would recommend this vaccine to relatives and friends, the proportion of students willing to be vaccinated with the 9vHPV vaccine was higher than that of students unwilling to be vaccinated. Among those who regarded the vaccine as safe and effective, the proportion of students willing to be vaccinated with the 9vHPV vaccine was also significantly higher than that of students unwilling to be vaccinated (all p < .01).
Table 2.
Participants’ knowledge about and attitude toward the HPV and 9-valent HPV vaccine.
| Item | All participants (N = 1547) |
Intention to receive HPV vaccine |
OR (95%CI) | P-value | |
|---|---|---|---|---|---|
| Vaccine hesitancy (N =850) |
Vaccine acceptance (N = 697) |
||||
| HPV can cause genital warts and certain cancers. | <.001 | ||||
| No | 541(34.97%) | 333(39.18%) | 208(29.84%) | Ref | |
| Yes | 1006(65.03%) | 517(60.82%) | 489(70.16%) | 1.514(1.224–1.873) | |
| HPV can only be transmitted through sexual behavior. | .686 | ||||
| No | 1186(76.66%) | 655(77.06%) | 531(76.18%) | Ref | |
| Yes | 361(23.34%) | 195(22.94%) | 166(23.82%) | 1.050(0.829–1.330) | |
| Men can’t be infected with HPV. | <.001 | ||||
| No | 1194(77.18%) | 627(73.76%) | 567(81.35%) | Ref | |
| Yes | 353(22.82%) | 223(26.24%) | 130(18.65%) | 0.645(0.505–0.823) | |
| 9-valent HPV vaccination can effectively prevent HPV-related cancers. | .166 | ||||
| No | 260(16.81%) | 153(18.00%) | 107(15.35%) | Ref | |
| Yes | 1287(83.19%) | 697(82.00%) | 590(84.65%) | 1.210(0.924–1.586) | |
| The best age for receiving the 9-valent HPV vaccine is before 26 years old. | .154 | ||||
| No | 318(20.56%) | 186(21.88%) | 132(18.94%) | Ref | |
| Yes | 1229(79.44%) | 664(78.12%) | 565(81.06%) | 1.199(0.934–1.539) | |
| Are you in support of promoting the 9-valent HPV vaccine for men? | <.001 | ||||
| No | 855(55.27%) | 611(71.88%) | 244(35.01%) | Ref | |
| Yes | 692(44.73%) | 239(28.12%) | 453(64.99%) | 4.746(3.825–5.890) | |
| Do you think the authorized 9-valent HPV vaccine is safe? | .003 | ||||
| No | 224(14.48%) | 144(16.94%) | 80(11.48%) | Ref | |
| Yes | 1323(85.52%) | 706(83.06%) | 617(88.52%) | 1.573(1.173–2.110) | |
| Do you think the 9-valent HPV vaccine could have unexpected side effects? | .096 | ||||
| No | 975(63.03%) | 520(61.18%) | 455(65.28%) | Ref | |
| Yes | 572(36.97%) | 330(38.82%) | 242(34.72%) | 0.838(0.681–1.032) | |
| Do you think the authorized 9-valent HPV vaccine is effective? | .003 | ||||
| No | 184(19.00%) | 120(14.12%) | 64(9.18%) | Ref | |
| Yes | 1363(81.00%) | 730(85.88%) | 633(90.82%) | 1.626(1.179–2.242) | |
| Would you recommend that your family and friends receive the 9-valent HPV vaccine? | <.001 | ||||
| No | 294(19.00%) | 220(25.88%) | 74(10.62%) | Ref | |
| Yes | 1253(81.00%) | 630(74.12%) | 623(89.38%) | 2.940(2.209–3.912) | |
Data are presented as number (percentage). P-values were calculated via univariate analysis between the “vaccine hesitancy” and “vaccine acceptance” groups. OR: odds ratio; CI: confidence interval.
Predictors of vaccination with the 9vHPV vaccine
The univariate analysis obtained 12 variables with a p-value of < .05, as shown in Tables 1 and 2. The multivariate logistic regression analysis was performed on 10 variables. Among them, six variables were crucial for the willingness to be vaccinated with the 9vHPV vaccine (p < .05) (Table 3): being a medical student (OR = 1.483, 95% CI: 1.029–2.137, p = .034 vs. non-medical students); students whose relatives and friends had cervical cancer (OR = 2.244, 95% CI: 1.257–4.006, p = .006 vs. none); students whose relatives and friends had received the 9vHPV vaccine (OR = 1.338, 95% CI: 1.048–1.708, p = .019 vs. none); students in a romantic relationship (OR = 1.602, 95% CI: 1.213–2.115, p < .001 vs. single or without romantic experience); students supporting the promotion of the 9vHPV vaccine for men (OR = 4.865, 95% CI: 3.848–6.152, p< .001 vs. non-supportive); and students who would recommend the 9vHPV vaccine to their relatives and friends (OR = 3.037, 95% CI: 2.103–4.385, p < .001 vs. would not). The multivariate logistic regression analysis was performed on all variables, and similar results were obtained (Supplement Table S1).
Table 3.
Predictors of intention to get the 9-valent HPV vaccine (12 variables with a P-value of < .05).
| Item | Intention to receive HPV vaccine |
AOR (95% CI) | P-value | |
|---|---|---|---|---|
| Vaccine hesitancy (N =855) | Vaccine acceptance (N = 692) | |||
| College grade | ||||
| Freshman | 361 | 266 | Ref | / |
| Sophomore | 330 | 242 | 0.872(0.660–1.152) | .335 |
| Junior | 108 | 115 | 1.249(0.821–1.899) | .299 |
| Senior and fifth | 51 | 74 | 0.983(0.557–1.732) | .952 |
| BMI (kg/m2) | ||||
| <18.5 | 110 | 78 | Ref | / |
| 18.5–24 | 548 | 486 | 1.368(0.960–1.949) | .083 |
| 24–28 | 151 | 107 | 1.283(0.836–1.967) | .254 |
| >28 | 41 | 26 | 0.754(0.380–0.497) | .420 |
| Are you a medical student? | ||||
| No | 777 | 599 | Ref | / |
| Yes | 73 | 98 | 1.483(1.029–2.137) | .034 |
| Romantic relationships | ||||
| Single, no romance experience | 353 | 233 | Ref | / |
| Single, have romantic experience | 276 | 211 | 0.938(0.712–1.235) | .649 |
| In a romantic relationship | 221 | 253 | 1.602(1.213–2.115) | .001 |
| Do you have relatives or friends with HPV-related cancers? | ||||
| No | 827 | 652 | Ref | / |
| Yes | 23 | 45 | 2.244(1.257–4.006) | .006 |
| Do you have friends or relatives who have received 9-valent HPV? | ||||
| No | 571 | 381 | Ref | / |
| Yes | 279 | 316 | 1.338(1.048–1.708) | .019 |
| HPV can cause genital warts and certain cancers. | ||||
| No | 333 | 208 | Ref | / |
| Yes | 517 | 489 | 1.061(0.825–1.365) | .644 |
| Men can’t be infected with HPV. | ||||
| No | 627 | 567 | Ref | / |
| Yes | 223 | 130 | 0.852(0.645–1.1.24) | .257 |
| Are you in support of promoting the 9-valent HPV vaccine for men? | ||||
| No | 611 | 244 | Ref | / |
| Yes | 239 | 453 | 4.865(3.848–6.152) | <.001 |
| Do you think the authorized 9-valent HPV vaccine is safe? | ||||
| No | 144 | 80 | Ref | / |
| Yes | 706 | 617 | 0.811(0.538–1.223) | .318 |
| Do you think the authorized 9-valent HPV vaccine is effective? | ||||
| No | 120 | 64 | Ref | / |
| Yes | 730 | 633 | 0.740(0.467–1.174) | .201 |
| Would you recommend that your family and friends receive the 9-valent HPV vaccine? | ||||
| No | 220 | 74 | Ref | / |
| Yes | 630 | 623 | 3.037(2.103–4.385) | <.001 |
P-values indicate whether the adjusted OR of a particular sub-category is significant compared to the reference category. OR: odds ratio; CI: confidence interval.
Structural equation model
In this study, demographic characteristics and basic information, knowledge and attitude were taken as latent variables, and the observed variables included in each latent variable were taken as explicit variables to establish a structural equation model. The connotations of latent variables and observed variables were shown in Table 4. Parameter estimation of the model was performed using weighted least squares estimator with adjustments for the mean and variance (WLSMV). Model fitting was evaluated using χ2/df, root mean square error of approximation, RMSEA), Standardized Root Mean Square Residual SRMR, Comparative fit index (CFI), Tuck-Lewis Index (TLI), etc. The fitting results are shown in Table 5. With Tucker-Lewis Index, which measured slight below 0.90, and the Standardized Root Mean Square Residual (SRMR), which measured slight above 0.050, other fit indices fulfill the accepted values. The χ2/df was estimated at 4.781, stipulating an acceptable fit, while Root Mean Square Error of Approximation (RMSEA) and Goodness of Fit Index (GFI) were estimated at 0.049 and 0.910 and indicates good fit. Path analysis of the model shows that demographic characteristics and basic information has a significant positive effect on knowledge and attitude, of which the direct effect value is 1.555, and 0.341, respectively (Table 6). The structural model between the variables of demographic characteristics and basic information, knowledge and attitude was shown in Figure 2.
Table 4.
Latent variable and observational variable.
| Latent variable | Observational variable |
|---|---|
| F1 (Demographic characteristics and basic information) | A1 Residence |
| A2 College grade | |
| A3 BMI | |
| A4 Are you a medical student? | |
| A5 Current smoking status | |
| A6 Current drinking status | |
| A7 Romantic relationships | |
| A8 Do you have relatives or friends with cervical cancer? | |
| A9 Do you have friends or relatives who received 9-valent HPV? | |
| F2 (knowledge) | B1 HPV can cause genital warts and certain cancers. |
| B2 HPV can only be transmitted through sexual behavior. | |
| B3 Men can’t be infected with HPV. | |
| B4 9-valent HPV vaccination can effectively prevent HPV-related cancers. | |
| B5 The best age for receiving the 9-valent HPV vaccine is before 26 years old. | |
| F3 (attitude) | C1 Are you in support of promoting the 9-valent HPV vaccine for men? |
| C2 Do you think the authorized 9-valent HPV vaccine is safe? | |
| C3 Do you think the 9-valent HPV vaccine could have unexpected side effects? | |
| C4 Do you think the authorized 9-valent HPV vaccine is effective? | |
| C5 Would you recommend that your family and friends receive the 9-valent HPV vaccine? |
Table 5.
Goodness of fit indices.
| Fit indices | Model value | Accepted value |
|---|---|---|
| χ2/df | 4.781 | <5 |
| Root Mean Square Error of Approximation (RMSEA) | 0.049 | <0.100 |
| Goodness of Fit Index (GFI) | 0.910 | >0.900 |
| Tucker-Lewis Index (TLI) | 0.897 | >0.900 |
| Standardized Root Mean Square Residul (SRMR) | 0.081 | <0.050 |
Table 6.
Model results of each path.
| Hypothesis | Paths | Coefficient | Standard error | P-value |
|---|---|---|---|---|
| H1 | F1→F2 | 1.555 | 0.362 | <.001 |
| H2 | F1→F3 | 0.341 | 0.121 | .005 |
Figure 2.
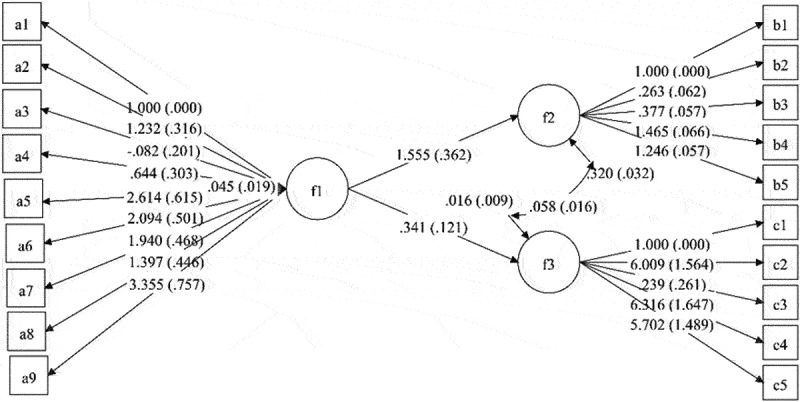
The structural model between the variables of demographic characteristics and basic information, knowledge and attitude.
Discussion
Both men and women face the risk of HPV infection, which may progress to HPV-related cancer. Vaccination with the 9vHPV vaccine is an efficient and safe method to prevent and treat HPV infections. The 9vHPV vaccine was approved for use by the United States (US) Food and Drug Administration on December 10, 2014. The vaccine is effective against HPV6, 11, 16, and 18 (types targeted by the 4-valent HPV vaccine), as well as HPV31, 33, 45, 52, and 58.24 At present, men in China cannot make an appointment to receive the 9vHPV vaccine, but clinical trials testing the 9vHPV vaccine have begun recruiting young men. In 2021, Merck & Co., Inc. launched a phase-3 clinical trial in China to evaluate the protective efficacy, immunogenicity, and safety of the 9vHPV vaccine in Chinese men. However, no study has investigated the acceptance of the 9vHPV vaccine by young Chinese men. Before probing into the vaccination of Chinese men with the 9vHPV vaccine, we conducted a questionnaire survey to assess the knowledge of male college students about, their attitude toward, and acceptance of the 9vHPV vaccine, offering some reference for follow-up vaccination.
We estimated that a minimum sample size of 630 was required. This study recruited a total of 1547 respondents, which was sufficient to draw statistically meaningful conclusions. Of the respondents, 54.95% were unwilling to be vaccinated with the 9vHPV vaccine, and 45.05% were willing. Similar studies in foreign countries reported a high willingness among male college students to be vaccinated against HPV. A survey of 18- to 30-year-old students in Italy reported that 79% of the unvaccinated male respondents expressed a willingness to be vaccinated.25 In 2014, a study of male high school and college students in South Korea also reported that 66.7% of unvaccinated male college students intended to get vaccinated.26 In a US-based study on adult men (mostly from colleges and universities), 69% were likely or very likely to get vaccinated against HPV if the vaccine was available.27 According to another study conducted in central Florida, US, between March 2007 and January 2009, 62% of male college students were willing to consider HPV vaccination.28 Another study conducted at Dutch universities reported that 48% of the respondents were willing to be vaccinated, similar to the present study results.29 Compared to similar studies in foreign countries, this study found a low acceptance of the 9vHPV vaccine among male college students, which might be related to differences in regions and populations included in the studies. The survey results yielded the following suggestions.
Development of personalized vaccination strategies for different populations
We found that the identity of medical students was a crucial factor influencing willingness to be vaccinated with the 9vHPV vaccine. In our study, 57.3% of the medical students were willing to be vaccinated against HPV. This result is similar to that in studies conducted in China. In a study of medical students in eastern, central, and western China conducted from November 2020 to March 2021, 60.82% of the respondents expressed their intention to get vaccinated.30 According to the results of a cross-sectional study conducted at four universities in Qingdao, Shandong Province, China, from September 2018 to January 2019, students majoring in health science scored higher than those majoring in other specialties in terms of HPV and HPV vaccine-related knowledge and were more willing to get vaccinated against HPV (82.2% vs. 69.9%).31 This may be because medical students, influenced by their specialty, have more knowledge about HPV and HPV-induced diseases and hold a more inclusive and open attitude toward vaccination with the 9vHPV vaccine.
Male college students in romantic relationships were more willing to be vaccinated than those who were not, and this result may be attributable to a sense of responsibility toward their partners. A study conducted in the Philippines revealed that the willingness of most men (53%) to receive vaccination was influenced by their intention to protect family members, and 40% of them said that protecting their sexual partners from infection was a major reason for getting vaccinated.32 A US-based study in 2011 indicated that emphasizing the altruism of being vaccinated could improve the willingness of young men to get vaccinated.33 This may also explain why male college students who are in romantic relationships may be willing to be vaccinated out of a sense of responsibility for their partners. Considering the cultural atmosphere in China, “acting responsibly for your partner” is a more plausible explanation.
According to the results of the multivariate regression analysis, a major influencing factor was relatives or friends who had HPV-related cancer or had been vaccinated with the 9vHPV vaccine. In 2014, a study in the US reported that vaccinating older siblings with the HPV vaccine was a positive factor in the vaccination of 9- to 13-year-old children (OR = 2.52 (1.94–3.27)).34 In a Chinese study, “having relatives and friends with certain cancers” was found to be a positive influencing factor for HPV vaccination (adjusted OR (AOR) = 1.290, 95% CI: 1.095–1.518).35 In Guangzhou, a study conducted from October to December 2018 identified “knowledge about vaccinated populations” as a crucial factor influencing vaccination willingness (OR = 3.1, 95% CI: 1.9–5.0).36 The experiences of relatives and friends acted as a source of HPV-related knowledge for male college students. That is, a male college student who had relatives and friends with HPV-related cancer was more likely to gain more HPV-related knowledge and thus closely focus on HPV protection. Similarly, a male college student with vaccinated relatives and friends was more likely to appreciate the importance of the 9vHPV vaccine and hold a more inclusive attitude toward vaccination, as indicated by 49.26% of the male college students learning about HPV from relatives and friends (Figure 1).
The structural equation model also indicated that the demographic characteristics and basic information has a significant positive effect on knowledge and attitude. Therefore, individualized recommendations are more suitable for convincing Chinese male college students to get vaccinated.
Expansion of knowledge dissemination to encourage vaccination
In this study, male college students who realized that HPV could cause genital warts and cancers and that men might be infected with HPV were more willing to be vaccinated with the 9vHPV vaccine. Male college students harboring more prejudices and misunderstandings about HPV tended to hold a careless attitude toward vaccination with the 9vHPV vaccine, thinking that HPV had nothing to do with them. In contrast, a scientific and correct understanding of HPV and the 9vHPV vaccine would help male college students better accept vaccination. Many studies have confirmed the preceding point. A study conducted in China from 2015 to 2016 reported that adolescents who had received sexual health education were more willing to be vaccinated (AOR: 1.35, 95% CI: 1.15–1.58, p < .00135).37 A cross-sectional survey conducted at a major university in Hong Kong from April to September 2015 identified vaccine knowledge as a major influencing factor.38 A foreign study in 2006 found that respondents who correctly answered two or three HPV-related questions manifested a significantly higher degree of acceptance of vaccination.39
Therefore, strengthening the science popularization of HPV-related knowledge among male college students is of great importance. Science popularization offers opportunities for students to acquire correct knowledge, correct prejudices, and fill gaps, which would help them form a healthier view of vaccination and prevent and control diseases. A study of medical students in China from November 2020 to March 2021 also reported that improving the understanding of the 9vHPV vaccine expanded the receipt of HPV vaccine.30 Many foreign studies also argued that the science popularization and publicity of HPV knowledge should be promoted.40–43 The present study found that among the different sources of HPV-related knowledge for male college students, media constituted the primary choice, followed by government agencies and medical staff. The science popularization and publicity efforts of government agencies have achieved initial results and should be further advanced. The government should also strengthen the supervision and regulation of media reports, minimize unscientific, misleading information, and ensure the scientific validity of media communications, which is the largest source of HPV-related knowledge.
Positive attitude toward the vaccine as a key force driving male college students to receive vaccination
The study data indicated that male college students who were supportive of promoting the 9vHPV vaccine for men, considered it safe or effective, and would recommend this vaccine to relatives and friends were more willing to be vaccinated with the 9vHPV vaccine. A positive attitude is a crucial force driving male college students to accept the vaccine.
One possible explanation follows. A positive attitude toward the vaccine comes from recognizing and trusting the safety and effectiveness of the vaccine. Male college students with a positive attitude toward the vaccine are more willing to get vaccinated and recommend it to others. Existing clinical studies showed that 9vHPV produced good immunogenicity and safety in men aged 16–26 years.44 Of the respondents who were willing to be vaccinated in this study, 73.17% chose the vaccine because of its safety, and 69.58% chose it because of its effectiveness. Relevant studies also reported the same results. A US-based study in 2009 found that men who had perceived the effectiveness of the vaccine were more willing to be vaccinated (OR = 1.86, 95% CI: 1.22–2.83).45 A survey on the HPV vaccine hesitancy of parents of Canadian boys and girls aged 9–16 years in September 2016 and July 2017 found that vaccine hesitancy was related to the safety and acceptability of the vaccine.46 A few domestic studies have also reported vaccine effectiveness and safety as key factors influencing the decision to receive vaccination. For example, a Hong Kong-based study conducted from April to September 2015 reported that students were willing to accept the HPV vaccine if it could prevent cervical cancer/anal cancer and genital warts.38 A study conducted in mainland China in 2019 found that a major obstacle preventing men from getting vaccinated against HPV was concerns about safety (37%).47 Supporting the promotion of the 9vHPV vaccine for men and recommending the vaccine to relatives and friends could largely reflect the positive attitude of male college students toward the vaccine, as only students who accepted the 9vHPV vaccine would recommend it to others. In a study based in eastern China, cancer patients willing to recommend the COVID-19 vaccine to their relatives and friends were more likely to get vaccinated with that vaccine.19 We believe that this is closely related to China’s social characteristics and cultural atmosphere as Chinese people attach great importance to their family values and a sense of connection with each other, care about and value their relatives and friends, and are willing to recommend the things they like to their relatives and friends.
Limitations
This study had limitations. First, this was a cross-sectional study in which data were collected through an online questionnaire survey. This made it impossible to directly infer the causality involved. Thus, further longitudinal research is required to validate the possible causal relationship. Second, this questionnaire was based on several previous questionnaires. However, due to the short time window for questionnaire development, we only conducted a small pilot study before distributing the questionnaire. Third, constrained by the geographical location of questionnaire distribution, the respondents were concentrated in central and eastern China and rarely came from western China. Thus, the samples of this study could not fully characterize Chinese male college students’ willingness to be vaccinated with 9vHPV.
Conclusions
Our survey reported the knowledge of Chinese male college students about, attitude toward, and acceptance of the 9vHPV vaccine and the independent predictors. Of the respondents, 54.95% were unwilling to be vaccinated with the 9vHPV vaccine, while 45.05% were willing. Medical students, students whose relatives and friends had cervical cancer, students whose relatives and friends had received the 9vHPV vaccine, were in romantic relationships, were supportive of promoting the 9vHPV vaccine to men, and students who would recommend the vaccine to their relatives and friends were crucial factors influencing their willingness to accept the vaccine. Efforts should be made to strengthen science popularization, and greater scientific understanding will lead to a more inclusive attitude and a higher degree of willingness among Chinese men.
Supplementary Material
Acknowledgments
We thank all participants involved in this study.
Funding Statement
This work was supported by the “Guhai Plan” of The First Affiliated Hospital of Naval Medical University and “Science and Technology Innovation Action Plan” medical innovation research Special Project (No. 22Y11921200).
Author contributions
SJ and JH designed the study. BP, JH and HJ performed the study and their analyses. SJ, DDH, QMZ, JH and YH were responsible for data collection. JH and SJ performed data analyses. All authors participated in data interpretation, manuscript review and writing. SJ and HJ were responsible for preparation of the Tables and Figures. All authors contributed to the scientific discussion of the data and of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2023.2272533.
References
- 1.Egawa N, Egawa K, Griffin H, Doorbar J.. Human papillomaviruses; epithelial tropisms, and the development of neoplasia. Viruses. 2015 July 16;7(7):3863–10. doi: 10.3390/v7072802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV, Snijders PJ, Meijer CJ, International Agency for Research on Cancer Multicenter Cervical Cancer Study Group . Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003 Feb 6;348(6):518–27. doi: 10.1056/NEJMoa021641. [DOI] [PubMed] [Google Scholar]
- 3.Denny L. Nine-valent human papillomavirus vaccine: great science, but will it save lives? Lancet. 2017 Nov 11;390(10108):2123–4. doi: 10.1016/S0140-6736(17)32144-X. [DOI] [PubMed] [Google Scholar]
- 4.Pils S, Joura EA. From the monovalent to the nine-valent HPV vaccine. Clin Microbiol Infect. 2015. Sep;21(9):827–33. doi: 10.1016/j.cmi.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 5.American Chemical Society . HPV and cancer; [accessed 2023 Feb 15]. https://www.cancer.org/healthy/cancer-causes/infectious-agents/hpv/hpv-and-cancer-info.html.
- 6.Woodman CB, Collins SI, Young LS. The natural history of cervical HPV infection: unresolved issues. Nat Rev Cancer. 2007. Jan;7(1):11–22. doi: 10.1038/nrc2050. [DOI] [PubMed] [Google Scholar]
- 7.Santella B, Schettino MT, Franci G, De Franciscis P, Colacurci N, Schiattarella A, Galdiero M. Microbiota and HPV: the role of viral infection on vaginal microbiota. J Med Virol. 2022. Sep;94(9):4478–84. doi: 10.1002/jmv.27837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Forman D, de Martel C, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, Bruni L, Vignat J, Ferlay J, Bray F, Plummer M, et al. Global burden of human papillomavirus and related diseases. Vaccine. 2012 Nov 20;30(Suppl 5):F12–23. doi: 10.1016/j.vaccine.2012.07.055. [DOI] [PubMed] [Google Scholar]
- 9.Huh WK, Joura EA, Giuliano AR, Iversen OE, de Andrade RP, Ault KA, Bartholomew D, Cestero RM, Fedrizzi EN, Hirschberg AL, et al. Final efficacy, immunogenicity, and safety analyses of a nine-valent human papillomavirus vaccine in women aged 16-26 years: a randomised, double-blind trial. Lancet. 2017 Nov 11;390(10108):2143–59. doi: 10.1016/S0140-6736(17)31821-4. [DOI] [PubMed] [Google Scholar]
- 10.Zou Z, Fairley CK, Ong JJ, Hocking J, Canfell K, Ma X, Chow EPF, Xu X, Zhang L, Zhuang G. Domestic HPV vaccine price and economic returns for cervical cancer prevention in China: a cost-effectiveness analysis. Lancet Glob Health. 2020. Oct;8(10):e1335–e44. doi: 10.1016/S2214-109X(20)30277-1. [DOI] [PubMed] [Google Scholar]
- 11.Garland SM. Prevention strategies against human papillomavirus in males. Gynecol Oncol. 2010. May;117(2 Suppl):S20–5. doi: 10.1016/j.ygyno.2010.01.027. [DOI] [PubMed] [Google Scholar]
- 12.Harder T, Wichmann O, Klug SJ, van der Sande MAB, Wiese-Posselt M. Efficacy, effectiveness and safety of vaccination against human papillomavirus in males: a systematic review. BMC Med. 2018 Jul 18;16(1):110. doi: 10.1186/s12916-018-1098-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization . Vaccination: European commission and world health organization join forces to promote the benefits of vaccines; [accessed 2023 Feb 15]. https://www.who.int/news/item/12-09-2019-vaccination-european-commission-and-world-health-organization-join-forces-to-promote-the-benefits-of-vaccines.
- 14.You D, Han L, Li L, Hu J, Zimet GD, Alias H, Danaee M, Cai L, Zeng F, Wong LP. Human papillomavirus (HPV) vaccine uptake and the willingness to receive the HPV vaccination among female college students in China: a multicenter study. Vaccines (Basel). 2020 Jan 16;8(1):31. doi: 10.3390/vaccines8010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Si M, Jiang Y, Su X, Wang W, Zhang X, Gu X, Ma L, Li J, Zhang S, Ren Z, et al. Willingness to accept human papillomavirus vaccination and its influencing factors using information-motivation-behavior skills model: a cross-sectional study of female college freshmen in mainland China. Cancer Control. 2021. Jan-Dec;28:10732748211032899. doi: 10.1177/10732748211032899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin Y, Lin Z, He F, Hu Z, Zimet GD, Alias H, Wong LP. Factors influencing intention to obtain the HPV vaccine and acceptability of 2-, 4- and 9-valent HPV vaccines: a study of undergraduate female health sciences students in Fujian, China. Vaccine. 2019 Oct 16;37(44):6714–23. doi: 10.1016/j.vaccine.2019.09.026. [DOI] [PubMed] [Google Scholar]
- 17.Gu C, Niccolai LM, Yang S, Wang X, Tao L. Human papillomavirus vaccine acceptability among female undergraduate students in China: the role of knowledge and psychosocial factors. J Clin Nurs. 2015. Oct;24(19–20):2765–78. doi: 10.1111/jocn.12871. [DOI] [PubMed] [Google Scholar]
- 18.Hong J, Pan B, Jiang HJ, Zhang QM, Xu XW, Jiang H, Ye JE, Cui Y, Yan XJ, Zhai XF, et al. The willingness of Chinese healthcare workers to receive monkeypox vaccine and its independent predictors: a cross-sectional survey. J Med Virol. 2023. Jan;95(1):e28294. doi: 10.1002/jmv.28294. [DOI] [PubMed] [Google Scholar]
- 19.Hong J, Xu XW, Yang J, Zheng J, Dai SM, Zhou J, Zhang QM, Ruan Y, Ling CQ. Knowledge about, attitude and acceptance towards, and predictors of intention to receive the COVID-19 vaccine among cancer patients in Eastern China: a cross-sectional survey. J Integr Med. 2022. Jan;20(1):34–44. doi: 10.1016/j.joim.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sari Y, Anam A, Sumeru A, Sutrisna E. The knowledge, attitude, practice and predictors of complementary and alternative medicine use among type 2 diabetes mellitus patients in Indonesia. J Integr Med. 2021. Jul;19(4):347–53. doi: 10.1016/j.joim.2021.04.001. [DOI] [PubMed] [Google Scholar]
- 21.Adjei Boakye E, Tobo BB, Rojek RP, Mohammed KA, Geneus CJ, Osazuwa-Peters N. Approaching a decade since HPV vaccine licensure: racial and gender disparities in knowledge and awareness of HPV and HPV vaccine. Hum Vaccin Immunother. 2017 Nov 2;13(11):2713–22. doi: 10.1080/21645515.2017.1363133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu Y, Di N, Tao X. Knowledge, practice and attitude towards HPV vaccination among college students in Beijing, China. Hum Vaccin Immunother. 2020;16(1):116–23. doi: 10.1080/21645515.2019.1638727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Farsi NJ, Baharoon AH, Jiffri AE, Marzouki HZ, Merdad MA, Merdad LA. Human papillomavirus knowledge and vaccine acceptability among male medical students in Saudi Arabia. Hum Vaccin Immunother. 2021 Jul 3;17(7):1968–74. doi: 10.1080/21645515.2020.1856597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Petrosky E, Bocchini JA Jr, Hariri S, Chesson H, Curtis CR, Saraiya M, Unger ER, Markowitz LE. Centers for disease control and prevention (CDC). Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. Morb Mortal Wkly Rep. 2015 Mar 27;64(11):300–4. [PMC free article] [PubMed] [Google Scholar]
- 25.Mascaro V, Pileggi C, Currà A, Bianco A, Pavia M. HPV vaccination coverage and willingness to be vaccinated among 18-30 year-old students in Italy. Vaccine. 2019 May 31;37(25):3310–6. doi: 10.1016/j.vaccine.2019.04.081. [DOI] [PubMed] [Google Scholar]
- 26.Choi JS, Park S. A study on the predictors of Korean male students’ intention to receive human papillomavirus vaccination. J Clin Nurs. 2016. Nov;25(21–22):3354–62. doi: 10.1111/jocn.13461. [DOI] [PubMed] [Google Scholar]
- 27.Hernandez BY, Wilkens LR, Thompson PJ, Shvetsov YB, Goodman MT, Ning L, Kaopua L. Acceptability of prophylactic human papillomavirus vaccination among adult men. Hum Vaccin. 2010. Jun;6(6):467–75. doi: 10.4161/hv.6.6.11279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Daley EM, Marhefka SL, Buhi ER, Vamos CA, Hernandez ND, Giuliano AR. Human papillomavirus vaccine intentions among men participating in a human papillomavirus natural history study versus a comparison sample. Sex Transm Dis. 2010. Oct;37(10):644–52. doi: 10.1097/OLQ.0b013e3181e1a14c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lenselink CH, Schmeink CE, Melchers WJ, Massuger LF, Hendriks JC, van Hamont D, Bekkers RL. Young adults and acceptance of the human papillomavirus vaccine. Public Health. 2008. Dec;122(12):1295–301. doi: 10.1016/j.puhe.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 30.Zhou L, Gu B, Xu X, Li Y, Cheng P, Huo Y, Liu G, Zhang X. On imported and domestic human papillomavirus vaccines: cognition, attitude, and willingness to pay in Chinese medical students. Front Public Health. 2022 May 12;10:863748. doi: 10.3389/fpubh.2022.863748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu Y, Bi W, Liu T, Jiang Y, Wang Q, Fan R. Factors associated with intention of human papillomavirus vaccination among Chinese college students: implications for health promotion. Hum Vaccin Immunother. 2021 Dec 2;17(12):5426–32. doi: 10.1080/21645515.2021.2007014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Young AM, Crosby RA, Jagger KS, Casquejo E, Pinote L, Ybañez P, Casquejo L, Estorgio D, Pinote L. Influences on HPV vaccine acceptance among men in the Philippines. J Men’s Health. 2011. May;8(2):126–35. doi: 10.1016/j.jomh.2011.01.007. [DOI] [Google Scholar]
- 33.Bonafide KE, Vanable PA. Male human papillomavirus vaccine acceptance is enhanced by a brief intervention that emphasizes both male-specific vaccine benefits and altruistic motives. Sex Transm Dis. 2015. Feb;42(2):76–80. doi: 10.1097/OLQ.0000000000000226. [DOI] [PubMed] [Google Scholar]
- 34.Donahue KL, Hendrix KS, Sturm LA, Zimet GD. Human papillomavirus vaccine initiation among 9-13-Year-olds in the United States. Prev Med Rep. 2015;2:892–8. doi: 10.1016/j.pmedr.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dai Z, Si M, Su X, Wang W, Zhang X, Gu X, Ma L, Li J, Zhang S, Ren Z, et al. Willingness to human papillomavirus (HPV) vaccination and influencing factors among male and female university students in China. J Med Virol. 2022. Jun;94(6):2776–86. doi: 10.1002/jmv.27478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ma Y, Wang C, Liu F, Lian G, Li S, He Q, Li T. Human papillomavirus vaccination coverage and knowledge, perceptions and influencing factors among university students in Guangzhou, China. Hum Vaccin Immunother. 2021 Oct 3;17(10):3603–12. doi: 10.1080/21645515.2021.1927411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang X, Wang Z, Ren Z, Li Z, Ma W, Gao X, Zhang R, Qiao Y, Li J. HPV vaccine acceptability and willingness-related factors among Chinese adolescents: a nation-wide study. Hum Vaccin Immunother. 2021 Apr 3;17(4):1025–32. doi: 10.1080/21645515.2020.1812314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chiang VC, Wong HT, Yeung PC, Choi YK, Fok MS, Mak OI, Wong HY, Wong KH, Wong SY, Wong YS, et al. Attitude, acceptability and knowledge of HPV vaccination among Local University students in Hong Kong. Int J Environ Res Public Health. 2016 May 11;13(5):486. doi: 10.3390/ijerph13050486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jones M, Cook R. Intent to receive an HPV vaccine among university men and women and implications for vaccine administration. J Am Coll Health. 2008. Jul-Aug;57(1):23–32. doi: 10.3200/JACH.57.1.23-32. [DOI] [PubMed] [Google Scholar]
- 40.Laserson AK, Oliffe JL, Krist J, Kelly MT. HPV vaccine and college-age men: a scoping review. Am J Mens Health. 2020. Nov-Dec;14(6):1557988320973826. doi: 10.1177/1557988320973826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sadlier C, Lynam A, O’Dea S, Delamere S, Quinlan M, Clarke S, Sheils O, Bergin C. HPV vaccine acceptability in HIV-infected and HIV negative men who have sex with men (MSM) in Ireland. Hum Vaccin Immunother. 2016 Jun 2;12(6):1536–41. doi: 10.1080/21645515.2016.1151588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Giuliani M, Vescio MF, Donà MG, Latini A, Frasca M, Colafigli M, Farinella M, Rezza G, Cristaudo A. Perceptions of human papillomavirus (HPV) infection and acceptability of HPV vaccine among men attending a sexual health clinic differ according to sexual orientation. Hum Vaccin Immunother. 2016 Jun 2;12(6):1542–50. doi: 10.1080/21645515.2015.1115935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oh JK, Lim MK, Yun EH, Lee EH, Shin HR. Awareness of and attitude towards human papillomavirus infection and vaccination for cervical cancer prevention among adult males and females in Korea: a nationwide interview survey. Vaccine. 2010 Feb 17;28(7):1854–60. doi: 10.1016/j.vaccine.2009.11.079. [DOI] [PubMed] [Google Scholar]
- 44.Van Damme P, Meijer CJLM, Kieninger D, Schuyleman A, Thomas S, Luxembourg A, Baudin M. A phase III clinical study to compare the immunogenicity and safety of the 9-valent and quadrivalent HPV vaccines in men. Vaccine. 2016 Jul 29;34(35):4205–12. doi: 10.1016/j.vaccine.2016.06.056. [DOI] [PubMed] [Google Scholar]
- 45.Reiter PL, Brewer NT, Smith JS. Human papillomavirus knowledge and vaccine acceptability among a national sample of heterosexual men. Sex Transm Infect. 2010. Jun;86(3):241–6. doi: 10.1136/sti.2009.039065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tatar O, Shapiro GK, Perez S, Wade K, Rosberger Z. Using the precaution adoption process model to clarify human papillomavirus vaccine hesitancy in canadian parents of girls and parents of boys. Hum Vaccin Immunother. 2019;15(7–8):1803–14. doi: 10.1080/21645515.2019.1575711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hu S, Xu X, Zhang Y, Liu Y, Yang C, Wang Y, Wang Y, Yu Y, Hong Y, Zhang X, et al. A nationwide post-marketing survey of knowledge, attitude and practice toward human papillomavirus vaccine in general population: implications for vaccine roll-out in mainland China. Vaccine. 2021 Jan 3;39(1):35–44. doi: 10.1016/j.vaccine.2020.11.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


