ABSTRACT
This anonymous cross-sectional study aimed to investigate the relationships between HIV infection and mpox-related focus issues among Chinese men who have sex with men (MSM). This study involved in 27 MSM social organizations and was conducted from July 31 to August 4, 2023. Mpox vaccination hesitancy was defined as the proportion of participants who expressed unwillingness to receive self-funded and free vaccines. Logistic regression models were employed to estimate odds ratios (OR) and 95% confidence interval (95%CI). Of 7196 MSMs, the prevalence of mpox differed between people living with HIV (PLWH) (1.04%, 20/1920) and people living without HIV (PLWoH) (0.55%, 29/5276) (P = .037). However, after adjusting for all covariates, there was no significant association between HIV status and mpox (aOR = 1.17; 95%CI = 0.58, 2.39; P = .658). Furthermore, the crude rates of vaccination hesitation (PLWoH: 5.91%, PLWH: 4.11%; P = .004) and consultation hesitation (PLWoH: 16.22%, PLWH: 10.78%; P < .001) were both lower in the PLWH. Compared with PLWoH, PLWH had lower odds ratios of vaccination hesitation (aOR = 0.70; 95%CI = 0.53, 0.92; P = .011) and consultation hesitation (aOR = 0.74; 95%CI = 0.60, 0.90; P = .003) among MSM. The estimate of association between HIV status and consultation hesitation was even smaller among MSM who reported hepatitis C infection or uncertainty (aOR = 0.30; 95%CI = 0.15, 0.56), compared with those without hepatitis C (aOR = 0.73; 95%CI = 0.60, 0.89) (P for interaction = .037). MSM living with HIV in China demonstrated a greater willingness to accept mpox vaccination and medical consultation. In the future, it is recommended that medical institutions establish good medical environment to control the mpox epidemic, especially for PLWH.
KEYWORDS: Mpox, HIV, vaccination, MSM, China
Introduction
Mpox (formerly known as monkeypox) virus infections usually occur in the African region and occasionally spread to the United Kingdom (UK) and the United States (US).1–3 At the beginning of 2022, since the UK reported an imported mpox case from Nigeria, multiple countries began to report mpox cases.4,5 This multinational outbreak was quickly defined as the Public Health Emergency of International Concern (PHEIC) by the World Health Organization (WHO) on July 23, 2022.6 By August 2, 2023, more than 88,000 confirmed mpox cases had been reported across 113 countries or territories.7 In contrast to previous cases, the main infected population in this outbreak was men who have sex with men (MSM).8,9 Although there are three antiviral agents with activity against mpox, including cidofovir, brincidofovir, and tecovirimat,10 the focus of human immunodeficiency virus (HIV) status in transmission and treatment of mpox occurred due to the similar risk population of mpox and HIV, immunosuppression of people living with HIV (PLWH), and stigma.8,11 Laurenson-Schafer et al. reported that 48% of mpox cases in the past year were PLWH (16961/35,329).8 Furthermore, mpox cases living with HIV had a higher odds ratio of hospitalization.8 However, there is a lack of recent national evidence on associations between HIV status and mpox virus infection.
On July 26, 2023, China subsequently announced the Mpox prevention and control program in order to control the spread of mpox, considering the nearly 500 confirmed cases of mpox across 23 provinces, autonomous regions and municipalities, as well as the size and activity of the MSM population in China.12–14 Vaccination is considered as the effective way to curb infectious diseases.15 Although there have been instances of infections or reinfections after vaccination, the clinical features and outcomes of them appear to be less severe.16 Currently, in China, there is no access to the mpox vaccine, but its development is underway.17 The rate of vaccination hesitation for other vaccines, particularly for influenza and human papilloma virus (HPV) is high among Chinese population.18,19 For instance, Wang et al. reported that the overall median rate of HPV vaccination refusal across China was 28.2%.19 Vaccination hesitation is not conducive to the popularization of vaccination and may hinder efforts to end the mpox epidemic in the future. In our previous study, we analyzed the factors that influenced mpox vaccination in PLWH and PLWoH.20 However, we did not analyze the association between HIV status and hesitation toward mpox vaccination. PLWH may face greater challenges in receiving the mpox vaccine due to concerns about the safety of the vaccine in immunocompromised populations.21
In China, individuals who engaged in high-risky behavior or a related epidemiological history, suspected infections, or close contacts with infected individuals could seek consultation for mpox at an infectious disease specialist hospital or the dermatology department of a general hospital. People could test mpox at hospitals and Chinese Centers for Disease Control and Prevention (CDC). Up until now, due to the limited number of cases in each province, most of the cases were tested for free using nucleic acid detection at the CDC. The hesitation to seek medical consultation hinders the timely detection, isolation, and treatment for mpox cases, thereby increasing the challenge of finding the source of infection and cutting off the transmission. Considering privacy concerns, stigma, and limited access to medical settings, PLWH may hesitate to seek medical consultation for mpox.
Up to now, the association of HIV status with mpox-related focus issues, including mpox virus infection, mpox vaccination hesitation, and consultation hesitation for mpox were unknown among Chinese MSM. This study aimed to provide the latest relevant evidence to assist in formulating clinical and public health management policies, with the assistance of the 27 social organizations for MSM in China.
Materials and methods
Data source
Our participants were recruited from 27 MSM social organizations across 21 provinces, municipalities, and autonomous regions of China, between July 31 and August 4, 2023. The details were described in our previous study.20 We recruited MSM who were at least 18 years old and reported engaging in sexual activities with at least one man in the past 12 months (including anal sex, oral sex, hand sex, hugging, touching, kissing, etc.) in mainland China. Participants provided informed consent. After excluding 342 MSM with unknown HIV status, we finally included 7196 MSM. The Ethics Committee of the Guizhou Center for Disease Control and Prevention (Q 2022–02) approved the study’s design, details, and procedures of the study.
Assessment of HIV status, mpox virus infection, mpox vaccination hesitation, and consultation hesitation for mpox
HIV status was assessed by asking one question: “Have you been diagnosed with HIV?.” Participants who answered “yes” were classified as PLWH, and those who answered “no” were classified as people living without HIV (PLWoH). Participants who selected the option of “uncertainty” were excluded from this study.
Our primary outcomes included mpox virus infection, mpox vaccination hesitation, and consultation hesitation for mpox. After informing participants about the symptoms of mpox and the diagnostic standard based on the Mpox prevention and control program,13 we classified those who answered “diagnosed by a medical institution” as mpox virus infections. Mpox vaccination hesitancy was defined as the proportion of participants who answered “not willing to take self-funded and free vaccines” when asked whether they were willing to receive vaccines against mpox if available. Medical consultation hesitation for mpox was assessed by asking one question: “If you were infected with the mpox virus, which of the following measures would you prefer?.” The options included the “infectious disease specialist hospital,” “the dermatology department of a general hospital,” “related social organizations,” “the local CDC,” “self-medication,” “quarantine at home” and “no measures.” Participants who did not select the first two options were considered to have consultation hesitation.
Covariates
All information was collected by trained healthcare personnel through an electronic questionnaire. Covariates included age group (18 ~ 35 years, ≥36 years), occupation (employed, unemployed), ethnicity (Han, minorities), educational level (junior high school and below, high school, undergraduate, postgraduate, and above), residence (eastern region, western region, and central region), marital status (married, unmarried, widowed, or divorced), sexual orientation (homosexual, bisexual, and unsure), mpox-related knowledge (low, moderate, high), sexual diseases excluding HIV (syphilis, gonorrhea, condyloma acuminatum, genital herpes, and genital chlamydia trachomatis, etc.; yes, no), hepatitis C (yes, no, unsure), and level of sexual risky behavior (low, moderate, high).
Seven items, including sources of infection, possible routes of transmission, susceptible populations, clinical symptoms, vaccines, specific drugs, and preventive measures were used to assess mpox-related knowledge based on our previous studies.22,23 We assigned one point for each correct answer and then calculated the total score for mpox-related knowledge. Total scores ranged from 0 to 23, with higher scores indicating better knowledge. A score of zero represented low mpox-related knowledge, while a score of one to six represented moderate mpox-related knowledge. A score of seven or higher represented high mpox-related knowledge.22,23 Sexual risky behavior was determined based on three sexual behaviors: condomless anal intercourse, commercial sex, and group sex in the last month, as indicated by previous studies.24,25 We assigned a score of zero for option “no” and a score of one for all other responses for the last two behavior components. Regarding the behavior component of condomless anal intercourse, we allocated a score of one for individuals who reported engaging in this behavior “always” or “often,” while a score of zero was assigned to those who reported engaging in it “never” or “seldom.” High sexual risky behavior was indicated by the presence of all three factors, while low sexual risky behavior was indicated by the absence of any of the three behaviors, otherwise moderate sexual risky behavior.
Data analysis
Means ± standard deviations (SDs) and percentages were employed to describe continuous variables and categorical variables, respectively.
Univariate analysis was conducted using Chi-square test. Logistic regression models were conducted to estimate odds ratios (OR) and 95% confidence intervals (95% CI), while accounting for various adjustments to control for potential confounding factors. Model 1 was a univariate model. Model 2 accounted for adjustments in age group, occupation, ethnicity, educational level, residence, and marital status. Based on model 2, we additionally adjusted sexual orientation, mpox-related knowledge, sexual diseases excluding HIV, hepatitis C, sexual risky behavior, and other two outcomes in model 3. The statistical significance of an interaction was assessed by incorporating a product term in the model 3 during the stratified analysis. We measured the interaction of the product term.26,27 All analyses were conducted using R 4.2.0. A two-sided P value less than .05 was considered to be statistically significant.
Results
Population characteristics
Table 1 displays the baseline characteristics of the participants. Of the 7163 MSM (32.25 ± 13.74 years), 44.44% of them lived in eastern China. More than half of them were younger than 35 years old (72.50%) and had a bachelor’s degree or higher (52.13%). The prevalence of mpox virus infection was 0.68% (49/7196). The rate of mpox vaccination hesitation and mpox consultation hesitation was 5.43% (391/7196) and 14.77% (391/7196), respectively (Table 1).
Table 1.
Population characteristics by mpox status among men who have sex with men in China.
| Characteristics | Overall (n, %) | Mpox |
Vaccination hesitation |
Consultation hesitation |
|||
|---|---|---|---|---|---|---|---|
| n(%) | P-value | n(%) | P-value | n(%) | P-value | ||
| 7196 | 49 (0.68) | 391 (5.43) | 1063 (14.77) | ||||
| Age group (years) | .526 | <.001 | <.001 | ||||
| 18 ~ 35 | 5217 (72.50) | 38 (0.73) | 252 (4.83) | 721 (13.82) | |||
| ≥36 | 1979 (25.67) | 11 (0.56) | 139 (7.02) | 342 (17.28) | |||
| Occupation | .011 | <.001 | .756 | ||||
| Employed | 6447 (89.59) | 38 (0.59) | 328 (5.09) | 949 (14.72) | |||
| Unemployed | 749 (10.41) | 11 (1.47) | 63 (8.41) | 114 (15.22) | |||
| Education level | <.001 | .01 | <.001 | ||||
| Junior high school and below | 620 (8.62) | 10 (1.61) | 47 (7.58) | 133 (21.45) | |||
| High school | 2825 (39.26) | 26 (0.92) | 148 (5.24) | 418 (14.80) | |||
| Undergraduate | 3018 (41.94) | 8 (0.27) | 145 (4.80) | 423 (14.02) | |||
| Postgraduate and above | 733 (10.19) | 5 (0.68) | 51 (6.96) | 89 (12.14) | |||
| Marital status | .02 | .002 | .001 | ||||
| Married | 952 (13.23) | 13 (1.37) | 70 (7.35) | 179 (18.80) | |||
| Unmarried | 5738 (79.74) | 34 (0.59) | 285 (4.97) | 808 (14.08) | |||
| Widowed or divorced | 506 (7.03) | 2 (0.40) | 36 (7.11) | 76 (15.02) | |||
| Ethnicity | .097 | .139 | <.001 | ||||
| Han | 6462 (89.80) | 40 (0.62) | 342 (5.29) | 920 (14.24) | |||
| Minorities | 734 (10.20) | 9 (1.23) | 49 (6.68) | 143 (19.48) | |||
| Residence | .406 | .192 | <.001 | ||||
| Eastern region | 3190 (44.33) | 21 (0.66) | 173 (5.42) | 440 (13.79) | |||
| Western region | 2528 (35.13) | 21 (0.83) | 125 (4.94) | 432 (17.09) | |||
| Central region | 1478 (20.54) | 7 (0.47) | 93 (6.29) | 191 (12.92) | |||
| Sexual orientation | .023 | .016 | .896 | ||||
| Homosexual | 5471 (76.03) | 30 (0.55) | 277 (5.06) | 806 (14.73) | |||
| Bisexual and unsure | 1725 (23.97) | 19 (1.10) | 114 (6.61) | 257 (14.90) | |||
| Mpox-related knowledge | .312 | <.001 | <.001 | ||||
| Low | 483 (6.71) | 3 (0.62) | 63 (13.04) | 407 (84.27) | |||
| Moderate | 597 (8.30) | 7 (1.17) | 49 (8.21) | 156 (26.13) | |||
| High | 6116 (84.99) | 39 (0.64) | 279 (4.56) | 500 (8.18) | |||
| Sexual diseases excluding HIV | <.001 | .218 | .793 | ||||
| No | 6792 (94.39) | 38 (0.56) | 375 (5.52) | 1001 (14.74) | |||
| Yes | 404 (5.61) | 11 (2.72) | 16 (3.96) | 62 (15.35) | |||
| Hepatitis C | <.001 | .174 | .011 | ||||
| No | 6662 (92.58) | 41 (0.62) | 353 (5.30) | 961 (14.43) | |||
| Unsure | 495 (6.88) | 2 (0.40) | 36 (7.27) | 96 (19.39) | |||
| Yes | 39 (0.54) | 6 (15.38) | 2 (5.13) | 6 (15.38) | |||
| Sexual risky behavior | <.001 | .062 | <.001 | ||||
| Low | 5755 (79.97) | 19 (0.33) | 296 (5.14) | 801 (13.92) | |||
| Moderate | 1388 (19.29) | 23 (1.66) | 90 (6.48) | 244 (17.58) | |||
| High | 53 (0.74) | 7 (13.21) | 5 (9.43) | 18 (33.96) | |||
The prevalence of mpox virus infection, the rate of mpox vaccination hesitation and consultation hesitation were all higher among unemployed MSM, those with an educational level of junior high school and below, and those who were married (Table 1). In addition, MSM who identified as bisexual (1.10%), those who reported having other sexual diseases (2.72%), hepatitis C (15.38%), and engaging in high-risky sexual behavior (13.21%) had a higher prevalence of mpox virus infection. Furthermore, MSM who were aged 36 years or older (7.02%), those who identified as bisexual (6.61%), and those who had low mpox-related knowledge (13.04%) had a higher rate of vaccination hesitation. It was found that MSM who were aged 36 years or older (50.76%), minorities (19.48%), those residing in the western region (17.09%), those who had low mpox-related knowledge (84.27%), those who reported unknown hepatitis C (19.39%), and those who reported engaging high-risky sexual behavior (33.96%) had a higher rate of consultation hesitation (Table 1).
Associations of HIV status with mpox virus infection, mpox vaccination hesitation and consultation hesitation for mpox
The crude prevalence of mpox virus infection was higher in the PLWH (1.04%, 20/1920), compared with PLWoH (0.55%, 29/5276) (P = .037). Compared with PLWoH, PLWH had a higher odds ratio of mpox virus infection in both univariate model 1 and model 2. However, after controlling for all covariates, HIV status was not associated with mpox virus infection (aOR = 1.17; 95%CI = 0.58, 2.39; P = .658) (Table 2). There was no significant interaction observed among subgroups in relation to the associations between HIV status and mpox virus infection (Table S1).
Table 2.
Associations of HIV status with mpox virus infection, mpox vaccination hesitation, and consultation hesitation for mpox.
| Outcomes | % (n/N) | Model 1 |
Model 2 |
Model 3 |
|||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | P-value | aOR (95% CI) | P-value | aOR (95% CI) | P-value | ||
| Mpox virus infection | |||||||
| Non-HIV | 0.55 (29/5276) | 1 (reference) | 1 (reference) | 1 (reference) | |||
| HIV | 1.04 (20/1920) | 1.90 (1.07, 3.37) | .027 | 1.90 (1.04, 3.48) | .037 | 1.17 (0.58, 2.39) | .658 |
| Mpox vaccination hesitation | |||||||
| Non-HIV | 5.91 (312/5276) | 1 (reference) | 1 (reference) | 1 (reference) | |||
| HIV | 4.11 (79/1920) | 0.68 (0.53, 0.88) | .003 | 0.64 (0.49, 0.84) | .001 | 0.70 (0.53, 0.92) | .011 |
| Consultation hesitation for mpox | |||||||
| Non-HIV | 16.22 (856/5276) | 1 (reference) | 1 (reference) | 1 (reference) | |||
| HIV | 10.78 (207/1920) | 0.62 (0.53, 0.73) | <.001 | 0.64 (0.54, 0.76) | <.001 | 0.74 (0.60, 0.90) | .003 |
Model 1 was a univariate model; model 2 adjusted age group, occupation, ethnicity, educational level, residence and marital status; based on model 2, model 3 additionally adjusted sexual orientation, mpox-related knowledge, sexual diseases excluding HIV, hepatitis C, sexual risky behavior, and other two outcomes. OR = odds ratio; 95%CI = 95% confidence interval.
The crude rate of mpox vaccination hesitation (PLWoH: 5.91%, 312/5276; PLWH: 4.11%, 79/1920; P = .004) and consultation hesitation for mpox (PLWoH: 16.22%, 856/5276; PLWH: 10.78%, 207/1920; P < .001) were both lower in the PLWH, compared with the PLWoH (Table 2). In the multivariable-adjusted analysis, after adjusting for all covariates, compared with PLWoH, PLWH had lower odds ratios of mpox vaccination hesitation (aOR = 0.70; 95%CI = 0.53, 0.92; P = .011) and consultation hesitation for mpox (aOR = 0.74; 95%CI = 0.60, 0.90; P = .003) (Table 2). Subgroup analysis showed that there was no significant interaction observed among subgroups in relation to the association between HIV status and mpox vaccination hesitation (Table S2). However, differences were observed within hepatitis C group regarding the relationship between HIV status and consultation hesitation for mpox (Figure 1). The estimated association between HIV status and consultation hesitation for mpox was found to be smaller among MSM who reported hepatitis C infection or were unsure (aOR = 0.30; 95%CI = 0.15, 0.56), compared with those without hepatitis C (aOR = 0.73; 95%CI = 0.60, 0.89) (P for interaction = .037).
Figure 1.
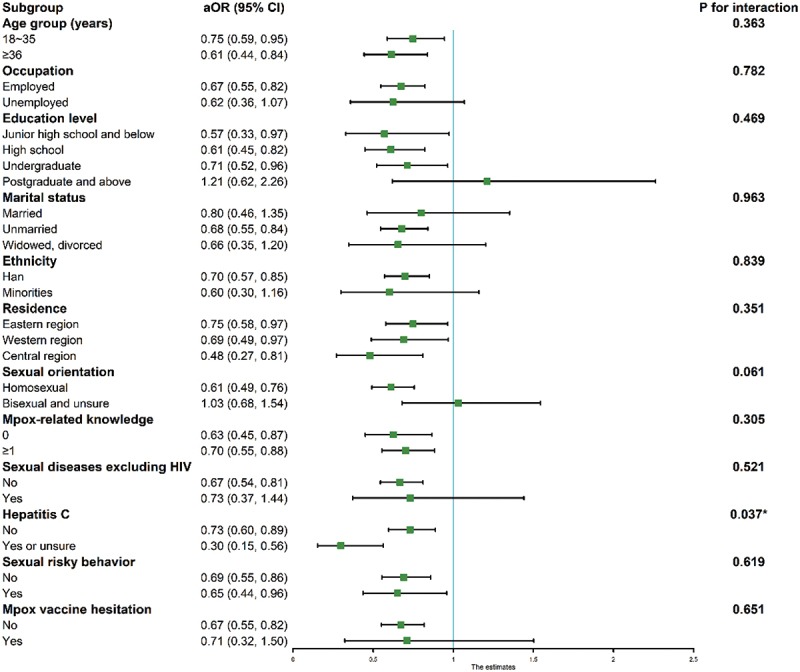
Subgroup analysis on associations between HIV status and consultation hesitation for mpox.
All models adjusted age group, occupation, ethnicity, educational level, residence, marital status, sexual orientation, mpox-related knowledge, sexual diseases excluding HIV, hepatitis C, sexual risky behavior, mpox virus infection and mpox vaccine hesitation. OR = odds ratio; 95%CI = 95% confidence interval.
Discussion
To the best of our knowledge, this study is the first to provide insights into the association between HIV status and mpox-related focus issues among MSM in China. Of 7196 MSM, we observed a higher crude prevalence of mpox virus infection in PLWH, compared with PLWoH. In contrast, the crude rate of mpox vaccination hesitation and consultation hesitation for mpox were both lower in PLWH, compared with PLWoH. However, after adjusting for all covariates, HIV status was not associated with mpox virus infection. Importantly, compared with PLWoH, PLWH had lower odds ratios of mpox vaccination hesitation and consultation hesitation for mpox.
PLWH accounted for approximately 48% of the mpox cases in the multinational outbreak between Jan 1, 2022, and Jan 29, 2023.8 HIV may increase the risk of hospitalization.8 Therefore, comprehending the HIV epidemic and its relation with mpox-related issues is crucial in order to effectively mitigate mpox epidemic. We observed a crude prevalence of mpox virus infection in the PLWH, compared with the PLWoH. However, after adjusting for all covariates, this relation was not significant. We speculated that PLWH were more likely to engage risky sexual behavior, resulting in a higher prevalence of mpox virus infection. Therefore, after controlling for other factors such as risky sexual behavior, HIV status was not associated with mpox virus infection.
Previous research has indicated that Chinese healthcare professionals have a higher acceptance rate of mpox vaccine, compared with those residing in other non-endemic countries in 2022.28 We supplemented the additional evidence regarding the differences in mpox vaccination hesitation among MSM with varying HIV status in China.28 Contrary to speculation, our findings revealed that compared with PLWoH, PLWH had a lower odds ratio of mpox vaccination hesitation. Li et al. found that PLWH expressed support for mpox vaccination promotion among MSM.29 Third-generation mpox vaccines were safer for use in immunocompromised populations.21 The vaccine effectiveness of the third-generation smallpox vaccine (MVA-BN) against mpox was 87% for one-dose vaccination and 89% for two-dose vaccination.30 The reduction of vaccination hesitancy among MSM living with can have significant benefits, such as promoting herd immunity and improving the capacity for public health emergency response in China. It was noted that development of the mpox vaccine should be continued with consideration for its applicability among PLWH. The requirement of two dose vaccines was still an impediment to rapid outbreak response.21 Furthermore, our findings indicate that PLWH were more likely to accept medical consultation for mpox, particularly those who were coinfected with hepatitis C. Medical consultation hesitancy had detrimental effects on the timely management of cases and the detection of close contacts, which are crucial in controlling the transmission of mpox. The Chinese CDC reported only 89.2% of the 491 cases were identified through proactive medical consultation.13 Approximately 69.2% of the participants agreed that media-related content about mpox contributed to the stigmatization of gay, bisexual, and other men who have sex with men in US.31 It is also important to consider the sociological perspective when addressing the treatment of infectious diseases in order to protect individuals’ privacy. Protecting individuals’ privacy and mitigating social stigma are essential factors that promote a proactive approach to seeking medical consultation. In addition, our study revealed that MSM those who lived in western region had a higher rate of consultation hesitation. The regional disparities in mpox-related issues also evident in the US.31,32 Owens et al.32 reported that rural MSM, in comparison with their urban counterparts, were less likely to report perceiving severe consequences acquiring mpox. The findings regarding regional disparities in mpox-related issues were crucial in formulating targeted interventions at the provincial level. Our study has demonstrated the necessity for hospitals to proactively prepare for prevention and control of mpox and establish a good medical environment in the future, particularly for PLWH.
The notable strength of this article was that it included a large sample size of over 7000 MSM in China. However, there were some limitations in our study. Firstly, it should be noted that the data regarding HIV status, other sexual diseases, hepatitis C, and mpox-related issues were obtained through self-reporting. This method of data collection may introduce a potential call bias. Furthermore, to ensure better comprehension among participants, we opted to use condyloma instead of HPV all-serotypes in the assessment of sexual diseases. It is noted that condyloma does not encompass all HPV-related infections or diseases. Therefore, we should investigate all HPV serotypes to thoroughly explore the relationship between other sexual diseases and mpox. In addition, it is important to acknowledge the high risk of social desirability bias that cannot be neglected because of stigma and privacy concerns. Secondly, our study did not account for other factors that may have influenced the association between HIV status and mpox virus infection, including the utilization of pre-exposure prophylaxis (PrEP) and smallpox vaccination. Thirdly, our study did not encompass the entire population of MSM in China, thus introducing a potential selection bias. However, due to the hidden nature of MSM population, the survey of MSM population based on 27 MSM social organizations can ensure the accessibility of the target population. Finally, it is important to highlight that the lack of access to the mpox vaccine in mainland China could potentially impact the rate of mpox vaccination hesitancy. Additionally, in accordance with the Mpox prevention and control program, we did not include self-assessment of mpox virus infections. However, self-assessment of infections may mean mpox infection of people who reported consultation hesitation. The actual rate of mpox virus infection may be underestimated.
In conclusion, our findings indicate that MSM living with HIV express a higher level of willingness to accept mpox vaccination and engage in medical consultation. In order to effectively curb the mpox epidemic, particularly among PLWH, it is imperative for medical institutions to establish a conducive medical environment in the future.
Supplementary Material
Acknowledgments
We appreciate the works by all authors for original data.
Funding Statement
This work was supported by the National Natural Science Foundation of China [grant numbers 72122001, 72211540398].
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are obtained according to corresponding author permission.
Ethics approval and consent to participate
The study’s design, details, and procedures were approved by the Ethics Committee of the Guizhou Center for Disease Control and Prevention (Q 2022–02). All participants had informed consent at the time of participation. The research has been performed in accordance with the Declaration of Helsinki.
Author contribution statement
MZ, GY, ML and JL conceptualized and designed the study, MD, MZ, YY, XQ, YZ, LM, RT, ZZ, FZ, SD and JY did data acquisition and data curation, MD did formal analysis, visualization and writing – original draft, JL, GY, ML and MZ did writing- reviewing and editing. All authors have seen and approved the submitted version of this manuscript.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2023.2290788.
References
- 1.Ng OT, Lee V, Marimuthu K, Vasoo S, Chan G, Lin RTP, Leo YS.. A case of imported Monkeypox in Singapore. Lancet Infect Dis. 2019;19(11):1166. doi: 10.1016/S1473-3099(19)30537-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costello V, Sowash M, Gaur A, Cardis M, Pasieka H, Wortmann G, Ramdeen S. Imported Monkeypox from international Traveler, Maryland, USA, 2021. Emerg Infect Dis. 2022;28(5):1002–7. doi: 10.3201/eid2805.220292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vaughan A, Aarons E, Astbury J, Balasegaram S, Beadsworth M, Beck CR, Chand M, O’Connor C, Dunning J, Ghebrehewet S, et al. Two cases of Monkeypox imported to the United Kingdom, September 2018. Euro Surveill. 2018;23(38):1800509. doi: 10.2807/1560-7917.ES.2018.23.38.1800509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walter K, Malani PN. What is Monkeypox? JAMA. 2022;328(2):222. doi: 10.1001/jama.2022.10259. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization . Multi-country Monkeypox outbreak: situation; 2023. Nov 3. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON393.
- 6.World Health Organization . Second meeting of the International Health Regulations (2005) (IHR) Emergency Committee regarding the multi-country outbreak of monkeypox. 2023 Nov 3. https://www.who.int/news/item/23-07-2022-second-meeting-of-the-international-health-regulations-(2005)-(ihr)-emergency-committee-regarding-the-multi-country-outbreak-of-monkeypox.
- 7.World Health Organization . Monkeypox and orthopoxvirus outbreak global map. Second meeting of the International Health Regulations (2005) (IHR) Emergency Committee regarding the multi-country outbreak of monkeypox; 2022. [2023 Nov 3]. https://www.who.int/news/item/23-07-2022-second-meeting-of-the-international-health-regulations-(2005)-(ihr)-emergency-committee-regarding-the-multi-country-outbreak-of-monkeypox. [Google Scholar]
- 8.Laurenson-Schafer H, Sklenovska N, Hoxha A, Kerr SM, Ndumbi P, Fitzner J, Almiron M, de Sousa LA, Briand S, Cenciarelli O, et al. Description of the first global outbreak of mpox: an analysis of global surveillance data. Lancet Glob Health. 2023;11(7):e1012–e1023. doi: 10.1016/S2214-109X(23)00198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Du M, Sun H, Zhang S, Yuan J, Yan W, Liu Q, Qin C, Liu M, Liu J. Global epidemiological features of human Monkeypox cases and their associations with social-economic level and international travel arrivals: a systematic review and ecological study. Int J Public Health. 2023;68:1605426. doi: 10.3389/ijph.2023.1605426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siegrist EA, Sassine J. Antivirals with activity against Mpox: a clinically oriented review. Clin Infect Dis. 2023;76(1):155–64. doi: 10.1093/cid/ciac622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stannah J, Soni N, Lam JKS, Giguère K, Mitchell KM, Kronfli N, Larmarange J, Moh R, Nouaman M, Kouamé GM, et al. Trends in HIV testing, the treatment cascade, and HIV incidence among men who have sex with men in Africa: a systematic review and meta-analysis. Lancet HIV. 2023;10(8):e528–e42. doi: 10.1016/S2352-3018(23)00111-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chinese Center for Disease Control and Prevention . Surveillance of mpox outbreak; 2023. Nov 3. https://www.chinacdc.cn/jkzt/crb/qt/szkb_13037/gwjszl_13092/202308/t20230809_268502.html.
- 13.Chinese Center for Disease Control and Prevention . Surveillance of mpox outbreak in July; 2023. Nov 3. https://www.chinacdc.cn/jkzt/crb/qt/szkb_13037/gwjszl_13092/202308/t20230809268502.html.
- 14.Zhou L, Wang Y, Li D, Han M, Shi G, Li Q. Consideration of Monkeypox surveillance in China, 2022. China CDC Wkly. 2022;4(41):924–928. doi: 10.46234/ccdcw2022.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deputy NP, Deckert J, Chard AN, Sandberg N, Moulia DL, Barkley E, Dalton AF, Sweet C, Cohn AC, Little DR, et al. Vaccine effectiveness of JYNNEOS against Mpox disease in the United States. N Engl J Med. 2023;388(26):2434–43. doi: 10.1056/NEJMoa2215201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hazra A, Zucker J, Bell E, Flores J, Gordon L, Mitjà O, Suñer C, Lemaignen A, Jamard S, Nozza S, et al. Mpox in people with past infection or a complete vaccination course: a global case series. Lancet Infect Dis. 2023;S1473-3099(23). doi: 10.1016/S1473-3099(23)00492-9. [DOI] [PubMed] [Google Scholar]
- 17.Hou F, Zhang Y, Liu X, Murad YM, Xu J, Yu Z, Hua X, Song Y, Ding J, Huang H, et al. mRNA vaccines encoding fusion proteins of monkeypox virus antigens protect mice from vaccinia virus challenge. Nat Commun. 2023. Sep 22;14(1):5925. doi: 10.1038/s41467-023-41628-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hou Z, Guo J, Lai X, Zhang H, Wang J, Hu S, Du F, Francis MR, Fang H, Hou Z, et al. Influenza vaccination hesitancy and its determinants among elderly in China: a national cross-sectional study. Vaccine. 2022;40(33):4806–4815. doi: 10.1016/j.vaccine.2022.06.063. [DOI] [PubMed] [Google Scholar]
- 19.Wang D, Wu J, Du J, Ong H, Tang B, Dozier M, Weller D, Campbell C. Acceptability of and barriers to human papillomavirus vaccination in China: a systematic review of the Chinese and English scientific literature. Eur J Cancer Care (Engl). 2022;31(3):e13566. doi: 10.1111/ecc.13566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng M, Du M, Yang G, Yao Y, Qian X, Zhi Y, Ma L, Tao R, Zhu Z, Zhou F, et al. Mpox vaccination hesitancy and its associated factors among men who have sex with men in China: a national observational study. Vaccines (Basel). 2023;11(9):1432. doi: 10.3390/vaccines11091432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poland GA, Kennedy RB, Tosh PK, Poland GA, Kennedy RB, Tosh PK. Prevention of monkeypox with vaccines: a rapid review. Lancet Infect Dis. 2022;22(12):e349–e358. doi: 10.1016/S1473-3099(22)00574-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zheng M, Qin C, Qian X, Yao Y, Liu J, Yuan Z, Ma L, Fan J, Tao R, Zhou F, et al. Knowledge and vaccination acceptance toward the human monkeypox among men who have sex with men in China. Front Public Health. 2022. Oct 25;10:997637. doi: 10.3389/fpubh.2022.997637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zheng M, Chen W, Qian X, Tao R, Ma L, Zhou F, Zhu Z, Yao Y, Yang G. Awareness of mpox-related knowledge among men who have sex with men in China. BMC Public Health. 2023;23(1):600. doi: 10.1186/s12889-023-15503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Newsum AM, Matser A, Schinkel J, van der Valk M, Brinkman K, van Eeden A, Lauw FN, Rijnders BJA, van de Laar TJW, van de Kerkhof M, et al. Incidence of HCV reinfection among HIV-Positive MSM and its association with sexual risk behavior: a longitudinal analysis. Clin Infect Dis. 2021;73(3):460–7. doi: 10.1093/cid/ciaa645. [DOI] [PubMed] [Google Scholar]
- 25.Braun DL, Marzel A, Steffens D, Schreiber PW, Grube C, Scherrer AU, Kouyos RD, Günthard HF, Anagnostopoulos A, Aubert V. High rates of subsequent asymptomatic sexually transmitted infections and risky sexual behavior in patients initially presenting with primary human immunodeficiency virus-1 infection. Clin Infect Dis. 2018;66(5):735–42. doi: 10.1093/cid/cix873. [DOI] [PubMed] [Google Scholar]
- 26.Zhang YB, Chen C, Pan XF, Guo J, Li Y, Franco OH, Liu G, Pan A. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ. 2021;373:n604. doi: 10.1136/bmj.n604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Du M, Tao L, Liu M, Liu J. Mediation of healthy behaviour on the association of Frailty with respiratory diseases mortality among 0.4 million participants: a prospective cohort study from UK biobank. Nutrients. 2022. Nov 27;14(23):5046. doi: 10.3390/nu14235046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lounis M, Riad A. Monkeypox (MPOX)-related knowledge and vaccination hesitancy in non-endemic countries: concise literature review. Vaccines (Basel). 2023;11(2):229. doi: 10.3390/vaccines11020229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li Y, Peng X, Fu L, Wang B, Sun Y, Chen Y, Lin YF, Wu X, Liu Q, Gao Y, et al. Monkeypox awareness and low vaccination hesitancy among men who have sex with men in China. J Med Virol. 2023;95(2):e28567. doi: 10.1002/jmv.28567. [DOI] [PubMed] [Google Scholar]
- 30.Xu M, Liu C, Du Z, Bai Y, Wang Z, Gao C. Real-world effectiveness of monkeypox vaccines: a systematic review. J Travel Med. 2023;30(5):taad048. doi: 10.1093/jtm/taad048. [DOI] [PubMed] [Google Scholar]
- 31.Owens C, Hubach RD. An exploratory study of the mpox media consumption, attitudes, and preferences of sexual and gender minority people assigned male at birth in the United States. LGBT Health. 2023;10(5):401–7. doi: 10.1089/lgbt.2022.0251. [DOI] [PubMed] [Google Scholar]
- 32.Owens C, Hubach RD. Rural-urban differences in monkeypox behaviors and attitudes among men who have sex with men in the United States. J Rural Health. 2023;39(2):508–15. doi: 10.1111/jrh.12726. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are obtained according to corresponding author permission.


