Since 2001 (more than twenty years ago) the Global Initiative for Obstructive Lung Disease (GOLD) publishes and updates every year a document that recommends how to best diagnose and manage chronic obstructive pulmonary disease (COPD). 1 This is an enormous and continued team effort, so we want to start by acknowledging the dedication and hard work of all GOLD members through the years (www.goldcopd.org). The GOLD 2024 document has just been released and is available for free download in the GOLD website, together with a pocket guide and a teaching slide set. 2 Here we present a brief overview of what we think are the most relevant changes (or lack of) introduced in this 2024 edition of the GOLD recommendations.
To begin with, it is worth mentioning that, to avoid potential duplications and improve readability of the document, Chapter 3 (Evidence supporting prevention and maintenance therapy) and Chapter 4 (Management of stable COPD) in the GOLD 2023 document have now been merged into a single chapter (new Chapter 3 in GOLD 2024: Prevention and Management of COPD). Besides, the GOLD Science Committee identified a number of topics that, although already discussed in GOLD 2023, required and deserved further discussion. Accordingly, the following aspects about the diagnosis or management of COPD have been expanded and updated in GOLD 2024.
DIAGNOSIS
Spirometry
GOLD 2024 continues to propose that a post-bronchodilator FEV 1 /FVC<0.7, in the appropriate clinical context, is mandatory to establish the diagnosis of COPD. 2 However, we also recognize that there is an ongoing, and not yet resolved, debate on two key aspects of this proposal. First, whether the use of the lower limit of normal (LLN) of the FEV1/FVC ratio would be better or worse than the use of the currently recommended fixed ratio <0.7. 3 As already discussed in GOLD 2023, and now expanded in GOLD 2024, both options have pros and cons. 2 For instance, subjects classified as normal using LLN criteria but obstructed or restricted using the fixed ratio have a higher risk of mortality. 4 Further, as we know that COPD can occur in young subjects, 5 and that, in them, a fixed ratio may underdiagnose patients who may need treatment. 6 , 7 Besides, whether the diagnosis of COPD has to be based on pre- or post-bronchodilator spirometric values is also controversial. In this context, it is worth noting the results of a recent analysis in the SPIROMIC cohort that shows that the presence of reversible obstruction is associated with an increased incidence of COPD over time. 8 The GOLD Science Committee will continue discussing these pro- and con- arguments in relation to this key key diagnostic tool for COPD with the goal of providing a more informed proposal in GOLD 2025.
Preserved Ratio Impaired Spirometry (PRISm)
PRISm is a spirometric pattern characterized by FEV1/FVC ≥ 0.70 and post-BD FEV1 < 80% pred. 9 The pathogenesis of PRISm is still unclear but potential causes may include cardiac disease (i.e., lung edema), initial stages of obstructive or restrictive lung disease, gas trapping and/or incomplete inspiration or expiration (insufficient cooperation). 9 , 10 Importantly, although PRISm may not be stable over time, it seems associated with an increased cardiovascular risk. 11 Clearly, as discussed in GOLD 2024, PRISm requires research to better understand its pathogenesis and to determine the best management alternatives. 2
Lung hyperinflation
This is one of the main mechanisms, if not the leading one, of dyspnea in patients with COPD. Hyperinflation can be static (at rest) or dynamic (during exercise) and has prognostic value. 12 Bronchodilator treatment benefits are likely related to pharmacological lung “deflation“. This is further discussed in detail in GOLD 2024
Interstitial lung abnormalities (ILA)
ILA are often found in patients with COPD. A new analysis in the COPDGene cohort showed that they are not always detrimental but that those ILAs associated with suspected interstitial lung disease have worse prognosis. 13
ADDRESSING UNDERDIAGNOSIS: SCREENING AND CASE FINDING
Recent data shows that 57% of 986 individuals screened for lung cancer with low dose CT in whom forced spirometry was also measured had COPD and that, importantly, 67% of them were undiagnosed (hence untreated).
MANAGEMENT OF STABLE PATIENT
Smoking cessation
The section on smoking cessation has been revised, and a new section on pharmacotherapies for smoking cessation has been added. Further, the possibility that e-cigarettes may help as a bridge for smoking cessation was revised and, based on the available evidence and the lack of knowledge about the long-term effects of e-cigarettes on respiratory health, 14 GOLD 2024 does not recommend this intervention for smoking cessation in patients with COPD.
Inhaled pharmacologic therapy
Inhaled therapy is the corner stone of pharmacologic treatment in patients with COPD. GOLD 2024 expands the discussion on how to choose the best inhaler device for a particular patient considering her/his ability to use the delivery system correctly. GOLD 2024 also discusses the potential environmental impact of different inhalers and recommend to use, whenever possible, green inhalers. 15
On the other hand, GOLD 2023 made a practical recommendation to consider initial treatment with triple therapy in E patients with more than 300 Eos/mL. Now, a recent retrospective analysis of a large, real-world database (the Clinical Practice Research Datalink) in the UK provides support for this recommendation although it has to be mentioned that this analysis was not based on randomized individuals. 16
Biologics
Previous studies of mepolizumab 17 and benralizumab 18 , 19 in COPD yielded inconclusive results. By contrast, the BOREAS study showed clear clinical effects of dupilumab in a selected subgroup of COPD patients (those with more than 300 eosinophils/mL who, despite the use of triple therapy, continue to suffer exacerbations and have symptoms of chronic bronchitis). 20 GOLD 2024 acknowledges these results pending confirmation studies. 2 If confirmed, this would finally open the possibility of using biologic therapy in patients with COPD. 21
VACCINATION
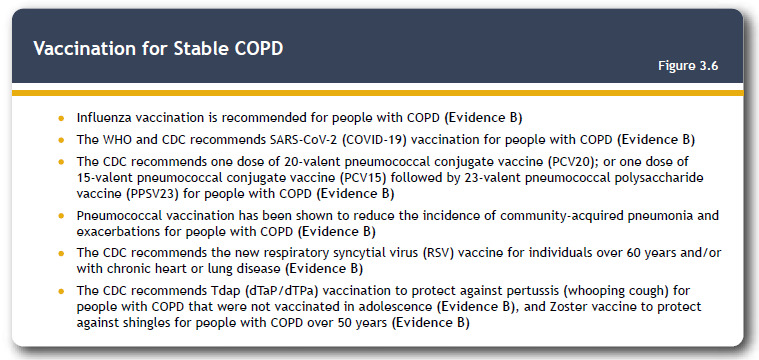
The term immunosenescence refers to the gradual deterioration of the immune system caused by advancing age. 22 It is associated with a reduced ability to respond to infections and develop long-term immune memory. 22 It plays a key role in the development of respiratory infections in the elderly, 22 particularly in patients with COPD. 23 Refraining from smoking, limiting alcohol consumption, regular exercise, appropriate diet and establishing a proper vaccination program can slow down the process of immunosenescence (immune fitness). 22 Figure 1 presents the vaccination recommendations for people with COPD, which has been updated in line with current guidance by the U.S. Centers for Disease Control (CDC). In particular, GOLD 2024 now recommends the vaccination of COPD patients with the new respiratory syncytial virus (RSV) vaccines, which are highly efficient both in the general population 24 and in older patients with cardio-respiratory comorbidities, 25 on top of those vaccines already recommended in GOLD 2023 (flu, pneumococcus, COVID-19, pertussis and shingles).
Figure 1. Vaccination for stable COPD. Reproduced from GOLD 2024 with permission. 2 .
EXACERBATIONS
Traditionally the severity of exacerbations has been determined post-hoc based on the type and site of treatment received: mild if ambulatory with minimal therapeutic changes, moderate if antibiotics and/or systemic steroids were prescribed, and severe if the patient was hospitalized. This classification have been extensively used in many clinical trials as well as to classify stable patients in the A, B, or E groups to guide their initial pharmacologic treatment. 2 It is useless, however, to guide treatment at the point of care during an actual episode of exacerbation. Because of this, GOLD 2023 adopted the Rome proposal for the definition and assessment of severity of the episodes of exacerbation of COPD at the point of care based on a number of physiological biomarkers independently of the type or site of treatment. 26 GOLD 2024 continues to propose the use of the Rome classification to guide the treatment of the actual exacerbation episode but discusses (and hopefully clarifies) several aspects that deserve consideration: 1. it is necessary to separate the physiological classification of exacerbations (Rome proposal), intended to guide treatment at the point of care, from the site of care (outpatient, inpatient), which may be dictated by the clinical severity of the exacerbation but also by the structure of different health systems, availability of resources and/or personal/social conditions (e.g., living alone, comorbidities). In fact, GOLD 2024 now discusses several retrospective studies that confirm the validity of the Rome proposal to predict mortality but also showed that a substantial proportion of hospitalized patients had, according to Rome, mild exacerbations 27 , 28 ; 2. the classification of the stable patient in the A, B or E groups to guide initial pharmacologic treatment must still rely (by necessity) on the history recall of previous exacerbations which will have to be classified as moderate or severe by the site and type of treatment received.
CONCLUSIONS
As discussed above, the GOLD 2024 document discusses relevant aspects for the diagnosis, prevention, and management of COPD. Like GOLD has done over the last two decades, 1 it will continue to provide the different stakeholders interested in COPD, including patients, practicing clinicians and other health care professionals, basic science investigators, epidemiologists, pharma industry and payers, with the most updated and critically reviewed evidence on a yearly basis in order to improve the care for COPD patients and the distant goal of eventually eliminate COPD. 29
ACKNOWLEDGMENTS
The authors acknowledge the work of Katie Lagerfeld (GOLD program Director) and Ruth Hadfield (medical writer) for their continued work to make possible the publication of the GOLD document every year.
REFERENCES
- 1.Rodriguez-Roisin R, Rabe KF, Vestbo J, Vogelmeier C, Agustí A. all previous and current members of the Science Committee and the Board of Directors of GOLD Global Initiative for Chronic Obstructive Lung Disease (GOLD) 20th Anniversary a brief history of time. Eur Respir J. 2017;50(1):1700671–1700671. doi: 10.1183/13993003.00671-2017. [DOI] [PubMed] [Google Scholar]
- 2.Global Initiative for Chronic Obstructive Lung Disease (GOLD) Global Strategy for Prevention, Diagnosis and Management of COPD: 2024 Report. Bethesda: GOLD; https://goldcopd.org/2024-gold-report [Google Scholar]
- 3.Mannino DM, Sonia Buist A, Vollmer WM. Chronic obstructive pulmonary disease in the older adult: what defines abnormal lung function? Thorax. 2007;62(3):237–241. doi: 10.1136/thx.2006.068379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mannino DM, Diaz-Guzman E. Interpreting lung function data using 80% predicted and fixed thresholds identifies patients at increased risk of mortality. Chest. 2012;141(1):73–80. doi: 10.1378/chest.11-0797. [DOI] [PubMed] [Google Scholar]
- 5.Martinez FJ, Agusti A, Celli BR, Han MK, Allinson JP, Bhatt SP. Treatment Trials in Young Patients with Chronic Obstructive Pulmonary Disease and Pre-Chronic Obstructive Pulmonary Disease Patients Time to Move Forward. Am J Respir Crit Care Med. 2022;205(3):275–287. doi: 10.1164/rccm.202107-1663SO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller MR, Quanjer PH, Swanney MP, Ruppel G, Enright PL. Interpreting lung function data using 80% predicted and fixed thresholds misclassifies more than 20% of patients [published correction appears in. Chest. 2011;139(3):733–733. doi: 10.1378/chest.10-0189. [DOI] [PubMed] [Google Scholar]
- 7.Bhatt SP, Sieren JC, Dransfield MT, Washko GR, Newell JD, Jr, Stinson DS. Comparison of spirometric thresholds in diagnosing smoking-related airflow obstruction. Thorax. 2014;69(5):409–414. doi: 10.1136/thoraxjnl-2012-202810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buhr RG, Barjaktarevic IZ, Quibrera PM, Bateman LA, Bleecker ER, Couper DJ. Reversible Airflow Obstruction Predicts Future Chronic Obstructive Pulmonary Disease Development in the SPIROMICS Cohort An Observational Cohort Study. Am J Respir Crit Care Med. 2022;206(5):554–562. doi: 10.1164/rccm.202201-0094OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wan ES. The Clinical Spectrum of PRISm. Am J Respir Crit Care Med. 2022;206(5):524–525. doi: 10.1164/rccm.202205-0965ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perez-Padilla R, Montes de Oca M, Thirion-Romero I, Wehrmeister FC, Lopez MV, Valdivia G, et al. Trajectories of Spirometric Patterns, Obstructive and PRISm, in a Population-Based Cohort in Latin America. Int J Chron Obstruct Pulmon Dis. 2023;18:1277–1285. doi: 10.2147/COPD.S406208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wan ES, Balte P, Schwartz JE, Bhatt SP, Cassano PA, Couper D. Association Between Preserved Ratio Impaired Spirometry and Clinical Outcomes in US Adults [published correction appears in. JAMA. 2022;327(3):286–286. doi: 10.1001/jama.2021.20939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Casanova C, Cote C, de Torres JP, Aguirre-Jaime A, Marin JM, Pinto-Plata V. Inspiratory-to-total lung capacity ratio predicts mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;171(6):591–597. doi: 10.1164/rccm.200407-867OC. [DOI] [PubMed] [Google Scholar]
- 13.Rose JA, Menon AA, Hino T, Hata A, Nishino M, Lynch DA. Suspected Interstitial Lung Disease in COPDGene Study. Am J Respir Crit Care Med. 2023;207(1):60–68. doi: 10.1164/rccm.202203-0550OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xie W, Kathuria H, Galiatsatos P, Blaha MJ, Hamburg NM, Robertson RM. Association of Electronic Cigarette Use With Incident Respiratory Conditions Among US Adults From 2013 to 2018. JAMA Netw Open. 2020;3(11):e2020816. doi: 10.1001/jamanetworkopen.2020.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pernigotti D, Stonham C, Panigone S, Sandri F, Ferri R, Unal Y. Reducing carbon footprint of inhalers analysis of climate and clinical implications of different scenarios in five European countries. BMJ Open Respir Res. 2021;8(1):e001071. doi: 10.1136/bmjresp-2021-001071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suissa S. Single-inhaler triple versus dual bronchodilator therapy for GOLD group E and other exacerbating patients with COPD real-world comparative effectiveness and safety. Eur Respir J. 2023;62(3):2300883–2300883. doi: 10.1183/13993003.00883-2023. [DOI] [PubMed] [Google Scholar]
- 17.Pavord ID, Chanez P, Criner GJ, Kerstjens HAM, Korn S, Lugogo N. Mepolizumab for Eosinophilic Chronic Obstructive Pulmonary Disease. N Engl J Med. 2017;377(17):1613–1629. doi: 10.1056/NEJMoa1708208. [DOI] [PubMed] [Google Scholar]
- 18.Brightling CE, Bleecker ER, Panettieri RA, Jr, Bafadhel M, She D, Ward CK. Benralizumab for chronic obstructive pulmonary disease and sputum eosinophilia a randomised, double-blind, placebo-controlled, phase 2a study. Lancet Respir Med. 2014;2(11):891–901. doi: 10.1016/S2213-2600(14)70187-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Criner GJ, Celli BR, Brightling CE, Agusti A, Papi A, Singh D. Benralizumab for the Prevention of COPD Exacerbations. N Engl J Med. 2019;381(11):1023–1034. doi: 10.1056/NEJMoa1905248. [DOI] [PubMed] [Google Scholar]
- 20.Bhatt SP, Rabe KF, Hanania NA, Vogelmeier CF, Cole J, Bafadhel M. Dupilumab for COPD with Type 2 Inflammation Indicated by Eosinophil Counts. N Engl J Med. 2023;389(3):205–214. doi: 10.1056/NEJMoa2303951. [DOI] [PubMed] [Google Scholar]
- 21.Agusti A. Biologics for COPD - Finally Here. N Engl J Med. 2023;389(3):274–275. doi: 10.1056/NEJMe2305752. [DOI] [PubMed] [Google Scholar]
- 22.Villar-Álvarez F, de la Rosa-Carrillo D, Fariñas-Guerrero F, Jiménez-Ruiz CA. Immunosenescence, Immune Fitness and Vaccination Schedule in the Adult Respiratory Patient. Open Respir Arch. 2022;4(3):100181–100181. doi: 10.1016/j.opresp.2022.100181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Faner R, Cruz T, Agusti A. Immune response in chronic obstructive pulmonary disease. Expert Rev Clin Immunol. 2013;9(9):821–833. doi: 10.1586/1744666X.2013.828875. [DOI] [PubMed] [Google Scholar]
- 24.Papi A, Ison MG, Langley JM, Lee DG, Leroux-Roels I, Martinon-Torres F. Respiratory Syncytial Virus Prefusion F Protein Vaccine in Older Adults. N Engl J Med. 2023;388(7):595–608. doi: 10.1056/NEJMoa2209604. [DOI] [PubMed] [Google Scholar]
- 25.Feldman RG, Antonelli-Incalzi R, Steenackers K, Lee DG, Papi A, Ison MG, et al. Respiratory Syncytial Virus Prefusion F Protein Vaccine Is Efficacious in Older Adults With Underlying Medical Conditions [published online ahead of print, 2023 Sep 12] Clin Infect Dis. 2023:ciad471–ciad471. doi: 10.1093/cid/ciad471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Celli BR, Fabbri LM, Aaron SD, Agusti A, Brook R, Criner GJ. An Updated Definition and Severity Classification of Chronic Obstructive Pulmonary Disease Exacerbations The Rome Proposal. Am J Respir Crit Care Med. 2021;204(11):1251–1258. doi: 10.1164/rccm.202108-1819PP. [DOI] [PubMed] [Google Scholar]
- 27.Crisafulli E, Sartori G, Huerta A, Gabarrús A, Fantin A, Soler N, et al. Association Between Rome Classification Among Hospitalized Patients With COPD Exacerbations and Short-Term and Intermediate-Term Outcomes [published online ahead of print, 2023 Jul 27] Chest. 2023 doi: 10.1016/j.chest.2023.07.021. [DOI] [PubMed] [Google Scholar]
- 28.Reumkens C, Endres A, Simons SO, Savelkoul PHM, Sprooten RTM, Franssen FME. Application of the Rome severity classification of COPD exacerbations in a real-world cohort of hospitalised patients. ERJ Open Res. 2023;9(3):00569–02022. doi: 10.1183/23120541.00569-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stolz D, Mkorombindo T, Schumann DM, Agusti A, Ash SY, Bafadhel M. Towards the elimination of chronic obstructive pulmonary disease a Lancet Commission. Lancet. 2022;400(10356):921–972. doi: 10.1016/S0140-6736(22)01273-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


