ABSTRACT
BACKGROUND
Delirium is the most commonly experienced disorder in consultation liaisons. There are currently research and guidelines in Japan for delirium treatment. Still, there is no retrospective observational study of consultation-liaison psychiatry (CLP) and antipsychotic-centered drugs. This study aims to examine CLP’s effectiveness and drug treatment.
METHODS
Using a Japanese national inpatient database of 2016 and 2017, we investigated the presence or absence of CLP for the treatment of delirium in postoperative delirium patients, the status of drug selection, delirium days, and the average days from surgery to discharge. We examined factors affecting days from surgery to discharge using multiple linear regression analysis.
RESULTS
This study was classified into a CLP group (n = 1,142) and a non-CLP group (n = 11,355). The days from surgery to discharge in the CLP and non-CLP groups was 16.7 and 17.1, respectively (p = 0.3613). There was a significant difference in the delirium days between the CLP and non-CLP groups (8.9 vs. 7.4; p < 0.00001). Haloperidol infusion was frequently used between the days from surgery to first day of delirium. It was prescribed less often than other oral drugs. Multiple regression analysis identified an association between age, men, CCI1-2, CCI ≥3, number of drugs used, days from surgery to first day of delirium, and early CLP (0–2days) with days from surgery to discharge.
CONCLUSIONS
We investigated the effectiveness of CLP and the actual conditions of pharmacotherapy for postoperative delirium. Our findings suggest that early CLP may be associated with shorter days from surgery to discharge.
Keywords: postoperative delirium, administrative database, consultation-liaison psychiatry, antipsychotic drugs
INTRODUCTION
The current health care environment’s increased focus on the quality of care has resulted in a need for consultation-liaison psychiatry (CLP) to better demonstrate their effectiveness in mental health care for medical and surgical patients. Given that the prevalence of psychiatric disorders in general hospitals ranges from 20–40% [1], data on CLP care outcomes are needed to justify resources and access to CLP services within general hospital settings [2]. A recognized outcome measure for CLP quality is length of hospital stay. Previous studies have explored the association between length of stay (LOS) and timing of CLP referral in hospital. In a systematic review of studies measuring CLP effectiveness, Wood and Wand [3] identified 5 studies examining the relationship between LOS and timing of referral to CLP. A total of 4 studies in the systemic review demonstrated a positive correlation between the time of referral to CLP and LOS [2, 4–8].
The prevalence of postoperative delirium varies from 15 to 53% in older individuals depending on the settings and populations. Although delirium tends to be underdiagnosed, early recognition and intervention can prevent the development and progress of the disease [9]. Numerous studies are exploring the risk factors of delirium, including contributing factors such as old age, cerebral infarction history, cognitive decline, inducers including changes in the environment and sensory blockage caused by hospitalization, and direct factors such as deterioration from physical disease and drug use [10]. For delirium, the treatment primarily focuses on the identification and elimination of underlying causes such as the treatment of physical conditions and discontinuing or changing prescription drugs. However, severe reactions such as violence against staff and the self-extraction of intravenous drips require immediate drug therapy as part of the continuing treatment of physical conditions [11].
Standard treatment for delirium is administering antipsychotic drugs in conjunction with investigating and eliminating the cause of delirium. Haloperidol infusion was the primary treatment method in the past. At present, non-typical antipsychotic drugs are used exclusively for oral administration because of their higher tolerability and decreased risk of extrapyramidal symptoms [12]. However, the primary medication for delirium is antipsychotic drugs. Depending on the dosage, the risk of falling, aspiration, or the mortality rate increases [13].
There are many research papers on the cause of delirium onset and its treatment. However, no research compares detailed data such as patient background, primary diagnoses, drugs used, and CLP or analysis using a national in-patient database in Japan. This study aimed to determine the actual status of drug therapy for postoperative delirium and CLP effectiveness. If this study leads to CLP’s effectiveness, such as reducing LOS, it will most likely reduce medical expenses.
METHODS
DATA SOURCE
The Diagnosis Procedure Combination (DPC) database is a national inpatient database in Japan that includes administrative claims data and detailed patient data. As of 2016 and 2017, the database included approximately 7 million inpatients from more than 1,000 hospitals in Japan, representing around 50% of all acute care inpatient admissions. The database consists of the following information: unique hospital identifiers, age and gender, primary diagnoses, and comorbidities present on admission. It also includes complications that occurred after admission recorded with text data in Japanese and using ICD-10 [14] codes, procedures, and discharge status. The responsible physicians are obliged to register the diagnoses referring to medical charts on discharge. For primary diagnosis, the physicians must enter only one ICD code [14].
The Ethical Committee, Faculty of Medicine, The University of Tokyo - Medical and Dental approved this study (approval No. M2000-788-09). Because the data was anonymous, informed consent was not required.
PARTICIPANT SELECTION AND DATA
In this study, in patients aged 20 years or older who underwent one inpatient surgery under general anesthesia in the general ward, postoperative delirium developed within seven days after surgery, according to the DPC survey data for fiscal 2016 and 2017. A receipt code for closed-circulation general anesthesia and surgery (excluding blood transfusion) was extracted using the receipt computer processing system of the Ministry of Health, Labor, and Welfare. The study extracted patients using CLP for the first time after onset. The study also excluded cases of an antipsychotic or antidepressant before delirium to exclude cases such as mental disorders, dementia, and schizophrenia. The study also excluded cases of death discharge (CLP group n = 310, non-CLP group n = 247) and transfer (CLP group n = 5,002, non-CLP group n = 1,656) to assess the treatment effectiveness.
We examined the following target patient background factors: gender, age, the Charlson Comorbidity Index (hence referred to as “CCI” [15]), which evaluates the severity of patients and predicts mortality by classifying or weighting comorbidities to assess disease burden and case mix, primary diagnoses, and length of hospital stay and days from surgery to discharge.
The Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), defines delirium as a disturbance of attention or awareness accompanied by a change in baseline cognition unexplained by a preexisting or evolving neurocognitive disorder [16]. In previous Japanese studies concerning delirium and dementia, 28.7% of all patients with schizophrenia diagnosis had this co-diagnosis [17]. The elderly with Alzheimer’s disease received powerful antipsychotics [18, 19]. For this reason, it is challenging to extract drug treatment for patients with postoperative delirium from this diagnosis. Although a formal cognitive assessment and history of acute onset of symptoms are necessary for the delirium diagnosis, we used the daily nursing necessity score nurses enter every day by identifying patients who, after having surgery, exhibited either dangerous behavior or misunderstood nursing instructions for the first time [20]. This study extracted cases with no problem with both dangerous behavior and misunderstood nursing instructions before surgery. Therefore, changes in score for either dangerous behavior or misunderstood nursing instructions include acute consciousness disturbances and cognitive function deterioration. We defined this as postoperative delirium. We also defined cases with no problem with both dangerous behavior and misunderstood nursing instructions as having delirium cured. In short, we used the last day of symptoms to specify the maximum days of delirium.
We defined CLP as receiving psychotherapy. It is a system of procedure codes for ‘inpatient psychotherapy’ coded using the Japanese Procedure Codes defines under the fee schedule of the national health insurance system. We defined early CLP as 0 to 2 days, and late CLP as 3 to 5 days from surgery to first day of psychiatric intervention. Also, cases in which five or more drugs were prescribed (n = 158), or in which delirium continued for 30 days or more after surgery (n = 8,063), were excluded for outliers and to avoided sampling bias.
For drug treatment, we obtained data regarding the total number, proportion, first day of prescription, prescription day, and dose of each drug within 1 week after delirium, each drug in both the CLP and non-CLP. We used median and quartile for the dose of each drug because there are disproportionate numbers. Moreover, we excluded cases prescribed antipsychotic drugs before postoperative delirium and prescription at discharge.
STATISTICAL ANALYSES
Continuous variables were expressed as mean ± SD, depending on the overall variable distribution. We defined categorical variables proportions for each CLP and non-CLP group. We obtained descriptive statistics for the study cohort. We conducted a comparison of consecutive values of two groups (such as age) without correspondence (Mann-Whitney U test), a comparison of categorical values of two groups (such as sex) with correspondence (Fisher’s exact test). This study examines the relationship of delirium days, the number of drugs used, and the time of referral to CLP to compare multiples (Steel-Dwass Tests).
To consider the confounding factors for days from surgery to discharge, we examined the following covariates: age, sex, CCI, days from surgery to first day of delirium, number of drugs used, and CLP. We based the inclusion of variables in the model on existing knowledge of risk factors for LOS. We divided days from surgery to first day of delirium into three categories (0–1, 2–3, or 3–4 days). We divided the number of drugs used into two categories (1–2, 3–4). These covariates mentioned above were conducted in the multiple linear regression model by the least squares method.
To consider the confounding factors for delirium days, we examined the following covariates: age, sex, CCI, days from surgery to first day of delirium, CLP, number of drugs used. We divided days from surgery to first day of delirium into three categories (0–1, 2–3, or 3–4 days). We divide number of drugs used into two categories so that the variable interval may not be equivalent (1–2, 3–4). We based the inclusion of variables in the model on existing knowledge of risk factors for delirium days. These covariates mentioned above were conducted in the multiple linear regression model by the least squares method.
All methods were two-sided, and we set the significance level at 0.05. We used JMP Pro 15 software.
RESULTS
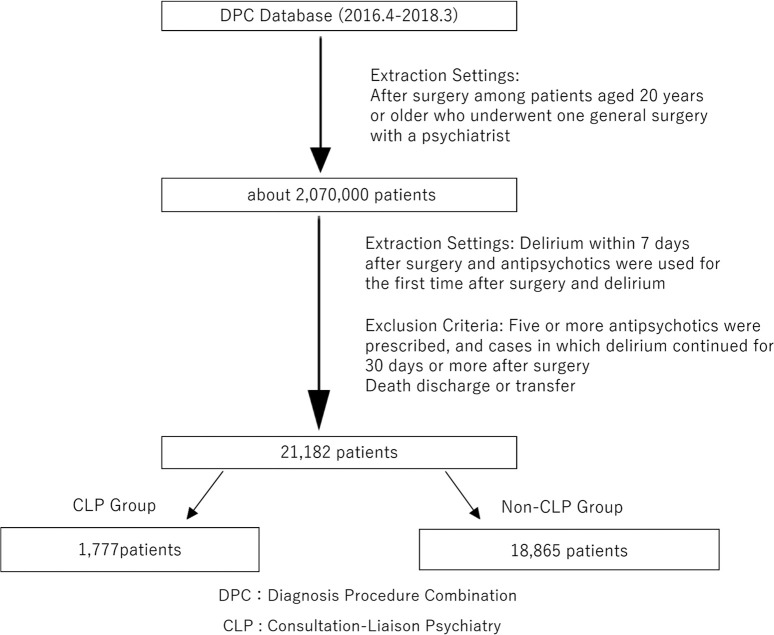
This study was classified into a CLP group (n = 1,777) and a non-CLP group (n = 18,865) after delirium onset (Fig. 1). In 20,642 patients, the average age was 75.8, with a male proportion of 61.5%. 88.1% of patients were 65 years of age or older. For CCI, 0 was 16.8%, 1–2 42.7%, and ≥3 40.4%. Table 1 shows the clinical background of each of the CLP /non-CLP groups. There were significant differences in mean age, percentage of male patients, patients over 65, and CCI in the CLP and non-CLP.
Fig. 1 . Flow diagram of the study.
DPC: Diagnosis Procedure Combination. CLP: Consultation-Liaison Psychiatry
Table 1. Demographic and Clinical Characteristics.
| All Patients (n = 20,642) | CLP Group (n = 1,777) | Non-CLP Group (n = 18,865) | p-value | |
|---|---|---|---|---|
| Age (years), mean, (SD) | 75.8 (11.5) | 74.6 (13.0) | 75.9 (11.4) | 0.0077 |
| Men (%) | 61.5% | 55.7% | 62.1% | <0.0001 |
| The Aged† (%) | 88.1% | 84.8% | 88.4% | <0.0001 |
| Charlson Comorbidity Index (%) | ||||
| 0 | 16.8% | 20.8% | 16.4% | <0.0001 |
| 1–2 | 42.7% | 43.0% | 42.7% | |
| ≥3 | 40.4% | 36.2% | 40.8% | |
| ICD-10codes (%) | ||||
| C (Cancer) | 43.4% | 41.6% | 45.3% | 0.1148 |
| K (Digestive Diseases) | 16.4% | 16.4% | 16.4% | 1.0000 |
| I (Cardiovascular Diseases) | 14.7% | 7.8% | 15.4% | <0.0001 |
| S (Trauma) | 7.2% | 8.9% | 7.0% | 0.0045 |
| M (Joint Diseases) | 7.3% | 13.1% | 6.8% | <0.0001 |
| Hospital Length of Stay, mean (SD) | 22.5 (17.3) | 20.3 (13.2) | 22.7 (17.3) | <0.0001 |
| Days from Surgery to Discharge, mean (SD) | 17.1 (15.1) | 16.7 (13.1) | 17.1 (15.3) | 0.3613 |
| Delirium Days, mean (SD) | 7.6 (6.1) | 8.9 (6.3) | 7.4 (6.0) | <0.0001 |
| Number of Drugs Used, mean (SD) | 1.4 (0.7) | 2.0 (0.9) | 1.3 (0.6) | <0.0001 |
| Days from Surgery to First Day of Delirium, mean (SD) | 1.7 (1.5) | 1.7 (1.5) | 1.7 (1.5) | 0.1089 |
| Maximum Days of Delirium, mean (SD) | 8.2 (6.2) | 9.5 (6.4) | 8.1 (6.1) | <0.0001 |
| First Day of Psychiatric Intervention, mean (SD) | 2.9 (1.8) | |||
| Number of Days from Onset Until First Intervention, mean (SD) | 1.2 (1.3) |
† ≥65-year-old
CLP: Consultation-Liaison Psychiatry.
Mann-Whitney U test: Age, Hospital Length of Stay, Days from surgery to discharge, Delirium Days, Number of Drugs Used, First Day of Delirium, Maximum Days of Delirium.
Fisher’s exact test: sex, The aged, CCI, ICD-10codes.
The primary diagnoses included cancer(C00–C97) (43.4%), digestive diseases(K00–K93) (16.4%), cardiovascular diseases(I00–I99) (14.7%), trauma(S00–S99) (7.2%) and joint diseases (M00–M99) (7.3%). In the CLP and non-CLP groups, we found differences in the primary diagnoses. There were significant differences in trauma, cardiovascular, and joint diseases, but not cancer and digestive diseases (Table 1).
The average length of hospital stays in all 20,642 patients was 22.5 days. Days from surgery to discharge was 17.1 days. The days from surgery to first day of delirium was 1.7 days after surgery. The total number of delirium days was 7.6 days. Although the non-CLP group had significantly fewer delirium days than the consultation-liaison psychiatry group (p < 0.0001), there were no significant difference in days from surgery to discharge (Table 1).
There were no patients in which no drug treatment after postoperative delirium. Table 2 showed drug treatment as each. Haloperidol infusion was frequently used on the days from surgery to first day of delirium and prescribed fewer days often than other oral drugs. The average number of drugs used for postoperative delirium patients was 1.4 in all cases. Still, there was a significant difference in the number of drugs used between the CLP and non-CLP groups (2.0 vs. 1.3; p < 0.00001) (Table 1). Among psychiatric medications used, the CLP group used antidepressants and almost antipsychotic drugs more frequently than the non-CLP group (Table 2).
Table 2. Drug Treatment for Postoperative Delirium.
| CLP Group (n = 1,777) | Non-CLP Group (n = 18,865) | p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | First Day of Prescription, mean (SD) | Prescription Days, mean (SD) | n | % | First Day of Prescription, mean (SD) | Prescription Days, mean (SD) | ||
| Haloperidol Infuison | 1035 | 58.2% | 1.7 (1.8) | 2.0 (1.8) | 12291 | 65.2% | 1.7 (2.3) | 1.6 (1.4) | <0.0001 |
| Risperidone | 845 | 47.6% | 2.9 (3.1) | 5.4 (9.8) | 5655 | 30.0% | 3.2 (4.6) | 3.1 (5.2) | <0.0001 |
| Quetiapine | 650 | 36.6% | 3.2 (3.5) | 7.5 (9.8) | 2204 | 11.7% | 3.6 (4.8) | 5.7 (8.2) | <0.0001 |
| Trazodone | 446 | 25.1% | 3.6 (3.8) | 5.7 (8.0) | 1624 | 8.6% | 4.4 (6.7) | 5.4 (8.3) | <0.0001 |
| Perospirone | 118 | 6.6% | 3.1 (2.4) | 5.1 (5.9) | 247 | 1.3% | 3.6 (5.3) | 4.3 (7.3) | <0.0001 |
| Olanzapine | 95 | 5.3% | 3.7 (7.7) | 9.0 (11.6) | 297 | 1.6% | 5.1 (7.5) | 7.4 (10.7) | <0.0001 |
| Mianserin | 77 | 4.3% | 4.8 (8.0) | 5.6 (7.1) | 330 | 1.7% | 4.5 (7.1) | 6.0 (9.1) | <0.0001 |
| Valproic Acid | 73 | 4.1% | 3.3 (4.2) | 7.8 (8.5) | 714 | 3.8% | 3.7 (6.8) | 7.9 (10.3) | 0.4340 |
| Tiapride | 49 | 2.8% | 4.4 (4.3) | 8.0 (8.6) | 410 | 2.2% | 4.3 (6.8) | 5.4 (6.6) | 0.0908 |
| Aripiprazole | 44 | 2.5% | 3.6 (6.4) | 9.7 (10.9) | 215 | 1.1% | 3.7 (6.0) | 7.0 (9.7) | <0.0001 |
| Clorpromazine | 34 | 1.9% | 5.0 (6.8) | 5.8 (9.0) | 250 | 1.3% | 6.2 (9.3) | 4.1 (6.4) | 0.0411 |
| Levomepromazine | 34 | 1.9% | 5.2 (7.0) | 5.7 (6.5) | 194 | 1.0% | 3.6 (5.0) | 6.1 (8.4) | 0.0012 |
| Haloperidol | 29 | 1.6% | 2.2 (3.1) | 8.5 (9.0) | 225 | 1.2% | 4.3 (6.9) | 5.8 (13.0) | 0.1114 |
| Clorpromazine Infusion | 28 | 1.6% | 2.1 (1.6) | 3.0 (4.1) | 571 | 3.0% | 0.8 (2.0) | 1.3 (1.0) | 0.0003 |
| Blonanserin | 18 | 1.0% | 2 (2.4) | 11.3 (9.6) | 41 | 0.2% | 5.1 (7.1) | 5.6 (4.9) | <0.0001 |
| Levomepromazine Infusion | 4 | 0.2% | 2.8 (1.7) | 1 (0) | 24 | 0.1% | 3.0 (2.3) | 1.3 (0.4) | 0.2939 |
CLP: Consultation-Liaison Psychiatry.
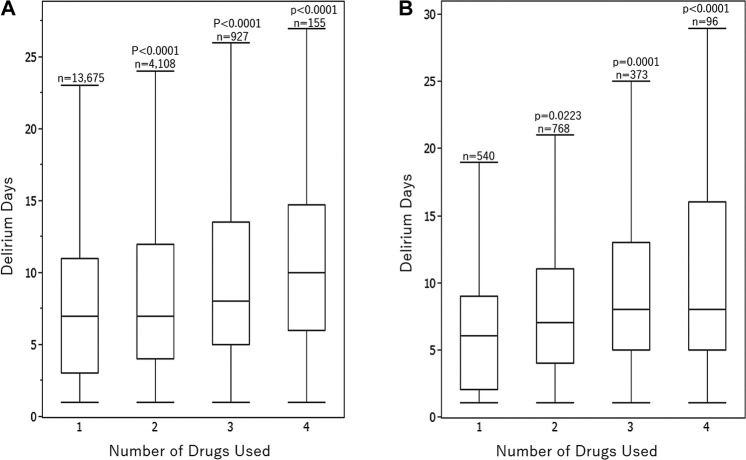
In 1,777 patients who received CLP, the first day of CLP was 2.9 days after surgery, and the number of days from onset until the first CLP was 1.2 days (Table 1). Patients with early CLP had a shorter period of delirium (Fig. 2). The longer delirium days, the more drugs use substantially, in both the CLP and non-CLP groups (Fig. 3). Fig. 3 showed A the box plot in the non-CLP group and B the box plot in the CLP group.
Fig. 2 . Box plot for the time of referral to CLP and delirium days.
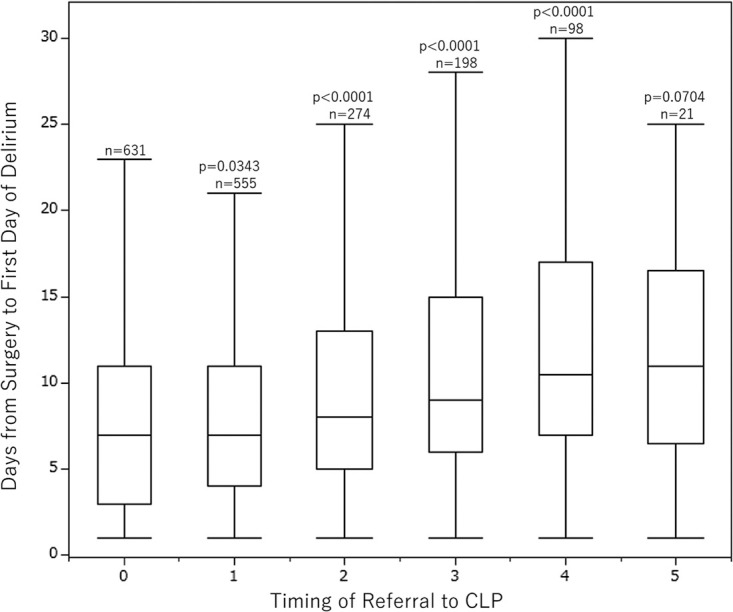
The Steel-Dwass test was performed, and the control group was 0. CLP: Consultation-Liaison Psychiatry
Fig. 3 . Box plot for the number of drugs used and delirium days in the CLP and non-CLP group.
(A) the box plot in the non-CLP group. (B) the box plot in the CLP group. The Steel-Dwass test was performed, and the control group was 1.
Table 3 showed factors associated with days from surgery to discharge. Multiple regression analysis identified a significant association between age(β = −0.026; 95% CI, −0.052 to −0.016; p = 0.0002), men (β = −0.033; 95% CI, −0.732 to −0.306; p < 0.0001), CCI 1–2 (β = 0.050; 95% CI; 0.939 to 2.114; p < 0.0001), CCI ≥3 (β = 0.095; 95% CI, 2.312 to 3.514; p < 0.0001), number of drug used 3–4 (β = 0.039; 95% CI, 1.446 to 3.016; p < 0.0001), days from surgery to first day of delirium 2–3 (β = 0.090; 95% CI; 2.490 to 3.397; p < 0.0001), days from surgery to first day of delirium 4–6 (β = 0.175; 95% CI; 7.123 to 8.363; p < 0.0001), and early CLP(β = −0.019; 95% CI, −1.942 to −0.330; p = 0.0057) with days from surgery to discharge. There was no significant association for late CLP(β = 0.002; 95% CI, −1.447 to 1.856; p = 0.9069) with days from surgery to discharge.
Table 3. Multiple Regression Analysis for Days from Surgery to Discharge (n = 20,642).
| Variables | Partial Regression Coefficient (B) | Standardized Coefficient (β) | 95% Confidence Intervals | p-value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Age (continuous variable) | −0.034 | −0.026 | −0.052 | −0.016 | 0.0002 |
| Men | −0.519 | −0.033 | −0.732 | −0.306 | <0.0001 |
| Charlson Comorbidity Index | |||||
| 0 (reference) | |||||
| 1–2 | 1.526 | 0.050 | 0.939 | 2.114 | <0.0001 |
| ≥3 | 2.913 | 0.095 | 2.312 | 3.514 | <0.0001 |
| Number of Drugs Used | |||||
| 1–2 (reference) | |||||
| 3–4 | 2.231 | 0.039 | 1.446 | 3.016 | <0.0001 |
| Days from Surgery to First Day of Delirium | |||||
| 0–1 (reference) | |||||
| 2–3 | 2.943 | 0.090 | 2.490 | 3.397 | <0.0001 |
| 4–6 | 7.744 | 0.175 | 7.123 | 8.363 | <0.0001 |
| Consultation-Liaison Psychiatry | |||||
| None (reference) | |||||
| Early (0–2 days) | −1.136 | −0.019 | −1.942 | −0.330 | 0.0057 |
| Late (3–5 days) | 0.205 | 0.002 | −1.447 | 1.856 | 0.9069 |
Table 4 showed factors associated with delirium days. Multiple regression analysis identified a significant association between age(β = 0.147; 95% CI, −0.052 to −0.016; p = 0.0002), men (β = −0.042, 95% CI, −0.346 to −0.175; p < 0.0001), CCI 1–2 (β = 0.026; 95% CI, 0.086 to 0.557; p = 0.0075), number of drug used 3–4 (β = 0.098; 95% CI, 1.937 to 2.567; p < 0.0001), days from surgery to first day of delirium 2–3 (β = −0.051; 95% CI, −0.852 to −0.488; p < 0.0001), days from surgery to first day of delirium 4–6 (β = −0.036; 95% CI, −0.898 to −0.401; p < 0.0001), early CLP(β = 0.024; 95% CI, 0.235 to 0.881; p < 0.0007) and late CLP(β = 0.064; 95% CI, 2.507 to 3.831; p < 0.0001) with delirium days. There was no significant association for CCI ≥3 (β = 0.004; 95% CI, 0.188 to 0.294; p = 0.6649) with delirium days.
Table 4. Multiple Regression Analysis for Delirium Days (n = 20,642).
| Variables | Partial Regression Coefficient (B) | Standardized Coefficient (β) | 95% Confidence Intervals | p-value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Age (continuous variable) | 0.077 | 0.147 | 0.070 | 0.084 | <0.0001 |
| Men | −0.261 | −0.042 | −0.346 | −0.175 | <0.0001 |
| Charlson Comorbidity Index | |||||
| 0 (reference) | |||||
| 1–2 | 0.321 | 0.026 | 0.086 | 0.557 | 0.0075 |
| ≥3 | 0.053 | 0.004 | 0.188 | 0.294 | 0.6649 |
| Number of Drugs Used | |||||
| 1–2 (reference) | |||||
| 3–4 | 2.225 | 0.098 | 1.937 | 2.567 | <0.0001 |
| Days from Surgery to First Day of Delirium | |||||
| 0–1 (reference) | |||||
| 2–3 | −0.670 | −0.051 | −0.852 | −0.488 | <0.0001 |
| 4–6 | −0.650 | −0.036 | −0.898 | −0.401 | <0.0001 |
| Consultation-Liaison Psychiatry | |||||
| None (reference) | |||||
| Early (0–2 days) | 0.558 | 0.024 | 0.235 | 0.881 | 0.0007 |
| Late (3–5 days) | 3.169 | 0.064 | 2.507 | 3.831 | <0.0001 |
Table 5 showed the cumulative dose of each drug within 1 week after delirium. The CLP group had significantly a large cumulative amount for almost drugs compared to non-CLP group. Haloperidol infusion was used twice as much for CLP as compared to non-CLP. Risperidone and Perospirone were significantly used 1.5 times as much for CLP as compared to non-CLP group. Quetiapine, Trazodone, and Mianserin were significantly used 1.3 to 1.4 times as much for CLP as compared to non-CLP group. Only Tiapride was significantly used 1.5 times less for CLP compared to non-CLP.
Table 5. Cumulative Dose of Each Drug within 1 Week After Delirium.
| CLP Group (n = 1,777) | Non-CLP Group (n = 18,865) | p-value | |||
|---|---|---|---|---|---|
| n | mg, median (IQR) | n | mg, median (IQR) | ||
| Haloperidol Infuison | 837 | 10 (5–15) | 9008 | 5 (5–10) | <0.0001 |
| Risperidone | 758 | 5 (3–10) | 4616 | 3 (2–6) | <0.0001 |
| Quetiapine | 612 | 213 (125–375) | 1846 | 150 (75–250) | <0.0001 |
| Trazodone | 396 | 200 (125–300) | 1296 | 150 (75–250) | <0.0001 |
| Perospirone | 112 | 36 (20–60) | 205 | 24 (16–40) | 0.0003 |
| Olanzapine | 87 | 25 (13–55) | 232 | 25 (15–54) | 0.994 |
| Mianserin | 65 | 100 (50–130) | 246 | 70 (50–133) | 0.126 |
| Valproic Acid | 62 | 2400 (800–4065) | 582 | 2800 (1400–5600) | 0.0129 |
| Tiapride | 46 | 163 (75–306) | 320 | 250 (150–400) | 0.0174 |
| Aripiprazole | 38 | 42 (25–74) | 166 | 23 (12–45) | 0.0081 |
| Clorpromazine | 26 | 150 (84–469) | 179 | 125 (75–263) | 0.2542 |
| Levomepromazine | 28 | 100 (36–175) | 164 | 123 (30–319) | 0.3365 |
| Haloperidol | 28 | 10 (6–24) | 180 | 7 (4–20) | 0.2688 |
| Clorpromazine Infusion | 22 | 28 (24–83) | 293 | 25 (10–30) | 0.0027 |
| Blonanserin | 17 | 40 (26–92) | 31 | 32 (14–96) | 0.3997 |
| Levomepromazine Infusion | 4 | 25 (25–25) | 20 | 25 (25–25) | 0.511 |
CLP: Consultation-Liaison Psychiatry.
DISCUSSION
We examined drug treatment for patients with postoperative delirium and CLP in the Japanese Administrative Database. This study is one of the first assessments of pharmacotherapy and CLP’s actual conditions for postoperative delirium using a Japanese national inpatient database to the best of our knowledge.
Multiple regression analysis indicated a relationship between early CLP and days from surgery to discharge. However there was no substantial relationship between late CLP and days from surgery to discharge. In the CLP group, delirium days was significantly longer, and patients were prescribed more drugs were used than in the non-CLP group. This fact suggests that the result of treatment for delirium in non-CLP group relates to timing of referral to CLP. In more detail, in cases where restlessness indicated persistent and hard-to-manage delirium, CLP was most likely considered first. However, it is very likely that other factors, such as the different clinical backgrounds in the CLP and non-CLP groups, have not been taken into account because of the focus on postoperative medication for patients with delirium. On the other hand, from previous studies, the use of antipsychotic drugs for dementia caused a risk of falling or aspiration, and the like, and increased the mortality rate [21]. Delays in drug treatment for delirium may be related to increased in hospital days from surgery to discharge. These findings suggest that drug treatment for delirium should be actively performed in an appropriate environment.
The demand for psychiatrists in general hospitals is increasing year by year. Still, the number of psychiatrists in general hospitals decreases [22]. This shortage of psychiatrists is a significant problem in Japan. The psychiatry of general hospitals is limited. The number of full-time psychiatrists who work there is not sufficient in Japan. Therefore, psychiatry who work in general hospitals does not receive consultation-liaison every day, and early CLP in all delirium cases can be difficult. Thus, an increased understanding of delirium as a doctor and co-medical as a whole combined with early intervention is recommended.
Regarding drug treatment, on the day of postoperative delirium, Haloperidol infusion was used most often in the CLP and non-CLP groups. Most likely, it was indicated in advance when patients were restless. For patients recovering from surgery for cancer, digestive tract, and similar diseases, vascular access is secured by infusion. After surgery, these patients cannot take oral antipsychotic drugs. Therefore antipsychotic infusion drugs such as Haloperidol are used. For this reason, Haloperidol infusion is essential. Still, the likelihood of extrapyramidal symptoms increases the risk of aspiration pneumonia and may increase the risk of delirium by requiring anticholinergic drugs [23]. Therefore, switching from Haloperidol infusion to non-typical antipsychotic drugs as soon as possible is recommended [24]. The prescription days for haloperidol infusion was the shortest of almost drugs in this analysis. This result supports the previous study.
Risperidone is often prescribed for delirium clinical treatment because it is easy to take to have liquid drugs. Delirium patients may not be able to follow instructions, and there can be some rejections. However, even if there is a passage disorder, this does not interfere with the administering oral medication. Therefore, this is an advantage for the clinical treatment of delirium [25].
Because Quetiapine is an antipsychotic drug with a short half-life, a strong sedative effect, less extrapyramidal symptoms, and fewer anticholinergic effects, it is prescribed frequently. For elderly patients, this type of medication is preferred since it is not as disturbing for the sleep-wake cycle. According to a previous study, 68% of psychiatrists working in a general hospital in Japan used Risperidone or Quetiapine for overactive delirium. In the case of infusion, 67% of psychiatrists used Haloperidol [24]. The results of this analysis support this.
For hypoactive delirium treatment, some experts recommend the use of Aripiprazole, Mianserin, and Trazodone [24]. Compared to hyperactive delirium, there is insufficient evidence regarding the use of drugs to treat hypoactive delirium [26]. The less sedative properties of Aripiprazole compared to other antipsychotics may have been the reason to use it for treating hypoactive delirium [27]. Furthermore, Trazodone and Mianserin are sedative antidepressants, and prescribing them is recommended to ensure sleep without worsening delirium. Perospirone is a weak sedative with a short half-life and useful for inducing rest [25]. However, the prescription rate is not as high as expected. This fact indicates that other antipsychotics such as Risperidone and Quetiapine are preferred.
Tiapride is the only antipsychotic drug approved in Japan for insurance treatment of delirium. Therefore, although the prescription rate is low, it is considered an antipsychotic drug that can easily prescribe. There seems to be no significant difference in the number of cases between the CLP and non-CLP groups.
Many drugs showed significant differences in case, first day of prescription, prescription days, and dose between the CLP and non-CLP groups. These results indicated that CLP and non-CLP groups have different drug treatments. In short, the CLP group has various choices of antipsychotics according to patients because psychiatrists always use antipsychotics and antidepressants.
Age, men, number of drugs used, CCI, and early CLP were common factors affecting the number of days from surgery to discharge and delirium days. Although early CLP affected delirium days longer, this affected days from surgery to discharge effectively compared to non-CLP. Early CLP may reduce days from surgery to discharge. Although late CLP affected delirium days longer, this did not affect days from surgery to discharge compared to non-CLP. Late CLP may not prolong days from surgery to discharge.
The development of delirium has been found to be associated with worse patient outcomes, including prolonged hospital stays, higher mortality rates, and other secondary negative impacts such as increased care costs and greater burdens on healthcare professionals [28]. Rates of delirium misdiagnosis range in the majority of studies from 41.8% to 64%. Factors affecting rates of delirium misdiagnosis include knowledge and training of clinicians and patient setting [29]. This study suggested there were many severe cases of poor control for delirium in the CLP group. Uncontrolled delirium was likely to have been hospitalized longer without CLP.
The limitations of this study are shown below. We used DPC data to analyze drug treatment for patients with postoperative delirium and CLP in Japan. The method of using DPC as a “classification of diagnosis group” was initially developed in Japan. A limitation of this study is defining the nursing requirement as a subset of patients with postoperative delirium onset. Most psychiatric medication is an off-label use for delirium treatment in Japan. It was difficult to extract the relationship between patients with postoperative delirium and psychiatric medication from diagnoses. Delirium defined in this study may also be mood disorders and dementia. Also, many hypoactive patients do not get the attention they need because of the characteristics of symptoms, and there were not enough criteria to extract hypoactive delirium [10]. Additionally, we cannot deny the risk of bias because we used new data from fiscal 2016 nursing requirements. We did not consider the severity of postoperative delirium or the amount and combination of drugs prescribed. Therefore, further analysis is considered necessary.
We focused on the analysis of antipsychotics-centered drugs and CLP, which are considered drug therapy, for patients with postoperative delirium. We concentrated on finding and removing the cause in actual clinical practice. Appropriate environmental maintenance and removing mental stress (anxiety, pain, restraint, various routines, exhaustion, and similar conditions.) often improves symptoms. There are limitations in determining the effect of antipsychotic treatment only. Non-pharmacologic delirium prevention interventions are effective in reducing delirium incidence and preventing falls, with trend towards decreasing length of stay and avoiding institutionalization [30]. Therefore, there may be cases where early delirium treatment other than drug treatment reduce not only hospital days but also avoid long-term antipsychotic drug administration and the use of multiple antipsychotic drugs. In the future, further studies on CLP are recommended for appropriate treatment without excess or deficiency for postoperative delirium patients.
CONCLUSIONS
We investigated the actual conditions of pharmacotherapy and CLP for postoperative delirium. Our findings suggest that there was a relationship between early CLP and days from surgery to discharge.
ACKNOWLEDGMENTS
We want to express our appreciation to Gregor Schmidt for providing native language help and proofreading the article.
CONFLICTS OF INTEREST
We declare that we have no conflicts of interest.
REFERENCES
- 1.Hansen MS, Fink P, Frydenberg M, Oxhøj M, Søndergaard L, Munk-Jørgensen P. Mental disorders among internal medical inpatients: prevalence, detection, and treatment status. J Psychosom Res 2001;50:199–204. [DOI] [PubMed] [Google Scholar]
- 2.Sockalingam S, Allzahrani A, Meaney C, Styra R, Tan A, Hawa R, et al. Time to Consultation-Liaison Psychiatry Service Referral as a Predictor of Length of Stay. Psychosomatics 2016;57:264–272. [DOI] [PubMed] [Google Scholar]
- 3.Wood R, Wand AP. The effectiveness of consultation-liaison psychiatry in the general hospital setting: a systematic review. J Psychosom Res 2014;76:175–192. [DOI] [PubMed] [Google Scholar]
- 4.Alhuthail YR. Timing of referral to consultation-liaison psychiatry. Int J Health Sci 2009;3:170–175. [PMC free article] [PubMed] [Google Scholar]
- 5.Kishi Y, Meller WH, Kathol RG, Swigart SE. Factors affecting the relationship between the timing of psychiatric consultation and general hospital length of stay. Psychosomatics 2004;45:470–476. [DOI] [PubMed] [Google Scholar]
- 6.Lyons J, Hammer J, Strain J, George F. The timing of psychiatric consultation in the general hospital and length of hospital stay. Gen Hosp Psychiatry 1986;8:159–162. [DOI] [PubMed] [Google Scholar]
- 7.Handrinos D, McKenzie D, Smith GC. Timing of referral to a consultation-liaison psychiatry unit. Psychosomatics 1998;39:311–317. [DOI] [PubMed] [Google Scholar]
- 8.Ormont MA, Weisman HW, Heller SS, Najara J, Shindledecke R. The timing of psychiatric consultation requests. Utilization, liaison, and diagnostic considerations. Psychosomatics 1997;38:38–44. [DOI] [PubMed] [Google Scholar]
- 9.Narei H, Jae-Yong P. The Motoric Types of Delirium and Estimated Blood Loss during Perioperative Period in Orthopedic Elderly Patients. Biomed Res Int 2018;9812041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kishi T, Hirota T, Matsunaga S, Iwata N. Antipsychotic medications for the treatment of delirium: a systematic review and meta-analysis of randomised controlled trials. J Neurol Neurosurg Psychiatry 2016;87:767–774. [DOI] [PubMed] [Google Scholar]
- 11.Someya T, Endo T, Hara T, Yagi G, Suzuki J. A survey on the drug therapy for delirium. Psychiatry Clin Neurosci 2001;55:397–401. [DOI] [PubMed] [Google Scholar]
- 12.Kim SW, Yoo JA, Lee SY, Kim SY, Bae KY, Yang SJ, et al. Risperidone versus olanzapine for the treatment of delirium. Psychopharmacol 2010;25:298–302. [DOI] [PubMed] [Google Scholar]
- 13.Herzig SJ, Rothberg MB, Guess JR, Stevens JP, Marshall J, Gurwitz JH, et al. Antipsychotic Use in Hospitalized Adults: Rates, Indications, and Predictors. J Am Geriatr Soc 2016;64:299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. WHO, 1992. [Google Scholar]
- 15.Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011;173:676–682. [DOI] [PubMed] [Google Scholar]
- 16.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 17.Cheung S, Hamuro Y, Mahlich J, Nakahara T, Sruamsiri R, Tsukazawa S. Drug Utilization of Japanese Patients Diagnosed with Schizophrenia: An Administrative Database Analysis. Clin Drug Investig 2017;37:559–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Urushihara H, Kobayashi S, Honjo Y Kosugi S, Kawakami K. Utilization of antipsychotic drugs in elderly patients with Alzheimer’s disease seen in ambulatory practice in Japan. Sci Postprint 2014;1:doi: 10.14340/spp.2014.01C0003. [DOI] [Google Scholar]
- 19.Kadohara K, Sato I, Doi Y, Arai M, Fujii Y, Matsunaga T, et al. Prescription patterns of medications for Alzheimer’s disease in Japan from 2010 to 2015: a descriptive pharmacy claims database study. Neurol Ther 2017;6:25–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koga Y, Moro E, Arita T, Obata Y, Kawashima K, Suzumechi Y, et al. The Current Situation Survey of Delirium Assessment and Delirium Care for Perioperative Ward after 2016 Revision of Medical Fee: Necessity of Clarification for Delirium Patients and Additional Medical Fee for Critical Care in Delirium Management Japan. Critical Care Nursing Society 2018;14:47–56. [Google Scholar]
- 21.Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA 2005;294:1934–1943. [DOI] [PubMed] [Google Scholar]
- 22.Sato S. Future Images of General Hospital Psychiatry. Seishin Shinkeigaku Zasshi 2016;118:688–694. [PubMed] [Google Scholar]
- 23.Mahar AR, Maglione M, Bagley S, Marika S, Hu JH, Brett E, et al. Efficacy and comparative effectiveness of atypical antipsychotic medications for off-label uses in adults: a systematic review and meta-analysis. JAMA 2011;306:1359–1369. [DOI] [PubMed] [Google Scholar]
- 24.Okumura Y, Hatta K, Wada K, Takeuchi T, Kishi Y. Expert opinions on the first-line pharmacological treatment for delirium in Japan: a conjoint analysis. Int Psychogeriatr 2016;28:1041–1050. [DOI] [PubMed] [Google Scholar]
- 25.Hatta K, Kishi Y, Wada K, Odawara T, Takeuchi T, Shiganami T, et al. Antipsychotics for delirium in the general hospital setting in consecutive 2453 inpatients: a prospective observational study. Int J Geriatr Psychiatry 2014;29:253–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carvalho J, Alvim R, Martins J, Bouza C, Zenaide P, Zantieff R, et al. Pharmacological treatment of hypoactive delirium in critically ill patients: a systematic review. Critical Care 2013;17:36. [Google Scholar]
- 27.Marder SR, McQuade RD, Stock E, Stephen K, Ronald M, Allan ZS, et al. Aripiprazole in the treatment of schizophrenia: safety and tolerability in short-time, placebo-controlled trials. Schizophr Res 2003;61:123–136. [DOI] [PubMed] [Google Scholar]
- 28.Kim S, Kim JJ, Oh J, Park J, Park JY. Delirium characteristics and outcomes in medical and surgical lnpatients: A subgroup analysis. J Crit Care 2018;43:156–162. [DOI] [PubMed] [Google Scholar]
- 29.Hercus C, Hudaib AR. Delirium misdiagnosis risk in psychiatry: a machine learning-logistic regression predictive algorithm. BMC Health Serv Res 2020;20:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tammy T, Jirong Y, Esther O, Margaret P, Sarah D, Thomas T, Sharon K, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med 2015;175:512–520. [DOI] [PMC free article] [PubMed] [Google Scholar]