Abstract
Cognitive-behavioral conjoint therapy for posttraumatic stress disorder (CBCT for PTSD; Monson & Fredman, 2012) is efficacious in improving PTSD symptoms and relationship adjustment among couples with PTSD. However, there is a need for more efficient delivery formats to maximize engagement and retention and to achieve faster outcomes in multiple domains. This nonrandomized trial was designed to pilot an abbreviated, intensive, multi-couple group version of CBCT for PTSD (AIM-CBCT for PTSD) delivered over a single weekend for 24 couples that included an active-duty service member or veteran with PTSD who had deployed in support of combat operations following September 11, 2001. All couples completed treatment. Assessments conducted by clinical evaluators 1 and 3 months after the intervention revealed significant reductions in clinician-rated PTSD symptoms (ds = −0.77 and −0.98, respectively) and in patients’ self-reported symptoms of PTSD (ds = −0.73 and −1.17, respectively), depression (ds = −0.60 and −0.75, respectively), anxiety (ds = −0.63 and −0.73, respectively), and anger (ds = −0.45 and −0.60, respectively), relative to baseline. By 3-month follow-up, partners reported significant reductions in patients’ PTSD symptoms (d = −0.56), as well as significant improvements in their own depressive symptoms (d = −0.47), anxiety (d = −0.60), and relationship satisfaction (d = 0.53), relative to baseline. Delivering CBCT for PTSD through an abbreviated, intensive multi-couple group format may be an efficient strategy for improving patient, partner, and relational well-being in military and veteran couples with PTSD.
Keywords: PTSD, treatment, couples, massed, retreat
Posttraumatic stress disorder (PTSD; American Psychiatric Association [APA], 2013) is a common mental health consequence of military deployment, affecting an estimated 15% of service members and 23% of veterans who have deployed to Iraq and/or Afghanistan since September 11, 2001 (Fulton et al., 2015; Thomas et al., 2010). There is also increasing recognition that PTSD is associated with relationship distress, physical and psychological aggression, and partner psychological distress (Lambert, Engh, Hasbun, & Holzer, 2012; Taft, Watkins, Stafford, Street, & Monson, 2011).
Interpersonal factors have been implicated in individual PTSD treatment outcomes. For instance, family negativity is associated with poorer individual treatment outcomes in cognitive-behavioral therapy for PTSD (e.g., Tarrier, Sommerfield, & Pilgrim, 1999). In addition, partners may engage in behaviors that inadvertently reinforce symptoms. For example, partners can accommodate patients’ symptoms by colluding in avoidance and safety behaviors to minimize patients’ PTSD-related distress or relationship conflict (Fredman, Vorstenbosch, Wagner, Macdonald, & Monson, 2014), which contributes to the maintenance of PTSD-related avoidance symptoms over time (Campbell, Renshaw, Kashdan, Curby, & Carter, 2017).
Cognitive-behavioral conjoint therapy for PTSD (CBCT for PTSD; Monson & Fredman, 2012), a 3-phase, 15-session treatment for PTSD delivered in a conjoint format, has demonstrated improvements in PTSD symptoms, comorbid symptoms, and relationship satisfaction in active-duty, veteran, and community couples (e.g., Monson et al., 2012; Monson et al., 2017; Schumm, Fredman, Monson, & Chard, 2013). Improvements in partners’ psychological distress have also been observed (Shnaider, Pukay-Martin, Fredman, Macdonald, & Monson, 2014). However, the 15-session weekly format can present challenges for treating couples, particularly when delivered during traditional clinic and work hours.
Difficulties with treatment retention are not unique to couple therapy; indeed, dropout from individual psychosocial treatment for PTSD is common (e.g., Berke et al., 2019) and increases with longer treatment duration (Imel, Laska, Jakupcak, & Simpson, 2013). Thus, more efficient delivery formats are needed to maximize engagement and retention. Research supports the use of massed (i.e., daily, intensively delivered) cognitive or behavioral individual therapies for PTSD (Ehlers et al., 2014; Foa et al., 2018), but there are no published trials on the use of brief, massed couple therapies for PTSD. To streamline delivery, Davis, Luedtke, and Monson (2015) conducted a randomized controlled trial in which post-9/11 veteran couples with PTSD received the first two phases of CBCT for PTSD integrated with mindfulness training in a multi-couple group format during a weekend retreat, followed by eight sessions of CBCT for PTSD Phase 3 content delivered to individual couples. There were large improvements in clinician-rated PTSD symptoms immediately following and 6 months after the full treatment, along with significant improvements in comorbid symptoms and relationship satisfaction. However, clinician assessments of PTSD severity were not conducted immediately after the retreat; thus, the effects of the weekend portion alone and without the mindfulness integration are unknown.
The investigation described in this paper served as an initial nonrandomized trial of an abbreviated, intensive, multi-couple group version of CBCT for PTSD (AIM-CBCT for PTSD) delivered over a single weekend for couples that included either a post-9/11 service member or veteran with PTSD (i.e., the patient) and their partner. It was hypothesized that there would be significant improvements with respect to (a) clinicians’ ratings of patients’ PTSD symptom severity, (b) patients’ self-reported PTSD symptoms and comorbid symptom severity, (c) partners’ psychological distress, and (d) both partners’ relationship satisfaction. We also examined participants’ satisfaction with the program.
Method
PARTICIPANTS
Participants were 24 heterosexual couples (mean relationship length = 14.56 years, SD = 9.15) enrolled in a nonrandomized trial designed to pilot an abbreviated, intensive, multi-couple group version of CBCT for PTSD (Monson & Fredman, 2012). Treatment was delivered over a single weekend from 2016–2017 and conducted as part of the work of the Consortium to Alleviate PTSD (CAP). The CAP is a multi-institutional and multidisciplinary research consortium jointly funded by the Department of Defense and the Department of Veterans Affairs focused on the prevention, diagnosis, and treatment of combat PTSD and related conditions in post-9/11 military service members, veterans, and their families. Each study funded by the CAP follows good clinical practice for clinical trials design, human subjects’ protection, data security, storage, archival access, and data analysis guidelines established by the CAP Coordinating Center and supporting research cores (Barnes et al., 2019). Active-duty military and veteran couples were recruited via clinician referral from care providers at the Carl R. Darnall Army Medical Center at the U.S. Army’s Fort Hood in Killeen, Texas, and self-referrals from the greater San Antonio, Texas, area through the STRONG STAR (South Texas Research Organizational Network Guiding Studies on Trauma and Resilience) website and phone line. Demographic and baseline characteristics of patients and partners are provided in Table 1.
Table 1.
Demographic Characteristics by Partner Status
| Characteristic | Patient | Partner |
|---|---|---|
| (n = 24) | (n = 24) | |
| M or n (SD or %) | M or n (SD or %) | |
| Age (years) | 40.49 (7.12) | 38.70 (8.18) |
| Male | 23 (95.83%) | 1 (4.17%) |
| Ethnicity | ||
| Hispanic | 7 (29.17%) | 8 (33.33%) |
| Race | ||
| African-American | 7 (29.17%) | 8 (33.33%) |
| Asian | 1 (4.17%) | 1 (4.17%) |
| Caucasian | 11 (45.83%) | 9 (37.50%) |
| Other | 5 (20.83%) | 6 (25.00%) |
| Education (years) | ||
| Some high school | 0 | 2 (8.33%) |
| GED | 0 | 2 (8.33%) |
| Some college | 15 (62.50%) | 8 (33.33%) |
| Associate degree | 5 (20.83%) | 2 (8.33%) |
| 4-year college degree | 2 (8.33%) | 4 (16.67%) |
| Master’s degree | 2 (8.33%) | 6 (25.00%) |
| Military status | ||
| Active duty | 17 (70.83%) | 2 (8.33%) |
| Veteran | 7 (29.17%) | 1 (4.17%) |
| Time in service (months) | 186.54 (74.27) | 99.67 (94.00) |
| Number of deployments | 2.75 (0.99) | 1.5 (0.71) |
| Military Grade | ||
| E-1 to E-3 | 1 (4.17%) | 0 |
| E-4 to E-6 | 13 (54.17%) | 2 (8.33%) |
| E-7 to E-9 | 7 (29.17%) | 1 (4.17%) |
| Officer | 3 (12.50%) | 0 |
| Employed at least part-time | 21 (87.5%) | 17 (70.83%) |
| Any psychotropic medication | 17 (70.83%) | 3 (12.50%) |
| Antidepressant | 16 (66.67%) | 3 (12.50%) |
| SSRI | 10 (41.67%) | 3 (12.50%) |
| Other antidepressant | 8 (33.00%) | 0 |
| Prazosin | 8 (33.00%) | 0 |
| Other sleep medication | 7 (29.17%) | 0 |
| Benzodiazepine | 5 (20.83%) | 0 |
| Topiramate (for migraines) | 3 (12.50%) | 0 |
| Gabapentin (for pain) | 6 (25.00%) | 0 |
| Medication for general medical conditions | 6 (25.00%) | 3 (12.50%) |
Note. E-1 to E-3 = junior enlisted; E-4 to E-6 = junior noncommissioned officers; E-7 to E-9 = senior noncommissioned officers; SSRI = selective serotonin reuptake inhibitor.
Couples were included if they were married or had been cohabiting for a minimum of 3 months and included a service member or veteran who met the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5; APA, 2013) diagnostic criteria for current PTSD according to the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers, Blake, et al., 2013) and had a CAPS-5 score ≥ 25. The service member/veteran with PTSD must have experienced a Criterion A trauma during deployment in support of combat operations following 9/11. In addition, both partners needed to be between the ages of 18–65 and able to speak and read English fluently. Couples were excluded if they were separated or planning to divorce or if either partner: (a) had experienced a recent manic episode (past 12 months) or a psychotic disorder; (b) was engaged in current and severe alcohol use warranting immediate intervention; (c) exhibited evidence of a moderate or severe traumatic brain injury; (d) endorsed current suicidal ideation severe enough to warrant immediate attention; and/or (e) endorsed severe intimate aggression in the relationship in response to a question adapted from items from the Conflict Tactics Scale-Revised (Straus, Hamby, McCoy, & Sugarman, 1996): “During the past 6 months, have you or your partner done any of the following to the other: used a knife or gun, punched or hit with something that could hurt, choked, slammed against a wall, beaten, burned or scalded, or kicked the other partner?” Couples were excluded if the partner met diagnostic criteria for PTSD according to the CAPS-5, if the patient was currently participating in cognitive processing therapy (Resick, Monson, & Chard, 2016) or prolonged exposure (Foa, Hembree, & Rothbaum, 2007), or if the couple was already receiving CBCT for PTSD.
MEASURES
PTSD Diagnostic Status and Symptom Severity
The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers, Blake, et al., 2013) is a gold-standard, semi-structured diagnostic interview for determining PTSD diagnosis and symptom severity. The 20 DSM-5 PTSD symptoms are rated on a 5-point rating scale ranging from 0 (“none”) to 4 (“extremely”) to assess trauma-related intrusions, effortful avoidance, alterations in arousal and anxiety, and negative alterations in cognition and mood symptoms in the past month. CAPS-5 scores range from 0 to 80, with higher scores indicating greater PTSD symptom severity. The CAPS-5 has strong psychometric properties in samples of service members and veterans (Barnes et al., 2019). The CAPS-5 was administered by clinical evaluators consisting of trained master’s- or doctoral-level assessors overseen by the CAP’s Assessment Core. Across the Consortium’s studies, interrater reliability for the CAPS-5 was excellent with respect to both presence/absence of PTSD (Cohen’s κ = .90) and correlation of PTSD symptom severity scores between clinical evaluators and expert rater (r = .98; Barnes et al., 2019).
The PTSD Checklist for DSM-5 (PCL-5; Weathers, Litz, et al., 2013) is a 20-item self-report measure that assesses the severity of each of the DSM-5 PTSD symptoms and was used to assess patient-reported PTSD symptom severity. A collateral version had partners rate their perceptions of patients’ PTSD severity. Scoring is based on how much the patient has been bothered by the symptoms in the past month on a scale from 0 (not at all) to 4 (extremely). Items are summed with total scores ranging from 0–80, with higher scores reflecting greater PTSD severity. The measure has demonstrated excellent psychometric properties (Barnes et al., 2019). In the present sample, internal consistency ranged from α = .88 to .93 for patients and α = .93 to .94 for partners across assessments.
Depressive Symptom Severity
Patient and partner depressive symptom severity were assessed via the Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2001). Respondents rate the frequency with which they have been bothered by depressive symptoms within the past 2 weeks on a scale ranging from 0 (not at all) to 3 (nearly every day). Items are summed to obtain a total severity score that ranges from 0 to 27, with higher scores reflecting greater symptom severity. In the present sample, internal consistency ranged from α = .76 to .86 for patients and from α = .82 to .94 for partners across assessments.
Anxiety Symptom Severity
The Generalized Anxiety Disorder Screener (GAD-7; Spitzer, Kroenke, Williams, & Lowe, 2006) was used to assess generalized anxiety symptomology. The GAD-7 is a 7-item measure that asks participants to rate the frequency with which they have been bothered by anxiety symptoms within the past 2 weeks on a 0 (not at all) to 3 (nearly every day) scale. Items are summed to obtain a total severity score ranging from 0 to 21, with higher scores reflecting greater anxiety. Across assessments, internal consistency ranged from α = .83 to .90 for patients and was α = .93 for partners.
Anger Symptom Severity
The State Anger (S-Anger) subscale of the State-Trait Anger Expression Inventory-2 (STAXI-2; Spielberger, 1999) was used to assess participants’ feelings of anger at a given moment. This subscale consists of 15 items that ask participants to indicate how much they are experiencing certain feelings and desires on a 4-point scale ranging from 1 (not at all) to 4 (very much so). Items are summed to assess the overall intensity of anger felt at a particular moment, with higher scores reflecting greater anger. Across assessments, internal consistency ranged from α = .89 to .96 for patients and from α = .88 to .99 for partners.
Relationship Satisfaction
Couples’ relationship satisfaction was assessed using the Couples Satisfaction Index (CSI; Funk & Rogge, 2007), a well-validated, 32-item, self-report measure that assesses satisfaction in intimate dyads. Items are summed to yield a total score ranging from 0 to 161, with higher scores indicating greater satisfaction. Across assessments, internal consistency ranged from α = .98 to .99 for patients and was α = .98 for partners.
Client Satisfaction
Participants’ satisfaction with the intervention was assessed using the Client Satisfaction Questionnaire-8 (CSQ-8; Attkisson & Greenfield, 2004), an 8-item measure used to assess satisfaction with treatment. Items are summed to yield a score ranging from 4 to 32, with higher scores indicating greater satisfaction. The CSQ-8 was administered to participants at 1- and 3-month follow-up assessments. At 1-month follow-up, α = .69 for patients and .86 for partners; at 3-month follow-up, α = .95 for patients and .90 for partners.
PROCEDURES
All study procedures were approved by the Institutional Review Boards (IRBs) at the University of Texas Health Science Center at San Antonio (UTHSCSA) and the South Texas Veterans Health Care System, as well as the Research Ethics Board at Ryerson University. The IRBs at the Pennsylvania State University and The Citadel deferred to the IRB at UTHSCSA. The U.S. Army Medical Research and Materiel Command Human Research Protections Office at Fort Detrick, Maryland monitored all the regulatory reviews and approvals.
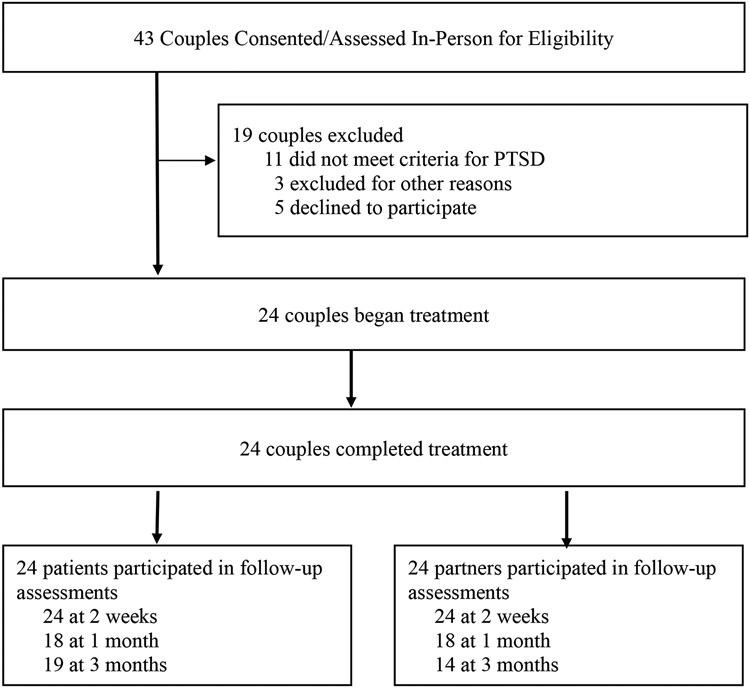
Prospective participants were screened by phone to determine initial eligibility. Interested individuals and their partners participated in an in-person assessment to determine eligibility; written informed consent was obtained by both members of the couple prior to their being assessed for study inclusion/exclusion criteria. In-person assessments were conducted by clinical evaluators trained and supervised by the CAP’s Assessment Core who did not deliver the therapy. Assessments included standardized administration of CAP Common Data Elements in the domains of demographic characteristics, military service, PTSD and comorbid symptom severity, suicidal ideation, substance use, general health, and psychosocial functioning (see Barnes et al., 2019, for additional details), as well as study-specific measures (e.g., CSI, CSQ-8). Assessments were repeated for both members of the couple 1 and 3 months after the retreat. The self-report and collateral versions of the PCL-5 were also administered to each partner approximately 2 weeks after the retreat and included in data analyses. A visual representation of participant flow through the study is depicted in Figure 1.
Figure 1.
Flow of participants through the study. PTSD = posttraumatic stress disorder.
TREATMENT PROTOCOL AND FIDELITY MONITORING
The weekend retreat portions of the treatment took place at a hotel in Austin, Texas, because of its geographical proximity to both recruitment sites. Couples were provided with lodging for two nights, breakfasts and lunches during the retreat, money for dinner on the Friday and Saturday evenings of the weekend ($75 for each night), and money towards childcare. In addition to the weekend retreat, individual couples participated in a meeting with one of the group therapists approximately 1 week before the retreat and again approximately 2 weeks after the retreat (described in further detail below).
WEEKEND RETREAT
The weekend retreat component of AIM-CBCT for PTSD consisted of approximately 12 hours of CBCT for PTSD programming delivered consecutively over 2 days, with a primary focus on content from the first two phases of CBCT for PTSD (Monson & Fredman, 2012). The first phase included psychoeducation about PTSD and relationship functioning, rationale for treatment, and the promotion of physical and emotional safety in the relationship via behavioral conflict management skills. The second phase included behaviorally focused interventions designed to enhance relationship functioning and assignment of couple-level approach tasks to address PTSD-related avoidance and partner accommodation of symptoms. Content was delivered in seven modules lasting approximately 60–90 minutes that corresponded to the content of Sessions 1–7 from the parent protocol (Monson & Fredman, 2012) and an eighth module that corresponded to parent protocol Session 15, which was designed to help couples to consolidate what they had learned and to plan for ongoing skill use once they returned home. Couples were not formally instructed to engage in historical reappraisals of the patient’s trauma(s), as is typically done in Phase 3 of CBCT for PTSD. Instead, parent protocol Session 2 content related to the value of trauma-related disclosure to a supportive other was emphasized throughout the weekend to highlight how couples could use specific skills to share their thoughts and feelings about the patients' trauma(s) if they wished. Therapists also noted that the skills to increase cognitive flexibility about here-and-now thoughts disrupted by the trauma (e.g., “It’s never safe to be in a crowd”) could be used to explore historical appraisals of the trauma (e.g., “It’s my fault that the trauma occurred”).
Seven different retreats, ranging in size from two to six couples, were co-led by two group therapists at a time. Treatment was delivered using a workshop format, with standardized slides adapted from a Department of Veterans Affairs’ clinician training workshop as part of its national dissemination of CBCT for PTSD. Each module followed a similar format: (a) a didactic presentation on the effects of PTSD on intimate relationships (e.g., the contribution of PTSD to communication difficulties); (b) introduction of a skill to address PTSD in a relational context (e.g., sharing feelings about the impact of PTSD on their relationship); (c) therapist role-play of that skill; (d) a break-out session in which individual dyads practiced the skill(s) and therapists provided feedback, (e) group debrief of the practice session; and (f) a review of the main points covered in that module. Therapists recapped key concepts at the end of Day 1 and at the end of the retreat to consolidate learning and encourage skill use. Throughout the weekend, commonalities in presenting problems were used to normalize participants’ experiences, and both structured and casual interactions with other group members served as informal opportunities to facilitate balanced thinking about unfamiliar others. Debriefing of skill use in the group context, which included input from other participants, was also used to potentiate vicarious learning and the exchange of social support.
Consistent with the original CBCT for PTSD protocol, multiple in vivo approach assignments were included throughout the retreat. For example, capitalizing on the multi-couple group format, couples were instructed to switch seats multiple times throughout the retreat, which allowed patients to target hypervigilance and increase their comfort sitting near windows and with others sitting behind them. They also participated in a dyadic out-of-workshop approach assignment for the Saturday evening of the retreat that doubled as a date (e.g., going out to dinner and sitting with one’s back to the door while at a crowded restaurant).
Pre- and Postretreat Meetings
Pre- and post-retreat meetings with individual couples took place at therapists’ offices at Fort Hood or San Antonio and typically lasted 60–90 minutes. At the preretreat meeting, therapists followed a study-specific structured interview designed to facilitate rapport with the couples and orient them to the structure, content, and expectations for the upcoming weekend. Therapists briefly introduced CBCT for PTSD and the rationale for the abbreviated, intensive, multi-couple group format. Couples then discussed their relationship history and strengths, desired areas for improvement in relationship domains impacted by PTSD, and their reasons for participating in the study. The session concluded with therapists assisting the couple in identifying one or two PTSD-related relationship goals and assigning couples to provide written responses to questions pertaining to the impact of PTSD on their relationship and how they imagined their relationship if the impact of PTSD were reduced in advance of the weekend. At the post-retreat meeting, the therapists reviewed each partner’s perceptions of the patient’s current PTSD symptoms, inquired about implementation of specific skills taught at the retreat, and discussed plans for continued implementation of skills to further consolidate gains with respect to PTSD symptoms and their relationship.
Therapist Training and Protocol Fidelity
Three therapists (two licensed clinical psychologists, one licensed clinical social worker) provided AIM-CBCT for PTSD and the pre- and postretreat individual dyad meetings. All therapists had extensive experience treating service members and veterans with PTSD and had been previously trained to deliver CBCT for PTSD to individual dyads. Therapists participated in a 1-day training provided by the first author on how to deliver CBCT for PTSD in an abbreviated, intensive weekend, multi-couple group format, followed by live supervision by the first author at the first two retreats. Therapists participated in ongoing group consultation with the first author throughout the study period.
Group therapy sessions were video-recorded, and pre- and postretreat meetings were audio-recorded for fidelity assessment. A random sample of 15% of group modules were rated for protocol adherence and therapist competence in delivering the specific, prescribed elements of that module, block randomized by day. In addition, 15% of the pre- and postretreat sessions delivered to individual dyads were also rated for adherence and competence. Adherence to the essential elements of the therapy was excellent, with 93.1% of these elements delivered. Competence in providing these treatment elements was very good to excellent, with an average rating of 6.52 (6 = very good and 7 = excellent).
STATISTICAL ANALYSES
To address the study aims, we conducted within-subjects mixed effects regressions with repeated measures using robust standard errors and restricted maximum likelihood estimation using PROC MIXED in SAS 9.3 (SAS Institute, Cary, NC). An unstructured covariance matrix in which time was modeled as a categorical variable was specified so that variances and covariances could be freely estimated across the repeated measures. As confirmed by Little’s MCAR (missing completely at random) test (Little, 1988), data were missing completely at random for both patients, χ2(37) = 33.66, p = .63, and partners, χ2(22) = 22.08, p = .46. As a further test, we examined whether findings differed when demographic and baseline functioning variables with at least a medium size association with missingness in the data were included in the models, and the pattern of significant findings was virtually the same.1 We also examined whether missingness was a function of gains made during the program, and it was not.
Least squares means (LSMs) and associated standard errors for each outcome at each assessment time point (pretreatment/baseline, 1-month follow-up, 3-month follow-up) were generated from the models. Planned contrasts between pretreatment and 1-month posttreatment LSMs, as well as between pretreatment and 3-month posttreatment LSMs, were conducted to determine whether there were statistically significant improvements in patients’ PTSD and comorbid symptoms, partners’ psychological distress, and both partners’ relationship satisfaction for each assessment relative to pretreatment levels. Within group effect sizes in the form of Cohen’s d were computed to determine the magnitude of change in outcomes from pretreatment to 1 and 3 months posttreatment, respectively, and were interpreted consistent with Cohen’s (1988) recommendations for small (d = .20), medium (d = .50), and large (d = .80) effect sizes.
Given the small sample size, improvement was also examined at the individual level with respect to PTSD symptom improvement. Proportions of patients no longer meeting PTSD diagnostic criteria according to DSM-5 (APA, 2013) criteria 1 and 3 months postretreat were calculated. As a more conservative test of individual improvement, we also examined whether changes in patients’ PTSD symptoms were reliable (i.e., greater than would be expected due to measurement error) and whether patients had achieved good end-state functioning. Following procedures described by Jacobson and Truax (1991), patients were classified as recovered, improved, unchanged, or deteriorated according to whether they experienced reliable change and achieved scores more than two standard deviations below the sample-specific baseline for PTSD severity (34.25 on the CAPS-5 and 48.79 on the PCL-5). Using the sample-specific baseline internal consistency reliability of α = .59 and baseline standard deviation of 6.85 for the CAPS-5, reliable change on the CAPS-5 was determined to be 12 points. Thus, to be considered recovered, patients were required to have a decrease of ≥ 12 points and to be rated as < 20 on the CAPS-5 at the follow-up assessment. Patients who experienced reliable change but whose symptoms were ≥ 20 on the CAPS-5 were considered improved but not recovered. Patient self-reported symptom severity on the PCL-5 was used as a secondary indicator of PTSD symptom change. To be considered recovered, follow-up scores needed to be ≥ 11 points lower than their baseline scores, and total scores needed to be ≤ 23 based on a sample-specific baseline α of .88 and standard deviation of 12.55. Proportions of patients and partners in the relationally satisfied range at pretreatment, 1-month follow-up, and 3-month follow-up were estimated using the recommended cut score of 104.5 on the CSI (Funk & Rogge, 2007).
Results
All 24 couples who attended the preretreat session also completed the retreat, and 23 of 24 couples attended the postretreat session. Presented in Table 2 are LSMs and their standard errors, along with t statistics and Cohen’s ds with 95% confidence intervals for planned contrasts to evaluate patient and partner outcomes relative to baseline levels. Proportions of patients in the recovered, improved, unchanged, and deteriorated categories are displayed in Table 3.
Table 2.
Pre- and Posttreatment Outcomes for Abbreviated, Intensive, Multi-Couple Group Cognitive-Behavioral Conjoint Therapy for Posttraumatic Stress Disorder (PTSD)
| Outcome | Least Squares Mean (Standard Error) | Pretreatment/1-Month Posttreatment | Pretreatment/3-Month Posttreatment | ||||
|---|---|---|---|---|---|---|---|
| Pretreatment | 1-Month Posttreatment |
3-Month Posttreatment |
t (23) | d (95% CI) | t (23) | d (95% CI) | |
| CAPS-5 | |||||||
| Patient† | 34.25 (1.37) | 26.60 (1.96) | 24.62 (2.30) | −3.71* | −0.77 (−1.21, −0.34) | −4.68* | −0.98 (−1.41, −0.54) |
| Partner | - | - | - | - | - | - | - |
| PCL-5†† | |||||||
| Patient | 48.79 (2.51) | 37.09 (3.25) | 31.31 (3.01) | −3.52* | −0.73 (−1.17, −0.30) | −5.63* | −1.17 (−1.60, −0.74) |
| Partner | 42.39 (3.66) | 33.70 (3.68) | 27.33 (4.05) | −1.99^ | −0.42 (−0.87, 0.02) | −2.65* | −0.56 (−1.01, −0.12) |
| PHQ-9 | |||||||
| Patient | 16.25 (0.86) | 12.42 (1.30) | 11.79 (0.95) | −2.86* | −0.60 (−1.03, −0.16) | −3.58* | −0.75 (−1.18, −0.31) |
| Partner | 4.71 (0.93) | 4.64 (1.34) | 2.94 (0.81) | −0.05 | −0.01 (−0.44, 0.42) | −2.24* | −0.47 (−0.90, −0.04) |
| GAD-7 | |||||||
| Patient | 15.21 (0.79) | 11.54 (1.13) | 11.69 (1.05) | −3.02* | −0.63 (−1.06, −0.20) | −3.50* | −0.73 (−1.16, −0.30) |
| Partner | 5.50 (1.17) | 4.34 (1.12) | 2.46 (0.71) | −0.91 | −0.19 (−0.62, 0.24) | −2.86* | −0.60 (−1.03 −0.17) |
| STAXI-2 | |||||||
| Patient | 26.04 (1.94) | 21.35 (2.06) | 21.30 (1.40) | −2.14* | −0.45 (−0.88, −0.02) | −2.87* | −0.60 (−1.03, −0.17) |
| Partner | 17.67 (0.90) | 18.00 (1.29) | 17.30 (2.03) | 0.21 | 0.04 (−0.39, 0.48) | −0.17 | −0.04 (−0.47, 0.40) |
| CSI | |||||||
| Patient | 110.17 (6.56) | 112.48 (7.60) | 113.33 (8.06) | 0.35 | 0.07 (−0.36, 0.50) | 0.49 | 0.10 (−0.33, 0.53) |
| Partner | 104.50 (7.18) | 113.57 (7.94) | 119.03 (7.15) | 1.91^ | 0.40 (−0.03, 0.83) | 2.52* | 0.53 (0.09, 0.96) |
Note. N = 24 couples. CI = confidence interval; CAPS-5 = Clinician-Administered PTSD Scale for DSM-5; PCL-5 = Posttraumatic Stress Disorder Checklist for DSM-5; PHQ-9 = Patient Health Questionnaire-9; GAD-7 = Generalized Anxiety Disorder Screener; STAXI-2 = State Trait Anger Expression Inventory-2 State Subscale; CSI = Couples Satisfaction Index. * p < .05, ^ p < .10.
The 1-month follow-up data for one patient were deemed invalid by the Consortium to Alleviate PTSD Assessment Core; thus, that participant’s data for that time point were not included in the analyses.
At 2-week follow-up, the least squares mean for PCL-5 for patients = 41.13 (2.95) and was significantly different from baseline: t(23) = −2.71, p = .013; d = −0.57 (−1.00, −0.13). At 2-week follow-up, the least squares mean for partner ratings of patient PTSD symptom severity on the PCL-5 = 29.53 (3.25) and was significantly different from baseline: t(22) = −3.63, p = .002; d = −0.77 (−1.22, −0.33). Because one partner’s ratings of patient PTSD symptom severity at baseline and 2-week follow-up were deemed to be outliers at p < .01 based on Grubbs’ test (Grubbs, 1969), and therefore invalid, that partner’s ratings were not included in the estimation of the least-squares means or the calculation of effect sizes for that outcome. Thus, the degrees of freedom for collateral ratings of patient PTSD symptom severity on the PCL-5 is 22 instead of 23.
Table 3.
Clinical Change Categories in PTSD Symptoms at 2-Week-, 1-Month-, and 3-Month Follow-Up
| Clinician-Rated PTSD Symptom Severity (CAPS-5) | ||||
|---|---|---|---|---|
| Recovered | Improved | Unchanged | Deteriorated | |
| 2 Weeks Post-Retreat | ||||
| Completers % (n/24) | - | - | - | - |
| Intent to treat % (n/24) | - | - | - | - |
| 1 Month Post-Retreat | ||||
| Completers % (n/16) | 12.5% (2) | 25.0 % (4) | 62.5% (10) | 0% (0) |
| Intent to treat % (n/24) | 8.3% (2) | 16.7% (4) | 75.0% (18) | 0% (0) |
| 3 Months Post-Retreat | ||||
| Completers % (n/19) | 31.6% (6) | 15.8% (3) | 52.6% (10) | 0% (0) |
| Intent to treat % (n/24) | 25.0% (6) | 12.5% (3) | 62.5% (15) | 0% (0) |
| Patient-Rated PTSD Symptom Severity (PCL-5) | ||||
| Recovered | Improved | Unchanged | Deteriorated | |
| 2 Weeks Post-Retreat | ||||
| Completers % (n/24) | 8.3% (2) | 33.3% (8) | 50.0% (12) | 8.3% (2) |
| Intent to treat % (n/24) | 8.3% (2) | 33.3% (8) | 50.0% (12) | 8.3% (2) |
| 1 Month Post-Retreat | ||||
| Completers % (n/16) | 12.5% (2) | 31.3% (5) | 56.3% (9) | 0% (0) |
| Intent to treat % (n/24) | 8.3% (2) | 20.8% (5) | 70.8% (17) | 0% (0) |
| 3 Months Post-Retreat | ||||
| Completers % (n/19) | 36.8% (7) | 31.6% (6) | 31.6% (6) | 0% (0) |
| Intent to treat % (n/24) | 29.2% (7) | 25.0% (6) | 45.8% (11) | 0% (0) |
Note. PTSD = Posttraumatic Stress Disorder; CAPS-5 = Clinician-Rated PTSD Scale for DSM-5; PCL-5 = PTSD Checklist for DSM-5.
Adverse events (AEs) were monitored throughout the trial using the STRONG STAR adverse events monitoring protocol, which is similar to how AEs are monitored in studies of medications or medical devices (Peterson, Roache, Raj, & Young-McCaughan, 2013). Sixteen patients reported a total of 26 AEs during the study, and 10 partners reported a total of 18 AEs. The most common AEs in patients were pain (n = 5), anger (n = 3), or agitation (n = 2), while anxiety (n = 4), stress (n = 2), and depression (n = 2) were most common in partners. Most AEs were not study-related, and the three serious AEs were all unrelated to the study (e.g., anaphylactic reaction). Four patients and three partners reported nonserious AEs that were at least possibly study-related. These included panic, agitation, social withdrawal, pain or swelling due to medical conditions neglected during the retreat (e.g., sciatica), and increased distress due to assessment.
PATIENT PTSD AND COMORBID SYMPTOMS, PARTNER PSYCHOLOGICAL DISTRESS, AND RELATIONSHIP SATISFACTION
Patient PTSD and Comorbid Symptoms
There was a significant difference in patients’ PTSD symptoms across assessments according to clinician ratings on the CAPS-5 (F(2,23) = 11.51, p < .001), patients’ self-report on the PCL-5 (F(3,23) = 11.42, p < .0001), and partners’ ratings on the collateral version of the PCL-5 (F(3,22) = 4.80, p = .010). Planned contrasts revealed significant and medium-to-large reductions in clinicians’ and patients’ ratings of PTSD symptoms by the 1-month follow-up and significant and large reductions by the 3-month follow-up, relative to baseline. According to partner report, there were marginally significant (p = .060) but small reductions in patients’ PTSD symptoms at 1-month follow-up and significant and medium reductions in patient symptoms by 3-month follow-up.
There was a significant difference across the three assessments for patients’ comorbid depressive (F(2,23) = 6.64, p = .005), anxiety (F(2,23) = 8.07, p = .002), and anger symptoms (F(2,23) = 4.15, p = .029). Relative to baseline, there were significant and medium reductions in patients’ depressive and anxiety symptoms at 1-month follow-up and significant and medium-to-large reductions at 3-month follow-up. Reductions in anger were significant and small-to-medium at 1-month follow-up and were significant and medium at 3-month follow-up, relative to baseline.
Partner Psychological Distress
There was a marginally significant difference in partners’ depressive symptoms across the three assessments (F(2,23) = 2.75, p = .085) and a significant difference in partners’ anxiety symptoms (F(2,23) = 5.56, p = .011). Planned contrasts indicated that there were significant and small-to-medium reductions in partners’ depressive symptoms and significant and medium reductions in anxiety symptoms observed by 3-month follow-up, relative to baseline. There was not a significant difference in partner anger across the three assessments (F(2,23) = 0.05, p = .954).
Relationship Satisfaction
There was not a significant difference in patients’ relationship satisfaction across the three assessments (F(2,23) = 0.13, p = .878). In contrast, there was a significant difference in partners’ relationship satisfaction (F(2,23) = 3.51, p = .047), with significant and medium increases in relationship satisfaction observed by 3-month follow-up, relative to baseline.
PTSD DIAGNOSTIC STATUS AND CLINICAL STATUS CATEGORIES
At the 1-month follow-up, 50% (8/16) of patients who completed the assessments no longer met diagnostic criteria for PTSD. By the 3-month follow-up, 63% (12/19) no longer met diagnostic criteria. Based on clinical evaluators’ ratings on the CAPS-5, 37.5% of patients who completed the assessment were classified as recovered or reliably improved by the 1-month follow-up, and this number increased to 47.4% by the 3-month follow-up. According to patients’ self-reported symptoms on the PCL-5, 43.8% of patients who completed the assessments were classified as recovered or reliably improved 1 month after treatment, and 68.4% were classified as recovered or reliably improved by the 3-month follow-up.
RELATIONALLY SATISFIED STATUS
Among patients, 66.7% (16/24) were relationally satisfied pretreatment. Among those who completed follow-up assessments, 76.5% (13/17) were relationally satisfied at 1-month follow-up, and 63.2% (12/19) were relationally satisfied at 3-month follow-up. Among partners, 50% (12/24) were relationally satisfied pretreatment. Of those who completed follow-up assessments, 72.2% (13/18) were relationally satisfied at the 1-month follow-up, and 78.6% (11/14) were relationally satisfied at the 3-month follow-up.
CLIENT SATISFACTION WITH TREATMENT
At 1- and 3-month follow-up, patients’ mean satisfaction with the intervention was 27.59 (SD = 2.81) and 27.95 (SD = 4.24), respectively. Partners’ mean satisfaction was 28.78 (3.12) and 27.86 (3.63), respectively. Collectively, this indicates a high degree of satisfaction with treatment by both partners.
MEDICATION CHANGES PRIOR TO TREATMENT
At study entry, there were five patients whose psychotropic medication regimens had changed within 8 weeks of the baseline assessment. Analyses were subsequently rerun without these patients to determine if the pattern of findings remained the same with respect to group-level patient outcomes and individual change categories for patient PTSD symptoms. The pattern of findings was the same with respect to group-level patient outcomes. For individual-level change in PTSD symptoms, among patients who completed follow-up assessments, the percent classified as recovered or reliably improved based on the CAPS-5 remained the same at 1-month follow-up (5/13, 38.5% vs. 6/16, 37.5%) and 3-month follow-up (7/15, 46.7% vs. 9/19, 47.4%). For patients’ self-reported symptoms on the PCL-5, proportions were 4/13 (30.8%) versus 7/16 (43.8%) at 1-month follow-up and were 11/15 (73.3%) versus 13/19 (68.4%) at 3-month follow-up.
Discussion
This nonrandomized pilot study served as an initial investigation of an abbreviated, intensive, multi-couple group version of CBCT for PTSD (AIM-CBCT for PTSD) with respect to patient PTSD and comorbid symptom severity, partners’ psychological distress, and both partners’ relationship satisfaction and satisfaction with the program. The massed treatment format represents a novel attempt to circumvent logistical barriers to the participation of military and veteran couples with PTSD by streamlining and condensing content from 15 weekly sessions into a single weekend of intensive couple therapy. In addition, we shifted from delivering the therapy to individual couples to groups of couples. This innovation provides developmental work for more scalable couple-based treatments for PTSD from a service delivery standpoint.
All 24 couples completed treatment, and treatment was well tolerated by both partners, with high satisfaction with the program. There were significant improvements across all patient symptom domains. By 1-month follow-up, there were medium-to-large reductions in clinician- and patient-rated PTSD symptoms, medium reductions in depressive and anxiety symptoms, and small-to-medium reductions in anger. By 3-month follow-up, there were large reductions in clinicians’ and patients’ ratings of PTSD symptoms, medium reductions in partner-rated PTSD symptoms, moderate-to-large reductions in depressive and anxiety symptoms, and medium reductions in anger. There were also significant improvements for partners. By 3-month follow-up, partners reported small-to-medium reductions in their depressive symptoms, medium reductions in their anxiety, and medium increases in their relationship satisfaction. In addition, we examined the proportion of patients who were either recovered or reliably improved. Of those completing the assessment 3 months after this 2-day treatment, nearly half (47.4%) were classified as recovered or reliably improved according to clinician assessment of PTSD symptoms and approximately two-thirds (68.4%) were classified as recovered or reliably improved according to self-reported PTSD symptoms.
Considered within the context of recent trials of evidence-based individual and group therapy for service members with PTSD conducted within the STRONG STAR Consortium, findings from the current trial are promising. For example, the magnitude of reductions in clinician-rated PTSD symptom severity by 3-month follow-up observed in this study (d = 0.98) is within the range of those observed at the final follow-up for large trials of cognitive processing therapy delivered individually or in a group (ds 0.90 to 1.21; Resick et al., 2017; Resick et al., 2015). A similar pattern of findings was observed for patient-rated PTSD symptoms (d = 1.17 at 3-month follow-up in the current trial, and ds of 0.60 to 1.30 for the other trials).
The 3-month follow-up effect sizes of 0.98 for clinician-rated symptoms and 1.17 for patient-rated symptoms for AIM-CBCT for PTSD are smaller than those observed for military/veteran couples treated with the traditional, 15-session format. For instance, Schumm et al. (2013), in their small, uncontrolled study of CBCT for PTSD delivered to post-9/11 veterans and their partners, reported ds of 1.51 and 1.43 for improvements in clinician- and patient-rated PTSD symptoms, respectively. However, the effect size for clinician-rated symptoms in this trial (d = 0.98) is similar to that observed after the first seven sessions of CBCT for PTSD in Monson et al.’s (2012) community sample in which the majority of patients were female civilians (d = 1.07; Macdonald, Fredman, & Monson, 2014). This suggests that abbreviated versions of CBCT for PTSD may reduce some challenges associated with standard care while delivering a majority of the benefits, which may have public health relevance for intervention access and reach.
Unlike partners, patients did not demonstrate an increase in relationship satisfaction by either the 1- or 3-month follow-up assessments, a pattern similar to that observed in other studies of CBCT for PTSD with samples comprised of predominantly male combat veterans with female partners (e.g., Monson, Schnurr, Stevens, & Guthrie, 2004; Schumm et al., 2013). Lambert et al.’s (2012) meta-analysis indicated that the negative association between PTSD symptoms and partners’ perceived relationship quality is stronger for female partners of male trauma survivors than for male partners of female trauma survivors. Indeed, patients in this trial, who were almost exclusively male, entered the study relatively more satisfied than partners, who were almost exclusively female. Thus, compared with partners, there may have been less opportunity for improvement of patients’ relationship satisfaction if they were relatively satisfied at the outset.
Through participation in programs such as the Army’s Strong Bonds marital enrichment weekends (www.strongbonds.org), many active-duty couples are likely to already be familiar with weekend retreats. This study also adds to the burgeoning data supporting the use of multi-dyad, retreat-style interventions for U.S. military and veteran couples. For example, in two studies of veterans from a wide range of service eras and their significant others participating in the Veteran Couples Integrative Intensive Retreat program (Monk, Ogolsky, & Bruner, 2016; Monk, Oseland, Nelson Goff, Ogolsky, & Summers, 2017), program evaluation data indicated that there were significant improvements in veterans’ self-reported PTSD symptoms, partners’ psychological distress, and intimate relationship adjustment for retreats conducted over 4 or 7 days. Relatedly, the multi-dyad format appears to be a useful format generally. For instance, REACH (Reaching out to Educate and Assist Caring, Healthy Families), a 9-month multifamily group psychoeducation program for veterans with PTSD and their family members, is associated with improvements in veterans’ and family members’ PTSD-related knowledge and coping skills, family functioning, and psychological distress in veterans from a wide range of service eras (Fischer, Sherman, Owen, & Han, 2013). Clinical interview-based assessment of post-9/11 veterans’ PTSD symptoms, as well as fidelity assessment of the interventions offered, will advance the field to determine the most efficient and effective methods for intervention.
There may be several reasons that this format of CBCT for PTSD was associated with significant improvements in patients’ PTSD and comorbid symptoms, partners’ psychological distress, and partners’ relationship satisfaction. First, as with the traditional delivery of CBCT for PTSD, it is a disorder-specific couple therapy designed to change behaviors, cognitions, and dyadic interactional patterns thought to maintain PTSD and relationship problems. Second, the single-weekend format allowed couples to intensively practice and consolidate skills without disruptions due to work demands or other schedule constraints. Third, the multi-couple group nature of this treatment likely afforded opportunities for vicarious learning from other couples grappling with similar individual and relational challenges through the normalization of experiences and sharing about successful skill use throughout the weekend. Interactions with other group members also served as opportunities to potentiate balanced thinking about the relative trustworthiness of unfamiliar others.
The continued reductions in PTSD symptoms over the follow-up period are also noteworthy and consistent with those observed in trials of other brief treatments for PTSD (e.g., Sloan, Marx, Lee, & Resick, 2018) as well as with other multi-couple group treatments for individual psychopathology (Kirby & Baucom, 2007). The relatively larger gains observed at the 3-month follow-up, compared with the more proximal 1-month follow-up assessment, may be a reflection of more accumulated opportunities for couples to continue practicing skills taught over the weekend and for both partners to perceive themselves and each other in a different light. Future studies that assess couples over a longer follow-up period (e.g., 6–12 months) would help to clarify whether AIM-CBCT for PTSD is associated with additional improvements in patient and partner well-being, as well as further increase confidence in the durability of gains.
This study provides compelling initial evidence for AIM-CBCT for PTSD for military and veteran couples with PTSD. However, the uncontrolled nature of the design is a notable limitation and precludes our ability to assert causal influence of the intervention on PTSD and related outcomes. Regression to the mean and natural recovery may have also inflated the size of the effects, although the small improvements in clinician-rated PTSD symptoms among those on waitlists in military/veteran samples (e.g., d = −0.24; Monson et al., 2006) suggests that these influences are likely to have been relatively modest. Evaluators’ knowledge that participants had received AIM-CBCT for PTSD is another limitation. Finally, the small sample size precluded statistical analyses accounting for all types of possible nesting of data (e.g., within couples, cohorts, therapists). Given that this was a proof-of-concept study to determine if it was possible to safely treat PTSD in a multi-couple group format in a single weekend, the decision was made to first pilot this new format in a relatively small (N = 24) sample of couples in a nonrandomized trial. Evaluation of AIM-CBCT for PTSD with a randomized controlled trial is required to demonstrate efficacy. This would also permit a more rigorous estimation of effect sizes. Future studies should include a larger sample, greater diversity of sexual orientation, a longer follow-up period, and a greater proportion of female service members and veterans, as women’s PTSD symptoms appear to be particularly responsive to the inclusion of family members in their mental health care (Laws, Glynn, McCutcheon, Schmitz, & Hoff, 2018).
The current study adds to the growing evidence base for couple-based interventions for PTSD and suggests novel possibilities for increasing the engagement and retention of post-9/11 service members and veterans with PTSD and their partners. Initial results from this pilot study are encouraging and indicate that future research is warranted to formally test the efficacy of this new modality. An efficient and potentially scalable conjoint therapy for PTSD offers the hope of increasing the reach of treatments that improve the well-being of the many service members, veterans, and family members whose lives have been touched by trauma and its aftereffects.
Acknowledgments
This research is supported by Consortium to Alleviate PTSD (CAP) award numbers W81XWH-13-2-0065 from the U.S. Department of Defense, Defense Health Program, Psychological Health and Traumatic Brain Injury Research Program (PH/TBI RP), and I01CX001136-01 from the U.S. Department of Veterans Affairs, Office of Research & Development, Clinical Science Research & Development Service. Additional funding comes from the Karl R. Fink and Diane Wendle Fink Early Career Professorship for the Study of Families and startup funds from The Pennsylvania State University to Steffany J. Fredman, grants KL2 TR002015 and UL1 TR002014 from the National Center for Advancing Translational Sciences to the Pennsylvania State University to support Steffany J. Fredman’s time, and the Military Health Institute at The University of Texas Health Science Center at San Antonio. We thank Michelle Barrera, Antoinette Brundige, John Kelly, and R. Bryce Williams for administrative support; Raymond Aguilar, Yiwen Xu, and Xueying Li for assistance with database management and statistical analyses; Timothy Brick, Damon Jones, Yogev Kivity, and Suzanne Pineles for consultation regarding data analysis; Andrea Myers, Amanda Proctor, and Venée Hummel for assistance with the weekend retreats; and Andréa Hobkirk, Nicole Pukay-Martin, and Steven Zarit for feedback on the manuscript.
The views expressed herein are solely those of the authors and do not reflect an endorsement by or the official policy or position of the U.S. Army, the Department of Defense, the Department of Veterans Affairs, the National Institutes of Health, or the U.S. Government.
The grant sponsor played no role in study design; the collection, analysis, and interpretation of data; the writing of this paper; or the decision to submit this paper for publication.
Footnotes
Conflict of Interest Statement
Steffany J. Fredman and Candice M. Monson receive royalties from Guilford Press for their published treatment manual on cognitive-behavioral conjoint therapy for PTSD. No other authors have conflicts of interest to declare.
Among partners, ethnicity had a medium size negative association with missingness (ϕ = −0.42) such that partners who self-identified as Hispanic were less likely to have missing data. When ethnicity was included in the model for partner depression, the p value for the baseline/3-month follow-up contrast increased from .035 to .055. When ethnicity was included in the model for partner relationship satisfaction, the p value for the overall effect of visit increased from .047 to .060, although the baseline/3-month follow-up contrast remained significant. The pattern of significant findings was unchanged for all other patient and partner outcomes.
Contributor Information
Steffany J. Fredman, The Pennsylvania State University
Alexandra Macdonald, The Citadel, Military College of South Carolina.
Candice M. Monson, Ryerson University
Katherine A. Dondanville, The University of Texas Health Science Center at San Antonio
Tabatha H. Blount, The University of Texas Health Science Center at San Antonio
Brittany N. Hall-Clark, The University of Texas Health Science Center at San Antonio
Brooke A. Fina, The University of Texas Health Science Center at San Antonio
Jim Mintz, The University of Texas Health Science Center at San Antonio.
Brett T. Litz, VA Boston Healthcare System, Boston University School of Medicine
Stacey Young-McCaughan, The University of Texas Health Science Center at San Antonio.
Allison K. Hancock, The University of Texas Health Science Center at San Antonio
Galena K. Rhoades, University of Denver
Jeffrey S. Yarvis, Carl R. Darnall Army Medical Center, Fort Hood, Texas
Patricia A. Resick, Duke University
John D. Roache, The University of Texas Health Science Center at San Antonio
Yunying Le, The Pennsylvania State University.
Jennifer S. Wachen, National Center for PTSD, VA Boston Healthcare System, Boston University School of Medicine
Barbara L. Niles, National Center for PTSD, VA Boston Healthcare System, Boston University School of Medicine
Cindy A. McGeary, The University of Texas Health Science Center at San Antonio
Terence M. Keane, National Center for PTSD, VA Boston Healthcare System, Boston University School of Medicine
Alan L. Peterson, The University of Texas Health Science Center at San Antonio, South Texas Veterans Health Care System, The University of Texas at San Antonio
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Attkisson CC, & Greenfield TK (2004). The UCSF Client Satisfaction Scales: I. The Client Satisfaction Questionnaire-8. In Maruish ME (Ed.), The use of psychological testing for treatment planning and outcomes assessment (pp. 1333–1346). Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Barnes JB, Presseau C, Jordan AH, Kline NK, Young-McCaughan S, Keane TM, … Litz BT; and the Consortium to Alleviate PTSD. (2019). Common data elements for military-related PTSD research applied in the Consortium to Alleviate PTSD. Military Medicine, 184, e218–e226. doi: 10.1093/milmed/usy226 [DOI] [PubMed] [Google Scholar]
- Berke DS, Kline NK, Wachen JS, McLean CP, Yarvis JS, Mintz J, … Litz BT; for the STRONG STAR Consortium. (2019). Predictors of attendance and dropout in PTSD treatment for active duty service members. Behaviour Therapy and Research, 118, 7–17. doi: 10.1016/j.brat.2019.03.003. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Renshaw KD, Kashdan TB, Curby TW, & Carter SP (2017). A daily diary study of posttraumatic stress symptoms and romantic partner accommodation. Behavior Therapy, 48, 222–234. doi: 10.1016/j.beth.2016.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences. (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Davis L, Luedtke BL & Monson CM (2015, August). Outcomes of two CBCT adaptations: Implications for future treatment and research. Paper presented at the annual meeting of the American Psychological Association Annual Convention, Toronto, Canada. [Google Scholar]
- Ehlers A, Hackmann A, Grey N, Wild J, Liness S, Albert I,… Clark DM (2014). A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. American Journal of Psychiatry, 171, 294–304. doi: 10.1176/appi.ajp.2013.13040552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer EP, Sherman MD, Owen R, & Han X (2013). Outcomes of participation in the REACH multifamily group program for Veterans with PTSD and their families. Professional Psychology: Research and Practice, 44, 127–134. doi: 10.1037/a0032024 [DOI] [Google Scholar]
- Foa EB, Hembree EA, & Rothbaum BO (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences: Therapist guide. New York, NY: Oxford University Press. [Google Scholar]
- Foa EB, McLean CP, Zang Y, Rosenfield D, Yadin E, Yarvis JS, … Peterson AL; for the STRONG STAR Consortium. (2018). Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: A randomized clinical trial. Journal of the American Medical Association, 319, 354–364. doi: 10.1001/jama.2017.21242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredman SJ, Vorstenbosch V, Wagner AC, Macdonald A, & Monson CM (2014). Partner accommodation in posttraumatic stress disorder: Initial testing of the Significant Others’ Response to Trauma Scale (SORTS). Journal of Anxiety Disorders, 28, 372–381. doi: 10.1016/j.janxdis.2014.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, … Beckham JC (2015). The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans: A meta-analysis. Journal of Anxiety Disorders, 31, 98–107. doi: 10.1016/j.janxdis.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Funk JL, & Rogge RD (2007). Testing the ruler with item response theory: Increasing precision of measurement for relationship satisfaction with the Couples Satisfaction Index. Journal of Family Psychology, 21, 572–583. doi: 10.1037/0893-3200.21.4.572 [DOI] [PubMed] [Google Scholar]
- Grubbs F. (1969). Procedures for detecting outlying observations in samples. Technometrics, 11, 1–21. doi: 10.2307/1266761 [DOI] [Google Scholar]
- Imel ZE, Laska K, Jakupcak M, & Simpson TL (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81, 394–404. doi: 10.1037/a0031474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, & Truax P (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59, 12–19. doi: 10.1037/0022-006X.59.1.12 [DOI] [PubMed] [Google Scholar]
- Kirby JS, & Baucom DH (2007). Treating emotion dysregulation in a couples context: A pilot study of a couples skills group intervention. Journal of Marital and Family Therapy, 33, 375–391. doi: 10.1111/j.1752-0606.2007.00037.x [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert JE, Engh R, Hasbun A, & Holzer J (2012). Impact of posttraumatic stress disorder on the relationship quality and psychological distress of intimate partners: A meta-analytic review. Journal of Family Psychology, 26, 729–37. doi: 10.1037/a0029341 [DOI] [PubMed] [Google Scholar]
- Laws HB, Glynn SM, McCutcheon SJ, Schmitz TM, & Hoff R (2018). Posttraumatic stress symptom change after family involvement in veterans' mental health care. Psychological Services, 15, 520–528. doi: 10.1037/ser0000200. [DOI] [PubMed] [Google Scholar]
- Little RJA (1988). A test of Missing Completely at Random for multivariate data with missing values. Journal of the American Statistical Association, 83: 404, 1198–1202, doi: 10.1080/01621459.1988.10478722 [DOI] [Google Scholar]
- Macdonald A, Fredman SJ, & Monson CM (2014). Cognitive-behavioral conjoint therapy for PTSD: Effects by phase of treatment. Unpublished raw data. [Google Scholar]
- Monk JK, Ogolsky BG, & Bruner V (2016). Veteran couples integrative intensive retreat model: An intervention for military veterans and their relational partners. Journal of Couple & Relationship Therapy, 15, 158–176. doi: 10.1080/15332691.2015.1089803 [DOI] [Google Scholar]
- Monk JK, Oseland LM, Nelson Goff BS, Ogolsky BG, & Summers K (2017). Integrative intensive retreats for veteran couples and families: A pilot study assessing change in relationship adjustment, posttraumatic growth, and trauma symptoms. Journal of Marital and Family Therapy, 43, 448–462. doi: 10.1111/jmft.12230 [DOI] [PubMed] [Google Scholar]
- Monson CM, & Fredman SJ (2012). Cognitive-behavioral conjoint therapy for posttraumatic stress disorder: Harnessing the healing power of relationships. New York, NY: Guilford Press. [Google Scholar]
- Monson CM, Fredman SJ, Macdonald AM, Pukay-Martin ND, Resick PA, & Schnurr PP (2012). Effect of cognitive-behavioral couple therapy for PTSD: A randomized controlled trial. Journal of the American Medical Association, 308, 700–709. doi: 10.1001/jama.2012.9307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, & Stevens SP (2006). Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 74, 898–907. doi: 10.1037/0022-006X.74.5.898 [DOI] [PubMed] [Google Scholar]
- Monson CM, Wagner AC, Pukay-Martin N, Blount T, Riggs DR, & the STRONG STAR Consortium. (2017, October). A randomized controlled trial of cognitive-behavioral conjoint therapy versus prolonged exposure for PTSD in active duty service members, veterans, and their intimate partners: Understanding dropout. Paper presented at the annual San Antonio Combat PTSD Conference, San Antonio, TX. [Google Scholar]
- Peterson AL, Roache JD, Raj J, & Young-McCaughan S; for the STRONG STAR Consortium. (2013). The need for proper adverse events monitoring in behavioral health clinical trials. Contemporary Clinical Trials, 34, 152–154. doi: 10.1016/j.cct.2012.10.009 [DOI] [PubMed] [Google Scholar]
- Resick PA, Monson CM, & Chard KM (2016). Cognitive processing therapy: A comprehensive guide. New York, NY: Guilford. [Google Scholar]
- Resick PA, Wachen JS, Dondanville KA, Pruiksma KE, Yarvis JS, Peterson AL,, & Mintz, J.; and the STRONG STAR Consortium. (2017). Effect of group vs individual cognitive processing therapy in active-duty military seeking treatment for posttraumatic stress disorder: A randomized clinical trial. JAMA Psychiatry, 74, 28–36. doi: 10.1001/jamapsychiatry.2016.2729 [DOI] [PubMed] [Google Scholar]
- Resick PA, Wachen JS, Mintz J, Young-McCaughan S, Roache JD, Borah AM, … Peterson AL; on behalf of the STRONG STAR Consortium. (2015). A randomized clinical trial of group cognitive processing therapy compared with group present-centered therapy for PTSD among active duty military personnel. Journal of Consulting and Clinical Psychology, 83, 1058–1068. doi: 10.1037/ccp0000016 [DOI] [PubMed] [Google Scholar]
- Schumm JA, Fredman SJ, Monson CM, & Chard KM (2013). Cognitive-behavioral conjoint therapy for PTSD: Initial findings for Operations Enduring and Iraqi Freedom male combat veterans and their partners. American Journal of Family Therapy, 41, 277–287. doi: 10.1080/01926187.2012.701592 [DOI] [Google Scholar]
- Shnaider P, Pukay-Martin ND, Fredman SJ, Macdonald A, & Monson CM (2014). Does cognitive-behavioral conjoint therapy for PTSD affect partners’ psychological functioning? Journal of Traumatic Stress, 27, 129–136. doi: 10.1002/jts.21893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan DM, Marx BP, Lee DJ, & Resick PA (2018). A brief exposure-based treatment vs cognitive processing therapy for posttraumatic stress disorder: A randomized noninferiority clinical trial. JAMA Psychiatry, 75, 233–239. doi: 10.1001/jamapsychiatry.2017.4249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, & Lowe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166, 1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Spielberger CD (1999). State-Trait Anger Expression Inventory-2 (STAXI-2): Professional manual. Tampa, FL: Psychological Assessment Resources. [Google Scholar]
- Straus MA, Hamby SL, McCoy SB, & Sugarman DB (1996). The Revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues, 17, 283–316. doi: 10.1177/019251396017003001 [DOI] [Google Scholar]
- Taft CT, Watkins LE, Stafford J, Street AE, & Monson CM (2011). Posttraumatic stress disorder and intimate relationship problems: A meta-analysis. Journal of Consulting and Clinical Psychology, 79, 22–33. doi: 10.1037/a0022196 [DOI] [PubMed] [Google Scholar]
- Tarrier N, Sommerfield C, & Pilgrim H (1999). Relatives' expressed emotion (EE) and PTSD treatment outcome. Psychological Medicine, 29, 801–811. doi: 10.1017/s0033291799008569 [DOI] [PubMed] [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, & Hoge CW (2010). Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry, 67, 614–623. doi: 10.1001/archgenpsychiatry.2010.54 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). Interview available from the National Center for PTSD at www.ptsd.va.gov [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov [Google Scholar]