Abstract
Background
Vaccine hesitancy is a major obstacle to the large efforts made by governments and health organizations toward achieving successful COVID-19 vaccination programs. Healthcare worker’s (HCWs) acceptance or refusal of the vaccine is an influencing factor to the attitudes of their patients and general population. This study aimed to report the acceptance rates for COVID-19 vaccines among HCWs in Arab countries and identify key factors driving the attitudes of HCWs in the Arab world toward vaccines.
Methods
This systematic review and meta-analysis followed the PRISMA guidelines. PubMed and Scopus databases were searched using pre-specified keywords. All cross-sectional studies that assessed COVID-19 vaccine hesitancy and/or acceptance among HCWs in Arab countries until July 2022, were included. The quality of the included studies and the risk of bias was assessed using the JBI critical appraisal tool. The pooled acceptance rate of the COVID-19 vaccine was assessed using a random-effects model with a 95% confidence interval.
Results
A total of 861 articles were identified, of which, 43 were included in the study. All the studies were cross-sectional and survey-based. The total sample size was 57,250 HCWs and the acceptance rate of the COVID-19 vaccine was 60.4% (95% CI, 53.8% to 66.6%; I2, 41.9%). In addition, the COVID-19 vaccine acceptance rate among males was 65.4% (95% CI, 55.9% to 73.9%; I2, 0%) while among females was 48.2% (95% CI, 37.8% to 58.6%; I2, 0%). The most frequently reported factors associated with COVID-19 vaccine acceptance were being male, higher risk perception of contracting COVID-19, positive attitude toward the influenza vaccine, and higher educational level. Predictors of vaccine hesitancy most frequently included concerns about COVID-19 vaccine safety, living in rural areas, low monthly income, and fewer years of practice experience.
Conclusion
A moderate acceptance rate of COVID-19 vaccines was reported among HCWs in the Arab World. Considering potential future pandemics, regulatory bodies should raise awareness regarding vaccine safety and efficacy and tailor their efforts to target HCWs who would consequently influence the public with their attitude towards vaccines.
Introduction
The coronavirus disease of 2019 (COVID-19) pandemic has resulted in a huge negative impact on global health and the economy. Even though hygienic and behavioral control measures are effective in tackling pandemics, vaccines have been proposed as the single most important method to provide protection and control the spread of the virus [1]. The World Health Organization (WHO) estimates that vaccinations prevent between 3.5 and 5 million deaths every year [2]. Since the start of the pandemic and the spread of the virus, efforts to create vaccines have been accelerated to prevent and control the disease.
Vaccine hesitancy has been considered by the WHO as a global health threat in 2019 as it is deemed a barrier to the success of vaccination programs [3]. Vaccine hesitancy has been defined by the Strategic Advisory Group of Experts on Immunization (SAGE) as “a delay in acceptance or refusal of vaccination despite the availability of vaccination services” [4]. There are multiple determinants that influence the attitude in relation to the acceptance of vaccination, including complacency, convenience, and confidence [4]. Multiple previous studies indicated that vaccine acceptance, in general, is declining globally, even though it has been proven that vaccines are safe and effective in controlling the spread and reducing mortality rates [5–9]. The three most common reasons for vaccine hesitancy are risk vs. benefit concerns, lack of awareness and knowledge of vaccinations and their importance, and certain religious and cultural beliefs [7].
In terms of COVID-19, surveys conducted prior to the availability of COVID-19 vaccines in the United States showed that 70% of residents planned to receive the vaccine when available [10]. On the other hand, an international study that investigated the attitudes of healthcare workers (HCWs) toward COVID-19 vaccination found that the rates of high acceptance, moderate acceptance, and hesitancy to receive the vaccine were 48.6%, 23%, and 28.4%, respectively. In addition, 40.88% agreed that the concern about vaccine safety was the most prevalent factor for vaccine hesitancy [11].
Recent studies have demonstrated multiple predictors of COVID-19 vaccine acceptance and/or hesitancy among HCWs. In a systematic review and meta-analysis, Ackah et. al. estimated Covid-19 vaccine acceptance in Africa among HCWs and the associated hesitancy predictors. The study reported a low acceptance rate of 46% that was associated with concerns about vaccines’ safety and efficacy, limited data, and expedited COVID-19 vaccine clinical trials [12].
Vaccine hesitancy and low acceptance rates are major obstacles to the large efforts made by governments and health organizations toward achieving successful COVID-19 vaccination programs [13, 14]. It is important that HCWs receive the vaccine and promote receiving it as they are on the frontlines in defending against COVID-19, which puts them at risk of being disease victims, as well as disease transmitters. This risk arises from frequent contact with COVID-19 patients, visitors, and other HCWs [15]. Moreover, HCWs are considered a reliable and trustworthy source of information by their patients and the public, which makes their acceptance or refusal of the vaccine an influencing factor for the attitudes of their patients and the general population toward receiving the vaccine [16]. Several studies from Arab World countries surveyed HCWs regarding their perception and attitude toward receiving the COVID-19 vaccine. This systematic review and meta-analysis aimed to report the acceptance rates for COVID-19 vaccines among HCWs in Arab countries and identify the predictors of vaccine acceptance. Findings from this review should benefit governments, decision-makers, and other HCWs in identifying key factors driving the attitudes of HCWs in the Arab world toward vaccines and inform decisions that can help change vaccine hesitancy to acceptance of booster doses for COVID-19, future pandemics, as well as when new critical vaccines are introduced into the market.
Methods
The reporting of this systematic review and meta-analysis was done in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [17]. The methodology was based on the manual for evidence synthesis by the Joanna Briggs Institute (JBI) [18].
Search strategy and study selection
PubMed and Scopus databases were searched independently by MA and AKT using the following keywords: (COVID-19 OR SARS-CoV-2 OR coronavirus) AND (vaccin* OR immunization* OR immunisation*) AND (hesitan* OR reluct* OR refus* OR accept* OR willing* OR intent* OR intend* OR reject* OR delay*) AND (Algeria OR Bahrain OR Comoros OR Djibouti OR Egypt OR Iraq OR Jordan OR Kuwait OR Lebanon OR Libya OR Mauritania OR Morocco OR Oman OR Palestine OR Qatar OR Saudi OR Somalia OR Sudan OR Syria OR Tunisia OR Emirates OR Yemen OR Arab*). The title and abstract screening process was performed by MA and AKT. Disagreements were handled via a discussion with the other study authors. All quantitative cross-sectional studies that assessed COVID-19 vaccine hesitancy and/or acceptance among HCWs in Arab countries up till July 25, 2022, were included. Qualitative (interview-based) studies and studies that included both HCWs along with the general public or students at schools of health sciences without reporting subgroup findings of HCWs were excluded.
Data extraction
Using a standardized data extraction form, data extraction was executed independently by five authors, MA, MAA, YG, HA, and MJA. The extracted data included the primary author’s name, year of publication, country, the profession of study participants, number of participants accepting the vaccine, the total number of participants, and predictors of vaccine hesitancy and acceptance. Controversies were resolved after a discussion with AKT, JJ, and KE. The data extraction process was revised independently by AKT and JJ.
Quality assessment
The quality of the included studies and the risk of bias was assessed using the JBI critical appraisal tool (18) by the same authors who performed the data extraction. Disagreements were handled via a discussion with AKT, KE, and JJ. The quality assessment process was revised by AKT.
Meta-analysis and data synthesis
The pooled acceptance rate of COVID-19 vaccine was assessed using a random-effects model with a 95% confidence interval (95% CI). Heterogeneity (I2) was assessed using Cochrane’s Q test. Subgroup analyses were performed to report the acceptance rate per country.
Results
Search results
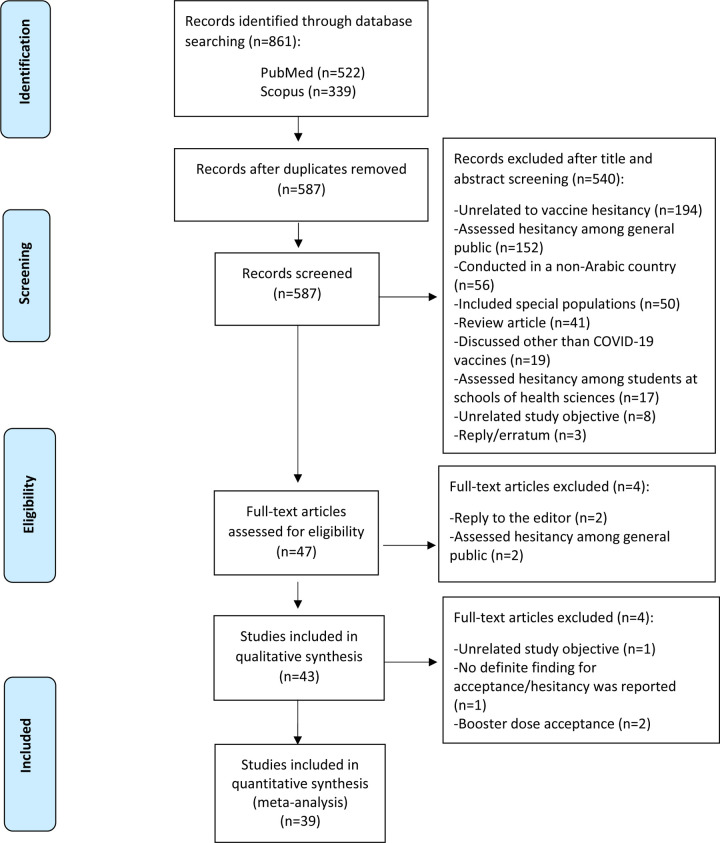
A total of 861 records were identified, where only 47 full-text articles met the inclusion criteria. Of the 47 full-text articles screened, 43 and 39 studies were included in the qualitative and quantitative synthesis, respectively. The reasons for excluding the other 514 studies are explained in the PRISMA flowchart (Fig 1). Four of the 47 eligible studies were excluded from the meta-analysis due to the following reasons: assessed hesitancy toward the booster dose exclusively [19, 20] reported vaccine hesitancy to each available vaccine rather than to the concept of vaccination as a whole [21], and assessed hesitancy using several questions with varied answers to each question [22].
Fig 1. PRISMA flowchart of literature search and review.
Characteristics of the included studies
The included studies are summarized in Table 1. All 39 included quantitative studies were cross-sectional and survey-based and were distributed to HCWs between July 2020 and November 2021. Most of the data were collected after December 2020 when the vaccines were available in many countries.
Table 1. The included studies for the quantitative analysis.
| Author | Country | Date of the survey | Profession of study participants | Number of Participants Accepting the Vaccine | Total Number of Participants (i.e., Sample Size) | |
|---|---|---|---|---|---|---|
| 1 | Alhofaian et al. | SA | Mar 2021 –Apr 2021 | Non-specific | 298 | 383 |
| 2 | Arif et al. | SA | Jul 2021 –Sep 2021 | Non-specific | 529 | 529 |
| 3 | Baghdadi et al. | SA | Jul 2020 –Sep 2020 | Non-specific | 222 | 363 |
| 4 | Barry et al. | SA | Nov 2020 | Non-specific | 1058 | 1512 |
| 5 | Elharake et al. | SA | Oct 2020 –Dec 2020 | Non-specific | 15299 | 23582 |
| 6 | Hershan et al. | SA | Dec 2020 | Non-specific | 104 | 186 |
| 7 | Maqsood et al. | SA | April 2021 –May 2021 | Non-specific | 996 | 1031 |
| 8 | Qattan et al. | SA | Dec 2020 | Non-specific | 340 | 673 |
| 9 | Temsah et al. | SA | Dec 2020 –Jan 2021 | Non-specific | 352 | 1058 |
| 10 | Yassin et al. | Sudan | April 2021 | Non-specific | 254 | 400 |
| 11 | Al Awaidy et al. | Oman | Dec 2020 | Non-specific | 264 | 608 |
| 12 | Khamis et al. | Oman | Jan-Feb 2021 | Non-specific | 176 | 433 |
| 13 | Maraqa et al. | Palestine | Dec 2020-Jan 2021 | Non-specific | 438 | 1159 |
| 14 | Belkebir et al. | Palestine | Jan 2021 | Nurses | 15 | 46 |
| 15 | Rabi et al. | Palestine | Jan 2021 | Nurses | 517 | 638 |
| 16 | Kumar et al. | Qatar | Oct-Nov 2020 | Non-specific | 619 | 1414 |
| 17 | Zammit et al. | Tunisia | Jan 2021 | Non-specific | 237 | 493 |
| 18 | Albahri et al. | UAE | Jul 2020 | Physicians and nurses | 104 | 176 |
| 19 | AlKetbi et al. | UAE | Nov 2020-Feb 2021 | Non-specific | 2525 | 2832 |
| 20 | Saddik et al. | UAE | Nov 2020 ‐ Jan 2021 | Non-specific | 312 | 517 |
| 21 | Aloweidi et al. | Jordan | Jan 2021 ‐ Feb 2021 | Non-specific | 131 | 287 |
| 22 | Lataifeh et al. | Jordan | Feb2021- March 2021 | Physicians and Nurses (including midwives) | 233 | 364 |
| 23 | Qunaibi et al. | Multi-national | 14–29 Jan 2021 | Non-specific | 1522 | 5708 |
| 24 | Al-Sanafi et al. | Kuwait | 18–29 March 2021 | Non-specific | 849 | 1019 |
| 25 | Nasr et al. | Lebanon | 15–22 Feb 2021 | Dentists | 455 | 529 |
| 26 | Youssef et al. | Lebanon | 10–31 Dec 2020 | Non-specific | 1044 | 1800 |
| 27 | Elhadi et al. | Libya | 1–18 Dec 2020 | Non-specific | 1781 | 2215 |
| 28 | Khalis et al. | Morocco | First 3 weeks of Jan 2021 | Non-specific | 119 | 170 |
| 29 | Ahmed et al. | SA | Not mentioned | Non-specific | 131 | 236 |
| 30 | Aldosary et al. | SA | Nov 2020 ‐ Dec 2020 | Nurses | 236 | 334 |
| 31 | Hammam et al. | Egypt | 1 week during April 2021 | Rheumatologist | 57 | 187 |
| 32 | Fares et al. | Egypt | Dec 2020 ‐ Jan 2021 | Non-specific | 81 | 385 |
| 33 | Elkhayat et al. | Egypt | Jun 2021 ‐ Aug 2021 | Non-specific | 142 | 341 |
| 34 | El-Sokkary et al. | Egypt | January 25 ‐ 31, 2021 | Non-specific | 80 | 308 |
| 35 | El Kibbi et al. | Arab World | April 13 ‐ May 11, 2021 | Non-specific | 1237 | 1517 |
| 36 | Noushad et al. | SA | Feb 2021 ‐ March 2021 | Non-specific | 433 | 674 |
| 37 | Shehata et al. | Egypt | March 2021 –May 2021 | Physicians | 495 | 1268 |
| 38 | Sharaf et al. | Egypt | Aug 2021 –Oct 2021 | dental faculty | 78 | 171 |
| 39 | Luma et al. | Iraq | Feb 2021 | Non-specific | 1229 | 1704 |
SA, Saudi Arabia; UAE, United Arab Emirates, Non-specific, included more than two healthcare professions.
Most of the studies were from Saudi Arabia (n = 15) [19–21, 23–34] followed by Egypt (n = 6) [35–40], Jordan (n = 3) [22, 41, 42], Palestine (n = 3) [43–45], United Arab Emirates (n = 3) [46–48], Iraq (n = 2) [49, 50], Lebanon (n = 2) [51, 52], and Oman (n = 2) [53, 54]. Only one study was found for each of the following countries: Kuwait [55], Libya [56], Morocco [57], Qatar [58], Sudan [59], and Tunisia [60]. No studies were found from the remaining eight Arab countries (Algeria, Bahrain, Yemen, Somalia, Syria, Mauritania, Djibouti, and Comoros Islands). Two studies reported vaccine hesitancy in HCWs among different Arab countries. Firstly, the ARCOVAX study which is a large cross-sectional study conducted among HCWs in 19 Arab countries [61]. Another study by Qunaibi et al. included Arabic-speaking HCWs residing inside and outside Arab countries [62].
The sample size per study ranged from 46 to 23,582 (median = 568) and the total sample size was 57,250. Of the chosen studies, 27 included < 1000 participants, 15 included 1000–3000 participants, and two included > 3000 participants.
While most studies targeted more than two HCWs professions (n = 35), others targeted the following: physicians and nurses (n = 2) [42, 46]; dentists/dental faculty (n = 2) [39, 51]; nurses (n = 3) [33, 44, 45]; rheumatologists (n = 1) [35]; and physicians (n = 1) [40].
The methodological quality of the included studies
S1 Table represents the quality assessment of the included studies using the JBI tool. The risk of bias was low for 37 studies and medium for seven studies [20, 23, 33, 35, 38, 40, 44].
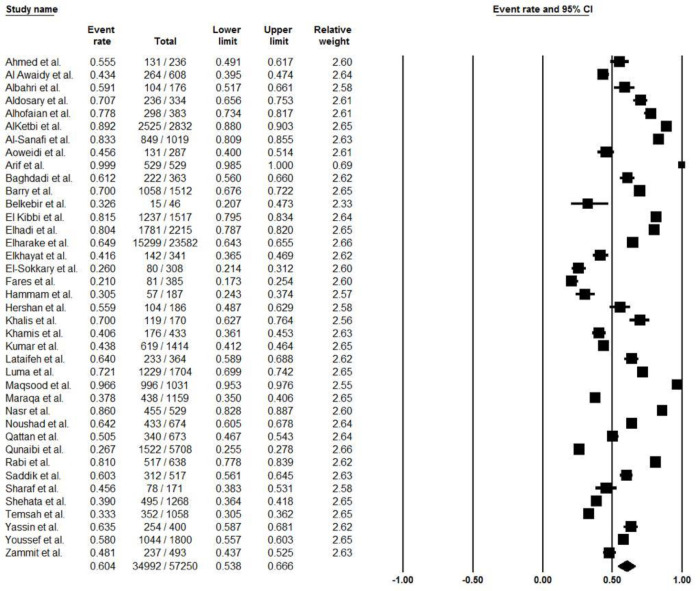
COVID-19 vaccine acceptance rate in Arab countries
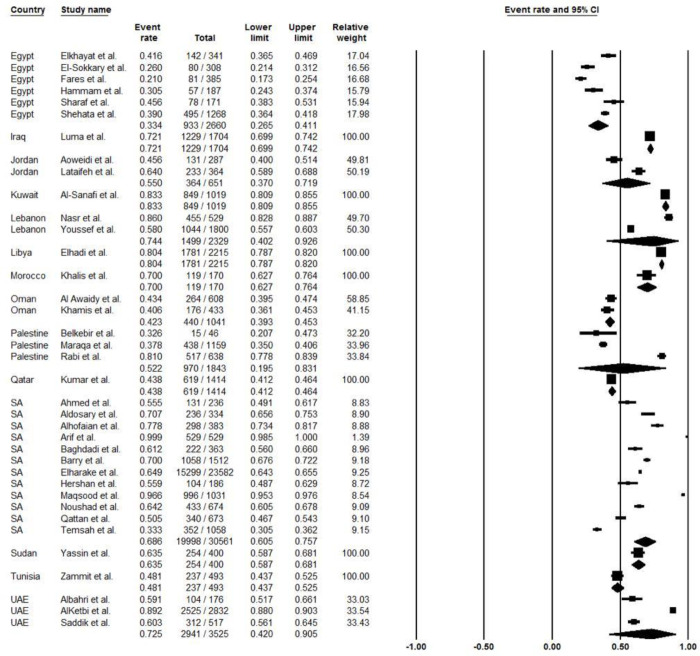
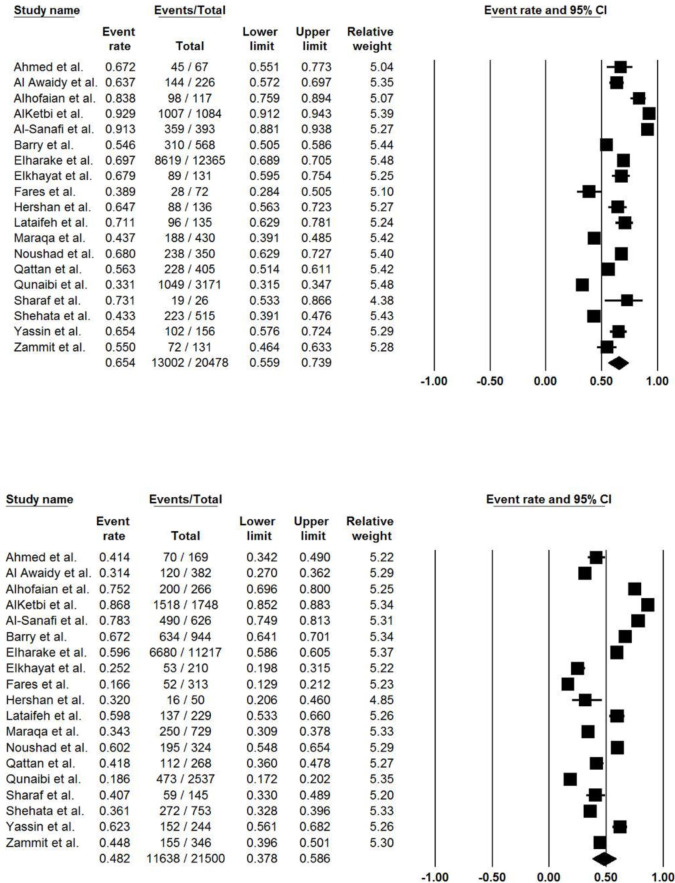
The pooled acceptance rate of COVID-19 vaccine was 60.4% (95% CI, 53.8% to 66.6%; I2, 41.9%) (Fig 2). The pooled vaccine acceptance rate estimated for each country was as follows: Egypt 33.4% (95% CI, 26.5% to 41.1%; I2, 13.7%), Jordan 55.0% (95% CI, 37.0% to 71.9%; I2, 0%), Lebanon 74.4% (95% CI, 40.2% to 92.6%; I2, 0%), Oman 42.3% (95% CI, 39.3% to 45.3%; I2, 0%), Palestine 52.2% (95% CI, 19.5% to 83.1%; I2, 0%), Saudi Arabia 68.6% (95% CI, 60.5% to 75.7%; I2, 74.9%), and United Arab Emirates 72.5% (95% CI, 42.0% to 90.5%; I2, 0%) (Fig 3). In addition, the COVID-19 vaccine acceptance rate among males was 65.4% (95% CI, 55.9% to 73.9%; I2, 0%) while among females was 48.2% (95% CI, 37.8% to 58.6%; I2, 0%) (Table 2), (Fig 4).
Fig 2. The overall acceptance rate of COVID-19 vaccines among Arab countries.
Fig 3. The acceptance rate of COVID-19 vaccines by country.
Table 2. COVID-19 vaccine acceptance among HCWs stratified by sex.
| Author | Country | Number of Participants Accepting the Vaccine | Total Number of Participants (i.e., Sample Size) | |||||
|---|---|---|---|---|---|---|---|---|
| Total | Male | Female | Total | Male | Female | |||
| 1. | Ahmed et al. | SA | 131 | 45 | 70 | 236 | 67 | 169 |
| 2. | Al Awaidy et al. | Oman | 264 | 144 | 120 | 608 | 226 | 382 |
| 3. | Albahri et al. | UAE | 104 | NR | NR | 176 | 18 | 158 |
| 4. | Aldosary et al. | SA | 236 | NR | NR | 334 | 25 | 309 |
| 5. | Alhofaian et al. | SA | 298 | 98 | 200 | 383 | 117 | 266 |
| 6. | AlKetbi et al. | UAE | 2525 | 1007 | 1518 | 2832 | 1084 | 1748 |
| 7. | Al-Sanafi et al. | Kuwait | 849 | 359 | 490 | 1019 | 393 | 626 |
| 8. | Aloweidi et al. | Jordan | 131 | NR | NR | 287 | 97 | 190 |
| 9. | Arif et al. | SA | 529 | NR | NR | 529 | 167 | 362 |
| 10. | Baghdadi et al. | SA | 222 | 107 | 115 | 363 | NR | NR |
| 11. | Barry et al. | SA | 1058 | 310 | 634 | 1512 | 568 | 944 |
| 12. | Belkebir et al. | Palestine | 15 | NR | NR | 46 | 13 | 33 |
| 13. | EI Kibbi et al. | Arab World | 1237 | NR | NR | 1517 | NR | NR |
| 14. | Elhadi et al. | Libya | 1781 | NR | NR | 2215 | 743 | 1472 |
| 15. | Elharake et al. | SA | 15299 | 8619 | 6680 | 23582 | 12365 | 11217 |
| 16. | Elkhayat et al. | Egypt | 142 | 89 | 53 | 341 | 131 | 210 |
| 17. | EI-Sokkary et al. | Egypt | 80 | 29 | 51 | 308 | NR | NR |
| 18. | Fares et al. | Egypt | 81 | 28 | 52 | 385 | 72 | 313 |
| 19. | Hammam et al. | Egypt | 57 | NR | NR | 187 | 28 | 159 |
| 20. | Hershan et al. | SA | 104 | 88 | 16 | 186 | 136 | 50 |
| 21. | Khalis et al. | Morocco | 119 | NR | NR | 170 | NR | NR |
| 22. | Khamis et al. | Khamis | 176 | NR | NR | 433 | 139 | 304 |
| 23. | Kumar et al. | Qatar | 619 | NR | NR | 1414 | NR | NR |
| 24. | Lataifeh et al.$ | Jordan | 233 | 96 | 137 | 364 | 135 | 229 |
| 25. | Luma et al. | Iraq | 1229 | NR | NR | 1704 | 978 | 726 |
| 26. | Maqsood et al. | SA | 996 | NR | NR | 1031 | 281 | 750 |
| 27. | Maraqa et al. | Palestine | 438 | 188 | 250 | 1159 | 430 | 729 |
| 28. | Nasr et al. | Lebanon | 455 | NR | NR | 529 | 292 | 237 |
| 29. | Noushad et al. | SA | 433 | 238 | 195 | 674 | 350 | 324 |
| 30. | Qattan et al. | SA | 340 | 228 | 112 | 673 | 405 | 268 |
| 31. | Qunaibi et al. | multinational | 1522 | 1049 | 473 | 5708 | 3171 | 2537 |
| 32. | Rabi et al. | Palestine | 517 | NR | NR | 638 | 115 | 523 |
| 33. | Saddik et al. | UAE | 312 | NR | NR | 517 | 187 | 330 |
| 34. | Sharaf et al. | Egypt | 78 | 19 | 59 | 171 | 26 | 145 |
| 35. | Shehata | Egypt | 495 | 223 | 272 | 1268 | 515 | 753 |
| 36. | Temsah et al. | SA | 352 | NR | NR | 1058 | 354 | 704 |
| 37. | Yassin et al. | Sudan | 254 | 102 | 152 | 400 | 156 | 244 |
| 38. | Youssef et al. | Lebanon | 1044 | NR | NR | 1800 | 593 | 1209 |
| 39. | Zammit et al. | Tunisia | 237 | 72 | 155 | 493 | 131 | 346 |
NR = Not reported and was excluded from the quantitative analysis; SA, Saudi Arabia; UAE, United Arab Emirates; $ not statistically significant.
Fig 4. COVID-19 vaccine acceptance stratified by sex.
(A) males (B) females.
Vaccine acceptance by country
Table 3 summarizes the factors associated with vaccine acceptance. Only factors that showed a significant association with acceptance (P < 0.05) among HCWs were listed. A total of 33 studies identified various predictors for COVID-19 vaccine acceptance. The most commonly reported predictor was sex (n = 24), where in 91.6% of the studies, male healthcare workers were more likely to accept the vaccine than female. Other commonly reported predictors were a high perception of getting COVID-19 (n = 14), belief in the COVID-19 vaccine’s benefit (n = 11), positive attitude towards influenza vaccine (n = 11), high level of knowledge regarding COVID-19 disease/vaccine (n = 9), use of a reliable source of information (n = 5), the belief that the vaccine should be mandatory (n = 4), and work in frontline position (n = 4).
Table 3. Significant predictors of COVID-19 vaccine acceptance among HCWs reported in each study.
| Predictors of Vaccine Acceptance | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Author/year, country | Reference No. | Variables (Statistically Significant) | ||||||||
| Age group | Sex | Marital Status | Education level | Presence of comorbidities | Flu vaccine | COVID risk/ susceptibility perception | Vaccine perceived benefit | Others | |||
| 1. | Alobaidi/2022, SA* | Male | Widow/divorced/separated | Higher (MS, PhD) | ✔ | • Nationality: Non-Saudi • Monthly income: higher (>15K SR) |
|||||
| 2. | Arif/2021, SA | Female | Married | Bachelor | • Monthly income: moderate (5K-10K SR) • Vaccine convenience (vaccination method, frequency, distance to vaccination site. etc) • Higher number of vaccinated friends/family members • Belief that vaccine should be mandated by the government |
||||||
| 3. | Baghdadi/2021, SA | Middle (30–49 yr) | Female | ✔ | ✔ | • Perceived severity of COVID-19 • Belief that all HCWs should be vaccinated against COVID-19 • Work experience: low (<5 yr) • Non-smokers • Having no fear of injections • Perceived lack of barriers to receive the vaccine |
|||||
| 4. | Barry/2021, SA | Male | Married | ✔ | ✔ | ✔ | • Working in adult ICU and isolated floors • Source of information: CDC |
||||
| 5. | Elharake/2021, SA | Younger (25–34 yr) | Male | • Nationalities: Non-Saudi | |||||||
| 6. | Maqsood/2022, SA | Male | ✔ | • Nationalities: Non-Saudi | |||||||
| 7. | Qattan/2021, SA | Male | ✔ | ✔ | • Being a frontline healthcare worker • Believe that COVID19 vaccine should be compulsory |
||||||
| 8. | Al Awaidy/2020, Oman | Male | ✔ | • Recommend COVID-19 to family members • Higher level of knowledge about COVID-19 vaccine • Trust in government • Positive attitude towards COVID-19 vaccine |
|||||||
| 9. | Khamis/2022, Oman | Male | ✔ | Belief that vaccine should be mandated | |||||||
| 10. | Maraqa/2021, Palestine | Younger | Male | ✔ | ✔ | • Physicians • Working in a non-governmental setting • Higher knowledge about COVID-19 • - High income |
|||||
| 11. | Rabi/2021, Palestine | Younger | • Higher level of knowledge about COVID-19 vaccine • Perception of the vaccine as safe • Preference of vaccination over natural immunity • No fear of injections • Not influenced by media misrepresentation • COVID-19 might cause or potentiate existing chronic diseases |
||||||||
| 12. | Kumar/2021, Qatar | 26–35 yr | Male | Married | ✔ | ✔ | ✔ | • Higher level of knowledge about COVID-19 and the vaccine • Recommending the vaccine to oneself children |
|||
| 13. | Zammit/2022, Tunisia | ≥ 40 yr | Male | • Works in North of Tunisia • Previously infected with COVID-19 • The national and official health websites as the primary source for COVID-19-related information |
|||||||
| 14. | Albahri/2021, UAE | • Nationality: non-Emirati • Profession: Nurses |
|||||||||
| 15. | AlKetbi/2021, UAE | Older | Male | • Physicians/surgeons • Working in private sector • Nationality: South Asian • Religion |
|||||||
| 16. | Saddik/2022, UAE | Male | ✔ | ✔ | • Positive attitude towardCOVID-19 vaccine • Belief that there are sufficient data about the vaccine • No concern about vaccine side effects |
||||||
| 17. | Aloweidi /2021, Jordan | Unmarried | ✔ | ✔ | • Medical personnel advice • Social media awareness campaigns • Reading a scientific article about the available vaccines • Trust in vaccine efficacy and safety • National medical studies to prove the efficacy of the vaccines |
||||||
| 18. | Lataifeh/2022, Jordan | ✔ | • Being a physician (vs. nurses) • Registering on COVID-19 vaccine special platform |
||||||||
| 19. | Qunaibi/2021, multinational | Older | Male | ✔ | |||||||
| 20. | Al-Sanafi/2021, Kuwait | Male | Postgraduate degree | • Being a physician or dentist • Nationality: Kuwaiti • Working in public sector |
|||||||
| 21. | Nasr/2021, Lebanon | ✔ | ✔ | • Moderate or high knowledge level regarding COVID-19 vaccine • fear of COVID-19 disease |
|||||||
| 22. | Youssef/2022, Lebanon | Male | ✔ | ✔ | • Frontline health workers • Concerns about limited accessibility to the vaccine • Concerns about availability of the vaccine. • Receiving reliable and adequate information about vaccine • Recommendation from health authorities and health facilities |
||||||
| 23. | Khalis/2021, Morocco | • Being a physician, nurse, or technician • high score of confidence in the information circulating about COVID-19 • high score of perceived severity of COVID-19 |
|||||||||
| 24. | Ahmed/2021, Saudi Arabia | • 36 > years | Female | ✔ | |||||||
| 25. | Aldosary/2021, Saudi Arabia | • Higher knowledge score about COVID-19 disease • Higher practice score toward COVID-19 measures |
|||||||||
| 26. | Alhasan/2021, Saudi Arabia* | • Saudi National • Receiving both vaccination doses (1st and 2nd shots) • High knowledge score about delta variant. • High perception score regarding COVID-19 measures (mask, lockdown..) • Believing that the Pfizer-BioNTech BNT162b2 vaccine is effective against Delta variant. • Agreement that mixing/matching vaccines is effective against Delta variant. |
|||||||||
| 27. | Fares/2021, Egypt | Male | ✔ | Those who took non-compulsory vaccines Those who recommended COVID-19 vaccination to others Those who received advice from their hospitals to get the vaccine Those who showed trust in vaccine producers Those who received sufficient information and trusting the information on COVID-19 vaccine Considering taking vaccine as a community responsibility |
|||||||
| 28. | Elkhayat/2021, Egypt | Younger people (18–<30) | Male | Single | Higher | ✔ | ✔ | ✔ | Using reliable source of information Urban residence Job category- Doctors Attending awareness sections |
||
| 29. | El-Sokkary/2021, Egypt | 42.5 ± 12.2 | Male | Higher | ✔ | ✔ | • Monthly income: > 5000 LE • > 10 years of working experience • Using reliable sources of information for vaccines and attending vaccine meetings. |
||||
| 30. | Shehata/2022, Egypt | Youngest group (18–30) | Male | Married | Lower (bachelor’s grade) | ✔ | ✔ | • Urban area • Physicians who worked in frontline positions • primary surgical and surgical subspecialty • physicians who had someone they knew diagnosed with COVID-19 and had direct contact with COVID-19 patients • Absence of comorbidities • Obesity • COPD • Non-smoking |
|||
| 31. | Sharaf/2022, Egypt | Male | ✔ | ✔ | • Not anxious about Covid-19 at all • never postponed other recommended vaccines • has intentions to travel internationally • responsibility and fear of transmitting the disease to relatives or friends • not concerned about the safety and efficacy of vaccines |
||||||
| 32. | Noushad/2021, SA | Oldest group (50 and above) | Male | ✔ | • updating self on the development of COVID-19 vaccines • opinion about the severity of COVID-19 (increased severity perception) • Greater compliance with COVID-19 preventive guidelines • higher level of anxiety about contracting COVID-19 • Saudi nationals |
||||||
| 33. | Hamdan- Mansour /2022, Jordan | Male | • History of COVID-19 infection • Higher level of knowledge and perception about COVID-19 vaccines. |
||||||||
*Evaluated the acceptance of the COVDI-19 vaccine booster dose.
Saudi Arabia
Vaccine acceptance among HCWs in Saudi Arabia was assessed in 15 national [19–21, 23–34], and two multinational [61, 62] studies. All the studies were conducted during the period between July 2020 and November 2021, and seven studies were conducted before the introduction of COVID-19 vaccines in Saudi Arabia (i.e., before December 2020) [21, 25–28, 30, 33].
Certain sociodemographic factors were linked to vaccine acceptance, including being male (n = 7) [26, 27, 29, 30, 32, 34, 62], being older (n = 2) [30, 62], and being married (n = 2) [24, 26]. Other predictors of vaccine acceptance included a high-risk perception of getting COVID-19 (n = 4) [25, 26, 30, 34], belief in the COVID-19 vaccine’s benefit (n = 3) [25, 26, 29], positive attitudes towards influenza vaccine (n = 3) [26, 30, 62], belief that the vaccine should be mandatory (n = 3) [24, 25, 30], vaccine convenience/lack of barriers towards receiving the vaccines, (n = 2) [24, 25], working directly in high-risk settings (n = 2) [26, 30], and history of chronic illness (n = 1) [32].
Two studies evaluated the prevalence and predictors of booster dose acceptance among HCWs in Saudi Arabia and reported vaccine acceptance rates between 55–71% [19, 20]. Alhasan et al. identified certain factors associated with higher acceptance for booster doses, including complete primary COVID-19 vaccination (1st and 2nd doses), knowledge about the delta variant, and belief in vaccines’ effectiveness against the delta variant [20].
Egypt
Six national studies [35–40] and one multinational study [61] evaluated COVID-19 vaccine acceptance among HCWs in Egypt. The studies took place between December 2020 and October 2021. This period covers the phase before and after the availability of vaccines in the country [35–40]. All the studies surveyed several HCWs of different professions; however, only a few included specific professions, such as dental faculty members [39] and rheumatologists [35].
Several sociodemographic factors were associated with vaccine acceptance. The most reported were male sex (n = 5) [36–40], younger age groups of 18–30 years (n = 2) [37, 40], and higher educational level (n = 2) [37, 38]. In addition, other factors were correlated with vaccine acceptance, including COVID-19 risk susceptibility perception (n = 5) [36–40], previous receipt of flu vaccine (n = 2) [37, 40], and perceived vaccine benefit (n = 2) [37, 38].
Among physicians, Shehata et. al. described more factors that were significantly associated with their vaccine acceptance, particularly physicians working in frontline positions, physicians with surgical specialty, personally knowing someone diagnosed with COVID-19, and absence of medical comorbidity [40].
Jordan
In addition to the multinational study by El Kibbi, et al [61], a total of three studies were conducted in Jordan. Of these, two were conducted between January 2021 to March 2021 [41, 42] while one did not specify the study period [22]. Aloweidi et al. compared between HCWs (defined as medical personnel working in direct contact with patients) vs non-medical personnel in terms of the factors that could predict vaccine acceptance. The factors that significantly influenced HCWs to receive the vaccines included awareness campaigns on social media, advice from other HCWs, availability of national studies proving the efficacy of the vaccine, and trust in vaccine efficacy and safety. Moreover, HCWs who read scientific articles reported higher vaccine acceptance rate [41].
Palestine
Three studies assessed vaccine hesitancy among HCWs in Palestine [43–45]. Surveys were distributed between December 2020 and January 2021. Two studies were conducted exclusively among nurses [44, 45]. The most frequently reported factors associated with vaccine acceptance were being younger (n = 2) [43, 45] and having higher knowledge about COVID-19 disease/vaccines (n = 2) [43, 45].
United Arab Emirates (UAE)
Three studies surveyed HCWs’ COVID-19 acceptance in the UAE from July 2020 to January 2021 [46–48]. In two studies, the male sex was reported as a predictor for vaccine acceptance [47, 48] Furthermore, Saddik et al. reported several other factors including, previously receiving the flu vaccine, COVID-19 risk susceptibility perception, positive attitude toward the vaccine, availability of sufficient data, and having no concerns regarding the side effects of the vaccine [48]. Interestingly, Albahri et al. reported that non-Emirati residents were more willing to receive the vaccine [46], particularly South Asian residents [47].
Iraq
Two studies were published in Iraq concerning HCWs’ acceptance of COVID-19 vaccines [49, 50]. However, the latter was excluded from the meta-analysis because they also included the general population in their analysis [50]. On the other hand, Luma et al. identified various factors associated with vaccine hesitancy including female sex, lower level of education, poor health, and pre-existing chronic diseases [49].
Lebanon
Two studies were published from Lebanon assessing HCWs’ acceptance of COVID-19 vaccines [51, 52]. The first by Nasr et al. included dentists only. The factors that were associated with vaccine acceptance were previously receiving the flu vaccine, COVID-19 risk susceptibility perception, and moderate to high knowledge level regarding the COVID-19 vaccine [51]. The second study by Youssef et al. surveyed HCWs of different professions and reported that male sex, previous receipt of the flu vaccine, vaccine perceived benefit, frontline health workers’ concerns about limited access and availability to the vaccine, receiving reliable information regarding the vaccine, and recommendations done by health authorities were all positively associated with COVID-19 vaccine acceptance [52].
Oman
Vaccine hesitancy among HCWs was assessed in two studies in Oman [53, 54]. One study was conducted in December 2020, before the vaccine rollout in the country [53]. In both studies, males were more likely to accept vaccines than females [53, 54]. Other factors associated with vaccine acceptance included a higher level of knowledge, a positive attitude toward the vaccine, and trusting the government.
Kuwait
Only one national study was reported from Kuwait that assessed COVID-19 vaccine acceptance, which was conducted in March 2021 and included HCWs of different professions. The reported predictors for vaccine acceptance were male sex, higher level of education (i.e., post-graduate degree), Kuwaiti citizens, being a physician or dentist, and working in the public sector [55].
Libya
Only one national study conducted in December 2020 by Elhadi et al. evaluated the acceptance of the COVID-19 vaccine in both HCWs and the general population in Libya. The authors reported that the odds of accepting the vaccine among HCWs were associated with the age group 31–50 years old and having a friend or relative infected with COVID-19 [56].
Morocco
Khalis et al. estimated the vaccine acceptance in Morocco in January 2021. They found that vaccine acceptance was more likely among certain professions, including physicians, nurses, and technicians. Moreover, higher confidence in information regarding the COVID-19 vaccine or high perceived severity of the disease were associated with accepting the vaccine [57].
Qatar
Only one study from Qatar evaluated the hesitancy toward COVID-19 vaccines among HCWs [58]. The data were collected between October and November 2020, before the vaccine became available in Qatar. Factors associated with vaccine acceptance were being younger (26–35 years), being male, having positive attitudes towards the influenza vaccine, and having higher knowledge about COVID-19 disease. Concerns about vaccine safety and effectiveness were the most common reasons for vaccine hesitancy [58].
Sudan
A multicenter hospital-based cross-sectional study was conducted by Yassin et al in April 2021 to evaluate the knowledge, perception, and acceptability of COVID-19 vaccination among HCWs in Sudan [59]. The study reported a statistically significant association between knowledge about vaccination and professions. Among the participants who were aware of COVID-19 vaccinations, 47.7% were nurses and technicians, 35.7% were physicians, and 16.5% were pharmacists. Most participants referred to social media (47.5%) and hospital announcements (45.3%) for vaccine-related information.
Tunisia
Zammit et al. reported vaccine acceptance among HCWs in Tunisia. Notably, the study surveyed different hospital staff, which also included administrators and janitors. The study reported several predictors that were positively associated with vaccine acceptance, including. male sex, age ≥ 40 years, positive history of COVID-19 infection, working in north Tunisia, and utilizing official health websites as a primary source of information related to COVID-19 [60].
Arab world
The COVID-19 vaccine acceptance was assessed in a multinational study by El Kibbi et al., which included 19 Arab countries. The study reported that the male sex, older age, higher level of education, previously receiving the flu vaccine, and COVID-19 risk susceptibility perception were all significantly associated with vaccine acceptance [61].
Discussion
Achieving herd immunity using vaccines is an essential strategy to prevent and control the COVID-19 pandemic, where the populations’ acceptance of them is key. The attitude of HCWs toward COVID-19 vaccines represents a triggering factor to the general population’s acceptance of them [16, 63]. In our analysis, we found that the average acceptance rate of COVID-19 vaccine among HCWs in Arab countries was 60.4%. We also noticed various predictors to be associated with vaccine acceptance, namely male sex, higher educational degree, vaccination against flu, COVID-19 risk susceptibility perception, and vaccine perceived benefit.
The rate of COVID-19 vaccine acceptance among HCWs has been found to be variable from region to region. For instance, Ackah et al., who conducted a systematic review and meta-analysis in Africa, reported a lower rate of COVID-19 vaccine acceptance (46%; 95% CI, 37% to 54%) [12]. This could be potentially attributed to the lower availability of and limited accessibility to COVID-19 vaccines in Africa compared to the Arab region [64]. On the other hand, Bianchi and colleagues, who included 14 studies from Italy, reported a COVID-19 vaccine acceptance rate of 87% [65]. This could be explained by Italy’s higher COVID-19-related morbidity and mortality [64]. Similarly, higher rates of COVID-19 vaccine acceptance were reported from meta-analyses that included studies from different parts of the world [66, 67].
More than half of the studies included in our quantitative analysis surveyed participants from the Gulf Cooperation Council (GCC) countries. A review that included 49 studies from the GCC countries that surveyed the general public reported a vaccine acceptance rate similar to the one reported in our study on HCWs (57%) [68]. Most of the GCC countries’ governments have put in notable efforts and taken effective precautionary measures to combat the pandemic, including distributing clear and continually updated COVID-19 vaccine-related resources [69, 70]. The source of COVID-19 vaccine-related information has been reported to influence the attitude toward the COVID-19 vaccine directly [71]. The similar rate of COVID-19 vaccine acceptance between the general public and HCWs, therefore, is possibly attributed to the official governments’ channels being their primary source of COVID-19-related information.
The most frequently reported factors associated with COVID-19 vaccine acceptance in the included studies were being male (n = 21), higher risk perception of contracting COVID-19 (n = 12), positive attitude toward the influenza vaccine (n = 10), and higher educational level or higher knowledge about COVID-19 vaccine (n = 9). Our results are consistent with previous meta-analyses of global studies [66, 67]. Additionally, Fisher and colleagues, who surveyed adults in the U.S., noted that a higher educational level was associated with COVID-19 vaccine acceptance [72]. Individuals with higher educational levels tend to be lifelong learners. Such correlation with vaccine acceptance might be due to their continuous reading of scientific information from reliable sources to keep themselves updated and well-informed. A potential additional explanation behind the higher rate of acceptance among males is that the majority of HCWs in GCC countries are foreigners who may also have dependents. Hence, since practice licensure maintenance and/or residence status renewal in most GCC countries was linked to the receipt of COVID-19 vaccine, these male HCWs had to accept it. This was evident in a cross-sectional study of 870 participants in the Arab world by Kaadan, et al who noticed that a significantly higher proportion of vaccine acceptors were males and those living outside their home countries (i.e., considered foreigners) [73]. Moreover, different Arab countries had different COVID-19 vaccine products (Russian, Chinese, American, or European) based on governmental agreements. As such, the type of the vaccine offered free of charge to the public and the available circulating information about them in the media and those offered by health authorities may have also influenced the decision to receive the vaccine. For example, in a study by Abu-Farha, et al on 2,925 participants from various Arab countries, participants had a higher preference to receive an American vaccine (i.e., Pfizer/BioNTech and Moderna) vs. other kinds of vaccines [74].
Interestingly, the pooled vaccine acceptance rate was lower among female HCWs in comparison to males (48.2% vs 65.4%, respectively). Such observation could be attributed to the females’ negative perception of vaccines’ side effects on fertility and teratogenicity that could carry serious harm [37, 60]. For instance, a cross-sectional study conducted in Saudi Arabia reported a higher hesitancy rate regarding COVID-19 vaccines among pregnant females and females who were planning for pregnancy [75]. In addition, the same results were supported in several studies among pregnant females [76–78]. Nonetheless, such claims lack generalizability since the reasons behind Arab female HCWs’ vaccine refusal were not studied enough, and the pregnancy status was not mentioned in the included studies. Lastly, some studies included more female participants than males [36, 38–40].
Concerns about COVID-19 vaccine safety were among the most commonly reported predictors of vaccine hesitancy [36, 38, 39, 42, 61]. The same concern was also reported globally among the general population and HCWs [64]. The spread of false information through social media is significantly associated with vaccine hesitancy, where some HCWs rely on social media as a major source of information, followed by scientific journals and television [60]. Furthermore, the issue of vaccine safety arises from the lack of long-term safety trials, the expedited approval of several vaccines, and the lack of trust in pharmaceutical companies [39, 61]. Although those factors were valid during the initial rollout of COVID-19 vaccines, trust in safety and effectiveness were built after the vaccines were administered to the masses. For instance, in the studies that evaluated booster doses vaccine acceptance in Saudi Arabia noted that higher knowledge level about COVID-19 variants and receiving the initial doses were positively associated with higher vaccine acceptance rates [19, 20]. Lastly, the geographic distribution of HCWs was also associated with vaccine hesitancy. For instance, HCWs living in rural areas were more likely to refuse the vaccine compared to those living in urban areas [52]. Moreover, HCWs with low monthly income and fewer years of experience were more likely to reject COVID-19 vaccines [38]. Those results are important for health authorities and vaccine campaigns that should tailor their vaccine promotion messages to suit all categories of HCWs.
Implications and recommendations
Ministries of health and healthcare institutions should conduct regular continuing medical education sessions concerning the development processes of vaccines as well as their safety and effectiveness throughout history. Such sessions should be centered to address the concerns and queries that HCWs might have, including the rationale behind the expedited process of COVID-19 vaccine approval as well as illustrating the precautionary measures taken by the legislative agencies to ensure meeting the standards for safety and efficacy. Regulatory bodies could tailor their efforts to target HCWs who have a negative attitude toward the influenza vaccine or vaccines in general, particularly those with a lower level of postgraduate training or education, given their higher tendency to be vaccine-hesitant. Additionally, HCWs should be encouraged to keep up with scientific publications as this has been found to be associated with higher rates of vaccine acceptance [41].
Strengths and limitations
This systematic review and meta-analysis is the first that reported the acceptance rate of COVID-19 vaccines by HCWs in the Arab World and examined the potential predictors of such outcome. We critically evaluated the evidence using a valid assessment tool to avoid biased estimates. We also limited the meta-analysis to studies that included only the targeted population. Nonetheless, our study has some limitations. First, all the included studies were self-administered, cross-sectional, survey-based studies, which implies that our findings could have been impacted by a social desirability bias (i.e., the tendency of participants to answer socially acceptable answers rather than those that reflect their true feelings and practices); hence, limits their generalizability. Second, about 35% of the included studies in the meta-analysis surveyed participants from Saudi Arabia, and no studies were reported from eight Arab countries, besides the different population sizes between Arab countries, which indicates that our findings might be a little skewed. Third, the wide variation of healthcare systems among Arab countries in terms of unequal resource allocation, the diversity of access to healthcare services, and the differences in healthcare management strategies [79] could impact the predictors of vaccine acceptance and COVID-19 vaccine acceptance rate. In addition, each country had its own policies and protocols in obligating COVID-19 vaccine administration that we could not assess and may have influenced the opinions of the HCWs. Fourth, the included studies were conducted at different periods of time with significant variations in the availability of COVID-19 vaccines as well as in the governmental and employers’ encouragement to receive the vaccine. Lastly, the definition of vaccine acceptance varied across the included studies, where some of them used a binary approach of yes/no for participants to express their willingness to receive the vaccine, whereas others used the 5-point Likert scale. Such heterogeneity could have an impact on the reliability of our findings.
Conclusion
A moderate acceptance rate of COVID-19 vaccines was reported among HCWs in the Arab World. Several predictors were associated with COVID-19 vaccine acceptance, such as being male, higher risk perception, positive attitude toward the influenza vaccine, and higher knowledge about COVID-19 vaccines. Considering the potential need for future booster doses of the COVID-19 vaccine or future pandemics, regulatory bodies should raise awareness regarding vaccine safety and efficacy as well as tailor their efforts to target HCWs who would consequently influence the general public with their attitude and perceptions of the vaccines. Future research could focus on exploring the reasons behind the low COVID-19 vaccine acceptance rate among the up-mentioned factors including female HCWs and addressing effective solutions and interventions to upcoming the barriers.
Supporting information
(DOCX)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work
References
- 1.Pogue K, Jensen JL, Stancil CK, Ferguson DG, Hughes SJ, Mello EJ, et al. Influences on attitudes regarding potential covid‐19 vaccination in the united states. Vaccines. 2020;8: 1–14. doi: 10.3390/vaccines8040582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lynch HJ, Marcuse EK. Vaccines and immunization. In: The Social Ecology of Infectious Diseases. 2007. pp. 275–299. doi: 10.1016/B978-012370466-5.50015-7 [DOI] [Google Scholar]
- 3.Friedrich MJ. WHO’s Top Health Threats for 2019. Jama. 2019;321: 1041. doi: 10.1001/jama.2019.1934 [DOI] [PubMed] [Google Scholar]
- 4.MacDonald NE, Eskola J, Liang X, Chaudhuri M, Dube E, Gellin B, et al. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33: 4161–4164. doi: 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- 5.Palache A, Oriol-Mathieu V, Abelin A, Music T. Seasonal influenza vaccine dose distribution in 157 countries (2004–2011). Vaccine. 2014;32: 6369–6376. doi: 10.1016/j.vaccine.2014.07.012 [DOI] [PubMed] [Google Scholar]
- 6.Andre FE, Booy R, Bock HL, Clemens J, Datta SK, John TJ, et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. 2008;86: 140–146. doi: 10.2471/blt.07.040089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lane S, MacDonald NE, Marti M, Dumolard L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine. 2018;36: 3861–3867. doi: 10.1016/j.vaccine.2018.03.063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wagner AL, Masters NB, Domek GJ, Mathew JL, Sun X, Asturias EJ, et al. Comparisons of vaccine hesitancy across five low- and middle-income countries. Vaccines. 2019;7. doi: 10.3390/vaccines7040155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Lancet Child & Adolescent Health. Vaccine hesitancy: a generation at risk. Lancet Child Adolesc Heal. 2019;3: 281. doi: 10.1016/S2352-4642(19)30092-6 [DOI] [PubMed] [Google Scholar]
- 10.The Washington Post. Washington Post-ABC News poll. [cited 26 Nov 2022]. Available: https://www.washingtonpost.com/context/may-25-28-2020-washington-post-abc-news-poll/bb30c35e-797e-4b5c-91fc-1a1cdfbe85cc/?itid=lk_inline_manual_2&itid=lk_inline_manual_2&itid=lk_inline_manual_2
- 11.Verger P, Scronias D, Dauby N, Adedzi KA, Gobert C, Bergeat M, et al. Attitudes of healthcare workers towards COVID-19 vaccination: A survey in France and French-speaking parts of Belgium and Canada, 2020. Eurosurveillance. 2021;26. doi: 10.2807/1560-7917.ES.2021.26.3.2002047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ackah M, Ameyaw L, Salifu MG, Asubonteng DPA, Yeboah CO, Annor EN, et al. COVID-19 vaccine acceptance among health care workers in Africa: A systematic review and meta-analysis. PLoS One. 2022;17: e0268711. doi: 10.1371/journal.pone.0268711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harrison EA, Wu JW. Vaccine confidence in the time of COVID-19. Eur J Epidemiol. 2020;35: 325–330. doi: 10.1007/s10654-020-00634-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alalawi M, Makhlouf M, Hassanain O, Abdelgawad AA, Nagy M. Healthcare workers’ mental health and perception towards vaccination during COVID-19 pandemic in a Pediatric Cancer Hospital. Sci Rep. 2023;13. doi: 10.1038/s41598-022-24454-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chou R, Dana T, Buckley DI, Selph S, Fu R, Totten AM. Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers; A Living Rapid Review. Ann Intern Med. 2020;173: 120–136. doi: 10.7326/M20-1632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deem MJ. Nurses’ voices matter in decisions about dismissing vaccine-refusing families. Am J Nurs. 2018;118: 11. doi: 10.1097/01.NAJ.0000544142.09253.e0 [DOI] [PubMed] [Google Scholar]
- 17.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.JBI. Critical Appraisal Tools. In: Joanna Briggs Institute [Internet]. 2020 [cited 8 Mar 2023]. Available: https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Fjbi.global%2Fsites%2Fdefault%2Ffiles%2F2021-10%2FChecklist_for_Analytical_Cross_Sectional_Studies.docx&wdOrigin=BROWSELINK
- 19.Alobaidi S, Hashim A. Predictors of the Third (Booster) Dose of COVID-19 Vaccine Intention among the Healthcare Workers in Saudi Arabia: An Online Cross-Sectional Survey. Vaccines. 2022;10: 1–15. doi: 10.3390/vaccines10070987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alhasan K, Aljamaan F, Temsah MH, Alshahrani F, Bassrawi R, Alhaboob A, et al. Covid-19 delta variant: Perceptions, worries, and vaccine-booster acceptability among healthcare workers. Healthc. 2021;9: 1–19. doi: 10.3390/healthcare9111566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Temsah MH, Barry M, Aljamaan F, Alhuzaimi A, Al-Eyadhy A, Saddik B, et al. Adenovirus and RNA-based COVID-19 vaccines’ perceptions and acceptance among healthcare workers in Saudi Arabia: A national survey. BMJ Open. 2021;11: 1–9. doi: 10.1136/bmjopen-2020-048586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hamdan-Mansour AM, Abdallah MH, Khalifeh AH, AlShibi AN, Shaher HH, Hamdan-Mansour LA. Determinants of Healthcare Workers’ Willingness to Receive COVID-19 Vaccination. Malaysian J Med Heal Sci. 2022;18: 5–13. [Google Scholar]
- 23.Alhofaian A, Tunsi A, Alaamri MM, Babkair LA, Almalki GA, Alsadi SM, et al. Perception of heath care providers about covid-19 and its vaccination in saudi arabia: Cross-sectional study. J Multidiscip Healthc. 2021;14: 2557–2563. doi: 10.2147/JMDH.S327376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arif SI, Aldukhail AM, Albaqami MD, Silvano RC, Titi MA, Arif BI, et al. Predictors of healthcare workers’ intention to vaccinate against COVID-19: A cross sectional study from Saudi Arabia. Saudi J Biol Sci. 2022;29: 2314–2322. doi: 10.1016/j.sjbs.2021.11.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baghdadi LR, Alghaihb SG, Abuhaimed AA, Alkelabi DM, Alqahtani RS. Healthcare workers’ perspectives on the upcoming covid-19 vaccine in terms of their exposure to the influenza vaccine in riyadh, saudi arabia: A cross-sectional study. Vaccines. 2021;9: 1–20. doi: 10.3390/vaccines9050465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barry M, Temsah MH, Alhuzaimi A, Alamro N, Al-Eyadhy A, Aljamaan F, et al. COVID-19 vaccine confidence and hesitancy among health care workers: A cross-sectional survey from a MERS-CoV experienced nation. PLoS One. 2021;16: 1–16. doi: 10.1371/journal.pone.0244415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elharake JA, Galal B, Alqahtani SA, Kattan RF, Barry MA, Temsah MH, et al. COVID-19 Vaccine Acceptance among Health Care Workers in the Kingdom of Saudi Arabia. Int J Infect Dis. 2021;109: 286–293. doi: 10.1016/j.ijid.2021.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hershan AA. Awareness of COVID-19, Protective Measures and Attitude towards Vaccination among University of Jeddah Health Field Community: A Questionnaire-Based Study. J Pure Appl Microbiol. 2021;15: 604–612. doi: 10.22207/JPAM.15.2.02 [DOI] [Google Scholar]
- 29.Maqsood MB, Islam MA, Al Qarni A, Nisa ZU, Ishaqui AA, Alharbi NK, et al. Assessment of COVID-19 Vaccine Acceptance and Reluctance Among Staff Working in Public Healthcare Settings of Saudi Arabia: A Multicenter Study. Front Public Heal. 2022;10: 1–8. doi: 10.3389/fpubh.2022.847282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qattan AMN, Alshareef N, Alsharqi O, Al Rahahleh N, Chirwa GC, Al-Hanawi MK. Acceptability of a COVID-19 Vaccine Among Healthcare Workers in the Kingdom of Saudi Arabia. Front Med. 2021;8: 1–12. doi: 10.3389/fmed.2021.644300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Temsah MH, Barry M, Aljamaan F, Alhuzaimi AN, Al-Eyadhy A, Saddik B, et al. SARS-CoV-2 B.1.1.7 UK Variant of Concern Lineage-Related Perceptions, COVID-19 Vaccine Acceptance and Travel Worry Among Healthcare Workers. Front Public Heal. 2021;9. doi: 10.3389/fpubh.2021.686958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahmed G, Almoosa Z, Mohamed D, Rapal J, Minguez O, Abu Khurma I, et al. Healthcare provider attitudes toward the newly developed covid-19 vaccine: Cross-sectional study. Nurs Reports. 2021;11: 187–194. doi: 10.3390/nursrep11010018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aldosary AH, Alayed GH. Willingness to vaccinate against Novel COVID-19 and contributing factors for the acceptance among nurses in Qassim, Saudi Arabia. Eur Rev Med Pharmacol Sci. 2021;25: 6386–6396. doi: 10.26355/eurrev_202110_27012 [DOI] [PubMed] [Google Scholar]
- 34.Noushad M, Nassani MZ, Alsalhani AB, Koppolu P, Niazi FH, Samran A, et al. COVID-19 vaccine intention among healthcare workers in Saudi Arabia: A cross-sectional survey. Vaccines. 2021;9: 1–12. doi: 10.3390/vaccines9080835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hammam N, Tharwat S, Shereef RRE, Elsaman AM, Khalil NM, Fathi HM, et al. Rheumatology university faculty opinion on coronavirus disease-19 (COVID-19) vaccines: the vaXurvey study from Egypt. Rheumatol Int. 2021;41: 1607–1616. doi: 10.1007/s00296-021-04941-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fares S, Elmnyer MM, Mohamed SS, Elsayed R. COVID-19 Vaccination Perception and Attitude among Healthcare Workers in Egypt. J Prim Care Community Heal. 2021;12. doi: 10.1177/21501327211013303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elkhayat MR, Hashem MK, Helal AT, Shaaban OM, Ibrahim AK, Meshref TS, et al. Determinants of Obtaining COVID-19 Vaccination among Health Care Workers with Access to Free COVID-19 Vaccination: A Cross-Sectional Study. Vaccines. 2022;10: 1–13. doi: 10.3390/vaccines10010039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.El-Sokkary RH, El Seifi OS, Hassan HM, Mortada EM, Hashem MK, Gadelrab MRMA, et al. Predictors of COVID-19 vaccine hesitancy among Egyptian healthcare workers: a cross-sectional study. BMC Infect Dis. 2021;21: 1–9. doi: 10.1186/s12879-021-06392-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sharaf M, Taqa O, Mousa H, Badran A. COVID-19 vaccine acceptance and perceptions among dental teaching staff of a governmental university in Egypt. J Egypt Public Health Assoc. 2022;97. doi: 10.1186/s42506-022-00104-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shehata WM, Elshora AA, Abu-Elenin MM. Physicians’ attitudes and acceptance regarding COVID-19 vaccines: a cross-sectional study in mid Delta region of Egypt. Environ Sci Pollut Res. 2022;29: 15838–15848. doi: 10.1007/s11356-021-16574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aloweidi A, Bsisu I, Suleiman A, Abu-Halaweh S, Almustafa M, Aqel M, et al. Hesitancy towards covid-19 vaccines: An analytical cross–sectional study. Int J Environ Res Public Health. 2021;18: 1–12. doi: 10.3390/ijerph18105111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lataifeh L, Al-Ani A, Lataifeh I, Ammar K, Alomary A, Al-Hammouri F, et al. Knowledge, Attitudes, and Practices of Healthcare Workers in Jordan towards the COVID-19 Vaccination. Vaccines. 2022;10: 1–12. doi: 10.3390/vaccines10020263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maraqa B, Nazzal Z, Rabi R, Sarhan N, Al-Shakhrah K, Al-Kaila M. COVID-19 vaccine hesitancy among health care workers in Palestine: A call for action. Prev Med (Baltim). 2021;149. doi: 10.1016/j.ypmed.2021.106618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Belkebir S, Maraqa B, Nazzal Z, Abdullah A, Yasin F, Al-Shakhrah K, et al. Exploring the Perceptions of Nurses on Receiving the SARS CoV-2 Vaccine in Palestine: A Qualitative Study. Can J Nurs Res. 2023;55: 34–41. doi: 10.1177/08445621211066721 [DOI] [PubMed] [Google Scholar]
- 45.Rabi R, Maraqa B, Nazzal Z, Zink T. Factors affecting nurses’ intention to accept the COVID-19 vaccine: A cross-sectional study. Public Health Nurs. 2021;38: 781–788. doi: 10.1111/phn.12907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Albahri AH, Alnaqbi SA, Alnaqbi SA, Alshaali AO, Shahdoor SM. Knowledge, Attitude, and Practice Regarding COVID-19 Among Healthcare Workers in Primary Healthcare Centers in Dubai: A Cross-Sectional Survey, 2020. Front Public Heal. 2021;9: 1–11. doi: 10.3389/fpubh.2021.617679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.AlKetbi LMB, Elharake JA, Memari S Al, Mazrouei S Al, Shehhi B Al, Malik AA, et al. COVID-19 vaccine acceptance among healthcare workers in the United Arab Emirates. IJID Reg. 2021;1: 20–26. doi: 10.1016/j.ijregi.2021.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Saddik B, Al-Bluwi N, Shukla A, Barqawi H, Alsayed HAH, Sharif-Askari NS, et al. Determinants of healthcare workers perceptions, acceptance and choice of COVID-19 vaccines: a cross-sectional study from the United Arab Emirates. Hum Vaccines Immunother. 2022;18: 1–9. doi: 10.1080/21645515.2021.1994300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Luma AH, Haveen AH, Faiq BB, Moramarco S, Leonardo EG. Hesitancy towards Covid-19 vaccination among the healthcare workers in Iraqi Kurdistan. Public Heal Pract. 2022;3. doi: 10.1016/j.puhip.2021.100222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Al-Metwali BZ, Al-Jumaili AA, Al-Alag ZA, Sorofman B. Exploring the acceptance of COVID-19 vaccine among healthcare workers and general population using health belief model. J Eval Clin Pract. 2021;27: 1112–1122. doi: 10.1111/jep.13581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nasr L, Saleh N, Hleyhel M, El-Outa A, Noujeim Z. Acceptance of COVID-19 vaccination and its determinants among Lebanese dentists: a cross-sectional study. BMC Oral Health. 2021;21: 1–10. doi: 10.1186/s12903-021-01831-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Youssef D, Abou-Abbas L, Berry A, Youssef J, Hassan H. Determinants of acceptance of Coronavirus disease-2019 (COVID-19) vaccine among Lebanese health care workers using health belief model. PLoS One. 2022;17: 1–17. doi: 10.1371/journal.pone.0264128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Awaidy STA, Al Siyabi H, Khatiwada M, Al Siyabi A, Al Mukhaini S, Dochez C, et al. Assessing COVID-19 Vaccine’s Acceptability Amongst Health Care Workers in Oman: A cross-sectional study. J Infect Public Health. 2022;15: 906–914. doi: 10.1016/j.jiph.2022.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khamis F, Badahdah A, Al Mahyijari N, Al Lawati F, Al Noamani J, Al Salmi I, et al. Attitudes Towards COVID-19 Vaccine: A Survey of Health Care Workers in Oman. J Epidemiol Glob Health. 2022;12: 1–6. doi: 10.1007/s44197-021-00018-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Al-Sanafi M, Sallam M. Psychological determinants of covid-19 vaccine acceptance among healthcare workers in kuwait: A cross-sectional study using the 5c and vaccine conspiracy beliefs scales. Vaccines. 2021;9. doi: 10.3390/vaccines9070701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Elhadi M, Alsoufi A, Alhadi A, Hmeida A, Alshareea E, Dokali M, et al. Knowledge, attitude, and acceptance of healthcare workers and the public regarding the COVID-19 vaccine: a cross-sectional study. BMC Public Health. 2021;21: 1–21. doi: 10.1186/s12889-021-10987-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Khalis M, Hatim A, Elmouden L, Diakite M, Marfak A, Ait El Haj S, et al. Acceptability of COVID-19 vaccination among health care workers: a cross-sectional survey in Morocco. Hum Vaccines Immunother. 2021;17: 5076–5081. doi: 10.1080/21645515.2021.1989921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kumar R, Alabdulla M, Elhassan NM, Reagu SM. Qatar Healthcare Workers’ COVID-19 Vaccine Hesitancy and Attitudes: A National Cross-Sectional Survey. Front Public Heal. 2021;9. doi: 10.3389/fpubh.2021.727748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yassin EOM, Faroug HAA, Ishaq ZBY, Mustafa MMA, Idris MMA, Widatallah SEK, et al. COVID-19 Vaccination Acceptance among Healthcare Staff in Sudan, 2021. J Immunol Res. 2022;2022. doi: 10.1155/2022/3392667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zammit N, Gueder A El, Brahem A, Ayouni I, Ghammam R, Fredj S Ben, et al. Studying SARS-CoV-2 vaccine hesitancy among health professionals in Tunisia. BMC Health Serv Res. 2022;22: 1–14. doi: 10.1186/s12913-022-07803-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.El Kibbi L, Metawee M, Hmamouchi I, Abdulateef N, Halabi H, Eissa M, et al. Acceptability of the COVID-19 vaccine among patients with chronic rheumatic diseases and health-care professionals: a cross-sectional study in 19 Arab countries. Lancet Rheumatol. 2022;4: e160–e163. doi: 10.1016/S2665-9913(21)00368-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Qunaibi E, Basheti I, Soudy M, Sultan I. Hesitancy of arab healthcare workers towards covid-19 vaccination: A large-scale multinational study. Vaccines. 2021;9: 1–13. doi: 10.3390/vaccines9050446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shakeel CS, Mujeeb AA, Mirza MS, Chaudhry B, Khan SJ. Global COVID-19 Vaccine Acceptance: A Systematic Review of Associated Social and Behavioral Factors. Vaccines. 2022;10: 110. doi: 10.3390/vaccines10010110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.World Health Organization. Coronavirus Disease Coronavirus World Health Organization. In: World Health Organization [Internet]. 2020 [cited 17 Feb 2023] pp. 1–20. Available: https://covid19.who.int/
- 65.Bianchi FP, Stefanizzi P, Brescia N, Lattanzio S, Martinelli A, Tafuri S. COVID-19 vaccination hesitancy in Italian healthcare workers: a systematic review and meta-analysis. Expert Rev Vaccines. 2022;21: 1289–1300. doi: 10.1080/14760584.2022.2093723 [DOI] [PubMed] [Google Scholar]
- 66.Galanis P, Vraka I, Katsiroumpa A, Siskou O, Konstantakopoulou O, Katsoulas T, et al. COVID-19 Vaccine Uptake among Healthcare Workers: A Systematic Review and Meta-Analysis. Vaccines. 2022;10. doi: 10.3390/vaccines10101637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang L, Wang Y, Cheng X, Li X, Yang Y, Li J. Acceptance of coronavirus disease 2019 (COVID-19) vaccines among healthcare workers: A meta-analysis. Front Public Heal. 2022;10. doi: 10.3389/fpubh.2022.881903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Alsalloum MA, Garwan YM, Jose J, Thabit AK, Baghdady N. COVID-19 vaccine hesitancy and acceptance among the public in the Gulf Cooperation Council countries: A review of the literature. Hum Vaccines Immunother. 2022;18. doi: 10.1080/21645515.2022.2091898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Alshammari TM, Alenzi KA, Alnofal FA, Fradees G, Altebainawi AF. Are countries’ precautionary actions against COVID-19 effective? An assessment study of 175 countries worldwide. Saudi Pharm J. 2021;29: 391–409. doi: 10.1016/j.jsps.2021.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Alshammari TM, Altebainawi AF, Alenzi KA. Importance of early precautionary actions in avoiding the spread of COVID-19: Saudi Arabia as an Example. Saudi Pharm J. 2020;28: 898–902. doi: 10.1016/j.jsps.2020.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gudi SK, George SM, Jose J. Influence of social media on the public perspectives of the safety of COVID-19 vaccines. Expert Rev Vaccines. 2022;21: 1697–1699. doi: 10.1080/14760584.2022.2061951 [DOI] [PubMed] [Google Scholar]
- 72.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: A survey of U.S. adults. Ann Intern Med. 2020;173: 964–973. doi: 10.7326/M20-3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kaadan MI, Abdulkarim J, Chaar M, Zayegh O, Keblawi MA. Determinants of COVID-19 vaccine acceptance in the Arab world: a cross-sectional study. Glob Heal Res Policy. 2021;6. doi: 10.1186/s41256-021-00202-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Abu-Farha R, Mukattash T, Itani R, Karout S, Khojah HMJ, Abed Al-Mahmood A, et al. Willingness of Middle Eastern public to receive COVID-19 vaccines. Saudi Pharm J. 2021;29: 734–739. doi: 10.1016/j.jsps.2021.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Samannodi M. COVID-19 vaccine acceptability among women who are pregnant or planning for pregnancy in Saudi Arabia: A cross-sectional study. Patient Prefer Adherence. 2021;15: 2609–2618. doi: 10.2147/PPA.S338932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Amiebenomo OM, Osuagwu UL, Envuladu EA, Miner CA, Mashige KP, Ovenseri-Ogbomo G, et al. Acceptance and Risk Perception of COVID-19 Vaccination among Pregnant and Non Pregnant Women in Sub-Saharan Africa: A Cross-Sectional Matched-Sample Study. Vaccines. 2023;11. doi: 10.3390/vaccines11020484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Azami M, Nasirkandy MP, Ghaleh HEG, Ranjbar R. COVID-19 vaccine acceptance among pregnant women worldwide: A systematic review and meta-analysis. PLoS One. 2022;17. doi: 10.1371/journal.pone.0272273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tao L, Wang R, Han N, Liu J, Yuan C, Deng L, et al. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: a multi-center cross-sectional study based on health belief model. Hum Vaccines Immunother. 2021;17: 2378–2388. doi: 10.1080/21645515.2021.1892432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Katoue MG, Cerda AA, García LY, Jakovljevic M. Healthcare system development in the Middle East and North Africa region: Challenges, endeavors and prospective opportunities. Front Public Heal. 2022;10. doi: 10.3389/fpubh.2022.1045739 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.