Abstract
Purpose
In the context of COVID-19, studies evaluating the adherence of dentists and dental students to infection control are relevant due to their high occupational exposure and risk, as well as their responsibility for disseminating information and good practices. This study evaluated the adherence of dentists and dental students to infection control in the oral radiology field in the setting of the COVID-19 pandemic on different continents.
Materials and Methods
This cross-sectional observational study involved individuals who performed intraoral radiographic examinations during the COVID-19 pandemic. The Questionnaire on Infection Control in Oral Radiology was administered virtually using a Google Form. Participants from different continents (the Americas, Africa, Europe, Asia, and Oceania) were recruited. Data were subjected to descriptive analysis and simple and multiple binary regression (5%).
Results
There were 582 valid answers, and 68.73% of the participants were from the Americas, 18.90% from Europe, and 12.37% from Asia. The median score for infection control protocols was 94 points for dental students and 104 points for dentists, and participants below the median were considered to have low adherence to infection control in oral radiology. Low access to infection control was found for 53.0% of dentists in the Americas, 34.0% from Europe, and 26.9% from Asia.
Conclusion
The adherence to infection control protocols in oral radiology was low even in the face of the COVID-19 pandemic. The results may help improve the awareness of students and professionals, since oral radiology routines have the potential for transmitting COVID-19.
Keywords: Radiography, Dental, Digital; Surveys and Questionnaires; Infection Control; COVID-19
Introduction
In December 2019, a notification was received regarding a group of individuals diagnosed with pneumonia without a defined etiology in the city of Wuhan, China, and later the condition was termed coronavirus disease 2019 (COVID-19) and its causative agent was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1,2,3 By late March 2020, reports indicated that COVID-19 had spread to over 200 countries and territories worldwide, leading the World Health Organization to declare it a global pandemic.1,4 This acute respiratory infection has had devastating effects across multiple dimensions, including the economy, social life, and health.1,5 The rapid spread of the virus and its evolving genome are of particular concern to society, especially healthcare professionals.6
Direct inhalation of aerosols or respiratory droplets, as well as indirect inhalation of virus-infected particles that have come into contact with contaminated surfaces, are among the primary reported modes of SARS-CoV-2 transmission.7,8 Consequently, dentists face a high risk of infection and can significantly contribute to the virus's spread.9,10,11,12 The virus's lengthy and unpredictable incubation period, coupled with a high rate of asymptomatic cases (80%), presents challenges that may undermine infection control practices in routine dental care.9
Considering the factors associated with virus transmission, dental procedures pose a significant risk for spreading COVID-19, particularly following the detection of the virus in the saliva of infected patients.10 Lung cells are the main target of the virus, but salivary gland ducts are also affected, resulting in the production of contaminated saliva.13,14,15 Nevertheless, despite the high exposure risk, dentists have continued to carry out essential clinical procedures throughout the COVID-19 outbreak.16
To minimize the risk of cross-infection within dental practices, health agencies have issued specific recommendations for infection control in dentistry. These include the use of barrier techniques, hand hygiene practices, sterilization and disinfection of equipment, as well as protection of radiography equipment and films.17,18 Thus, dentists should be attentive toward preventive management to protect staff and patients.11,19
The COVID-19 pandemic has posed significant challenges to the global health system, particularly in the field of oral radiology. Intraoral radiographic exams, which are crucial for diagnosing major maxillofacial pathological changes, have been especially affected. These routine procedures involve direct contact with body fluids such as saliva and blood, as well as exposure to aerosols produced by choking and coughing11,20 and contamination of work surfaces.21 According to a study that investigated the potential route of SARS-CoV-2 infection in the mucosa of the oral cavity, oral epithelial cells express high levels of angiotensin-converter enzyme 2 receptor (ACE2), contributing to SARS-CoV-2 infiltration into host cells.22 Therefore, it is essential to disinfect all surfaces thoroughly. SARS-CoV-2 can persist on inanimate surfaces for hours or even days, depending on factors such as temperature, humidity, and viral load.23,24
At the height of the pandemic, the Centers for Disease Control and Prevention (CDC) advocated for the use of extraoral imaging in place of intraoral imaging.25 However, panoramic radiography and cone-beam computed tomography could potentially expose the patient to elevated radiation levels, or may not serve as suitable alternatives to intraoral images.25 In this context, the CDC’s guidelines included specific considerations for infection control in oral radiology,26 since restricting access to care and implementing infection control protocols were the only mechanisms that could mitigate the spread of the disease.27
Although there are several recommendations for infection control in oral radiology, little is known about professional compliance in routine practice. Considering the recent emergence of COVID-19, studies evaluating the adherence of dentists and dental students to infection control have become increasingly relevant. Investigating the role of dentists and dental students in the prevention and monitoring of viral infections is essential, because this group not only faces a high risk of occupational exposure, but is also responsible for the dissemination of information and good practices.28
The present study aimed to evaluate the adherence of dentists and dental students to infection control in oral radiology in the setting of the COVID-19 outbreak in different continents.
Materials and Methods
This cross-sectional observational study was reviewed and approved by the Ethics Committee on Research with Human Beings, under protocol 4.267.744/2020. All participants were thoroughly informed about the study's nature and agreed to participate by completing a free and informed consent form. This form was virtually presented to them before they answered the questionnaire.
The sample included dentists, general practitioners, specialists in various fields of dentistry, and dental students from both public and private institutions. Individuals from all continents were invited to participate via email, WhatsApp, and Instagram, with no restrictions based on gender, age, race, social class, or religion. Eligibility for inclusion in the sample required participants to have performed intraoral radiographic examinations in their clinical practice during the COVID-19 pandemic, specifically from September 2020 to April 2021. Various information was collected from the participants, including gender, age, country and state of residence, marital status, household size, whether they cohabitate with elderly individuals and/or children, presence of comorbidities or systemic changes, professional performance, professional qualifications, primary area of activity in dentistry, length of time in the profession, and whether they were affiliated with a public or private network.
To increase engagement and aid in the recruitment of potential study participants, an Instagram profile was established. This profile featured information about the research and regular posts. In terms of gathering participants' emails, a search was conducted on the websites of universities (both public and private) across the globe. From platforms that share faculty data, an email was dispatched, requesting their participation and asking them to spread the word among their network of individuals involved in dental practice.
The Questionnaire on Infection Control in Oral Radiology (QICOR) was administered via Google Forms™ in both Portuguese and English. This questionnaire, specifically designed to evaluate infection control in oral radiology, was previously developed and validated in both languages by da Costa et al.29,30 The decision to use an online format was influenced by the need for social distancing due to the ongoing pandemic. The study was disseminated by ten researchers who managed to engage participants from various countries across five continents. However, due to the extremely low response rate from participants in Africa and Oceania, responses from these continents were excluded. Consequently, the recorded responses were only from the Americas, Europe, and Asia. This makes the study an international collaborative effort involving participants from three continents and 38 countries worldwide.
The questionnaire included nine domains: hand hygiene, glove use, clothing, accessories, radiographic receptors, equipment protection/disinfection, glove-related practices, digital radiographic systems, and cleaning and disinfection procedures. Each domain offered objective answer options, with some questions including an "other" option for respondents to describe alternative infection control methods used in their clinical practice. In response to the updated infection control protocols due to the pandemic, additional options were incorporated into the "clothing" domain, such as an N95/FFP2/FFP3 mask or equivalent, face shield, and foot protector. The highest possible score was 136 points, while the lowest was 25 points.
The data were analyzed using descriptive statistics, simple binary regression, and multiple binary regression to achieve the study's proposed objectives. The sample was divided based on the median into low scores (median ≤104 for the dentists' sample and median ≤94 for the students' sample) and high scores (median >104 for the dentists' sample and median >94 for the students' sample). This division was done to ensure balance and enhance the power of the test. Participants who scored below the median were deemed to have low infection control in oral radiology. The R software (R Foundation for Statistical Computing, Vienna, Austria) was utilized, with a P-value of less than 0.05 considered significant.
Results
A total of 582 valid responses were collected, comprising 391 females, 190 males, and 1 individual of another gender. The respondents included 193 dental students and 389 dentists (Table 1). The majority of participants (68.73%) were from the Americas, followed by 18.90% from Europe, and 12.37% from Asia. The median age of the dental students was 22 years, while for the dentists, it was 36 years (Table 1).
Table 1. Characteristics of dental students and dentists.
*: 5 missing dental student data, a: median for students equal to 94 and for dentists equal to 104, QICOR: questionnaire on infection control in oral radiology
Among the undergraduate students surveyed, 150 were from private schools, while 38 were from the public school system. A significant majority (93.78%) were from the Americas. Of the dentists, 130 were employed in the public system, 220 were in private practice, and 39 worked in both sectors. The geographical distribution of the dentists who responded to the survey was diverse, with 56.30% from the Americas, 26.48% from Europe, and 17.22% from Asia. When considering their dental specialties, 63.75% were engaged in fields other than oral radiology, while 36.25% practiced within the realm of oral radiology. As for their professional experience, 47.30% of the dentists had less than 10 years in the field, while 52.70% had more than a decade of experience (Table 1).
The median score for adherence to infection control protocols was 94 points among dental students and 104 points among dentists. Those who scored below the median were categorized as having low adherence to these protocols in the field of oral radiology. In the Americas, 53.0% of dentists scored below the median, in contrast to 26.9% in Asia and 34.0% in Europe (Table 1).
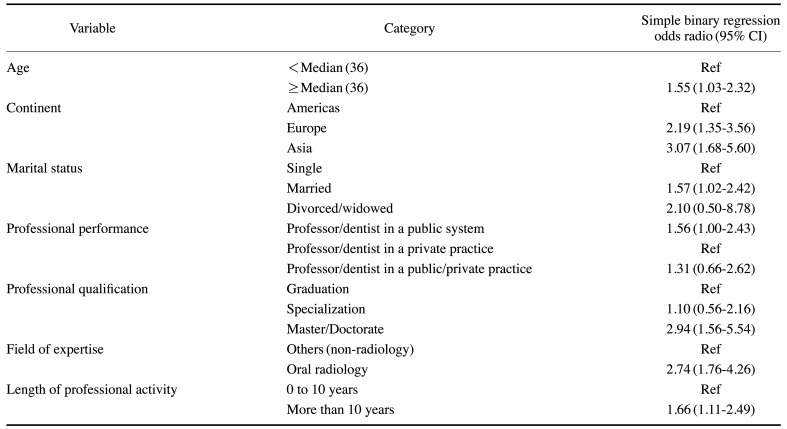
The simple binary regression analysis results for QICOR scores among dentists (n=389) revealed several significant associations. First, individuals aged 36 years or older were 1.55 times more likely (95% CI, 1.03-2.32) to adhere to infection control protocols in oral radiology than those below the median age. Additionally, participants from Europe were 2.19 times more likely (95% CI, 1.35-3.56) to adhere to infection control compared to those from the Americas. Similarly, individuals from Asian countries were 3.07 times more likely (95% CI, 1.68-5.60) to adhere to infection control practices than their American counterparts (Table 2).
Table 2. Simple binary logistic regression for questionnaire on infection control in oral radiology (QICOR) scores in dentists (n=389).
CI: confidence interval, Ref: reference variable
It was observed that married individuals were 1.57 times (95% CI, 1.02–2.42) more likely to adhere to infection control in oral radiology than their single counterparts. In terms of professional performance, teachers/dentists in the public system were 1.56 times (95% CI, 1.00–2.43) more likely to adhere to infection control compared to those in private practice (Table 2). The simple binary regression analysis also indicated that individuals with a master's or doctorate degree were 2.94 times (95% CI, 1.56–5.54) more likely to adhere to infection control than professionals with only undergraduate degrees (Table 2).
In the evaluation of practice fields, professionals in oral radiology were found to be 2.74 times (95% CI, 1.76–4.26) more likely to adhere to infection control protocols than professionals from other fields. Furthermore, dentists with over 10 years of experience were 1.66 times (95% CI, 1.11–2.49) more likely to adhere to these protocols than professionals with 0 to 10 years of experience (Table 2).
The multiple binary regression analysis indicated that, when considering a set of factors (age, continent, marital status, professional performance, professional qualification, field of activity, and duration of professional activity), only the field of activity significantly influenced adherence to infection control in oral radiology. Professionals in oral radiology were found to be 2.08 times more likely to adhere to infection control measures (95% CI, 1.22-3.56) than professionals in other fields (Table 3).
Table 3. Multiple binary regression for questionnaire on infection control in oral radiology (QICOR) scores in dentists (n=389).
CI: confidence interval, Ref: reference variable
For the dental students, only a simple binary regression was performed because there was no P-value<0.05; thus, none of the criteria evaluated were significant (Table 4).
Table 4. Simple binary logistic regression for questionnaire on infection control in oral radiology (QICOR) scores in dental students (n=193).
a: reference variable, b: 5 missing dental student data, CI: confidence interval, Ref: reference variable
Upon analyzing the proportion of participants falling below the median in terms of professional qualifications, it was noted that a larger percentage (44.56%) of dental students fell below the median in adherence to infection control, compared to dentists (43.44%). This suggested that students demonstrated less proficiency in adhering to biosafety protocols.
Discussion
The present study evaluated the adherence of both dentists and dental students to infection control measures in oral radiology amid the COVID-19 pandemic across various continents. The QICOR was utilized as it is a standardized questionnaire, and to date, it is the only specific and updated tool for evaluating infection control in oral radiology.29,30 Although it was recently developed, minor modifications were made to assess infection control in light of COVID-19 protocol updates. However, these changes were not significant enough to necessitate further validation.
The present study showed that individuals from the European continent were more likely to adhere to infection control protocols than those from the Americas, and individuals from Asia were more likely to adhere to infection control protocols than those from the Americas. This disparity between continents could be attributed to the cultural diversity of each social group, which may influence their propensity to adopt rules, including those related to infection control. Despite being the continent most impacted by COVID-19, the Americas demonstrated the lowest likelihood of adhering to infection control measures in oral radiology compared to other continents.
Individuals aged 36 years or older were more likely to adhere to infection control protocols than younger individuals. Similarly, a previous study31 found that dentists aged 40 years or younger demonstrated lower adherence to infection control protocols. However, this finding is not universally agreed upon, as there are studies suggesting that younger or less experienced professionals may be more inclined to follow guidelines compared to their older, more experienced colleagues.32,33 This could be attributed to the fact that professionals with less training tend to exercise more caution in clinical practice, which includes adhering to infection control measures.
Da Costa et al.30 found that professional variables (such as length of professional activity, graduate status, specialty, and employment in public or private service) and age did not significantly impact the likelihood of adhering to infection control measures. Interestingly, despite the extended training period of dentists, which would suggest a higher level of clinical experience, this did not increase the likelihood of adherence to infection control in oral radiology. However, in contrast, the present study found that dentists with more professional experience were more likely to adhere to infection control measures in oral radiology. This discrepancy between the studies could be attributed to the pandemic conditions under which this study was conducted. This unique situation may have influenced changes in attitudes, leading to the adoption of infection control habits that could reduce the spread and transmission of the virus.
A previous study conducted among dentists in Lebanon34 found that, taking into account sociodemographic and professional variables, dentists with over 20 years of experience showed a higher adherence to hand hygiene and the use of personal protective equipment (such as glasses and masks) compared to their less experienced counterparts. This finding is consistent with the results reported in other studies.31,35,36
The literature has reported that scores were associated with professional qualifications.37 According to Tada et al.,33 specialists had a significantly higher adherence to all items of infection control practice than general practitioners. Ebrahimi et al.36 presented outcomes consistent with the results of the present study, showing that dental personnel with a PhD presented a significantly higher level of infection control knowledge than those with only a diploma. These findings suggest that a professional's level of scientific knowledge can positively influence their attitudes toward infection control.
The findings of this study regarding the context of clinical practice (i.e., in a private or public system), this study is in accordance with another that performed a descriptive evaluation of universal precautionary measures for infection control adopted by dentists at public and private offices.38 Although private practices are often viewed as models for infection control, the results highlighted issues such as the use of aprons and caps in the clinical setting. Even when the professional was not directly attending to the patient, adherence was lower than that in public practices.38 Contrary to the findings of this study, other research has shown that the level of compliance with sterilization and disinfection practices by radiologists in private clinics was significantly better than the adherence levels of those working in public and academic institutions.39 This discrepancy may be attributed to the heightened concern of professionals in private care to provide a service that will yield a better financial return, with the aim of satisfying and attracting patients.
Da Costa et al.34 reported that certain students only performed infection control procedures within the radiographic system during their oral radiology course. They further emphasized that despite dentists and students protecting the receptor for digital radiography, there was a breakdown in the aseptic chain with the items used during the execution of digital imaging procedures. Moreover, in dental schools, issues with infection control become more critical due to the high volume of patients and radiographic equipment operators involved. The inexperience of the majority of these operators, who were undergraduate students, further complicated the implementation of stringent infection control protocols.40
Although the present study found a higher rate of dental students falling below the median in infection control compared to dentists, an integrative literature review41 emphasized that their lack of experience during procedures can actually promote adherence to biosafety standards. This is largely due to their persistent fear of contracting an infectious disease. Conversely, dentists, drawing from their experience, tend to overlook these standards. Engelmann et al.42 agreed with the notion that dental professionals often neglect to implement the methods proven effective in maintaining aseptic conditions, as outlined in the literature. The discrepancy between the findings of this study and previous literature, particularly in the comparison between dentists and dental students, may be attributed to the onset of the COVID-19 pandemic. This global health crisis necessitated a shift in professional behavior towards stricter adherence to infection control practices in oral radiology, in order to sustain their professional activities.
A limitation of the current study is the small sample size, particularly from public institutions, due to the COVID-19 pandemic. This is because most universities suspended classes during the research period. Consequently, the inclusion criterion of being engaged in clinical practice and performing intraoral radiographs during the pandemic restricted the student sample. To address this, a prior sample calculation was conducted, resulting in an appropriate "N".
Peng et al.19 reported that only 40% of professionals in the Department of Radiology possessed adequate knowledge of infection control. There is an urgent need to establish and enhance biosafety precautions in oral radiology clinics, given the importance of imaging exams in supplementing diagnoses and informing treatment plans.43 It is crucial to analyze the guidelines of infection prevention and control in Departments of Oral Radiology in order to prevent cross-infection and protect professionals and patients.44 Numerous biosafety instructions are recommended to prevent cross-contamination in radiological clinics, and it is also advised to intensify training activities related to infection control practices for the oral radiology clinic team, particularly during significant outbreaks of infectious diseases such as COVID-19.43,44
It is important to emphasize that the field of oral radiology, particularly the acquisition of intraoral radiography, plays a pivotal role in diagnosing primary maxillofacial pathologies.22 However, despite the existence of numerous recommendations for infection control in oral radiology, these findings underscore the necessity for ongoing education on this subject among dental students and practicing dentists. Given the current COVID-19 pandemic scenario, adherence to infection control protocols is a strategy that can help curb the spread of the disease.
Despite the COVID-19 pandemic, adherence to infection control measures in oral radiology among dental professionals and students was found to be low. There was a significant difference observed in infection control procedures, particularly across different age groups and continents. Individuals from Europe and Asia were more likely to adhere to infection control measures than those from the Americas.
Thus, it is necessary to raise awareness through continuing education related to infection control in oral radiology among students and professionals. This is particularly important for intraoral radiographic techniques, which pose a potential risk for COVID-19 transmission.
Footnotes
Conflicts of Interest: None
References
- 1.World Health Organization. Virtual press conference on COVID-19 – 11 March 2020 [Internet] Geneva: World Health Organization; 2020. [cited Sep 29, 2023]. Available from: https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-full-and-final-11mar2020.pdf . [Google Scholar]
- 2.McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M, Schwartz NG, et al. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382:2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shamszadeh S, Parhizkar A, Mardani M, Asgary S. Dental considerations after the outbreak of 2019 novel coronavirus disease: a review of literature. Arch Clin Infect Dis. 2020;15:e103257 [Google Scholar]
- 5.Gralinski LE, Menachery VD. Return of the coronavirus: 2019-nCoV. Viruses. 2020;12:135. doi: 10.3390/v12020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malik YS, Sircar S, Bhat S, Sharun K, Dhama K, Dadar M, et al. Emerging novel coronavirus (2019-nCoV) - current scenario, evolutionary perspective based on genome analysis and recent developments. Vet Q. 2020;40:68–76. doi: 10.1080/01652176.2020.1727993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jamal M, Shah M, Almarzooqi SH, Aber H, Khawaja S, El Abed R, et al. Overview of transnational recommendations for COVID-19 transmission control in dental care settings. Oral Dis. 2021;27 Suppl 3:655–664. doi: 10.1111/odi.13431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ibrahim NK, Alwafi HA, Sangoof SO, Turkistani AK, Alattas BM. Cross-infection and infection control in dentistry: knowledge, attitude and practice of patients attended dental clinics in King Abdulaziz University Hospital, Jeddah, Saudi Arabia. J Infect Public Health. 2017;10:438–445. doi: 10.1016/j.jiph.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.To KK, Tsang OT, Yip CC, Chan KH, Wu TC, Chan JM, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;71:841–843. doi: 10.1093/cid/ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fallahi HR, Keyhan SO, Zandian D, Kim SG, Cheshmi B. Being a front-line dentist during the Covid-19 pandemic: a literature review. Maxillofac Plast Reconstr Surg. 2020;42:12. doi: 10.1186/s40902-020-00256-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li Y, Ren B, Peng X, Hu T, Li J, Gong T, et al. Saliva is a non-negligible factor in the spread of COVID-19. Mol Oral Microbiol. 2020;35:141–145. doi: 10.1111/omi.12289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee Y, Min P, Lee S, Kim SW. Prevalence and duration of acute loss of smell or taste in COVID-19 patients. J Korean Med Sci. 2020;35:e174. doi: 10.3346/jkms.2020.35.e174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamedani S, Farshidfar N. The practice of oral and maxillofacial radiology during COVID-19 outbreak. Oral Radiol. 2020;36:400–403. doi: 10.1007/s11282-020-00465-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.ADA Council on Scientific Affairs and ADA Council on Dental Practice. Infection control recommendations for the dental office and the dental laboratory. J Am Dent Assoc. 1996;127:672–680. doi: 10.14219/jada.archive.1996.0280. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Recommended infection-control practices for dentistry, 1993. MMWR Recomm Rep. 1993;42(RR-8):1–12. [PubMed] [Google Scholar]
- 19.Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Guidance for dental settings during the COVID-19 response [Internet] Atlanta: Centers for Disease Control and Prevention; 2020. [cited Sep 29, 2023]. Available from: https://emergency.cdc.gov/coca/ppt/2020/Final-COCA-Call-Slides_06-03-2020.pdf . [Google Scholar]
- 21.Pinheiro SL, Martoni SC, Ogera RR. Assessment of microbial contamination of radiographic equipment and materials during intraoral imaging procedures. Minerva Stomatol. 2012;61:197–203. [PubMed] [Google Scholar]
- 22.Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12:8. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Revel MP, Parkar AP, Prosch H, Silva M, Sverzellati N, Gleeson F, et al. COVID-19 patients and the radiology department - advice from the European Society of Radiology (ESR) and the European Society of Thoracic Imaging (ESTI) Eur Radiol. 2020;30:4903–4909. doi: 10.1007/s00330-020-06865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGuigan MB, Duncan HF, Horner K. An analysis of effective dose optimization and its impact on image quality and diagnostic efficacy relating to dental cone beam computed tomography (CBCT) Swiss Dent J. 2018;128:297–316. doi: 10.61872/sdj-2018-04-395. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Summary of infection prevention practices in dental settings: basic expectations for safe care [Internet] Atlanta: Centers for Disease Control and Prevention; 2016. [cited Sep 29, 2023]. Available from: https://www.cdc.gov/oralhealth/infectioncontrol/pdf/safe-care2.pdf . [Google Scholar]
- 27.A AS, Srivastava KC, Shrivastava D, Hosni HA, Khan ZA, Al-Johani K, et al. Recommendations, practices and infrastructural model for the dental radiology set-up in clinical and academic institutions in the COVID-19 era. Biology. 2020;9:334. doi: 10.3390/biology9100334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prati C, Pelliccioni GA, Sambri V, Chersoni S, Gandolfi MG. COVID-19: its impact on dental schools in Italy, clinical problems in endodontic therapy and general considerations. Int Endod J. 2020;53:723–725. doi: 10.1111/iej.13291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.da Costa ED, Pinelli C, da Silva Tagliaferro EP, Corrente JE, Ambrosano GM. Development and validation of a questionnaire to evaluate infection control in oral radiology. Dentomaxillofac Radiol. 2017;46:20160338. doi: 10.1259/dmfr.20160338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.da Costa ED, da Costa AD, Lima CA, Possobon RF, Ambrosano GM. The assessment of adherence to infection control in oral radiology using newly developed and validated questionnaire (QICOR) Dentomaxillofac Radiol. 2018;47:20170437. doi: 10.1259/dmfr.20170437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al-Rabeah A, Moamed AG. Infection control in the private dental sector in Riyadh. Ann Saudi Med. 2002;22:13–17. doi: 10.5144/0256-4947.2002.13. [DOI] [PubMed] [Google Scholar]
- 32.Francke AL, Smit MC, de Veer AJ, Mistiaen P. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak. 2008;8:38. doi: 10.1186/1472-6947-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tada A, Watanabe M, Senpuku H. Factors influencing compliance with infection control practice in Japanese dentists. Int J Occup Environ Med. 2014;5:24–31. [PMC free article] [PubMed] [Google Scholar]
- 34.Dagher J, Sfeir C, Abdallah A, Majzoub Z. Infection control measures in private dental clinics in Lebanon. Int J Dent. 2017;2017:5057248. doi: 10.1155/2017/5057248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ozdede M, Akarslan Z, Altunkaynak B, Peker I. Turkish adaptation and implementation of the modified infection control questionnaire in intraoral digital imaging. Eur Oral Res. 2020;54:130–135. doi: 10.26650/eor.20200129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ebrahimi M, Ajami BM, Rezaeian A. Longer years of practice and higher education levels promote infection control in Iranian dental practitioners. Iran Red Crescent Med J. 2012;14:422–429. [PMC free article] [PubMed] [Google Scholar]
- 37.Kamate SK, Sharma S, Thakar S, Srivastava D, Sengupta K, Hadi AJ, et al. Assessing knowledge, attitudes and practices of dental practitioners regarding the COVID-19 pandemic: a multinational study. Dent Med Probl. 2020;57:11–17. doi: 10.17219/dmp/119743. [DOI] [PubMed] [Google Scholar]
- 38.Garbin AJI, Garbin CA, Arcieri RM, Crossato M, Ferreira NF. Biosecurity in public and private office. J Appl Oral Sci. 2005;13:163–166. doi: 10.1590/s1678-77572005000200013. [DOI] [PubMed] [Google Scholar]
- 39.Alakhras M, Al-Mousa DS, Mahasneh A, AlSa'di AG. Factors affecting compliance of infection control measures among dental radiographers. Int J Dent. 2020;2020:8834854. doi: 10.1155/2020/8834854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Malta CP, Damasceno NN, Ribeiro RA, Silva CS, Devito KL. Microbiological contamination in digital radiography: evaluation at the radiology clinic of an educational institution. Acta Odontol Latinoam. 2016;29:239–247. [PubMed] [Google Scholar]
- 41.Bezerra AL, Sousa MN, Feitosa AN, Assis EV, Barros CM, Carolino EC. Biosafety in dentistry. ABCS Health Sci. 2014;39:29–33. [Google Scholar]
- 42.Engelmann AI, Daí AA, Miura CS, Bremm LL, Boleta-Ceranto DC. Evaluation of procedures performed by suregen-dentists from Cascavel state of Parana and surroundings for biossecurity control. Odontol Clín Cient. 2010;9:161–165. [Google Scholar]
- 43.Pieralisi N, Souza-Pinto GN, Iwaki VL, Chicarelli-Silva M, Tolentino SE. Biosecurity perspectives in oral and maxillofacial radiology in times of coronavirus disease (COVID-19): a literature review. Int J Odontostomat. 2021;15:77–81. [Google Scholar]
- 44.Yu J, Ding N, Chen H, Liu XJ, He WJ, Dai WC, et al. Infection control against COVID-19 in Departments of Radiology. Acad Radiol. 2020;27:614–617. doi: 10.1016/j.acra.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]