Abstract
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has triggered a rise in the global phenomenon of self-medication. The use of medicines with unsubstantiated claims of benefit for the prevention and/or treatment of infected people has been widely adopted.
Objective
To determine the factors associated with the use of medicines and self-medication by Latin American populations during the COVID-19 pandemic.
Methods
This analytical cross-sectional study was conducted via an analysis of secondary data collected from 8777 responses from 12 Latin American countries obtained from a survey on the use of medicines and self-medication during the pandemic.
Results
Respondents who reported using Paracetamol, Ibuprofen, or antibiotics (ABx) disclosed this as self-medication in 26.9%, 16.6%, and 9.7% of cases respectively. In our multivariate analysis, significant associations were found between: self-medication by individual choice and the use of Hydroxychloroquine, ABx, or non-steroidal anti-inflammatory drugs (NSAIDs) (p = 0.026, = 0.003, and <0.001 respectively); self-medication on the recommendation of a family member, with ABx, Paracetamol, Ibuprofen, or other NSAIDs (p <0.001, <0.001, <0.001, and <0.001 respectively); and self-medication on the recommendation of another person, with Chloroquine, Hydroxychloroquine, Azithromycin, Penicillin, other ABx, Warfarin, Ivermectin, Paracetamol, Ibuprofen, or other NSAIDs (p <0.001, <0.001, <0.001, = 0.001, <0.001, <0.001, = 0.004, <0.001, <0.001, and <0.001 respectively).
Conclusion
There was a significantly high prevalence of self-medication in our Latin American study population, including the use of medicines not recommended for COVID-19 treatment and/or prevention. The implementation of public health measures aimed at combating the worrying COVID-19 infodemic is essential to prevent this ongoing issue and its associated negative impacts on both current public health and future medication efficacy. This is especially important in the case of ABx due to the threat of a future antimicrobial resistance pandemic.
Keywords: Self-medication, Prescription drugs, COVID-19, Pandemics, Latin America
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has represented the most significant public health challenge of the 21st century [1], with more than 676,600,000 confirmed cases of the disease worldwide and approximately 6,881,000 deaths (as of 14/03/2023). Of the Latin American countries, Brazil, Mexico, and Peru, occupy the second, fifth and, sixth positions respectively, in terms of the global number of deaths from COVID-19 (as of 14/03/2023) [2]. Within this context the pandemic has had serious negative impacts on the usual functioning of local economy, politics, and daily social life [3].
In addition to the rapid spread of COVID-19, coupled with the fact that it was a new disease to be identified in humans, the evidence to support and approve effective medicines for its treatment is both recent and ongoing [4]. As a result, medicines for the disease are not yet widely available through national healthcare services in many countries around the world, especially in developing countries [5]. By contrast, during most of the pandemic, the use of medicines with unsubstantiated claims of benefit for the prevention and/or treatment of infected people has been widely adopted by the public, largely due to fear of the disease [6]. Three examples of such medications are Hydroxychloroquine, Azithromycin, and Ivermectin, which were subject to much debate and controversy on the part of governments and scientists [7,8], and particularly on social media, as there remained a lack of robust scientific evidence for their use against COVID-19 [6,8].
Faced with the knowledge that people are taking the use of medications into their own hands, it is of imminent importance to know which unproven medicines have been used for COVID-19 prevention and/or treatment in Latin American countries during the pandemic. Further, it may be beneficial to identify factors associated with their use, since there are many cultures and beliefs across the region which could predispose to self-medication [6], in addition to the influence of the media [9,10]. With this knowledge in hand, effective and population-targeted public health measures could then be implemented in order to better inform and help people, thereby minimizing health risks. However, to date, only a few studies on this subject involving Latin American countries have been published. Thus, in this novel study we determine the factors associated with the use of medicines and self-medication by the Latin American population during the COVID-19 pandemic.
2. Methods
2.1. Design and participants
This is an analytical cross-sectional study of secondary data obtained from a survey conducted by members of the Latin American Federation of Scientific Societies of Medical Students (FELSOCEM). People over the age of 18 years old, from Bolivia, Chile, Colombia, Costa Rica, Ecuador, El Salvador, Guatemala, Honduras, Mexico, Panama, Paraguay, and Peru were included in the study. Participants who did not fully complete the survey were excluded. A total of 10557 respondents answered the survey, of which 1780 did not meet the inclusion criteria. Thus, a total of 8777 respondents were included in the analysis, with a response rate of 82.98%.
A power calculation was performed [11], of which 8 cases did not achieve a power of 80% and were therefore not considered; since they had a reduced confidence in the associations found. These are the following: individual self-medication with Azithromycin (0.0799), Penicillin (0.7758), other antibiotics (ABx) (0.7205), Warfarin (0.0987), Paracetamol (0.7025), Ibuprofen (0.4818), Hydroxychloroquine (0.0404), and self-medication with Ivermectin on the recommendation of a family member (0.4301).
The sample size selection process is detailed below (Fig. 1). The survey was distributed through social networks, in this case, via the social networking groups of members of FELSOCEM.
Fig. 1.
Flowchart of study sample size selection.
2.2. Ethics and procedures
The present study was approved by the Research Ethics Committee of the Universidad Peruana de Ciencias Aplicadas (FCS-CEI/777-12-20). The retrospective data of this study were obtained from a previous virtual survey [supplementary material]. The survey was conducted between June and August 2020, to learn about the reality of part of the Latin American population during the COVID-19 pandemic, given that the first peak in the spread of the disease occurred during this period. Participants were informed that the survey would be anonymous and consent was requested as a pre-requisite for participation. The mentioned survey was distributed with detailed instructions. Participants were also informed that they could decline to answer any or all of the questions if they wished. Responses were recorded in a Google Form, which was the platform used to distribute the survey.
2.3. Variables
For this study three types of self-medication were considered and analyzed: self-medication by individual choice, on the recommendation of a family member or on the recommendation of another person. The survey asked about the use of 10 types of medications: Paracetamol, Ibuprofen, other non-steroidal anti-inflammatory drugs (NSAIDs), Hydroxychloroquine, Chloroquine, Azithromycin, Penicillin, other ABx, Warfarin, and Ivermectin. It was asked about the frequency of use of each type of medication, as well as if their use was by medical prescription or self-medication. Each respondent was also asked whether or not they consumed any of these medicines during the pandemic. In addition, demographic data, including age (quantitative variable), gender (male or female), country of residence (Peru, Chile, Paraguay, Mexico, Colombia, Bolivia, Panama, Ecuador, Costa Rica, El Salvador, Honduras, and Guatemala), and educational level (secondary school or high school, technical school, university, postgraduate) were collected. The survey was conducted in Spanish, since this is the language spoken in the countries participating in the study. All responses were later translated into English by the authors of the study.
2.4. Statistics
The data collection strategy was carried out as described above. The collected data was assessed by experts from the countries that participated in the research. For the univariate statistics, the categorical variables were described by absolute and relative frequencies, aside from the quantitative variable ‘age’, which was described by median interquartile range. For the bivariate and multivariate analysis, a p-value <0.05 was considered statistically significant. The dependent variables were medicines use and self-medication. Models with robust variances were used. For the bivariate and multivariate analysis of the factors associated with self-medication, the Poisson regression model was used, where each analysis was adjusted for age, gender, country of residence, and education level.
3. Results
Of the total respondents, 59.6% (6314) were female, and the average age was 22 years old (interquartile range: 20–28). Peru was found to be the country with the highest number of respondents, with 4293 participants (48.9% of the study population) (Table 1).
Table 1.
Demographic details of participants.
| Variable | n = 8777 | % |
|---|---|---|
| Gender | ||
| Women | 5235 | 59.6 |
| Man | 3542 | 40.4 |
| Age∗ | M = 22 | IQR = 20-28 |
| Country | ||
| Peru | 4293 | 48.9 |
| Chile | 777 | 8.9 |
| Mexico | 677 | 7.7 |
| Paraguay | 644 | 7.3 |
| Colombia | 481 | 5.5 |
| Bolivia | 429 | 4.9 |
| Panama | 418 | 4.8 |
| Ecuador | 291 | 3.3 |
| Costa Rica | 257 | 2.9 |
| El Salvador | 209 | 2.4 |
| Honduras | 185 | 2.1 |
| Guatemala | 116 | 1.3 |
| Education level | ||
| Secondary school or high school | 1895 | 21.6 |
| Technical school | 679 | 7.7 |
| University | 5560 | 63.4 |
| Postgraduate | 643 | 7.3 |
Age reported in years, median (M) and interquartile range (IQR) are given.
Paracetamol was the most widely used medication, reported by 2361 participants (26.9% of the study population) (Table 2).
Table 2.
Medications used by participants.
| Variable | n = 8777 | % |
|---|---|---|
| Chloroquine | ||
| Consumption | 105 | 1.2 |
| No consumption | 8672 | 98.8 |
| Hydroxychloroquine | ||
| Consumption | 124 | 1.4 |
| No consumption | 8653 | 98.6 |
| Azithromycin | ||
| Consumption | 387 | 4.4 |
| No consumption | 8390 | 95.6 |
| Penicillin | ||
| Consumption | 211 | 2.4 |
| No consumption | 8566 | 97.6 |
| Other ABx | ||
| Consumption | 849 | 9.7 |
| No consumption | 7928 | 90.3 |
| Warfarin | ||
| Consumption | 108 | 1.2 |
| No consumption | 8669 | 98.8 |
| Ivermectin | ||
| Consumption | 209 | 2.4 |
| No consumption | 8568 | 97.6 |
| Paracetamol | ||
| Consumption | 2361 | 26.9 |
| No consumption | 6416 | 73.1 |
| Ibuprofen | ||
| Consumption | 1456 | 16.6 |
| No consumption | 7321 | 83.4 |
| Other NSAIDs | ||
| Consumption | 951 | 10.8 |
| No consumption | 7826 | 89.2 |
ABx: antibiotics. NSAIDs: non-steroidal anti-inflammatory drugs.
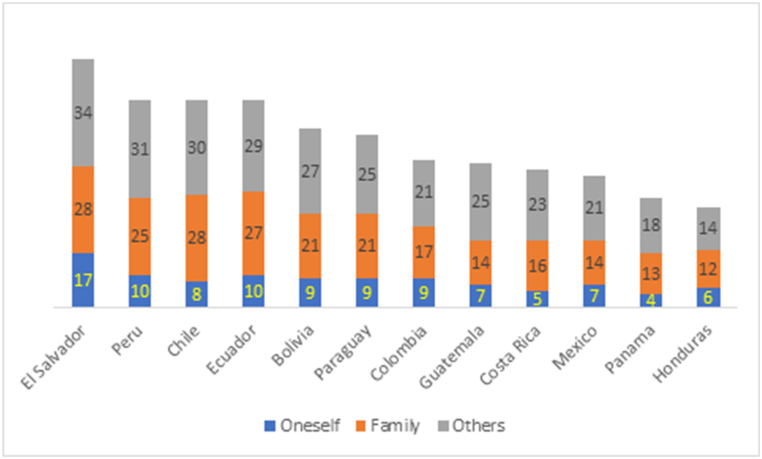
The countries reporting the highest cumulative percentages of self-medication (individual choice, on the recommendation of a family member, and on the recommendation of another person) were El Salvador with 79%, followed by Peru, Chile, and Ecuador with 66% each. Those with the lowest percentages were Panama and Honduras with 35% and 32%, respectively (Fig. 2).
Fig. 2.
Percentages of individual self-medication, on the recommendation of a family member, and on the recommendation of another person in 12 Latin American countries during the pandemic, based on the survey.
When bivariate and multivariate analysis were performed for the self-medication by individual choice group, we found a higher use of Hydroxychloroquine (p = 0.026), other ABx (p = 0.003), and other NSAIDs (p <0.001), while there was lower use of Ivermectin (p = 0.005). Furthermore, for all medicines aside from Hydroxychloroquine, there was a higher prevalence of use amongst men (all p-values <0.05). A positive association with increasing age of the respondents (all p-values <0.001) was also observed. All associations were adjusted for participants having COVID-19, their gender, age, educational level, and country of residence (Table 3).
Table 3.
Bivariate (n = 3860) and multivariate (n = 3814) analysis of factors associated with self-medication by individual choice.
| Medicine | Bivariate analysis | Multivariate analysis according to |
|||
|---|---|---|---|---|---|
| Self-medication | Positive COVID-19 | Gender ♂ | Age | ||
| Chloroquine | 0.446 | 0.107 | 0.182 | 0.049 + | <0.001 + |
| Hydroxychloroquine | 0.327 | 0.026 + | 0.308 | 0.052 | <0.001 + |
| Azithromycin | 0.837 | 0.517 | 0.161 | 0.045 + | <0.001 + |
| Penicillin | 0.505 | 0.650 | 0.269 | 0.046 + | <0.001 + |
| Other ABx | 0.201 | 0.003 + | 0.181 | 0.040 + | <0.001 + |
| Warfarin | 0.916 | 0.798 | 0.090 | 0.040 + | <0.001 + |
| Ivermectin | 0.259 | 0.005 - | 0.115 | 0.038 + | <0.001 + |
| Paracetamol | 0.080 | 0.137 | 0.206 | 0.028 + | <0.001 + |
| Ibuprofen | 0.254 | 0.066 | 0.121 | 0.029 + | <0.001 + |
| Other NSAIDs | 0.031 + | <0.001 + | 0.176 | 0.037 + | <0.001 + |
COVID-19: coronavirus disease 2019. ABx: antibiotics. NSAIDs: non-steroidal anti-inflammatory drugs. P-values were obtained using generalized linear models, with the Poisson distribution and a logarithmic link function, and models for robust variance adjusted. In the multivariate model, we adjusted for educational level and country of residence. The sign indicates whether the prevalence of drug use was found to be higher (+) or lower (−).
When considering factors associated with self-medication on the recommendation of a family, an increased use of other ABx (p = 0.003), Paracetamol (p <0.001), Ibuprofen (p <0.001), and other NSAIDs (p <0.001) was elicited by the multivariate analysis. In addition, there was an increased use of these medications in participants who had COVID-19 (all p-values <0.001). All associations were adjusted for participants having COVID-19, their gender, age, educational level, and country of residence (Table 4).
Table 4.
Bivariate (n = 3869) and multivariate (n = 3823) analysis of factors associated with self-medication on the recommendation of a family member.
| Medicine | Bivariate analysis | Multivariate analysis according to |
|||
|---|---|---|---|---|---|
| Self-medication | Positive COVID-19 | Gender ♂ | Age | ||
| Chloroquine | 0.234 | 0.251 | 0.976 | 0.377 | 0.316 |
| Hydroxychloroquine | 0.968 | 0.899 | 0.887 | 0.414 | 0.265 |
| Azithromycin | 0.037 + | 0.051 | 0.956 | 0.338 | 0.325 |
| Penicillin | 0.365 | 0.323 | 0.974 | 0.385 | 0.261 |
| Other ABx | <0.001 + | <0.001 + | 0.942 | 0.513 | 0.806 |
| Warfarin | 0.472 | 0.321 | 0.789 | 0.460 | 0.249 |
| Ivermectin | 0.664 | 0.348 | 0.934 | 0.381 | 0.270 |
| Paracetamol | <0.001 + | <0.001 + | 0.880 | 0.609 | 0.381 |
| Ibuprofen | <0.001 + | <0.001 + | 0.738 | 0.961 | 0.878 |
| Other NSAIDs | <0.001 + | <0.001 + | 0.990 | 0.559 | 0.248 |
COVID-19: coronavirus disease 2019. ABx: antibiotics. NSAIDs: non-steroidal anti-inflammatory drugs. P-values were obtained using generalized linear models, with the Poisson distribution and a logarithmic link function, and models for robust variance adjusted. In the multivariate model, we adjusted for educational level and country of residence. The sign indicates whether the prevalence of drug use was found to be higher (+) or lower (−).
Finally, in the multivariate analysis of factors associated with self-medication on the recommendation of another person, there was an increased use of all the study-assessed medications (Penicillin (p = 0.001), Ivermectin (p = 0.004), and the other medicines (all p-values <0.001)). This positive statistical relationship was further observed in all cases of participants with COVID-19 (all p-values <0.001). All associations were adjusted for participants having COVID-19, their gender, age, educational level, and country of residence (Table 5).
Table 5.
Bivariate (n = 3866) and multivariate (n = 3820) analysis of factors associated with self-medication on the recommendation of another person.
| Medicine | Bivariate analysis |
Multivariate analysis according to |
|||
|---|---|---|---|---|---|
| Self-medication | Positive COVID-19 | Gender ♂ | Age | ||
| Chloroquine | <0.001 + | <0.001 + | <0.001 + | 0.207 | 0.547 |
| Hydroxychloroquine | 0.005 + | <0.001 + | <0.001 + | 0.227 | 0.505 |
| Azithromycin | <0.001 + | <0.001 + | <0.001 + | 0.183 | 0.661 |
| Penicillin | 0.006 + | 0.001 + | <0.001 + | 0.266 | 0.471 |
| Other ABx | <0.001 + | <0.001 + | <0.001 + | 0.370 | 0.641 |
| Warfarin | 0.016 + | <0.001 + | <0.001 + | 0.218 | 0.482 |
| Ivermectin | 0.029 + | 0.004 + | <0.001 + | 0.235 | 0.487 |
| Paracetamol | <0.001 + | <0.001 + | <0.001 + | 0.899 | 0.333 |
| Ibuprofen | <0.001 + | <0.001 + | <0.001 + | 0.766 | 0.794 |
| Other NSAIDs | <0.001 + | <0.001 + | <0.001 + | 0.413 | 0.419 |
COVID-19: coronavirus disease 2019. ABx: antibiotics. NSAIDs: non-steroidal anti-inflammatory drugs. P-values were obtained using generalized linear models, with the Poisson distribution and a logarithmic link function, and models for robust variance adjusted. In the multivariate model, we adjusted for educational level and country of residence. The sign indicates whether the prevalence of drug use was found to be higher (+) or lower (−).
4. Discussion
We demonstrated evidence of a high prevalence of self-medication tendencies in the Latin American populations in the 12 included countries. The majority of respondents were young, with a median age of 22 years, and female (59.6%). We observed that the most frequently used medicine in the study population was Paracetamol (26.9%), followed by Ibuprofen (16.6%). We also noted an increased use of these medicines in patients who had been infected with COVID-19. Corroborating our findings, a previous study reported that Acetaminophen (an alternative name for Paracetamol) was the most frequent choice of self-medication used by undergraduate nursing students for symptoms including fever, headache, cough, and sore throat, with a prevalence of 87% [12].
For this study, three classes of self-medication were considered and analyzed: self-medication by individual choice, on the recommendation of a family member, or on the recommendation of another person. When combining these three classes of self-medication, we found that El Salvador was the country with the highest degree of self-medication among the 12 Latin American countries evaluated (79%), followed closely by Peru, Chile, and Ecuador, while Honduras was the country with the lowest level of self-medication (32%). By individual class, self-medication on the recommendation of another person was predominant in El Salvador. Although to date there is little robust published evidence on self-medication and medicines used in Latin America during the pandemic, data describing the rates of self-medication in other countries, such as Togo, show an overall prevalence of 34.2% for self-medication during this period [13]. Moreover, another study conducted in Uganda found a decrease in self-medication practices during the confinement period [14], which means that some Latin American countries may have actually had a higher prevalence of self-medication during the pandemic on a global scale.
We also found that Hydroxychloroquine, other ABx, and other NSAIDs were frequently consumed, while Ivermectin was consumed in a lower proportion. According to the Peruvian study by Zavala-Flores and Salcedo-Matienzo, uncertainties surrounding the prevention and/or treatment of COVID-19 have led to the widespread use of medications based on “pathophysiological plausibility” or findings from in-vitro studies. In addition, difficulties faced by the public in accessing healthcare services may well have contributed to the adoption of self-medication. The above authors observed that around 80% of patients hospitalized by COVID-19 in their sample, had received or taken some form of ‘treatment’ prior to admission, of which 33.9% were without a medical prescription [15]. Another recent Colombian study also shows high levels of self-medication among adults during the lockdown period [16], which supports our findings on self-medication in Latin American countries during the pandemic.
A further important point in the present study was the greater rate of self-medication amongst the male participants. The most commonly used medicines in this group were Chloroquine, Azithromycin, Penicillin, other ABx, Warfarin, Ivermectin, Paracetamol, Ibuprofen, and other NSAIDs, whilst the least consumed drug was Hydroxychloroquine. The increasing age of male participants was found to be directly proportional to the chance of self-medication. This result contradicts the results of a previous study on factors associated with self-medication for COVID-19 by Peruvian healthcare students, which reported that female gender was associated with higher rates of self-medication [17]. This could be due to different factors. First, the survey used in our study was conducted during the first few months of the pandemic. Second, women tend to have a greater degree of anxiety, thus leading to a greater potential tendency to self-medication [18].
It is also worth highlighting that our findings surrounding self-medication on the recommendation of a family member revealed that the most used medicines were other ABx, Paracetamol, Ibuprofen, and other NSAIDs. Although the recommendation to self-medication can come from friends, family, neighbors, pharmacists, clinicians, or even previous prescriptions, the current trend of seeking advice online has been intensified by the role of the media [19,20].
Despite the above, self-medication on the recommendation of another person still occurred with significant rates across all 10 medication groups in this study. Our results can be viewed in conjunction with those of a study entitled “Self-medication in adults in 11 Latin American cities”, which inquired about who recommended which medicines to the participants. Whilst 56.1% of participants reported that the recommendation came from family and friends, only 26.8% reported that the recommendation came from a pharmacist [21]. This fact is of critical importance, as it indicates the weight which the opinions of trusted third parties can hold in the decisions taken by this Latin American population. Therefore, this should present a prime opportunity for interventions to build trust and influence amongst healthcare professionals, in order to avoid the potential harmful effects on health which may present with unadvised self-medication.
In addition to this finding, we also observed a higher rate of self-medication on the recommendation of another person of all the studied medications by participants with COVID-19. Although the inherent risks of the disease are known to many people, this may not necessarily have a significant impact on decisions about self-medication. Also, in the absence of widely available robust scientific evidence about COVID-19 prevention and/or treatment during the early stages of the pandemic, the proliferation of false information, misinformation, and medical mistrust may in fact have occurred and spread amongst vulnerable populations [19,20]. Indeed, the influence of social media has been critically devastating with regards to causing confusion and fear, and propagating false information, which has certainly contributed to an increase in self-medication, including the use of home remedies, with unsubstantiated claims of reliability and efficacy [20,22].
This study is not without its limitations. It suffers potential selection bias, due to the type of sampling used, and it is therefore not possible to extrapolate the results directly to all the surveyed countries, since the study intention was only to analyze associations. This is due to the non-probabilistic convenience sampling used, which is not significant for the entire populations of each included country. Furthermore, in our survey there were no specific questions that could determine which type of person/professional recommended self-medication in cases of self-medication on the recommendation of another person, which should be evaluated in future research. Nevertheless, our results are meaningful and robust, given the large sample of people who completed the survey between June and August 2020, which is the period in which the pandemic had the first severe impact on Latin America. Further, our results build upon previous published material based on only one Latin American country [23], thereby extending their applicability and impact.
5. Conclusion
This study shows a significantly high prevalence of self-medication among the population of different countries in Latin America, including the use of medicines not recommended for COVID-19 prevention and/or treatment. Although the public is advised against consuming medications without proper medical advice or prescription, due to health-related risks, more action is needed so that the general public is indeed properly educated and informed before taking any medication when seeking medical assistance, either by teleconsultation or via face-to-face medical consultation, as well as when buying over-the-counter medications. To achieve this, public health measures aimed at combating the worrying COVID-19 infodemic should be implemented in order to prevent this ongoing issue and its associated negative impacts on both current public health and future medication efficacy.
Funding
Universidad Peruana de Ciencias Aplicadas/UPC-EXPOST-2023-2.
Data availability statement
Data included in article/supp. material/referenced in article.
CRediT authorship contribution statement
Christian R. Mejia: Writing – original draft, Validation, Supervision, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Mely Ruiz-Aquino: Writing – original draft, Resources, Investigation, Conceptualization. Gianela Garcia-Arteta: Writing – original draft, Resources, Investigation, Conceptualization. Gin Ramos: Writing – original draft, Resources, Investigation, Conceptualization. Isabel Astete-Pérez: Writing – original draft, Resources, Investigation, Conceptualization. Mariana Pineda-Cáceres: Writing – original draft, Resources, Investigation, Conceptualization. Mariluz Collahua-Briceño: Writing – original draft, Resources, Investigation, Conceptualization. Katherine Vargas-Patiño: Writing – original draft, Resources, Investigation, Conceptualization. Dennis Arias-Chávez: Writing – original draft, Resources, Investigation, Formal analysis, Data curation, Conceptualization. Thomas Franchi: Writing – review & editing, Writing – original draft, Methodology, Formal analysis. Paolo Pedersini: Writing – review & editing, Writing – original draft, Methodology, Formal analysis. Marcos Roberto Tovani-Palone: Writing – review & editing, Writing – original draft, Supervision, Project administration, Methodology, Investigation, Formal analysis.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
PP thanks the Italian Ministry of Health-Ricerca Corrente 2023, and MRT-P thanks the Saveetha Institute of Medical and Technical Sciences and SRM Institute of Science and Technology for supporting this study. CRM, GG-A, GR, IA-P, MP-C, and MC-B thank the Dirección de Investigación of the Universidad Peruana de Ciencias Aplicadas for the support provided to this research with the grant UPC-EXPOST-2023-2.
Contributor Information
Christian R. Mejia, Email: christian.mejia.md@gmail.com.
Marcos Roberto Tovani-Palone, Email: marcos_palone@hotmail.com.
References
- 1.World Health Organization (WHO) WHO; Geneva: 2021. Weekly Epidemiological Update on COVID-19-31 August 2021.https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---31-august-2021 [accessed 2022 Jun 01]. Available from: [Google Scholar]
- 2.Johns Hopkins Coronavirus Resource Center World Map [Internet] https://coronavirus.jhu.edu/map.html [accessed 2023 Mar 14]. Available at:
- 3.Bański J., Mazur M., Kamińska W. Socioeconomic conditioning of the development of the COVID-19 pandemic and its global spatial differentiation. Int. J. Environ. Res. Publ. Health. 2021;18(9):4802. doi: 10.3390/ijerph18094802. PMID: 33946284; PMCID: PMC8125126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) WHO; Geneva: 2021. On New Recommendation for Treatment of COVID-19 Patients: WHO Calls for Equitable Access to Casirivimab and Imdevimab for COVID-19.https://www.who.int/news/item/24-09-2021-on-new-recommendation-for-treatment-of-covid-19-patients-who-calls-for-equitable-access-to-casirivimab-and-imdevimab-for-covid-19 [accessed 2022 Jun 01]. Available at: [Google Scholar]
- 5.Silverman E. STAT; Boston: 2021. WHO Adds Regeneron Drug to Recommended Covid-19 Treatments, but Criticizes its Pricing.https://www.statnews.com/pharmalot/2021/09/24/who-adds-regeneron-drug-to-recommended-covid-19-treatments-but-criticizes-its-pricing/#:∼:text=The%20World%20Health%20Organization,distribution%20of%20the%20drug%20globally [accessed 2022 Jun 01]. Available at: [Google Scholar]
- 6.Yáñez J.A., Chung S.A., Román B.R., Hernández-Yépez P.J., Garcia-Solorzano F.O., Del-Aguila-Arcentales S., et al. 2021. Prescription, over-the-counter (OTC), herbal, and other treatments and preventive uses for COVID-19; pp. 379–416. (Environmental and Health Management of Novel Coronavirus Disease (COVID-19)). PMCID: PMC8237643. [DOI] [Google Scholar]
- 7.Biernath A. 2021. Tratamento precoce | 'Kit covid é kit ilusão': os dados que apontam riscos e falta de eficácia do suposto tratamento [Early treatment | 'Kit covid is an illusion kit': data that point to risks and lack of effectiveness of the supposed treatment]. São Paulo: BBC News Brasil.https://www.bbc.com/portuguese/brasil-55775106 [accessed 2022 Jun 01]. Portuguese. Available at: [Google Scholar]
- 8.Mega E.R. Latin America’s embrace of an unproven COVID treatment is hindering drug trials. Nature. 2020;586(7830):481–482. doi: 10.1038/d41586-020-02958-2. PMID: 33077974. [DOI] [PubMed] [Google Scholar]
- 9.Mejia C.R., Ticona D., Rodriguez-Alarcon J.F., Campos-Urbina A.M., Catay-Medina J.B., Porta-Quinto T., et al. The media and their informative role in the face of the coronavirus disease 2019 (COVID-19): validation of fear perception and magnitude of the issue (MED-COVID-19) Electron. J. Gen. Med. 2020;17(6) doi: 10.29333/ejgm/7946. [DOI] [Google Scholar]
- 10.Tovani-Palone M.R., Ali S. The media and the early dissemination of information on medicines for COVID-19: current scenario in Pakistan. Einstein (Sao Paulo) 2021;19 doi: 10.31744/einstein_journal/2021CE6354. PMID: 33886936; PMCID: PMC8029642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramos-Vera C.A. Un método de cálculo de tamaño muestral de análisis de potencia a priori en modelos de ecuaciones estructurales [A sample size calculation method for a priori power analysis in structural equation models] Rev Cuerpo Med HNAAA. 2021;14(1):104–105. [Google Scholar]
- 12.Faqihi A.H.M.A., Sayed S.F. Self-medication practice with analgesics (NSAIDss and acetaminophen), and antibiotics among nursing undergraduates in University College Farasan Campus, Jazan University, KSA. Ann. Pharm. Fr. 2021;79(3):275–285. doi: 10.1016/j.pharma.2020.10.012. PMID: 33098875; PMCID: PMC7577276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sadio A.J., Gbeasor-Komlanvi F.A., Konu R.Y., Bakoubayi A.W., Tchankoni M.K., Bitty-Anderson A.M., et al. Assessment of self-medication practices in the context of the COVID-19 outbreak in Togo. BMC Publ. Health. 2021;21(1):58. doi: 10.1186/s12889-020-10145-1. PMID: 33407321; PMCID: PMC7787400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dare S.S., Eze E.D., Echoru I., Usman I.M., Ssempijja F., Bukenya E.E., Ssebuufu R. Behavioural response to self-medication practice before and during Covid-19 pandemic in Western Uganda. Patient Prefer. Adherence. 2022;16:2247–2257. doi: 10.2147/PPA.S370954. PMID: 36034331; PMCID: PMC9400814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zavala-Flores Ernesto, Jannin Salcedo-Matienzo. Medicación prehospitalaria en pacientes hospitalizados por COVID-19 en un hospital público de Lima-Perú [Pre-hospitalary medication in COVID-19 patients from a public hospital in Lima-Peru] Acta Méd. Peru. 2020;37(3):393–395. doi: 10.35663/amp.2020.373.1277. Spanish. [DOI] [Google Scholar]
- 16.Gaviria-Mendoza A., Mejía-Mazo D.A., Duarte-Blandón C., Castrillón-Spitia J.D., Machado-Duque M.E., Valladales-Restrepo L.F., et al. Self-medication and the 'infodemic' during mandatory preventive isolation due to the COVID-19 pandemic. Ther. Adv. Drug Saf. 2022;13 doi: 10.1177/20420986221072376. PMID: 35237406; PMCID: PMC8882931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miñan-Tapia A., Conde-Escobar A., Calderon-Arce D., Cáceres-Olazo D., Peña-Rios A.J., Carlos Donoso-Romero R.C. Scielo Preprints; Spanish: 2020. Factores asociados a la automedicación con fármacos relacionados a COVID-19 en estudiantes de ciencias de la salud de una ciudad peruana [Associated factors to self-medication with drugs related to COVID-19 in health science students from a peruvian city] p. 22.https://preprints.scielo.org/index.php/scielo/preprint/view/1225 Available from: [Google Scholar]
- 18.Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Niveles de estrés, ansiedad y depresión en la primera fase del brote del COVID-19 en una muestra recogida en el norte de España [Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain] Cad. Saúde Pública. 2020;36(4) doi: 10.1590/0102-311X00054020. PMID: 32374806. [DOI] [PubMed] [Google Scholar]
- 19.The Lancet Infectious Diseases The COVID-19 infodemic. Lancet Infect. Dis. 2020;20(8):875. doi: 10.1016/S1473-3099(20)30565-X. PMID: 32687807; PMCID: PMC7367666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmad S., Babar M.S., Essar M.Y., Sinha M., Nadkar A. Infodemic, self-medication and stockpiling: a worrying combination. East. Mediterr. Health J. 2021;27(5):438–440. doi: 10.26719/emhj.21.010. PMID: 34080670. [DOI] [PubMed] [Google Scholar]
- 21.Escobar-Salinas J., Sebastián, Rios-González C., Miguel Automedicación en adultos de 11 ciudades de Latinoamérica, 2015-2016: estudio multicéntrico [Self-medication for adults in 11 cities in Latin America, 2015-2016: a multicenter study] CIMEL. 2017;22(2):19–23. Spanish. [Google Scholar]
- 22.Cinelli M., Quattrociocchi W., Galeazzi A., Valensise C.M., Brugnoli E., Schmidt A.L., Zola P., Zollo F., Scala A. The COVID-19 social media infodemic. Sci. Rep. 2020;10(1) doi: 10.1038/s41598-020-73510-5. PMID: 33024152; PMCID: PMC7538912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quispe-Cañari J.F., Fidel-Rosales E., Manrique D., Mascaró-Zan J., Huamán-Castillón K.M., Chamorro-Espinoza S.E., et al. Self-medication practices during the COVID-19 pandemic among the adult population in Peru: a cross-sectional survey. Saudi Pharmaceut. J. 2021;29(1):1–11. doi: 10.1016/j.jsps.2020.12.001. PMID: 33519270; PMCID: PMC7832015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supp. material/referenced in article.