Abstract
Acrylamide is an environmental electrophile that has been produced in large amounts for many years. There is concern about the adverse health effects of acrylamide exposure due to its widespread industrial use and also presence in commonly consumed foods and others. IL-1β is a key cytokine that protects the brain from inflammatory insults, but its role in acrylamide-induced neurotoxicity remains unknown. We reported recently that deletion of IL-1β gene exacerbates ACR-induced neurotoxicity in mice. The aim of this study was to identify genes or signaling pathway(s) involved in enhancement of ACR-induced neurotoxicity by IL-1β gene deletion or ACR-induced neurotoxicity to generate a hypothesis mechanism explaining ACR-induced neurotoxicity. C57BL/6 J wild-type and IL-1β KO mice were exposed to ACR at 0, 12.5, 25 mg/kg by oral gavage for 7 days/week for 4 weeks, followed by extraction of mRNA from mice cerebral cortex for RNA sequence analysis. IL-1β deletion altered the expression of genes involved in extracellular region, including upregulation of PFN1 gene related to amyotrophic lateral sclerosis and increased the expression of the opposite strand of IL-1β. Acrylamide exposure enhanced mitochondria oxidative phosphorylation, synapse and ribosome pathways, and activated various pathways of different neurodegenerative diseases, such as Alzheimer disease, Parkinson disease, Huntington disease, and prion disease. Protein network analysis suggested the involvement of different proteins in related to learning and cognitive function, such as Egr1, Egr2, Fos, Nr4a1, and Btg2. Our results identified possible pathways involved in IL-1β deletion-potentiated and ACR-induced neurotoxicity in mice.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00204-023-03627-9.
Keywords: Acrylamide, IL-1β, Neurotoxicity, Transcriptome, Mouse cerebral cortex
Introduction
Acrylamide (ACR) has been used extensively in paper and textile industries, as well as for soil conditioning, wastewater treatment, and polymer production (Smith and Oehme 1991). In 1994, ACR was listed as a class 2A substance by the International Agency for Research on Cancer (IARC) (Zhang and Zhang 2007). In 2002, the finding of ACR in various cooked foods and the mechanism of ACR formation through the Maillard reaction was reported (Mottram et al. 2002; Stadler et al. 2002). Current evidence suggests that exposure to ACR is associated with selective neurotoxicity in humans (LoPachin and Gavin 2012). Case reports suggested the major clinical features of human ACR intoxication are related to polyneuropathy, including ataxia, skeletal muscles weakness, and numbness of the extremities (Auld and Bedwell 1967), as well as damage of the central nervous system. More recently, experimental studies demonstrated that exposure to ACR-induced peripheral and central nerve fiber degeneration, which occurs first in the extremities of long and large nerve fibers (LoPachin et al. 2003). LoPachin and colleagues proposed that the nerve terminals were the primary site of ACR action, and that ACR-induced neurotoxicity was based on impaired synaptic transmission in peripheral nerves and the central nervous system due to ACR-induced formation of adducts with cysteine residues on specific proteins involved in synaptic transmission (LoPachin et al. 2003; LoPachin 2004; LoPachin and Gavin 2012). Their studies suggested that these changes ultimately lead to dysfunction and neuronal degeneration (LoPachin 2004).
On the other hand, the roles of glial cells and inflammatory signals in ACR-induced neurotoxicity remains elusive at this stage. Glial cells, such as astrocytes and microglia, play an important role in brain function, including neurotrophic support, transporter regulation, pathogen elimination, induction of neuronal differentiation, and modulation of the immune response (Anderson and Swanson 2000; Streit et al. 1988). When activated by injury or infection, glial cells are known to secrete various neurotoxic signals, such as reactive oxygen species (ROS) and proinflammatory mediators, such as cytokines (Li et al. 2014; Sloan and Barres 2014). Furthermore, glial cells play an important role in the onset and progression of neurotoxicity and various brain pathologies (Dheen et al. 2007). The neuroinflammatory response following CNS injury can be either harmful or paradoxically beneficial (Szalay et al. 2016; Ransohoff et al. 2015), but the role of inflammation in the progression of degeneration and regeneration following CNS trauma remains elusive (Mietto et al. 2015). IL-1β is secreted in the brain by activated astroglia and microglia, where it has a wide range of effects on immune function and coordination of various aspects of the acute phase response to trauma and infection (Murray et al. 2015; John et al. 2005). It is widely accepted that the inflammatory processes stimulated by IL-1β are harmful and can exacerbate the primary damage caused by CNS infections (Medel-Matus et al. 2014). Overexpression of IL-1β has been identified in various inflammatory and degenerative CNS conditions (Silva et al. 2015; Hopkins and Rothwell 1995). Although proinflammatory cytokines are thought to be important mediators of neuroinflammation, their role in the case of brain injury is unidentified.
We reported previously microglial activation and upregulation of proinflammatory cytokines, including IL-1b, in ACR-induced degeneration of monoaminergic axons both in in vivo and in vitro experiments (Zong et al. 2019). Following that study, we demonstrated that the deletion of IL-1β potentiated the ACR-induced increase in landing foot spread, which serves as a marker of motor dysfunction (Fergany et al. 2023). Additionally, IL-1β deletion exacerbated the ACR-induced decrease in the density of noradrenergic (NA) axons in the somatosensory cortex area. These neurological changes were accompanied by specific alterations in oxidative stress parameters. IL-1β deletion suppressed the ACR-induced increase in both total and oxidized glutathione levels. Furthermore, IL-1β deletion resulted in the suppression of ACR-induced upregulation of antioxidant genes, including Gpx1, Gpx4, and Gclc. Conversely, there was a downregulation of these antioxidant genes in IL-1β knockout (KO) mice compared to their wild-type counterparts. These findings emphasize the significant role of IL-1β in modulating motor dysfunction, axon density, and oxidative stress responses triggered by ACR exposure.
The present study is an extension to the above studies and involved transcriptome analysis to understand the molecular mechanism of the protective effect of proinflammatory cytokine IL-1β in ACR-induced neurotoxicity of mouse brain.
Materials and methods
Chemicals and preparation
Acrylamide was purchased from Sigma–Aldrich (lot #A9099, purity > 99%, St. Louis, MO). It was freshly prepared at the start of each week by dissolving in drinking water filtered through a G-10 ion exchange cartridge (Organo Co., Tokyo, Japan), stored at 4 °C and administered each day in autoclaved tubes by oral gavage.
Animal husbandry and experimental design
A total of 18 IL-1β-knockout mice (C57BL/6msSlc background purchased from SLC Japan, Inc., Hamamatsu, Japan) were produced and used in the study at 10 weeks of age. The IL-1β KO mice (Horai et al. 1998) were backcrossed C57BL/6msSlc having a congenicity of > 99.998 at the Institute of Medical Science, the University of Tokyo. At 6–8 weeks of age, the DNA was extracted from ear samples obtained from each mouse and analyzed by polymerase chain reaction (PCR) to confirm its genotype using primers (Lac Z GAGGTGCTGTTTCTGGTCTTCACC, IL-1β common CACATATCCAGCACTCTGCTTTCAG, IL-1β W TGGTCAGTGTGTGGGTTGCCTT). The PCR was conducted by a three-step cycle under conditions of 96 °C for 2 min followed by 35 cycles of 96 °C for 20 s, 59 °C for 30 s and 72 °C for 45 s. The amplified DNA samples were then run on a 2% agarose gel electrophoresis and visualized by a CCD camera (Fusion Solo S, Vilber Lourmat, Collegien, France). IL-1β KO mice (−/−) showed one band (600 bp) which confirmed that all the mice were homozygous recessive. Specific pathogen-free age matched male C57BL/6msSlc wild-type control mice (n = 18) were purchased from SLC Japan, Inc. (Hamamatsu) and acclimatized to the new environment for 1 week before the start of treatment or toxicity studies. All mice were initially housed in separate cages of 4–6 and had access to filtered drinking water and normal chow diet (Charles River Formular-1; 5LR1) ad libitum. They were housed in a controlled environment of temperature (23–25 °C), humidity (57–60%), and light (lights on 0800 h, off 2000 h). After the acclimatization period, the mouse was weighed first and then assigned at random to one of six groups, each consisting of 10 mice, which were exposed to acrylamide (0, 12.5 or 25 mg/kg). Groups 1 to 3 (wild-type mice) and groups 4–6 (IL-1 β KO mice) were exposed to acrylamide. Acrylamide was dissolved in drinking water filtered through G-10 ion exchange cartridge (Organo Co.) and administered by oral gavage. Mice of each group (n = 6 each) were housed six per cage for morphology and biochemical analysis and treated with the compounds every day of the week for 4 weeks. In the present study, 25 mg/kg was used as the highest exposure level for acrylamide based on the findings of previous studies in rats using 20 mg/kg body weight (Zong et al. 2019).
The study protocol and experimental design were approved by the animal experiment committee of the Tokyo University of Science (Experiment approval Number Y 21016) and strictly followed the guidelines of Tokyo University of Science on animal experiments in accordance with the Japanese act on welfare and management of animals.
Isolation of total mRNA
Total messenger RNA (mRNA) was isolated from the cerebral cortex (n = 6 per group) using the ReliaPrep™ RNA Tissue Miniprep System (Promega, Madison, WI) and the instructions provided by the manufacturer. The concentration of the extracted mRNA following elution with RNase-free water was measured using a NanoDrop 2000 spectrophotometer (Thermo Fisher Scientific, Waltham, MA). The quality of mRNA was determined by confirming that the A260/A280 ratio was ≥ 2.0 after measuring absorbance at 260 nm and 280 nm.
Preparation of bulk-RNA sequencing library
Transcriptome libraries were prepared from RNA samples harvested from the cerebral cortex of both the wild-type and IL-1β KO mice. PolyA RNAs were isolated using Dynabeads M-270 Streptavidin (Thermo Fisher Scientific) conjugated with biotin-3’ WTA-EcoP-dT25, according to the method described previously with some modifications (GSE110711) (Shichino et al. 2019; Aoki et al. 2021). To perform reverse transcription, beads were suspended in 10 μL of RT mix [5 × Superscript IV buffer (Thermo Fisher Scientific), 1 mM dNTP (Roche), 5 mM DTT (Thermo Fisher Scientific), 1 M betaine (Sigma), 6 mM MgCl2, 1 U/μL RNaseIn Plus Rnase Inhibitor (Promega, Madison, WI), and 10 U/μL Superscript IV (Thermo Fisher Scientific)], and then incubated for 5 min at 35 °C, 30 min at 42 °C, and immediately cooled on ice. The beads were washed once with B&W-T buffer [5 mM Tris–HCl (pH 8.0) (Nippon Gene, Tokyo), 1 M NaCl (Merck), 1 mM EDTA (Nippon Gene) and 0.05% Tween-20 (Merck)], and once with Tris–HCl (pH 8.0). To digest free-primer, beads were then suspended in 10 μL of Exo I mix [10 × Exo I buffer (New England Biolabs, Ipswich, MA), 2 U/μL Exonuclease I (New England Biolabs)], and incubated for 30 min at 37 °C and immediately cooled on ice. The beads were washed twice with B&W-T buffer, and once with Tris–HCl (pH 8.0). To add polyC tail, the beads were then suspended in 10 μL of polyC tailing mix [10 × Thermopol buffer (New England Biolabs), 2 mM dCTP (Roche), 0.1 mM ddCTP (GE Healthcare), 1 mM CoCl2 (Roche), RNaseH (Invitrogen), and 15 U/μL TdT enzyme (Roche)], and incubated for 30 min at 37 °C, followed by immediate cooling on ice. The beads were washed once with B&W–T buffer, and once with Tris–HCl (pH 8.0). To synthesize the second strand, the beads were suspended in 10 μL of 2nd strand mix [1 × KAPA Hifi Hotstart ReadyMix (KAPA Biosystems, Wilmington, MA), 0.4 μM of primer (illumina-i7-9G)], and the thermal cycling was performed under the following condition: 3 min at 95 °C, 20 s at 98 °C, 16 cycles of 1 min at 47 °C and 2 min at 72 °C, followed by 5 min at 72 °C, and hold at 4 °C. To amplify the total cDNA, 10 μL of the cDNA-containing beads were added with 15 μL of the first PCR mix [0.32 μM of primer (illumina-i7), 0.48 μM of primer (NH2-3’ WTA), and 1× KAPA Hifi Hotstart ReadyMix], and the thermal cycling was performed under the following condition: 3 min at 95 °C, 12 cycles of 20 s at 98 °C, 15 s at 65 °C, and 5 min at 72 °C, followed by 5 min at 72 °C, and hold at 4 °C. The first PCR products were purified by AmPure XP beads (Beckman-Coulter) at 0.6:1 ratio of reagents to sample and eluted with 25 μL of nuclease-free water. Then, 6.3 mL of the purified first PCR product was mixed with the 8.7 μL of the second PCR mix [0.4 μM of primers (illumina-i7, NH2-3’ WTA), and 1× KAPA Hifi Hotstart ReadyMix], and the thermal cycling was performed as follows: 3 min at 95 °C, 5 cycles of 20 s at 98 °C, 15 s at 65 °C, and 5 min at 72 °C, followed by 5 min at 72 °C, and hold at 4 °C. The second PCR products were purified by AmPure XP beads at 0.6:1 ratio of reagent to sample and eluted with 15 μL of 10 mM Tris–HCl (pH 8.0). Furthermore, 100 ng of the whole-transcriptome library was subjected to fragmentation/end-repair/A-tailing using NEBNext Ultra II FS DNA Library Prep Kit for Illumina (New England Biolabs) with some modifications. The thermal cycling was performed as follows: 7 min at 32 °C, 30 min at 65 °C, and hold at 4 °C. Then, 1.25 μL of 1.5 μM illumine adapter was used for adapter ligation. The ligated products were purified by double size selection with 0.4× → 0.7× (final 1.1×) AmPure XP beads and eluted with 10 μL of nuclease-free water. The barcoding PCR was performed with 22.5 µL of barcoding mix [7.5 μL of the resulted eluates, 1 μM primers (ILMN_[UDI]_i5 and ILMN_[UDI]_i7), and 1× NEBNext Ultra II Q5 (New England Biolabs)], and the thermal cycling was performed as follows: 30 s at 98 °C, 9 cycles of 10 s at 98 °C, and 75 s at 65 °C, followed by 5 min at 65 °C, and hold at 4 °C. The resultant products were purified twice by double size selection with 0.5× → 0.8× (final 1.3×) AmPure XP beads and elution with 12 μL of 10 mM Tris–HCl, pH 8.0. The size distribution of the amplified products was analyzed by the MultiNA system (Shimazu, Kyoto, Japan) at appropriate dilutions. Final transcriptome libraries, with lengths around 300 base pairs, were quantified using the KAPA Library Quantification Kit (KAPA Biosystems). The pooled libraries were sequenced by Illumina Novaseq 6000 sequencer (Illumina, San Diego, CA).
Analysis of bulk-RNA sequencing data
Adapter trimming and quality filtering of the sequencing data were performed by using Cutadpat-v2.10. The filtered reads were mapped to a reference RNA (GRCm38 release-101), using Bowtie2-2.4.2 (parameters: -p 2-L 16-very-sensitive-local-N 1-nofw-seed 656565-reorder) and the read numbers of each gene were counted. The transcriptome data were analyzed as described previously (Shichino et al. 2019). Briefly, between-sample normalization was performed against raw count data using the R 3.5.1. (https://cran.r-project.org/) and TCC package (EEE-E method) (Sun et al. 2013; Tang et al. 2015). Genes with the adjusted P < 0.05, fold change ≥ 2, and maximum expression ≥ 100 were identified as statistically significant DEGs. The raw data generated from the experiment have been deposited in the NCBI Gene Expression Omnibus (GEO, http://www.ncbi.nlm.nih.gov/geo), gene bank accession number (GSE211746). Co expressed gene modules among the DEGs were detected by using WGCNA package version 1.71 (Langfelder and Horvath 2008). Functional analysis of the gene module groups was performed using David software. Pathway enrichment analysis was performed on unique ACR-induced up- and down-regulated DEGs in wild-type and IL-1β KO mice in the cerebral cortex, using David software. Significantly enriched GO terms (Ashburner et al. 2000) (GO biological process, GO levels 3–8, version: 2021/5/1) and Kyoto Encyclopedia of Genes and Genomes (KEGG, version: 2020/8/5) pathway terms (Kanehisa and Goto 2000) in gene module groups were explored and grouped, and a term network was constructed based on the overlap of their elements using the default software setting. Leading terms within each group were defined as the most significantly enriched term in each group. DEGs were converted to Mouse Ensemble IDs (species: Mus musculus), which were used as the input gene list. The analyses included the selected canonical pathway databases: GO Biological process and KEGG. Differentially expressed genes in the mice cerebral cortex that were unique to wild-type and IL-1β KO mice treated with different doses of ACR (0, 12.5, 25 mg/kg) were identified for both upregulated and downregulated DEGs. Gene Ontology (GO) analysis was performed on unique up- and down-regulated DEGs using David software (https://david.ncifcrf.gov/). GO biological process terms were identified using a Bengimin Hoschet and a false discovery rate of 0.05 (Ashburner et al. 2000; Mi et al. 2017).
Functional protein association network
The protein network for each module was analyzed using STRING database website (https://string-db.org/) by inputting the list of genes into the STRING database, followed by calculating the network, visualizing the network and calculating the degree by cytoHubba plugin using Cytoscape version (3.9.1) software.
Results
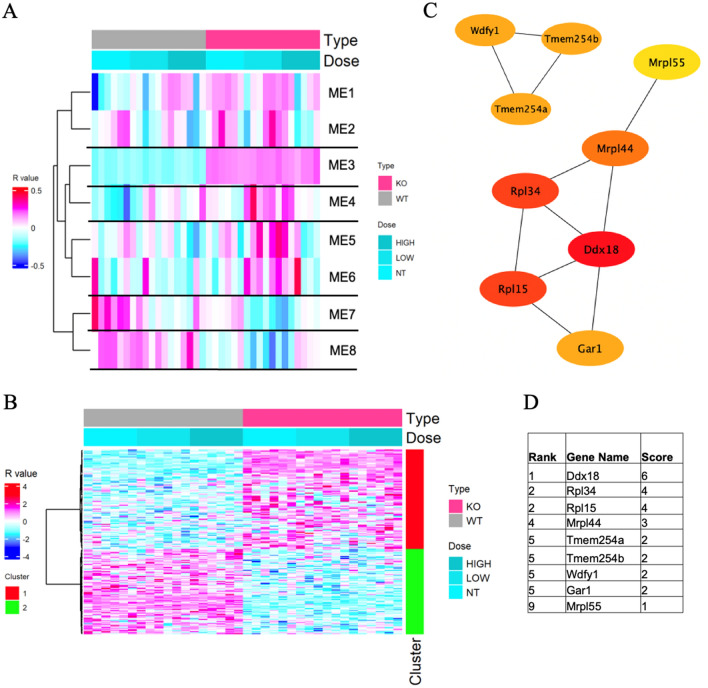
RNA sequence analysis was carried out to determine the effects of IL-1β deletion and exposure to ACR on the gene expression in the cerebral cortex. The analysis identified 2187 DEGs with adjusted P values < 0.05 (q value); fold change of ≥ 2 between at least two samples; and maximum expression of ≥ 100, compared with eight modules by WGCNA (Fig. 1A).
Fig. 1.
A Heatmap of co-expressed gene modules identified by the weight co-expressed network analysis of wild-type (WT) and IL-1ß KO mice. Columns: acrylamide exposure groups (0, 12.5, 25 mg/kg) for 28 days of both WT and IL-1ß KO mice. Rows: individual module eigengene. B Heatmap of module eigengene 3 (ME3, 184 genes) of the cerebral cortex of acrylamide-exposed WT and IL-1ß KO mice. Columns: acrylamide exposure groups at 0, 12.5, 25 mg/kg. Red cluster (1): upregulated genes, green cluster (2): downregulated genes in IL-1ß KO mice compared to WP mice. C Protein network analysis of ME3 module using STRING software. D Table shows the scores of the top proteins in the ME3 arranged from the highest score (top) to the lowest score (bottom) (color figure online)
Bulk RNA transcriptome analysis of the IL-1β KO mice brain showed increased expression of the IL-1b antisense strand (IL1bos, FC = 3.39) (Supplementary Table 1). In module eigengene 3 (ME3) (Fig. 1B), which provides comparison of the two genotypes (wild-type and IL-1β KO mice), overexpression was identified by David software analysis in 184 genes listed in the GO and KEGG. The analysis showed overexpression of the GO: 0005576-extracellular region (q = 0.0070) (Table 1), with significant upregulation of the SNORC (q = 2.05E-07), PFN1 (q = 2.81E−17), CRHBP (q = 6.21E−09), PARM1 (q = 0.002867) genes, and significant downregulation of the LY86 (q = 5.84E−27), MYOC (q = 5.77E−08) and NMI (q = 0.000248) genes (Table 2). Protein network analysis of module ME3 that included genes with a q value of < 0.05 showed the highest scores for Ddx18, RPL15, RPL34, Mrpl44 (Fig. 1C, D).
Table 1.
GO (biological process) and KEGG pathways for different modules of transcriptome analysis in wild-type and IL-1b KO mice exposed to ACR at 0, 12.5, or 25 mg/kg for 28 days by oral gavage
| Category | Term | Module | Count | p value | q value (p value)* | Genes |
|---|---|---|---|---|---|---|
| GOTERM_CC_DIRECT | GO: 0005576 ~ extracellular region | ME3 | 25 | 3.43E−05 | 0.007023595 | TNFAIP6, HMGB2, THBS2, ISM1, THBS4, FSTL5, CRHBP, PNP, ADAMTS13, DPP7, REG2, PTGDS, PAMR1, LAG3, PLA2G12A, MYOC, COL25A1, IL15, LY86, RNASE4, NMI, SNORC, PFN1, PAM, HBEGF |
| KEGG_PATHWAY | mmu05012: Parkinson disease | ME4 | 16 | 3.18E−05 | 0.007536264 | NDUFB8, NDUFA12, DUSP1, SDHB, MT-ND3, MT-ATP8, PSMA7, PSMB6, UBB, PSMB2, PSMB3, NDUFAB1, MT-CYTB, NDUFV2, CALM2, SLC39A3 |
| KEGG_PATHWAY | mmu05014: Amyotrophic lateral sclerosis | ME4 | 17 | 4.11E−04 | 0.039042011 | MAP2K3, NDUFB8, NDUFA12, DNAH7A, GPX8, SDHB, MT-ND3, MT-ATP8, PSMA7, PSMB6, PSMB2, PSMB3, NDUFAB1, CASP1, MT-CYTB, NDUFV2, NUP37 |
| KEGG_PATHWAY | mmu05016: Huntington disease | ME4 | 15 | 4.94E−04 | 0.039042011 | NDUFB8, NDUFA12, DNAH7A, GPX8, SDHB, MT-ND3, MT-ATP8, PSMA7, PSMB6, PSMB2, PSMB3, NDUFAB1, POLR2D, MT-CYTB, NDUFV2 |
| KEGG_PATHWAY | mmu05022: Pathways of neurodegeneration—multiple diseases | ME4 | 19 | 8.04E−04 | 0.04764275 | MAP2K3, NDUFB8, MAP2K2, NDUFA12, DNAH7A, GPX8, SDHB, HSD17B10, MT-ND3, MT-ATP8, PSMA7, PSMB6, UBB, PSMB2, PSMB3, NDUFAB1, MT-CYTB, NDUFV2, CALM2 |
| GOTERM_BP_DIRECT | GO: 0006366 ~ transcription from RNA polymerase II promoter | ME4 | 15 | 1.96E−05 | 0.034801066 | GTF2A2, SLC40A1, FOS, SCAF1, FOSL2, SNAPC5, NR4A1, AR, BCL6, POLR2D, FOSB, TAF9B, HMGN3, JUNB, BCL9L |
| KEGG_PATHWAY | mmu00190: Oxidative phosphorylation | ME7 | 21 | 1.34E−13 | 2.68E−11 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA4, NDUFA3, COX17, NDUFA1, UQCR11, NDUFC1, UQCR10, ATP5J2, NDUFB4C, UQCRQ, NDUFS6, NDUFS5, ATP5E, NDUFV3 |
| KEGG_PATHWAY | mmu04714: Thermogenesis | ME7 | 23 | 6.64E−11 | 4.85E−09 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA4, NDUFA3, COX17, NDUFA1, UQCR11, NDUFC1, UQCR10, ATP5J2, NDUFAF8, NDUFB4C, UQCRQ, NDUFS6, NDUFS5, ATP5E, NDUFV3, COX20 |
| KEGG_PATHWAY | mmu04723: Retrograde endocannabinoid signaling | ME7 | 19 | 7.28E−11 | 4.85E−09 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, SLC32A1, NDUFB6, NDUFA4, NDUFA3, NDUFA1, NDUFC1, GNG11, GNG13, GNGT2, NDUFB4C, NDUFS6, NDUFS5, NDUFV3 |
| KEGG_PATHWAY | mmu05208: Chemical carcinogenesis—reactive oxygen species | ME7 | 21 | 1.41E−09 | 7.05E−08 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA4, NDUFA3, NDUFA1, CYBA, UQCR11, NDUFC1, UQCR10, VEGFA, NDUFB4C, UQCRQ, NDUFS6, NDUFS5, ATP5E, NDUFV3 |
| KEGG_PATHWAY | mmu05415: Diabetic cardiomyopathy | ME7 | 20 | 3.78E−09 | 1.51E−07 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA4, NDUFA3, NDUFA1, CYBA, UQCR11, NDUFC1, UQCR10, NDUFB4C, UQCRQ, NDUFS6, NDUFS5, ATP5E, NDUFV3 |
| KEGG_PATHWAY | mmu04932: Non-alcoholic fatty liver disease | ME7 | 17 | 1.09E−08 | 3.64E−07 | NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA4, NDUFA3, NDUFA1, UQCR11, NDUFC1, UQCR10, NDUFB4C, UQCRQ, NDUFS6, NDUFS5, NDUFV3 |
| KEGG_PATHWAY | mmu05020: Prion disease | ME7 | 20 | 1.83E−07 | 5.22E−06 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA4, NDUFA3, NDUFA1, CYBA, UQCR11, NDUFC1, UQCR10, NDUFB4C, UQCRQ, NDUFS6, NDUFS5, ATP5E, NDUFV3 |
| KEGG_PATHWAY | mmu05016: Huntington disease | ME7 | 21 | 2.57E−07 | 6.43E−06 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA4, NDUFA3, NDUFA1, UQCR11, NDUFC1, UQCR10, NDUFB4C, UQCRQ, NDUFS6, NDUFS5, ATP5E, NDUFV3, POLR2J, POLR2L |
| KEGG_PATHWAY | mmu05012: Parkinson disease | ME7 | 19 | 7.01E−07 | 1.56E−05 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA4, NDUFA3, NDUFA1, UQCR11, NDUFC1, UQCR10, NDUFB4C, UQCRQ, NDUFS6, NDUFS5, ATP5E, NDUFV3 |
| KEGG_PATHWAY | mmu05014: Amyotrophic lateral sclerosis | ME7 | 21 | 5.86E−06 | 1.17E−04 | MT-ND6, RANBP2, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA4, NDUFA3, NDUFA1, UQCR11, NDUFC1, UQCR10, NDUFB4C, UQCRQ, NDUFS6, NDUFS5, ATP5E, NOS1, NDUFV3 |
| KEGG_PATHWAY | mmu05010: Alzheimer disease | ME7 | 21 | 1.02E−05 | 1.86E−04 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, CHRM1, NDUFA5, NDUFB6, NDUFA4, NDUFA3, NDUFA1, UQCR11, NDUFC1, UQCR10, NDUFB4C, UQCRQ, NDUFS6, NDUFS5, ATP5E, NOS1, NDUFV3 |
| KEGG_PATHWAY | mmu05022: Pathways of neurodegeneration—multiple diseases | ME7 | 22 | 6.42E−05 | 0.001069333 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, CHRM1, NDUFA5, NDUFB6, NDUFA4, NDUFA3, NDUFA1, UQCR11, NDUFC1, UQCR10, PDYN, NDUFB4C, UQCRQ, NDUFS6, NDUFS5, ATP5E, NOS1, NDUFV3 |
| GOTERM_CC_DIRECT | GO: 0070469 ~ respiratory chain | ME7 | 17 | 1.11E−14 | 4.46E−12 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA4, NDUFA3, NDUFA1, UQCR11, NDUFC1, UQCR10, UQCRQ, NDUFS6, NDUFS5, NDUFV3 |
| GOTERM_CC_DIRECT | GO: 0005747 ~ mitochondrial respiratory chain complex I | ME7 | 15 | 2.74E−13 | 5.50E−11 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA4, NDUFA3, NDUFA1, NDUFC1, NDUFB4C, NDUFS6, NDUFS5, NDUFV3 |
| GOTERM_CC_DIRECT | GO: 0005743 ~ mitochondrial inner membrane | ME7 | 35 | 1.18E−10 | 1.57E−08 | MT-ND6, NDUFA13, NDUFB7, NDUFB6, MRPS33, UQCR11, MRPL14, UQCR10, MRPL33, ATP5E, ROMO1, NDUFV3, CHCHD1, DNAJC19, TIMM8B, MRPS28, NDUFA7, NDUFA6, MRPS24, NDUFA5, PET100, UQCC2, NDUFA4, NDUFA3, NDUFA1, MRPS21, NDUFC1, MRPL23, ATP5J2, MRPS18C, TMEM256, UQCRQ, NDUFS6, NDUFS5, COX20 |
| GOTERM_CC_DIRECT | GO: 0005739 ~ mitochondrion | ME7 | 64 | 1.31E−06 | 1.31E−04 | MT-ND6, NDUFA13, HJURP, CISD3, MRPL33, GMPPB, NOS1, SERAC1, CHCHD1, DLGAP5, TMEM8B, MRPS28, MRPS24, ATPIF1, MRPS21, CYBA, NDUFC1, ATP5J2, MRPS18C, RPUSD4, QTRT2, NDUFS6, NDUFS5, SDHAF4, FXN, FCOR, NDUFB7, NDUFB6, MRPS33, COX17, CEBPZOS, IBA57, UQCR11, MRPL14, UQCR10, HIGD1B, NT5C, NDUFB4C, ATP5E, MTHFSL, ROMO1, NDUFV3, PPARGC1B, DNAJC19, EEFSEC, RANBP2, TIMM8B, NDUFA7, NDUFA6, PET100, NDUFA5, UQCC2, NDUFA4, NDUFA3, TXNRD1, NDUFA1, MTHFS, MRPL23, LYRM2, NDUFAF8, UQCRQ, FMC1, ATP5MPL, COX20 |
| GOTERM_CC_DIRECT | GO: 0005840 ~ ribosome | ME7 | 14 | 6.09E−05 | 0.004886691 | MRPS28, RPS4L, MRPS24, MRPS33, MRPS21, MRPL14, MRPL23, MRPL33, MRPS18C, RPS27, RPS19, RPL35, RPS11, CHCHD1 |
| GOTERM_CC_DIRECT | GO: 0005763 ~ mitochondrial small ribosomal subunit | ME7 | 6 | 3.80E−04 | 0.025389075 | MRPS28, MRPS24, MRPS33, MRPS21, CHCHD1, MRPS18C |
| GOTERM_MF_DIRECT | GO: 0003735 ~ structural constituent of ribosome | ME7 | 14 | 2.44E−05 | 0.012610695 | NDUFA7, RPS4L, MRPS24, MRPS21, MRPL14, MRPL23, MRPL33, MRPS18C, RPS27, RPS19, RPS18-PS5, RPS27RT, RPL35, RPS11 |
| GOTERM_BP_DIRECT | GO: 0042776 ~ mitochondrial ATP synthesis coupled proton transport | ME7 | 15 | 2.78E−12 | 4.88E−09 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA3, NDUFA1, NDUFC1, ATP5J2, NDUFS6, NDUFS5, ATP5E, NDUFV3 |
| GOTERM_BP_DIRECT | GO: 0009060 ~ aerobic respiration | ME7 | 15 | 1.88E−11 | 1.64E−08 | MT-ND6, NDUFA13, NDUFA7, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA3, NDUFA1, NDUFC1, UQCR10, NDUFS6, NDUFS5, NDUFV3, FXN |
| GOTERM_BP_DIRECT | GO: 0032981 ~ mitochondrial respiratory chain complex I assembly | ME7 | 13 | 4.72E−10 | 2.76E−07 | MT-ND6, NDUFA13, NDUFB7, NDUFA6, NDUFA5, NDUFB6, NDUFA3, NDUFA1, NDUFC1, NDUFAF8, NDUFB4C, NDUFS6, NDUFS5 |
| GOTERM_BP_DIRECT | GO: 0032543 ~ mitochondrial translation | ME7 | 10 | 3.41E−05 | 0.014945752 | MRPS28, NDUFA7, MRPS24, MRPS33, MRPS21, MRPL14, MRPL23, CHCHD1, MRPL33, MRPS18C |
| KEGG_PATHWAY | mmu03010: Ribosome | ME8 | 23 | 3.38E−26 | 1.93E−24 | RPL30, RPL10, RPLP1, RPL11, RPL22, RPSA, N-R5S121, N-R5S143, N-R5S113, N-R5S111, N-R5S144, N-R5S128, RPS3A1, RPL27A, GM25018, N-R5S138, RPS20, RPS2, RPS27A, RPL18, RPS10, RPS13, RPS23 |
| KEGG_PATHWAY | mmu05171: Coronavirus disease—COVID-19 | ME8 | 15 | 1.09E−11 | 3.10E−10 | RPL30, RPL10, RPLP1, RPL11, RPL22, RPSA, RPS3A1, RPL27A, RPS20, RPS2, RPS27A, RPL18, RPS10, RPS13, RPS23 |
| KEGG_PATHWAY | mmu03008: Ribosome biogenesis in eukaryotes | ME8 | 8 | 1.94E−06 | 3.68E−05 | N-R5S113, N-R5S111, N-R5S144, N-R5S128, N-R5S138, GM25018, N-R5S121, N-R5S143 |
| GOTERM_CC_DIRECT | GO: 0022626 ~ cytosolic ribosome | ME8 | 15 | 1.43E−20 | 2.26E−18 | RPL30, RPL10, RPLP1, RPL11, RPL22, RPSA, RPS3A1, RPL27A, RPS20, RPS2, RPS27A, RPL18, RPS10, RPS13, RPS23 |
| GOTERM_CC_DIRECT | GO: 0005840 ~ ribosome | ME8 | 15 | 4.60E−15 | 3.63E−13 | RPL30, RPL10, RPLP1, RPL11, RPL22, RPSA, RPS3A1, RPL27A, RPS20, RPS2, RPS27A, RPL18, RPS10, RPS13, RPS23 |
| GOTERM_CC_DIRECT | GO: 0022627 ~ cytosolic small ribosomal subunit | ME8 | 9 | 4.26E−12 | 2.25E−10 | RPS3A1, GM49804, RPSA, RPS20, RPS2, RPS27A, RPS10, RPS13, RPS23 |
| GOTERM_CC_DIRECT | GO: 0045202 ~ synapse | ME8 | 21 | 1.00E−10 | 3.95E−09 | RPL30, PTPRN2, RPL10, RPLP1, RPL11, RPL22, HSPB1, RPSA, RPS3A1, RPL27A, EEF1A2, RPS20, RPS2, DLGAP3, RPS27A, RPL18, RPS10, RPS13, BCAS1, YWHAH, RPS23 |
| GOTERM_CC_DIRECT | GO: 0098794 ~ postsynapse | ME8 | 13 | 3.10E−10 | 9.81E−09 | RPL30, RPL10, RPLP1, RPL22, RPSA, FXR2, RPS3A1, RPL27A, RPS20, RPS2, RPS27A, RPS10, RPS23 |
| GOTERM_CC_DIRECT | GO: 0022625 ~ cytosolic large ribosomal subunit | ME8 | 8 | 4.12E−09 | 1.08E−07 | RPL30, RPL10, RPL27A, RPLP1, RPL11, RPL22, RPL18, RPL9-PS6 |
| GOTERM_CC_DIRECT | GO: 0015935 ~ small ribosomal subunit | ME8 | 5 | 1.78E−06 | 4.02E−05 | RPS3A1, RPSA, RPS20, RPS2, RPS23 |
| GOTERM_CC_DIRECT | GO: 0005829 ~ cytosol | ME8 | 31 | 2.54E−05 | 5.01E−04 | RPL30, RPL10, RPLP1, URM1, RPL11, CXXC1, SEC14L2, RGS5, FXR2, KLC2, COTL1, RPS2, RPS27A, RPL18, RPS10, RPS13, WDTC1, BCAS1, YWHAH, CAP1, DAPK3, RPL22, IRGM1, RPSA, MT2, MED27, FMNL1, RPS3A1, RPL27A, RPS20, RPS23 |
| GOTERM_CC_DIRECT | GO: 0098793 ~ presynapse | ME8 | 8 | 5.05E−05 | 8.70E−04 | FXR2, PTPRN2, RPL10, RPL27A, RPL22, RPS27A, RPS10, YWHAH |
| GOTERM_CC_DIRECT | GO: 0005737 ~ cytoplasm | ME8 | 43 | 5.51E−05 | 8.70E−04 | CEP57, MACF1, RPL30, RPL10, RPLP1, URM1, RPL11, HSPB1, HSD17B11, PPP1R18, SEC14L2, RGS5, FXR2, KLC2, CSRP1, NPHP1, COTL1, RPS2, RPS27A, RPL18, RPS10, TSPOAP1, RPS13, WDTC1, BCAS1, YWHAH, CAP1, PTPRN2, TAF10, DAPK3, RPL22, HAUS3, RPSA, MT2, TPPP3, FMNL1, RPS3A1, RPL27A, ID1, EEF1A2, RPS20, SFI1, RPS23 |
| GOTERM_CC_DIRECT | GO: 0042788 ~ polysomal ribosome | ME8 | 4 | 2.33E−04 | 0.003340004 | RPL30, RPL11, RPL18, RPS23 |
| GOTERM_MF_DIRECT | GO: 0003735 ~ structural constituent of ribosome | ME8 | 18 | 2.91E−19 | 4.63E−17 | RPL30, RPL10, RPLP1, GM49804, RPL11, RPL22, RPSA, RPL9-PS6, RPS3A1, RPL27A, RPS20, RPS2, GM49711, RPS27A, RPL18, RPS10, RPS13, RPS23 |
| GOTERM_BP_DIRECT | GO: 0002181 ~ cytoplasmic translation | ME8 | 15 | 2.79E−20 | 1.21E−17 | RPL30, RPLP1, RPL11, RPL22, RPSA, RPL9-PS6, RPS3A1, RPL27A, RPS20, RPS2, RPS27A, RPL18, RPS10, RPS13, RPS23 |
| GOTERM_BP_DIRECT | GO: 0006412 ~ translation | ME8 | 15 | 1.14E−12 | 2.48E−10 | RPL10, RPL11, RPL22, RPSA, LARS2, RPS3A1, RPL27A, EEF1A2, RPS20, RPS2, GM49711, RPS27A, RPL18, RPS13, RPS23 |
*Corrected by the Benjamini–Hochberg method
The analysis was performed by DAVID software
Table 2.
GO (biological process) over representation analysis of ME3 module and list of involved genes in wild-type mice and IL-1b KO mice exposed to acrylamide at 0, 12.5, 25 mg/kg for 28 days by oral gavage
| Gene name | Regulation | q value | Fold change | Wild-type (mg/kg) (mean ± SD) | IL-1b KO (mg/kg) (mean ± SD) | GO/KEGG term | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 12.5 | 25 | 0 | 12.5 | 25 | |||||
| SNORC (Secondary Ossification Center Associated Regulator of Chondrocyte Maturation) | Upregulated | 2.05E−07 | 4.608 | 2.93 ± 0.974 | 2.63 ± 2.45 | 4.41 ± 2.19 | 8.51 ± 4.0 | 13 ± 3.8 | 12.52 ± 4.94 | GO: 0005576 ~ extracellular region |
| PFN1 (Profilin 1) | Upregulated | 2.81E−17 | 1.788 | 384.52 ± 46.48 | 486.09 ± 43.51 | 442.1 ± 41.3 | 610.58 ± 47.46 | 687.7 ± 48.8 | 683 ± 81.33 | |
| CRHBP (Corticotropin-releasing hormone binding protein) | Upregulated | 6.21E−09 | 1.572 | 203.34 ± 21.6 | 219.6 ± 15.6 | 246.9 ± 22.2 | 301.7 ± 21.3 | 319.6 ± 37.0 | 276.5 ± 18.14 | |
| PAMR1 (Peptidase domain containing associated with muscle regeneration) | Upregulated | 0.002867 | 1.539 | 74.4 ± 12.9 | 88.2 ± 6.97 | 93 ± 8.55 | 100.8 ± 14.1 | 114.6 ± 11.7 | 104.18 ± 21.96 | |
| LY86 (Lymphocyte antigen 86) | Downregulated | 5.84E−27 | 0.435 | 95 ± 17.4 | 110.4 ± 20.3 | 120.4 ± 13.1 | 43.74 ± 8.0 | 41.4 ± 7.7 | 50.1 ± 7 | |
| MYOC (Myocilin) | Downregulated | 5.77E−08 | 0.546 | 36.13 ± 6.4 | 52.45 ± 12.2 | 45.82 ± 8.41 | 25.5 ± 12.88 | 19.73 ± 7.54 | 24.84 ± 15.19 | |
| NMI (N-myc-interactor | Downregulated | 0.000248 | 0.559 | 36.05 ± 8.43 | 37.41 ± 5.39 | 42.85 ± 6.73 | 26.93 ± 6.38 | 27.57 ± 16.61 | 20.15 ± 5.64 | |
DAVID software was used for analysis. Data of normalized values for gene expression are mean ± SD, n = 6. All P value for gene expression were adjusted using Benjamini–Hochberg method and expressed as q values. Fold change represents the ratio of the mean value of the group to the mean of the 0 mg/kg wild-type group when the absolute value of logarithm of the ratio is the maximum
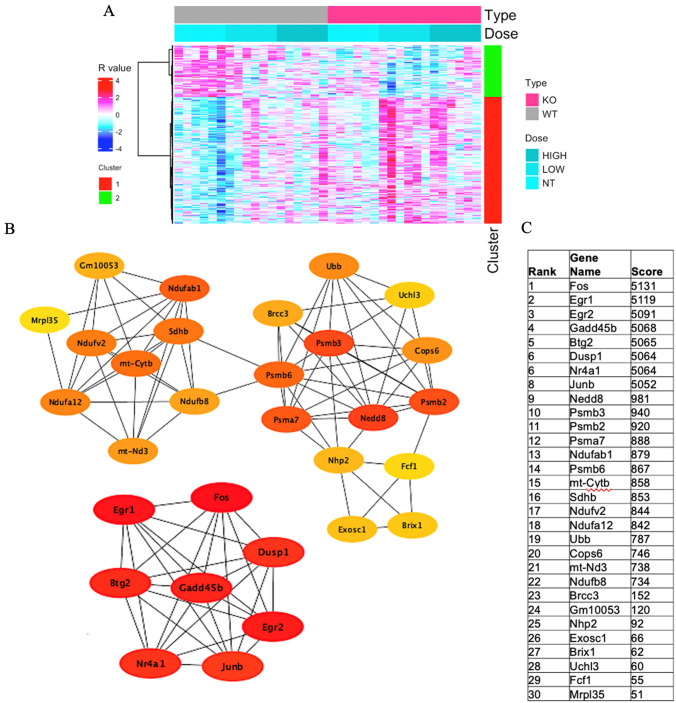
Similar analysis in module eigengene 4 (ME4) (Fig. 2A), which provides assessment of ACR effect on gene expression both in the wild-type and IL-1β KO, showed overexpression of 417 genes. The analysis showed that the KEGG mmu05012: Parkinson disease (q = 0.007), KEGG mmu05014: amyotrophic lateral sclerosis (q = 0.039), KEGG mmu05016: Huntington disease (q = 0.039), KEGG mmu05022: Pathways of neurodegeneration—multiple diseases (q = 0.047) and GO-BP: 0006366 ~ transcription from RNA polymerase II promoter (q = 0.034) were significantly expressed in this module (Table 1). The following genes were upregulated significantly: NDUFB8 (q = 3.20E−06), MT-ATP8 (q = 6.33E−10), PSMB6 (q = 4.48E−07), NDUFA12 (8.91E−06), DNAH7A (0.072927), PSMB3 (q = 1.76E−07), and MT-CYTB (q = 8.06E−06), while the following genes were significantly downregulated: DUSP1 (q = 0.0002670), MT-ND3 (q = 0.013479), and SLC39A3 (q = 0.044957) (Table 3).
Fig. 2.
A Heatmap of module eigengene 4 (ME4, 417 genes) of the cerebral cortex of acrylamide-exposed WT and IL-1ß KO mice. Columns: exposure groups (0, 12.5, 25 mg/kg). Red cluster (1): upregulated genes, green cluster (2): downregulated genes. B Protein network analysis of ME4 module using STRING software. C Table shows the scores of the top proteins in the ME4 arranged from the highest score (top) to the lowest score (bottom) (color figure online)
Table 3.
GO (biological process) and KEGG pathway over representation analysis of ME4 module and list of involved genes in acrylamide-exposed wild-type mice and IL-1b KO mice groups at 0, 12.5, 25 mg/kg for 28 days by oral gavage
| Gene name | Regulation | q value | Fold change | Wild-type (mg/kg) (mean ± SD) | IL-1b KO (mg/kg) (mean ± SD) | GO/KEGG term | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 12.5 | 25 | 0 | 12.5 | 25 | |||||
| NDUFB8 | Upregulated | 3.20E−06 | 1.577 | 3394 ± 467 | 4460 ± 591 | 4465 ± 468 | 4161 ± 316 | 5355 ± 478 | 4890 ± 1132 | KEGG-mmu05012: PD, KEGG-mmu05014: ALS, KEGG-mmu05016: Huntington disease, KEGGmmu05022: Pathways of neurodegeneration—multiple diseases |
| MT-ATP8 | Upregulated | 6.33E−10 | 1.757 | 62,983 ± 13,582 | 755,528 ± 8682 | 80,676 ± 13,604 | 84,387 ± 9436 | 110,711 ± 14,621 | 105,250 ± 16,832 | KEGG-mmu05012: PD, KEGG-mmu05014: ALS, KEGG-mmu05016: Huntington disease, KEGGmmu05022: Pathways of neurodegeneration—multiple diseases |
| PSMB6 | Upregulated | 4.48E−07 | 1.588 | 1639 ± 147 | 2220 ± 281 | 2230 ± 173 | 1980 ± 148 | 2603 ± 230 | 2340 ± 518 | KEGG-mmu05012: PD, KEGG-mmu05014: ALS, KEGG-mmu05016: Huntington disease, KEGG-mmu05022: Pathways of neurodegeneration—multiple diseases |
| NDUFA12 | Upregulated | 8.91E−06 | 1.558 | 2240 ± 283 | 2764 ± 330 | 2805 ± 300 | 2706 ± 186 | 3491 ± 493 | 3141 ± 740 | KEGG-mmu05012: PD, KEGG-mmu05014: ALS |
| DNAH7A | Upregulated | 0.072927 | 1.571 | 35.30 ± 6.7 | 49 ± 10 | 46 ± 6.9 | 50 ± 9.3 | 56 ± 6.4 | 53 ± 13 | KEGG-mmu05012: PD, KEGG-mmu05014: ALS |
| PSMB3 | Upregulated | 1.76E−07 | 1.559 | 736 ± 62.8 | 1009 ± 98 | 974 ± 107 | 869 ± 51 | 1148 ± 177 | 1081 ± 162 | KEGG-mmu05014: ALS, KEGG-mmu05016: Huntington disease, KEGGmmu05022: Pathways of neurodegeneration—multiple diseases |
| MT-CYTB | Upregulated | 8.06E−06 | 1.526 | 36,367 ± 5894 | 40,408 ± 2631 | 443,691 ± 10,266 | 48,664 ± 4571 | 555,194 ± 6567 | 51,310 ± 7948 | KEGG-mmu05012: PD |
| DUSP1 | Downregulated | 0.000267 | 0.518 | 110 ± 29 | 106 ± 31 | 76 ± 30 | 57 ± 22 | 80 ± 24 | 80 ± 36 | KEGG-mmu05012: PD |
| MT-ND3 | Downregulated | 0.013479 | 0.699 | 2942 ± 300 | 2681 ± 501 | 2569 ± 620 | 2836 ± 369 | 2059 ± 675 | 26,371 ± 508 | KEGG-mmu05012: PD, KEGG-mmu05014: ALS, KEGG-mmu05016: Huntington disease, KEGG-mmu05022: Pathways of neurodegeneration—multiple diseases |
| SLC39A3 | Downregulated | 0.044957 | 0.709 | 104 ± 18 | 89 ± 17 | 74 ± 14 | 76 ± 12 | 81 ± 8 | 83 ± 5.8 | KEGG-mmu05012: PD |
DAVID software was used for the analysis. Data of normalized values for gene expression are mean ± SD, n = 6. All P value for the gene expression were adjusted using Benjamini–Hochberg method and expressed as q values. Fold change represents the ratio of the mean value of the group to the mean of the 0 mg/kg wild-type when the absolute value of the logarithm of the ratio is the maximum
PD Parkinson disease, ALS amyotrophic lateral sclerosis, NDUFB8 NADH: ubiquinone oxidoreductase subunit B8, MT-ATP8 mitochondrially encoded ATP synthase membrane subunit 8, PSMB6 proteasome 20S subunit beta 6, NDUFA12 NADH: ubiquinone oxidoreductase subunit A12, DNAH7A dynein, axonemal, heavy chain 7A, PSMB3 proteasome subunit beta type-3, MT-CYTB mitochondrially encoded cytochrome B, DUSP1 dual specificity phosphatase 1, MT-ND3 mitochondrially encoded NADH: ubiquinone oxidoreductase core subunit 3, SLC39A3 solute carrier family 39 member 3
Protein network analysis of ME4 of genes with q value < 0.05 showed involvement of different proteins that are highly expressed and involved in cell proliferation, such as Fos and Btg2, Egr1 and Egr2, and Nr4a proteins involved in memory and learning. Other groups of proteins also showed high scores, including proteasomal protein Psmb2, Psmb3, Psmb6, and Psma7. Mitochondrial proteins Nudfab1, Nudfa12, Nudfv2, mt-Cytb, and Sdhb also showed interaction, indicating the involvement of oxidative stress (Fig. 2B, C).
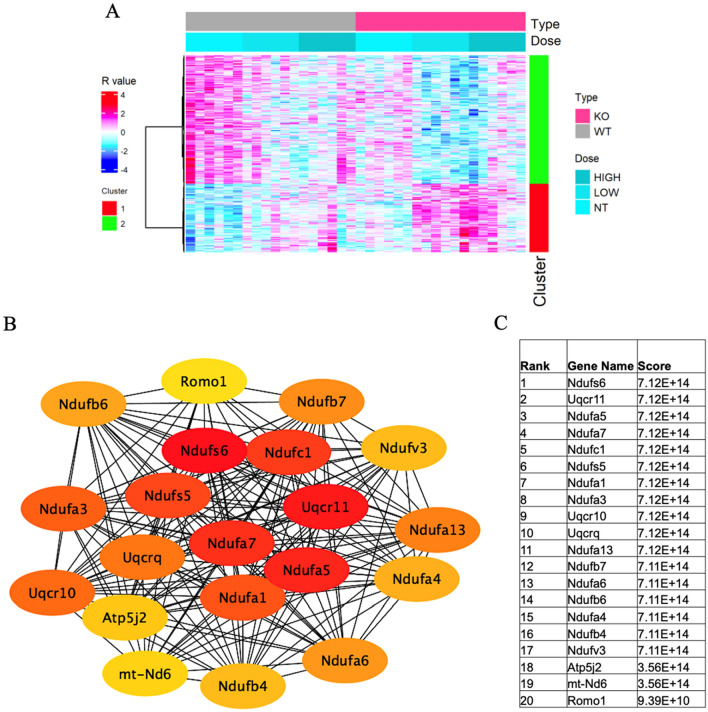
Similar analysis of module eigengene 7 (ME7) (Fig. 3A) showed high expression of 578 genes. Specifically, the analysis identified overexpression of KEGG mmu00190: Oxidative phosphorylation (q = 2.68E−11), KEGG mmu04714: Thermogenesis (q = 4.85E−09), KEGG mmu04723: Retrograde endocannabinoid signaling (q = 4.85E−09), KEGG mmu05208: Chemical carcinogenesis-reactive oxygen species (q = 7.05E−08), KEGG mmu05415: Diabetic cardiomyopathy (q = 1.51E−07), KEGG mmu05020: Prion disease (q = 5.22E−06), KEGG mmu05016: Huntington disease (q = 6.43E−06), KEGG mmu05012: Parkinson disease (q = 1.56E−05), KEGG mmu05014: Amyotrophic lateral sclerosis (q = 1.17E−04), KEGG mmu05010: Alzheimer disease (q = 1.86E−04), KEGG mmu05022: Pathways of neurodegeneration-multiple diseases (q = 0.001), KEGG mmu04932: Non-alcoholic fatty liver disease (q = 3.64E−07), GO-CC: 0070469-respiratory chain (q = 4.46E−12), GO-CC: 0005747-mitochondrial respiratory chain complex I (q = 5.50E−11), GO-CC O: 0005743-mitochondrial inner membrane (q = 1.57E−08), GO-CC: 0005739-mitochondrion (q = 1.31E−04), GO-CC: 0005840-ribosome (q = 0.004), GO-CC: 0005763-mitochondrial small ribosomal subunit (q = 0.025), GO-MF: 0003735-structural constituent of ribosome (q = 0.0126), GO-BP: 0042776-mitochondrial ATP synthesis coupled proton transport (q = 4.88E−09), GO-BP: 0009060-aerobic respiration (q = 1.64E−08), GO-BP: 0032981-mitochondrial respiratory chain complex I assembly (q = 2.76E−07), and GO-BP: 0032543-mitochondrial translation (q = 0.014) (Table 1).
Fig. 3.
A Heatmap of module eigengene 4 (ME7, 578 genes) of the cerebral cortex of acrylamide-exposed WT and IL-1ß KO mice. Columns: exposure groups (0, 12.5, 25 mg/kg). Red cluster (1): upregulated genes, green cluster (2): downregulated genes. B Protein network analysis of ME7 module using STRING software. C Table shows the scores of top proteins in the ME7 arranged from the highest score (top) to the lowest score (bottom) (color figure online)
The following genes showed significant upregulation in the ME7 module: CEBPZOS (q = 1.10E−22), NDUFS6 (q = 1.48E−14), SDHAF4 (q = 6.04E−10), NDUFA13 (q = 5.93E−11), NDUFB7 (q = 2.27E−10), NDUFA3 (q = 1.32E−09), MRPL14 (q = 5.46E−10), CYBA (q = 0.001343), MRPL33 (q = 2.10E−06), RPL35 (q = 0.000127), MRPS33 (q = 1.63E−05), MRPS21 (q = 2.32E−06), NDUFS5 (q = 3.84E−06), and MRPS28 (3.84E−05). On the other hand, significant downregulation of RPS4L (q = 4.88E−05) and MT-ND6 (q = 5.76E−15) genes was noted (Table 4). Protein network analysis of the ME7 module showed the association of multiple mitochondrial proteins, including Ndufs6, uqcr11, Ndufa5, Ndufa7, Ndufc1, Ndufs5, Ndufa1, Ndufa3, Uqrc10, Uqcrq, Ndufa13, Ndufb7, Ndufa6, Ndufb6, Ndufa4, and Ndufv3, with high scores, indicating possible involvement of these proteins in ACR-induced oxidative stress and subsequent neurotoxicity (Fig. 3B, C).
Table 4.
GO (biological process) and KEGG pathway over representation analysis of ME7 module and list of involved genes in wild-type and IL-1b KO mice exposed to acrylamide at 0, 12.5, 25 mg/kg for 28 days by oral gavage
| Gene | Regulation | q value | Fold change | Wild type (mg/kg) (mean ± SD) | IL-1b KO (mg/kg) (mean ± SD) | GO/KEGG term | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 12.5 | 25 | 0 | 12.5 | 25 | |||||
| CEBPZOS | Upregulated | 1.10E−22 | 2.409 | 666 ± 78 | 896.93 ± 116 | 892 ± 89 | 787 ± 51 | 1606 ± 199 | 1291 ± 471 | GO-CC: 0005739 ~ mitochondrion |
| NDUFS6 | Upregulated | 1.48E E−14 | 1.874 | 14,924 ± 131 | 1923 ± 157 | 1936 ± 326 | 2134 ± 111 | 2797 ± 334 | 2591 ± 490 | KEGG-mmu00190: Oxidative phosphorylation, mmu04714: Thermogenesis, mmu04723: Retrograde endocannabinoid signaling, mmu05208: Chemical carcinogenesis-ROS, mmu05415: Diabetic cardiomyopathy, mmu05020: Prion disease, mmu05016: Huntington disease, mmu05012: PD, mmu05014: ALS, mmu05010: AD, mmu05022: Pathways of neurodegeneration—multiple diseases, mmu04932: Non-alcoholic fatty liver disease, GO-CC GO: 0070469 ~ respiratory chain, GO: 0005747 ~ mitochondrial respiratory chain complex I,GO: 0005743 ~ mitochondrial inner membrane, GO: 0005739 ~ mitochondrion, GO-BP: 0042776 ~ mitochondrial ATP synthesis coupled proton transport, GO-BP: 0009060 ~ aerobic respiration, GO-BP: 0032981 ~ mitochondrial respiratory chain complex I assembly |
| SDHAF4 | Upregulated | 6.04E E−10 | 1.768 | 927 ± 101 | 1354 ± 203 | 1373 ± 217 | 1173 ± 91 | 1639 ± 136 | 1469 ± 362 | GO-CC: 0005739 ~ mitochondrion |
| NDUFA13 | Upregulated | 5.93E E−11 | 1.747 | 2873 ± 273 | 3651 ± 480 | 3699 ± 426 | 3552 ± 328 | 5019 ± 591 | 4536 ± 877 | KEGG-mmu00190: Oxidative phosphorylation, mmu04714: Thermogenesis, mmu04723: Retrograde endocannabinoid signaling, mmu05208: Chemical carcinogenesis—ROS, mmu05415: Diabetic cardiomyopathy, mmu05020: Prion disease, mmu05016: Huntington disease, mmu05012: PD, mmu05014: ALS, mmu05010: AD, mmu05022: Pathways of neurodegeneration—multiple diseases, mmu04932: Non-alcoholic fatty liver disease, GO-CC GO: 0070469 ~ respiratory chain, GO: 0005747 ~ mitochondrial respiratory chain complex I,GO: 0005743 ~ mitochondrial inner membrane, GO: 0005739 ~ mitochondrion, GO-BP: 0042776 ~ mitochondrial ATP synthesis coupled proton transport, GO-BP: 0009060 ~ aerobic respiration, GO-BP: 0032981 ~ mitochondrial respiratory chain complex I assembly |
| NDUFB7 | Upregulated | 2.27E E−10 | 1.745 | 1376 ± 149 | 18,855 ± 253 | 1816 ± 156 | 1756 ± 76 | 2403 ± 256 | 2073 ± 322 | KEGG-mmu00190: Oxidative phosphorylation, mmu04714: Thermogenesis, mmu04723: Retrograde endocannabinoid signaling, mmu05208: Chemical carcinogenesis—ROS, mmu05415: Diabetic cardiomyopathy, mmu05020: Prion disease, mmu05016: Huntington disease,mmu05012: PD, mmu05014: ALS, mmu05010: AD, mmu05022: Pathways of neurodegeneration—multiple diseases, mmu04932: Non-alcoholic fatty liver disease, GO-CC GO: 0070469-respiratory chain, GO: 0005747-mitochondrial respiratory chain complex I,GO: 0005743-mitochondrial inner membrane, GO: 0005739-mitochondrion, GO-BP: 0042776-mitochondrial ATP synthesis coupled proton transport, GO-BP: 0009060 ~ aerobic respiration, GO-BP: 0032981 ~ mitochondrial respiratory chain complex I assembly |
| NDUFA3 | Upregulated | 1.32E E−09 | 1.740 | 2280 ± 171 | 2926 ± 255 | 2988 ± 568 | 2664 ± 174 | 3968 ± 880 | 3439 ± 678 | KEGG-mmu00190: Oxidative phosphorylation, mmu04714: Thermogenesis, mmu04723: Retrograde endocannabinoid signaling, mmu05208: Chemical carcinogenesis—ROS, mmu05415: Diabetic cardiomyopathy, mmu05020: Prion disease, mmu05016: Huntington disease,mmu05012: PD,mmu05014: ALS,mmu05010: AD, mmu05022: Pathways of neurodegeneration—multiple diseases, mmu04932: Non-alcoholic fatty liver disease, GO-CC GO: 0070469-respiratory chain, GO: 0005747-mitochondrial respiratory chain complex I,GO: 0005743 ~ mitochondrial inner membrane, GO: 0005739 ~ mitochondrion, GO-BP: 0042776-mitochondrial ATP synthesis coupled proton transport, GO-BP: 0009060-aerobic respiration, GO-BP: 0032981-mitochondrial respiratory chain complex I assembly |
| MRPL14 | Upregulated | 5.46E E−10 | 1.7126 | 503 ± 40 | 732 ± 94 | 705 ± 86 | 632 ± 52 | 862 ± 101 | 792 ± 142 | GO-CC: 0005840-ribosome, GO-MF: 0003735-structural constituent of ribosome, GO-BP: 0032543-mitochondrial translation |
| CYBA | Upregulated | 0.001343 | 1.693 | 43 ± 5.6 | 50.9 ± 10 | 50.7 ± 4.7 | 49.3 ± 9.1 | 59.7 ± 10.3 | 72.2 ± 12.8 | KEGG-mmu05208: Chemical carcinogenesis—ROS, mmu05415: Diabetic cardiomyopathy, mmu05020: Prion disease |
| MRPL33 | Upregulated | 2.10E E−06 | 1.623 | 643 ± 71 | 808 ± 134 | 858 ± 130 | 766 ± 90 | 1043 ± 175 | 949 ± 262 | GO-CC: 0005840 ~ ribosome, GO-MF: 0003735 ~ structural constituent of ribosome, GO-BP: 0032543 ~ mitochondrial translation |
| RPL35 | Upregulated | 0.000127 | 1.604 | 409 ± 41.9 | 509 ± 76 | 477 ± 51 | 473 ± 32 | 607 ± 82 | 539 ± 84 | GO-CC: 0005840 ~ ribosome |
| MRPS33 | Upregulated | 1.63E E−05 | 1.537 | 2104 ± 173 | 2786 ± 408 | 2725 ± 282 | 2533 ± 233 | 3235 ± 314 | 2958 ± 735 | GO-CC: 0005840 ~ ribosome, GO: 0005763 ~ mitochondrial small ribosomal subunit, GO-BP: 0032543 ~ mitochondrial translation |
| MRPS21 | Upregulated | 2.32E E−06 | 1.537 | 1034 ± 93 | 1394 ± 185 | 1387 ± 224 | 1206 ± 25 | 1592 ± 228 | 1459 ± 254 | GO-CC: 0005840 ~ ribosome, GO: 0005763 ~ mitochondrial small ribosomal subunit, GO-BP: 0032543 ~ mitochondrial translation |
| NDUFS5 | Upregulated | 3.84E E−06 | 1.552 | 3073 ± 282 | 4023 ± 472 | 3960 ± 741 | 3566 ± 325 | 4772 ± 654 | 4372 ± 833 | GO-BP: 0042776 ~ mitochondrial ATP synthesis coupled proton transport, GO: 0009060 ~ aerobic respiration, GO: 0032981 ~ mitochondrial respiratory chain complex I assembly |
| MRPS28 | Upregulated | 3.84E E−05 | 1.509 | 292 ± 32 | 376 ± 47 | 370 ± 42 | 352 ± 33 | 440 ± 50 | 420 ± 82 | GO-CC: 0005840 ~ ribosome, GO-CC: 0005739 ~ mitochondrion, GO: 0005763 ~ mitochondrial small ribosomal subunit |
| RPS4L | Down regulated | 4.88E E−05 | 0.695 | 147 ± 26 | 168 ± 29 | 137 ± 27 | 124 ± 14 | 102 ± 15 | 119 ± 25 | GO-CC: 0005840 ~ ribosome |
| MT-ND6 | Down regulated | 5.76E E−15 | 0.509 | 1338 ± 126 | 1086 ± 175 | 978 ± 146 | 1182 ± 1493 | 682 ± 100 | 821 ± 164 | KEGG-mmu00190: Oxidative phosphorylation, mmu04714: Thermogenesis, mmu04723: Retrograde endocannabinoid signaling, mmu05208: Chemical carcinogenesis—ROS, mmu05415: Diabetic cardiomyopathy, mmu05020: Prion disease, mmu05016: Huntington disease, mmu05012: PD, mmu05014: ALS,mmu05010: AD, mmu05022: Pathways of neurodegeneration—multiple diseases, mmu04932: Non-alcoholic fatty liver disease, GO-CC GO: 0070469 ~ respiratory chain, GO: 0005747 ~ mitochondrial respiratory chain complex I, GO: 0005743 ~ mitochondrial inner membrane, GO: 0005739 ~ mitochondrion, GO-BP: 0042776 ~ mitochondrial ATP synthesis coupled proton transport, GO-BP: 0009060 ~ aerobic respiration, GO-BP: 0032981 ~ mitochondrial respiratory chain complex I assembly |
DAVID software was used for analysis. Data of normalized values for gene expression are mean ± SD, n = 6. Fold change represents the ratio of the group mean relative to the mean value of the 0 mg/kg wild-type group when the absolute value of logarithm of the ratio is the maximum. All P values for gene expression were adjusted using Benjamini–Hochberg method and expressed as q values
PD Parkinson’s disease, ALS amyotrophic lateral sclerosis, AD Alzheimer disease, ROS reactive oxygen species CEBPZOS, CEBPZ Opposite Strand, NDUFS6 NADH: ubiquinone oxidoreductase subunit S6, SDHAF4 succinate dehydrogenase complex assembly factor 4, NDUFA13 NADH: ubiquinone oxidoreductase subunit A13; NDUFB7, NADH: ubiquinone oxidoreductase subunit b7, NDUFA3 NADH: ubiquinone oxidoreductase subunit A3, MRPL14 mitochondrial ribosomal protein L14, CYBA cytochrome B-245 alpha chain, MRPL33 mitochondrial ribosomal protein L33, RPL35 ribosomal protein L35, MRPS33 mitochondrial ribosomal protein S33, MRPS21 mitochondrial ribosomal protein S2, NDUFS5 NADH: ubiquinone oxidoreductase subunit S5, MRPS28 mitochondrial ribosomal protein S28, RPS4L ribosomal protein S4-like, MT-ND6 mitochondrially encoded NADH: ubiquinone oxidoreductase core subunit 6
In module eigengene 8 (ME8) (Fig. 4A), increased expression of 142 genes was noted in different GO and KEGG by David software. The analysis showed various GO and KEGG pathways with significant expression, including KEGG mmu03010: Ribosome (q = 1.93E−24), KEGG mmu05171: Coronavirus disease—COVID-19 (q = 3.10E−10), KEGG mmu03008: Ribosome biogenesis in eukaryotes (q = 3.68E−05), GO-CC: 0022626-cytosolic ribosome (q = 2.26E−18), GO-CC: 0005840-ribosome (q = 3.63E−13), GO-CC: 0022627-cytosolic small ribosomal subunit (q = 2.25E−10), GO-CC: 0045202-synapse (q = 3.95E−09), GO-CC: 0098794-postsynapse (q = 9.81E−09), GO-CC: 0022625-cytosolic large ribosomal subunit (q = 1.08E−07), GO-CC: 0015935-small ribosomal subunit (q = 4.02E−05), GO-CC: 0005829-cytosol (q = 5.01E−04), GO-CC: 0098793-presynapse (q = 8.70E−04), GO-CC: 0005737-cytoplasm (q = 8.70E−04), GO-CC: 0042788-polysomal ribosome (q = 0.003), GO-MF: 0003735- ~ structural constituent of ribosome (q = 4.63E−17), GO-BP: 0002181-cytoplasmic translation (q = 1.21E−17), and GO-BP: 0006412-translation (q = 2.48E−10) (Table 1).
Fig. 4.
A Heatmap of module eigengene 4 (ME8, 142 genes) of the cerebral cortex of acrylamide-exposed WT and IL-1ß KO mice. Columns: exposure groups (0, 12.5, 25 mg/kg). Red cluster (1): upregulated genes, green cluster (2): downregulated genes. B Protein network analysis of ME8 module using STRING software. C Table shows the scores of the top proteins in ME8 arranged from the highest score (top) to the lowest score (bottom) (color figure online)
The following genes were upregulated in the ME8 module: MACF1 (q = 1.27E−20), YWHAH (q = 5.08E−05), MT2 (q = 0.00586), RPS27A (q = 0.012784), and RPL18 (q = 0.041199), while the following were downregulated: PTPRN2 (q = 0.017284), RPS20 (q = 4.63E−05), KLC2 (q = 0.008854), RPS2 (q = 1.02E−06), EEF1A2 (q = 1.46E−08), N-R5S113 (q = 0.02546), N-R5S111 (q = 0.045153), and N-R5S121 (q = 0.02531) (Table 5). Protein network analysis of ME8 indicated the involvement of different ribosomal proteins, with high scores, including RPl18, Rps10, Rpl30, Rpl27a, Gm7536, Rps2, Rps13, Rpl9-ps6, Eef1a2, Rps27a, Rpl10, Rps20, and Rpsa (Fig. 4B, C).
Table 5.
GO (biological process) and KEGG pathway over representation analysis of ME8 module and list of involved genes in wild-type and IL-1b KO mice exposed to acrylamide at 0, 12.5, 25 mg/kg for 28 days by oral gavage
| Gene | Regulation | q value | Fold change | Wild-type (mg/kg) (mean ± SD) | IL-1b KO (mg/kg) (mean ± SD) | GO/KEGG term | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 12.5 | 25 | 0 | 12.5 | 25 | |||||
| MACF1 | Upregulated | 1.27E−20 | 1.951 | 270 ± 34 | 242 ± 8 | 266 ± 14 | 253 ± 23 | 528 ± 63 | 365 ± 13 | GO-CC: 0005737-cytoplasm |
| YWHAH | Upregulated | 5.08E−05 | 1.537 | 4874 ± 2777 | 5990 ± 851 | 6335 ± 937 | 6201 ± 487 | 7494 ± 1116 | 6304 ± 933 | GO-CC: 0045202-synapse, GO-CC: 0098793-presynapse,GO-CC: 0005829-cytosol |
| MT2 | Upregulated | 0.00586 | 1.287 | 490 ± 115 | 608 ± 131 | 632 ± 106 | 451 ± 86 | 519 ± 137 | 546 ± 78 | GO-CC: 0005829-cytosol, GO-CC: 0005737-cytoplasm |
| RPS27A | Upregulated | 0.012784 | 1.163 | 2972 ± 314 | 3458 ± 257 | 3353 ± 967 | 2687 ± 280 | 2617 ± 531 | 2908 ± 575 | KEGG-mmu03010: Ribosome, GO-CC: 0022626-cytosolic ribosome, GO-CC: 0005840-ribosome, GO-CC: 0022627-cytosolic small ribosomal subunit, GO-CC: 0045202-synapse, GO-CC: 0098794-postsynapse, GO-CC: 0015935-small ribosomal subunit, GO-MF: 0003735-structural constituent of ribosome, GO-BP: 0002181-cytoplasmic translation, GO-BP: 0006412-translation |
| RPL18 | Upregulated | 0.041199 | 1.152 | 1185 ± 57 | 1366 ± 104 | 1276 ± 243 | 1110 ± 137 | 1045 ± 164 | 1215 ± 150 | KEGG-mmu03010: Ribosome, KEGG- mmu05171: Coronavirus disease—COVID-19, GO-CC: 0022626-cytosolic ribosome, GO-CC: 0005840-ribosome, GO-CC: 0045202-synapse, GO-CC: 0022625-cytosolic large ribosomal subunit, GO-CC: 0015935-small ribosomal subunit, GO-CC: 0005737-cytoplasm, GO-CC: 0005829-cytosol, GO-CC: 0042788-polysomal ribosome, GO-MF: 0003735-structural constituent of ribosome, GO-BP: 0002181-cytoplasmic translation, GO-BP: 0006412-translation |
| PTPRN2 | Downregulated | 0.017284 | 0.715 | 171 ± 28 | 171 ± 14 | 152 ± 20 | 142 ± 22 | 122 ± 21 | 143 ± 30 | GO-CC: 0045202-synapse, GO-CC: 0098793-presynapse,GO-CC: 0005737-cytoplasm |
| RPS20 | Downregulated | 4.63E−05 | 0.706 | 1566 ± 220 | 1647 ± 176 | 1497 ± 419 | 1306 ± 112 | 1106 ± 200 | 1269 ± 222 | KEGG-mmu03010: Ribosome, KEGG-mmu05171: Coronavirus disease—COVID-19, GO-CC: 0022626-cytosolic ribosome, GO-CC: 0005840-ribosome, GO-CC: 0022627-cytosolic small ribosomal subunit, GO-CC: 0045202-synapse, GO-CC: 0098794-postsynapse, GO-CC: 0015935-small ribosomal subunit, GO-MF: 0003735-structural constituent of ribosome, GO-BP: 0002181-cytoplasmic translation, GO-BP: 0006412-translation |
| KLC2 | Downregulated | 0.008854 | 0.679 | 247 ± 37 | 226 ± 20 | 207 ± 54 | 190 ± 36 | 168 ± 35 | 204 ± 38 | GO-CC: 0005829-cytosol |
| RPS2 | Downregulated | 1.02E−06 | 0.672 | 2142 ± 339 | 2303 ± 299 | 2155 ± 324 | 2203 ± 290 | 1441 ± 216 | 1935 ± 363 | KEGG-mmu03010: Ribosome, KEGG-mmu05171: Coronavirus disease—COVID-19, GO-CC: 0022626-cytosolic ribosome, GO-CC: 0005840-ribosome, GO-CC: 0045202-synapse, GO-CC: 0015935-small ribosomal subunit, GO-CC: 0005829-cytosol, GO-MF: 0003735-structural constituent of ribosome, GO-BP: 0002181-cytoplasmic translation, GO-BP: 0006412-translation |
| EEF1A2 | Downregulated | 1.46E−08 | 0.568 | 528 ± 64 | 483 ± 67 | 422 ± 91 | 361 ± 64 | 300 ± 44 | 401 ± 88 | GO-CC: 0045202-synaps, GO-CC: 0005737-cytoplasm |
| N-R5S113 | Downregulated | 0.02546 | 0.318 | 10 ± 4.0 | 8.9 ± 3.6 | 8.2 ± 1.8 | 3.2 ± 1.4 | 3.2 ± 3.2 | 6.7 ± 7.3 | KEGG-mmu03010: Ribosome, KEGG-mmu03008: Ribosome biogenesis in eukaryotes |
| N-R5S111 | Downregulated | 0.045153 | 0.31 | 14.6 ± 4.6 | 13 ± 6.9 | 11.3 ± 7.7 | 8.4 ± 2.8 | 5.2 ± 3.2 | 7.1 ± 4.7 | KEGG-mmu03010: Ribosome, KEGG-mmu03008: Ribosome biogenesis in eukaryotes |
| N-R5S121 | Downregulated | 0.02531 | 0.316 | 15.8 ± 4 | 10.6 ± 4.6 | 11.0 ± 4.9 | 6.4 ± 2.8 | 5 ± 4.3 | 9.4 ± 8.3 | KEGG-mmu03010: Ribosome, KEGG-mmu03008: Ribosome biogenesis in eukaryotes |
DAVID software was used for analysis. Data of normalized values for gene expression are mean ± SD, n = 6. All P values for the gene expression were adjusted using Benjamini–Hochberg method and expressed as q values. Fold change represents the ratio of the mean of any group to the mean of the 0 mg/kg wild-type group when the absolute value of logarithm of the ratio is the maximum
MACF1 microtubule actin crosslinking factor 1, YWHAH tyrosine 3-monooxygenase/tryptophan 5-monooxygenase activation protein eta, MT2 metallothionein 2, RPS27A ribosomal protein S27a, RPL18 ribosomal protein l18, PTPRN2 protein tyrosine phosphatase receptor type N2, RPS20 ribosomal protein S20, KLC2 kinesin light chain 2, RPS2 ribosomal protein S2, EEF1A2 elongation factor 1-alpha 2, n-R5s113 nuclear-encoded rRNA 5S 113, n-R5s111 nuclear-encoded rRNA 5S 111, N-R5S121 nuclear-encoded rRNA 5S 121
Discussion
IL-1b deletion activates genes in extracellular regions
Transcriptome analysis of ME3 demonstrated upregulation of genes by IL-1β deletion in the GO-extracellular regions, including SNORC, PFN1, CRHBP, and PAMR1 (Table 2). The function of SNORC in the central nervous system is unknown at present, but it is highly expressed in the white matter, spinal cord and medulla oblongata and in astrocytes as well as in excitatory neurons at a single cell level (https://www.proteinatlas.org/). A recent study involving transcriptome analysis reported the expression of SNORC in the brain of control subjects but not in cases with Alzheimer disease (Chen et al. 2022). On the other hand, PFN1 (Profilin) gene was reported to be involved in amyotrophic lateral sclerosis (ALS) (Henty-Ridilla et al. 2017). PFN1, which is expressed in almost all eukaryotic cells, was the first actin-binding protein identified to regulate actin dynamics (Zhao et al. 2018). PFN1 is involved in various cellular physiological processes, such as autophagy (Lu et al. 2018) and apoptosis (Yang et al. 2017), as well as in oxidative stress (Li et al. 2018). Knockdown of PFN1 inhibited M1 microglial polarization and promoted M2 microglia polarization 48 h after OGDR stimulation in BV2 cells (Lu et al. 2020). Knockdown of PFN1 also significantly attenuated brain infarcts and edema, improved cerebral blood flow and neurological deficits in MCAO-injured mice (Lu et al. 2020).
The CRHBP gene is linked to the stress pathway, which has been associated with the development of several substance use disorders (SUDs), relapse susceptibility (Levran et al. 2014, 2018), and major depressive disorders (O'Connell et al. 2018). CRH-BP codes for a high affinity binding protein for corticotrophin releasing hormone (CRH), the primary mediator of the mammalian neuroendocrine and behavioral response to stress (Chan et al. 2000). CRH-BP modulates CRH, which influences cortical and hippocampal EEG activity and is the primary mediator of the neuroendocrine stress response. In humans, it has been mapped in several brain regions, including the cerebral cortex (Wang et al. 2007). Thus, the CRHBP is considered candidate gene for anxiety and addiction and possibly required in NMDAR-mediated excitatory postsynaptic currents in the VTA area (Ungless et al. 2003). PAMR1 is known to be downregulated in the hippocampi of homozygous 3xTg AD mouse (Hokama et al. 2014). The MYOC gene is expressed and secreted by optic nerve astrocytes and differentiation of optic nerve oligodendrocytes is delayed in Myocilin-null mice. Optic nerves of Myocilin-null mice contain low levels of several myelin-associated proteins, including myelin basic protein, myelin proteolipid protein, and 2′3′-cyclic nucleotide 3′-phosphodiesterase, compared with those of wild-type littermates (Kwon et al. 2014). LY86 is mainly expressed in microglia in the central nervous system (protein atlas). In a genomic-wide-association study, alteration of the LY86 gene was noted in the AppNL−G−F/NL−G−F cortex, suggesting it is a risk factor for AD, as identified by genetic nodes in late-onset AD (Castillo et al. 2017).
A recent study involving protein network analysis in ME3 showed the involvement of WDFY1 protein in a mouse model of schizophrenia (Sancho-Balsells et al. 2020). Furthermore, the same group also described accumulation of WDFY1 protein in the CA1 area of the hippocampus and in the dorsolateral prefrontal cortex in postmortem samples from schizophrenic patients, but not in AD (Sancho-Balsells et al. 2020). Tmem254a is a transmembrane protein known to be expressed in various body tissues, including the brain (https://www.ncbi.nlm.nih.gov) and its expression has been identified in 4 of 18 independent BioProjects that assessed the effects of different stressors on the brain transcriptome in mice (Flati et al. 2020).
The antisense oligonucleotide is a single-strand RNA complementary to a protein coding (mRNA) with which it hybridizes and blocks its translation into protein. The primary function of asRNA is the regulation of gene expression at multiple levels, including transcription, post-transcription, and epigenetic modification (Pelechano and Steinmetz 2013; Wahlestedt 2013; Weiss et al. 1999). Previous studies showed that overexpression of antisense IL-1β transcript suppressed IL-1β expression, suggesting that the antisense-transcripts of innate-immunity-related genes play a role by regulating cytokine expression (Lu et al. 2013). However, the physiological role of IL-1bos remains obscure, but it may play a role in stabilization of the IL-1β KO mice model or in development.
Mitochondrial oxidative phosphorylation
Several mitochondrial proteins (NADH: ubiquinone oxidoreductase, Ndufs5, Ndufs6, Ndufa7, Ndufa5, Ndufa1, Ndufc1) detected in the present study by the protein network analysis of ME4 and ME7 are known to play important roles in oxidative stress-related processes (Figs. 2B, C, 3B, C). Inefficient oxidative phosphorylation may result in the generation of reactive oxygen species (ROS), leading to mitochondrial dysfunction and worsening of the oxidative stress process (Singh et al. 2019). The upregulated genes identified by KEGG analysis of ME4 (NDUFB8, MT-ATP8, NDUFA12, DNAH7A, MT-CYTB) are also related to mitochondria oxidative phosphorylation process, in addition to the proteasome-related genes PSMB6 and PSMB3 (Table 3). These genes have been reported to be involved in various neurodegenerative diseases, such as Parkinson disease, amyotrophic lateral sclerosis, Huntington disease, Pathways of neurodegeneration-multiple diseases (Table 3). GO and KEGG analyses of ME7 also identified upregulation of genes related to mitochondrial oxidative phosphorylation, including NDUFS6, NDUFA13, NDUFB7, NDUFA3, and NDUFS5, which are involved in a variety of neurodegenerative diseases (Table 4). Complex I (CI or NADH: ubiquinone oxidoreductase) is the largest ETC enzyme of the mitochondria, containing 44 subunits, and the main contributor to ROS production and functional impairments in CI, and seems to be correlated to increased oxidative stress caused by defects in the OXPHOS system (Giachin et al. 2016). Mitochondrial dysfunction represents a common pathogenic mechanism in NDs like Alzheimer’s disease (AD), Parkinson’s disease (PD), ALS, Huntington’s disease, and prion diseases (Lin and Beal 2006; Tillement et al. 2011; Federico et al. 2012; Schapira 2012; Butterfield et al. 2016). Additional complex I deficiency clinical phenotypes have also been associated with pediatric neurodegenerative diseases, including Leigh-like syndrome (LS), leukoencephalopathy, MELAS and NARP syndromes (Giachin et al. 2016). Mutations in 6 mtDNA-encoded (ND1 to 6) and 13 nuclear-encoded (NDUFS1 to 8; NDUFV1; NDUFA1, 2, 9, 10, and 12) CI subunits are considered to be correlated with LS (Rodenburg 2016). NDUFB8 is a signature of the mitochondrial complex I subunit, which is vital for normal mitochondrial function, but when present at high levels, it leads to cellular dysfunction (Davis et al. 2010). On the other hand, mutation of the NDUFA13 subunit leads to instability of mitochondrial complex I that affects motor nerve control by the brain (Angebault et al. 2015). Various in vivo and in vitro models of ALS and patient tissues have confirmed the role of mitochondrial dysfunction in various diseases (Gautam et al. 2019; Nakaya and Maragkakis 2018). This is because motor neurons depend on optimal mitochondrial function to fulfill their energy requirements. Mitochondrial damage causes insufficient ATP production and mediates motor neuron intraneuronal damage and even neuronal death, mediated through high calcium-induced excitotoxicity, increased ROS generation, and activation of the intrinsic apoptotic pathway (Manfredi and Xu 2005; Yakes and VanHouten 1997).
Mitochondrial DNA mutations in the MT-CYTB gene have been detected in the substantia nigra pars compacta and the frontal cortices of patients with PD, compared to the control individuals (Coxhead et al. 2016). ATPase 8 is one of the subunits of the mitochondrial ATP synthase complex (MT-ATP8) and this enzyme is responsible for most of ATP production in the cells (Senior et al. 2002). Several mutations affecting MT-ATP8 have been described in patients presenting with heterogeneous clinical features, varying from neurological to cardiac disorders (Dautant et al. 2018). Overall, mitochondrial respiratory deficiencies have been observed in numerous neurodegenerative disorders, such as AD and PD (Schon and Przedborski 2011). The mitochondrial defects are instrumental in provoking neuronal death in common adult-onset neurodegenerative disorders (Area-Gomez et al. 2019).
Proteasome
Changes in proteasome activity are closely associated with various neurological conditions, such as AD, PD, HD, and ALS (Im and Chung 2016). Our protein network results showed the involvement of various proteasomes subunits in ME4 in ACR neurotoxicity (Fig. 2B, C).
Ribosomal proteins
Alteration of ribosomal protein have been reported in a mouse model of frontotemporal dementia (FTD) (Evans et al. 2021). The present study also found changes in the expression of various ribosomal proteins (Fig. 4B, C) and association among ribosomal proteins, as shown by protein network analysis of modules 3 and 8 (Fig. 1C).
Synapse-related genes
Our results showed significant downregulation of DUSP1, MT-ND3 in ME4 (Table 3). The DUSP1 gene plays a role in the regulation of synaptic plasticity and neuronal morphology, and impairment of the physiological function of DUSP1 has been documented in AD, including the presence of low levels in cortical tissues of AD patients and correlation of these levels with tau pathology and cognitive decline (Perez-Sen et al. 2019). Downregulation in DUSP1 transcripts was also described in the cortex and striatum of mice models of Huntington’s disease (HD) and postmortem samples of HD patients (Luthi-Carter et al. 2002; Taylor et al. 2013), in addition to decrease in DUSP1 activity in PD patients (Collins et al. 2013). Other studies suggested that mitochondrial ND3 (MT-ND3) Aβ interaction could explain, at least in part, the low activity of Complex I in astrocytes and neurons in AD patients (Cruz-Rivera et al. 2018).
In module ME8, ACR exposure significantly upregulated YWHAH, which is involved in synapse pathway (Table 5). The YWHA gene family plays important roles in neuronal and synaptic development, function, and plasticity (Berg et al. 2003; Cornell and Toyo-Oka 2017; Toyo-oka et al. 2003). These genes also participate in the activation of tyrosine and tryptophan hydroxylases, the rate limiting enzymes in the synthesis of certain neurotransmitters, including serotonin and dopamine (Ichimura et al. 1987). Pathologically, evidence suggests that dysregulation of YWHA gene family is involved in the early stages of psychosis (Demars et al. 2020). In our study, the observed upregulation of YWHAH gene suggests its potential role in ACR-induced neurotoxicity and synaptic disfunction in mice. Another gene, Rpl18, is reported to be upregulated in hippocampal lysates of APP/PS1 mice model of SD (Elder et al. 2021). Furthermore, dysregulation of Rpl18 gene expression occurs early in the AD process (Martinez-Ballesteros et al. 2017). Other genes identified in our study, RPS20 and EEF1A, were reported to be downregulated in AD patients (Garcia-Esparcia et al. 2017).
Genes involved in learning and memory
Humans exposed to electrophiles, such as ACR and 1-bromopropane showed cognitive dysfunction (Ichihara et al. 2002; Igisu et al. 1975). In this regard, protein network analysis in ME4 showed changes in genes known to be involved in learning and memory proteins, such as Egr1, Egr2, Fos, Nr4a1, Btg2 (Barros et al. 2015; Bonow et al. 2009; Poirier et al. 2007; Suzuki et al. 2021; Hawk and Abel 2011) (Fig. 2B, C).
Our recent study demonstrated that exposure to ACR upregulated expression of Gpx1, Gpx4 and Gclc in wild-type mice but downregulated them in IL-1β knockout mice (Fergany et al. 2023). In our transcriptome study, the Gpx4 and Gclm show ACR-induced increase in expression in wild-type, but such increase disappeared inIL-1b KO mice. The expression of Gstm1 and Gstt2 was altered by ACR exposure similarly in both wild-type and IL-1b KO mice (Supplementary Fig. 1) and there is no ACR-related alteration in expression of Gpx1 and Gclc in both genotypes. These results are partially in consistence with result of (Fergany et al. 2023) which explain the protective effect of IL-1b against acrylamide-induced neurotoxicity.
In conclusions, we have demonstrated in the present study that IL-1b deletion, which potentiates the neurotoxicity of ACR, altered the expression of genes involved in the extracellular region. The results also showed that exposure of mice to ACR or IL-1b deletion altered the expression of genes involved in mitochondrial oxidative phosphorylation, proteasome, ribosome, synapse, learning, and memory, which have been described to be involved in the pathology of various neurodegenerative diseases.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank Ms. Arai for the excellent secretarial support and Tatsuro Ogawa (Tokyo University of Science) for the support in transcriptome data analysis.
Abbreviations
- ACR
Acrylamide
- AD
Alzheimer disease
- ALS
Amyotrophic lateral sclerosis
- EEG
Electroencephalogram
- FTD
Frontotemporal dementia
- HD
Huntington’s disease
- MACO
Middle cerebral artery occlusion
- MELAS syndrome
Mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes
- NARP syndrome
Neuropathy, ataxia, and retinitis pigmentosa
- NDs
Neurodegenerative diseases
- PD
Parkinson’s disease
- ROS
Reactive oxygen species
- sRNA
Antisense oligonucleotide
- VTA
Ventral trigeminal area
Funding
Open access funding provided by Tokyo University of Science. This work was supported in part by grants #17H06396 and #19H04279 from the Japan Society for the Promotion of Science.
Data Availability
The raw data generated from the experiment have been deposited in the NCBI Gene Expression Omnibus (GEO, http://www.ncbi.nlm.nih.gov/geo), gene bank accession number (GSE211746).
Declarations
Conflict of interest
All authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Anderson CM, Swanson RA. Astrocyte glutamate transport: review of properties, regulation, and physiological functions. Glia. 2000;32:1–14. doi: 10.1002/1098-1136(200010)32:1<1::AID-GLIA10>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- Angebault C, Charif M, Guegen N, et al. Mutation in NDUFA13/GRIM19 leads to early onset hypotonia, dyskinesia and sensorial deficiencies, and mitochondrial complex I instability. Hum Mol Genet. 2015;24:3948–3955. doi: 10.1093/hmg/ddv133. [DOI] [PubMed] [Google Scholar]
- Aoki H, Ueha S, Nakamura Y, et al. Greater extent of blood-tumor TCR repertoire overlap is associated with favorable clinical responses to PD-1 blockade. Cancer Sci. 2021;112:2993–3004. doi: 10.1111/cas.14975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Area-Gomez E, Guardia-Laguarta C, Schon EA, Przedborski S. Mitochondria, OxPhos, and neurodegeneration: cells are not just running out of gas. J Clin Investig. 2019;129:34–45. doi: 10.1172/JCI120848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashburner M, Ball CA, Blake JA, et al. Gene Ontology: tool for the unification of biology. Nat Genet. 2000;25:25–29. doi: 10.1038/75556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auld RB, Bedwell SF. Peripheral neuropathy with sympathetic overactivity from industrial contact with acrylamide. Can Med Assoc J. 1967;96:652. [PMC free article] [PubMed] [Google Scholar]
- Barros VN, Mundim M, Galindo LT, Bittencourt S, Porcionatto M, Mello LE. The pattern of c-Fos expression and its refractory period in the brain of rats and monkeys. Front Cell Neurosci. 2015 doi: 10.3389/fncel.2015.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg D, Holzmann C, Riess O. 14-3-3 proteins in the nervous system. Nat Rev Neurosci. 2003;4:752–762. doi: 10.1038/nrn1197. [DOI] [PubMed] [Google Scholar]
- Bonow RH, Aid S, Zhang Y, Becker KG, Bosetti F. The brain expression of genes involved in inflammatory response, the ribosome, and learning and memory is altered by centrally injected lipopolysaccharide in mice. Pharmacogenom J. 2009;9:116–126. doi: 10.1038/tpj.2008.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butterfield DA, Palmieri EM, Castegna A. Clinical implications from proteomic studies in neurodegenerative diseases: lessons from mitochondrial proteins. Expert Rev Proteom. 2016;13:259–274. doi: 10.1586/14789450.2016.1149470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castillo E, Leon J, Mazzei G, et al. Comparative profiling of cortical gene expression in Alzheimer's disease patients and mouse models demonstrates a link between amyloidosis and neuroinflammation. Sci Rep-UK. 2017 doi: 10.1038/s41598-017-17999-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan RKW, Vale WW, Sawchenko PE. Paradoxical activational effects of a corticotropin-releasing factor-binding protein “ligand inhibitor” in rat brain. Neuroscience. 2000;101:115–129. doi: 10.1016/S0306-4522(00)00322-5. [DOI] [PubMed] [Google Scholar]
- Chen S, Chang Y, Li L, et al. Spatially resolved transcriptomics reveals genes associated with the vulnerability of middle temporal gyrus in Alzheimer's disease. Acta Neuropathol Commun. 2022;10:188. doi: 10.1186/s40478-022-01494-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, O'Keeffe GW, Long-Smith CM, et al. Mitogen-activated protein kinase phosphatase (MKP)-1 as a neuroprotective agent: promotion of the morphological development of midbrain dopaminergic neurons. Neuromol Med. 2013;15:435–446. doi: 10.1007/s12017-013-8230-5. [DOI] [PubMed] [Google Scholar]
- Cornell B, Toyo-Oka K. 14–3-3 proteins in brain development: neurogenesis, neuronal migration and neuromorphogenesis. Front Mol Neurosci. 2017 doi: 10.3389/fnmol.2017.00318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coxhead J, Kurzawa-Akanbi M, Hussain R, Pyle A, Chinnery P, Hudson G. Somatic mtDNA variation is an important component of Parkinson's disease. Neurobiol Aging. 2016;38:217.e1–217.e6. doi: 10.1016/j.neurobiolaging.2015.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz-Rivera YE, Perez-Morales J, Santiago YM, et al. A selection of important genes and their correlated behavior in Alzheimer's disease. J Alzheimers Dis. 2018;65:193–205. doi: 10.3233/JAD-170799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dautant A, Meier T, Hahn A, Tribouillard-Tanvier D, di Rago JP, Kucharczyk R. ATP synthase diseases of mitochondrial genetic origin. Front Physiol. 2018 doi: 10.3389/fphys.2018.00329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CW, Hawkins BJ, Ramasamy S, et al. Nitration of the mitochondrial complex I subunit NDUFB8 elicits RIP1- and RIP3-mediated necrosis. Free Radic Biol Med. 2010;48:306–317. doi: 10.1016/j.freeradbiomed.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demars F, Kebir O, Marzo A, et al. Dysregulation of peripheral expression of the YWHA genes during conversion to psychosis. Sci Rep UK. 2020 doi: 10.1038/s41598-020-66901-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dheen ST, Kaur C, Ling EA. Microglial activation and its implications in the brain diseases. Curr Med Chem. 2007;14:1189–1197. doi: 10.2174/092986707780597961. [DOI] [PubMed] [Google Scholar]
- Elder MK, Erdjument-Bromage H, Oliveira MM, Mamcarz M, Neubert TA, Klann E. Age-dependent shift in the de novo proteome accompanies pathogenesis in an Alzheimer's disease mouse model. Commun Biol. 2021 doi: 10.1038/s42003-021-02324-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans HT, Taylor D, Kneynsberg A, Bodea LG, Gotz J. Altered ribosomal function and protein synthesis caused by tau. Acta Neuropathol Commun. 2021 doi: 10.1186/s40478-021-01208-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federico A, Cardaioli E, Da Pozzo P, Formichi P, Gallus GN, Radi E. Mitochondria, oxidative stress and neurodegeneration. J Neurol Sci. 2012;322:254–262. doi: 10.1016/j.jns.2012.05.030. [DOI] [PubMed] [Google Scholar]
- Fergany A, Zong C, Ekuban FA, et al. Deletion of IL-1beta exacerbates acrylamide-induced neurotoxicity in mice. Toxicol Sci. 2023;194:246–256. doi: 10.1093/toxsci/kfad077. [DOI] [PubMed] [Google Scholar]
- Flati T, Gioiosa S, Chillemi G, et al. A gene expression atlas for different kinds of stress in the mouse brain. Sci Data. 2020 doi: 10.1038/s41597-020-00772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Esparcia P, Sideris-Lampretsas G, Hernandez-Ortega K, et al. Altered mechanisms of protein synthesis in frontal cortex in Alzheimer disease and a mouse model. Am J Neurodegener Dis. 2017;6:15–25. [PMC free article] [PubMed] [Google Scholar]
- Gautam M, Jara JH, Kocak N, et al. Mitochondria, ER, and nuclear membrane defects reveal early mechanisms for upper motor neuron vulnerability with respect to TDP-43 pathology. Acta Neuropathol. 2019;137:47–69. doi: 10.1007/s00401-018-1934-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giachin G, Bouverot R, Acajjaoui S, Pantalone S, Soler-Lopez M. Dynamics of human mitochondrial complex I assembly: implications for neurodegenerative diseases. Front Mol Biosci. 2016 doi: 10.3389/fmolb.2016.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawk JD, Abel T. The role of NR4A transcription factors in memory formation. Brain Res Bull. 2011;85:21–29. doi: 10.1016/j.brainresbull.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henty-Ridilla JL, Juanes MA, Goode BL. Profilin directly promotes microtubule growth through residues mutated in amyotrophic lateral sclerosis. Curr Biol. 2017;27:3535–3543.e4. doi: 10.1016/j.cub.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hokama M, Oka S, Leon J, et al. Altered expression of diabetes-related genes in Alzheimer's disease brains: the Hisayama study. Cereb Cortex. 2014;24:2476–2488. doi: 10.1093/cercor/bht101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins SJ, Rothwell NJ. Cytokines and the nervous system. I: expression and recognition. Trends Neurosci. 1995;18:83–88. doi: 10.1016/0166-2236(95)80029-2. [DOI] [PubMed] [Google Scholar]
- Horai C, Asano M, Sudo K, Kanuka H, Suzuki M, Nishihara M, Takahashi M, Iwakuraet Y. Production of mice deficient in genes for interleukin (IL)-1α IL-1β IL-1α/β and IL-1 receptor antagonist shows that IL-1β Is Crucial in Turpentine-induced Fever development and glucocorticoid secretion. J Exp Med. 1998;187(9):1463–1475. doi: 10.1084/jem.187.9.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ichihara G, Miller JK, Ziolkokwska A, Itohara S, Takeuchi Y. Neurological disorders in three workers exposed to 1-bromopropane. J Occup Health. 2002;44:1–7. doi: 10.1539/joh.44.1. [DOI] [Google Scholar]
- Ichimura T, Isobe T, Okuyama T, Yamauchi T, Fujisawa H. Brain 14-3-3 protein is an activator protein that activates tryptophan 5-monooxygenase and tyrosine 3-monooxygenase in the presence of Ca2+, calmodulin-dependent protein kinase-II. FEBS Lett. 1987;219:79–82. doi: 10.1016/0014-5793(87)81194-8. [DOI] [PubMed] [Google Scholar]
- Igisu H, Goto I, Kawamura Y, Kato M, Izumi K, Kuroiwa O. Acrylamide encephaloneuropathy due to well water-pollution. J Neurol Neurosurg Psychiatry. 1975;38:581–584. doi: 10.1136/jnnp.38.6.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im E, Chung KC. Precise assembly and regulation of 26S proteasome and correlation between proteasome dysfunction and neurodegenerative diseases. BMB Rep. 2016;49:459–473. doi: 10.5483/BMBRep.2016.49.9.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John GR, Lee SC, Song X, Rivieccio M, Brosnan CF. IL-1-regulated responses in astrocytes: relevance to injury and recovery. Glia. 2005;49:161–176. doi: 10.1002/glia.20109. [DOI] [PubMed] [Google Scholar]
- Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28:27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon HS, Nakaya N, Abu-Asab M, Kim HS, Tomarev SI. Myocilin is involved in NgR1/Lingo-1-mediated oligodendrocyte differentiation and myelination of the optic nerve. J Neurosci. 2014;34:5539–5551. doi: 10.1523/JNEUROSCI.4731-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langfelder P, Horvath S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinform. 2008 doi: 10.1186/1471-2105-9-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levran O, Randesi M, Li Y, et al. Drug addiction and stress-response genetic variability: association study in African Americans. Ann Hum Genet. 2014;78:290–298. doi: 10.1111/ahg.12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levran O, Peles E, Randesi M, et al. Genetic variations in genes of the stress response pathway are associated with prolonged abstinence from heroin. Pharmacogenomics. 2018;19:333–341. doi: 10.2217/pgs-2017-0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Tan MS, Jiang T, Tan L. Microglia in Alzheimer's disease. Biomed Res Int. 2014 doi: 10.1155/2014/437483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Liu JJ, Chen B, Fan LH. A positive feedback loop of profilin-1 and RhoA/ROCK1 promotes endothelial dysfunction and oxidative stress. Oxid Med Cell Longev. 2018 doi: 10.1155/2018/4169575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin MT, Beal MF. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature. 2006;443:787–795. doi: 10.1038/nature05292. [DOI] [PubMed] [Google Scholar]
- LoPachin RM. The changing view of acrylamide neurotoxicity. Neurotoxicology. 2004;25:617–630. doi: 10.1016/j.neuro.2004.01.004. [DOI] [PubMed] [Google Scholar]
- LoPachin RM, Gavin T. Molecular mechanism of acrylamide neurotoxicity: lessons learned from organic chemistry. Environ Health Perspect. 2012;120:1650–1657. doi: 10.1289/ehp.1205432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LoPachin RM, Balaban CD, Ross JF. Acrylamide axonopathy revisited. Toxicol Appl Pharm. 2003;188:135–153. doi: 10.1016/S0041-008X(02)00072-8. [DOI] [PubMed] [Google Scholar]
- Lu J, Wu X, Hong M, Tobias P, Han J. A potential suppressive effect of natural antisense IL-1beta RNA on lipopolysaccharide-induced IL-1beta expression. J Immunol. 2013;190:6570–6578. doi: 10.4049/jimmunol.1102487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu YC, Wang Y, Xu H, Shi C, Jin FY, Li W. Profilin 1 induces drug resistance through Beclin1 complex-mediated autophagy in multiple myeloma. Cancer Sci. 2018;109:2706–2716. doi: 10.1111/cas.13711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu E, Wang Q, Li S, et al. Profilin 1 knockdown prevents ischemic brain damage by promoting M2 microglial polarization associated with the RhoA/ROCK pathway. J Neurosci Res. 2020;98:1198–1212. doi: 10.1002/jnr.24607. [DOI] [PubMed] [Google Scholar]
- Luthi-Carter R, Hanson SA, Strand AD, et al. Dysregulation of gene expression in the R6/2 model of polyglutamine disease: parallel changes in muscle and brain. Hum Mol Genet. 2002;11:1911–1926. doi: 10.1093/hmg/11.17.1911. [DOI] [PubMed] [Google Scholar]
- Manfredi G, Xu ZS. Mitochondrial dysfunction and its role in motor neuron degeneration in ALS. Mitochondrion. 2005;5:77–87. doi: 10.1016/j.mito.2005.01.002. [DOI] [PubMed] [Google Scholar]
- Martinez-Ballesteros M, Garcia-Heredia JM, Nepomuceno-Chamorro IA, Riquelme-Santos JC. Machine learning techniques to discover genes with potential prognosis role in Alzheimer's disease using different biological sources. Inform Fusion. 2017;36:114–129. doi: 10.1016/j.inffus.2016.11.005. [DOI] [Google Scholar]
- Medel-Matus JS, Alvarez-Croda DM, Martinez-Quiroz J, Beltran-Parrazal L, Morgado-Valle C, Lopez-Meraz ML. IL-1beta increases necrotic neuronal cell death in the developing rat hippocampus after status epilepticus by activating type I IL-1 receptor (IL-1RI) Int J Dev Neurosci. 2014;38:232–240. doi: 10.1016/j.ijdevneu.2014.09.006. [DOI] [PubMed] [Google Scholar]
- Mi H, Huang X, Muruganujan A, et al. PANTHER version 11: expanded annotation data from gene ontology and reactome pathways, and data analysis tool enhancements. Nucleic Acids Res. 2017;45:D183–D189. doi: 10.1093/nar/gkw1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mietto BS, Mostacada K, Martinez AM. Neurotrauma and inflammation: CNS and PNS responses. Mediat Inflamm. 2015;2015:251204. doi: 10.1155/2015/251204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mottram DS, Wedzicha BL, Dodson AT. Acrylamide is formed in the Maillard reaction. Nature. 2002;419:448–449. doi: 10.1038/419448a. [DOI] [PubMed] [Google Scholar]
- Murray KN, Parry-Jones AR, Allan SM. Interleukin-1 and acute brain injury. Front Cell Neurosci. 2015 doi: 10.3389/fncel.2015.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakaya T, Maragkakis M. Amyotrophic lateral sclerosis associated FUS mutation shortens mitochondria and induces neurotoxicity. Sci Rep UK. 2018 doi: 10.1038/s41598-018-33964-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connell CP, Goldstein-Piekarski AN, Nemeroff CB, et al. Antidepressant outcomes predicted by genetic variation in corticotropin-releasing hormone binding protein. Am J Psychiatry. 2018;175:251–261. doi: 10.1176/appi.ajp.2017.17020172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelechano V, Steinmetz LM. Gene regulation by antisense transcription. Nat Rev Genet. 2013;14:880–893. doi: 10.1038/nrg3594. [DOI] [PubMed] [Google Scholar]
- Perez-Sen R, Queipo MJ, Gil-Redondo JC, et al. Dual-specificity phosphatase regulation in neurons and glial cells. Int J Mol Sci. 2019 doi: 10.3390/ijms20081999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poirier R, Cheval H, Mailhes C, Charnay P, Davis S, Laroche S. Paradoxical role of an Egr transcription factor family member, Egr2/Krox20, in learning and memory. Front Behav Neurosci. 2007 doi: 10.3389/neuro.08.006.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransohoff RM, Schafer D, Vincent A, Blachere NE, Bar-Or A. Neuroinflammation: ways in which the immune system affects the brain. Neurotherapeutics. 2015;12:896–909. doi: 10.1007/s13311-015-0385-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodenburg RJ. Mitochondrial complex I-linked disease. BBA Bioenerget. 2016;1857:938–945. doi: 10.1016/j.bbabio.2016.02.012. [DOI] [PubMed] [Google Scholar]
- Sancho-Balsells A, Brito V, Fernandez B, et al. Lack of helios during neural development induces adult schizophrenia-like behaviors associated with aberrant levels of the TRIF-recruiter protein WDFY1. Front Cell Neurosci. 2020;14:93. doi: 10.3389/fncel.2020.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schapira AHV. Mitochondrial diseases. Lancet. 2012;379:1825–1834. doi: 10.1016/S0140-6736(11)61305-6. [DOI] [PubMed] [Google Scholar]
- Schon EA, Przedborski S. Mitochondria: the next (neurode)generation. Neuron. 2011;70:1033–1053. doi: 10.1016/j.neuron.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senior AE, Nadanaciva S, Weber J. The molecular mechanism of ATP synthesis by F1F0-ATP synthase. BBA Bioenerget. 2002;1553:188–211. doi: 10.1016/S0005-2728(02)00185-8. [DOI] [PubMed] [Google Scholar]
- Shichino S, Ueha S, Hashimoto S, et al. Transcriptome network analysis identifies protective role of the LXR/SREBP-1c axis in murine pulmonary fibrosis. JCI Insight. 2019 doi: 10.1172/jci.insight.122163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva B, Sousa L, Miranda A, et al. Memory deficit associated with increased brain proinflammatory cytokine levels and neurodegeneration in acute ischemic stroke. Arq Neuropsiquiatr. 2015;73:655–659. doi: 10.1590/0004-282X20150083. [DOI] [PubMed] [Google Scholar]
- Singh A, Kukreti R, Saso L, Kukreti S. Oxidative stress: a key modulator in neurodegenerative diseases. Molecules. 2019;24:1583. doi: 10.3390/molecules24081583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan SA, Barres BA. Mechanisms of astrocyte development and their contributions to neurodevelopmental disorders. Curr Opin Neurobiol. 2014;27:75–81. doi: 10.1016/j.conb.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith E, Oehme F. Acrylamide and polyacrylamide: a review of production, use, environmental fate and neurotoxicity. Rev Environ Health. 1991;9:215–228. doi: 10.1515/REVEH.1991.9.4.215. [DOI] [PubMed] [Google Scholar]
- Stadler RH, Blank I, Varga N, et al. Acrylamide from Maillard reaction products. Nature. 2002;419:449–450. doi: 10.1038/419449a. [DOI] [PubMed] [Google Scholar]
- Streit WJ, Graeber MB, Kreutzberg GW. Functional plasticity of microglia—a review. Glia. 1988;1:301–307. doi: 10.1002/glia.440010502. [DOI] [PubMed] [Google Scholar]
- Sun JQ, Nishiyama T, Shimizu K, Kadota K. TCC: an R package for comparing tag count data with robust normalization strategies. BMC Bioinform. 2013 doi: 10.1186/1471-2105-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki K, Shinohara M, Uno Y, et al. Deletion of B-cell translocation gene 2 (BTG2) alters the responses of glial cells in white matter to chronic cerebral hypoperfusion. J Neuroinflammation. 2021;18:86. doi: 10.1186/s12974-021-02135-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szalay G, Martinecz B, Lenart N, et al. Microglia protect against brain injury and their selective elimination dysregulates neuronal network activity after stroke. Nat Commun. 2016 doi: 10.1038/ncomms11499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang M, Sun J, Shimizu K, Kadota K. Evaluation of methods for differential expression analysis on multi-group RNA-seq count data. BMC Bioinform. 2015;16:361. doi: 10.1186/s12859-015-0794-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor DM, Moser R, Regulier E, et al. MAP kinase phosphatase 1 (MKP-1/DUSP1) is neuroprotective in Huntington's disease via additive effects of JNK and p38 inhibition. J Neurosci. 2013;33:2313–2325. doi: 10.1523/JNEUROSCI.4965-11.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Human Proteinatlas (2023) https://www.proteinatlas.org/
- Tillement L, Lecanu L, Papadopoulos V. Alzheimer's disease: effects of beta-amyloid on mitochondria. Mitochondrion. 2011;11:13–21. doi: 10.1016/j.mito.2010.08.009. [DOI] [PubMed] [Google Scholar]
- Toyo-oka K, Shionoya A, Gambello MJ, et al. 14-3-3 epsilon is important for neuronal migration by binding to NUDEL: a molecular explanation for Miller–Dieker syndrome. Nat Genet. 2003;34:274–285. doi: 10.1038/ng1169. [DOI] [PubMed] [Google Scholar]
- Ungless MA, Singh V, Crowder TL, Yaka R, Ron D, Bonci A. Corticotropin-releasing factor requires CRF binding protein to potentiate NMDA receptors via CRF receptor 2 in dopamine neurons. Neuron. 2003;39:401–407. doi: 10.1016/S0896-6273(03)00461-6. [DOI] [PubMed] [Google Scholar]
- Wahlestedt C. Targeting long non-coding RNA to therapeutically upregulate gene expression. Nat Rev Drug Discov. 2013;12:433–446. doi: 10.1038/nrd4018. [DOI] [PubMed] [Google Scholar]
- Wang B, You ZB, Rice KC, Wise RA. Stress-induced relapse to cocaine seeking: roles for the CRF2 receptor and CRF-binding protein in the ventral tegmental area of the rat. Psychopharmacology. 2007;193:283–294. doi: 10.1007/s00213-007-0782-3. [DOI] [PubMed] [Google Scholar]
- Weiss B, Davidkova G, Zhou LW. Antisense RNA gene therapy for studying and modulating biological processes. Cell Mol Life Sci. 1999;55:334–358. doi: 10.1007/s000180050296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yakes FM, VanHouten B. Mitochondrial DNA damage is more extensive and persists longer than nuclear DNA damage in human cells following oxidative stress. Proc Natl Acad Sci USA. 1997;94:514–519. doi: 10.1073/pnas.94.2.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang DF, Wang Y, Jiang MN, et al. Downregulation of profilin-1 expression attenuates cardiomyocytes hypertrophy and apoptosis induced by advanced glycation end products in H9c2 cells. Biomed Res Int. 2017;2017:1–11. doi: 10.1155/2017/9716087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Zhang Y. Formation and reduction of acrylamide in Maillard reaction: a review based on the current state of knowledge. Crit Rev Food Sci Nutr. 2007;47:521–542. doi: 10.1080/10408390600920070. [DOI] [PubMed] [Google Scholar]
- Zhao JR, Wade B, Ma J, Hart CM, Sutliff R. Differential ubiquitination of profilin-1 in hypoxia-induced pulmonary hypertension. FASEB J. 2018 doi: 10.1096/fasebj.2018.32.1_supplement.628.4. [DOI] [Google Scholar]
- Zong C, Hasegawa R, et al. Role of microglial activation and neuroinflammation in neurotoxicity of acrylamide in vivo and in vitro. Arch Toxicol. 2019;93:2007–2019. doi: 10.1007/s00204-019-02471-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data generated from the experiment have been deposited in the NCBI Gene Expression Omnibus (GEO, http://www.ncbi.nlm.nih.gov/geo), gene bank accession number (GSE211746).