Abstract
Objective
High body mass index is a well-established modifiable comorbidity that is known to increase postoperative complications in all types of surgery, including spine surgery. Obesity is increasing in prevalence amongst the general population. As this growing population of obese patients ages, understanding how they faire undergoing cervical disc arthroplasty (CDA) is important for providing safe and effective evidence-based care for cervical degenerative pathology.
Methods
Our study used the Healthcare Cost and Utilization Project’s National Inpatient Sample to assess patients undergoing CDA comparing patient characteristics and outcomes in nonobese patients to obese patients from 2004 to 2014.
Results
Our study found a significant increase in the overall utilization of CDA as a treatment modality (p = 0.012) and a statistically significant increase in obese patients undergoing CDA (p < 0.0001) from 2004 to 2014. Obesity was identified as an independent risk factor associated with increased rates of inpatient neurologic complications (odds ratio [OR], 6.99; p = 0.03), pulmonary embolus (OR, 5.41; p = 0.05), and wound infection (OR, 6.97; p < 0.001) in patients undergoing CDA from 2004 to 2014.
Conclusion
In patients undergoing CDA, from 2004 to 2014, obesity was identified as an independent risk factor with significantly increased rates of inpatient neurologic complications, pulmonary embolus and wound infection. Large prospective trials are needed to validate these findings.
Keywords: Arthroplasty, Replacement, Obesity, Cervical vertebrae
INTRODUCTION
Cervical disc arthroplasty (CDA) is becoming increasingly utilized as an alternative to anterior cervical discectomy and fusion (ACDF) in the treatment of cervical degenerative disc disease. Patient selection remains crucial for satisfactory outcomes after CDA and numerous studies have been devoted to investigating the ideal radiographic and clinical findings that define the best surgical candidate. However, the current body of literature is distinctly lacking in data on how obese patients fare after CDA [1-3].
There is substantial evidence on how obese patients, those with a body mass index (BMI) greater than 30, undergoing ACDF have higher complication rates than patients undergoing ACDF with a normal BMI [4-6]. The increased complication rate is multifactorial with systemic changes playing a role but may be related to a challenging neck dissection and placement of retractors, increased retraction on critical structures, and consequently, local edema, increased blood loss, tissue ischemia, and prolonged operative time [7]. This is further supported by the findings that patients who underwent bariatric surgery within 2 years before undergoing ACDF had significantly lower pulmonary complications, renal complications, sepsis, and 90 day readmissions [8]. However, the literature on the impact of obesity specifically on CDA surgical outcomes is not well documented.
Elucidating how obesity affects outcomes after CDA is especially relevant since epidemiological studies show that patients with a high BMI are more likely to develop degenerative spine pathologies [9-11]. In cases of CDA, preliminary studies show a higher BMI has been associated with increased risk of prolonged length of stay (LOS) and hospital readmission [12]. There is also evidence showing that obese patients had lower patient reported outcome scores and patient reported improvement compared to nonobese patients for all types of cervical spine surgery performed for degenerative pathology [13].
Further examination of the relationship between BMI and CDA outcomes is necessary to understand how BMI can serve as a predictor of complications and indications for use of CDA in obese patients. Establishing this level of understanding in the literature can contribute to better patient counseling, patient outcomes, and reduced perioperative complications. Our study aims to determine the effect of obesity on CDA outcomes and postoperative complications.
MATERIALS AND METHODS
1. Data Source and Indices
The Nationwide Inpatient Sample (NIS) is the largest publicly available data source for all-payer, inpatient health care in the United States (US). This database is developed by the Healthcare Cost and Utilization Project (HCUP). Which represents a random subsample of 20% of US inpatients totaling nearly 35 million annual discharges. The Elixhauser readmission and mortality indices are validated scoring systems that identify variables in the NIS when correlated with overall patient health, mortality risk and 30 readmission risk [14,15]. The STROBE (strengthening the reporting of observational studies in epidemiology) statement was implemented for this manuscript. This study uses publicly available, deidentified data and did not require Institutional Review Board approval.
2. Definition of Cases
The NIS was evaluated from 2004 to 2014 and discharges with International Classification of Diseases (ICD-9-CM) procedure codes indicating CDA were identified as ICD-9-CM 84.60, 84.61, 84.62, and 80.52. The ICD-9-CM diagnosis codes were further delineated for obesity, 278.0x, which is defined as a BMI greater than 30.0 kg/m2. Other parameters studied include age, sex, frailty score, obesity, weekend admission status, patient income, race, Elixhauser comorbidity index, number of levels treated with disc arthroplasty and use of intraoperative monitoring [14].
3. Statistical Methods
Aggregate national estimates of yearly discharge frequencies were calculated utilizing weighted observations supplied by HCUP. For the years 2004–2011 and 2012–2014 the adjusted weights (TRENDWT) and normal weights (DISCWT) were utilized, respectively, to adjust for temporal database changes. Statistical analysis was performed with SAS 9.4 (SAS Institute Inc., Cary, NC, USA) utilizing the SURVEYMEANS, SURVEYLOGISTIC, SURVEYFREQ, and SUVERYREG procedures that account for NIS stratified-cluster sampling methodology. NIS sampling is clustered by hospital identification (HOSPID) for all years and stratified by hospital region or hospital division for the years 2004–2011 and 2012–2014, respectively.
The normality of continuous variables was assessed graphically and statistically. Continuous variables with yearly nonparametric distributions were represented as yearly weighted median estimates; whereas, those with yearly normal distributions were represented as yearly weighted mean estimates. Comparisons of means/distributions of normally continuous variables were carried out using least squared means analysis; while, nonparametric distributions were compared with a modern extension of the Wilcoxon rank-sum test that adjusts for clustering, stratification, and weights [16].
Categorical variables were presented as an estimated weighted frequency and percent. Statistical analyses of categorical variables were carried out using chi-square and Fisher exact with the Monte Carlo simulation tests, as appropriate [17]. Time trend series plots were created for the yearly incidence of ACDF-obesity patients, using GraphPad PRISM ver. 9 (GraphPad Software Inc., La Jolla, CA, USA). To yield a quantitative measurement of yearly distribution trends, yearly means/medians of continuous variables were assessed with univariable logistic regression, with year assessed separately as either a categorical or continuous variable.
Separate univariable followed by multivariable logistic regression analysis were performed for the likelihood of the following dependent inpatient outcomes: inpatient mortality, neurological deficit, dysphagia, cardiac, respiratory, hematologic, gastrointestinal, or genitourinary complications, pulmonary embolus, wound infection, hardware failure, or durotomy. All available NIS hospital, patient, Elixhauser, and economic variables were utilized as covariates. Covariates that met a significance level of p < 0.05 in the univariable analysis were included in the multivariable analysis. A backwards multivariable logistic regression was performed and only variables that met significance were included in the final model. Only the results of obesity are displayed. Only p-values of less than 0.05 were considered statistically significant.
RESULTS
From 2004 to 2014, 6,509 CDA cases were identified in the NIS. Of these cases, 582 (8.9%) were obese (Table 1). Over this time period, CDA was increasingly utilized as a treatment modality for cervical degenerative disease (p = 0.012) (Table 2). The incidence of comorbid obesity in patients undergoing CDA also increased and by 2014 patients undergoing CDA were 1.27 times more likely to have comorbid obesity in 2014 compared to 2004 (p < 0.001) (Fig. 1). Only 0.2% of patients undergoing CDA were obese in 2004 compared to 1.08% in 2014. There was no significant difference in LOS between obese patients, LOS=1.0 days, and nonobese patients, LOS=0.9 days (p = 0.562). There was no significant difference in weekend admissions, sex, socioeconomic status, or regional location within the US (Table 1). Hospital teaching status also had no significant statistical significance with regards to incidence of obesity amongst patients undergoing CDA.
Table 1.
Patient characteristics stratified for obesity for those undergoing CDA from 2004 to 2014
| Characteristic | Overall | Obese | Nonobese | p-value |
|---|---|---|---|---|
| No. of patients | 6,509 | 582 | 5,927 | |
| Female sex | 3,325 (51.28) | 300 (51.55) | 3,025 (51.26) | 0.942 |
| Age (yr) | 47.81 (55.63–41.36) | 48.79 (55.90–41.88) | 47.72 (55.61–41.33) | 0.644 |
| LOS (day) | 0.90 (1.83–0.43) | 1.00 (1.97–1.00) | 0.90 (1.83–0.43) | 0.562 |
| Weekend admission | 62 (0.95) | 10 (1.72) | 52 (0.88) | 0.33 |
| Zip code income quartile | 0.635 | |||
| $1–24,999 | 1,079 (17.00) | 94 (16.72) | 985 (17.03) | |
| $25,000–34,999 | 1,455 (22.92) | 132 (23.44) | 1,323 (22.87) | |
| $35,000–44,999 | 1,668 (26.28) | 172 (30.55) | 1,496 (25.88) | |
| $45,000 or more | 2,079 (32.76) | 155 (27.53) | 1,924 (33.26) | |
| Hospital region | 0.669 | |||
| Northeast | 1,527 (23.46) | 126 (21.65) | 1,401 (23.64) | |
| Midwest | 1,042 (16.01) | 111 (19.07) | 931 (15.71) | |
| South | 2,173 (33.38) | 205 (35.22) | 1,968 (33.20) | |
| East | 1,767 (27.14) | 139 (23.88) | 1,628 (24.47) | |
| Multilevel procedure | 4,339 (66.67) | 415 (9.56) | 3,924 (90.44) | 0.259 |
| Readmission index | 0.025 ± 0.011 | 0.11 ± 0.080 | 0.016 ± 0.009 | 0.08 |
| Mortality index | 0.018 ± 0.008 | 0.081 ± 0.057 | 0.012 ± 0.007 | 0.08 |
| Discharge disposition | 0.219 | |||
| Home | 5,800 (89.25) | 500 (8.62) | 5,300 (91.38) | |
| Other facility | 201 (3.09) | 33 (16.42) | 168 (83.58) | |
| Home health care | 498 (7.66) | 48 (9.64) | 450 (90.36) | |
| Mortality | 1 (0.02) | 0 (0) | 1 (0.02) | - |
| LOS following surgery (day) | 0.92 (1.85–0.44) | 1.00 (2.21–1.00) | 0.92 (1.84–0.44) | 0.281 |
| Race | - | |||
| White | 4,650 (99.64) | 405 (8.71) | 4,245 (91.29) | |
| African-American | 418 (8.96) | 34 (9.24) | 384 (8.96) | |
| Hispanic | 459 (9.84) | 52 (14.13) | 407 (9.47) | |
| Asian | 95 (2.04) | 0 (0) | 95 (2.21) | |
| Native American | 9 (0.19) | 0 (0) | 9 (0.21) | |
| Other | 219 (4.69) | 15 (4.08) | 204 (4.75) |
Values are presented as number (%), mean±standard deviation, or median (interquartile range).
This table shows patient characteristics of patients identified in the NIS from 2004 to 2014 that underwent CDA, a total of 6,509 cases. Of these cases, 582 (8.9%) were obese.
CDA, cervical disc arthroplasty; NIS, Nationwide Inpatient Sample; LOS, length of stay.
Table 2.
Regression analysis of CDA incidence between 2004 and 2014
| Year | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | p-value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | 43 (0.65) | 288 (4.42) | 367 (5.64) | 510 (7.84) | 726 (11.16) | 1,016 (66.67) | 812 (58.86) | 752 (56.22) | 545 (50.05) | 630 (53.44) | 820 (60.00) | 0.012 |
Values are presented as number (%).
Statistically significant increase in cervical disc arthroplasty (CDA) utilization as a treatment modality for cervical degenerative disease from 2004 to 2014.
Fig. 1.
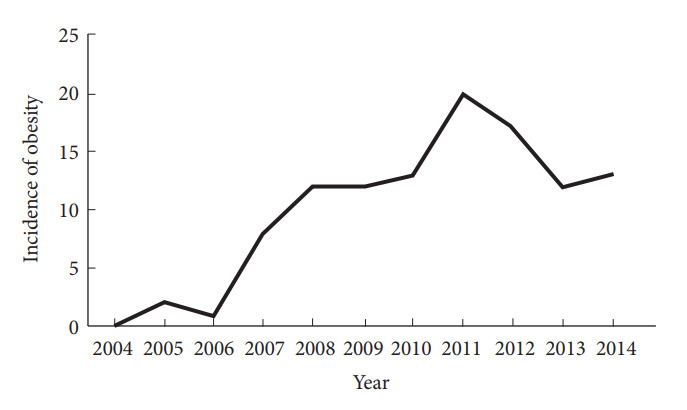
Univariable logistic regression trends of obesity incidence in cervical disc arthroplasty (CDA) patients. This figure shows graphic representation of the univariable logistic regression trends of obesity incidence in CDA patients from the years 2004 through 2014.
Univariable analysis of various complication rates and outcomes for patients that underwent CDA from 2004 to 2014, stratified by obesity, is represented in Table 3. Obese patients that underwent CDA had statistically significant increased rates of neurologic complications (1.55% vs. 0.24%, p = 0.014), pulmonary embolism (1.72% vs. 0.32%, p = 0.03), and wound infection (4.12% vs. 0.62%, p < 0.001) compared to nonobese patients, respectively.
Table 3.
Complications following CDA stratified by obesity (n=6,509)
| Variable | Overall | Obese | Nonobese | p-value |
|---|---|---|---|---|
| Neurological | 23 (0.36) | 9 (1.55) | 14 (0.24) | 0.014 |
| Respiratory | 121 (1.86) | 24 (4.12) | 97 (1.64) | 0.053 |
| Cardiologic | 15 (0.23) | 5 (0.86) | 10 (0.17) | 0.155 |
| Hematologic | 135 (2.08) | 9 (1.55) | 126 (2.13) | 0.704 |
| GI | 58 (0.89) | 5 (0.86) | 53 (0.89) | NS |
| GU | 36 (0.55) | 5 (0.86) | 31 (0.52) | NS |
| PE | 29 (0.45) | 10 (1.72) | 19 (0.32) | 0.03 |
Values are presented as number (%).
This table shows the results of univariable analysis of various complication rates and outcomes for patients that underwent CDA from 2004 to 2014, stratified by obesity.
CDA, cervical disc arthroplasty; GI, gastrointestinal; GU, genitourinary; PE, pulmonary embolus.
Obesity was found to be independently associated with higher rates of inpatient neurologic complications (OR, 6.99; p=0.03), pulmonary embolism (OR, 5.41; p = 0.05), and wound infection (OR, 6.97; p < 0.001), in patients undergoing CDA from 2004 to 2014. This data is reflected in Table 4 and is the result of separate multivariable analyses adjusted for patient age, sex, frailty score, obesity, weekend admission status, patient income, race, Elixhauser comorbidity index, hospital, and operative covariates such as number of levels treated with disc arthroplasty and use of intraoperative monitoring.
Table 4.
Adjusted effect of obesity on CDA outcomes
| Variable | OR | LL | UL | p-value |
|---|---|---|---|---|
| Neurological | 6.99 | 1.15 | 42.52 | 0.03 |
| Respiratory | 2.59 | 0.95 | 7.06 | 0.06 |
| Cardiologic | 4.85 | 0.44 | 54.13 | 0.199 |
| Hematologic | 0.76 | 0.18 | 3.242 | 0.705 |
| GI | 0.97 | 0.12 | 7.56 | 0.973 |
| GU | 1.67 | 0.199 | 14.04 | 0.637 |
| PE | 5.41 | 0.98 | 29.99 | 0.05 |
| Wound infection | 6.97 | 2.24 | 21.74 | < 0.001 |
| Hardware malfunction | 0.26 | 0.04 | 1.91 | 0.184 |
| Dysphagia | 3.39 | 0.68 | 17.08 | 0.138 |
| Durotomy | 1.31 | 0.51 | 3.39 | 0.579 |
This table shows the results of separate multivariable analyses adjusted for patient, hospital, and operative covariates to determine if obesity is independently associated with increased adverse outcomes.
CDA, cervical disc arthroplasty; OR, odds ratio; LL, lower limit; UL, upper limit; GI, gastrointestinal; GU, genitourinary; PE, pulmonary embolus.
Additionally, multivariable analysis revealed there was no statistically significant difference in respiratory (OR, 2.59; p = 0.06) or cardiologic complications (OR, 4.85; p = 0.199) between obese and nonobese patients undergoing CDA (Table 4). There was also no significant difference in reported hardware malfunction, dysphagia or durotomy between obese and nonobese patients.
DISCUSSION
Obesity is a global public health issue in the developed world. The mean BMI worldwide is increasing steadily by 0.4–0.5 kg/m2 per decade since 1980 [15], with the US having the highest prevalence in the world at 93.3 million adults (men, 35%; women, 40.4%) [16]. Over the 10-year study period, there was a significant increase in obesity incidence among the CDA population. From 2002 to 2007 CDA in the US was only performed under investigative purposes as Medtronic completed clinical trials for their Prestige Cervical Disc (Medtronic, Minneapolis, MN, USA), which received Food and Drug Administration approval in 2007. Thus, the incidence of CDA use and obesity amongst CDA patients expanded as the device was available for use outside of clinical trials [17]. This trend is expected as the US obese population continues to grow steadily [18].
Since the number of obese patients undergoing CDA has expanded in the last decade the potential negative impact on surgical outcomes in spinal surgery has become increasingly relevant. While studies in the literature show an association between obesity and an increase in mortality, hospitalization, cost, comorbidities, and postoperative complications in patients undergoing general and cardiac surgeries, these studies are often small single-center cohorts and are not specific to CDA or anterior approach for cervical surgeries [19,20]. CDA and ACDF use almost an identical approach to the anterior cervical spine. While there are no specific studies prospectively evaluating the effect of obesity on outcomes in patients undergoing CDA, there are prospective, randomized controlled studies showing that obesity leads to worse outcomes in ACDF and even more technically nuanced studies that associate obesity with more challenging neck dissection and placement of retractors, increased retraction on critical structures, and consequently, local edema, increased blood loss, tissue ischemia, and prolonged operative time, ultimately leading to worse outcomes [7]. Given that the approaches to the anterior cervical spine for CDA and ACDF are nearly identical, literature evaluating the impact of obesity in ACDF is often used to extrapolate risks for obesity in CDA. However, the procedures are not identical, and some studies have shown longer surgical times and retraction time on critical structures during multilevel CDA versus ACDF [21]. This could mean the impacts of obesity on CDA outcomes are underestimated when extrapolating from the ACDF literature since retraction time and total surgical time can be longer. Unfortunately, obesity was not evaluated as an independent risk factor in this comparative study [21]. Our study allows for the first retrospective analysis on a broad cohort of inpatients undergoing CDA and determining if obesity had an impact on outcome.
Several studies have investigated the association between BMI and functional outcomes in cervical, thoracic and lumbar spine surgery [22-26]. A meta-analysis published by Jiang et al. [5] and a large retrospective cross-sectional study of 84,607 patients published by Kalanithi et al. [22] found similar results to our study. Both studies found higher rates of wound infection and pulmonary embolism amongst obese patients undergoing spine surgery, which is consistent with the results of our study. Both studies found that obesity was a risk factor for mortality, however we did not find that association.
A study published by Perez-Roman et al. [4] evaluated the impact of obesity on ACDF outcomes using the NIS database from 2004 to 2014. Their study included 1,212,475 patients, compared to 6,509 patients in our study. They found patients undergoing ACDF in 2014 were 2.5 times more likely to be obese than those in 2004 (p < 0.001). We also found an increased incidence of obesity amongst CDA patients and in 2014 patients were 1.27 times more likely to be obese than in 2004 (p < 0.001). Both our study and the study by Perez-Roman et al. [4] found obesity to be an independent risk factor for increased rates of neurologic complications (OR, 6.99; p = 0.03 vs. OR, 1.40; p = 0.02) and pulmonary emboli (OR, 5.41; p = 0.05 vs. OR, 2.08; p < 0.001) on multivariate analysis. Both studies found significantly increased rates of wound infections in obese versus nonobese patients with 0.84% of obese ACDF patients developing wound infection (p = 0.011) [4] and 4.12% of obese CDA patients developing wound infection (p < 0.001).
Obese patient’s undergoing CDA had no statistically significant increase in incidence of dysphagia, durotomy, hardware failure, cardiac, respiratory, hematologic or genitourinary complications compared to nonobese patients undergoing CDA (Table 4). However, in the study by Perez-Roman et al. [4] obese patients undergoing ACDF had statistically significant increased rates of dysphagia (p < 0.001), durotomy (p < 0.001), hardware failure (p = 0.023), cardiac (p < 0.001), respiratory (p < 0.001), hematologic (p < 0.001), and genitourinary complications (p < 0.001) compared to nonobese patients undergoing ACDF. Both studies found no significant difference in mortality rates. The ACDF study had a much larger sample size, as ACDF was more commonly utilized during this time compared to CDA, which could explain some of these differences. However, these differences could be due to the difference in the interbody used, the lack of BMP used on CDA compared to ACDF, and the lack of anterior plating system on CDA compared to that used on ACDF. No causality can be determined from either of these types of studies but these differences could be validated and further investigated with prospective randomized controlled studies comparing obese and nonobese patients undergoing either CDA or ACDF.
There is no study specifically evaluating the impact of obesity on postoperative CDA complications, LOS, and morbidity with which to validate the findings from our study. Loidolt et al. [27] is a prospective randomized trial evaluating the differences in adverse events occurring over a 10-year period in patients that underwent ACDF and CDA. This study found no significant difference in rates of adverse events between the 2 groups. Although, this paper is excellent for understanding rates of adverse events amongst their cohort of ACDF and CDA patients, they excluded extremely obese patients from the trial and did not stratify for obesity as an independent risk factor for adverse events, thus this study cannot be used to extrapolate the rates of adverse events amongst obese patients that undergo CDA.
Malik et al. [8] in 2021 further evaluated this trend by using the Medicare Standard Analytical Files from 2007 to 2013 to assess if undergoing bariatric surgery in the 2 years prior to having an ACDF reduced complication rates. They compared patients that underwent bariatric surgery 2 years before ACDF versus obese patients that did not undergo bariatric surgery within the 2 years before undergoing ACDF. They found that there was a statistically significant reduction in pulmonary complications (OR, 0.53; p = 0.002), cardiac complications (OR, 0.69; p = 0.012), sepsis (OR, 0.69; p=0.035), renal complications (OR, 0.54; p=0.044), and 90-day readmissions (OR, 0.53; p = 0.015) in patients that had undergone bariatric surgery within 2 years before undergoing elective ACDF. A similar study using these databases specifically evaluating the impact of obesity on outcomes after CDA could further elucidate trends in national patient databases for these patients.
The retrospective nature of this study does not allow for determining causality and merely allows for determining correlation. ICD-9 coding in the NIS is subject to errors and can significantly alter the patient selection. The NIS database is an estimate of national data inpatient hospital trends and lacks the detail of retrospective or prospective patient series. It is also known that the NIS significantly underreports obesity [28]. The NIS does not include adverse events following discharge. Heterotopic ossification (HO), a known complication of CDA [29], could not be assessed in this study since there is no ICD-9 code specific to HO in the cervical spine. Using the NIS limits analysis to the immediate inpatient postoperative period following CDA. Further research with prospective randomized study, including obese patients, evaluating for obesity as an independent risk factor for adverse events in the immediate postoperative period in patients undergoing CDA would be helpful in validating our data. Ultimately, long-term prospective randomized trials assessing immediate and long-term outcomes amongst obese patients undergoing CDA is warranted.
CONCLUSION
Our study found a significant increase in the overall utilization of CDA as a treatment modality along with a significant increase in obese patients undergoing CDA (p < 0.001) from 2004 to 2014. This study demonstrates that, in patients undergoing CDA, obesity was identified as an independent risk factor with significantly increased rates of inpatient neurologic complications, pulmonary embolus and wound infection. However, unlike ACDF, obesity was not associated with a statistically significant increase in dysphagia, durotomy, hardware failure, cardiac, respiratory, hematologic or genitourinary complications for obese CDA patients [4]. Gaining a better understanding of how obesity impacts complication rates is imperative for improved patient selection and outcomes, especially since this study also found a significant increase in the utilization of CDA in obese patients over a 10-year period. Large prospective trials are needed to validate these findings.
Footnotes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: KMB, EML; Formal Analysis: VG, EML; Investigation: KMB, EML, VG; Methodology: VG, EML, KMB; Project Administration: KMB; Writing – Original Draft: KMB, KM, CB; Writing – Review & Editing: RJPR, EML, ADL.
REFERENCES
- 1.Zou S, Gao J, Xu B, et al. Anterior cervical discectomy and fusion (ACDF) versus cervical disc arthroplasty (CDA) for two contiguous levels cervical disc degenerative disease: a meta-analysis of randomized controlled trials. Eur Spine J. 2017;26:985–97. doi: 10.1007/s00586-016-4655-5. [DOI] [PubMed] [Google Scholar]
- 2.Koreckij TD, Gandhi SD, Park DK. Cervical disk arthroplasty. J Am Acad Orthop Surg. 2019;27:e96–104. doi: 10.5435/JAAOS-D-17-00231. [DOI] [PubMed] [Google Scholar]
- 3.Reinas R, Kitumba D, Pereira L, et al. Multilevel cervical arthroplasty-clinical and radiological outcomes. J Spine Surg. 2020;6:233–42. doi: 10.21037/jss.2020.01.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perez-Roman RJ, McCarthy D, Luther EM, et al. Effects of body mass index on perioperative outcomes in patients undergoing anterior cervical discectomy and fusion surgery. Neurospine. 2021;18:79–86. doi: 10.14245/ns.2040236.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jiang J, Teng Y, Fan Z, et al. Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis. Clin Orthop Relat Res. 2014;472:968–75. doi: 10.1007/s11999-013-3346-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malik AT, Jain N, Kim J, et al. The impact of metabolic syndrome on 30-day outcomes following elective anterior cervical discectomy and fusions. Spine (Phila Pa 1976) 2019;44:E282–7. doi: 10.1097/BRS.0000000000002824. [DOI] [PubMed] [Google Scholar]
- 7.Mehta AI, Babu R, Sharma R, et al. Thickness of subcutaneous fat as a risk factor for infection in cervical spine fusion surgery. J Bone Joint Surg Am. 2013;95:323–8. doi: 10.2106/JBJS.L.00225. [DOI] [PubMed] [Google Scholar]
- 8.Malik AT, Noria S, Xu W, et al. Bariatric surgery before elective anterior cervical discectomy and fusion (ACDF) in obese patients is associated with reduced risk of 90-day postoperative complications and readmissions. Clin Spine Surg. 2021;34:171–5. doi: 10.1097/BSD.0000000000001120. [DOI] [PubMed] [Google Scholar]
- 9.Nilsen TI, Holtermann A, Mork PJ. Physical exercise, body mass index, and risk of chronic pain in the low back and neck/shoulders: longitudinal data from the Nord-Trondelag Health Study. Am J Epidemiol. 2011;174:267–73. doi: 10.1093/aje/kwr087. [DOI] [PubMed] [Google Scholar]
- 10.Teraguchi M, Yoshimura N, Hashizume H, et al. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: the Wakayama Spine Study. Osteoarthritis Cartilage. 2014;22:104–10. doi: 10.1016/j.joca.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 11.Liuke M, Solovieva S, Lamminen A, et al. Disc degeneration of the lumbar spine in relation to overweight. Int J Obes (Lond) 2005;29:903–8. doi: 10.1038/sj.ijo.0802974. [DOI] [PubMed] [Google Scholar]
- 12.Zeidan M, Goz V, Lakomkin N, et al. Predictors of readmission and prolonged length of stay after cervical disc arthroplasty. Spine (Phila Pa 1976) 2021;46:487–91. doi: 10.1097/BRS.0000000000003839. [DOI] [PubMed] [Google Scholar]
- 13.Auffinger B, Lam S, Kraninger J, et al. The impact of obesity on surgeon ratings and patient-reported outcome measures after degenerative cervical spine disease surgery. World Neurosurg. 2014;82:e345–52. doi: 10.1016/j.wneu.2013.09.053. [DOI] [PubMed] [Google Scholar]
- 14.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Kaplan SA. Re: National, regional, and global trends in bodymass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. J Urol. 2011;186:1982–3. doi: 10.1016/j.juro.2011.07.061. [DOI] [PubMed] [Google Scholar]
- 16.Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315:2284–91. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Derman PB, Zigler JE. Cervical disc arthroplasty: rationale and history. Int J Spine Surg. 2020;14(s2):S5–13. doi: 10.14444/7086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief. 2017;(288):1–8. [PubMed] [Google Scholar]
- 19.Buerba RA, Fu MC, Grauer JN. Anterior and posterior cervical fusion in patients with high body mass index are not associated with greater complications. Spine J. 2014;14:1643–53. doi: 10.1016/j.spinee.2013.09.054. [DOI] [PubMed] [Google Scholar]
- 20.Moore BJ, White S, Washington R, et al. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser Comorbidity Index. Med Care. 2017;55:698–705. doi: 10.1097/MLR.0000000000000735. [DOI] [PubMed] [Google Scholar]
- 21.Fay LY, Huang WC, Tsai TY, et al. Differences between arthroplasty and anterior cervical fusion in two-level cervical degenerative disc disease. Eur Spine J. 2014;23:627–34. doi: 10.1007/s00586-013-3123-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalanithi PA, Arrigo R, Boakye M. Morbid obesity increases cost and complication rates in spinal arthrodesis. Spine (Phila Pa 1976) 2012;37:982–8. doi: 10.1097/BRS.0b013e31823bbeef. [DOI] [PubMed] [Google Scholar]
- 23.Cao J, Kong L, Meng F, et al. Impact of obesity on lumbar spinal surgery outcomes. J Clin Neurosci. 2016;28:1–6. doi: 10.1016/j.jocn.2015.10.034. [DOI] [PubMed] [Google Scholar]
- 24.Patel N, Bagan B, Vadera S, et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine. 2007;6:291–7. doi: 10.3171/spi.2007.6.4.1. [DOI] [PubMed] [Google Scholar]
- 25.Vaidya R, Carp J, Bartol S, et al. Lumbar spine fusion in obese and morbidly obese patients. Spine (Phila Pa 1976) 2009;34:495–500. doi: 10.1097/BRS.0b013e318198c5f2. [DOI] [PubMed] [Google Scholar]
- 26.Knutsson B, Michaëlsson K, Sandén B. Obesity is associated with inferior results after surgery for lumbar spinal stenosis: a study of 2633 patients from the Swedish spine register. Spine (Phila Pa 1976) 2013;38:435–41. doi: 10.1097/BRS.0b013e318270b243. [DOI] [PubMed] [Google Scholar]
- 27.Loidolt T, Kurra S, Riew KD, et al. Comparison of adverse events between cervical disc arthroplasty and anterior cervical discectomy and fusion: a 10-year follow-up. Spine J. 2021;21:253–64. doi: 10.1016/j.spinee.2020.10.013. [DOI] [PubMed] [Google Scholar]
- 28.Al Kazzi ES, Lau B, Li T, et al. Differences in the prevalence of obesity, smoking and alcohol in the United States Nationwide Inpatient Sample and the behavioral risk factor surveillance system. PLoS One. 2015;10:e0140165. doi: 10.1371/journal.pone.0140165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mehren C, Suchomel P, Grochulla F, et al. Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976) 2006;31:2802–6. doi: 10.1097/01.brs.0000245852.70594.d5. [DOI] [PubMed] [Google Scholar]


