Abstract
Peroral endoscopic myotomy (POEM) is an intervention for the treatment of achalasia which has gained popularity over the last decade. It’s efficacy and invasiveness are comparable to laparoscopic Heller myotomy (LHM). The purpose of this systematic review is to compare POEM to existing therapies. The systematic review was performed following the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. MEDLINE, EMBASE, Web of Science and Cochrane Libraries were searched using keywords: esophageal achalasia, POEM, LHM, pneumatic dilation (PD), and related terms. The studied outcomes were Eckardt score, clinical success, hospital stay, cost-utility analysis, complications, and post-treatment gastro-esophageal reflux disease. Articles were reviewed by one researcher and uncertainty was resolved by a second researcher. The search strategy retrieved 1948 citations. After removing duplicates and applying the exclusion criteria, 91 studies were selected for full-text review of which a total of 31 studies were considered eligible for further analysis, including two studies which were found through manual searching. POEM has improved efficacy compared to PD with similar cost-effectiveness. POEM results showed comparable patient outcomes when compared with laparoscopic myotomy. Overall, POEM is a feasible first-line treatment for achalasia.
Keywords: achalasia, benign esophageal diseases, dilation, diseases of the esophagus, endoscope, endoscopic mucosal resection, endoscopic submucosal dissection, endoscopic surgery, treatment
BACKGROUND
Achalasia is an esophageal motility disorder characterized by a failure of relaxation of the lower esophageal sphincter.1 Its presentation is characterized by progressive dysphagia to solids and liquids. Additional symptoms include retrosternal chest pain, regurgitation, and weight loss.2
Current pharmacological therapies have little effectiveness beyond the short term and their use is limited by significant side effects.3 Endoscopic therapies are available. Botulinum toxin can be injected into the lower esophageal sphincter. This provides better efficacy than pharmacological treatments but needs to be repeated at intervals as the effects wane.3 Pneumatic dilation (PD) involves using an endoscopic balloon to disrupt the sphincter muscle fibers with a circular force. This treatment provides good symptom relief but usually leads to recurrence.4 The disadvantage of endoscopic treatments is the need for repeated treatment.
The gold standard treatment for achalasia is laparoscopic Heller myotomy (LHM). This surgical technique involves exterior myotomy of the lower esophageal sphincter and is usually performed with an anti-reflux procedure.4 It is as effective as pneumatic dilatation and longer lasting.5,6 Peroral endoscopic myotomy (POEM) was first described in humans in 2009 and involves dissection of the lower esophageal mucosa via an endoscopic approach.7 It is thought that POEM may offer the long-term efficacy of Heller myotomy.8 This literature review aims to compare medium to long-term efficacy of POEM.
METHODS
A systematic review of the literature was undertaken following the PRISMA guidelines. MEDLINE, EMBASE, Web of Science and Cochrane Library databases were searched for POEM studies using the keywords: esophageal achalasia, POEM, LHM, PD, and related terms. Articles published from January 2008 to December 2021 in English were included using search filters. Searches were undertaken on 11 November 2021 and follow up search on 22 July 2022. Manual searching was undertaken of Pubmed database and bibliographies of included studies. Inclusion and exclusion criteria are detailed in Table 1. Papers were reviewed by one researcher and any uncertainty was resolved by a second researcher. Analysis included: (1) baseline characteristics of studies: first author, year of publication, study duration, study design, number of patients and interventions compared and (2) clinical outcomes of studies: pre- and post- Eckardt score, clinical success, hospital stay, cost-utility analysis, complications, and post-treatment GORD. Eckardt score is detailed in Table 2.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| English language | Systematic review or meta-analysis |
| Comparison of POEM and either LHM or PD | Pediatric studies |
| Adequate follow up period of at least 3 months | Robot assisted myotomy |
LHM, laparoscopic Heller myotomy; PD, pneumatic dilation; POEM, peroral endoscopic myotomy.
Table 2.
Eckardt scoring system for achalasia3
| Score | Symptom | |||
|---|---|---|---|---|
| Weight loss (kg) | Dysphagia | Retrosternal pain | Regurgitation | |
| 0 | None | None | None | None |
| 1 | <5 | Occasional | Occasional | Occasional |
| 2 | 5–10 | Daily | Daily | Daily |
| 3 | >10 | Each meal | Each meal | Each meal |
Medium-long term efficacy was defined as efficacy at greater than 12-month follow-up. Short term follow-up was defined as results obtained within the 12-months following intervention.
Critical appraisal of papers was performed to assess risk of bias using CASP tools.
RESULTS
A PRISMA flowchart of this systematic review is included in Fig. 1. Following application of inclusion and exclusion criteria and manual searching, 31 studies were included in review.
Fig. 1.
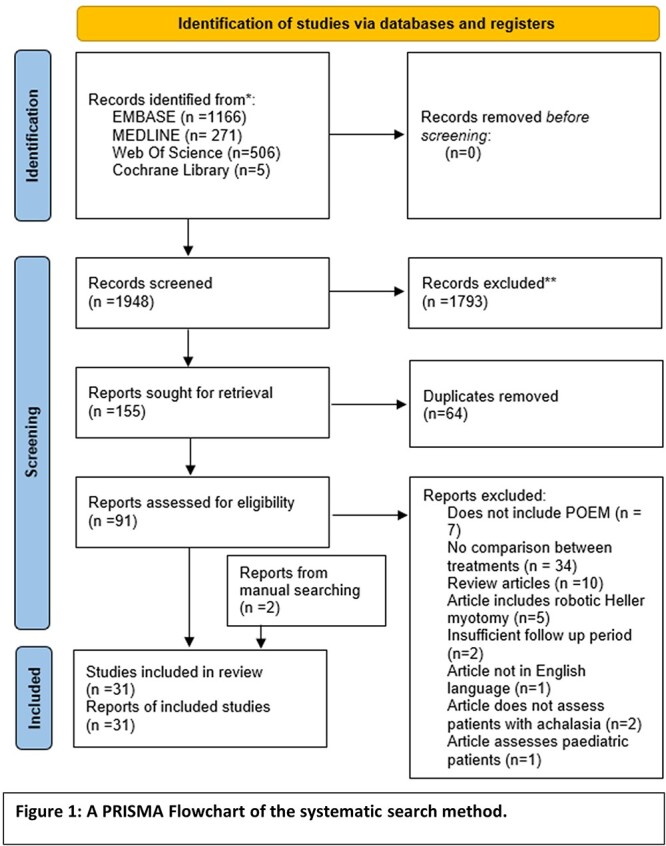
A PRISMA Flowchart of the systematic search method.
Details of each article included in the analysis are shown in Table 3. Following critical appraisal, no articles exhibited high risk of bias. Fig. 2 details the number of participants investigated in each individual study.
Table 3.
Summary of details of articles included in systematic review
| Study | Year of Publication | Country | Intervention | Duration of study (months) | Study design | Number of participants (n) |
|---|---|---|---|---|---|---|
| Akimoto et al. | 2021 | Japan | POEM vs. LHM | 278 | Retrospective | 25 |
| Attaar et al. | 2021 | USA | POEM vs. LHM | 116 | Retrospective | 159 |
| Bhayani et al. | 2014 | USA | POEM vs. LHM | 72 | Prospective | 101 |
| Chan et al. | 2016 | Hong Kong | POEM vs. LHM | 180 | Retrospective | 56 |
| Conte et al. | 2020 | Brazil | POEM vs. LHM | — | RCT | 40 |
| Costantini et al. | 2020 | Italy | POEM vs. LHM | 48 | Retrospective | 280 |
| De Pascale et al. | 2017 | Italy | POEM vs. LHM | 40 | Retrospective | 74 |
| Greenleaf et al. | 2018 | USA | POEM vs. LHM | 6 | Retrospective | 41 |
| Hanna et al. | 2018 | USA | POEM vs. LHM | 60 | Retrospective | 96 |
| Hungness et al. | 2013 | USA | POEM vs. LHM | 99 | Prospective vs. Retrospective | 73 |
| Kahaleh et al. | 2020 | International | POEM vs. LHM | 60 | Retrospective | 133 |
| Khoraki et al. | 2021 | USA | POEM vs. LHM | 39 | Public Database Searching | 11,270 |
| Kim et al. | 2019 | Korea | POEM vs. PD | 331 | Retrospective | 241 |
| Kumagai et al. | 2015 | Sweden | POEM vs. LHM | 19 | Prospective vs. Retrospective | 83 |
| Meng et al. | 2017 | China | POEM vs. PD | 44 | Retrospective | 72 |
| Miller et al. | 2017 | USA | POEM vs. LHM vs. PD vs. BI | 60 | Retrospective | 207 |
| Peng et al. | 2017 | China | POEM vs. LHM | 48 | Retrospective | 31 |
| Podboy et al. | 2021 | USA | POEM vs. LHM | 48 | Retrospective | 98 |
| Ponds et al. | 2019 | International | POEM vs. PD | 40 | RCT | 133 |
| Ramirez et al. | 2018 | Argentina | POEM vs. LHM | 69 | Prospective vs. Retrospective | 70 |
| Schneider et al. | 2016 | Sweden | POEM vs. LHM | 49 | Retrospective | 50 |
| Sudarshan et al. | 2021 | USA | POEM vs. LHM | 64 | Retrospective | 71 |
| Trieu et al. | 2021 | USA | POEM vs. LHM | 12 | Public Database Searching | 3430 |
| Ujiki et al. | 2013 | USA | POEM vs. LHM | 46 | Prospective | 39 |
| Vigneswaran et al. | 2014 | USA | POEM vs. LHM | 33 | Prospective | 8 |
| Wang et al. | 2016 | China | POEM vs. PD | 72 | Retrospective | 31 |
| Ward et al. | 2021 | USA | POEM vs. LHM | 60 | Retrospective | 100 |
| Werner et al. | 2019 | International | POEM vs. LHM | 35 | RCT | 221 |
| Wirsching et al. | 2019 | USA | POEM vs. LHM | 48 | Prospective | 51 |
| Zheng et al. | 2019 | China | POEM vs. PD | 43 | Retrospective | 66 |
LHM, laparoscopic Heller myotomy; PD, pneumatic dilation; POEM, peroral endoscopic myotomy; RCT, randomized controlled trial.
Fig. 2.

Total number of participants included in each study. Khoraki et al., 2021 and Trieu et al., 2021 were excluded from this figure due to the large scale nature of database searching.
Medium-long term efficacy
Efficacy is improved following POEM compared to pneumatic dilation,9–12 as evidenced by observation of statistically significant symptom improvements in a 133-patient randomized controlled trial (RCT)9 at 2 years and in 2 retrospective studies.10,11 In addition, statistically significant improvements in treatment success rates (100 vs. 50% with Eckardt <3) were noted in type III achalasia patients retrospectively at 1 year follow-up12.
POEM is of similar efficacy to LHM in follow-up.13–19 Comparable treatment success was observed by two RCTs13,14 on analysis of 221 and 40 patients. A retrospective analysis of 98 patients observed significantly longer time to treatment failure in POEM groups compared to LHM despite no difference in Eckardt scores at 36 months.20 Additionally, significantly improved integrated resting pressures were observed in POEM patients without reciprocal improvements in Eckardt scores following retrospective analysis of 71 patients. 21 A multicentre retrospective analysis of 133 patients noted significantly improved Eckardt and lower esophageal sphincter pressures in POEM patients.22
Short term efficacy
Efficacy is improved following POEM compared to pneumatic dilation10,11,12,23,. Significantly lower Eckardt scores were observed in POEM patients compared with patients undergoing PD in retrospective studies.10,12 Other retrospective studies observed statistically similar treatment success rates.11,23
Treatment success is comparable between POEM and LHM.14,24–33 A RCT noted no significant difference in Eckardt scores or basal LOS pressure at 6-month follow-up14. A number of prospective unrandomized studies observed comparable Eckardt scores at follow-up.24–26 These findings were reflected in retrospective analyses.27–33 Comparable barium esophagogram measurements of column height and percentage esophageal emptying were observed in another study.29
Complications and re-treatment
Complication rates are comparable following POEM and PD.11,23 In the studies that assessed this, cumulatively there was one adverse event in the POEM groups compared to zero in the PD groups and there was no statistically significant difference in complication rates.
Complication rates are higher following POEM compared with LHM.13,16–20,22,24,29–31,33,34,36 A database search of over 3000 admissions in the USA noted no difference in adverse events.34 However, a similar study of over 11,000 patients found significantly higher rates of adverse events following POEM compared with LHM35. An RCT from Brazil observed statistically higher complication rates following POEM compared with LHM (64.3 vs. 35.7%).14 A larger RCT noted no statistically significant difference in complication rates following intervention with POEM compared with LHM13. A number of non-randomized studies concluded that complication rates in POEM and LHM were comparable.16–20,22,24,29–31,33,36
PD has higher rates of symptom recurrence than POEM, leading to higher rates of re-treatment.9,10,12 Significantly higher rates of re-treatment were noted in a multicentre RCT (PD = 46%, POEM = 8%).9 This was mirrored in a retrospective study from Korea (PD = 45.2%, POEM = 7.8%).10 Another retrospective study noted significantly more PD patients experienced symptom recurrence compared to POEM patients at 36 months (40% vs. 7%).12
LHM and POEM lead to comparable symptom recurrence and re-treatment rates.18,20,28,33 Significantly higher rates of re-intervention were noted in LHM patients compared to POEM patients in a multicentre retrospective analysis (40% vs. 14%).22 A number of retrospective studies noted no statistically significant difference in treatment failure rates or re-treatment.18,20,28,33
Gastro-oesophageal reflux disease
POEM may lead to higher rates of gastro-esophageal reflux disease (GORD) symptoms than PD.9,11 A multicentre RCT observed significantly higher rates of GORD symptoms in POEM patients at 24-month follow-up (41 vs. 7%).9 A retrospective analysis observed comparable ‘classical’ GORD symptoms but significantly higher rates of mild heartburn in POEM patients 12 months after treatment.11 Another retrospective analysis noted comparable rates of GORD symptoms greater than 24 months post-treatment.12
POEM leads to higher rates of GORD symptoms after treatment compared with LHM.13,14,16,19,30 Significantly higher rates of GORD symptoms were noted in POEM patients combined with significantly more cases of endoscopic esophagitis at 24-month follow-up in a large RCT (Odds ratio 2.00).13 Another RCT observed significantly higher rates of esophagitis symptoms and endoscopy findings in POEM patients.14 A retrospective analysis noted significantly higher rates of esophagitis on endoscopy that was not reflected in reported GORD symptoms.19 A small retrospective analysis of patients who had previously undergone a LHM with fundoplication observed higher rates of GORD symptoms in POEM patients despite an existing anti-reflux procedure.30 Despite this, a number of observational analyses found comparable rates of GORD symptoms between the groups.15,16,18,20,24,26,28,29,32,33
Cost-effectiveness
POEM leads to significantly higher treatment-associated costs than PD, but the cost-effectiveness of PD diminishes over time.23,37 A retrospective financial analysis in the USA concluded that PD was significantly more cost-effective than POEM initially, but that cost-effectiveness became comparable after 4 years due to retreatment.37 A retrospective analysis of 31 patients observed significantly higher hospitalization costs per patient for POEM compared to PD ($2620.3 vs.$1212.6, P value <0.001).23
POEM is similar to LHM in terms of cost-effectiveness.17,24,35,37,38 An American retrospective analysis concluded that POEM incurred significantly fewer total charges compared to LHM30. However, database searching of over 3000 admissions found significantly higher charges assigned to POEM patients than LHM patients.34 A similar study of over 11,000 patients noted comparable associated costs.35 This finding was reflected in a number of other studies.17,24,37,38 Conte et al.14 reported a small RCT which found significantly higher cost-per-patient in the POEM group compared to the LHM group.
Length of hospital stay
Length of stay is statistically significantly shorter following PD than POEM.12 A retrospective analysis of 72 patients in China noted significantly shorter length of stay in PD patients post procedure (3 days vs. 8 days).
POEM results in shorter length of hospital stay compared to LHM.14,16,20,26–28,38 A randomized controlled trial found significantly shorter length of stay in the POEM cohort (3.7 days vs. 5.4 days, P value = 0.009).14 Multiple retrospective studies found that significantly shorter hospital stay was seen after POEM compared with LHM (2 days vs. 3 days, P value <0.001),16 (1 day vs. 2 days),27 (2 days vs. 3 days, P value = 0.0014).19 Similar findings of shorter hospital stay in POEM were noted in a number of other observational studies.20,22,26,28,38 Other observational studies have reported no difference in stay.25,29,31,33,35,36
DISCUSSION
POEM results in a marked improvement in achalasia symptoms following treatment with benefit for an extended length of time.9–12,23 Effective symptom improvement has been evidenced in studies with large cohorts.9,10 This improvement appears to be especially beneficial in type III achalasia patients, the subtype that poses significant difficulties in treatment.10,12,39 Additionally, this improvement in treatment success is not accompanied by an increased likelihood of adverse events. This suggests POEM is a safe and effective treatment compared to pneumatic dilation.
Furthermore, POEM appears to be more likely to result in long lasting benefit without the need to undergo additional intervention.9,10,12 Significantly, almost half of PD patients experienced symptom recurrence during follow-up that required retreatment, compared to fewer than 10% of POEM patients. However, it appears that POEM patients go on to experience post-operative symptoms of gastro-esophageal reflux.9 The findings in this study may be accounted for by the use of a single session of pneumatic dilatation compared to the accepted practice of graded dilatations.9 It is understood that treatment related costs are higher in POEM.40,41 However, dedicated financial analysis concluded that cost-effectiveness of PD reduces to comparable levels due to the requirement for serial dilations.37 It can be deduced that POEM is a superior choice than PD due to the superior efficacy, particularly in the long term, and relative cost-effectiveness. Once initial costs of equipment sourcing are covered, superior patient outcomes can be obtained for costs similar to pneumatic dilation.37
Treatment of achalasia with POEM results in equivalent patient outcomes when compared to LHM. Patient outcomes at all timepoints appear to be comparable.13–19,24–33 This finding includes patients with type III achalasia where comparable patient outcomes were noted.13,15 It appears that the safety of POEM is not inferior to that of LHM.34,35 The finding of a significantly higher rate of recurrent symptoms in LHM patients compared to POEM in a multicentre analysis is contrasted by converse findings in a randomized controlled trial.14,22
POEM patients do experience GORD symptoms. This finding was highlighted by significantly higher rates of patient reported symptoms and endoscopic findings of esophagitis.13,14 Despite the presence of an existing anti-reflux procedure, POEM still leads to esophageal reflux and associated symptoms.30,42 These symptoms may be manageable conservatively compared to symptoms of achalasia through the use of proton pump inhibitors.43,44 POEM does not demand significantly higher funding than LHM and results in comparable cost-effectiveness.35,37 These findings suggest that POEM is non-inferior to LHM in terms of symptom relief and recurrence, and the increased development of GORD can be controlled medically.
It should be noted that POEM and LHM require significant skill and experience to be carried out effectively.45,46 Studies suggest comparable learning curves for these techniques. Due to the relatively uncommon nature of these interventions, many institutions may not see benefit in adoption of these as first line treatments due to the timeframe of training.
A number of limitations are present in this study. Most study designs included are retrospective without matching, introducing the possibility of bias. This may be improved in future literature as POEM is adopted as a treatment standard and randomization of treatment is justified. Few of the included studies undertook follow-up of POEM patients beyond 24 months, this was often compared to longer follow-up in LHM and PD patients leading to potential missed recurrence in POEM patients. Financial implications were considered in this study, however, no formal economic model was formulated.
Future recommendations include further RCTs to compare the outcomes of POEM compared to LHM/PD with reduced chance of bias. Additionally, long term follow-up of current studies would be beneficial to investigate the extended long-term outcomes of POEM. Further, review of the literature in pediatric and teenage cases may be beneficial as this age group would be most impacted by long-term post-operative esophageal reflux.
CONCLUSIONS
This review has compared the clinical outcomes of achalasia patients following POEM procedure compared to PD or LHM patients. POEM has improved efficacy compared to PD with similar cost-effectiveness. POEM results in comparable patient outcomes compared to LHM. POEM patients do experience an increased rate of post-operative GORD. However, this can be managed effectively medically long-term. Further RCTs into this topic may result in confirmation of these findings and lead to adoption of POEM as a standard treatment for achalasia in patients that can tolerate general anesthetic.
Author contributions
Nila Tewari (Writing—review & editing).
Financial support: None
Conflicts of interest: The authors declare that they have no conflict of interest.
Contributor Information
Adam North, Warwick Medical School, University of Warwick, Coventry, UK.
Nilanjana Tewari, General Surgery Department, University Hospitals of Derby and Burton, Derby, UK.
References
- 1. Richter J E. Oesophageal motility disorders. Lancet 2001; 358(9284): 823–8. [DOI] [PubMed] [Google Scholar]
- 2. Patel D A, Lappas B M, Vaezi M F. An overview of achalasia and its subtypes. Gastroenterol Hepatol (N Y) 2017; 13(7): 411–21. [PMC free article] [PubMed] [Google Scholar]
- 3. Arora Z, Thota P N, Sanaka M R. Achalasia: current therapeutic options. Ther Adv Chronic Dis 2017; 8(6–7): 101–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rolland S, Paterson W, Bechara R. Achalasia: current therapeutic options. Neurogastroenterol Motil 2023; 35(1): e14459. [DOI] [PubMed] [Google Scholar]
- 5. Boeckxstaens G E, Annese V, Des Varannes S B et al. Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. N Engl J Med 2011; 364(19): 1807–16. [DOI] [PubMed] [Google Scholar]
- 6. Moonen A, Annese V, Belmans A et al. Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut 2016; 65(5): 732–9. [DOI] [PubMed] [Google Scholar]
- 7. Inoue H, Minami H, Satodate H, Kudo S-E. First clinical experience of submucosal endoscopic myotomy for esophageal achalasia with no skin incision. Gastrointest Endosc 2009; 69(5): AB122. [Google Scholar]
- 8. Kohn G. Peroral endoscopic myotomy for achalasia—a review. Ann Laparosc Endosc Surg 2019; 4: 4. [Google Scholar]
- 9. Ponds F A, Fockens P, Lei A et al. Effect of peroral endoscopic myotomy vs pneumatic dilation on symptom severity and treatment outcomes among treatment-naive patients with achalasia: a randomized clinical trial. JAMA 2019; 322(2): 134–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kim G H, Jung K W, Jung H Y et al. Superior clinical outcomes of peroral endoscopic myotomy compared with balloon dilation in all achalasia subtypes. J Gastroenterol Hepatol 2019; 34(4): 659–65. [DOI] [PubMed] [Google Scholar]
- 11. Zheng Z, Zhao C, Su S et al. Peroral endoscopic myotomy versus pneumatic dilation - result from a retrospective study with 1-year follow-up. Z Gastroenterol 2019; 57(3): 304–11. [DOI] [PubMed] [Google Scholar]
- 12. Meng F, Li P, Wang Y et al. Peroral endoscopic myotomy compared with pneumatic dilation for newly diagnosed achalasia. Surg Endosc 2017; 31(11): 4665–72. [DOI] [PubMed] [Google Scholar]
- 13. Werner Y B, Hakanson B, Martinek J et al. Endoscopic or surgical myotomy in patients with idiopathic achalasia. N Engl J Med 2019; 381(23): 2219–29. [DOI] [PubMed] [Google Scholar]
- 14. Conte T M, Haddad L B P, Ribeiro I B, de Moura E T H, DʼAlbuquerque L A C, De Moura E G H. Peroral endoscopic myotomy (POEM) is more cost-effective than laparoscopic Heller myotomy in the short term for achalasia: economic evaluation from a randomized controlled trial. Endosc Int Open. 2020; 8(11): E1673–E80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ward M A, Clothier J S, Ebrahim A, Ogola G O, Leeds S G. Comparison of objective intermediate-term outcomes between per-oral endoscopic myotomy and laparoscopic Heller myotomy show equivalence. Surg Innov 2021; 28(3): 295–302. [DOI] [PubMed] [Google Scholar]
- 16. Costantini A, Familiari P, Costantini M et al. Poem versus laparoscopic Heller myotomy in the treatment of esophageal achalasia: a case-control study from two high volume centers using the propensity score. J Gastrointest Surg 2020; 24(3): 505–15. [DOI] [PubMed] [Google Scholar]
- 17. Hanna A N, Datta J, Ginzberg S, Dasher K, Ginsberg G G, Dempsey D T. Laparoscopic Heller myotomy vs per oral endoscopic myotomy: patient-reported outcomes at a single institution. J Am Coll Surg 2018; 226(4): 465–72.e1. [DOI] [PubMed] [Google Scholar]
- 18. Peng L, Tian S, Du C, Yuan Z, Guo M, Lu L. Outcome of peroral endoscopic myotomy (POEM) for treating achalasia compared with laparoscopic Heller myotomy (LHM). Surg Laparosc Endosc Percutan Tech 2017; 27(1): 60–4. [DOI] [PubMed] [Google Scholar]
- 19. de Pascale S, Repici A, Puccetti F, Carlani E, Rosati R, Fumagalli U. Peroral endoscopic myotomy versus surgical myotomy for primary achalasia: single-center, retrospective analysis of 74 patients. Dis Esophagus 2017; 30(8): 1–7. [DOI] [PubMed] [Google Scholar]
- 20. Podboy A J, Hwang J H, Rivas H et al. Long-term outcomes of per-oral endoscopic myotomy compared to laparoscopic Heller myotomy for achalasia: a single-center experience. Surg Endosc 2021; 35(2): 792–801. [DOI] [PubMed] [Google Scholar]
- 21. Sudarshan M, Raja S, Adhikari S et al. Peroral endoscopic myotomy provides effective palliation in type III achalasia. J Thorac Cardiovasc Surg 2022; 163(2): 512–9.e1. [DOI] [PubMed] [Google Scholar]
- 22. Kahaleh M, Tyberg A, Suresh S et al. How does per-oral endoscopic myotomy compare to Heller myotomy? The Latin American perspective. Endosc Int Open 2020; 8(10): E1392–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wang X, Tan Y, Lv L et al. Peroral endoscopic myotomy versus pneumatic dilation for achalasia in patients aged ≥ 65 years. Rev Esp Enferm Dig 2016; 108(10): 637–41. [DOI] [PubMed] [Google Scholar]
- 24. Wirsching A, Boshier P R, Klevebro F et al. Comparison of costs and short-term clinical outcomes of per-oral endoscopic myotomy and laparoscopic Heller myotomy. Am J Surg 2019; 218(4): 706–11. [DOI] [PubMed] [Google Scholar]
- 25. Ujiki M B, Yetasook A K, Zapf M, Linn J G, Carbray J M, Denham W. Peroral endoscopic myotomy: a short-term comparison with the standard laparoscopic approach. Surgery 2013; 154(4): 893–7 discussion 7-900. [DOI] [PubMed] [Google Scholar]
- 26. Bhayani N H, Kurian A A, Dunst C M, Sharata A M, Rieder E, Swanstrom L L. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 2014; 259(6): 1098–103. [DOI] [PubMed] [Google Scholar]
- 27. Attaar M, Su B, Wong H J et al. Comparing cost and outcomes between peroral endoscopic myotomy and laparoscopic Heller myotomy. Am J Surg 2021; 222(1): 208–13. [DOI] [PubMed] [Google Scholar]
- 28. Ramirez M, Zubieta C, Ciotola F et al. Per oral endoscopic myotomy vs. laparoscopic Heller myotomy, does gastric extension length matter? Surg Endosc 2018; 32(1): 282–8. [DOI] [PubMed] [Google Scholar]
- 29. Kumagai K, Tsai J A, Thorell A, Lundell L, Håkanson B. Per-oral endoscopic myotomy for achalasia. Are results comparable to laparoscopic Heller myotomy? Scand J Gastroenterol 2015; 50(5): 505–12. [DOI] [PubMed] [Google Scholar]
- 30. Akimoto S, Yano F, Omura N et al. Redo laparoscopic Heller myotomy and dor fundoplication versus rescue peroral endoscopic myotomy for esophageal achalasia after failed Heller myotomy: a single-institution experience. Surg Today 2021; 52: 401–7. [DOI] [PubMed] [Google Scholar]
- 31. Vigneswaran Y, Yetasook A K, Zhao J C, Denham W, Linn J G, Ujiki M B. Peroral endoscopic myotomy (POEM): feasible as reoperation following Heller myotomy. J Gastrointest Surg 2014; 18(6): 1071–6. [DOI] [PubMed] [Google Scholar]
- 32. Schneider A M, Louie B E, Warren H F, Farivar A S, Schembre D B, Aye R W. A matched comparison of per oral endoscopic myotomy to laparoscopic Heller myotomy in the treatment of achalasia. J Gastrointest Surg 2016; 20(11): 1789–96. [DOI] [PubMed] [Google Scholar]
- 33. Chan S M, Wu J C, Teoh A Y et al. Comparison of early outcomes and quality of life after laparoscopic Heller's cardiomyotomy to peroral endoscopic myotomy for treatment of achalasia. Dig Endosc 2016; 28(1): 27–32. [DOI] [PubMed] [Google Scholar]
- 34. Trieu J A, Dua A, Enofe I, Shastri N, Venu M. Population trends in achalasia diagnosis and management: a changing paradigm. Dis Esophagus 2021; 34(5): 1–6. [DOI] [PubMed] [Google Scholar]
- 35. Khoraki J, Campos G M, Alwatari Y, Mazzini G S, Mangino M J, Wolfe L G. Perioperative outcomes of inpatient laparoscopic Heller myotomy and per-oral endoscopic myotomy in the United States. Surgery 2021; 171: 1263–72. [DOI] [PubMed] [Google Scholar]
- 36. Hungness E S, Teitelbaum E N, Santos B F et al. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 2013; 17(2): 228–35. [DOI] [PubMed] [Google Scholar]
- 37. Miller H J, Neupane R, Fayezizadeh M, Majumder A, Marks J M. POEM is a cost-effective procedure: cost-utility analysis of endoscopic and surgical treatment options in the management of achalasia. Surg Endosc 2017; 31(4): 1636–42. [DOI] [PubMed] [Google Scholar]
- 38. Greenleaf E K, Winder J S, Hollenbeak C S, Haluck R S, Mathew A, Pauli E M. Cost-effectiveness of per oral endoscopic myotomy relative to laparoscopic Heller myotomy for the treatment of achalasia. Surg Endosc 2018; 32(1): 39–45. [DOI] [PubMed] [Google Scholar]
- 39. Salvador R, Costantini M, Zaninotto G et al. The preoperative manometric pattern predicts the outcome of surgical treatment for esophageal achalasia. J Gastrointest Surg 2010; 14(11): 1635–45. [DOI] [PubMed] [Google Scholar]
- 40. Chue K M, Teh J L, So J B Y. Per-oral endoscopic myotomy (POEM) for achalasia: techniques, outcomes and clinical applications. Surgery Open Digestive Advance 2021; 1: 100007. [Google Scholar]
- 41. Bright T. Pneumatic balloon dilatation for achalasia—how and why I do it. Ann Esophagus 2020; 3(25): 1–4. [Google Scholar]
- 42. Tang Y, Xie C, Wang M, Jiang L, Shi R, Lin L. Association of high-resolution manometry metrics with the symptoms of achalasia and the symptomatic outcomes of peroral esophageal myotomy. PloS One 2015; 10(9): e0139385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sandhu D S, Fass R. Current trends in the management of gastroesophageal reflux disease. Gut Liver 2018; 12(1): 7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Iwakiri K, Kinoshita Y, Habu Y et al. Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2015. J Gastroenterol 2016; 51(8): 751–67. [DOI] [PubMed] [Google Scholar]
- 45. El Zein M, Kumbhari V, Ngamruengphong S et al. Learning curve for peroral endoscopic myotomy. Endosc Int Open 2016; 4(5): E577–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yano F, Omura N, Tsuboi K et al. Learning curve for laparoscopic Heller myotomy and dor fundoplication for achalasia. PloS One 2017; 12(7): e0180515. [DOI] [PMC free article] [PubMed] [Google Scholar]


