Abstract
Background
Displacement is a psychologically stressful event. Since the war began, the people of Tigray were subjected to stressful events such as torture, rape, the killing of a family member, forced displacement, and even ethnic cleansing in their home countries. Especially displaced individuals are faced mental health problems. This study aimed to assess the prevalence of depression and associated factors among community internally displaced people due to the war on Tigray, in 2021.
Methods
The community-based cross-sectional study design was applied from August 06 to 30, 2021 in all Weredas of Tigray. A total of 1,990 cIDP were recruited through a two-stage sampling technique. A structured and standardized questionnaire was used to collect data. Both bivariate and multivariable logistic regression was applied to identify associated risk factors and AOR with 95% confidence interval was used to select statistically significant variables.
Results
The prevalence of depression among internally displaced people was 81.2% (95% CI: 79.4–83%), with more than 60% categorized as moderate and severe depression. The married and divorced marital status, being government employee, having family size > = 4, destruction of household fixed assets, looting of cereals, and having disabled family members due to the war were the significantly associated risk factors of depression.
Conclusions
The prevalence of depression among community internally displaced people during the war on Tigray is very high compared to other studies conducted elsewhere. Almost 8 of 10 IDPs are developed depression and this is a very series health issue that needs immediate intervention by local, international organizations and communities around the world.
Keywords: Depression, War, IDP, Tigray
Background
War causes significant displacement of people due to the destruction of homes, environment, religious places, political persecution, and economic necessity. Internally displaced persons (IDPs) are persons who have been forced to flee their homes or places of usual residence as a result of armed conflicts, situations of generalized violence, violations of human rights, and disasters but remain within the borders of their own country. The number of internally displaced persons in the world has been increasing from time to time as a result of human-made or natural disasters [1, 2]. In 2022, more than 100 million people were displaced globally and 52.3% of them are internally displaced persons as a consequence of war and violence. The mass majority of the IDPs were from low-and middle-income countries [3].
Displacement is a psychologically stressful event [4]. The displaced individuals may be subject to stressful events such as torture, rape, assassination, and even ethnic cleansing in their home countries and throughout their journey [5]. Displaced survivors who experienced multiple war events perceived multiple negative effects of war on their life domains related to individuals who lived in war areas [6, 7]. Considering the effects, displacement may be accepted as a public health problem and a type of disaster, as it may lead to loss of resources, economic uncertainty, absence of health services and education, insouciant compensation for fundamental human requirements, and disintegration of public structure [5, 8]. IDPs, mainly those affected by wars, are in high danger of mental health problems. The frequently stated psychological responses are depression as a response to loss [2, 9, 10].
In different epidemiological surveys and studies on the psychopathology of war survivors depression is among the most prevalent mental health problems [5, 11]. Depression affects about 121 million people internationally. And it is one of the highest causes of disability globally [12]. Across different studies, the prevalence rates of depression and other mental health problems among war-affected populations vary widely. The prevalence of depression among people affected by armed conflicts ranges between 2.3 to 80% [5]. Studies conducted in Turkey and Afghanistan indicated that the prevalence of depression was 5% and 38.5% respectively [5]. The literature revealed that aggravating factors associated with depression among IDPs were factors such as gender, marital status, a distance of displacement, experiencing a lack of food or water, and experiencing sexual abuse [6, 13].
As a result of the war that began between the Tigray regional government and the Ethiopia federal government on Nov 04/2020, an estimated 2.1 million Tigreans have been internally displaced from their homes and over 61,000 Tigreans including children and women arrived in eastern Sudan days after the war [14–16]. Internally Displaced Persons (IDPs) are among the hardest hit by the war, most of who are hosted by the community while others are living in crowded collective centers [17]. As IDPs have left their homes forcibly they are less accessible by the international humanitarian agencies. They are in a more desperate situation than even refugees and remain at the forefront of the humanitarian agenda.
The war was waged by the Ethiopian government forces, Eritrean government forces, Amhara regional state special forces, and Amhara militia, against the regional government of Tigray [18, 19]. In Tigray's war, the non-combatant population had been agonized and tortured, were murdered and humiliated extensively in mass, were forcefully displaced with the abduction of their properties, battered, became forced laborers, sexually slaved (women and girls were raped in groups, raped in front of their families and relatives, the soldiers were inserting foreign bodies like nails, stones, sponges and other foreign substances into their genitalia) [17, 20–25].
The war in Tigray resulted in millions of displacements, starvation (due to the full blockade of humanitarian aid), and many thousand deaths. Due to that intolerable exposure to different stressors, mental health problems may last and affect the community at large. Even though there are high rates of IDPs due to the war in Tigray and the level of depression was not studied yet. Thus, this study aimed to assess the level of depression and associated factors among Community hosted Internally Displaced Persons (cIDPs) due to the war crisis in Tigray.
Methods
Study setting and design
This study was conducted using a community-based cross-sectional study design from August 06 to 30, 2021 in Tigray. Tigray was a regional state of Ethiopia that bordered with Amhara and Afar regions of Ethiopia in the south, Eritrea in the north and east, and Sudan in the west. Based on the USAID 2021 report Tigray had 2.1 million internally displaced persons due to the war launched by the government of Ethiopia [15].
Study population
The study population of this study was all households (HH) heads of community hosted internally displaced persons hosted in a community of all zones of Tigray except the western zone. But HH heads who were not available after twice check-ups were excluded from the study and replaced with a nearby household of cIDPs.
Sample size and sampling technique
The sample size was calculated based on the double proportion formula using the assumption of previously conducted studies with the variable of 'seriously injured'; with an odds ratio of 1.4, 60.8% percent of not seriously injured due to the war, and 1.5 design effect, and 5% non-response rate. Based on the assumption, the minimum sample size was 1,990 [13].
Two-stage sampling techniques were applied to select study participants. The sampling frame of households was received from the social affairs of the districts and towns. After selecting those households that hosted cIDPs, the displaced family's heads were interviewed for the assessment. When there were two or above family members in the same hosting HH, one family member was selected based on randomly.
Data collection tool and technique
The interviewer-administered structured and standardized questionnaire was used to collect the data at the household level by trained data collectors and supervisors. The questionnaire had four parts: socio-demographic, economy-related questions, health-related questions, and a checklist for MDD based on the criteria of the Diagnostic Statistical Manual for Mental Health Disorders (DSM-IV). PHQ-9 checklist has nine items, each of which offers four response choices ranging from not at all (scores 0 points) to nearly every day (scores 3 points) with a total score of 27 [12, 26]. And the tool (PHQ-9) is validated in Ethiopia and showed good internal (Cronbach's alpha = 0.85) and test re-test reliability (intra-class correlation coefficient = 0.92) [27].
Variables and measurements
The outcome variable of this study was having depression which was measured using PHQ-9 with a 3-point severity scale over the last two weeks. Based on the validated standard of PHQ-9 score ≥ 5 is considered to meet the symptom of depression. The instrument was incorporated with the Diagnostic and Statistical Manual for mental disorder version IV (DSM-IV) depression criteria with other leading depression symptoms into a brief self-report tool [12, 26, 27].
The independent variables were also, Socio-demographic characteristics: Age, marital status, educational status, occupation, and displaced family size; Economic-related variables: condition of fixed Assets, property loss during the war, shortage/Lack of necessities, looting of domestic animals, looting of Machineries/ House commodities and looting of cereals; Health-related variables: Losing contact with a family member, death of family member due to war, family member faced disability and family member experienced acute health problem.
Internally displaced persons are those who are displaced from their residential areas in Tigray due to the war in other areas within Tigray [28, 29].
Data processing and analysis
After finishing data collection and coding, the data were entered using Epi-data 3.1 and then exported to SPSS V-26 for cleaning and analysis. First, descriptive analysis was done for the sociodemographic factors, economic factors, and health condition of the family using frequency with percentages and graphs for categorical variables. To determine the level of depression, respondents were categorized into no depression (scored less than 5 denoted “zero”) and having depression (scored more than or equal to 5 denoted “1”). The severity of depression was also ordered from minimum depression to severe depression denoted from “1” to “5” respectively.
Binary logistic regression was applied for identifying associated factors with depression. Variables that had < 0.25 P-value in bivariate analysis were entered into a multivariable logistic regression analysis to identify the associated independent variables. To minimize the effect of confounders, multi-Collinearity was checked by a variance inflation factor (VIF), and those with a VIF of < 10 was included. The fitness of the model was tested by Hosmer and Lemeshow's goodness-of-fit test and the value was 0.809. Finally, an Adjusted odds ratio (AOR) with a 95% confidence interval was used to show the strength of the association and a P-value < 0.05 was taken to declare the statistical significance of a variable.
Ethical consideration
Ethical clearance was obtained from Mekelle University, College of Health Science Ethical Review Board on August 2, 2021, with IRB Ref: MU-IRB 1908/2021. The Ethics committee has also approved the informed verbal consent of participants. For those who can not read and write, the informed consent form was read to them by the interviewer and then requested to sign using finger stamp self-ink. Additional support letter from Tigray Health Bureau, woreda health offices, and verbal consent from the participant was assured before actual data collection. The HH heads and other eligible study participants were communicated and verbal consent was obtained before the data collection. To protect the participants, no individual identifying information was collected.
Results
Socio-demographic characteristics
A total of 1,965 participants were interviewed in this survey study with a response rate of 98.7%. The median age of the participants was 31 (IQR = 14) and more than half (55.3%) were female participants. Regarding the marital status and religion of the family head of displaced people who were hosted within the community of Tigray; 69% of them were married and 98% were orthodox Christianity followers (Table 1).
Table 1.
Socio-demographic characteristics of cIDP due to the war crisis of Tigray, 2021 (n = 1,965)
| Variables | Category | No Depression | With Depression |
|---|---|---|---|
| Age of HH head in Years | < 20 | 45 (36.3%) | 79 (63.7%) |
| 21–35 | 213 (19.2%) | 899 (80.8%) | |
| 36–50 | 87 (15.6%) | 469 (84.4%) | |
| > 50 | 22 (14.3%) | 132 (85.7%) | |
| Address of HH head | Southern | 24 (16.4%) | 122 (83.6%) |
| South-eastern | 25 (23.8%) | 80 (76.2%) | |
| Mekelle | 29 (31.2%) | 64 (68.8%) | |
| Eastern | 55 (17.4%) | 261 (82.6%) | |
| Central | 52 (28.1%) | 133 (71.9%) | |
| North-western | 61 (17.9%) | 279 (82.1%) | |
| Western | 110 (14.9%) | 630 (85.1%) | |
| Sex of HH head | Male | 173 (19.7%) | 703 (80.3%) |
| Female | 194 (17.9%) | 889 (82.1%) | |
| Marital Status of HH head | Single | 113 (26.4%) | 315 (73.6%) |
| Married | 228 (17%) | 1114 (83%) | |
| Divorced/Widowed | 27 (15.3%) | 149 (84.7%) | |
| Educational Status of HH head | No formal education | 27 (15.8%) | 144 (84.2%) |
| Primary | 96 (17.8%) | 444 (82.2%) | |
| Secondary | 136 (21.5%) | 498 (78.5%) | |
| College + | 49 (15.1%) | 276 (84.9%) | |
| The religion of HH head | Orthodox | 364 (19%) | 1551 (81%) |
| Muslim | 2 (5.1%) | 37 (94.9%) | |
| Occupation of HH head before displacement | Farmer | 48 (16%) | 252 (84%) |
| Gov’t employee | 57 (15.8%) | 303 (84.2%) | |
| Private employee | 19 (18.6%) | 83 (81.4%) | |
| Merchant & Investor | 108 (18.3%) | 485 (81.7%) | |
| Daily labor | 42 (17.1%) | 203 (82.9%) | |
| Othera | 92 (25.8%) | 264 (74.2%) |
ano job, student, housewife
Prevalence of depression
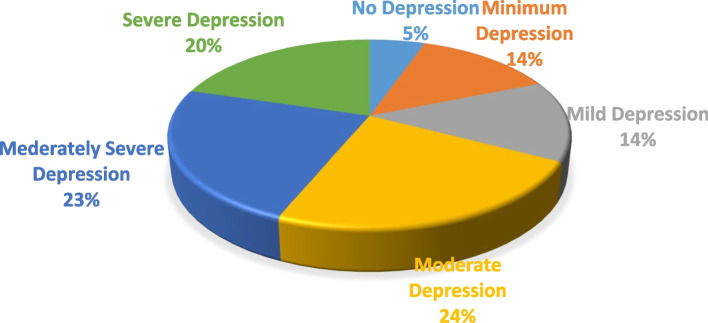
The prevalence of depression was 1,596 [ 81.2% (95% CI: 79.4–83%)]. Regarding the severity of depression; according to DSM-V classification around 67% of the participants were classified as having moderate to severe depression (Fig. 1).
Fig. 1.
Classification of depression based on severity among cIDP due to war crisis in Tigray, 2021 (n = 1,965)
The median estimated monetary value of looted and destroyed properties was 100,000 (IQR = 309,469) ETB. Around half 49.2% and 51.9% of the displaced population hosted in the community had family sizes of 4–6 and 5–8 respectively. Seventy-three percent of fixed assets and 65.6% of cereals were looted (by Eritrean, Ethiopian, and Amhara troops) during this war crisis. Among displaced Family sizes accounting 4–6 and > 6, 84.6% and 89.3% had depression consequently. From participants who have faced their fixed assets destroyed/burnt 87.7% of them developed depression. As participants' time stayed increased in months the prevalence of depression increased by 79.9%, 80.3%, and 81.5% respectively for < 4 months, 4 – 6 months, and > 6 months stay displaced in IDPs (Table 2).
Table 2.
Level of depression and economic-related factors among cIDPs of Tigray due to the war crisis in Tigray, 2021 (n = 1,965)
| Variable | Category | No Depression | With Depression |
|---|---|---|---|
| Displaced Family Size | 1–3 | 215 (24.5%) | 664 (75.5%) |
| 4–6 | 114 (15.4%) | 624 (84.6%) | |
| > 6 | 18 (10.7%) | 150 (89.3%) | |
| Family size of host HH | 1–4 | 145 (20.1%) | 578 (79.9%) |
| 5–8 | 161 (18.3%) | 719 (81.7%) | |
| 9–12 | 17 (18.1%) | 77 (81.9%) | |
| How is the condition of your fixed asset | Normal | 49 (27.7%) | 128 (72.3%) |
| Destroyed/Burnt | 34 (12.3%) | 243 (87.7%) | |
| Looted | 185 (15.1%) | 1040(84.9%) | |
| Length of time stayed displaced in IDP | < 4 month | 42 (20.1%) | 167 (79.9%) |
| 4 – 6 months | 47 (19.7%) | 191 (80.3%) | |
| > 6 month | 278 (18.5%) | 1228(81.5%) | |
| Shortage/Lack of necessities | No | 33 (31.4%) | 72 (68.6%) |
| Yes | 134 (15.7%) | 719 (84.3%) | |
| Looted property during the war | Yes | 248 (16.1%) | 1295(83.9%) |
| No | 119 (29.2%) | 289 (70.8%) | |
| Looted domestic animals | No | 83 (19%) | 354 (81%) |
| Yes | 32 (10.3%) | 279 (89.7%) | |
| Looted Machine/ house commodities | No | 23 (19%) | 98 (81%) |
| Yes | 86 (14.1%) | 523 (85.9%) | |
| Looted cereals | No | 196 (30.5%) | 447 (69.5%) |
| Yes | 156 (12.7%) | 1072(87.3%) | |
| The estimated monetary value of looted/damaged properties in ETB | < = 35,000 | 71 (16.9%) | 348 (83.1%) |
| 35,001–100,000 | 79 (18.9%) | 340 (81.1%) | |
| 100,00–344469 | 56 (14.7%) | 324 (85.3%) | |
| > = 344,470 | 47 (11.6%) | 359 (88.4%) |
Regarding the health status-related questions; Eighty-two percent of family members whose family had separated had depression, while around 86.1% of participants who had lost contact with family members had depression. Also, out of the participants who had lost family members, 87.2 had developed depression (Table 3).
Table 3.
Level of depression and health status-related factors among cIDPs of Tigray due to the war crisis in Tigray, 2021 (n = 1,965)
| Variables | Category | No-Depression | Have Depression |
|---|---|---|---|
| Separated family members | No | 270 (19.1%) | 1146 (80.9%) |
| Yes | 95 (18.1%) | 429 (81.9%) | |
| Lost contact with Family members | No | 321 (20.1%) | 1273 (79.9%) |
| Yes | 39 (13.9%) | 241 (86.1%) | |
| Family member death (n = 1882) | No | 340 (20.2%) | 1346 (79.8%) |
| Yes | 25 (12.8%) | 171 (87.2%) | |
| Family member faced disability | No | 343 (20.5%) | 1331 (79.5%) |
| Yes | 13 (8.6%) | 139 (91.4%) | |
| Family members with medical illnesses | No | 305 (19.7%) | 1247 (80.3%) |
| Yes | 43 (14%) | 265 (86%) | |
| Family members experience new health problems | No | 298 (21.2%) | 1105 (78.8%) |
| Yes | 54 (12.8%) | 369 (87.2%) |
Factors associated with depression
Multiple factors were associated with depression in bivariate analysis. Variables with p < 0.25 were entered into the multivariable analysis (Table 4). In multivariable analysis, married respondents of IDP had 1.43 times (AOR = 1.43 95% CI 1.07–1.91) and divorced/widowed had 1.77 times (AOR = 1.77 95% CI 1.08–2.91) higher rate of depression than single respondents. Government employees were two times (AOR = 2.02 95% CI 1.27–3.2) more depressed compared to farmers. Similarly, daily laborers were 2.01 times (AOR = 2.01 95% CI 1.21–3.32) more depressed compared to farmers. Displaced people with family sizes 4–6 and > 6 family size was more depressed (AOR = 1.39 95% CI 1.05–1.83) and (AOR = 1.85 95% CI 1.07–3.2) respectively than those who have less than three family members. Participants with destroyed fixed assets (AOR = 1.75 95% CI 1.03–2.98) and looted cereals (AOR 2.12 95% CI 1.59–2.84) were more depressed than their counterparts. At last, cIDP who had a family member that faced disability due to the war crisis were 2.58 times (AOR = 2.58 95% CI 1.4–4.74) more depressed than those who didn’t face this problem (Table 4).
Table 4.
Factors associated with depression among cIDPs of Tigray due to the war crisis in Tigray, 2021 (n = 1,965) (n = 1,965)
| Variable name | Category | COR (CI-95%) | AOR (CI-95%) |
|---|---|---|---|
| Age of family head (Year) | < 20 | 1 | 1 |
| 21–35 | 2.4(1.62–3.57) *** | 1.2(0.72–1.85) | |
| 36–50 | 3.07(1.99–4.23) *** | 2.7(1.81–4.28) | |
| > 50 | 3.42 (1.91–6.11) *** | 2.36(1.23–4.17) | |
| Marital status | Single | 1 | 1 |
| Married | 1.75(1.35–2.67) *** | 1.43(1.07–1.91) * | |
| Divorced/Widowed | 1.98 (1.25–3.14) ** | 1.77(1.08–2.91) * | |
| Educational Status | No Formal Education | 1 | 1 |
| Primary | 0.87(0.54–1.38) | 1.8(0.54–1.76) | |
| Secondary | 0.69 (0.44–1.08) | 0.93(0.65–1.54) | |
| College and + | 1.06 (0.63–1.76) | 2.1(1.23–3.68) | |
| Occupation | Farmer | 1 | 1 |
| Gov’t Employee | 1.01(0.67–1.54) | 2.02(1.27–3.2) ** | |
| NG-Employee | 0.83(0.46–1.5) | 1.7(0.9–3.23) | |
| Merchant | 0.86(0.59–1.24) | 1.35(0.9–2.04) | |
| Daily laborer | 0.92(0.59–1.45) | 2.01(1.21–3.32) ** | |
| Other | 0.55(0.37–0.81)** | 1.18(0.76–1.83) | |
| Displaced family size | 1–3 | 1 | 1 |
| 4–6 | 1.77(1.38–2.28) *** | 1.39(1.05–1.83) * | |
| > 6 | 2.7(1.62–4.51) *** | 1.85(1.07–3.2) * | |
| Condition of Fixed Asset | Normal | 1 | 1 |
| Destroyed | 2.74(1.68–4.45) *** | 1.75(1.03–2.98) * | |
| Looted | 2.15(1.5–3.1) *** | 1.37(0.9–2.09) | |
| Shortage/Lack of necessities | No | 1 | 1 |
| Yes | 2.46(1.57–2.86) *** | 1.86(1.25–3.32) | |
| Property loss during the war | No | 1 | 1 |
| Yes | 2.15(1.67–2.77) *** | ||
| Looted domestic animals | No | 1 | 1 |
| Yes | 2.04(1.32–3.16) ** | 1.57(0.97–2.56) | |
| Looted Machineries/ House commodities | No | 1 | 1 |
| Yes | 1.43(0.86–2.37) | 1.5(0.86–2.63) | |
| Looted Cereals | No | 1 | 1 |
| Yes | 3.01(2.38–3.82) *** | 2.12(1.59–2.84) *** | |
| Lost contact with a family member | No | 1 | 1 |
| Yes | 1.56(1.09–2.23) * | 1.09(0.83–2.42) | |
| A family member died due to war | No | 1 | 1 |
| Yes | 1.73(1.12–2.67) * | 1.38(0.87–2.2) | |
| Family members faced disability | No | 1 | 1 |
| Yes | 2.76(1.54–4.92) ** | 2.58(1.4–4.74) ** | |
| A family member experienced an acute health problem | No | 1 | 1 |
| Yes | 1.84(1.35–2.52) *** | 1.38(0.99–1.92) |
COR Crude odds ratio, AOR Adjusted odds ratio, CI Confidence interval and 1: reference group
*p < 0.05, **p < 0.01, ***p < 0.001
Discussion
Based on this study, the overall prevalence of depression was found 81.2%. The factors significantly associated with the outcome variable were married and divorced marital status, being government employee, having family size > = 4, destruction of fixed assets, looting of cereals, and injury of a family member/s.
The finding of this study showed that the overall prevalence of depression among community-hosted internally displaced persons was 81.2%. This result is higher compared to the study conducted in different countries such as: 30.7% in Uganda [29], 50% in South Sudan [30], 59% in Somali [31], 38.3% in Southeast Ethiopia [32], 37.8% in Eritrean Refugees [33], and 26.4% in a pooled prevalence of 81 studies done using a systematic study [34]. In this study, this might be due nature/severity of the war and exposure to double burden/impact which are; facing different difficulties as a result of the war (death/injury to oneself or a family member, being displaced from their original area, losing their properties…) and being unable to even get humanitarian aid from government and international community that would help them survive for some time due to the complete siege put on Tigray [18, 19]. The high prevalence of depression among the sampled population sounds for structured interferences to deal with mental health problems. And also it implies the need for more study (preferably qualitative) on the mental health issues in this population.
Regarding factors associated with depression, divorced/widowed /married displaced household heads were more depressed than single ones. This finding is similar to the study done in Uganda [13] and Southern Sudan [30]. This might be due to having additional responsibility and thinking about family members and other household administrations. In addition to this, they are more vulnerable to facing financial problems since they lost their properties, have no cash, no electricity, no transport, no communication, and other public infrastructures that help the daily survival life of them and their families [25, 31, 34, 35].
The other significant factor associated with depression was the occupational status of the cIDPs. Unemployment is also more associated with depression according to some studies done on Somali refugees [36], and Eritrean refugees [32]. In this study government employees and daily labourers were more depressed than farmers. This is a unique finding which might be due to the absence of salary and the deliberate closing of banks making it hard for government employees to even access what they had in their accounts, and their source of money/expenditure; not having it, especially when they have a family to take care of, makes it hard for them and puts them in a depressive state. Similarly, due to the current absence of construction or other jobs which require labor, the absence of transactions at the previous level. In general, may the war made it hard for daily laborers to feed themselves and their families and puts them in depression [23].
Family size was also found to be a significant factor for depression in this study, those with 4 or more family sizes were more depressed than those who had less family size, this is still believed to be associated with financial issues i.e. the bigger family size they have the more they are going to struggle with financial issues; which is hard due to the complete siege that there was no banks, no communication lines, no sufficient resources for daily utility use throughout Tigray. In addition to this, there was not farming during the whole war period, no transport in and out of Tigray and the uncertainty about for how long it is going to last worries the people.
In addition to this, cIDPs who were looted of their cereals, destructed of their fixed assets, and lost of their property were found to be associated with depression. This finding is consistent with a study done in Croatia [6]. This is obvious that, where ever in the world a person lives, as a human being, it is hard when one loses everything they have worked for and their home in a blink of an eye due to the war they didn't expect. Displacement deteriorates health outcomes, increase loss of employment, and inability to access public services. This may result in hopelessness and loss of one's direction.
Injury of family members due to the war in Tigray was also another factor associated with depression. This is similar to studies done in Northern Uganda [13], Islamabad-Pakistan [33], and Croatia [6] where war stressors like being seriously injured or having a close family member who got injured or experiencing the death of close persons were found to be associated with depression. Even though resilience and how a person deals with a stressful situation; hence whether a person becomes depressed as a result of stressors differs from one person to another, it's no surprise that one might develop symptoms of depression as a result of lasting injuries of trauma more compared to those who were in a war situation but didn't experience such lasting effects of the war.
Strengths and limitations of the study
This study was done in the all woredas/districts of Tigray (with a large sample size) at the community level and this may have external validity and generalization for internal and other IDPs globally. However, as a limitation of this study; since the study was cross-sectional it doesn't create a temporal causal relationship between the outcome variable with the significant factors. Also, this study focused on interviewing only the HH heads of the cIDPs so the other members were not interviewed which might have underestimated the finding of the study.
Conclusions
The prevalence of depression among community internally displaced people during the war on Tigray is very high compared to other studies conducted elsewhere. Almost 8 out of 10 IDPs developed depression and this is a very series health issue and needs immediate psycho-social health intervention by local and international organizations with the collaboration of governmental and non-governmental institutions based on the study's findings.
Acknowledgements
Mekelle University College of Health Science, Tigray Bureau of Health, supervisors, data collectors, and study participants are acknowledged for their cooperation and support.
Guidelines statement
All methods were carried out in accordance with relevant guidelines and regulations.
Abbreviations
- cIDPs
Community hosted Internally Displaced Persons
- HH
Households
- PHQ
Patient Health Questionnaire
- SPSS
Statistical Package for Social Sciences
- CI
Confidence interval
- DSM
Diagnostic Statistical Manual for mental health disorder
- IQR
Inter Quartile Range
- MDD
Major Depressive Disorder
- TBH
Tigray Bureau of Health
- VIF
Variance Inflation Factor
Authors’ contributions
AG is the first author of this study who conceptualized of the study, providing methodology, study investigation, funding acquisition, validation, and writing of the manuscript. AT, FS, LM, TG, KT, AGG, KG, and SG contributed on supervision, data collection, recruited study participants, data analysis, and writing of the manuscript. FT was the senior and corresponding author who provide high-level feedback and critically reviewed the manuscript. In the end, all authors have read and approved the manuscript.
Funding
Tigray Bureau of Health was the funder of this study. The sponsor of the study had no role in study design, data collection, data analysis, or interpretation, but provided certain training materials, organized the training, and did review this report before submission for publication. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Availability of data and materials
All the data supporting the findings is contained within the manuscript, when there is in need the data set used for the present study's conclusion can be accessible from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from Mekelle University, College of Health Science Ethical Review Board on August 2, 2021, with IRB Ref: MU-IRB 1908/2021. Additional support letters from the Tigray Bureau of Health, woreda health offices, and verbal consent from the participant were assured before actual data collection. The HH heads and other eligible study participants were communicated and verbal consent was obtained before the data collection. To protect the participants, no individual identifying information was collected.
Verbal informed consent from the participant were assured before the actual data collection and Mekelle University, College of Health Science Ethical Review Board. For those who cannot read and write, the informed consent form was read to the participants by the interviewer and then requested to sign using finger stamp self-ink.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Owoaje ET, Uchendu OC, Ajayi TO, Cadmus EO. A review of the health problems of the internally displaced persons in Africa. Niger Postgrad Med J. 2016;23(4):161–171. doi: 10.4103/1117-1936.196242. [DOI] [PubMed] [Google Scholar]
- 2.Global Protection Cluster (GPC). Handbook for the Protection of Internally Displaced Persons. 2010. Available at: https://www.refworld.org/docid/4790cbc02.html. Accessed 12 Nov 2023.
- 3.Madoro D, Kerebih H, Habtamu Y, G/Tsadik M, Mokona H, Molla A, Wondie T, Yohannes K. Post-traumatic stress disorder and associated factors among internally displaced people in South Ethiopia: a cross-sectional study. Neuropsychiatr Dis Treat. 2020;16:2317–26. doi: 10.2147/NDT.S267307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Essizoglu A, Keser I. Post-traumatic stress disorder in internally displaced people subjected to displacement by armed forces. J Trauma Stress Disor Treat. 2014;3(2):2–6. [Google Scholar]
- 5.Mahmood, Ibrahim Post-traumatic stress disorder and depression among Syrian refugees residing in the Kurdistan region of Iraq. Confl Health. 2019;13:51. doi: 10.1186/s13031-019-0238-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Letica-Crepulja M, Salcioglu E, Frančišković T, Basoglu M. Factors associated with posttraumatic stress disorder and depression in warsurvivors displaced in Croatia. Croat Med J. 2011;52(6):709–717. doi: 10.3325/cmj.2011.52.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rieder H, Elbert T. Rwanda–lasting imprints of a genocide: trauma, mental health and psychosocial conditions in survivors, former prisoners and their children. Confl Heal. 2013;7(1):1–3. doi: 10.1186/1752-1505-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bapolisi AM, Song SJ. Post-traumatic stress disorder, psychiatric comorbidities and associated factors among refugees in Nakivale camp in southwestern Uganda. BMC Psychiatry. 2020;20:53. doi: 10.1186/s12888-020-2480-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.International Committee of the Red Cross, internal displacement in armed conflict facing up to the challenges. 2009. https://www.icrc.org/en/doc/assets/files/other/icrc_002_4014.pdf. Accessed 12 Nov 2023.
- 10.Cohen R. The guiding principles on internal displacement: a new instrument for international organizations and NGOs. Forced Migration Rev. 1998;2:31–33. [Google Scholar]
- 11.Richards A, Ospina-Duque J, Barrera-Valencia M, Escobar-Rincón J, Ardila-Gutiérrez M, Metzler T, Marmar C. Posttraumatic stress disorder, anxiety and depression symptoms, and psychosocial treatment needs in Colombians internally displaced by armed conflict: a mixed-method evaluation. Psychol Trauma Theory Res Pract Policy. 2011;3(4):384. doi: 10.1037/a0022257. [DOI] [Google Scholar]
- 12.Steel JL, Dunlavy AC, Stillman J, Pape HC. Measuring depression and PTSD after trauma: common scales and checklists. Injury. 2011;42(3):288–300. doi: 10.1016/j.injury.2010.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roberts B, Ocaka KF, Browne J, Oyok T, Sondorp E. Factors associated with post-traumatic stress disorder and depression amongst internally displaced persons in northern Uganda. BMC Psychiatry. 2008;8:1–9. doi: 10.1186/1471-244X-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.UNHCR Ethiopia Operation, UNHCR Situation Update Ethiopia, Tigray 30 July 2021. 2021. https://reliefweb.int/report/ethiopia/unhcr-ethiopia-operation-tigray-situation-update-30-july-2021. Accessed 12 Nov 2023.
- 15.USAID, Ethiopia – Tigray Crisis September 30, 2021. 2021. https://www.usaid.gov/sites/default/files/2022-05/2021_09_30_USG_Tigray_Fact_Sheet_11.pdf. Accessed 12 Nov 2023.
- 16.Worl Food Program, WFP Ethiopia Tigray Emergency Response Situation Report # 1 Month WFP Food and Nutrition Assistance Supply Chain. 2021. https://www.wfp.org/emergencies/ethiopia-emergency.
- 17.UNHCR Ethiopia Operation: Tigray Situation Update. 2021. https://reliefweb.int/report/ethiopia/unhcr-ethiopia-operation-tigray-situation-update-06-september-2021.
- 18.Human Rights Watch, “We Will Erase You from This Land” Crimes Against Humanity and Ethnic Cleansing in Ethiopia’s Western Tigray Zone. 2022. https://www.hrw.org/report/2022/04/06/we-will-erase-you-land/crimes-against-humanity-and-ethnic-cleansing-ethiopias.
- 19.Amnesty International, “We will erase you from this land” crimes against humanity and ethnic cleansing in Ethiopia’s Western Tigray zone. 2022. https://www.hrw.org/report/2022/04/06/we-will-erase-you-land/crimes-against-humanity-and-ethnic-cleansing-ethiopias.
- 20.Fisaha Tesfay, Hailay Gesesew. The health crisis in Ethiopia's war-ravaged Tigray. Ethiopian Insight. 2021. https://www.ethiopia-insight.com/2021/02/24/the-health-crisis-in-ethiopias-war-ravaged-tigray/. Accessed 12 Nov 2023.
- 21.Unicef, Situation analysis of children and women: Tigray Region. 2020. https://www.unicef.org/ethiopia/media/2351/file/Tigray%20region%20.pdf.
- 22.UNHCR Ethiopia Operation, Ethiopia situation (Tigray region) 1 March – 15 March. 2021. https://reliefweb.int/report/ethiopia/unhcr-ethiopia-operation-tigray-situation-update-31-march-2021?gad_source=1&gclid=CjwKCAiA6byqBhAWEiwAnGCA4NCwlu7MiodQEBk1ghDKVi8cTu9kSwKj_NN0K1zo99C-raBa8lXwQBoCHOQQAvD_BwE.
- 23.D’Costa B. Tigray’s complex emergency, expulsions and the aspirations of the responsibility to protect. Global Responsib Protect. 2022;14(1):5–11. doi: 10.1163/1875-984X-14010004. [DOI] [Google Scholar]
- 24.UNHCR Ethiopia Operation, UNHCR Situation Update Ethiopia, Tigray 06 September 2021. 2022. https://reliefweb.int/report/ethiopia/unhcr-ethiopia-operation-tigray-situation-update-06-september-2021?gad_source=1&gclid=CjwKCAiA6byqBhAWEiwAnGCA4Cz_-wCGO6KcQIytizEtLGJ-G69HkUex8e5-D1YNoJ73CbcMTu9JGBoCM_gQAvD_BwE.
- 25.World Vision, Assessment of Internally displaced people in Tigray. 2021.
- 26.Roehr B. American psychiatric association explains DSM-5. BMJ. 2013;346. https://www.bmj.com/content/346/bmj.f3591. [DOI] [PubMed]
- 27.Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, Wondimagegn D, Lemenhe A, Fann JR, Vander Stoep A, Zhou XH. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013;210(2):653–661. doi: 10.1016/j.psychres.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Phuong C. The International Protection of Internally Displaced Persons (Cambridge Studies in International and Comparative Law). Cambridge: Cambridge University Press; 2005. 10.1017/CBO9780511494062.
- 29.Deng F. Internally Displaced Persons: Report of the Representative of the UN Secretary-General, Mr. Francis Deng. Commission on Human Rights, January 1994. Int'l J. Refugee L.. 1994;6:291. https://heinonline.org/HOL/LandingPage?handle=hein.journals/intjrl6&div=42&id=&page=. Accessed 12 Nov 2023.
- 30.Roberts B, Ocaka KF, Browne J, Oyok T, Sondorp E. Factors associated with the health status of internally displaced persons in northern Uganda. J Epidemiol Community Health. 2009;63(3):227–232. doi: 10.1136/jech.2008.076356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ali M, Mutavi T, Mburu JM, Mathai M. Prevalence of posttraumatic stress disorder and depression among internally displaced persons in Mogadishu-Somalia. Neuropsychiatr Dis Treat. 2023;19:469–78. doi: 10.2147/NDT.S398423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frontières MS. People left with few healthcare options in Tigray as facilities looted, destroyed. Médecins Sans Frontières. 2021. Available: https://www.MSF.org/health-facilities-targeted-tigray-region-Ethiopia2021. Accessed 12 Nov 2023.
- 33.OCHA, Northern Ethiopia - Humanitarian Update Situation Overview Last updated: 3 Mar 2022. 2022. https://reliefweb.int/report/ethiopia/ethiopia-northern-ethiopia-humanitarian-update-situation-report-3-mar-2022. Accessed 12 Nov 2023.
- 34.Bedaso A, Duko B. Epidemiology of depression among displaced people: a systematic review and meta-analysis. Psychiatry Res. 2022;311:114493. doi: 10.1016/j.psychres.2022.114493. [DOI] [PubMed] [Google Scholar]
- 35.Roberts B, Damundu EY, Lomoro O, Sondorp E. Post-conflict mental health needs: a cross-sectional survey of trauma, depression and associated factors in Juba. Southern Sudan BMC psychiatry. 2009;9(1):1. doi: 10.1186/1471-244X-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gesesew H, Berhane K, Siraj ES, Siraj D, Gebregziabher M, Gebre YG, Gebreslassie SA, Amdeslassie F, Tesema AG, Siraj A, Aregawi M. The impact of war on the health system of the Tigray region in Ethiopia: an assessment. BMJ Glob Health. 2021;6(11):e007328. doi: 10.1136/bmjgh-2021-007328. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data supporting the findings is contained within the manuscript, when there is in need the data set used for the present study's conclusion can be accessible from the corresponding author upon reasonable request.