Abstract
Purpose of review
Poor diet and food insecurity contribute to the dramatic rise in diet-related chronic disease and increasing cost of healthcare. The Food as Medicine (FAM) framework describes food-based interventions designed to prevent, manage, and treat diet-related diseases. However, FAM interventions have not been widely implemented or evaluated in pediatric populations, so critical questions remain about their optimal delivery and design, efficacy, and funding opportunities. We have reviewed the recent literature and offer insights into potential funding and implementation strategies for pediatric healthcare providers.
Recent findings
Data from adult and population-level interventions provide evidence that FAM interventions positively impact diet quality, food security, health outcomes, and healthcare utilization and cost in adults and households with children. Evidence from recent pediatric-based FAM interventions and population data from recent changes to federal nutrition programs support the use of food-based interventions to improve child diet quality, food insecurity, and potentially impact long-term health and healthcare utilization and cost.
Summary
Applying the entire spectrum of evidence-based FAM interventions in pediatric settings from prenatal to adolescent stages will offer the greatest opportunity to ensure all children have access to enough healthful food so they can achieve their highest potential in life.
Keywords: diet quality, diet-related chronic disease, food insecurity, health-related social needs, nutrition security
INTRODUCTION
A background on food and nutrition security
In addition to managing clinical disease, healthcare providers – who for the purposes of this review include individual clinicians, health systems, and health insurance systems – may play a critical role in addressing a variety of health-related social needs. One social need that can have a serious impact on health is food insecurity, which occurs when the household struggles to afford adequate quality and quantity of food for every person in the household to live an active, healthy life [1]. Households that experience food insecurity may progress and cycle through a series of maladaptive coping behaviors related to stress responses, food purchasing, and adaptation of consumption patterns. An early coping stage of food insecurity is food anxiety, and preoccupation with food access, along with mental distress. Subsequently, the family may begin purchasing cheaper, convenient, and highly-palatable foods to stretch dollars, decrease stress, limit waste, and ease decision making [2–4]. These coping strategies often result in an overall reduction in food quality and variety. Lastly, adult members of the household will cope by decreasing the quantity of food eaten to off-set the limited availability of food. Eventually, children begin decreasing food consumption as well. The toxic impacts of food insecurity likely contribute toward the higher risk of developing chronic conditions in those exposed to food insecurity [5]. In 2022, rates of food insecurity were significantly higher than the previous year, at 12.8% of United States (US) households and 17.3% of households with children [1]. In children, food insecurity is associated with poor diet quality [6], poor health [7], excess healthcare utilization [8,9], and lower cognitive performance [10]. Also, households experiencing food insecurity have approximately $2400 greater annual healthcare expenditures versus households experiencing food security [11▪]. Given the strong association between food insecurity and child health, it is critical that healthcare providers screen for food insecurity as part of routine care delivery, provide interventions to address food insecurity for patients, and advocate for resources to address food insecurity to improve pediatric health from birth into adulthood [12].
Although quality nutrition has always been a part of definitions of food insecurity, recently, the United States Department of Agriculture has defined “nutrition security” as the consistent accessibility, availability, and affordability of foods that promote well being [13]. Nutrition security is an important consideration because the majority of U.S. children do not consume the recommended amount of fruits or vegetables [14]. Additionally, 70% of calories consumed by all children are ultra-processed foods [15] which are associated with an increased cardiometabolic and mental health risk [16]. The past two decades have seen an alarming rise in rates of diet-related chronic diseases in U.S. children, with the rates of type 2 diabetes among children doubling to a prevalence of 0.67 per 1000 [17], the rate of overweight and obesity increasing to 35% [18], and nearly 10% of children now having elevated blood pressures [19]. Considering poor diet and obesity in childhood often continue into adulthood, and the cost of diet-related chronic diseases in adults is estimated to be over 1 trillion annually [20], there is great motivation to improve child nutrition to prevent and reverse diet-related chronic disease risk in children.
Box 1.
no caption available
A background on federal nutrition programs and their impact on child nutrition and health
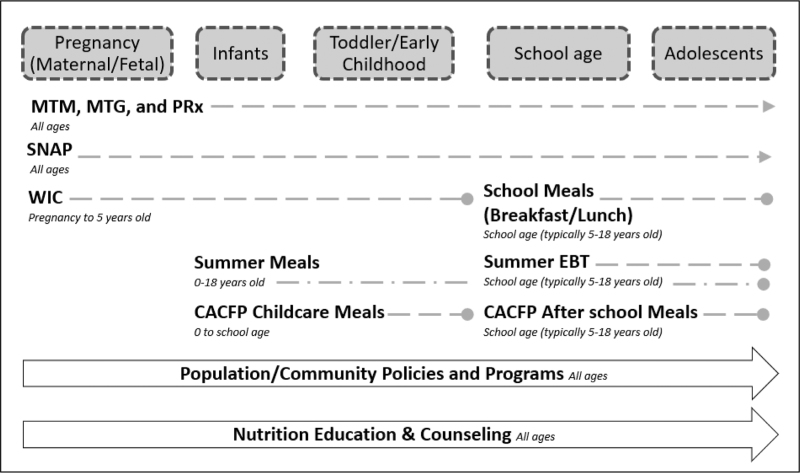
FNPs play an essential role in supporting food and nutrition security and are a powerful tool for disease prevention. FNPs offer support across the pediatric age continuum, including Supplemental Nutrition Assistance Program (SNAP) for all ages, the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) from prenatal to 5 years old, and school meals programs, including the School Breakfast Program and the National School Lunch Program, covering all school-age children (which typically begins around 5 years old), and the Child and Adult Care Food Program (CACFP) and Summer Nutrition programs supporting children 0--18 years old (see Fig. 1).
FIGURE 1.
Food as Medicine Pediatric Implementation Continuum. This figure highlights the robustness of the pediatric nutrition safety net with its overlapping and complementary array of programs. In the pediatric setting, various Food as Medicine interventions can be implemented across the age continuum, from the prenatal period into late adolescence (dashed lines). There are opportunities for overlap with more than one FNPs (e.g., WIC and Summer meals) and ideally no gaps in access to FNPs (e.g., between WIC discontinuation and eligibility for School Meals), and if there are gaps, other programs can fill in (such as Summer or CACFP meals). In addition to FNPs, access to MTMs, MTGs, and PRx can offer a supplemental source of nutrition and vital nutrition education. Lastly, ongoing advocacy efforts should prioritize policies and programs that secure greater access FAM interventions and to the pediatric nutrition safety net. CACFP, Child and Adult Care Food Program; MTG, Medically Tailored Groceries; MTM, Medically Tailored Meals; PRx, Produce Prescriptions; SNAP, Supplemental Nutrition Assistance Program; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Supplemental Nutrition Assistance Program
SNAP use in households with children is associated with improvements in healthy food access [21], academic achievements [22], and self-reported health and excess healthcare use in adults [23]. Enrolling in SNAP has also been associated with healthcare cost savings of 16–21% within the first 2 years of SNAP participation [24▪▪]. While SNAP serves approximately 97% of eligible children [25], there is a clear gap in enrollment and use, particularly in immigrant populations [26]. Additionally, once enrolled, allotment amounts are often inadequate to support a family throughout the entire month, potentially leading to maladaptive coping strategies and negative health consequences [27,28]. Increases in SNAP purchasing power, such as through increases in SNAP allotments or incentive programs like Double Up Bucks, help reduce food insecurity, improve diet quality [29▪,30] and health outcomes [31], and provides food autonomy and dignity of choice [32].
Special supplemental program for women, infants, and children
Decades of research support the relationship between participation in WIC and higher diet quality, better pregnancy and childhood health, and higher academic achievement [33,34▪]. WIC serves 53% of all infants born in the USA, but enrollment drops significantly to 57% for 1-year-olds and even further to 24% for 4-year-olds [35]. This large drop-off has negative nutritional [36▪] and food security [37▪] implications on families. Increases in WIC funding, changes in allowable items in 2009 and 2020, WIC farmers market incentive programs, and the increased WIC Cash Value Benefits all provide evidence that greater access to produce through WIC may improve household consumption of nutrient rich foods.
School meals
School breakfast and lunch may provide more than half a child's daily calorie intake and are considered to be the most nutritious meals many children consume [38]. Federal waivers allowed schools to offer all students meals at no charge throughout the pandemic, resulting in increased participation in both school breakfast and lunch. However, during the 2022–2023 school year, most schools returned to the traditional, tiered-eligibility system and school meal participation significantly dropped to 88%. Furthermore, 54% of public schools nationwide reported a decrease in both breakfast and lunch school meal participation [39]. Declining and partial participation in school meal programs hinders students’ access to healthful foods, particularly fruits and vegetables.
Child and adult care food program
An estimated 60% of children under 6 years-old attend approximately 27 h per week of child care, making daycares an important venue for healthy meals. The CACFP program offers meals in after school programs and in daycare settings for young children. School and daycare participation in CACFP meals is associated with higher diet quality and food security [40▪]. Daycare centers that participate in CACFP must adhere to federal nutrition guidelines based on the Dietary Guidelines for Americans that support a greater variety of produce, whole grains, lean proteins, and low-fat dairy, while limiting saturated fat and added sugar. As a result, these sites are likely to provide more nutritionally supportive foods compared to non-CACFP participating sites.
Summer nutrition programs
Summer nutrition programs, which include the Seamless Summer Option, the Summer Food Service Program and the Summer-EBT, are critically important to children from households with low incomes as food insecurity rates increase when students lose access to school meals. Recently, the United States Department of Agriculture (USDA) established a new, permanent summer nutrition program starting in the summer of 2024 called Summer-EBT [41], which is estimated to benefit almost 30 million children nationwide.
Role of the healthcare provider
Given the scope and benefit of Federal Nutrition Programs (FNPs) for pediatric nutrition and health it is critical that healthcare providers maximize access and participation in these important programs for families in need. Pediatric healthcare providers can support families experiencing food insecurity by screening for food insecurity and connecting children to FNPs by sharing accurate information about the programs, highlighting their nutritional quality, advocating against stigma associated with participation, and connecting families to the full spectrum of programs. Better integration and co-location of FNP service support (enrollment and reauthorization) within healthcare systems may prompt clinicians to more consistently refer families to FNPs and enhance accessibility of these services for families, which may ultimately increase FNP participation and support all families in getting the healthy nutritious food they need. While clinicians may not have the capacity to directly connect families to extensive resources during clinic visits, referrals to other essential staff (such as social workers, patient navigators, or community health workers) or external CBOs may be very effective ways to connect families to necessary resources.
A background on food as medicine
There are clear nutrition and health benefits of FNPs, however, barriers such as access, participation, and adequacy limit their reach and effectiveness, so additional support is needed. Addressing pediatric food insecurity and nutrition security in a healthcare setting may result in health improvements and potential cost savings. In the clinical setting, our research group and others have focused on efforts to address pediatric food insecurity and fruit and vegetable intake by increasing access to produce and offering nutrition education for families within the healthcare system [42,43]. However, despite some success, pediatric interventions to increase fruit and vegetable consumption often report difficulty improving child eating habits, especially vegetable consumption [44▪], and little is known regarding the optimal healthcare-based strategy (i.e., dose, implementation strategy, length of treatment, scalability) to effectively address food insecurity and nutrition, and whether such interventions impact long-term healthcare outcomes and cost in children.
Decades of research provide evidence that addressing diet-related chronic disease with diet modifications prevents chronic disease such as cardiovascular disease [45] and cancers [46]. Pediatric providers understand well that “an ounce of prevention is worth a pound of cure”; however, the integration of dietary interventions within healthcare systems has only recently become a priority. With the emergence of value-based care and payment models, which link healthcare provider payments to the quality of care delivered, interventions that prevent both the onset and exacerbation of chronic conditions are becoming more of a priority for the healthcare system. A strategy that has emerged as a promising avenue to effectively prevent and manage diet-related chronic diseases through mitigation of risk factors like poor diet and food insecurity is “Food as Medicine” (FAM) also known as “Food is Medicine.” FAM interventions are designed to work within and alongside the healthcare setting to prevent, manage, and treat diseases by providing high-risk patients with greater access to high-quality foods and nutrition education. FAM interventions are often categorized into five levels: Medically Tailored Meals (MTM), Medically Tailored Groceries (MTGs), Produce Prescriptions (PRx), FNPs, and Population/Community-level food policies and programs [47]. While most of these interventions are applicable across the entire pediatric age spectrum, a few interventions within the FNP realm are uniquely tailored to specific pediatric age groups as illustrated in Table 1. In addition to providing food resources, core to FAM interventions is inclusion of meaningful passive or active culturally tailored nutrition education and counseling through materials or from a Registered Dietitian, or other experts and trusted community leaders. As such, FAM interventions benefit from partnerships between healthcare providers, clinic staff, and Community-Based Organizations (CBO). Food delivery FAM interventions (MTM, MTG, and PRx) addressing food insecurity have been associated with positive clinical outcomes and healthcare utilization and cost in adults, but data regarding these FAM interventions in pediatric populations are limited [48▪].
Table 1.
Example advocacy opportunities for healthcare providers (Clinicians, Health Systems, Accountable Care Organizations, and so on) to support food as medicine initiatives for children
| Food as medicine intervention | Advocacy considerations | Local level | State level | Federal level |
| Medically Tailored Meals (MTM) | Expand Centers for Medicaid and Medicare Services (CMS) coverage and flexibilities around food as medicine initiatives and encourage states to utilize thema | X | X | |
| Support historically and economically marginalized farmers and distributors through collaboration and consistent purchasing of food for intervention distributiona | X | X | X | |
| Medically Tailored Groceries (MTG) | Support clinic food pantries providing MTGs through partnerships with food banks or other food delivery vendors | X | ||
| Produce Prescriptions (PRx) | Build relationships with local food hubs, grocers, or farmers markets to streamline produce deliveries | X | X | |
| Partner with food growers and distributors who prioritize equitable and sustainable practices to help build a better food system that rewards climate-smart and environmentally friendly practicesa | X | X | X | |
| Federal Nutrition Programs | Permanently offer all children access to healthy meals throughout the school day and summertime | X | X | |
| Support Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) enrollment and utilization (such as co-locating services within a healthcare setting) | X | X | X | |
| Support extension of WIC age eligibility to support children starting kindergarten at age 6 years old | X | X | ||
| Population/Community Health Food Policies & Programs | Support automated processes to ease enrollment, share applications for Medicaid members to enroll/recertify for desired eligible federal nutrition programs | X | X | |
| Nutrition Education & Counseling | Encourage food insecurity screening and intervening as part of standard dietary assessment and management protocol | X |
Applicable for Medically Tailored Meals, Medically Tailored Groceries, and Produce Prescriptions.
The goal of the following sections of this narrative review is to explore FAM strategies for pediatric populations, which we have identified across the pediatric lifespan, from the prenatal period into late adolescence (Fig. 1). This figure highlights the robustness of the pediatric nutrition safety net with its overlapping and complementary array of programs. In the pediatric setting, various FAM interventions can be implemented across the age continuum, from the prenatal period into late adolescence (dashed lines). There are opportunities for overlap with more than one FNPs (e.g., WIC and Summer meals) and ideally no gaps in access to FNPs (e.g., between WIC ending and eligibility for School Meals), and if there are gaps, other programs can fill in (such as Summer or CACFP meals). In addition to FNPs, access to MTMs, MTGs, and PRx can offer a supplemental source of nutrition and vital nutrition education. Additionally, ongoing advocacy efforts should prioritize policies and programs that secure greater access FAM interventions and to the pediatric nutrition safety net. We offer insights into potential opportunities for healthcare providers to obtain funding and implement FAM policies and programs for children and families experiencing food insecurity and diet-related diseases.
Food as medicine strategies and considerations for pediatric healthcare providers
Medically Tailored Meals
MTMs are the most intensive and require the largest up-front, per patient cost of the FAM interventions. The goal of MTMs is to provide preprepared meals to vulnerable individuals with chronic conditions who may struggle with daily activities such as cooking or grocery shopping. MTMs are treatment-focused, providing meals that adhere to evidence-based dietary recommendations for a given chronic disease and are often designed by a Registered Dietitian and culinary experts. US-based, adult-focused MTM interventions have reported improvements in FI, diet quality, health outcomes, rates of hospitalization, medication adherence, and healthcare cost [49–52,53▪].
To our knowledge, there are no pediatric-focused MTM interventions that have published results. However, it appears the opportunities for pediatric-based MTM interventions are on the horizon. The Food is Medicine Coalition (FIMC), an advocacy group supporting MTMs nationwide, has issued guidelines around MTM standards and offers an accelerator program to help nonprofits launch MTMs in their communities. An organization delivering MTMs in the Washington, District of Columbia, metro area, “Food and Friends,” has suggested clinical criteria for delivering MTMs for children [54]. At the federal and state government level, the Centers for Medicare & Medicaid Services (CMS) allow demonstration waivers as a path to expanded coverage of nutrition services to include home delivery of healthy meals for children or pregnant women. The Medicaid 1115 waiver has been initiated to expand services for pediatric populations in 6 states: Arkansas, Massachusetts, New Jersey, North Carolina, Oregon, and Washington [55].
Currently, the opportunity for pediatric healthcare systems to offer MTMs is largely funded by philanthropy such as national child antihunger organizations or national health promotion organizations. The opportunity to partner with state CMS agencies and other healthcare payers to offer MTMs (and other food delivery interventions) to children is limited to small pilots due to cost and complexity. If proven effective, however, the ultimate goal would be for wider coverage of food delivery interventions, including MTMs, as medical interventions. Until then, health providers could explore collaborations with philanthropic foundations or insurance payor pilot studies.
Medically Tailored Groceries
MTGs provide produce and other healthy food options (i.e., whole grains, legumes/beans, lean proteins, etc.) to patients with diet-related disease or risk factors who are capable of preparing their own meals. When implemented in the healthcare setting, eligible patients are offered MTGs in partnership with farmers markets, grocers, or CBOs, such as food banks/pantries or food hubs, which may be co-located within clinics to enhance access for patients [56]. US-based MTGs have reported improved dietary quality, medication adherence, and HbA1c in adults [57▪,58,59,60▪▪].
Data in pediatric populations are sparse and the studies that have been conducted are primarily small, pilot, feasibility studies [61▪]. Two MTG studies have reported pediatric outcomes, which included increased child acceptance of grains, vegetables, and legumes and whole grain intake [59], and self-reported improvements in food access, nutrition knowledge and behaviors [62].
With the emergence of studies reporting potential benefits of MTGs and their relative lower cost and complexity compared to MTMs, MTGs may become increasingly appealing to healthcare systems that are interested in addressing food insecurity and nutrition security in at-risk populations. CBOs can serve an integral role in the MTGs delivery model; however, as these organizations have limited staffing and capacity, adequate support must be invested in community partners to ensure they have the appropriate infrastructure and funding to partner effectively. Funding opportunities are similar to those described for MTMs.
Produce Prescriptions
The National Produce Prescription Collaborative (NPPC) defines PRx as a prescription generated by a healthcare provider or health insurance plan, fulfilled through a food retailer, that enables patients to access healthy produce with no added fats, sugars, or salt, at low or no cost to the patient [63]. In adults, PRx interventions are associated with improved food security, healthier food purchasing and consumptions, improvements in disease metrics (HbA1c, blood pressure, BMI), and financial benefits for patients [64,65,66▪▪]. Despite these positive outcomes, PRx studies have identified some barriers to utilizing prescriptions that must be considered, such as ease of voucher use, redemption or “fulfillment” location or transportation issues, and a lack of knowledge and skill regarding produce preparation [42,67▪,68,69].
Pediatric-focused PRx studies have shown positive associations with food insecurity [66▪▪,69–73], produce consumption [42,66▪▪,69–71,73–75], and BMI in children who have obesity [70], while other pediatric studies have shown no relationship with BMI [66▪▪]. Recently, the largest multisite PRx project published findings from 2064 adults and 1817 children (2–17 years old) at risk for or with cardiometabolic disease and food insecurity. This study reported increased produce intake, enhanced self-reported health status, and improved food security in adults and children. While they reported improved HbA1c, hypertension, and BMI in adults, they reported no statistically significant change in these metrics in children [66▪▪]. Although the reason behind the lack of significant results in children was not explained, the study was likely underpowered to detect a significant change. Additionally, metabolic abnormalities are less common and often less severe in children, making them harder to detect and change. Because health outcomes like metabolic changes are not likely to change in response to pediatric PRx interventions, proxy measures could be used as an indicator of intervention impact in a relatively healthy pediatric population. Such behavioral proxy measures include change in fruit and vegetable consumption but could also include changes in child preference and acceptance of produce and changes in culinary and nutrition skills and knowledge. These outcomes have been reported in pediatric PRx interventions [67▪,68,75] and a self-selection PRx intervention in adults [76▪]. Nearly all pediatric PRx studies published to date have been feasibility or qualitative studies, therefore critical questions remain regarding how to best implement PRx interventions, the ideal target population, dose and duration, the minimum standards for a redemption or fulfillment setting, and the long-term impact on pediatric health and health proxy outcomes, healthcare utilization, and cost.
Much like MTGs, PRx offers a tangible opportunity to address pediatric health and social needs with a more reasonable cost and ease of implementation compared to MTMs and requires strong partnerships with CBOs. Funding opportunities are like those described for MTMs and MTGs and additionally, federal grants from the USDA fund PRx programs in clinic settings across the country [29▪].
Considerations for pediatric-based Medically Tailored Meals, Medically Tailored Groceries, Produce Prescriptions interventions
There is still a lot to learn about implementation and evaluation of best practices for these pediatric FAM interventions and additional research within pediatric patients is needed. It is not yet clear what food prescription FAM interventions are most appropriate or effective for different age ranges. A child's specific medical condition or social circumstances may be an appropriate criterion for FAM intervention selection. For example, MTM, MTG, and PRx intervention can apply to patients with Type 1 or type 2 diabetes mellitus or with a rapid weight gain trajectory because these are conditions that are often responsive to changes in diet. MTMs, MTGs, and PRx are typically prescribed to individuals; however, they may be more effective if provision of food can also meet the needs of vulnerable children in the home. A recent change to the Massachusetts Medicaid program enables adjustments of nutrition support benefit size based on household size, so there will eventually be empirical data to test this hypothesis. Regarding evaluations, change in clinical health outcomes, utilization, and cost metrics can take many years to manifest in a young, relatively healthy pediatric population. If evaluators use the same outcome metrics to assess adult and pediatric FAM interventions, we miss a major national opportunity to influence developmental trajectories and prevent future disease risk in children. Pediatric FAM interventions should measure impact by quantitatively and qualitatively assessing change in behaviors, food insecurity, quality of life, engagement with primary and emergency care, knowledge and attitudes about healthy behaviors, and program reach, engagement, and participation with shared metrics with a focus on prevention outcomes. To maximize the collective impact of these interventions, results should be shared publicly so policymakers can make informed decisions about funding for FAM as a covered benefit through healthcare. It is very likely that primary prevention of chronic disease in children now will ultimately save money on costly healthcare treatments for diet-related chronic disease in the future.
Population/community health food policies and programs
FAM approaches at the policy level reach the widest audience and are focused on prevention and population health. Healthcare providers can engage in FAM intervention at this level by supporting policies that aim to increase access and adequacy of MTMs, MTGs, PRx, and FNPs, which we summarize in Table 1. The list of opportunities is not exhaustive. We highlight potential actions at federal, state, and local levels that may promote greater access to the nutrition and economic safety net for families with children. FAM policies can prioritize efforts that support local and sustainable food systems to support local economies and the health of the planet.
CONCLUSION
FAM interventions have gained momentum over the last few years. Thus far, FAM has mainly focused on adults, and although this work is essential, it will not always directly translate to pediatric populations. It is important for pediatric-focused FAM interventions to measure impact beyond laboratory and anthropometric shifts, but also assess health proxy outcomes and changes in behaviors, quality of life, food security, and engagement with the healthcare system, and when possible, engage the whole family unit. The effects of food insecurity, nutrition insecurity, and diet-related chronic disease will be cumulative on young children and to improve long term health and curb costs early prevention is necessary. To make the case that these interventions are effective, they must be rigorously evaluated in pediatric settings by multidisciplinary teams and collaborations. Applying the entire spectrum of FAM interventions in pediatric settings from prenatal to adolescent stages will offer the greatest opportunity to ensure all children have access to enough healthful food so they can achieve their highest potential in life.
Acknowledgements
The authors acknowledge the valuable feedback from our colleagues and friends.
Financial support and sponsorship
There were no sources of funding for this work.
Conflicts of interest
The authors have no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Rabbitt M, Hales L, Burke M, Coleman-Jensen A. Household food security in the United States in 2022. Washington, DC: US Department of Agriculture, Economic Research Service; 2023. [Google Scholar]
- 2.Butcher LM, O'Sullivan TA, Ryan MM, et al. To dine in or not to dine in: a comparison of food selection and preparation behaviours in those with and without food security. Health Promot J Austr 2021; 32:267–282.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruel MT, Garrett JL, Hawkes C, Cohen MJ. The food, fuel, and financial crises affect the urban and rural poor disproportionately: a review of the evidence. J Nutr 2010; 140:170S–176S.. [DOI] [PubMed] [Google Scholar]
- 4.Ciciurkaite G, Brown RL. The link between food insecurity and psychological distress: the role of stress exposure and coping resources. J Community Psychol 2022; 50:1626–1639.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Essel K, Courts KA. Epidemiology and pathophysiology of food insecurity [Internet]. In: Kersten HB, Beck AF, Klein M, editors. Identifying and addressing childhood food insecurity in healthcare and community settings. Springer International Publishing; 2018; 2–6. [Google Scholar]
- 6.Landry MJ, Van Den Berg AE, Asigbee FM, et al. Child-report of food insecurity is associated with diet quality in children. Nutrients 2019; 11:1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brochier A, Messmer E, Wexler MG, et al. A cross-sectional study of relationships between social risks and prevalence and severity of pediatric chronic conditions. BMC Pediatr 2023; 23:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas MMC, Miller DP, Morrissey TW. Food insecurity and child health. Pediatrics 2019; 144:e20190397. [DOI] [PubMed] [Google Scholar]
- 9.Ghani F, Wang H, Manning SE, Sambamoorthi U. Interactive association of chronic illness and food insecurity with emergency department utilization among school-age children in the United States: a cross-sectional study. Health Sci Rep 2023; 6:e1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shankar P, Chung R, Frank DA. Association of food insecurity with children's behavioral, emotional, and academic outcomes: a systematic review. J Dev Behav Pediatr 2017; 38:135–150.. [DOI] [PubMed] [Google Scholar]
- 11▪.Palakshappa D, Garg A, Peltz A, et al. Food insecurity was associated with greater family healthcare expenditures in the US, 2016–17: study examines the relationship between food insecurity and family healthcare expenditures. Health Aff (Millwood) 2023; 42:44–52.. [DOI] [PMC free article] [PubMed] [Google Scholar]; Results from nationally representative data show that food-insecure families had 20% greater total healthcare expenditures than food-secure families, for an annual difference of $2456.
- 12. Ashbrook A, Essel K, Montez K, Bennett-Tejes D. SCREEN AND INTERVENE: a toolkit for pediatricians to address food insecurity [Internet]. 2021. https://frac.org/wp-content/uploads/FRAC_AAP_Toolkit_2021_032122.pdf. [Accessed 22 September 2023] [Google Scholar]
- 13. U.S. DEPARTMENT OF AGRICULTURE. Food and Nutrition Security [Internet]. https://www.usda.gov/nutrition-security. [Accessed 23 August 2023] [Google Scholar]
- 14.Liu J, Rehm CD, Onopa J, Mozaffarian D. Trends in diet quality among youth in the United States, 1999–2016. JAMA 2020; 323:1161–1174.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang L, Martínez Steele E, Du M, et al. Trends in consumption of ultraprocessed foods among US youths aged 2-19 years, 1999–2018. JAMA 2021; 326:519–530.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hall KD, Ayuketah A, Brychta R, et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab 2019; 30:67–77.. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lawrence JM, Divers J, Isom S, et al. Trends in prevalence of Type 1 and Type 2 diabetes in children and adolescents in the US, 2001–2017. JAMA 2021; 326:717–727.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. NCHS Health E-Stats. 2020. [Google Scholar]
- 19.Jackson SL, Zhang Z, Wiltz JL, et al. Hypertension among youths — United States, 2001–2016. MMWR Morb Mortal Wkly Rep 2018; 67:758–762.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. True cost of food measuring what matters to transform the U.S. Food System [Internet]. The Rockefeller Foundation; 2021. https://www.rockefellerfoundation.org/wp-content/uploads/2021/07/True-Cost-of-Food-Full-Report-Final.pdf. [Accessed 13 September 2023] [Google Scholar]
- 21.Malbi J, Castner L, Ohls J, et al. Food expenditures and diet quality among low-income households and individuals. Alexandria, VA: US Department of Agriculture, Food and Nutrition Service; 2010. [Google Scholar]
- 22.Frongillo EA, Jyoti D F, Jones S J. Food Stamp Program participation is associated with better academic learning among school children. J Nutr 2006; 136:1077–1080.. [DOI] [PubMed] [Google Scholar]
- 23.Gregory CA, Deb P. Does SNAP improve your health? Food Policy 2015; 50:11–19.. [Google Scholar]
- 24▪▪.Dillman L, Eichner J, Humienny A, et al. The impact of Supplemental Nutrition Assistance Program (SNAP) enrollment on health and cost outcomes. NEJM Catal [Internet] 2023; 4: http://catalyst.nejm.org/doi/10.1056/CAT.22.0366 [Google Scholar]; This study reports results from a prospective, longitudinal study to understand hospital admissions, ED use, and unplanned healthcare usage, along with the costs associated with medical, pharmacy, dental, and vision care in dual-eligible individuals who were newly enrolled in SNAP benefits. SNAP enrollment was a statistically significant predictor of pharmacy cost and total cost of care but not medical costs. SNAP enrollees’ total cost of care was 16% lower than that of non-SNAP enrollees during both year 1 and year 2. SNAP enrollees’ pharmacy costs were 21% lower than non-SNAP enrollees during years 1 and 2.
- 25. Vigil A. Trends in Supplemental Nutrition Assistance Program participation rates: fiscal year 2016 to fiscal year 2020. Food and Nutrition Service, Office of Policy Support. [Google Scholar]
- 26. Lacarte V, Hinkle L, Broberg BL. SNAP access and participation in U.S.-born and immigrant households: a data profile. Washington, DC: Migration Policy Institute; 2023. [Google Scholar]
- 27.Kharmats AY, Jones-Smith JC, Cheah YS, et al. Relation between the Supplemental Nutritional Assistance Program cycle and dietary quality in low-income African Americans in Baltimore, Maryland. Am J Clin Nutr 2014; 99:1006–1014.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heflin C, Hodges L, Mueser P. Supplemental Nutrition Assistance Program benefits and emergency room visits for hypoglycaemia. Public Health Nutr 2017; 20:1314–1321.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29▪. GusNIP NTAE. Gus Schumacher Nutrition Incentive Program (GusNIP): year 3 impact findings: 3: September 1, 2021, to August 31, 2022 [Internet]. U.S. Department of Agriculture, National Institute of Food and Agriculture; 2023. https://nutritionincentivehub.org/media/2uwlf3ch/gusnip-y3-impact-findings-report.pdf. [Google Scholar]; This report presents outcomes and impacts from projects that used GusNIP and/or GusCRR funding to provide nutrition incentive interventions. The average fruit and vegetable intake among GusNIP nutrition incentive program participants was greater than the average US adult fruit and vegetable intake.
- 30.Engel K, Ruder EH. Fruit and Vegetable Incentive Programs for Supplemental Nutrition Assistance Program (SNAP) Participants: a scoping review of program structure. Nutrients 2020; 12:1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Samuel LJ, Szanton SL, Wolff JL, Gaskin DJ. Supplemental nutrition assistance program 2009 expansion and cardiometabolic markers among low-income adults. Prev Med 2021; 150:106678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gundersen C. Ensuring the dignity and autonomy of SNAP recipients. Physiol Behav 2020; 221:112909. [DOI] [PubMed] [Google Scholar]
- 33.Center on Budget and Policy Priorities, Carlson S, Neuberger Z. WIC Works: addressing the nutrition and health needs of low-income families for more than four decades. 2021. [Google Scholar]
- 34▪.Venkataramani M, Ogunwole SM, Caulfield LE, et al. Maternal, infant, and child health outcomes associated with the Special Supplemental Nutrition Program for women, infants, and children: a systematic review. Ann Intern Med 2022; 175:1411–1422.. [DOI] [PubMed] [Google Scholar]; This systematic review of literature identified 20 studies providing evidence for impact of WIC participation during pregnancy on risk of preterm birth, low birthweight, infant mortality, inadequate gestational weight gain, well child visits, and childhood immunizations.
- 35.U S Department of Agriculture Food and Nutrition Service, Farson Gray K, Balch-Crystal E, Giannarelli L, Johnson P. National- and State-level estimates of WIC eligibility and WIC program reach in 2019. 2022. [Google Scholar]
- 36▪.Smith TA, Valizadeh P. Aging out of WIC and child nutrition: evidence from a regression discontinuity design. American J Agri Economics 2023. 1–21.. [Google Scholar]; This is a regression analysis of data from the public-use National Health and Nutrition Examination Survey (NHANES) of children around the age of 5 found that aging out of WIC prior to entering school was associated with a 20–30% decline in diet quality, primarily driven by reductions in consumption of WIC-target foods.
- 37▪.Cho SJ. The effect of aging out of the Women, Infants, and Children (WIC) program on food insecurity. Health Econ 2022; 31:664–685.. [DOI] [PubMed] [Google Scholar]; Data from Current Population Survey (CPS) were analyzed and identified aging out of WIC increases child food insecurity by an estimated 1.1–3.5%, with higher estimated in lower income families. The authors suggest the prevalence of child food insecurity would decline by 15% if WIC extended its cutoff age until children enroll in kindergarten.
- 38.Forrestal S, Potamites E, Guthrie J, Paxton N. Associations among food security, school meal participation, and students’ diet quality in the First School Nutrition and Meal Cost Study. Nutrients 2021; 13:307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Food Research & Action Center, Hysom E, FitzSimons C. Large school district report operating school nutrition programs as the nation recovers from the pandemic [Internet]. 2023; https://frac.org/wp-content/uploads/large-school-district-report-2023.pdf [Google Scholar]
- 40▪.Yoong SL, Lum M, Wolfenden L, et al. Healthy eating interventions delivered in early childhood education and care settings for improving the diet of children aged six months to six years. Cochrane Database Syst Rev 2023. 2023.http://doi.wiley.com/10.1002/14651858.CD013862.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a systematic literature review to describe the early childhood education center-based healthy eating interventions versus usual practice or no intervention on child diet quality. There is evidence that interventions likely increase children's consumption of fruit, vegetables, but likely result in little to no difference in children's consumption of noncore foods or consumption of sugar-sweetened beverages.
- 41. USDA Food and Nutrition Service. Summer EBT [Internet]. [cited 22 September 2022]. https://www.fns.usda.gov/sebt. [Google Scholar]
- 42.Fischer L, Bodrick N, Mackey ER, et al. Feasibility of a Home-Delivery Produce Prescription Program to address food insecurity and diet quality in adults and children. Nutrients 2022; 14:2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Johnson S, Fischer L, Gupta S, et al. I felt like I had something I could do about it”: pediatric clinician experiences with a Food Insecurity-Focused Produce Prescription Program. Clin Pediatr (Phila) 2023. 000992282211506. [DOI] [PubMed] [Google Scholar]
- 44▪.Beals E, Deierlein A, Katzow M. Clinical interventions to increase vegetable intake in children. Curr Opin Pediatr 2023; 35:138–146.. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a literature review summarizing lessons learned from behavioral interventions in the pediatric primary care setting to improve vegetable intake. Interventions should be tailored to the child age/stage and focus on parental role modeling, motivational interviewing, and frequent follow-up.
- 45.Shan Z, Li Y, Baden MY, et al. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med 2020; 180:1090–1100.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Castro-Espin C, Agudo A. The role of diet in prognosis among cancer survivors: a systematic review and meta-analysis of dietary patterns and diet interventions. Nutrients 2022; 14:348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mozaffarian D, Blanck HM, Garfield KM, et al. A Food is Medicine approach to achieve nutrition security and improve health. Nat Med 2022; 28:2238–2240.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48▪.Norris K, Jilcott Pitts S, Reis H, Haynes-Maslow L. A systematic literature review of nutrition interventions implemented to address food insecurity as a social determinant of health. Nutrients 2023; 15:3464. [DOI] [PMC free article] [PubMed] [Google Scholar]; This systematic literature review identified 21 studies reporting outcomes from Food as Medicine interventions MTMs, MTGs, and PRx. The majority of studies were conducted in adults with only three reporting pediatric outcomes.
- 49.Berkowitz SA, Delahanty LM, Terranova J, et al. Medically tailored meal delivery for diabetes patients with food insecurity: a randomized cross-over trial. J Gen Intern Med 2019; 34:396–404.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Berkowitz SA, Terranova J, Randall L, et al. Association between receipt of a medically tailored meal program and healthcare use. JAMA Intern Med 2019; 179:786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Berkowitz SA, Terranova J, Hill C, et al. Meal delivery programs reduce the use of costly healthcare in dually eligible Medicare and Medicaid beneficiaries. Health Aff (Millwood) 2018; 37:535–542.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Palar K, Napoles T, Hufstedler LL, et al. Comprehensive and medically appropriate food support is associated with improved HIV and diabetes health. J Urban Health 2017; 94:87–99.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53▪.Kempainen S, Cutts DB, Robinson-O’Brien R, et al. A collaborative pilot to support patients with diabetes through tailored Food Box Home Delivery. Health Promot Pract 2023; 24:963–968.. [DOI] [PubMed] [Google Scholar]; This reports results from a randomized, controlled prospective pilot study to determine feasibility and impact of home-delivered food to adults with type 2 diabetes experiencing food insecurity. Treatment group reported improved food security and health status. There were no differences in HbA1c or healthcare utilization measures between the two groups. Findings support feasibility, intervention acceptance, and program satisfaction.
- 54. [2022] Quick Eligibility Chart [Internet]. [cited 4 September 2023]. https://foodandfriends.org/wp-content/uploads/2022/10/2022-Quick-Eligibility-Chart.pdf. [Google Scholar]
- 55. KFF. Medicaid Waiver Tracker: approved and pending section 1115 waivers by state [Internet]. 2023 [cited 9 September 2023]. https://www.kff.org/medicaid/issue-brief/medicaid-waiver-tracker-approved-and-pending-section-1115-waivers-by-state/#Table3. [Google Scholar]
- 56.Hess A, Passaretti M, Coolbaugh S. Fresh Food Farmacy. Am J Health Promot 2019; 33:830–832.. [DOI] [PubMed] [Google Scholar]
- 57▪.Biber DD. A pilot evaluation of the Food as Medicine program for patients with type 2 diabetes. Eval Program Plann 2023; 97:102234. [DOI] [PubMed] [Google Scholar]; This is a pilot MTG program enrolled adult participants with diabetes. There were no statistically significant changes in prepost hemoglobin A1C, diabetes self-care activities, or physical activity. Qualitative data revealed benefits of the program and barriers to participation, learning outcomes, and suggested program changes.
- 58.Wetherill MS, Chancellor McIntosh H, Beachy C, Shadid O. Design and implementation of a clinic-based food pharmacy for food insecure, uninsured patients to support chronic disease self-management. J Nutr Educ Behav 2018; 50:947–949.. [DOI] [PubMed] [Google Scholar]
- 59.Tester JM, Leak TM. Fiber-rich foods delivered to Low-Income Households: a feasibility study of children with prediabetes and spillover effect on their caregivers. Prev Med Rep 2021; 24:101511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60▪▪.Ranjit N, Aiyer JN, Toups JD, et al. Clinical outcomes of a large-scale, partnership-based regional food prescription program: results of a quasi-experimental study. BMC Res Notes 2023; 16:13. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a secondary analysis of data from an adult-focused multisite food prescription program designed to assess impact of program on cardio-metabolic markers. Participants experienced a significantly greater reduction in hemoglobin A1C and blood pressure versus nonparticipants. The decline in clinical markers was associated with “dose” or frequency of visits to the food bank.
- 61▪.Woo Baidal JA, Meyer D, Partida I, et al. Feasibility of Food FARMacia: mobile food pantry to reduce household food insecurity in pediatric primary care. Nutrients 2022; 14:1059. [DOI] [PMC free article] [PubMed] [Google Scholar]; A clinically based mobile food pantry pilot program targeting families with children less than six years old reached the target population and was feasible.
- 62.Aiyer JN, Raber M, Bello RS, et al. A pilot food prescription program promotes produce intake and decreases food insecurity. Transl Behav Med 2019; 9:922–930.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. National Produce Prescription Collaborative - NPPC [Internet]. Natl. Prod. Prescr. Collab. - NPPC. [cited 5 January 2023]. https://www.nppc.health. [Google Scholar]
- 64.Veldheer S, Scartozzi C, Knehans A, et al. A systematic scoping review of how healthcare organizations are facilitating access to fruits and vegetables in their patient populations. J Nutr 2020; 150:2859–2873.. [DOI] [PubMed] [Google Scholar]
- 65.Little M, Rosa E, Heasley C, et al. Promoting healthy food access and nutrition in primary care: a systematic scoping review of Food Prescription Programs. Am J Health Promot 2022; 36:518–536.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66▪▪.Hager K, Du M, Li Z, et al. Impact of produce prescriptions on diet, food security, and cardiometabolic health outcomes: a multisite evaluation of 9 Produce Prescription Programs in the United States. Circ Cardiovasc Qual Outcomes 2023; 16:e009520. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study reports results from a multisite PRx intervention, enrolling adults and children. Fruit and vegetable intake increased among adults and children, and odds of food insecurity dropped. Odds of improving self-reported health status increased for adults and children. Hemoglobin A1C, blood pressure and BMI decreased in adults with high hemoglobin A1C, hypertension and obesity at baseline, respectively.
- 67▪.Brown R, Reilly G, Patel F, et al. Farm to Families: clinic-based produce provision to address food insecurity during the pandemic. Pediatrics 2022; 150:e2022057118. [DOI] [PubMed] [Google Scholar]; This is a qualitative feasibility study to examine ability to reach families with food insecurity without eligibility criteria, and caregiver experiences and preferences for programming in a family-focused PRx. The intervention was acceptable to caregivers due to efficiency and ease, quality of produce, and interactions with program staff. Participants reported improved attitudes toward produce and confidence in buying produce, increased exposure, interest, and acceptance of fruits and vegetables.
- 68.Esquivel M, Higa A, Guidry A, et al. A qualitative study on the motivators, barriers and supports to participation in a Pediatric Produce Prescription Program in Hawai‘i. Int J Environ Res Public Health 2022; 19:16682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Burrington CM, Hohensee TE, Tallman N, Gadomski AM. A pilot study of an online produce market combined with a fruit and vegetable prescription program for rural families. Prev Med Rep 2020; 17:101035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jones LJ, VanWassenhove-Paetzold J, Thomas K, et al. Impact of a Fruit and Vegetable Prescription Program on health outcomes and behaviors in young Navajo children. Curr Dev Nutr 2020; 4:nzaa109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Orsega-Smith E, Slesinger N, Cotugna N. Local pediatricians partner with food bank to provide produce prescription program. J Hunger Environ Nutr 2020; 15:353–359.. [Google Scholar]
- 72.Ridberg RA, Bell JF, Merritt KE, et al. A pediatric fruit and vegetable prescription program increases food security in low-income households. J Nutr Educ Behav 2019; 51:224–230.. e1. [DOI] [PubMed] [Google Scholar]
- 73.Saxe-Custack A, LaChance J, Jess J, Hanna-Attisha M. Influence of a Pediatric Fruit and Vegetable Prescription Program on child dietary patterns and food security. Nutrients 2021; 13:2619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Forbes JM, Forbes CR, Lehman E, George DR. Prevention Produce”: integrating medical student mentorship into a fruit and vegetable prescription program for at-risk patients. Perm J 2019; 23:18–238.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Saxe-Custack A, LaChance J, Hanna-Attisha M. Child consumption of whole fruit and fruit juice following six months of exposure to a pediatric Fruit and Vegetable Prescription Program. Nutrients 2019; 12:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76▪.Johnson JK, Vingilis E, Terry AL. Patients’ experiences with a community fruit and vegetable box program prescribed by their health provider. BMC Public Health 2023; 23:869. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a study exploring the lived experience of adults with food insecurity who were recipients of a PRx program. Participants perceived benefits to their health by participating in PRx. Follow up with health providers helped support behavior change toward better nutrition. Self-section of produce was suggested by most to help meal planning and to increase autonomy.