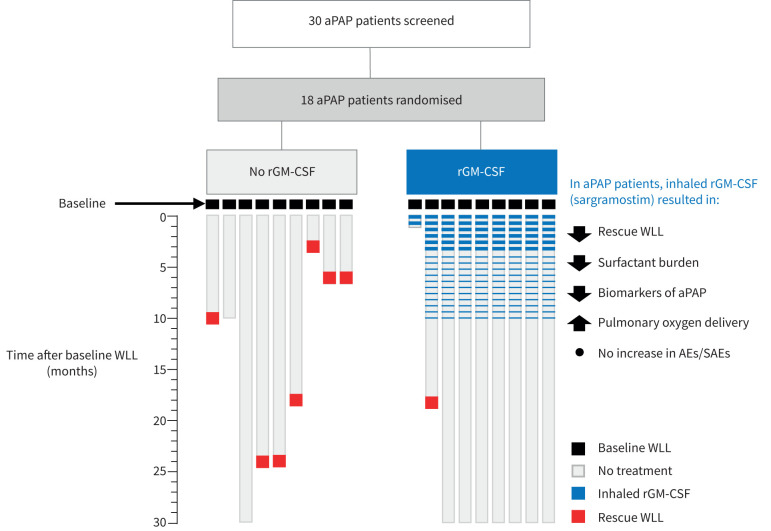
Graphical abstract
Overview of the study. aPAP: autoimmune pulmonary alveolar proteinosis; rGM-CSF: recombinant granulocyte–macrophage colony-stimulating factor; WLL: whole lung lavage; AE: adverse event; SAE: serious adverse event.
Abstract
Rationale
Whole lung lavage (WLL) is a widely accepted palliative treatment for autoimmune pulmonary alveolar proteinosis (aPAP) but does not correct myeloid cell dysfunction or reverse the pathological accumulation of surfactant. In contrast, inhaled recombinant granulocyte–macrophage colony-stimulating factor (rGM-CSF) is a promising pharmacological approach that restores alveolar macrophage functions including surfactant clearance. Here, we evaluate WLL followed by inhaled rGM-CSF (sargramostim) as therapy of aPAP.
Methods
18 patients with moderate-to-severe aPAP were enrolled, received baseline WLL, were randomised into either the rGM-CSF group (receiving inhaled sargramostim) or control group (no scheduled therapy) and followed for 30 months after the baseline WLL. Outcome measures included additional unscheduled “rescue” WLL for disease progression, assessment of arterial blood gases, pulmonary function, computed tomography, health status, biomarkers and adverse events. Patients requiring rescue WLL were considered to have failed their assigned intervention group.
Results
The primary end-point of time to first rescue WLL was longer in rGM-CSF-treated patients than controls (30 versus 18 months, n=9 per group, p=0.0078). Seven control patients (78%) and only one rGM-CSF-treated patient (11%) required rescue WLL, demonstrating a 7-fold increase in relative risk (p=0.015). Compared to controls, rGM-CSF-treated patients also had greater improvement in peripheral arterial oxygen tension, alveolar–arterial oxygen tension difference, diffusing capacity of the lungs for carbon monoxide and aPAP biomarkers. One patient from each group withdrew for personal reasons. No serious adverse events were reported.
Conclusions
This long-term, prospective, randomised trial demonstrated inhaled sargramostim following WLL reduced the requirement for WLL, improved lung function and was safe in aPAP patients. WLL plus inhaled sargramostim may be useful as combined therapy for aPAP.
Tweetable abstract
Following whole lung lavage (WLL), inhaled recombinant GM-CSF reduces the requirement for further WLL in aPAP patients, resulting in greater improvement in lung function, and is safe https://bit.ly/3MD2Klh
Introduction
Autoimmune pulmonary alveolar proteinosis (aPAP) is an acquired disorder of myeloid cell dysfunction, progressive surfactant accumulation, hypoxaemia, dyspnoea, innate immune deficiency and, in some individuals, serious infections, pulmonary fibrosis, respiratory failure and death [1–5]. Prevalence is reported at 7–26 per million [6–8]. Pathogenesis is mediated by autoantibodies that block granulocyte–macrophage colony-stimulating factor (GM-CSF) signalling [5, 9–11], which alveolar macrophages require to clear surfactant [12] and neutrophils require to constitutively stimulate host defence functions [9]. An increased serum GM-CSF autoantibody level is diagnostic of aPAP [13] but serum concentration does not correlate with disease severity [14], a phenomenon explained by a critical threshold of autoantibodies (5 μg·mL−1 [11, 13, 15]) above which GM-CSF-dependent functions are completely blocked and cannot be further reduced by higher autoantibody levels [9, 15]. Most people with aPAP experience slow to moderate progression of symptoms (dyspnoea, cough, fatigue) and reduced quality of life, while some experience rapid progression, and a small percentage appear to improve spontaneously [16, 17].
Whole lung lavage (WLL) has remained widely accepted as therapy for pulmonary alveolar proteinosis (PAP) since its introduction in 1963 [16, 18, 19]. However, it requires hospitalisation, a medical team to administer and general anaesthesia. WLL involves the endotracheal isolation of each lung and simultaneous mechanical ventilation of the non-treated lung while the treated lung is repeatedly filled with saline, the chest is percussed to emulsify surfactant and saline, and effluent is drained to physically remove the excess surfactant, typically, with ≥30 L of saline per lung [16, 19]. While therapeutic effects are evident within days and reduce disease-specific mortality [2], WLL does not stop surfactant accumulation or correct alveolar macrophage dysfunction [20, 21] and patients with aPAP require WLL repeatedly with a reported median time between procedures of 15 months [2].
Inhaled recombinant human GM-CSF (rGM-CSF) is a promising pharmacological treatment approach that patients with aPAP can self-administer at home using a handheld nebuliser [22]. It reverses the pathophysiological abnormalities of alveolar macrophages by restoring GM-CSF-dependent differentiation and functions including surfactant clearance and host defence [23–29]. As of 2009 when the present study was initiated, case reports and small series had shown inhaled rGM-CSF improved gas exchange in aPAP [30–36]. However, no studies had determined the optimal dosage, treatment duration or minimal clinically important differences in end-points for patients with aPAP, and no prospective, randomised, blinded, placebo-controlled studies of inhaled rGM-CSF therapy of aPAP had been reported.
The initial goal of this study was to test a treatment regimen believed capable of complete resolution of aPAP by using WLL to reduce the surfactant burden and inhaled rGM-CSF to restore alveolar macrophage functions. While eliminating the need for WLL is considered to indicate resolution of aPAP, the effects of rGM-CSF on the need for WLL have not been studied, partly because the long median time between procedures suggests that a long-duration study would be necessary. Further, although pulmonary gas exchange, pulmonary function tests, quality of life measures and biomarkers have been used as outcome measures, none have been validated in patients with aPAP for use in clinical trials. Thus, the present study was undertaken as a long-term, prospective, randomised, open-label, single-centre phase 2 trial with time to subsequent WLL as the primary end-point. Results indicate inhaled rGM-CSF (sargramostim) following WLL is safe and effective as therapy of aPAP.
Methods and materials
Study patients
Patients were eligible for inclusion if they were ≥18 years of age and had moderate-to-severe aPAP defined by chest computed tomography (CT) findings and lung histology or bronchoalveolar lavage cytology consistent with PAP [2], an abnormal serum GM-CSF autoantibody test [37] and a resting peripheral arterial oxygen tension (PaO2) of <60 mmHg or of >60 mmHg combined with a resting peripheral oxygen saturation (SpO2) of <90% or a ≥5% decline during exercise [38]. Patients were excluded if they were pregnant, breastfeeding, had another lung disease resulting in respiratory failure (e.g. emphysema, pulmonary fibrosis or pulmonary embolism) or other clinically significant heart, metabolic or other disease that would interfere with the study. All participants provided written informed consent.
Study design and end-points
The study was designed by Professor Maurizio Luisetti and was approved by the independent ethics committee of the Fondazione IRCCS Policlinico San Matteo, where it was conducted according to the Declaration of Helsinki and Good Clinical Practice guidelines.
The study design included a screening visit to establish subject eligibility (month −3), an observation period to establish the presence of unremitting/progressive aPAP (months −3 to −1), a pre-WLL visit to evaluate aPAP disease severity (month −1), a baseline visit at which all patients received a scheduled bilateral WLL (month 0) and baseline testing (approximately 1 week later), an open-label treatment period (months 0–10) and a follow-up period with no scheduled treatments (months 10–30) (supplementary figure S1). Eligible patients were randomised in a 1:1 ratio to receive inhaled sargramostim (Leukine; rGM-CSF group) or no scheduled therapy (control group) during the open-label treatment period. Inhaled sargramostim was administered using an AKITA2 APIXNEB vibrating mesh nebuliser (Activaero, Vectura GmbH, Gauting, Germany) [39] in two phases: a high-dose treatment-induction phase (250 μg daily, 7 consecutive days every other week for 12 weeks beginning 1 week after the baseline WLL) followed by a 4-week washout period, and a low-dose treatment-maintenance phase (250 μg daily on days 1 and 3 of every consecutive 14-day period for 6 months beginning 17 weeks after the baseline WLL). For ethical reasons, all patients were eligible to receive unscheduled “rescue” WLL at any time during the trial as necessary for aPAP disease progression, which was strictly defined by a resting PaO2 (determined at our hospital in Pavia, Italy) of <60 mmHg or PaO2 >60 mmHg with SpO2 <90% at rest or a decline of 5% during exercise testing.
The primary outcome measure was the time in months between the scheduled baseline WLL and the first administration of unscheduled rescue WLL (termed “time to rescue WLL”). Key secondary outcome measures included responses in PaO2, alveolar–arterial oxygen tension difference (PA–aO2), diffusing capacity of the lungs for carbon monoxide (DLCO) as a percentage of the predicted value, ground glass opacification (GGO) of the lungs measured by visual scoring of chest CT scans [40], serum biomarkers of PAP (carcinoembryonic antigen (CEA), Krebs von den Lungen-6 (KL-6) antigen and cytokeratin-19 fragment (Cyfra21.1) antigen) and vital capacity (VC). Other outcome measures included the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36), serum GM-CSF autoantibody concentration and peripheral white blood cell and platelet counts. Primary and secondary outcomes (except GGO) were measured at each visit as described in the study calendar (supplementary table S1).
Adverse events were assessed at every study visit and during periodic telephone calls at 12 and 24 months. Patients were questioned about the potential occurrence of suspected adverse events of special interest including bronchospasm, bone and joint pain, cough, fever and myalgias. The potential for bronchospasm was assessed by pulmonary function testing 20 min after the first administration of inhaled sargramostim in each patient. Laboratory testing to assess safety included haematology tests.
Statistical analysis
The analyses were performed according to the intention-to-treat (ITT) principle. The primary end-point was the median difference in time to rescue WLL between the rGM-CSF and control groups, compared using the Mann–Whitney test. Primary analysis of key secondary outcomes was performed by determining between-group differences using repeated measures ANOVA (RM-ANOVA) after adjustment for baseline values, gender, age and the number of patients at risk at each time point. Secondary analysis was performed by determining the between-group difference at each visit, after imputation of missing data using the last observation carried forward method. Comparisons of the corresponding group means (parametric data), medians (nonparametric data) or numbers (categorical data) were made using t-test, Mann–Whitney test or Fisher's exact test, as appropriate. All reported p-values are two-sided and have not been adjusted for multiple testing. p-values <0.05 were considered to indicate statistical significance. Analysis by RM-ANOVA was performed using Stata software version 14.2 (StataCorp LLC, College Station, TX, USA) and other analyses were performed using Prism for Mac OS software, version 9.51 (GraphPad Software, San Diego, CA, USA).
Further details of the study design, interventions, outcome measures and statistical analysis are included in the supplementary appendix and at ClinicalTrials.gov (NCT00901511).
Results
Patients
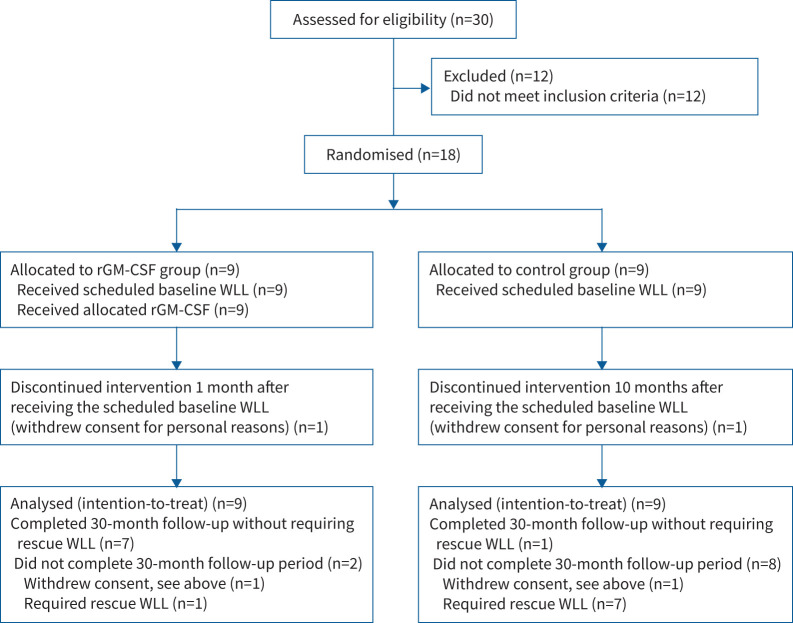
From July 2009 through to December 2012, 30 adult patients with aPAP receiving medical care at the Fondazione IRCCS Policlinico San Matteo of Pavia were assessed for eligibility and 18 were enrolled (figure 1). All had moderate-to-severe aPAP based on the Inoue et al. [41] PAP disease severity score (DSS), degree of restrictive lung physiology (measured by reductions in forced vital capacity (FVC), forced expiratory flow in 1 s (FEV1), total lung capacity (TLC) and VC), impaired pulmonary gas exchange (measured by abnormalities in PaO2, PA–aO2 and DLCO % predicted), degree of abnormal surfactant accumulation (measured by visual assessment of GGO on chest CT scans), increased biomarkers of aPAP and impaired general health status (measured by the SF-36 questionnaire) (table 1). Of the 18 patients randomised and treated, 16 (89%) completed the study; one from each group withdrew participation for personal reasons (figure 1).
FIGURE 1.
Screening, randomisation, treatment and follow-up of the study participants with moderate-to-severe autoimmune pulmonary alveolar proteinosis. rGM-CSF: recombinant granulocyte–macrophage colony-stimulating factor; WLL: whole lung lavage.
TABLE 1.
Demographics and clinical characteristics of the aPAP patients and effect of the baseline WLL
| Demographic or clinical parameter | Pre-WLL visit# | Post-WLL “Baseline”# | p-value¶ |
| Participants (n) | 18 | 18 | |
| Age at diagnosis (years) | 40±12 | – | – |
| Gender (% female) | 7 (39) | – | – |
| BMI (kg·m−2) | 26±3 | – | – |
| Smoking history | |||
| Current smoker | 3 (17) | – | – |
| Ex-smoker | 2 (44) | – | – |
| Never-smoker | 7 (39) | – | – |
| Symptoms and signs | |||
| Dyspnoea | 17 (94) | – | – |
| Cough | 11 (61) | – | – |
| Fever | 0 (0) | – | – |
| Sputum production | 0 (0) | – | – |
| PAP DSS | 4.0 (2.5–5.0) | 1.0 (1.0–3.0) | <0.001 |
| Spirometry and lung volumes | |||
| FEV1 (% predicted) | 62±17 (n=14) | 76±14 | 0.015 |
| FVC (% predicted) | 61±16 (n=14) | 77±14 | 0.007 |
| FEV1/FVC (% predicted) | 98±12 (n=14) | 102±9.7 | 0.291 |
| TLC (% predicted) | 66±8 (n=10) | 76±11 (n=14) | 0.022 |
| VC (% predicted) | 62±14 (n=15) | 75±14 | 0.011 |
| Pulmonary gas exchange | |||
| DLCO (% predicted) | 41±15 (n=13) | 54±13 | 0.008 |
| PaO2 (mmHg) | 59±15 | 77±14 | <0.001 |
| PA–aO2 (mmHg) | 49±14 | 29±14 | <0.001 |
| PaCO2 (mmHg) | 34±2 | 35±3 | 0.291 |
| Radiological evaluation of the lungs | |||
| Chest CT GGO score | 4.9±0.33 (n=17) | – | – |
| Haematology indices | |||
| WBC ×1000·mL−1 | 7.0±1.7 (n=17) | 8.0±2.0 (n=17) | 0.137 |
| Platelets ×1000·mL−1 | 264±80 (n=17) | 280 ±93 (n=17) | 0.60 |
| Serum biomarkers of aPAP | |||
| GM-CSF autoantibody (mg·mL−1) | 42±54 | 38.9±47.9 (n=17) | 0.85 |
| Cyfra21.1 (ng·mL−1) | 19±15 (n=15) | 7.9±4.9 | 0.0046 |
| CEA (ng·mL−1) | 15±14 (n=15) | 9.2±7.2 (n=16) | 0.138 |
| KL-6 (U·mL−1) | 8817±6407 | 10 224±10 343 (n=17) | 0.630 |
| SF-36 component scores | |||
| General health | 35 (23–58) (n=17) | 85 (73–95) | <0.0001 |
| Health change | 0 (0–25) (n=17) | 88 (25–100) | 0.0023 |
| Physical function | 0 (0–67) (n=17) | 100 (100–100) | 0.0001 |
| Energy/fatigue | 56 (42–68) (n=17) | 78 (59–85) | 0.0098 |
| Pain | 40 (23–48) (n=17) | 75 (54–80) | <0.0001 |
| Social function | 38 (13–69) (n=17) | 81 (63–91) | 0.0006 |
| Emotional well-being | 75 (41–100) (n=17) | 100 (98–100) | 0.0008 |
| Role limitations due to physical health | 45 (50–80) (n=17) | 73 (60–80) | 0.0002 |
| Role limitations due to emotional problems | 13 (0–44) (n=17) | 100 (69–100) | <0.0001 |
Enrolled patients had moderate or severe aPAP as indicated by the results shown for all patients in both recombinant GM-CSF and control groups. The baseline visit occurred a median (interquartile range) of 8 (4–16) days after the scheduled baseline WLL. Data are presented as mean±sd, median (interquartile range) or n (%), unless otherwise indicated. Bold text indicates statistical significance. aPAP: autoimmune pulmonary alveolar proteinosis; WLL: whole lung lavage; BMI: body mass index; PAP: pulmonary alveolar proteinosis; DSS: disease severity score; FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; TLC: total lung capacity; VC: (slow) vital capacity; DLCO: diffusing capacity of the lung for carbon monoxide; PaO2: arterial oxygen tension; PA–aO2: alveolar–arterial oxygen tension difference; PaCO2: arterial carbon dioxide tension; CT: computed tomography; GGO: ground glass opacification; WBC: (total) white blood cell count; GM-CSF: granulocyte–macrophage colony-stimulating factor; Cyfra21.1: cytokeratin-19 fragment antigen; CEA: carcinoembryonic antigen; KL-6: Krebs von den Lungen; SF-36: Short Form 36-question Health Survey. #: n<18 indicates missing data; ¶: calculated by comparing corresponding data in patients before and after the baseline bilateral WLL using t-test or Mann–Whitney test.
Effects of the scheduled baseline WLL
The scheduled baseline WLL reduced the severity of aPAP lung disease in all patients as demonstrated by improvement in the DSS, FEV1, FVC, TLC, VC, PaO2, PA–aO2, DLCO % predicted, all SF-36 component scores and Cyfra21.1 concentration (table 1). Following the baseline WLL, patients in the rGM-CSF and control groups were reasonably well matched for these variables (table 2).
TABLE 2.
Comparability of the patient groups after the scheduled baseline WLL
| End-point | Control# | rGM-CSF# | p-value ¶ |
| Participants (n) | 9 | 9 | |
| PAP DSS, median (IQR) | 1.0 (1.0–3.5) | 1.0 (1.0, 1.0) | 0.29 |
| Spirometry and lung volumes | |||
| FEV1 (% predicted) | 77±11 | 75±18 | 0.82 |
| FVC (% predicted) | 76±12 | 78±17 | 0.76 |
| TLC (% predicted) | 73±6.0 (n=6) | 79±14 (n=8) | 0.31 |
| VC (% predicted) | 74±11 | 76±17 | 0.83 |
| Pulmonary gas exchange | |||
| DLCO (% predicted) | 52±12 | 55±14 | 0.62 |
| PaO2 (mmHg) | 72±15 | 82±11 | 0.15 |
| PA–aO2 (mmHg) | 33±15 | 26±12 | 0.28 |
| Haematology indices | |||
| WBC (×1000·mL−1) | 7.5±1.7 | 8.7±2.7 (n=8) | 0.28 |
| Platelets (×1000·mL−1) | 290±111 | 269±73 (n=8) | 0.64 |
| SF-36 general health score | 77±29 | 85±15 | 0.33 |
| Biomarkers | |||
| GM-CSF autoantibody (mg·mL−1) | 25±22 (n=8) | 52±61 | 0.23 |
| Cyfra21.1 (ng·mL−1) | 9.5±6.4 | 5.5±1.7 | 0.07 |
| CEA (ng·mL−1) | 12±9 (n=8) | 6.3±3.2 (n=8) | 0.11 |
| KL-6 (U·mL−1) | 12 142±7049 (n=8) | 8518±12 787 | 0.49 |
Enrolled patients received a scheduled, baseline WLL a median of 8 days (IQR 4–16 days) after enrolment. Data are presented as mean±sd, unless otherwise indicated. WLL: whole lung lavage; rGM-CSF: recombinant granulocyte–macrophage colony-stimulating factor; PAP: pulmonary alveolar proteinosis; DSS: disease severity score; IQR: interquartile range; FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; TLC: total lung capacity; VC: (slow) vital capacity; DLCO: diffusing capacity of the lung for carbon monoxide; PaO2: arterial oxygen tension; PA–aO2: alveolar–arterial oxygen tension difference; WBC: (total) white blood cell count; SF-36: Short Form 36-question Health Survey; Cyfra21.1: cytokeratin-19 fragment antigen; CEA: carcinoembryonic antigen; KL-6: Krebs von den Lungen. #: n<9 indicates missing data; ¶: comparison of the rGM-CSF and control groups using t-test.
Primary analysis
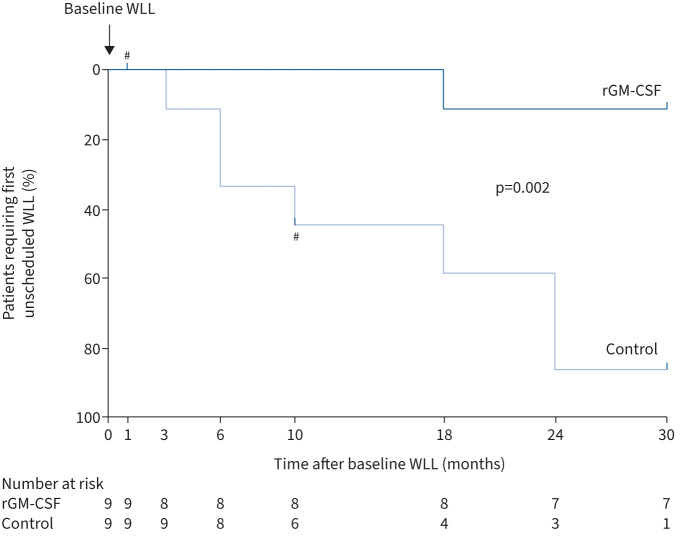
Progression of aPAP lung disease requiring rescue WLL, determined by strict adherence to predefined lung function parameters, occurred less frequently in the rGM-CSF-treated group than control group as shown by Kaplan–Meyer analysis (p=0.002; log-rank Mantel–Cox test) (figure 2 and supplementary figure S2). Seven of nine control patients (78%) and only one of nine rGM-CSF-treated patients (11%) required rescue WLL during the 30 months following the scheduled baseline WLL (month 0), which is a 7-fold increase in relative risk (p<0.015; Fisher's exact test). The primary end-point, the time to rescue WLL, was greater in the rGM-CSF group than the control group (median 30 months (IQR 30–30 months) versus 18 months (6–27 months); p<0.0078, Mann–Whitney) (table 3). These results demonstrate inhaled rGM-CSF (sargramostim) following WLL reduced further use of WLL for progression of aPAP lung disease.
FIGURE 2.
Effect of inhaled recombinant granulocyte–macrophage colony-stimulating factor (rGM-CSF) on the requirement for unscheduled rescue whole lung lavage (WLL) therapy. Kaplan–Meier analysis shows the percentage of study participants in each group (indicated) who required an unscheduled rescue WLL as a function of time during the 30 months following the scheduled baseline WLL at month 0. The number of participants who had not received an unscheduled rescue WLL at each visit is shown below (number at risk). Significance values (p-values) were determined with the log-rank Mantel–Cox test. #: participants who withdrew from the study for personal reasons.
TABLE 3.
Evaluation of the time to rescue WLL, numbers of patients requiring rescue WLL and temporal changes in key secondary outcome measures
| Outcome measure | Study month # | Control | rGM-CSF | p-value |
| Time to first rescue WLL (months), median (IQR) | NR | 18 (6–27) | 30 (30–30) | 0.0078 ¶ |
| Patients requiring rescue WLL (n (%)) | NR | 7 (78) | 1 (11) | 0.015 + |
| PaO2 (mmHg) | 3 | 68±10 | 89±9.2 | 0.0004 § |
| 10 | 73±13 | 92±12 | 0.0149 § | |
| 30 | 71±14 | 82±14 | 0.1158§ | |
| PA–aO2 (mmHg) | 3 | 37±12 | 18±8.1 | 0.0015 § |
| 10 | 34±13 | 18±12 | 0.0152 § | |
| 30 | 35±13 | 24±13 | 0.0921§ | |
| DLCO (% predicted) | 3 | 62±16 | 72±17 | 0.2287§ |
| 10 | 59±20 | 70±15 | 0.1833§ | |
| 30 | 59±21 | 63±15 | 0.6374§ | |
| VC (% predicted) | 3 | 78±17 | 80±15 | 0.7752§ |
| 10 | 78±14 | 82±18 | 0.6393§ | |
| 30 | 77±13 | 79±17 | 0.8159§ | |
| GGO score, median (IQR) | 0 | 5 (5–5) | 5 (5–5) | 0.9999¶ |
| 3 | 4 (4–5) | 3 (2–4) | 0.0332 ¶ | |
| 10 | 5 (3–5) | 3 (2–4) | 0.0676¶ | |
| 18 | 5 (4–5) | 3 (2–4) | 0.0629¶ | |
| 30 | 5 (4–5) | 4 (3–5) | 0.9999¶ | |
| SF-36 general health score | 3 | 79±18 | 93±6.1 | 0.0478 § |
| 10 | 72±26 | 84±15 | 0.2634§ | |
| 30 | 71±28 | 88±8.7 | 0.1043§ |
Data are presented as mean±sd, unless otherwise indicated. Bold text indicates statistical significance. WLL: (bilateral) whole lung lavage; rGM-CSF: recombinant granulocyte–macrophage colony-stimulating factor; IQR: interquartile range; NR: not relevant; PaO2: arterial oxygen tension; PA–aO2: alveolar–arterial oxygen tension difference; DLCO: diffusing capacity of the lungs for carbon monoxide; VC: (slow) vital capacity; GGO: ground glass opacification; SF-36: Short Form 36-question Health Survey. #: month 3=end of rGM-CSF induction therapy period, month 10=end of rGM-CSF maintenance therapy period, month 30=end of follow-up period (20 months after completing inhaled rGM-CSF therapy); ¶: Mann–Whitney U test; +: Fisher's exact test; §: t-test.
Effects of inhaled rGM-CSF on disease severity were evaluated as the between-group difference in key secondary outcomes across all study visits compared using RM-ANOVA. rGM-CSF-treated patients had greater improvement in pulmonary gas exchange than control patients as shown by the difference in PaO2, PA–aO2 and DLCO % predicted (table 4). The lung GGO score was numerically reduced in the rGM-CSF group compared to the control group, but the difference was not significant (table 4). Serum biomarkers of PAP were improved in the rGM-CSF group compared to the control group as shown by between-group differences in CEA, KL-6 and Cyfra21.1 (table 4). Notwithstanding, no further significant improvement was observed in lung mechanics or SF-36 general health score as shown by between-group differences in VC and SF-36 general health score, respectively (table 4). These results demonstrate inhaled sargramostim following WLL improved pulmonary gas exchange and biomarkers of aPAP.
TABLE 4.
Primary analysis of key secondary end-points
| End-point | Estimated difference (95% CI) (rGM-CSF versus control) # | p-value # |
| Pulmonary gas transfer | ||
| PaO2 (mmHg) | 9.5 (5.7–13.3) | <0.0001 |
| PA–aO2 (mmHg) | −10.1 (−14.8– −5.4) | <0.0001 |
| DLCO (% predicted) | 11.6 (1.9–21.3) | 0.022 |
| Pulmonary function | ||
| VC (% predicted) | 2.3 (−5.3–9.9) | 0.532 |
| Radiological assessment | ||
| GGO score | −0.822 (−1.7–0.01) | 0.053 |
| SF-36 general health score | 4.72 (−1.88–11.33) | 0.149 |
| Serum biomarkers | ||
| CyFra21.1 (ng·mL−1) | −0.24 (−0.44– −0.04) | 0.022 |
| CEA (ng·mL−1) | −0.47 (−0.71– −0.22) | 0.001 |
| KL-6 (U·mL−1) | −3689 (−6972– −406) | 0.030 |
rGM-CSF: recombinant granulocyte–macrophage colony-stimulating factor; PaO2: arterial oxygen tension; PA–aO2: alveolar–arterial oxygen tension difference; DLCO: diffusing capacity of the lung for carbon monoxide; VC: (slow) vital capacity; GGO: ground glass opacification; SF-36: Short Form 36-question Health Survey; Cyfra21.1: cytokeratin-19 fragment antigen; CEA: carcinoembryonic antigen; KL-6: Krebs von den Lungen. #: after adjustment for baseline value, gender, age and the numbers of patients at risk at each point, the between-group difference (95% CI) and p-value were calculated using repeated measures ANOVA.
Secondary analyses
Effects of inhaled rGM-CSF on disease severity were also evaluated by comparing secondary end-points at each study visit. Because use of rescue WLL, an indicator of treatment failure, was greater in the control group than the rGM-CSF group (figure 3a), imputation of missing data was used to maintain ITT analysis and minimise selection bias.
FIGURE 3.
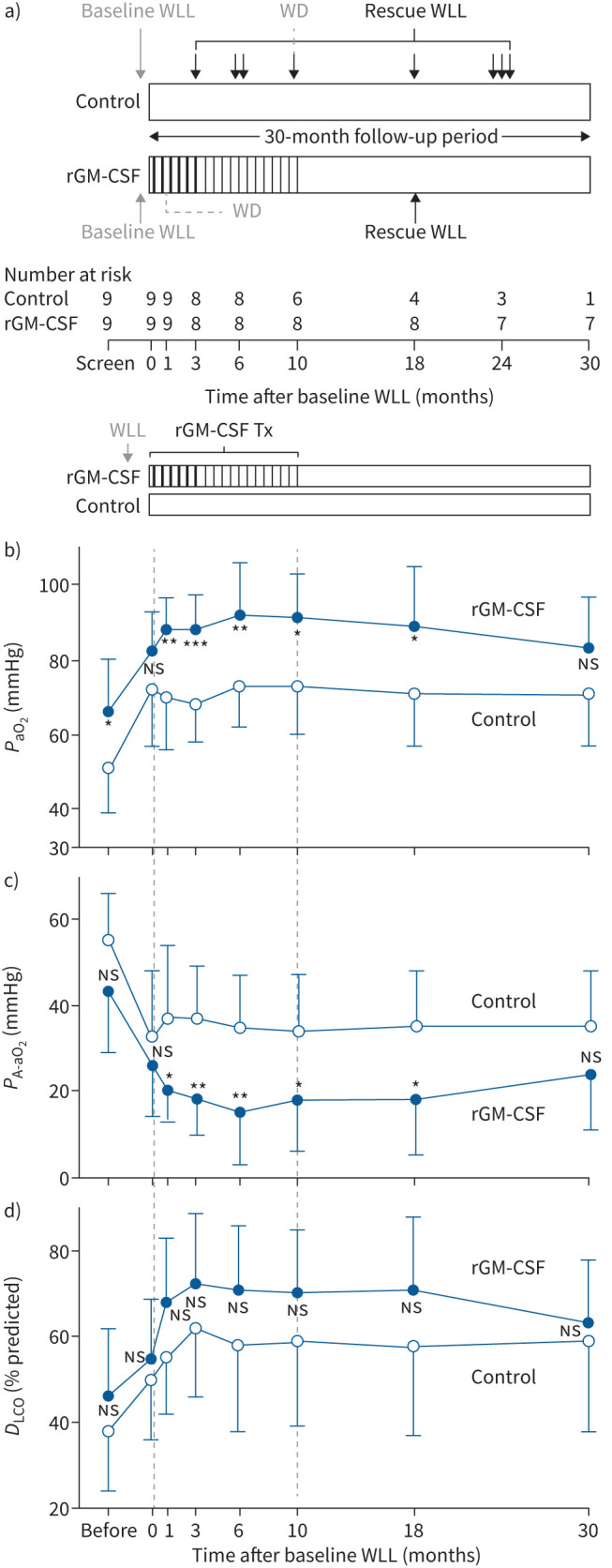
Effects of inhaled recombinant granulocyte–macrophage colony-stimulating factor (rGM-CSF) on pulmonary gas transfer. a) Schematic showing for each study group the administration of the baseline whole lung lavage (WLL) (grey arrows) and unscheduled rescue WLL (black arrows), and inhaled rGM-CSF administered as induction therapy (thick vertical black lines) or maintenance therapy (thin vertical black lines). Open boxes indicate follow-up periods without scheduled intervention. The number of participants who have not yet required an unscheduled rescue WLL at each study visit is shown (number at risk). The times at which two study subjects withdrew (WD) from trial participation for personal reasons is indicated. b) Mean peripheral arterial oxygen tension (PaO2) at each visit for each group (indicated). c) Mean alveolar–arterial oxygen tension difference (PA–aO2) at each visit for each group. d) Mean diffusing capacity of the lungs for carbon monoxide (DLCO) % predicted at each visit for each group. T-bars represent the standard deviation. The timing of administration of inhaled rGM-CSF as induction therapy (thick vertical black lines) or maintenance therapy (thin vertical black lines) to participants in the rGM-CSF group as well as periods with no scheduled intervention are shown above b for b–d. The dashed vertical lines in panels b–d indicate the beginning and end of inhaled rGM-CSF therapy (months 0 and 10, respectively). Tx: therapy; ns: nonsignificant; *: p<0.05; **: p<0.01; ***: p<0.001, for between-group comparison at each visit.
Baseline WLL improved the PaO2 in all patients (table 1). Subsequently and compared to the control group, the PaO2 in the rGM-CSF group was similar at baseline (month 0) (table 2), increased at the end of rGM-CSF induction therapy (month 3) and maintenance therapy (month 10), but declined and was similar to the control group 20 months after discontinuing inhaled rGM-CSF (month 30) (figure 3b and table 3). Changes in PA–aO2 paralleled the changes in PaO2 (figure 3c, tables 1–3). The pattern of changes in DLCO % predicted was similar but differences did not reach significance at any visit (figure 3d and tables 1–3).
Baseline WLL improved the restrictive lung impairment in all patients (table 1), which was similar in both groups at baseline (month 0) (table 2). VC was similar in the groups at 3, 10 and 30 months, indicating no significant further effect of inhaled rGM-CSF on restrictive lung impairment (tables 2 and 3).
The degree of pulmonary surfactant accumulation, measured as the GGO score, was similar among the groups at screening, reduced in the rGM-CSF group compared to the control group at the end of rGM-CSF induction therapy (month 3) and similar among the groups thereafter (table 3 and supplementary figure S3).
Although the serum biomarkers of aPAP (CEA, KL-6, Cyfra21.1) were numerically improved in the rGM-CSF group compared to the control group when evaluated at each study visit, none of the differences reached significance (supplementary figure S4). Serum GM-CSF antibody levels were not different at any study visit (supplementary figure S5).
SF-36 health survey component scores were low (worse) at screening (month −1) and all were increased (improved) after baseline WLL (month 0) in all patients (table 1). Compared to the control group, only the general health score was further improved in the rGM-CSF group at the 3- and 6-month visits (p<0.05); all other SF-36 component scores were similar between the two groups at all subsequent visits (p>0.100) (supplementary figure S6).
Safety assessment
Inhaled rGM-CSF was well tolerated and not associated with bronchospasm or allergic or immunological reactions in any patients (not shown). There were no deaths, serious adverse events, adverse events of special interest or clinically meaningful adverse events related to peripheral blood white blood cell counts (supplementary figure S7a), platelet counts (supplementary figure S7b) or other laboratory assessments, vital signs, physical examination or electrocardiograms in either group (not shown). Progression of aPAP was not considered an adverse event because it was expected in all patients.
Discussion
This long-term, prospective, randomised, single-centre phase 2 study in patients with moderate-to-severe aPAP demonstrated that inhaled rGM-CSF (sargramostim) following WLL reduced the need for WLL and improved pulmonary gas exchange, pulmonary surfactant burden and serum aPAP biomarkers, and was well tolerated, safe and not associated with more frequent adverse events than WLL alone.
The observation that inhaled sargramostim reduced the need for WLL is an important finding of this study, supporting its efficacy as therapy of aPAP. This conclusion is further supported by the recent IMPALA trial in which patients with mild-to-moderate aPAP received inhaled molgramostim, a non-glycosylated form of rGM-CSF prepared in Escherichia coli [42]. Although IMPALA did not meet its secondary end-point related to WLL, time to first rescue WLL use during a 6-month blinded treatment period, administration of rescue WLL was less frequent in patients receiving daily molgramostim than in those receiving placebo [42]. Additional support comes from an uncontrolled study reporting that WLL improved the response to inhaled sargramostim in five patients with intractable aPAP [43]. PAGE, a recently reported randomised, double-blinded, placebo-controlled trial of inhaled sargramostim in 64 patients with mild-to-moderate aPAP, did not assess rescue WLL use [44]. Differences in WLL use between the controlled studies and this study can be explained in part by the disease severity of the patients enrolled and duration of follow-up. Both the IMPALA and PAGE trials included patients with mild-to-moderate aPAP [42, 44] while the present study included patients with moderate-to-severe aPAP. Compared to current estimates of the median time between WLL procedures required by patients with aPAP of 7–15 months [2, 45, 46], both IMPALA and PAGE employed a shorter evaluation period (6 months) [42, 44] while the present study employed a longer period (30 months). The observed reduction in repeated WLL use associated with inhaled rGM-CSF administration has implications for improved quality of life including fewer hospitalisations, reduced general anaesthesia and mechanical ventilation use and related morbidity, and the convenience of a self-administered home-based medical therapy.
The observation of improvement across multiple outcome measures (rescue WLL use, PA–aO2, PaO2, DLCO % predicted, GGO score and PAP biomarkers) further supports the efficacy of inhaled sargramostim as therapy of aPAP. The IMPALA trial showed daily administration of inhaled molgramostim improved gas exchange (PA–aO2, DLCO % predicted), health status (St George's Respiratory Questionnaire total score) and surfactant burden (GGO score), but not exercise capacity (6-min walk test distance) [42]. The PAGE trial demonstrated inhaled sargramostim improved gas exchange (PA–aO2) and surfactant burden (GGO score) but not clinical measures [44].
One limitation of the present study was its small size, necessitated by the high costs of a long follow-up period. Another was the choice of inhaled rGM-CSF dosing and administration, which was made long before the recent reporting of information from controlled studies [42, 44]. The IMPALA trial demonstrated daily administration of molgramostim was superior to placebo whereas daily administration on alternating weeks was not [42]. Further, daily administration improved gas exchange, surfactant burden, biomarkers, health status and WLL use frequency in IMPALA [42] and only gas exchange and surfactant burden in PAGE [44]. The total amount of rGM-CSF administered to each patient in the present study (13.5 mg, sargramostim) was less than PAGE (21 mg, sargramostim) or IMPALA (25.2 or 50.4 mg, molgramostim). The duration of administration (66 of 252 days) was also less than in PAGE (84 of 168 days, sargramostim) or IMPALA (84 or 168 of 168 days). While “off-label” clinical use of inhaled sargramostim suggests that less frequent/lower-dose administration (i.e. maintenance therapy) may sustain the treatment effects achieved during more frequent/higher-dose administration (i.e. induction therapy) [40], this approach has not been tested in controlled studies. While the use of a high-efficiency, vibrating mesh nebuliser capable of alveolar deposition of 50% of the inhaled dose [39] may have partially mitigated the effects of the less frequent administration used in our study, we speculate that consistent daily administration of a relatively higher dose (250 μg·day−1) for a longer time (12 months) would have resulted in larger improvements than those observed. Although the ethical requirement to provide continuous access to the current standard of care (WLL) complicated the study design, it influenced the choice of rescue WLL use as an outcome measure and the employment of a long-term follow-up period.
These results add to an increasing number of reports supporting the feasibility, safety and efficacy of inhaled sargramostim as pharmacotherapy of aPAP.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material ERJ-01233-2023.SUPPLEMENT (918.5KB, pdf)
Shareable PDF
Acknowledgements
The authors dedicate this report to our dear colleague, Professor, Doctor Maurizio Luisetti, who initiated this study but suffered a myocardial infarction and passed away during its conduct (in May 2012 and October 2014, respectively) and was therefore unable to see its completion. He is remembered for his kindness, deep passion for helping others and leadership, particularly by his colleagues who helped complete this study. Reporting of this study was also delayed by the global COVID-19 pandemic. The authors express their sincere thanks to the PAP patients for their perseverance and collaboration in completing this study, Carmine Tinelli (Fondazione Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) Policlinico San Matteo, Pavia, Italy) for contributions to the statistical analysis, Jennifer Stock and Claudia Chalk (Cincinnati Children's Hospital Medical Center) for conducting the GM-CSF autoantibody testing, and Gerhard Scheuch and Bernhard Muellinger (Vectura Fertin Pharma) for providing AKITA nebulisers.
Footnotes
This study is registered at ClinicalTrials.gov with identifier number NCT00901511. No data sharing provision has been made for the study.
This article has an editorial commentary: https://doi.org/10.1183/13993003.01982-2023
Ethics statement: All participants provided written informed consent. The study was was approved by the independent ethics committee of the Fondazione IRCCS Policlinico San Matteo, where it was conducted according to the Declaration of Helsinki and Good Clinical Practice guidelines.
Author contributions: Maurizio Luisetti designed the study. F. Mariani, Z. Kadija, E. Paracchini and G. Rodi managed the PAP patients. I. Campo collected and organised study-related data. I. Campo, M. Zorzetto, M. Griese, M. De Amici, B.C. Carey and B.C. Trapnell analysed the results. A. De Silvestri performed the primary analysis of key secondary outcomes. I. Campo, B.C. Carey and B.C. Trapnell wrote the first draft of the manuscript. All authors had access to the data, contributed to the writing, approved the final version of the manuscript, and vouched for conduct of the trial and accuracy of the data.
Conflict of interest: I. Campo, B.C. Trapnell and B.C. Carey serve as investigators on another clinical trial of inhaled rGM-CSF therapy of autoimmune PAP. B.C. Trapnell and B.C. Carey have served as consultants regarding the development of inhaled rGM-CSF as therapy of aPAP. No other authors have no financial or other conflicts of interest to declare related to this work.
Support statement: This trial was supported by the Agenzia Italiana del Farmaco (FARM7MCPK4 to M. Luisetti), Italy. B.C. Trapnell and B.C. Carey were supported by grants from the National Heart, Lung, and Blood Institute (R01 HL085453 to B.C. Trapnell) and Translational Pulmonary Science Center and Division of Pulmonary Biology, Cincinnati Children's Hospital Medical Center. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Rosen SG, Castleman B, Liebow AA. Pulmonary alveolar proteinosis. N Engl J Med 1958; 258: 1123–1142. doi: 10.1056/NEJM195806052582301 [DOI] [PubMed] [Google Scholar]
- 2.Seymour JF, Presneill JJ. Pulmonary alveolar proteinosis: progress in the first 44 years. Am J Respir Crit Care Med 2002; 166: 215–235. doi: 10.1164/rccm.2109105 [DOI] [PubMed] [Google Scholar]
- 3.McCarthy C, Carey BC, Trapnell BC. Autoimmune pulmonary alveolar proteinosis. Am J Respir Crit Care Med 2022; 205: 1016–1035. doi: 10.1164/rccm.202112-2742SO [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borie R, Danel C, Debray MP, et al. Pulmonary alveolar proteinosis. Eur Respir Rev 2011; 20: 98–107. doi: 10.1183/09059180.00001311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trapnell BC, Whitsett JA, Nakata K. Pulmonary alveolar proteinosis. N Engl J Med 2003; 349: 2527–2539. doi: 10.1056/NEJMra023226 [DOI] [PubMed] [Google Scholar]
- 6.Inoue Y, Trapnell BC, Tazawa R, et al. Characteristics of a large cohort of patients with autoimmune pulmonary alveolar proteinosis in Japan. Am J Respir Crit Care Med 2008; 177: 752–762. doi: 10.1164/rccm.200708-1271OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCarthy C, Avetisyan R, Carey BC, et al. Prevalence and healthcare burden of pulmonary alveolar proteinosis. Orphanet J Rare Dis 2018; 13: 129. doi: 10.1186/s13023-018-0846-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kitamura N, Ohkouchi S, Tazawa R, et al. Incidence of autoimmune pulmonary alveolar proteinosis estimated using Poisson distribution. ERJ Open Res 2019; 5: 00190-2018. doi: 10.1183/23120541.00190-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uchida K, Beck DC, Yamamoto T, et al. GM-CSF autoantibodies and neutrophil dysfunction in pulmonary alveolar proteinosis. N Engl J Med 2007; 356: 567–579. doi: 10.1056/NEJMoa062505 [DOI] [PubMed] [Google Scholar]
- 10.Sakagami T, Uchida K, Suzuki T, et al. Human GM-CSF autoantibodies and reproduction of pulmonary alveolar proteinosis. N Engl J Med 2009; 361: 2679–2681. doi: 10.1056/NEJMc0904077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sakagami T, Beck D, Uchida K, et al. Patient-derived granulocyte–macrophage colony-stimulating factor autoantibodies reproduce pulmonary alveolar proteinosis in nonhuman primates. Am J Respir Crit Care Med 2010; 182: 49–61. doi: 10.1164/rccm.201001-0008OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trapnell BC, Whitsett JA. GM-CSF regulates pulmonary surfactant homeostasis and alveolar macrophage-mediated innate host defense. Annu Rev Physiol 2002; 64: 775–802. doi: 10.1146/annurev.physiol.64.090601.113847 [DOI] [PubMed] [Google Scholar]
- 13.Uchida K, Nakata K, Carey B, et al. Standardized serum GM-CSF autoantibody testing for the routine clinical diagnosis of autoimmune pulmonary alveolar proteinosis. J Immunol Methods 2014; 402: 57–70. doi: 10.1016/j.jim.2013.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seymour JF, Doyle IR, Nakata K, et al. Relationship of anti-GM-CSF antibody concentration, surfactant protein A and B levels, and serum LDH to pulmonary parameters and response to GM-CSF therapy in patients with idiopathic alveolar proteinosis. Thorax 2003; 58: 252–257. doi: 10.1136/thorax.58.3.252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uchida K, Nakata K, Suzuki T, et al. Granulocyte–macrophage colony-stimulating factor autoantibodies and myeloid cell immune functions in healthy subjects. Blood 2009; 113: 2547–2556. doi: 10.1182/blood-2008-05-155689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trapnell BC, McCarthy C. Pulmonary alveolar proteinosis syndrome. In: Broaddus VC, Ernst JD, King TE, Lazarus SC, Sarmiento KF, Schnapp LM, Stapleton RD, Gotway MB, eds. Murray & Nadel's Textbook of Respiratory Medicine. 7th Edn. Philadelphia, Elsevier, 2022; pp. 1363–1377. [Google Scholar]
- 17.Trapnell BC, Nakata K, Bonella F, et al. Pulmonary alveolar proteinosis. Nat Rev Dis Primers 2019; 5: 16. doi: 10.1038/s41572-019-0066-3 [DOI] [PubMed] [Google Scholar]
- 18.Ramirez-Rivera J, Schultz R, Dutton R. Pulmonary alveolar proteinosis: a new technique and rationale for treatment. Arch Intern Med 1963; 112: 173–185. doi: 10.1001/archinte.1963.03860020071008 [DOI] [PubMed] [Google Scholar]
- 19.Beccaria M, Luisetti M, Rodi G, et al. Long-term durable benefit after whole lung lavage in pulmonary alveolar proteinosis. Eur Respir J 2004; 23: 526–531. doi: 10.1183/09031936.04.00102704 [DOI] [PubMed] [Google Scholar]
- 20.Campo I, Luisetti M, Griese M, et al. Whole lung lavage therapy for pulmonary alveolar proteinosis: a global survey of current practices and procedures. Orphanet J Rare Dis 2016; 11: 115. doi: 10.1186/s13023-016-0497-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Campo I, Luisetti M, Griese M, et al. A global survey on whole lung lavage in pulmonary alveolar proteinosis. Chest 2016; 150: 251–253. doi: 10.1016/j.chest.2016.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tazawa R, Nakata K, Inoue Y, et al. Granulocyte–macrophage colony-stimulating factor inhalation therapy for patients with idiopathic pulmonary alveolar proteinosis: a pilot study; and long-term treatment with aerosolized granulocyte–macrophage colony-stimulating factor: a case report. Respirology 2006; 11: Suppl., S61–S64. doi: 10.1111/j.1440-1843.2006.00811.x [DOI] [PubMed] [Google Scholar]
- 23.Shibata Y, Berclaz PY, Chroneos ZC, et al. GM-CSF regulates alveolar macrophage differentiation and innate immunity in the lung through PU.1. Immunity 2001; 15: 557–567. doi: 10.1016/S1074-7613(01)00218-7 [DOI] [PubMed] [Google Scholar]
- 24.Bonfield TL, Raychaudhuri B, Malur A, et al. PU.1 regulation of human alveolar macrophage differentiation requires granulocyte–macrophage colony-stimulating factor. Am J Physiol Lung Cell Mol Physiol 2003; 285: L1132–L1136. doi: 10.1152/ajplung.00216.2003 [DOI] [PubMed] [Google Scholar]
- 25.Schoch OD, Schanz U, Koller M, et al. BAL findings in a patient with pulmonary alveolar proteinosis successfully treated with GM-CSF. Thorax 2002; 57: 277–280. doi: 10.1136/thorax.57.3.277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shibata Y, Berclaz p-Y, Trapnell BC. Arrest of alveolar macrophage differentiation, in vivo, in GM-CSF-deficient mice is associated with altered expression of transcription factors PU.1 and ICSBP. Respir Crit Care Med 2001; 163: A790. [Google Scholar]
- 27.Berclaz PY, Shibata Y, Whitsett JA, et al. GM-CSF, via PU.1, regulates alveolar macrophage FcγR-mediated phagocytosis and the IL-18/IFN-γ-mediated molecular connection between innate and adaptive immunity in the lung. Blood 2002; 100: 4193–4200. doi: 10.1182/blood-2002-04-1102 [DOI] [PubMed] [Google Scholar]
- 28.Berclaz PY, Zsengeller Z, Shibata Y, et al. Endocytic internalization of adenovirus, nonspecific phagocytosis, and cytoskeletal organization are coordinately regulated in alveolar macrophages by GM-CSF and PU.1. J Immunol 2002; 169: 6332–6342. doi: 10.4049/jimmunol.169.11.6332 [DOI] [PubMed] [Google Scholar]
- 29.Berclaz PY, Carey B, Fillipi MD, et al. GM-CSF regulates a PU.1–dependent transcriptional program determining the pulmonary response to LPS. Am J Respir Cell Mol Biol 2007; 36: 114–121. doi: 10.1165/rcmb.2006-0174OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arai T, Hamano E, Inoue Y, et al. Serum neutralizing capacity of GM-CSF reflects disease severity in a patient with pulmonary alveolar proteinosis successfully treated with inhaled GM-CSF. Respir Med 2004; 98: 1227–1230. doi: 10.1016/j.rmed.2004.08.011 [DOI] [PubMed] [Google Scholar]
- 31.Price A, Manson D, Cutz E, et al. Pulmonary alveolar proteinosis associated with anti-GM-CSF antibodies in a child: successful treatment with inhaled GM-CSF. Pediatr Pulmonol 2006; 41: 367–370. doi: 10.1002/ppul.20347 [DOI] [PubMed] [Google Scholar]
- 32.Arndt CA, Koshkina NV, Inwards CY, et al. Inhaled granulocyte–macrophage colony-stimulating factor for first pulmonary recurrence of osteosarcoma: effects on disease-free survival and immunomodulation. A report from the Children's Oncology Group. Clin Cancer Res 2010; 16: 4024–4030. doi: 10.1158/1078-0432.CCR-10-0662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ohashi K, Sato A, Takada T, et al. Direct evidence that GM-CSF inhalation improves lung clearance in pulmonary alveolar proteinosis. Respir Med 2012; 106: 284–293. doi: 10.1016/j.rmed.2011.10.019 [DOI] [PubMed] [Google Scholar]
- 34.Papiris SA, Tsirigotis P, Kolilekas L, et al. Long-term inhaled granulocyte–macrophage colony-stimulating factor in autoimmune pulmonary alveolar proteinosis: effectiveness, safety, and lowest effective dose. Clin Drug Investig 2014; 34: 553–564. doi: 10.1007/s40261-014-0208-z [DOI] [PubMed] [Google Scholar]
- 35.Gajewska ME, Sritharan SS, Santoni-Rugiu E, et al. Autoimmune pulmonary alveolar proteinosis in an adolescent successfully treated with inhaled rhGM-CSF (molgramostim). Respir Med Case Rep 2018; 23: 167–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wylam ME, Ten R, Prakash UB, et al. Aerosol granulocyte-macrophage colony-stimulating factor for pulmonary alveolar proteinosis. Eur Respir J 2006; 27: 585–593. doi: 10.1183/09031936.06.00058305 [DOI] [PubMed] [Google Scholar]
- 37.Kusakabe Y, Uchida K, Hiruma T, et al. A standardized blood test for the routine clinical diagnosis of impaired GM-CSF signaling using flow cytometry. J Immunol Methods 2014; 413: 1–11. doi: 10.1016/j.jim.2014.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lerman J, Bruce RA, Sivarajan E, et al. Low-level dynamic exercises for earlier cardiac rehabilitation: aerobic and hemodynamic responses. Arch Phys Med Rehabil 1976; 57: 355–360. [PubMed] [Google Scholar]
- 39.Luisetti M, Kroneberg P, Suzuki T, et al. Physical properties, lung deposition modeling, and bioactivity of recombinant GM-CSF aerosolised with a highly efficient nebulizer. Pulm Pharmacol Ther 2011; 24: 123–127. doi: 10.1016/j.pupt.2010.08.004 [DOI] [PubMed] [Google Scholar]
- 40.Tazawa R, Trapnell BC, Inoue Y, et al. Inhaled granulocyte–macrophage colony-stimulating factor as therapy for pulmonary alveolar proteinosis. Am J Respir Crit Care Med 2010; 181: 1345–1354. doi: 10.1164/rccm.200906-0978OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Inoue Y, Trapnell BC, Tazawa R, et al. Characteristics of a large cohort of patients with autoimmune pulmonary alveolar proteinosis in Japan. Am J Respir Crit Care Med 2008; 177: 752–762. 10.1164/rccm.200708-1271OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Trapnell BC, Inoue Y, Bonella F, et al. Inhaled molgramostim therapy in autoimmune pulmonary alveolar proteinosis. N Engl J Med 2020; 383: 1635–1644. doi: 10.1056/NEJMoa1913590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ohkouchi S, Akasaka K, Ichiwata T, et al. Sequential granulocyte–macrophage colony-stimulating factor inhalation after whole-lung lavage for pulmonary alveolar proteinosis. A report of five intractable cases. Ann Am Thorac Soc 2017; 14: 1298–1304. doi: 10.1513/AnnalsATS.201611-892BC [DOI] [PubMed] [Google Scholar]
- 44.Tazawa R, Ueda T, Abe M, et al. Inhaled GM-CSF for pulmonary alveolar proteinosis. N Engl J Med 2019; 381: 923–932. doi: 10.1056/NEJMoa1816216 [DOI] [PubMed] [Google Scholar]
- 45.Campo I, Mariani F, Rodi G, et al. Assessment and management of pulmonary alveolar proteinosis in a reference center. Orphanet J Rare Dis 2013; 8: 40. doi: 10.1186/1750-1172-8-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bonella F, Bauer PC, Griese M, et al. Wash-out kinetics and efficacy of a modified lavage technique for alveolar proteinosis. Eur Respir J 2012; 40: 1468–1474. doi: 10.1183/09031936.00017612 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material ERJ-01233-2023.SUPPLEMENT (918.5KB, pdf)
This one-page PDF can be shared freely online.
Shareable PDF ERJ-01233-2023.Shareable (806.3KB, pdf)