Abstract
Background
Disparities have been found in the utilization of palliative care (PC). However, a limitation of existing research is that it co-mingles factors affecting whether a patient is offered PC with factors affecting whether a patient accepts/refuses PC. Our objective is to identify the determinants and disparities of neurosurgery patients accepting/refusing inpatient PC after a provider recommends an inpatient PC consult.
Methodology
In this single-center retrospective cohort study, the last 750 consecutive neurosurgery patient medical records were screened. Inclusion criteria were as follows: (1) the patient was seen by the neurosurgery service during their hospitalization and (2) the patient had a documented inpatient PC consult ordered or the patient had at least one progress note documenting PC in the plan of care. Excluded were patients not seen by the neurosurgery service during the hospitalization in which the PC consult order or plan was documented. Analysis was performed using multivariate logistic regression with backward stepwise variable selection. Candidate variables included age, gender, race, ethnicity, language, marital status, insurance type, surrogate decision-maker (SDM) relationship to patient, advanced directive, Charlson Comorbidity Index (CCI), ambulation, activities of daily living (ADL) dependence, primary diagnosis category, Glasgow Coma Scale (GCS) at the time of admission, GCS at the time of PC consult, GCS at the time of discharge, duration of hospitalization, and hospitalization mortality.
Results
Of the last 750 neurosurgery patients, this study included 144 patients (33.3% female; mean age 57.53±19.89 years). Among these patients, 109 patients (75.7%) accepted PC and 35 patients (24.3%) refused PC. Univariate analysis showed that patients refusing PC tended to be older (p=0.003) and have a shorter duration of hospitalization (p=0.023). Chi-squared analysis found associations between PC acceptance/refusal and preferred language (p=0.026), religion (p<0.001), and SDM relationship to patient (p=0.004). Multivariate logistic regression found that predictors of PC refusal were older age (OR=0.965, p=0.049), non-English (OR=0.219, p=0.004), adult child SDM (OR=0.246, p=0.023), and other relative/friend SDM (OR=0.208, p=0.011). Religious patients were more likely to accept PC (OR=7.132, p<0.001). Race and ethnicity factors were not found to be significant predictors of PC refusal: Black (p=0.649), other race (p=0.189), and Hispanic (p=0.525).
Conclusion
Nearly one-quarter of neurosurgery patients offered PC refused this care. Predictors of PC refusal were older age, non-English, adult child SDM, and other relative/friend SDM. Religious patients were more likely to accept PC. Race and ethnicity were not found to be significant predictors of accepting/refusing PC, which may suggest these previously identified disparities stem from minority patients being offered less PC. Additional research is needed to replicate these findings among different patient populations. Because PC is compatible with life-prolonging therapies and aims to provide additional emotional and spiritual support to the patient and family, the finding that nearly one-quarter of patients refused PC may demonstrate a pervasive misconception and need for patient education.
Keywords: surrogate decision-maker, minority, ethnicity, race, religion, age, palliative care, neurosurgery, disparity, determinant
Introduction
A growing body of research investigates the utilization of palliative care (PC) and the disparities therein. Drivers of PC utilization can be subdivided into supply and demand factors. Supply factors are those that affect whether a referral is given and have been identified as a lack of resources; lack of provider awareness of available resources; referrer reluctance due to fear of upsetting/abandoning the patient, admitting failure, or not understanding the benefit of PC; and restrictive program eligibility [1]. Demand factors are those that affect whether a patient accepts/refuses PC and include a reluctance to acknowledge suffering or death [2], fear of disease controlling treatment withdrawn [1], mistrust of the healthcare system [3], and lack of awareness or understanding of PC [4].
Ubiquitous in this area of research are retrospective studies examining the binary outcome of whether a patient receives PC and comparing demographic differences to report disparities [5-10]. A limitation of this research design is that it co-mingles these supply and demand factors. Our research adds to the literature by building upon this knowledge and investigates demand-side disparities through examining PC utilization among patients who have already been offered an inpatient PC consult.
Neurosurgery patients are among the largest groups of patients receiving PC [11], and it has been shown that racial and ethnic disparities exist among this population, particularly with White patients receiving nearly twice the rate of PC utilization compared to Black and Hispanic patients with severe traumatic brain injuries [12]. Our study aims to identify the determinants and disparities of PC acceptance/refusal among neurosurgery patients after a provider recommends an inpatient PC consult to better understand utilization from the patient perspective.
Materials and methods
This single-center retrospective cohort study was performed at Arrowhead Regional Medical Center (ARMC), a tertiary care trauma and stroke center in southern California. Approval was obtained from the IRB in connection with ARMC for this protocol (approval number: 22-30). Medical records of the last 750 consecutive neurosurgery patients were screened using inclusion and exclusion criteria. Inclusion criteria were as follows: (1) the patient was seen by the neurosurgery service during their hospitalization and (2) the patient had a documented inpatient PC consult ordered or the patient had at least one progress note documenting PC in the plan of care. Excluded were patients not seen by the neurosurgery service during the hospitalization in which the PC consult order or plan was documented.
While the surrogate decision-maker (SDM) accepted/refused PC on behalf of the patients in this study, the authors abbreviate this scenario for simplicity by stating that the patient accepted/refused PC. A patient was considered to have been offered PC if their chart showed either a PC consult order or a progress note with PC documented in the plan of care. A patient was considered to have accepted PC if the chart showed the presence of at least one PC consult or progress note authored by a member of the PC service. A patient was considered to have refused PC if (1), explicitly, the PC consult order was discontinued with the stated reason being "patient refused" or (2), implicitly, if the patient was offered PC (as defined above) and no notes authored by the PC service exist. The primary outcome under investigation was the acceptance/refusal of PC after a consult had been recommended by a provider. Using these criteria, our sample included 144 patients.
Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 28.0 (Released 2021; IBM Corp., Armonk, New York, United States) (142). Summary statistics for quantitative data have been reported using mean±standard deviation (SD) and nominal data as percentages. Qualitative variables were analyzed using the chi-squared (ꭓ2) or Fisher's exact test, and quantitative variables were analyzed using the t-test or analysis of variance (ANOVA) with a significance level of <0.05. Two multivariate logistic regression models were created to assess candidate determinants of acceptance/refusal of PC among neurosurgery patients. For Model 1, variable selection was performed using backward stepwise selection with a threshold p-value of 0.1. Candidate variables entered into Model 1 prior to backward stepwise selection included age, gender, race, ethnicity, language, marital status, insurance type, SDM relationship to patient, advanced directive, comorbidity burden measured by the Charlson Comorbidity Index (CCI) [13], ambulation, activities of daily living (ADL) dependence, primary diagnosis category, Glasgow Coma Scale (GCS) at the time of admission, GCS at the time of PC consult, GCS at the time of discharge, duration of hospitalization, and hospitalization mortality. For Model 2, variable selection included those selected in Model 1 and, additionally, manual selection of race and ethnicity factors. Results were reported as odds ratios (OR) and 95% confidence intervals (CI) with a forest plot.
Results
Upon review of the last 750 consecutive neurosurgery patients, this study included 144 patients (33.3% female; mean age 57.53±19.89 years). Among these patients, 109 patients (75.7%) accepted PC and 35 patients (24.3%) refused PC. Table 1 shows the patient demographics and characteristics dichotomized by decision to accept/refuse PC. Univariate analysis showed that patients refusing PC tended to be older (p=0.003) and have a shorter duration of hospitalization (p=0.023). Chi-squared analysis found associations between PC acceptance/refusal and preferred language (p=0.026), religion (p<0.001), and SDM relationship to patient (p=0.004).
Table 1. Patient demographics and characteristics.
***: statistically significant; p<0.05; PC: palliative care; SD: standard deviation; CCI: Charlson Comorbidity Index; ADL: activities of daily living; GCS: Glasgow Coma Scale
Accepting PC is defined as having a PC consult or progress note authored by the PC service. Medicaid insurance category includes all patients with Medicaid regardless of other coverage. Private insurance category includes all patients with private insurance regardless of other coverage. Medicare insurance category includes patients with only Medicare insurance. Other relative/friend SDM includes siblings and non-first-degree relatives.
| Accepted PC | Refused PC | ||||
| Characteristic | Mean (n) | SD (%) | Mean (n) | SD (%) | p-value |
| n | 109 | 75.7% | 35 | 24.3% | |
| Age (in years) | 54.74 | 19.63 | 66.23 | 18.65 | 0.003*** |
| <18 | 0 | 0.0% | 0 | 0.0% | |
| 18-65 | 75 | 68.8% | 17 | 48.6% | |
| >65 | 34 | 31.2% | 18 | 51.4% | |
| Gender | 0.583 | ||||
| Male | 74 | 67.9% | 22 | 62.9% | |
| Female | 35 | 32.1% | 13 | 37.1% | |
| Race | 0.765 | ||||
| White | 46 | 42.2% | 13 | 37.1% | |
| Black | 11 | 10.1% | 2 | 5.7% | |
| Asian | 4 | 3.7% | 1 | 2.9% | |
| Other | 37 | 33.9% | 16 | 45.7% | |
| Unknown | 11 | 10.1% | 3 | 8.6% | |
| Ethnicity | 0.175 | ||||
| Hispanic | 59 | 54.1% | 25 | 71.4% | |
| Not Hispanic | 39 | 35.8% | 7 | 20.0% | |
| Unknown | 11 | 10.1% | 3 | 8.6% | |
| Preferred language | 0.026*** | ||||
| English | 76 | 69.7% | 16 | 45.7% | |
| Non-English | 27 | 24.8% | 17 | 48.6% | |
| Unknown | 6 | 5.5% | 2 | 5.7% | |
| Marital status | 0.097 | ||||
| Single | 43 | 39.4% | 11 | 31.4% | |
| Married | 40 | 36.7% | 10 | 28.6% | |
| Widowed | 6 | 5.5% | 7 | 20.0% | |
| Divorced | 6 | 5.5% | 1 | 2.9% | |
| Unknown | 14 | 12.8% | 6 | 17.1% | |
| Religion | <0.001*** | ||||
| Catholic | 50 | 45.9% | 13 | 37.1% | |
| Christian | 31 | 28.4% | 2 | 5.7% | |
| Other | 6 | 5.5% | 0 | 0.0% | |
| None | 8 | 7.3% | 4 | 11.4% | |
| Unknown | 14 | 12.8% | 16 | 45.7% | |
| Insurance | 0.633 | ||||
| Medicaid | 64 | 58.7% | 19 | 54.3% | |
| Private | 27 | 24.8% | 7 | 20.0% | |
| Medicare | 3 | 2.8% | 1 | 2.9% | |
| Uninsured | 15 | 13.8% | 8 | 22.9% | |
| Surrogate decision-maker | 0.004*** | ||||
| Spouse | 40 | 36.7% | 6 | 17.1% | |
| Parent | 24 | 22.0% | 2 | 5.7% | |
| Adult child | 20 | 18.3% | 15 | 42.9% | |
| Other relative/friend | 25 | 22.9% | 12 | 34.3% | |
| Pre-hospitalization CCI | 3.20 | 3.09 | 3.23 | 2.40 | 0.963 |
| Pre-hospitalization ambulatory status | 0.126 | ||||
| Ambulatory | 87 | 79.8% | 22 | 62.9% | |
| Ambulatory with assistive device | 10 | 9.2% | 6 | 17.1% | |
| Non-ambulatory | 12 | 11.0% | 7 | 20.0% | |
| Pre-hospitalization ADL | 0.153 | ||||
| Independent | 90 | 82.6% | 25 | 71.4% | |
| Dependent | 19 | 17.4% | 10 | 28.6% | |
| Principal diagnosis category | 0.844 | ||||
| Trauma | 50 | 45.9% | 15 | 42.9% | |
| Tumor | 21 | 19.3% | 8 | 22.9% | |
| Hemorrhagic stroke | 23 | 21.1% | 6 | 17.1% | |
| Ischemic stroke | 8 | 7.3% | 2 | 5.7% | |
| Other | 7 | 6.4% | 4 | 11.4% | |
| GCS | |||||
| GCS at admission | 9.43 | 4.92 | 10.74 | 4.80 | 0.415 |
| GCS at palliative consult | 8.02 | 4.82 | 8.91 | 5.38 | 0.094 |
| GCS at discharge | 7.53 | 5.13 | 8.51 | 5.63 | 0.067 |
| Days of hospitalization | 21.31 | 22.62 | 12.06 | 13.48 | 0.023*** |
| Days until PC consult | 7.21 | 11.23 | 7.40 | 11.30 | 0.931 |
| Advanced directive | 0.937 | ||||
| Yes | 13 | 11.9% | 4 | 11.4% | |
| No | 96 | 88.1% | 31 | 88.6% | |
| Hospitalization mortality | 0.929 | ||||
| Yes | 52 | 47.7% | 17 | 48.6% | |
| No | 57 | 52.3% | 18 | 51.4% | |
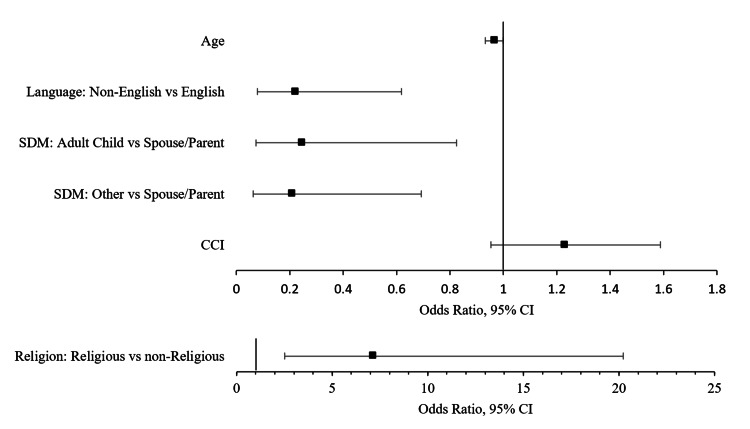
Multivariate logistic regression was used to assess predictors of acceptance/refusal of PC. For Model 1, backward stepwise selection using a threshold p-value of 0.1 included the following independent variables: age, non-English, religious, adult child SDM, other relative/friend SDM, and pre-hospitalization CCI. The comparison case reflected by the constant is English, non-religious, and spouse or parent SDM. Model 1 correctly predicted 79.9% of cases with a Cox and Snell R2 of 0.265 (Table 2). Significant predictors of PC refusal were age (OR=0.965, p=0.049), non-English (OR=0.219, p=0.004), adult child SDM (OR=0.246, p=0.023), and other relative/friend SDM (OR=0.208, p=0.011). Religious patients were significantly more likely to accept PC (OR=7.132, p<0.001). A forest plot is shown in Figure 1.
Table 2. Model 1 logistic regression with backward stepwise selection for neurosurgery patients accepting PC.
***: statistically significant; p<0.05; CI: confidence interval; PC: palliative care; CCI: Charlson Comorbidity Index
Other relative/friend SDM includes siblings and non-first-degree relatives. Accepting PC is defined as having a PC consult or progress note authored by the PC service.
| Variable | Odds ratio | Lower 95% CI | Upper 95% CI | p-value | |
| Y | Accepted PC | ||||
| X0 | Constant | 18.922 | 0.003*** | ||
| X1 | Age | 0.965 | 0.932 | 1 | 0.049*** |
| X2 | Non-English | 0.219 | 0.078 | 0.619 | 0.004*** |
| X3 | Religious | 7.132 | 2.514 | 20.228 | <0.001*** |
| X4 | Adult child SDM | 0.246 | 0.074 | 0.825 | 0.023*** |
| X5 | Other relative/friend SDM | 0.208 | 0.063 | 0.693 | 0.011*** |
| X6 | CCI | 1.231 | 0.953 | 1.588 | 0.111 |
Figure 1. Model 1 forest plot of logistic regression output for neurosurgery patients accepting PC.
PC: palliative care; SDM: surrogate decision-maker: CCI: Charlson Comorbidity Index; GCS: Glasgow Coma Scale
Religion was plotted in a separate forest plot for clarity using a different axis scale. Significant predictors include age (OR=0.965, p=0.049), non-English (OR=0.219, p=0.004), adult child SDM (OR=0.246, p=0.023), other relative/friend SDM (OR=0.208, p=0.011), and religious (OR=7.132, p<0.001).
Model 2, with the manual addition of race and ethnicity variables including Black, other race, and Hispanic, correctly predicted 79.2% of cases with a Cox and Snell R2 of 0.278 (Table 3). All predictors identified as significant in Model 1 were robust and significant in Model 2. Race and ethnicity factors were not found to be significant predictors of PC refusal: Black (p=0.649), other race (p=0.189), and Hispanic (p=0.525).
Table 3. Model 2 logistic regression including race and ethnicity predictors for neurosurgery patients accepting PC.
***: statistically significant; p<0.05; CI: confidence interval; PC: palliative care; CCI: Charlson Comorbidity Index
Other relative/friend SDM includes siblings and non-first-degree relatives. Accepting PC is defined as having a PC consult or progress note authored by the PC service.
| Variable | Odds ratio | Lower 95% CI | Upper 95% CI | p-value | |
| Y | Accepted PC | ||||
| X0 | Constant | 40.892 | 0.001*** | ||
| X1 | Age | 0.96 | 0.926 | 0.995 | 0.027*** |
| X2 | Non-English | 0.273 | 0.093 | 0.804 | 0.018*** |
| X3 | Religious | 8.009 | 2.751 | 23.316 | <0.001*** |
| X4 | Adult child SDM | 0.282 | 0.08 | 0.989 | 0.048*** |
| X5 | Other relative/friend SDM | 0.207 | 0.059 | 0.725 | 0.014*** |
| X6 | CCI | 1.25 | 0.964 | 1.621 | 0.092 |
| X7 | Black | 0.625 | 0.083 | 4.731 | 0.649 |
| X8 | Other race | 0.49 | 0.169 | 1.419 | 0.189 |
| X9 | Hispanic | 0.68 | 0.207 | 2.231 | 0.525 |
Discussion
This study aims to identify the determinants and disparities of PC acceptance/refusal among neurosurgery patients after a provider recommends an inpatient PC consult to better understand utilization from the patient perspective. While the SDM accepted/refused PC on behalf of the patients in this study, the authors abbreviate this scenario by stating that the patient accepted/refused PC. Nearly one-quarter of neurosurgery patients in this study who were offered PC refused this care. We found that predictors of PC refusal included older age, non-English, adult child SDM, and other relative/friend SDM. Religious patients were more likely to accept PC. Race and ethnicity factors were not found to be predictors of PC acceptance/refusal.
Given that PC is compatible with life-prolonging therapies and aims to provide emotional and spiritual support for not only the patient but also the family, the finding that nearly one-quarter of SDMs refused PC should be seen as a communication failure [2,14,15]. Thematically, we found that PC given to neurosurgery patients typically involved supporting the family through answering questions, providing bereavement support, and liaising with chaplain services. If presented in this manner, it is unlikely such a high proportion of SDMs would decline the additional support. This proposed communication failure is supported by the finding that non-English patients were significantly more likely to refuse PC. While the language preference of the patient does not necessarily reflect that of the SDM, the robustness of this finding in Model 2 while holding race and ethnicity factors constant suggests that the non-English variable measured some degree of communication barriers between SDMs and providers such that there was a significantly higher rate of PC refusal.
Race and ethnicity were a focus of this analysis because prior work demonstrated these disparities among neurosurgery patients [12]. Although these factors were not selected for inclusion in Model 1 using backward stepwise selection, they were manually added in Model 2 and found insignificant in the acceptance/refusal of PC. Our results do not contradict existing literature that has repeatedly shown race and ethnicity to be associated with decreased PC utilization [5-9,12,16-19]. Rather, the finding that race and ethnicity are not predictors of PC refusal after PC has been recommended suggests that these disparities may be supply-side driven and instead predict whether providers offer PC. Future research could evaluate this supply-side claim by collecting demographic data of patients who meet predefined criteria for PC and comparing patients who are offered PC with those who are not offered PC. Additionally, because it has been found that inpatient settings mitigate racial and ethnic disparities in PC utilization, outpatient PC should be included in the analysis [17].
Neurosurgery patients are a unique subset of PC patients due to their frequent incapacitation which necessitates an SDM [20]. The average GCS at the time of PC consult for patients in our study who refused vs. accepted PC was 8.91 vs. 8.02, respectively. The fundamental challenge SDMs face is reconciling their own wishes with their loved one's values [21-23]. We found that adult child and other relative/friend SDMs, who often have less insight into the patient's wishes than spouse and parent SDMs, were significantly more likely to refuse PC. This underscores the courage necessary to make end-of-life decisions and may suggest that the less confident the SDM is of the patient's wishes, the less likely the SDM is to accept a comfort approach to care even if compatible with life-prolonging therapies. Additionally, SDMs with less insight into the patient's wishes may be more susceptible to engaging in behaviors known to contribute to PC refusal such as focusing on small details while avoiding the big picture, relying on personal beliefs about the patient, seeking confirmation bias of favorable prognosis from other sources, and avoiding prognostic information [24].
This study also found that older patients were more likely to refuse PC. These results are consistent with a systematic review finding significantly lower use of PC among cancer patients above the age of 65 compared to younger adult cancer patients [25]. The authors hypothesized that (1) older patients may have a reduced need for PC for symptom management due to self-reporting symptoms less frequently as "very distressing" [26] and (2) older patients may have their needs for PC met through other providers such as their generalist. Because neurosurgery patients from this sample had acute conditions and were often incapacitated requiring the involvement of SDMs, our findings are not supported by these hypotheses. We hypothesize that the link between older age and PC refusal may be anticipation: older age is associated with more anticipation of suffering or death, which may heighten denial of these topics among both patients and SDMs.
This study found that religious patients were more likely to accept PC, which is consistent with results from existing literature. In addition to religion being important to patients and families in end-of-life care, religiousness has been found to be associated with wanting all measures to extend life [27-29]. Our finding may reflect a communication success in explaining to SDMs that that PC is compatible with life-prolonging therapies and providing spiritual support, which commonly involved liaising with chaplain services.
A limitation of this study is generalizability due to the patient population. ARMC serves California's San Bernardino (SB) county, which is demographically heterogeneous from national averages with respect to its Hispanic/Latino population (67.6% SB vs. 18.9% US), language other than English spoken at home (52.2% SB vs. 21.7% US), and persons in poverty (20.9% SB vs. 11.6% US) [30]. Therefore, these findings should be interpreted cautiously until further replication in different geographies among different patient populations. Second, misclassification bias may have occurred if a miscommunication existed between a provider documenting a recommendation for PC and the PC service actually seeing the patient. Third, demographic data such as language spoken reflects the patient rather than the SDM who accepted/refused the PC. Fourth, race and ethnicity data were taken from the medical record and may have under-represented multiracial patients. Lastly, this study only included PC rendered by the inpatient PC service, and data of subsequent outpatient PC was not available.
Conclusions
Nearly one-quarter of neurosurgery patients offered PC refused this care. Predictors of PC refusal were older age, non-English, adult child SDM, and other relative/friend SDM. Religious patients were more likely to accept PC. Race and ethnicity were not found to be significant predictors of accepting/refusing PC, which may suggest these previously identified disparities stem from minority patients being offered less PC. Additional research is needed to replicate these findings among different patient populations. Because PC is compatible with life-prolonging therapies and aims to provide additional emotional and spiritual support to the patient and family, the finding that nearly one-quarter of patients refused PC may demonstrate a pervasive misconception and need for patient education.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Arrowhead Regional Medical Center IRB issued approval 22-30. The information provided was reviewed and accepted by the Institutional Review Board
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Barriers to access to palliative care. Hawley P. Palliat Care. 2017;10:1178224216688887. doi: 10.1177/1178224216688887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Discussing palliative care with patients. Lo B, Quill T, Tulsky J, et al. Ann Intern Med. 1999;130:744–749. [PubMed] [Google Scholar]
- 3.Cultural mistrust and use of hospice care: challenges and remedies. Cort MA. J Palliat Med. 2004;7:63–71. doi: 10.1089/109662104322737269. [DOI] [PubMed] [Google Scholar]
- 4.Demographic factors and awareness of palliative care and related services. Koffman J, Burke G, Dias A, Raval B, Byrne J, Gonzales J, Daniels C. Palliat Med. 2007;21:145–153. doi: 10.1177/0269216306074639. [DOI] [PubMed] [Google Scholar]
- 5.Racial disparity in hospice use in the United States in 2002. Connor SR, Elwert F, Spence C, Christakis NA. Palliat Med. 2008;22:205–213. doi: 10.1177/0269216308089305. [DOI] [PubMed] [Google Scholar]
- 6.Ethnic disparities in hospice use among Asian-American and Pacific Islander patients dying with cancer. Ngo-Metzger Q, Phillips RS, McCarthy EP. J Am Geriatr Soc. 2008;56:139–144. doi: 10.1111/j.1532-5415.2007.01510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hospice use by Hispanic and non-Hispanic white cancer decedents. Lackan NA, Ostir GV, Freeman JL, Kuo YF, Zhang DD, Goodwin JS. Health Serv Res. 2004;39:969–983. doi: 10.1111/j.1475-6773.2004.00267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hospice usage by minorities in the last year of life: results from the National Mortality Followback Survey. Greiner KA, Perera S, Ahluwalia JS. J Am Geriatr Soc. 2003;51:970–978. doi: 10.1046/j.1365-2389.2003.51310.x. [DOI] [PubMed] [Google Scholar]
- 9.Racial and ethnic differences in hospice use among patients with heart failure. Givens JL, Tjia J, Zhou C, Emanuel E, Ash AS. Arch Intern Med. 2010;170:427–432. doi: 10.1001/archinternmed.2009.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Race/ethnicity, socioeconomic status, and healthcare intensity at the end of life. Brown CE, Engelberg RA, Sharma R, et al. J Palliat Med. 2018;21:1308–1316. doi: 10.1089/jpm.2018.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palliative care needs of patients with neurologic or neurosurgical conditions. Chahine LM, Malik B, Davis M. Eur J Neurol. 2008;15:1265–1272. doi: 10.1111/j.1468-1331.2008.02319.x. [DOI] [PubMed] [Google Scholar]
- 12.Palliative care consultations in patients with severe traumatic brain injury: who receives palliative care consultations and what does that mean for utilization? Williamson TL, Adil SM, Shalita C, et al. Neurocrit Care. 2022;36:781–790. doi: 10.1007/s12028-021-01366-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Charlson ME, Pompei P, Ales KL, MacKenzie CR. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 14.Palliative care: the World Health Organization's global perspective. Sepúlveda C, Marlin A, Yoshida T, Ullrich A. J Pain Symptom Manage. 2002;24:91–96. doi: 10.1016/s0885-3924(02)00440-2. [DOI] [PubMed] [Google Scholar]
- 15.Clinical practice. Palliative care. Morrison RS, Meier DE. N Engl J Med. 2004;350:2582–2590. doi: 10.1056/NEJMcp035232. [DOI] [PubMed] [Google Scholar]
- 16.Racial and ethnic disparities in palliative care. Johnson KS. J Palliat Med. 2013;16:1329–1334. doi: 10.1089/jpm.2013.9468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Disparities in palliative care in patients with cancer. Griggs JJ. J Clin Oncol. 2020;38:974–979. doi: 10.1200/JCO.19.02108. [DOI] [PubMed] [Google Scholar]
- 18.Gaps in provision of primary and specialty palliative care in the acute care setting by race and ethnicity. Chuang E, Hope AA, Allyn K, Szalkiewicz E, Gary B, Gong MN. J Pain Symptom Manage. 2017;54:645–653. doi: 10.1016/j.jpainsymman.2017.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Racial and ethnic disparities in palliative care: a systematic scoping review. Gardner DS, Doherty M, Bates G, et al. Fam Soc. 2018;99:301–316. [Google Scholar]
- 20.The changing role of palliative care in the ICU. Aslakson RA, Curtis JR, Nelson JE. Crit Care Med. 2014;42:2418–2428. doi: 10.1097/CCM.0000000000000573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.I don't want to be the one saying 'we should just let him die': intrapersonal tensions experienced by surrogate decision makers in the ICU. Schenker Y, Crowley-Matoka M, Dohan D, Tiver GA, Arnold RM, White DB. J Gen Intern Med. 2012;27:1657–1665. doi: 10.1007/s11606-012-2129-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hope, truth, and preparing for death: perspectives of surrogate decision makers. Apatira L, Boyd EA, Malvar G, Evans LR, Luce JM, Lo B, White DB. Ann Intern Med. 2008;149:861–868. doi: 10.7326/0003-4819-149-12-200812160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Identifying family members who may struggle in the role of surrogate decision maker. Majesko A, Hong SY, Weissfeld L, White DB. Crit Care Med. 2012;40:2281–2286. doi: 10.1097/CCM.0b013e3182533317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24."It hurts to know... and it helps": exploring how surrogates in the ICU cope with prognostic information. Schenker Y, White DB, Crowley-Matoka M, Dohan D, Tiver GA, Arnold RM. J Palliat Med. 2013;16:243–249. doi: 10.1089/jpm.2012.0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The effect of age on referral to and use of specialist palliative care services in adult cancer patients: a systematic review. Burt J, Raine R. Age Ageing. 2006;35:469–476. doi: 10.1093/ageing/afl001. [DOI] [PubMed] [Google Scholar]
- 26.Dying when you're old. Cartwright A. Age Ageing. 1993;22:425–430. doi: 10.1093/ageing/22.6.425. [DOI] [PubMed] [Google Scholar]
- 27.Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. Balboni TA, Vanderwerker LC, Block SD, Paulk ME, Lathan CS, Peteet JR, Prigerson HG. J Clin Oncol. 2007;25:555–560. doi: 10.1200/JCO.2006.07.9046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Religion, risk, and medical decision making at the end of life. Van Ness PH, Towle VR, O'Leary JR, Fried TR. J Aging Health. 2008;20:545–559. doi: 10.1177/0898264308317538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.How parents of children receiving pediatric palliative care use religion, spirituality, or life philosophy in tough times. Hexem KR, Mollen CJ, Carroll K, Lanctot DA, Feudtner C. J Palliat Med. 2011;14:39–44. doi: 10.1089/jpm.2010.0256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.United States Census Bureau: United States Census QuickFacts. [ Jul; 2023 ]. 2022. https://www.census.gov/quickfacts/fact/table/sanbernardinocitycalifornia/RHI225221 https://www.census.gov/quickfacts/fact/table/sanbernardinocitycalifornia/RHI225221