Abstract
Background
Breathing exercises have been reported to have positive physiological effects on the body. The incidence of hypertension has become a major risk factor for cardiac complications leading to higher morbidity and mortality. Our aim was to conduct a systematic review and meta-analysis to study the effect of breathing exercises on blood pressure (BP) and heart rate (HR).
Methods
A systematic review and meta-analysis analyzing randomized clinical trials (RCTs) about the effect of breathing exercises on blood pressure was conducted (PROSPERO Registration ID: CRD42022316413). PubMed, ScienceDirect, WebofScience, and Cochrane Library databases were screened for RCTs from January 2017 to September 2022. The main search terms included “breathing exercise”, “Pranayam”, “Bhramari”, “alternate nostril breathing”, “deep breathing”, “slow breathing”, “hypertension”, and “high blood pressure”. The primary outcome was the value of the systolic blood pressure and diastolic blood pressure after the intervention. The effect on heart rate was also analyzed as a secondary outcome.
Results
A total of 15 studies were included in the meta-analysis. Breathing exercises have a modest but significant effect on decreasing systolic blood pressure (−7.06 [-10.20, −3.92], P = <0.01) and diastolic blood pressure (−3.43 [-4.89, −1.97], P = <0.01) mm Hg. Additionally, breathing exercises were also observed to cause a significant decrease in the heart rate (−2.41 [-4.53, −0.30], P = 0.03) beats/minute.
Conclusion
In a comprehensive systematic review and meta-analysis of breathing exercises and its effect on BP and HR, there is a moderate but significant positive effect. The studies are not deprived of bias.
Keywords: Breathing exercises, Hypertension, Pranayam, Blood pressure, Systematic review
1. Introduction
Hypertension (HTN) is one of the most common causes of morbidity and mortality in developed countries. Currently, there are approximately one billion people suffering from HTN and it has been estimated that this figure might increase to 1.5 billion by 2025.1 According to the American Heart Association (AHA), HTN is defined as systolic blood pressure (SBP) > 140 mmHg and diastolic blood pressure (DBP) > 90 mmHg.2 As per the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, HTN is the most prevalent risk factor for cardiovascular diseases.3 Uncontrolled HTN may lead to various cardiovascular complications including stroke, aneurysm, myocardial infarction, and heart failure.4.
There is a strong correlation between blood pressure (BP) and adverse cardiovascular outcome and it is reported that even a small decrease of 5 mmHg BP in hypertensive patients can lead to an approximate 25 % decrease in cardiovascular complications.5 In the United States, around 75 % of hypertensive patients take medications to control their BP.6 The cost of anti-hypertensive drugs, and the burden on hospitalizations due to drug interaction, non-adherence, and complications add to 100–300 billion dollars per year.7 There are myriad medications that are available to control BP but only a few are utilized because of cost limitations, compliance issues, and adverse effects. The proven first-line therapy for HTN still remains a change in lifestyle including exercise, weight loss, and low sodium diet (DASH diet).8.
As per the 2015 National Health Statistics report, complementary and alternative medicine (CAM) is being used by approximately 33.2 % of the patients, in addition to medications.9 One of the non-pharmacological methods is device-guided breathing, which is recommended by the AHA to control BP,[10], [11], [12] but the high cost of the device is a limitation for its use. However, Hateren et al.13 and Landman et al.14 reported no short-term beneficial effect of device-guided breathing exercises on the reduction of BP among hypertensive patients.
Yoga is one of the forms of alternative therapy that is now being used to control hypertension, diabetes, and hypothyroidism, among many other co-morbidities. Yoga is an ancient tradition that incorporates asanas (postures), pranayama (breathing exercises), and dhyana (meditation).[15], [16], [17] Pranayam is made up of two words: ‘Prana’ and ‘Ayama’. Prana means ‘vital energy’ or ‘life force’ and Ayama means ‘expansion’. There are many kinds of breathing exercises like alternate nostril breathing (Nadi Suddhi), Sheetali Pranayama, Sheetkari pranayama, slow breathing, deep breathing, Kapalbati, Bhastrika, Bramari, Bahir Kumbhaka, Ujjayi pranayama, and others.
There are several studies examining the anti-hypertensive effect of Yoga.[18], [19], [20], [21] The effect of breathing exercises is not limited to controlling BP and HR but can also lead to an improvement in anxiety,22,23 depression,24 pain perception,25 chronic obstructive pulmonary disease,26 asthma,27 insomnia,28 stress,29 PTSD,30 and cancer.31 Although multiple studies have reported a positive effect of breathing exercises on reducing BP [[32], [33], [34]] and HR,32 there is no pooled data concluding this individual component of yoga leads to a decrease in BP and HR. Also, the degree to which breathing exercises can decrease BP and HR remains unclear.
To address this gap, this is the first systematic review and meta-analysis of the RCTs studying the effect of various breathing exercises on blood pressure (SBP and DBP) and heart rate (HR).
2. Materials and methods
2.1. Data sources and literature search
This systematic review and meta-analysis of the effect of breathing exercises on BP was conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. The protocol was registered on PROSPERO (Registration ID: CRD42022316413).
A thorough literature search was performed on PubMed, ScienceDirect, Cochrane library, and Web of Science for relevant articles from January 2017 to September 2022. Our search strategy included keywords such as “Breathing exercise*” OR “Pranayam*” OR “Bhramari” OR “Alternate nostril breathing” OR “Deep breathing” OR “Slow breathing” OR “Slow breathing” with “Hypertension” OR “High blood pressure”, while “pulmonary hypertension” was excluded. The detailed inclusion and exclusion criteria are stated below.
2.2. Inclusion and exclusion criteria
Inclusion criteria
-
•
Studies reporting the effect of breathing exercises on BP,
-
•
Peer-reviewed, English language articles (randomized clinical trials [RCT], cohort studies, case series),
-
•
Studies reporting the pre-and post-intervention BP,
-
•
Studies having a control group (non-intervention group),
-
•
Studies published between January 2017 and September 2022,
-
•
Studies including only adult subjects ≥18 years of age.
Exclusion criteria
-
•
Non-English language manuscripts,
-
•
Studies not reporting BP as an outcome,
-
•
Other literature (systematics reviews, meta-analysis, book chapters, conferences, case reports, posters),
-
•
Abstracts only were excluded because of a lack of methodology and outcomes,
-
•
Non-human studies.
2.3. Data extraction
The relevant articles from the selected databases were exported to the ‘Rayyan’ screening and data extraction web tool. The first step was to identify and eliminate the duplicates from all the retrieved articles. Each article was initially screened by two investigators (PG, AM) based on the title and abstracts, followed by full-text screening of selected articles to check for their relevance. References of the short-listed articles were also screened for additional studies. All disagreements were resolved with discussions between the two authors, or with input from a third independent author reviewer. The articles that did not meet the inclusion criteria were discarded from the study. The following data was extracted by investigators in duplication to Microsoft Excel from each paper: average SBP, DBP, HR before and after the intervention with standard deviation, type of intervention (breathing exercise), number of participants in control and case group, any adverse effects and location of the study performed along with the demographic details. Effect on SBP and DBP were the primary outcomes studied. The HR was the secondary outcome of interest. For the eligible studies in which the BP values were not present, the corresponding authors were emailed in order to provide the data.
2.4. Risk of bias
Cochrane Risk of Bias Tool 35 was used to determine the risk of bias in each study independently by two authors and disagreements were resolved by discussion to achieve a final decision. Each study was assessed based on the following domains: sequence generation, allocation concealment, blinding participants and personnel, blinding outcome assessors, incomplete outcome data, selective reporting and other bias (rating-low risk, high risk, unclear risk). Any discrepancies between the authors were resolved by a third reviewer through discussion.
2.5. Data analysis
All the data was analyzed by Review Manager (RevMan) Version 5.1 from the Cochrane Collaboration 36 and the forest plots were constructed with P = 0.05 as a cut-off point for removal. P < 0.05. (P < 0.10 for heterogeneity) was considered statistically significant. Subgroup analysis was conducted to investigate the sources of heterogeneity and to identify subgroups of patients who are more likely to benefit from the intervention. If the effect sizes are different between the subgroups, this suggests that the characteristic is moderating the effect of the intervention. Publication bias was assessed by visually inspecting funnel plots and employing Egger's regression test. Visual inspection of the funnel plot aimed to identify any asymmetry, while Egger's regression test evaluated the intercept of the funnel plot. A significant intercept in Egger's regression test suggests that the observed effect size is larger than the true effect size, indicating the presence of publication bias.
3. Results
3.1. Literature search
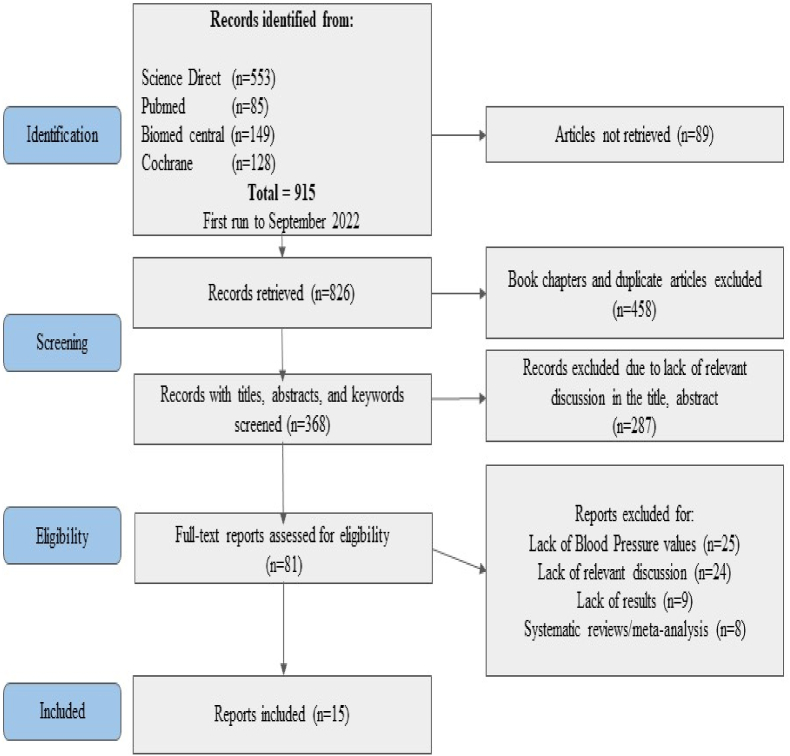
A total of 915 articles matched the inclusion criteria during the initial database search on PubMed, Cochrane library, ScienceDirect, and Web of Science. Of these, 89 articles were not retrieved. From the remaining 826 articles, 458 duplicates and book chapters were identified which were removed before the screening. The remaining 368 articles were screened by two authors independently and 287 articles were excluded due to a lack of relevant discussion in the title and abstract. Out of this, a total of 81 articles were sought for full-text review. Eventually, 15 articles that met the eligibility criteria were included and 66 articles were excluded (Fig. 1).
Fig. 1.
PRISMA flow diagram.
3.2. Study characteristics
The 15 included articles were published between January 2017 and September 2022. These articles were from several countries i.e., India (n = 6), Brazil (n = 2), Thailand (n = 1), Poland (n = 1), China (n = 1), USA (n = 1), Nepal (n = 1), Malaysia (n = 1) and Columbia (n = 1). These studies included a mean (±SD) of 75 ± 45 participants ranging from 21 to 170 (Table 1). There were a total of 1097 participants from all the included studies, with n = 586 (53 %) in the study group (practicing breathing exercise) and n = 511 (47 %) in the control group. The baseline characteristics in the study were similar between the case and control group (Table 2) [[37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50]]. Around 89 % completed the study in the breathing group as compared to 94 % in the control group. On baseline, the participants in the breathing group had a BMI of 26.9 (±2.3) as compared to the control group with the BMI of 27.2 (±2.2). An average age of 54.8 (±8.9) years was noted in the breathing group as compared to 54.4 (±8.7) years in the control group. The baseline SBP and DBP in the breathing group were 139.8 ± 11.1 mmHg and 84.7 ± 8.6 mmHg respectively as compared to 136.4 ± 12.0 mmHg and 83.7 ± 6.6 mmHg respectively in the control group. A baseline HR of 75.7 ± 7.9 bpm was noted in the breathing group as compared to 76.0 ± 7.7 bpm in the control group. The studies had 11 different types of breathing exercises i.e., slow loaded breathing (n = 7), Sheetali, Sheetkari Pranayam (n = 2), deep-breathing, alternate nostril breathing, yogic breathing, Ujjayi breathing, Bee-humming, Buteyko & Bhramari pranayam. The length of studies ranged from a single session to multiple sessions up to 90 days, and the duration of the breathing exercises ranged from 10 min to 75-min sessions (Table 1, Table 2). The breathing group was supervised in a total of 9 studies and was not supervised in six studies (Table 3). shows the characteristics of each included study. Fig. 2, Fig. 3, Fig. 4 shows the baseline characteristic difference in the SBP, DBP and HR in the case and control groups respectively.
Table 1.
Demographic details of studies included.
| Study details | Age (Case group) | Age (Control group) | Gender (Study group) ratio | Gender (Control group) ratio | |||||
|---|---|---|---|---|---|---|---|---|---|
| S.no. | Author/Date | Country | Type of breathing exercise studied | Mean | SD | Mean | SD | M:F | M:F |
| 1 | De Barros et al., 2017 | Brazil | Device guided slow breathing | 49 | 9 | 52 | 11 | 47 | 23/73 |
| 2 | Shetty et al., 2017 | India | Sheetali and Sheetkari pranayamas | – | – | – | – | – | |
| 3 | Li et al., 2017 | China | Slow breathing | 54.08 | 5.18 | 53.6 | 4.83 | 30 | 30/30 |
| 4 | Kow et al., 2018 | Malaysia | Music guided breathing | 62.6 | 9.6 | 59.7 | 9.6 | 57.1:42.9 | 48.9:51.1 |
| 5 | Ublosakka- Jones et al., 2018 | Thailand | Slow loaded breathing training | 66.4 | 4.2 | 68.2 | 4.8 | 1/8 | 8/8 |
| 6 | Kalaivani et al., 2019 | India | alternate nostril breathing exercise | – | – | – | – | 31/54 | 39/46 |
| 7 | Lachowska et al., 2019 | Poland | device-guided SLOWB | 52 | 17 | 52 | 17 | 16 (76 %) | 16 (76 %) |
| 8 | Misra et al., 2019 | Columbia | Yogic breathing exercises | 61.6 | 11.3 | 58.6 | 12 | 54:46:00 | 46:54:00 |
| 9 | Srinivasan et al., 2019 | India | Slow breathing (4 s inspiration and 6 s expiration) | 45.1 | 8.25 | 42.2 | 9.23 | 65/35 | 60/40 |
| 10 | Fetter et al., 2020 | Brazil | Ujjayi pranayam | 59 | 1.1 | 58 | 1.2 | 14 | All Females |
| 11 | Ghati et al., 2021 | India | Bee-humming exercise | 49.59 | 7.88 | 48.25 | 8.45 | 53:47:00 | 54:46:00 |
| 12 | Sathe et al., 2020 | India | Buteyko breathing and bhramari group | 60.57 | 8.96 | 59.71 | 8.95 | 11 | 11:10 |
| 13 | Thanalakshmi et al., 2020 | India | Sheetali pranayama | 37.8 | 12.21 | 39.2 | 10.8 | 28/12 | 29/11 |
| 14 | Dhungana et al., 2021 | Nepal | Pranayam | 47.1 | 11 | 48.4 | 10.7 | 42.6:57.4 | 61.6:38.3 |
| 15 | Craighead et al., 2021 | USA | high‐resistance Inspiratory muscle strength training (IMST) | 67 | 2 | 67 | 2 | 8 | 9:09 |
Table 2.
Characteristics of studies included.
| S.no. | Author/Location/Date | Sample size (breathing, control) | % completed (breathing, Control) | Study population | Breathing exercise intervention (study group) | Breathing exercise frequency/duration of session | Adverse events |
|---|---|---|---|---|---|---|---|
| 1 | De Barros et al.37, 2017, Brazil | 22,19 | 77, 78 | Hypertensive adults (>18years), both-genders, with or without treatment, without any comorbidities | Device-guided slow breathing (DGB) | 15 min/day - 4 weeks | Nil |
| 2 | Shetty et al.4, 2017, India | 30,30 | 100,100 | Hypertensive adults of age between 25 and 65 years on regular medication, without any comorbidities | Sheetali and Sheetkari Pranayama | 20 min/day - 30 days | Nil |
| 3 | Li et al.38, 2017, China | 60,60 | 100,100 | Hypertensive patients without any regular medication use, and co-morbid condition | Slow Breathing | One session −16 min | Nil |
| 4 | Kow et al.39, 2018, Malaysia | 42,45 | 92,97 | Adult patients with Stage I hypertension diagnosed at least 6 months back, with/without medications and without any co-morbid condition | Music guided deep breathing exercise | 15 min/day - 8 weeks | Nil |
| 5 | Ublosakka- Jones et al.40, 2018, Thailand | 16,16 | 100,100 | Old Adults between the age of 60–80 years, with controlled isolated systolic hypertension, without any comorbid condition | Slow guided breathing | 10 min/day - 8 weeks | Nil |
| 6 | Kalaivani et al.41, 2019, India | 85,85 | 100,100 | Hypertensive adults between the age of 30 and 60 years on regular medications | Alternate nostril breathing | 20 min/day - 5 days | Nil |
| 7 | Lachowska et al.42, 2019, Poland | 11,10 | 100,80 | Adults, >18 years of age, with HFeEF on optimal medical management | Device- guided slow breathing | 30 min/day - 3 months | Nil |
| 8 | Misra et al.43, 2019, Columbia | 101,32 | 60,69 | Adults with uncontrolled hypertension, regardless of pharmacological therapy, without any comorbid condition, 52 % male, mean age of 61 years | Yogic breathing exercise | 15 min/day - 6 weeks (5 times a week) | Nil |
| 9 | Srinivasan et al.44, 2019, India | 20,20 | 100,100 | Adults with pre and stage I hypertension between the age of 30 and 60 years, including both genders, with no comorbidities | Slow breathing (4 s inspiration and 6 s expiration) | One session - 30 min | Nil |
| 10 | Fetter et al.45, 2020, Brazil | 14,10 | 100,100 | Females between the age of 45 and 68 years, with a blood pressure of >140/90 mmHg, on medication (CCB), without any comorbidities | Ujjayi breathing | 75-min session, twice a week - 12 weeks | Nil |
| 11 | Ghati et al., 46 2021, India | 35,35 | 91,100 | Adults from 30 to 70 years of age, with blood pressure >140 and > 90, including both genders, on medication, without any comorbidities | Bee-humming exercise | 1 session | Nil |
| 12 | Sathe et al.47, 2020, India | 21,21 | 100,100 | Adults with age >40 years with hypertension from the past 20 years, with a history of CAD, on medications | Buteyko and bhramari pranayam | 6 cycles/day -one month | nil |
| 13 | Thanalakshmi et al.48, 2020, India | 50,50 | 80,84 | Adults with primary hypertension from age 18–60 years including both genders, without any comorbidities | Sheetali Pranayama | 30 min session - 90 days | Nil |
| 14 | Dhungana et al.49, 2021, Nepal | 61,60 | 96, 98 | Adults with stage 1 hypertension including both genders, taking anti-hypertensive medications without any comorbidities | Pranayam | 30 min/day for 5 days a week - 90 days | Nil |
| 15 | Craighead et al.50, 2021, USA | 18,18 | 83, 77 | Men and postmenopausal women with systolic BP more than 120 mmHg, without any co-morbidities | High‐resistance Inspiratory muscle strength training (IMST) | 6 days per week - 6 weeks | Nil |
Table 3.
Supervision of subjects in the studies included.
| Author/Location/Date | Supervised or not | Ways to ensure compliance | Comments |
|---|---|---|---|
| De Barros et al., 2017 | No | ABPM (Ambulatory blood pressure monitoring) using Mobil-O-Graph NG device (IEM, Germany) was used to monitor blood pressure remotely | |
| Shetty et al., 2017 | Yes | ||
| Li et al., 2017 | Yes | ||
| Kow et al., 2018 | No | Asked them to record the time and duration of their practice in a record book given to them | The authors also report that the lack of supervision may affect the quality of the breathing exercise and compliance for the same |
| Ublosakka- Jones et al., 2018 | No | Subjects were given a checklist on which they recorded the time and duration of the exercise and heart rate and blood pressure after the exercise. | Contacted via telephone once a week and were encouraged to do the exercise. The subjects were asked to record the details of their session like time, duration and any side effects. |
| Kalaivani et al., 2019 | Yes | ||
| Lachowska et al., 2019 | No | Used a RESPeRATE device | They were called weekly via a trainer and obtained various information about the time, duration and vital parameters from the device. |
| Misra et al., 2019 | No | The subjects logged their time and duration of the exercise and submitted their logs once a week. | |
| Srinivasan et al., 2019 | Yes | ||
| Fetter et al., 2020 | Yes | ||
| Ghati et al., 2021 | Yes | ||
| Sathe et al., 2020 | No | No mention of compliance | |
| Thanalakshmi et al., 2020 | Yes | ||
| Dhungana et al., 2021 | Yes | ||
| Craighead et al., 2021 | Yes |
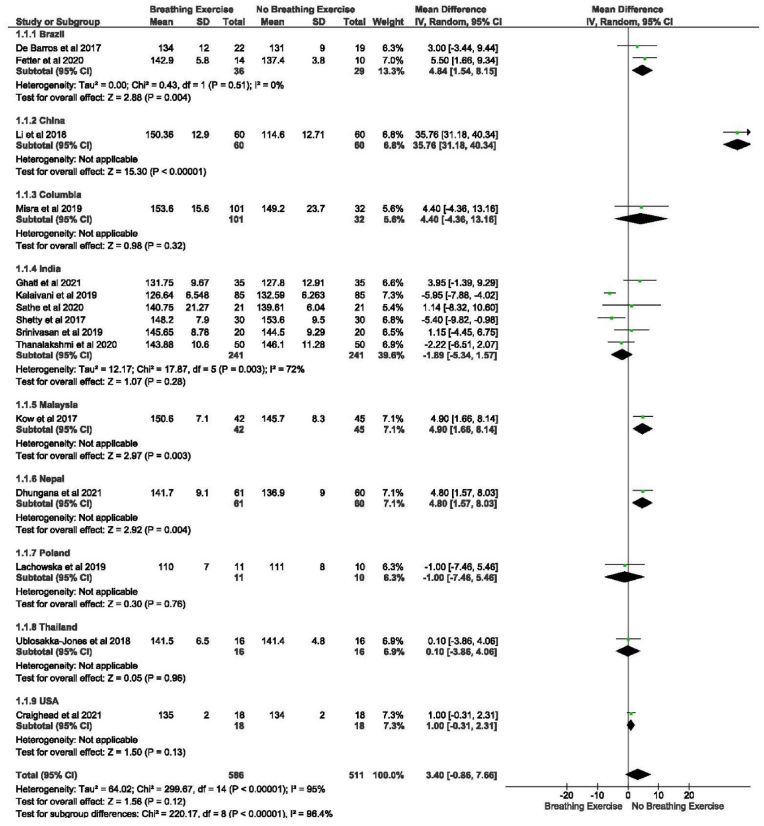
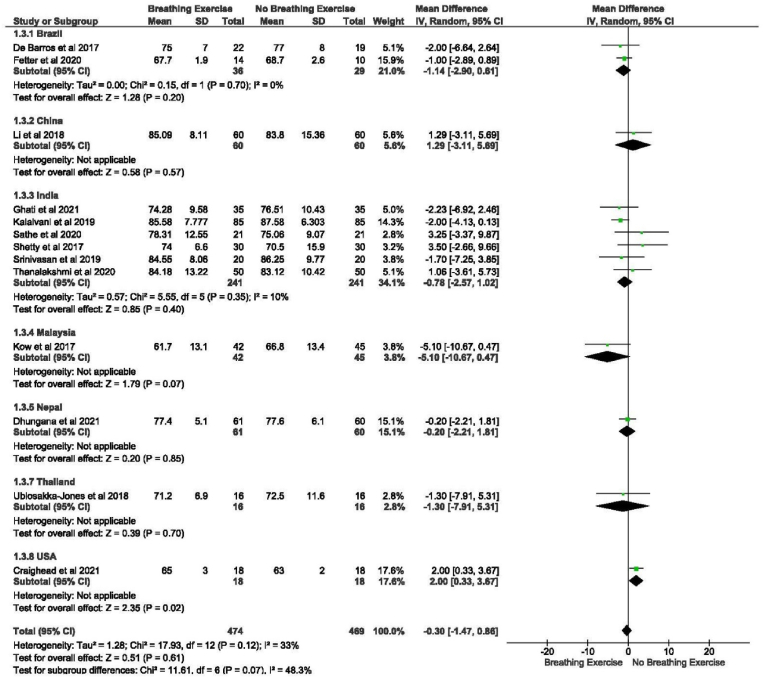
Fig. 2.
Characteristics baseline SBP.
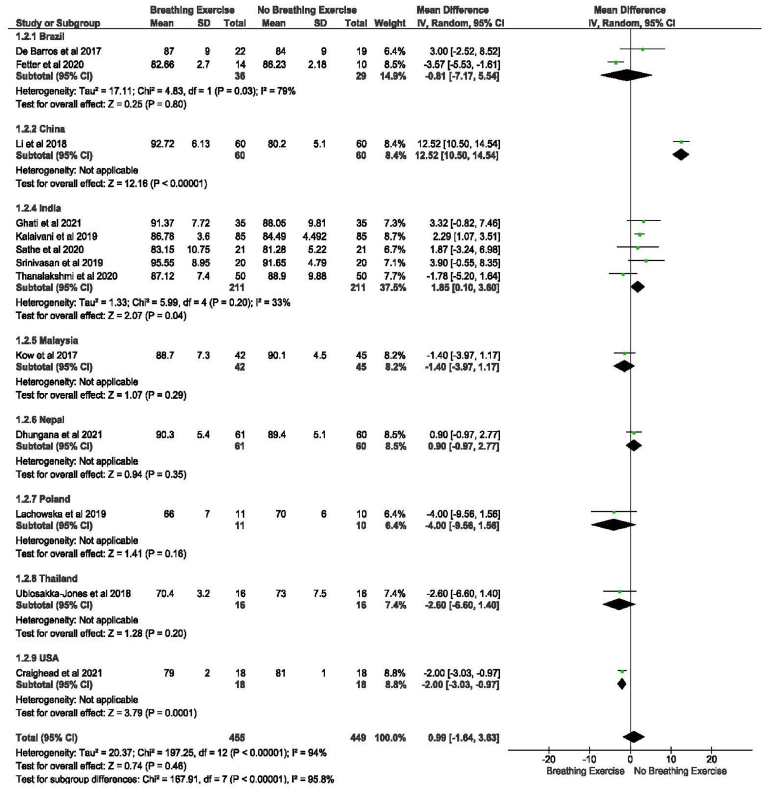
Fig. 3.
Characteristics baseline DBP
Fig. 4.
Characteristics baseline heart rate.
3.3. Effects of breathing exercise on BP and HR
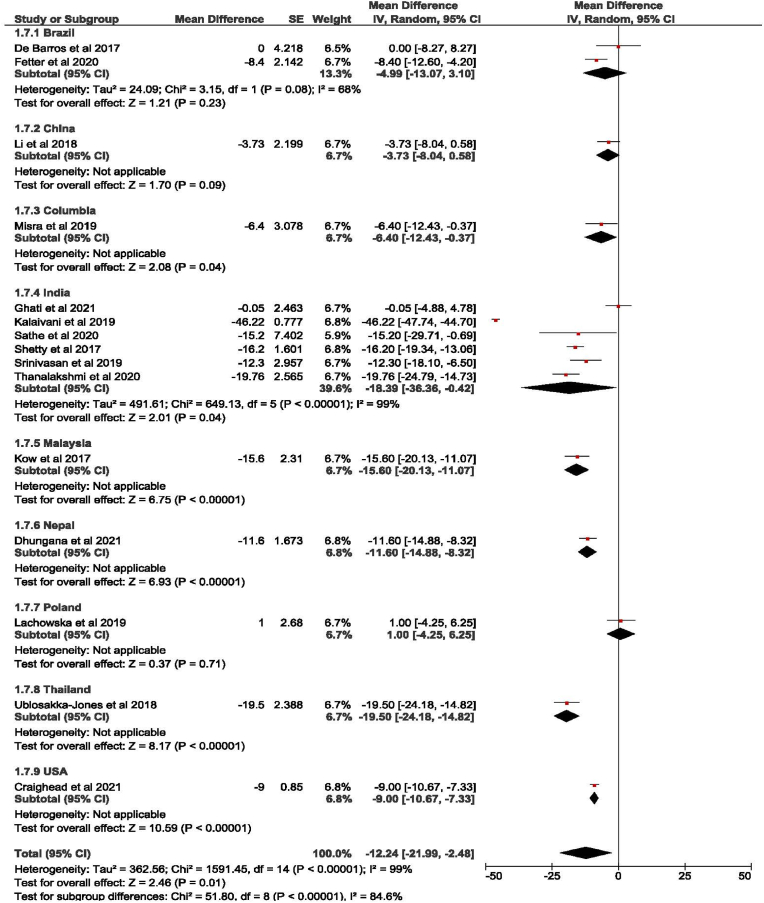
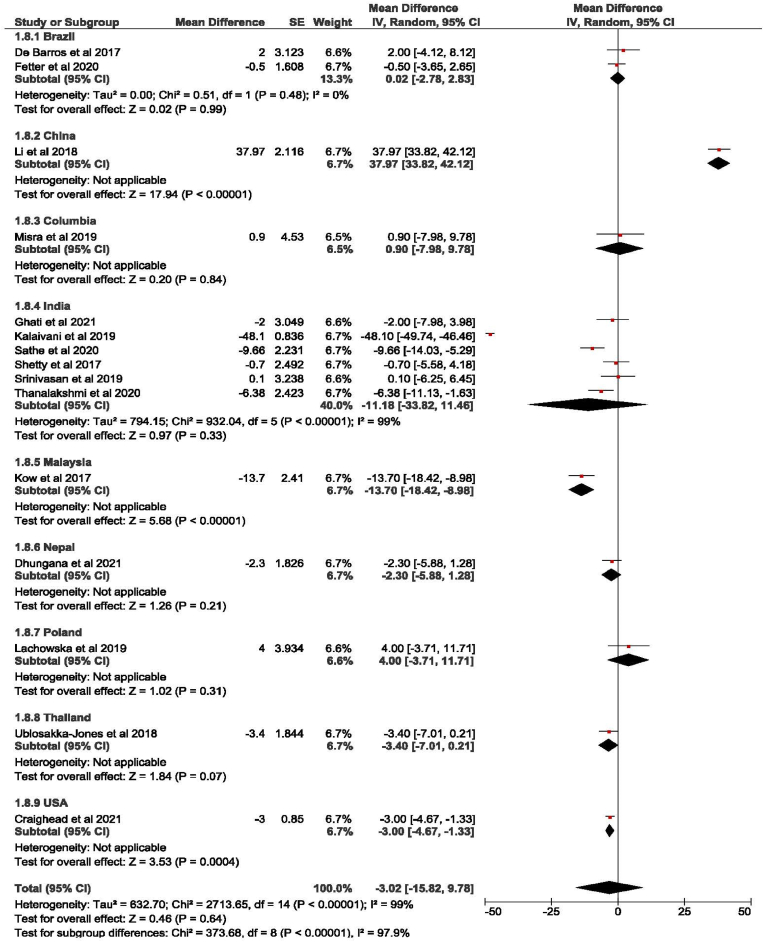
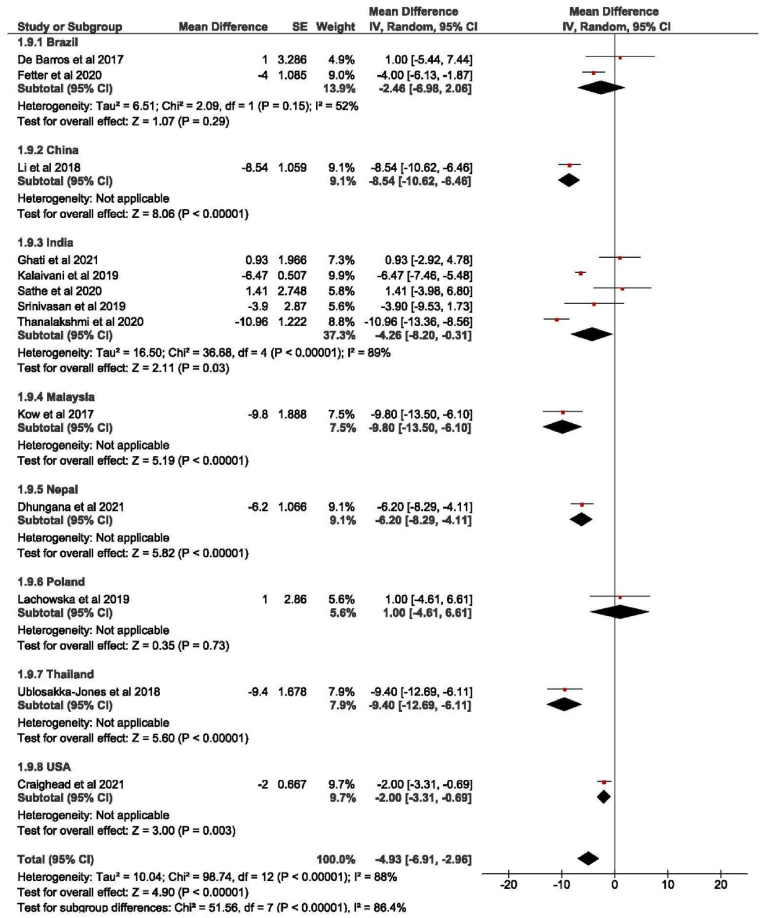
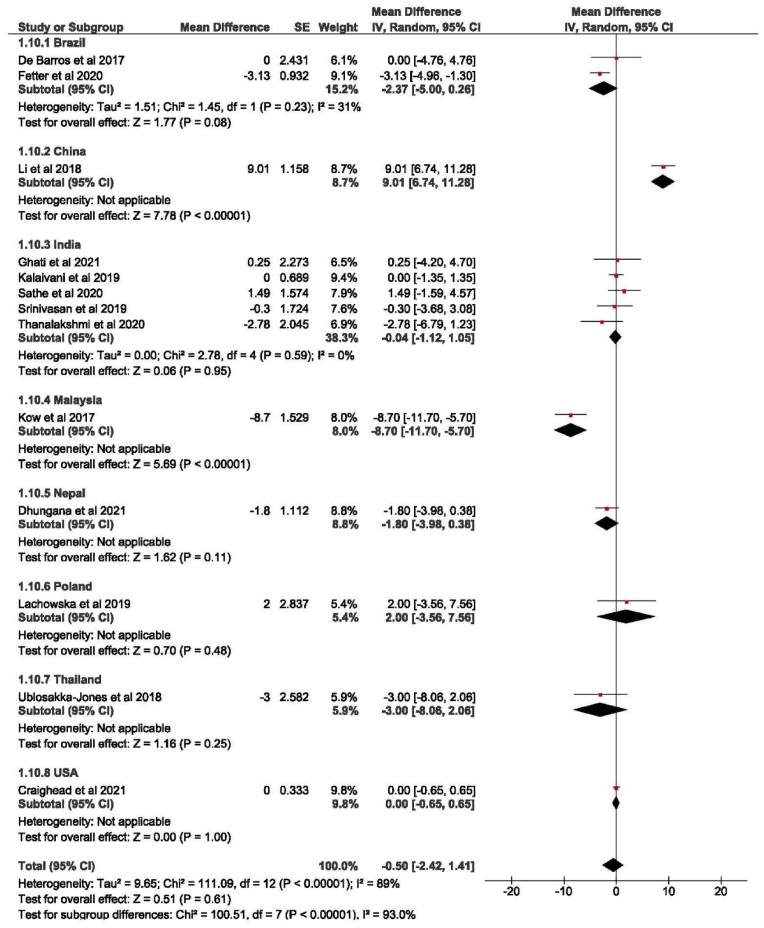
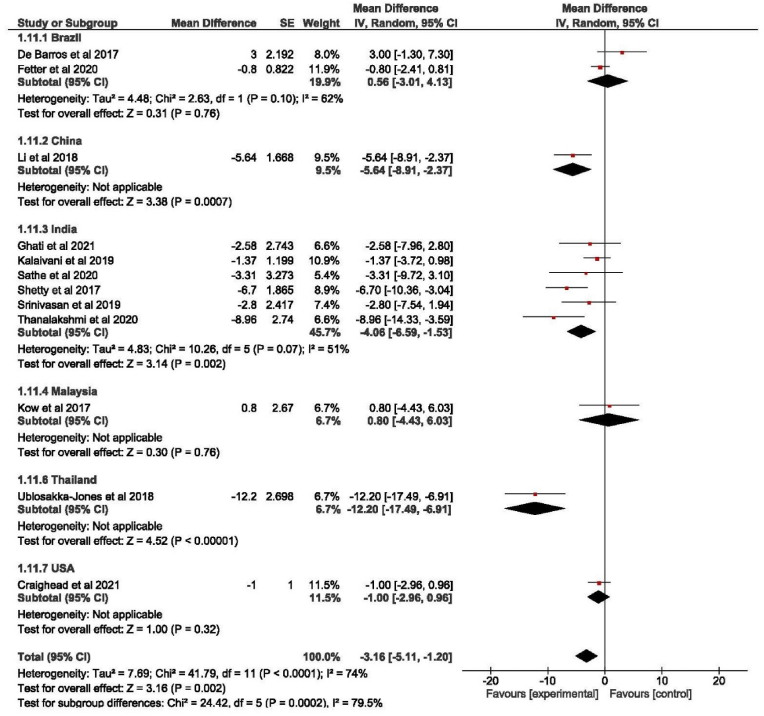
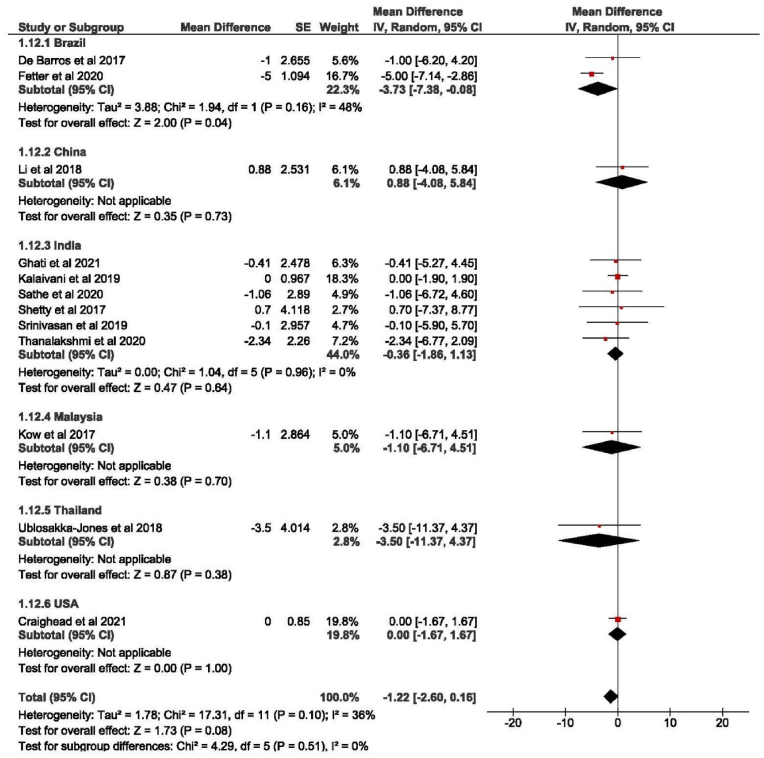
Breathing exercises lead to a significant reduction of SBP in the intervention group (−12.24 [−21.99, −2.48], p < 0.001) as compared to a non-significant reduction of SBP in the control group (−3.02 [−15.82, 9.78]) as shown by the forest plots in Fig. 5, Fig. 6. The reduction of DBP in the intervention group was −4.93 [−6.91, −2.96], p < 0.001 whereas the reduction was negligible in the control group (−0.50 [−2.42, 1.41]) as shown in Fig. 7, Fig. 8. The effect of breathing exercises on HR in the intervention group was also found to be statistically significant i.e., (−3.16 [−5.11, −1.20], p= <0.001) whereas the effect of breathing exercise in control group was −1.22 [−2.60, 0.16] as shown by the forest plot in Fig. 9, Fig. 10 respectively. However clinical significance of difference of 3.2 beats/min would be up for debate. There is a substantial heterogeneity present among all the included papers: Tau2 = 28.98; Chi2 = 141.10, df = 14, (p < 0.001), I2 = 90 % for SBP and Tau2 = 5.11; Chi2 = 55.01, df = 12, (p < 0.001), I2 = 78 % for DBP. We conducted subgroup analysis based on country of origin where trial was conducted. The effect size is then calculated for each subgroup. Thus, different effect sizes across the subgroups indicate that the country of origin may be a moderating factor (Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7, Fig. 8, Fig. 9, Fig. 10).
Fig. 5.
SBP variation in intervention group.
Fig. 6.
SBP variation in control group.
Fig. 7.
Dbp variation in intervention group.
Fig. 8.
Dbp variation in control group.
Fig. 9.
Heart rate variation in intervention group.
Fig. 10.
Heart rate variation in control group.
3.4. Risk of bias
All 15 studies which were included in the review have an unclear or high risk of bias. E-Table 1 shows the assessment of the risk of bias of the included study based on the Cochrane Risk of Bias Tool. Assessment of publication bias was performed using visual inspection of funnel plots and Egger's regression test, as presented in supplemental e-Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7, Fig. 8, Fig. 9. Detailed descriptions of the funnel plots, Egger regression test results, and respective interpretations of publication bias are also provided in the supplemental figures (e-Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7, Fig. 8, Fig. 9).
4. Discussion
The current systematic review and meta-analysis of 15 studies from 2017 to September 2022 provides a comprehensive assessment of the effect of breathing exercises on BP and HR. It indicated a positive effect of breathing exercises on SBP and DBP among adult subjects. Breathing exercises also showed an association with reduction in the HR, which was analyzed as a secondary outcome of our study.
Breathing exercises are a component of yoga practice. A systematic review and meta-analysis performed by Haggins et al.51 showed a significant effect of yoga, including pranayama/breathing exercises, on the reduction of SBP by 8.17 mmHg and DBP by 6.14 mmHg as compared to control group. Similarly, a recent meta-analysis by Wu et al.19 showed that regular practice of yoga and breathing exercises about three times a week decreased the SBP by 11 mmHg and DBP by 6 mmHg in the hypertensive group. Wu et al.19 also reported that the reduction in SBP was more pronounced in patients performing breathing exercises (∼8 mmHg) as compared to those not performing any breathing exercise (∼2 mmHg). However, both these studies considered other components of Yoga and other exercises, which may have led to a confounding bias towards the outcome. Comparatively, a reduction of 6 mmHg in SBP and 3 mmHg in DBP was reported in the breathing group as compared to the control group in our study.
Our findings were in concordance with Cramer et al.52 who also reported a decrease of 6.56 mmHg in SBP and 3.42 mmHg in DBP in the RCTs that excluded physical postures as compared to a decrease of 10.43 mmHg in SBP and 8.20 mmHg in DBP in the RCTs that included yoga physical postures. Whereas a study by Goncalves et al.53 which specifically focused on the effect of slow breathing exercises on BP, showed no significant reduction in the BP. However, they did not take into consideration other types of breathing exercises. Our study, on the other hand, included different types of breathing exercises to assess their effect on BP and found a significant reduction in SBP with various breathing exercises. Contradictory to these, Nivethitha et al.54 showed that there was an increase in BP after doing Bahir Kumbhaka (external breath retention), a type of breathing exercise. In this study, the increase in BP was expected as it was measured just after the exercise. A desirable effect could have been appreciated if it would have been practiced regularly for a sufficient amount of time, rather than just once as it was performed in this study.54 Ananda et al.55 showed a significant decrease in SBP, pulse pressure, and HR after practicing breathing exercises for 30 days regularly. Similarly, Naik et al.32 also showed a significant decrease in SBP, DBP, and HR after 12 weeks of regular practice of slow breathing exercises.
In patients with HTN, it is hypothesized that there is an increase in sympathetic activity. It is reported to be due to the following reasons: increased sympathetic innervation,56 lower sensitivity of the baroreceptor,57 higher sensitivity of carotid chemoreceptor, 58 changes with noradrenergic transmission and uptake,56, 59 and increased pulmonary vascular pressure. 59,60 Slow and deep breathing exercise decrease respiration rate, thus causing increased inhalation and exhalation volume, which eventually leads to an increased amount of oxygen entering into the bloodstream.61 Multiple studies have shown that breathing exercises, especially those involving deep breathing, can help in arteriolar dilatation as they inhibit sympathetic nervous system activity and activate cardiopulmonary mechanoreceptors which ultimately leads to a decrease in both SBP and DBP in hypertensive patients. [[62], [63], [64]] Our meta-analysis supports these findings by reporting a reduction in both SBP and DBP in patients performing breathing exercises when compared to control group.
Breathing exercises have been found to significantly increase HR variability in pre-hypertensive as well as hypertensive population due to an increase in baroreflex sensitivity.11,63 These exercises tend to cause a state of relaxation which slows down the HR and that has been linked to a decrease in SBP as well.65 Our study found similar association between breathing exercises and HR depicted by post-intervention decrease in HR by ∼2.5 beats per minute.
The proven and documented effect of breathing exercises was shown to be comparable to the reduction of BP reported due to other non-pharmacological modalities like reduction in salt intake, and exercise in a study by Soudarssanane et al.66 Our meta-analysis shows a reduction in SBP, DBP, and HR after doing breathing exercises, thus supporting the use of breathing exercises as an alternative way to control BP. Other reasons to support its use include, accessibility, enjoyability, low/no cost, and ease of practice. This leads to an increase in compliance and helps in maintaining the overall physical, and mental wellbeing.40.
This is the first systematic review and meta-analysis to study the effects of various breathing exercises on BP and HR. Strengths of this study include a thorough literature search using multiple databases, a duplicate review of the included articles, a systematic analysis of the data using standardized PRISMA checklist, and a quality assessment of the risk of bias in each study.
However, our study has its limitations. There were several different types of breathing exercises that were included, thereby decreasing the specificity of the exercise that leads to the most decrease in BP. The effect of breathing exercises could have been influenced by many other factors like meditation, diet, aerobic exercise, stress levels, and/or medications, which our study could not take into consideration. Also, the information on the duration of interventions in the included studies was very limited, therefore a knowledge gap exists about the extent of the long-term effect of breathing exercises on BP. We could not report the intensity and accuracy with which the participants performed their breathing exercises which could have also affected their BP. Other limitations of our study are that it included articles only in the English language, and some of the included studies had a small sample size.
5. Conclusion
Our systematic review and meta-analysis suggest that breathing exercises have positive effect on decreasing the blood pressure and heart rate. It is a safe practice that does not require any equipment. It could be an important adjunct non-pharmacological modality to control hypertension. Additional RCTs of longer duration and larger sample size are required to further confirm the extent to which breathing exercises impact the reduction in blood pressure and heart rate.
CRediT authorship contribution statement
Piyush Garg: Conceptualization, Data curation, Investigation, Methodology, Supervision, Validation, Visualization, Writing - original draft, Writing - review & editing. Ayushi Mendiratta: Data curation, Supervision, Writing - original draft, Writing - review & editing. Akshat Banga: Conceptualization, Investigation, Methodology, Project administration, Validation, Writing - original draft, Writing - review & editing. Anna Bucharles: Data curation, Resources, Supervision, Writing - original draft. Piccoli Victoria: Data curation, Investigation, Methodology, Writing - original draft. Balakrishnan Kamaraj: Conceptualization, Data curation, Writing - original draft. Rakhtan K. Qasba: Data curation, Investigation, Writing - original draft. Vikas Bansal: Data curation, Formal analysis, Investigation, Software, Supervision, Writing - original draft, Writing - review & editing. Jayaraman Thimmapuram: Supervision, Writing - original draft, Writing - review & editing. Robert Pargament: Supervision, Writing - original draft, Writing - review & editing. Rahul Kashyap: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing - original draft.
Handling Editor: Dr D Levy
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcrp.2023.200232.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Kearney P.M., Whelton M., Reynolds K., Muntner P., Whelton P.K., He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.Whelton P.K., Carey R.M., Aronow W.S., et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the Prevention, Detection, evaluation, and management of high blood pressure in adults: Executive summary: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Hypertension. 2017;71(6):1269–1324. doi: 10.1161/HYP.0000000000000066. 2018. [DOI] [PubMed] [Google Scholar]
- 3.Chobanian A.V. The seventh report of the Joint national committee on prevention, detection, evaluation, and treatment of high blood PressureThe JNC 7 report. JAMA. 2003;289(19):2560. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 4.Shetty P., Reddy B.K.K., Lakshmeesha D.R., Shetty S.P., Kumar G.S., Bradley R. Effects of Sheetali and Sheetkari pranayamas on blood pressure and autonomic function in hypertensive patients. Integr Med Encinitas Calif. 2017;16(5):32–37. [PMC free article] [PubMed] [Google Scholar]
- 5.James P.A., Oparil S., Carter B.L., et al. evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427. 2014. [DOI] [PubMed] [Google Scholar]
- 6.Hajjar I. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003;290(2):199. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 7.Benjamin R.M. Medication adherence: helping patients take their medicines as directed. Public Health Rep Wash DC. 1974;127(1):2–3. doi: 10.1177/003335491212700102. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luma G.B., Spiotta R.T. Hypertension in children and adolescents. Am. Fam. Physician. 2006;73(9):1558–1568. [PubMed] [Google Scholar]
- 9.Clarke T.C., Black L.I., Stussman B.J., Barnes P.M., Nahin R.L. Trends in the use of complementary health approaches among adults: United States, 2002-2012. Natl Health Stat Rep. 2015;79:1–16. [PMC free article] [PubMed] [Google Scholar]
- 10.Schein M.H., Gavish B., Herz M., et al. Treating hypertension with a device that slows and regularises breathing: a randomised, double-blind controlled study. J. Hum. Hypertens. 2001;15(4):271–278. doi: 10.1038/sj.jhh.1001148. [DOI] [PubMed] [Google Scholar]
- 11.Elliot W.J., Izzo J.L., White W.B., et al. Graded blood pressure reduction in hypertensive outpatients associated with use of a device to assist with slow breathing. J Clin Hypertens Greenwich Conn. 2004;6(10):553–559. doi: 10.1111/j.1524-6175.2004.03553.x. quiz 560-561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson D.E., McNeely J.D., Windham B.G. Regular slow-breathing exercise effects on blood pressure and breathing patterns at rest. J. Hum. Hypertens. 2010;24(12):807–813. doi: 10.1038/jhh.2010.18. [DOI] [PubMed] [Google Scholar]
- 13.Hateren KJ van, Landman G.W., Logtenberg S.J., Bilo H.J., Kleefstra N. Device-guided breathing exercises for the treatment of hypertension: an overview. World J. Cardiol. 2014;6(5):277. doi: 10.4330/wjc.v6.i5.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Landman G.W.D., van Hateren Kjj, van Dijk P.R., et al. Efficacy of device-guided breathing for hypertension in blinded, randomized, active-controlled trials: a meta-analysis of individual patient data. JAMA Intern. Med. 2014;174(11):1815. doi: 10.1001/jamainternmed.2014.4336. [DOI] [PubMed] [Google Scholar]
- 15.Gordon L., Morrison E., Mcgrowder D., et al. Changes in clinical and metabolic parameters after exercise therapy in patients with type 2 diabetes. Arch. Med. Sci. 2008;4:427–437. [Google Scholar]
- 16.Karthik P.S., Chandrasekhar M., Ambareesha K., Nikhil C. Effect of pranayama and suryanamaskar on pulmonary functions in medical students. J Clin Diagn Res JCDR. 2014;8(12):BC04–6. doi: 10.7860/JCDR/2014/10281.5344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nalbant G., Hassanein Z.M., Lewis S., Chattopadhyay K. Content, structure, and delivery characteristics of yoga interventions for managing hypertension: a systematic review and meta-analysis of randomized controlled trials. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.846231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tyagi A., Cohen M. Yoga and hypertension: a systematic review. Alternative Ther. Health Med. 2014;20(2):32–59. [PubMed] [Google Scholar]
- 19.Wu Y., Johnson B.T., Acabchuk R.L., et al. Yoga as antihypertensive lifestyle therapy: a systematic review and meta-analysis. Mayo Clin. Proc. 2019;94(3):432–446. doi: 10.1016/j.mayocp.2018.09.023. [DOI] [PubMed] [Google Scholar]
- 20.Park S.H., Han K.S. Blood pressure response to meditation and yoga: a systematic review and meta-analysis. J Altern Complement Med N Y N. 2017;23(9):685–695. doi: 10.1089/acm.2016.0234. [DOI] [PubMed] [Google Scholar]
- 21.Brandani J.Z., Mizuno J., Ciolac E.G., Monteiro H.L. The hypotensive effect of Yoga's breathing exercises: a systematic review. Compl. Ther. Clin. Pract. 2017;28:38–46. doi: 10.1016/j.ctcp.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 22.Jerath R., Crawford M.W., Barnes V.A., Harden K. Self-regulation of breathing as a primary treatment for anxiety. Appl. Psychophysiol. Biofeedback. 2015;40(2):107–115. doi: 10.1007/s10484-015-9279-8. [DOI] [PubMed] [Google Scholar]
- 23.Kirkwood G. Yoga for anxiety: a systematic review of the research evidence * Commentary. Br. J. Sports Med. 2005;39(12):884–891. doi: 10.1136/bjsm.2005.018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brown R.P., Gerbarg P.L. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: part I-neurophysiologic model. J Altern Complement Med N Y N. 2005;11(1):189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 25.Busch V., Magerl W., Kern U., Haas J., Hajak G., Eichhammer P. The effect of deep and slow breathing on pain perception, autonomic activity, and mood processing--an experimental study. Pain Med Malden Mass. 2012;13(2):215–228. doi: 10.1111/j.1526-4637.2011.01243.x. [DOI] [PubMed] [Google Scholar]
- 26.Lin F.L., Yeh M.L., Lai Y.H., Lin K.C., Yu C.J., Chang J.S. Two-month breathing-based walking improves anxiety, depression, dyspnoea and quality of life in chronic obstructive pulmonary disease: a randomised controlled study. J. Clin. Nurs. 2019;28(19–20):3632–3640. doi: 10.1111/jocn.14960. [DOI] [PubMed] [Google Scholar]
- 27.Das R.R., Sankar J., Kabra S.K. Role of breathing exercises and yoga/pranayama in childhood asthma: a systematic review. Curr. Pediatr. Rev. 2019;15(3):175–183. doi: 10.2174/1573396315666190121122452. [DOI] [PubMed] [Google Scholar]
- 28.Jagadeesan T., R A R K, et al. Effect of Bhramari Pranayama intervention on stress, anxiety, depression and sleep quality among COVID 19 patients in home isolation. J. Ayurveda Integr. Med. 2022;13(3) doi: 10.1016/j.jaim.2022.100596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rung O., Stauber L., Loescher L.J., Pace T.W. Alternate nostril breathing to reduce stress: an option for pregnant women survivors of intimate partner violence? J Holist Nurs Off J Am Holist Nurses Assoc. 2021;39(4):393–415. doi: 10.1177/0898010120983659. [DOI] [PubMed] [Google Scholar]
- 30.Descilo T., Vedamurtachar A., Gerbarg P.L., et al. Effects of a yoga breath intervention alone and in combination with an exposure therapy for post-traumatic stress disorder and depression in survivors of the 2004 South-East Asia tsunami. Acta Psychiatr. Scand. 2010;121(4):289–300. doi: 10.1111/j.1600-0447.2009.01466.x. [DOI] [PubMed] [Google Scholar]
- 31.Hayama Y., Inoue T. The effects of deep breathing on “tension-anxiety” and fatigue in cancer patients undergoing adjuvant chemotherapy. Compl. Ther. Clin. Pract. 2012;18(2):94–98. doi: 10.1016/j.ctcp.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Naik G.S., Gaur G.S., Pal G.K. Effect of modified slow breathing exercise on perceived stress and basal cardiovascular parameters. Int. J. Yoga. 2018;11(1):53–58. doi: 10.4103/ijoy.IJOY_41_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Telles S., Verma S., Sharma S.K., Gupta R.K., Balkrishna A. Alternate-nostril yoga breathing reduced blood pressure while increasing performance in a vigilance test. Med Sci Monit Basic Res. 2017;23:392–398. doi: 10.12659/msmbr.906502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saptharishi L., Soudarssanane M., Thiruselvakumar D., et al. Community-based randomized controlled trial of non-pharmacological interventions in prevention and control of hypertension among young adults. Indian J Community Med Off Publ Indian Assoc Prev Soc Med. 2009;34(4):329–334. doi: 10.4103/0970-0218.58393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Higgins J.P., Savović J., Page M.J., Elbers R.G., Sterne J.A. In: Cochrane Handbook for Systematic Reviews of Interventions. first ed. Higgins J.P.T., Thomas J., Chandler J., et al., editors. Wiley; 2019. Assessing risk of bias in a randomized trial; pp. 205–228. [DOI] [Google Scholar]
- 36.Review Manager (RevMan) [Computer Program]. Version 5.1, The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark. 2011. [Google Scholar]
- 37.de Barros S., da Silva G.V., de Gusmão J.L., et al. Effects of long term device-guided slow breathing on sympathetic nervous activity in hypertensive patients: a randomized open-label clinical trial. Blood Pres. 2017;26(6):359–365. doi: 10.1080/08037051.2017.1357109. [DOI] [PubMed] [Google Scholar]
- 38.Li C., Chang Q., Zhang J., Chai W. Effects of slow breathing rate on heart rate variability and arterial baroreflex sensitivity in essential hypertension. Medicine (Baltim.) 2018;97(18) doi: 10.1097/MD.0000000000010639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kow F.P., Adlina B., Sivasangari S., et al. The impact of music guided deep breathing exercise on blood pressure control - a participant blinded randomised controlled study. Med. J. Malaysia. 2018;73(4):233–238. [PubMed] [Google Scholar]
- 40.Ublosakka-Jones C., Tongdee P., Pachirat O., Jones D.A. Slow loaded breathing training improves blood pressure, lung capacity and arm exercise endurance for older people with treated and stable isolated systolic hypertension. Exp. Gerontol. 2018;108:48–53. doi: 10.1016/j.exger.2018.03.023. [DOI] [PubMed] [Google Scholar]
- 41.Kalaivani S., Kumari M., Pal G. Effect of alternate nostril breathing exercise on blood pressure, heart rate, and rate pressure product among patients with hypertension in JIPMER, Puducherry. J. Educ. Health Promot. 2019;8(1):145. doi: 10.4103/jehp.jehp_32_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lachowska K., Bellwon J., Narkiewicz K., Gruchała M., Hering D. Long-term effects of device-guided slow breathing in stable heart failure patients with reduced ejection fraction. Clin. Res. Cardiol. 2019;108(1):48–60. doi: 10.1007/s00392-018-1310-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Misra S., Smith J., Wareg N., Hodges K., Gandhi M., McElroy J.A. Take a deep breath: a randomized control trial of Pranayama breathing on uncontrolled hypertension. Adv Integr Med. 2019;6(2):66–72. doi: 10.1016/j.aimed.2018.08.002. [DOI] [Google Scholar]
- 44.Srinivasan B., Rajkumar D. Effects of slow breathing on blood pressure and end tidal carbon dioxide in hypertension: randomised controlled trial. J Clin Diagn Res. Published online. 2019 doi: 10.7860/JCDR/2019/42327.13121. [DOI] [Google Scholar]
- 45.Fetter C., Marques J.R., de Souza L.A., et al. Additional improvement of respiratory technique on vascular function in hypertensive postmenopausal women following yoga or stretching video classes: the YOGINI study. Front. Physiol. 2020;11:898. doi: 10.3389/fphys.2020.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ghati N., Killa A.K., Sharma G., et al. A randomized trial of the immediate effect of Bee-Humming Breathing exercise on blood pressure and heart rate variability in patients with essential hypertension. Explore. 2021;17(4):312–319. doi: 10.1016/j.explore.2020.03.009. [DOI] [PubMed] [Google Scholar]
- 47.Sathe S., Rajandekar T., Thodge K., Bhawane A., Thatere U. Immediate effect of Buteyko breathing and Bhramari pranayama on blood pressure, heart rate and oxygen saturation in hypertensive patients: a comparative study. Indian J Forensic Med Toxicol. 2020;14(4):7106–7111. doi: 10.37506/ijfmt.v14i4.12764. [DOI] [Google Scholar]
- 48.Thanalakshmi J., Maheshkumar K., Kannan R., Sundareswaran L., Venugopal V., Poonguzhali S. Effect of Sheetali pranayama on cardiac autonomic function among patients with primary hypertension - a randomized controlled trial. Compl. Ther. Clin. Pract. 2020;39 doi: 10.1016/j.ctcp.2020.101138. [DOI] [PubMed] [Google Scholar]
- 49.Dhungana R.R., Pedisic Z., Joshi S., et al. Effects of a health worker-led 3-month yoga intervention on blood pressure of hypertensive patients: a randomised controlled multicentre trial in the primary care setting. BMC Publ. Health. 2021;21(1):550. doi: 10.1186/s12889-021-10528-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Craighead D.H., Heinbockel T.C., Freeberg K.A., et al. Time‐efficient inspiratory muscle strength training lowers blood pressure and improves endothelial function, NO bioavailability, and oxidative stress in midlife/older adults with above‐normal blood pressure. J. Am. Heart Assoc. 2021;10(13) doi: 10.1161/JAHA.121.020980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hagins M., States R., Selfe T., Innes K. Effectiveness of yoga for hypertension: systematic review and meta-analysis. Evid Based Complement Alternat Med. 2013;2013:1–13. doi: 10.1155/2013/649836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cramer H., Haller H., Lauche R., Steckhan N., Michalsen A., Dobos G. A systematic review and meta-analysis of yoga for hypertension. Am. J. Hypertens. 2014;27(9):1146–1151. doi: 10.1093/ajh/hpu078. [DOI] [PubMed] [Google Scholar]
- 53.de Freitas Gonçalves K.S., Queiroz Godoy Daniel A.C., Tatagiba Lamas J.L., et al. Device and nondevice‐guided slow breathing to reduce blood pressure in hypertensive patients: a systematic review and meta‐analysis. Health Sci Rep. 2022;5(3) doi: 10.1002/hsr2.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nivethitha L., Mooventhan A., Manjunath N.K. Evaluation of cardiovascular functions during the practice of different types of yogic breathing techniques. Int. J. Yoga. 2021;14(2):158–162. doi: 10.4103/ijoy.IJOY_61_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bhavanani A.B., null Madanmohan, Sanjay Z. Immediate effect of chandra nadi pranayama (left unilateral forced nostril breathing) on cardiovascular parameters in hypertensive patients. Int. J. Yoga. 2012;5(2):108–111. doi: 10.4103/0973-6131.98221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Adams M.A., Bobik A., Korner P.I. Differential development of vascular and cardiac hypertrophy in genetic hypertension. Relation to sympathetic function. Hypertension. 1989;14(2):191–202. doi: 10.1161/01.HYP.14.2.191. [DOI] [PubMed] [Google Scholar]
- 57.Parati G., Esler M. The human sympathetic nervous system: its relevance in hypertension and heart failure. Eur. Heart J. 2012;33(9):1058–1066. doi: 10.1093/eurheartj/ehs041. [DOI] [PubMed] [Google Scholar]
- 58.Tan Z.Y., Lu Y., Whiteis C.A., et al. Chemoreceptor hypersensitivity, sympathetic excitation, and overexpression of ASIC and TASK channels before the onset of hypertension in SHR. Circ. Res. 2010;106(3):536–545. doi: 10.1161/CIRCRESAHA.109.206946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cabassi A., Vinci S., Quartieri F., Moschini L., Borghetti A. Norepinephrine reuptake is impaired in skeletal muscle of hypertensive rats in vivo. Hypertens Dallas Tex. 1979;37(2 Pt 2):698–702. doi: 10.1161/01.hyp.37.2.698. 2001. [DOI] [PubMed] [Google Scholar]
- 60.Leimbach W.N., Wallin B.G., Victor R.G., Aylward P.E., Sundlöf G., Mark A.L. Direct evidence from intraneural recordings for increased central sympathetic outflow in patients with heart failure. Circulation. 1986;73(5):913–919. doi: 10.1161/01.cir.73.5.913. [DOI] [PubMed] [Google Scholar]
- 61.Ma X., Yue Z.Q., Gong Z.Q., et al. The effect of diaphragmatic breathing on attention, negative affect and stress in healthy adults. Front. Psychol. 2017;8:874. doi: 10.3389/fpsyg.2017.00874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Joseph C.N., Porta C., Casucci G., et al. Slow breathing improves arterial baroreflex sensitivity and decreases blood pressure in essential hypertension. Hypertens Dallas Tex. 1979;46(4):714–718. doi: 10.1161/01.HYP.0000179581.68566.7d. 2005. [DOI] [PubMed] [Google Scholar]
- 63.Wang S.Z., Li S., Xu X.Y., et al. Effect of slow abdominal breathing combined with biofeedback on blood pressure and heart rate variability in prehypertension. J Altern Complement Med N Y N. 2010;16(10):1039–1045. doi: 10.1089/acm.2009.0577. [DOI] [PubMed] [Google Scholar]
- 64.Mourya M., Mahajan A.S., Singh N.P., Jain A.K. Effect of slow- and fast-breathing exercises on autonomic functions in patients with essential hypertension. J Altern Complement Med N Y N. 2009;15(7):711–717. doi: 10.1089/acm.2008.0609. [DOI] [PubMed] [Google Scholar]
- 65.Shaffer F., Ginsberg J.P. An overview of heart rate variability metrics and norms. Front. Public Health. 2017;5:258. doi: 10.3389/fpubh.2017.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Soudarssanane Mb, Thiruselvakumar D., Sahai A., et al. Non-pharmacological interventions in hypertension: a community-based cross-over randomized controlled trial. Indian J. Community Med. 2011;36(3):191. doi: 10.4103/0970-0218.86519. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.