With COVID-19 intensifying longstanding patterns of stress, overwork, and disillusionment among the healthcare workforce, burnout is at all all-time high in medicine. Critical care clinicians have some of the highest rates of burnout of all specialties1–5—as high as 70% prevalence among physicians6, and up to 80% among nurses.7 Burnout is an occupational phenomenon characterized by 1) fatigue or exhaustion, 2) negative feelings toward one’s job, and 3) reduced professional efficacy.8 It is associated with higher rates of mental disorders and psychological distress,9,10 and has potential negative repercussions for patient safety and care.11 Growing media attention and expanding research on burnout have brought increased recognition that burnout is a significant problem facing the healthcare workforce. Yet most studies have focused on individual-level causes and solutions, such as mindfulness training, yoga, and other relaxation-based exercises12,13—interventions that do little to identify and respond to the broader structural (i.e. extra-individual) forces shaping clinician burnout.
In 1975, the medical sociologist and epidemiologist John McKinlay popularized the metaphor of “upstream” factors contributing to healthcare problems.14 Suppose that you are standing on the banks of a river and hear the cries of someone drowning. You dive in to save them, only to hear another cry for help nearby. Again and again, you dive in to save a drowning person, without stopping to consider the source of the crisis. This metaphor, which has been widely influential in public health and the sociology of medicine,15 highlights the need to move upstream to understand why so many healthcare workers are drowning. It’s not that the downstream approaches are wholly ineffective or inadvisable. Rather, it’s that on their own, they cannot address the root cause of the problem, which necessarily affects more than individual clinicians. When up to 80% of critical care professionals are drowning, it’s worth stopping to ask who or what is pushing them in to these dangerous waters.
In 2019, a National Academies of Sciences, Engineering, and Medicine consensus study proposed a systems model of clinician burnout that specifically called for more attention to structural (i.e., upstream) factors affecting clinician burnout and wellbeing.16 This model has informed our ongoing sociological study in which we have been interviewing frontline hospital-based physicians in four U.S. cities about their experiences caring for COVID-19 patients (www.steppsmed.com). Participants have told us repeatedly that downstream approaches miss the mark. As a critical care pulmonologist in New Orleans put it,
There are a number of ways that you could reduce physician burnout, if you actually asked physicians what parts of their job they hate, [it’s] the admin stuff, the extra EMR [electronic medical record] time, all of these very clear things that were different long time ago. But instead of doing that, they’re just gonna make suggestions to add things, “Well, you could all do yoga.”
For this physician, targeting downstream interventions like yoga to the exclusion of work environment factors such as burdensome electronic health record documentation is insulting because administrators already know that yoga cannot fix the underlying structural causes of healthcare worker burnout. Yet, the implication remains: clinicians, breathe and stretch your way out of burnout.
So, yoga aside, what can be done? Because burnout is a product of the work environment, upstream interventions aimed at organizational units, institutions, health professions, and health systems will be essential to addressing the epidemic of healthcare worker burnout. Our model for clinician burnout suggests that there are multiple nested layers for intervention as we move progressively upstream. (See Figure 1.) Above the downstream terrain where many current intervention strategies focus (e.g., yoga, mindfulness-based meditation, relaxation training webinars, eating, and sleeping habits), lies the midstream of institutional interventions. These approaches include strategies aimed at organizational units and work environments—such as changes to staffing models and team debriefs—and those focused on health care institutions, such as leadership training to be more responsive to physicians’ concerns and transparent communication of institutional decisions and policies. Finally, upstream targets for intervention include structural targets like reforming government and insurance policies, and redesigning EMR infrastructure, as well as targets for cultural change like clinical training practices and professional norms and expectations. Preliminary findings from our ongoing study suggest that for interventions to be effective, they must offer solutions that move progressively upstream, recognizing that different layers of the healthcare environment operate synergistically with one another. This means that interventions should simultaneously target stressors at multiple levels, as upstream factors can often shape midstream and downstream ones.
Figure 1.
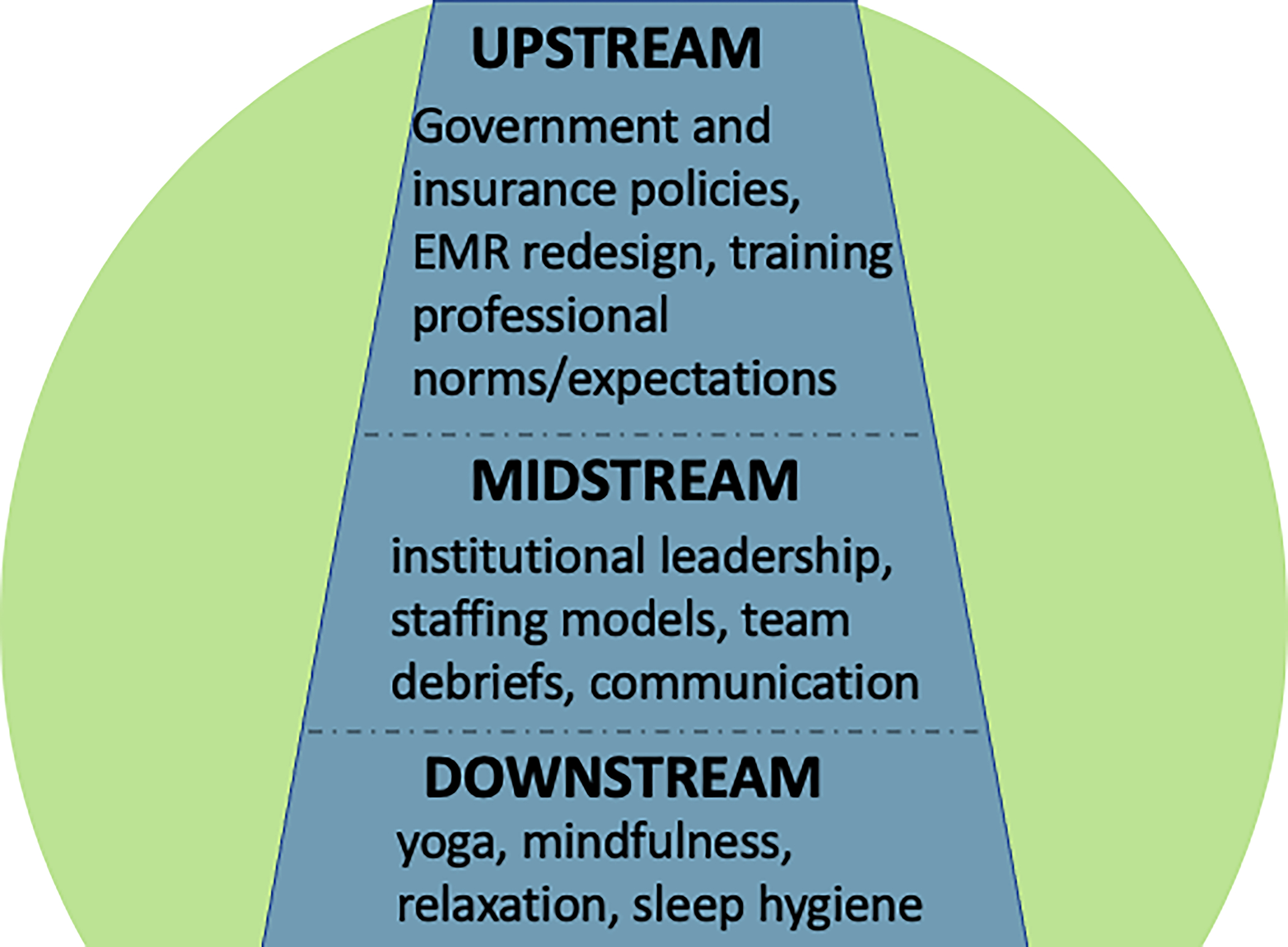
Sample Targets for Reducing Clinical Burnout
Expanding the healthcare workforce to reduce overwork among staff is one example of an important target for addressing healthcare worker burnout in critical care. A multi-prong strategy should incorporate both midstream and upstream interventions. At the upstream level, some federal legislation is already beginning to tackle this issue. For example, for the first time since 1997, the U.S. federal government has raised the cap on the number of Medicare-funded residency positions by 1,000, specifically targeting high-needs hospitals.17 Similarly, the Build Back Better Act (which has yet to pass the Senate), proposes to expand funding, education, and grantmaking programs aimed at training and retaining healthcare workers, among others. These efforts represent a good start for increasing the healthcare workforce, but they need to be expanded and supplemented by additional upstream and midstream interventions. These could include reforming the norms and structure of graduate medical education by spreading out the work over more trainees, thereby making it easier for them to take time off when needed. It may also require a reorientation of institutional priorities by making hiring and retaining of staff at all levels a stated priority, even if that cuts into their bottom line.
Combating structural forces that work against clinicians’ utilization of mental health services is another important target for improving clinical burnout. Upstream interventions along these lines might include reform of discriminatory medical malpractice and disability insurance policies that disincentivize clinicians from seeking mental health treatment, as well as efforts to reduce professional stigma around mental health treatment through culture change and awareness campaigns. Even if this stigma can be reduced, however, it may still be difficult for critical care professionals facing fluctuating schedules to find time for routine therapy sessions. Therefore, complementary midstream interventions such as scheduling accommodations and unit-level leadership changes will be necessary to increase uptake of mental health services.
The time has come to think ‘big’ about the factors making the health workforce sick, and to consider even those factors that extend beyond one’s unit or hospital, to the broader profession and healthcare system. Clinicians are often trained to think downstream—a particularly useful skill when rescuing people who are drowning. Yet to develop and implement the kind of multi-dimensional interventional strategies that The Critical Care Societies Collaborative has endorsed for improving intensive care unit work environments and individual coping,18,19 it may be useful for clinicians to work alongside others who are specifically trained to think upstream. Social scientists and policy experts can help conceptualize burnout as an outcome shaped by the social determinants of health.
Neglecting the upstream factors leading to clinician burnout is not simply ineffective. It is also harmful. For one thing, it risks contributing to victim-blaming and stigma: the onus is placed in individuals to “toughen up” and ‘heal themselves’ of an unhealthy work environment.20 Second, the emphasis on self-care strategies, while well-intentioned, may also divert resources and attention away from upstream problems that are contributing to burnout in medicine.
It is time to invest in research and policy change to support novel solutions for dealing with burnout in critical care. Doing so will require a shift in thinking to prioritize efforts further upstream. The lives of drowning clinicians depend on it.
References
- 1.Chlan L Burnout syndrome among critical care professionals: a cause for alarm. Crit Care Alert. 2013;21:65–68. [Google Scholar]
- 2.Embriaco N, Azoulay E, Barrau K, et al. High level of burnout in intensivists: prevalence and associated factors. American Journal of Respiratory and Critical Care Medicine. 2007;175(7):686–692. [DOI] [PubMed] [Google Scholar]
- 3.Mikkelsen M, Anderson B, Bellini L, Schweikert W, Fuchs B, Kerlin M. Burnout, and fulfillment, in the profession of critical care medicine. American Journal of Respiratory and Critical Care Medicine. 2019;200(7):931–933. [DOI] [PubMed] [Google Scholar]
- 4.Sharp M, Burkart K, Adelman M, et al. A national survey of burnout and depression among fellows training in pulmonary and critical care medicine: a special report by the Association of Pulmonary and Critical Care Medicine Program Directors. Chest. 733;159(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta A, Lockhart S, Reed K, et al. Drivers of Burnout Among Critical Care Providers: A Multicenter Mixed-Methods Study. Chest. 2021;article in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Mol MMC, Kompanje EJO, Benoit DD, Bakker J, Nijkamp MD. The Prevalence of Compassion Fatigue and Burnout among Healthcare Professionals in Intensive Care Units: A Systematic Review. Plos One. 2015;10(8). doi: 10.1371/journal.pone.0136955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Browning S Burnout in critical care nurses. Critical Care Nursing Clinics of North America. 2019;31(4):527–536. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Burn-out an “occupational phenomenon”: International Classification of Diseases. Published 2019. https://www.who.int/mental_health/evidence/burn-out/en/
- 9.Mealer M Burnout syndrome in the intensive care unit future directions for research. Annals of the American Thoracic Society. 2016;13(7):997–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seaman J, Cohen T, White D. Reducing the stress on clinicians working in the ICU. JAMA. 320(19):1981–1982. [DOI] [PubMed] [Google Scholar]
- 11.Salyers M, Bonfils K, Luther L, et al. The Relationship Between Professional Burnout and Quality and Safety in Healthcare: A Meta-Analysis. Journal of General Internal Medicine. 2017;32(4):475–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–2281. doi: 10.1016/s0140-6736(16)31279-x [DOI] [PubMed] [Google Scholar]
- 13.Chuang CH, Tseng PC, Lin CY, Lin KH, Chen YY. Burnout in the intensive care unit professionals A systematic review. Medicine. 2016;95(50). doi: 10.1097/md.0000000000005629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McKinlay JB. A case for refocusing upstream: the political economy of illness. International Association for Population Health Sciences Reprinted with permissions from the American Heart Association. Published online November 18, 2019. Accessed January 6, 2022. https://iaphs.org/wp-content/uploads/2019/11/IAPHS-McKinlay-Article.pdf [Google Scholar]
- 15.Metzl J, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Social Science & Medicine. 2014;103:126–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being, National Academy of Medicine, National Academies of Sciences, Engineering, and Medicine. Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. National Academies Press; 2019:25521. doi: 10.17226/25521 [DOI] [PubMed] [Google Scholar]
- 17.Schleiter K, Johnson L. Federal Bills Raise Cap on Medicare-Funded Residency Positions and Modify Graduate Medical Education Policies. Journal of Graduate Medical Education. 13(4):602–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moss M, Good V, Gozal D, Kleinpell R, Sessler CN. A Critical Care Societies Collaborative Statement: Burnout Syndrome in Critical Care Health-care Professionals. A Call for Action. American Journal of Respiratory and Critical Care Medicine. 2016;194(1):106–113. [DOI] [PubMed] [Google Scholar]
- 19.Kleinpell R, Moss M, Good VS, Gozal D, Sessler CN . The Critical Nature of Addressing Burnout Prevention: Results from the Critical Care Societies Collaborative’s National Summit on Prevention and Management of Burnout in the ICU. Critical Care Medicine. 2020;48(2):249–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shanafelt T Physician burnout: stop blaming the individual. NEJM Catalyst. Published online 2016. Accessed January 18, 2022. 10.1056/CAT.16.0806 [DOI] [Google Scholar]


